- 1Department of Biomedical and Biotechnological Sciences, Section of Anatomy, Histology and Movement Science, School of Medicine, University of Catania, Catania, Italy
- 2Department of Coaching Science, Lithuanian Sports University, Kaunas, Lithuania
- 3Research Center on Motor Activities (CRAM), University of Catania, Catania, Italy
- 4Department of Biology, Sbarro Institute for Cancer Research and Molecular Medicine, College of Science and Technology, Temple University, Philadelphia, PA, United States
Introduction: Wheelchair basketball (WB) is a Paralympic sport ideated for people with motor disabilities, and the research on this topic still requires attention. It is fundamental to evaluate physical fitness characteristics with appropriate tests and standardized routines to plan and monitor the training. Considering that a standard operating procedure is a document that makes the test battery replicable, the objective of the present study was to review the literature on physical fitness assessment in WB players and to create a standard operating procedure.
Methods: Studies were collected from different databases, and after a screening process, data were discussed narratively.
Results: Only 18 articles met the eligibility criteria. The test batteries presented similarities in different studies.
Conclusion: The suggested standard operating procedure consists of 10-min warm-up followed by handgrip evaluation (only if the instrument is available), 20-m sprint test, maximal pass, modified push-up, back scratch test, and the Yo-Yo intermittent recovery test adapted test Version 1.
Introduction
The Paralympic Games, an event parallel to the Olympic Games, is the most important sports competition for people with physical disabilities (amputation or limb deficiencies), nervous impairments (cerebral palsy or spinal cord-related disability), visual and intellectual impairment, or other disabilities (not included in the previous classifications) (1). One sport of the Paralympic program is wheelchair basketball (WB), and it includes athletes with motor disabilities (2). WB is characterized by high-intensity activities alternated with long recovery periods; it generally requires high levels of aerobic and anaerobic fitness (3). In the high-intensity period, WB athletes repeat short, intense exercise bouts that include rapid acceleration and deceleration, dynamic position changes, and maintaining or obtaining one’s position on the court (4).
To plan and monitor the training and know the level of the athletes, it is fundamental that a periodic evaluation is performed. Field tests are easier, faster, and cheaper to administer than laboratory evaluation (5), making them ideal during the season. As was done in other Paralympic sports (6, 7), the evaluation routine could be proposed as a standard operating procedure (SOP). An SOP is a document that provides details of a process to allow for a correct repetition of the various steps, to make the testing session replicable, and to ensure the normalization of data (8). For the above reasons, the objective of this study was to review the literature to propose an SOP to evaluate physical fitness with field tests in WB players.
Materials and methods
Participants included were elite athletes practicing WB. No limitations were adopted related to the intervention. For comparison, physical fitness had to be evaluated with field tests. Only English-written original manuscripts were included.
Studies were collected from PubMed, Web of Science (WoS), and Scopus databases, if published before July 22, 2022. The keywords wheelchair basketball, wheel chair basketball, wheelchair basket and physical fitness, sports physiology, and performance analysis were matched by adopting the Boolean operator AND/OR.
Field tests adopted to evaluate health-related physical fitness components (cardiorespiratory endurance, muscular strength and endurance, flexibility, and body composition) as classified by Caspersen et al. (9) were considered.
Results and discussion
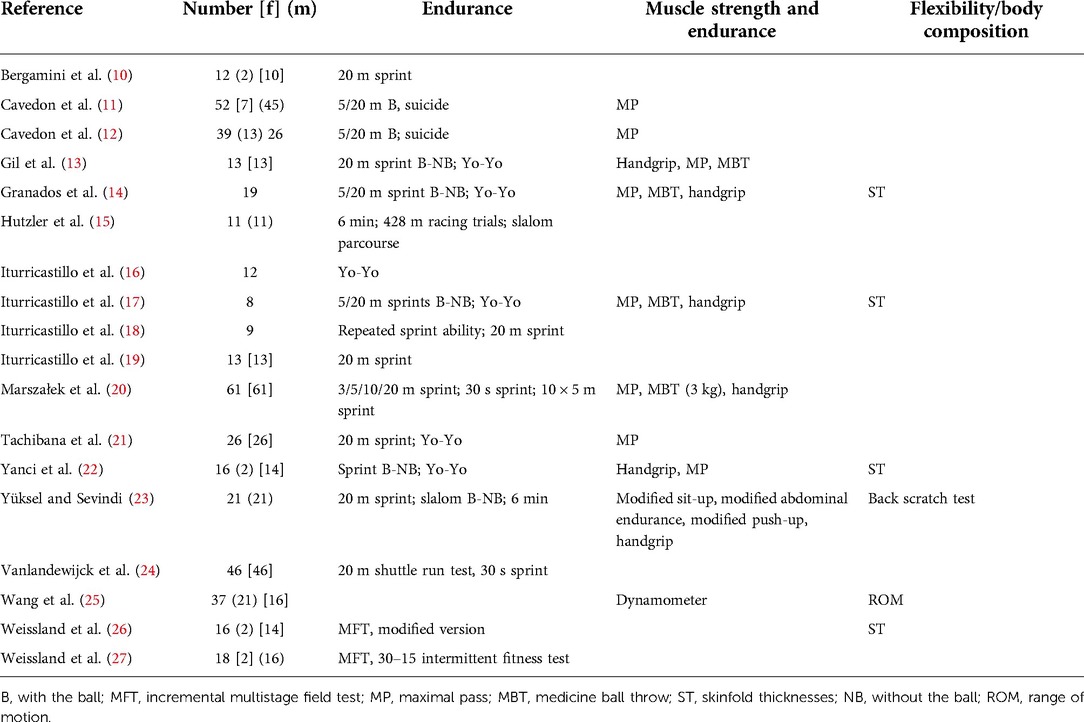
A total of 349 (155 PubMed, 166 WoS, 28 Scopus) articles were found. After duplicate removal, 292 manuscripts were detected. A total of 18 studies were analyzed after the eligibility criterion selection. The sample of the studies included ranged from 8 to 61 athletes, and the adopted tests were heterogeneous. More details about the analyzed physical fitness test sets are provided in Table 1.
Cardiorespiratory endurance
The most adopted test (n = 6) to evaluate cardiorespiratory endurance was the Yo-Yo intermittent recovery adapted test Version 1. The protocol adopted was previously published (28), and it was adapted to the athlete's conditions (22). The test consisted of 10-m wheelchair shuttle runs with increased velocities, alternated with 10 s of active recovery until exhaustion (the athlete failed twice to reach the front line in time or felt unable to cover another shuttle at the dictated speed). The total distance covered during the test was measured. This test is included in our SOP not only because it is the most used test but also because the Yo-Yo test is, generally, a valid and simple method to collect data on the capacity of the athlete to perform repeated intense exercise (29). Other adopted tests were the suicide test, the incremental multistage field test and its modified version (n = 2), the 20-m shuttle run test, the repeated sprint ability test (12 × 20 m every 20 s or 10 × 5 m version), and the 30–15 intermittent fitness test (n = 1). Other tests adopted to evaluate cardiorespiratory endurance were 6 min continuous wheeling around an elliptical concrete track of 107 m circumference (n = 2), 428-m racing trial (n = 1), and a unique wheelchair slalom parcourse, including 15 direction changes and four short sprints of 10 m each (n = 1).
Widely adopted was the 20-m sprint test (n = 11). The protocol of Gorostiaga et al. (30) was followed by four authors: it consists of three maximal wheelchair sprints alternated with 120 s of rest, with the best value adopted for analysis. The participants were placed at 0.5 m from the starting point and began when they felt ready. An option was to detect split times at 5 (31) and 20 m (24). Two maximal sprints were adopted in two studies (17, 19, 21). Cavedon et al. (11) asked to start the test to a proper signal. The same protocol was proposed in four studies (11, 13, 14, 22) with the ball, following the official game rules for dribbling (31). A similar protocol was adopted by Cavedon et al. (12). Other distances adopted were 5 (n = 5), 3, and 10 m (n = 1). Less adopted sprint evaluation (n = 2) consisted of a 30-s sprint test.
Muscle strength and endurance
The handgrip evaluation was used in five studies. It was measured in the dominant hand, with the arm in extension and in the vertical axis. The participants performed the test seated in their wheelchairs with the arm fully extended and not touching the wheelchairs (32). The testing protocol consisted of three maximal isometric contractions for 5 s, with a rest period of at least 60 s. The highest value was used for analysis. The dynamometer had to be squeezed as hard as possible. Visual feedback on the recorded strength was provided. Bilateral handgrip was measured by Marszalek et al. (20), and the combination of the value for the right and left hands was recorded. This test presents validity and reliability (33, 34), making it ideal for strength evaluation. Muscle strength was also measured at the shoulder, elbow, and wrist joints of the dominant arm using a dynamometer (25).
The maximal pass was adopted in five studies. Front wheels behind a line, in a stationary position (one researcher holds the basketball wheelchair still), participants had to pass a basketball ball with a two-arm overhand throw as far as possible. The distance between the participant and where the ball hit the floor was measured (meters). The end score was the average distance of five passes. The tested domain was passing (explosiveness) (31). A similar version was also used (11, 12) with a basketball chest pass using both arms as symmetrically as possible (20). Tachibana et al. (21) adopted a similar procedure but evaluated three types of passes: chest, baseball, and hook pass. The medicine ball throw was also adopted in five studies (four studies adopted a 5 kg ball, while one study adopted a 3 kg ball), but it was not suggested in the SOP because it requires specific equipment.
Muscle endurance was evaluated with the modified sit-up, modified abdominal endurance, and modified push-up (23). Among these tests, the modified push-up is the one that can be adopted in the SOP because it evaluates the strength of the upper body and is an indicator of different health outcomes, such as perceived health, mobility, and disability (35). Furthermore, this test presents reliability and a test–retest variation that is small (36).
Flexibility
To evaluate shoulder flexibility, the back scratch test (n = 1) has been adopted following a previously published protocol (37). From a sitting position with the back vertical, the distance (centimeters) was measured between the second finger of the two hands placed behind the back: if the fingers were in contact, the value was 0. One arm reached over the shoulder and the other one down the back. This test is included in the Brockport Physical Fitness test manual (38), making it ideal for people with disabilities. The range of motion of the shoulder, elbow, and wrist joints was also measured using a double-arm goniometer (n = 1), but since it requires specific tasks to be adopted, it is not suggested in our SOP.
Anthropometric variables
Skinfold thicknesses (in millimeters) were measured at four sites (triceps, subscapular, abdominal, and suprailiac) in five studies. Skinfold thickness is generally a cheap, valid, and accurate body composition measurement (39). Rather than using the four points, in the SOP, a two-point skinfold evaluation could be adopted because it is simpler and faster to administer (40).
Standard operating procedure
The SOP that could be adopted to evaluate WB athletes starts with the anthropometric and two-point skinfold evaluation. After that, participants do a 10-min warm-up, as adopted in different studies (20, 21), including sprints, ball-handling, passing, shooting, propelling the basketball wheelchair around the court, and the dynamic stretching of upper limbs and trunk. The intensity should be low to medium, and stretching exercises should be included (11, 12). The following tests could be proposed: handgrip evaluation (only if the instrument is available); 20-m sprint test, maximal pass, modified push-up, back scratch test, and the Yo-Yo intermittent recovery adapted test Version 1. Participants have to be instructed to perform all tests at maximum intensity with adequate rest between tests (15 min of rest time before the Yo-Yo test) and the possibility to practice before the test trial (11, 12). Considering the study of Cavedon et al. (11), the sequence of tests could be handgrip evaluation, 20-m sprint, maximal pass, Yo-Yo test, with at least 2-min rest between the tests. During data collection, each participant used their basketball wheelchair. No indication for the propulsion strategy is given, and players freely use their push rate and modality (27).
An important limitation of the present study is the poor number of included studies, but this highlights the importance of future original articles on this topic. The proposed SOP is in its first step in which published articles are analyzed, and the conclusions are made from other studies’ results. In the next step, the validity and feasibility of the SOP should be analyzed with original studies.
Conclusion
The creation of an SOP for the physical fitness evaluation of WB athletes will help researchers further develop this topic, working in the same direction all over the world. In this way, it will be possible to compare the findings and create normative data according to the players’ level and experience. The SOP will also be useful for coaches to compare their team data to better understand the level and plan the training appropriately.
Author contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Webborn N, Van de Vliet P. Paralympic medicine. Lancet. (2012) 380(9836):65–71. doi: 10.1016/S0140-6736(12)60831-9
2. Seron BB, Oliveira de Carvalho EM, Greguol M. Analysis of physiological and kinematic demands of wheelchair basketball games—a review. J Strength Cond Res. (2019) 33(5):1453–62. doi: 10.1519/JSC.0000000000003069
3. Goosey-Tolfrey VL. Physiological profiles of elite wheelchair basketball players in preparation for the 2000 paralympic games. Adapt Phys Activ Q. (2005) 22(1):57–66. doi: 10.1123/apaq.22.1.57
4. Coutts KD. Dynamics of wheelchair basketball. Med Sci Sports Exerc. (1992) 24(2):231–4. doi: 10.1249/00005768-199202000-00012
5. Heyward VH. Advanced fitness assessment and exercise prescription. 3rd ed. Champaign, Illinois: Human Kinetics Books (1991). p. 1–50.
6. Petrigna L, Giustino V, Zangla D, Aurea S, Palma R, Palma A, et al. Physical fitness assessment in goalball: a scoping review of the literature. Heliyon. (2020) 6(7):e04407. doi: 10.1016/j.heliyon.2020.e04407
7. Petrigna L, Petta A, Giustino V, Leale I, Pillitteri G, Zangla D, et al. How physical fitness is evaluated in sitting volleyball players? A scoping review. J Sports Med Phys Fitness. (2022). doi: 10.23736/S0022-4707.22.13982-4
8. Petrigna L, Pajaujiene S, Delextrat A, Gómez-López M, Paoli A, Palma A, et al. The importance of standard operating procedures in physical fitness assessment: a brief review. Sport Sci Health. (2022) 18:21–26. doi: 10.1007/s11332-021-00849-1
9. Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. (1985) 100(2):126–31.3920711
10. Bergamini E, Morelli F, Marchetti F, Vannozzi G, Polidori L, Paradisi F, et al. Wheelchair propulsion biomechanics in junior basketball players: a method for the evaluation of the efficacy of a specific training program. Biomed Res Int. (2015) 2015:275965. doi: 10.1155/2015/275965
11. Cavedon V, Zancanaro C, Milanese C. Physique and performance of young wheelchair basketball players in relation with classification. PLoS One. (2015) 10(11):e0143621. doi: 10.1371/journal.pone.0143621
12. Cavedon V, Zancanaro C, Milanese C. Anthropometry, body composition, and performance in sport-specific field test in female wheelchair basketball players. Front Physiol. (2018) 9:568. doi: 10.3389/fphys.2018.00568
13. Gil SM, Yanci J, Otero M, Olasagasti J, Badiola A, Bidaurrazaga-Letona I, et al. The functional classification and field test performance in wheelchair basketball players. J Hum Kinet. (2015) 46:219–30. doi: 10.1515/hukin-2015-0050
14. Granados C, Yanci J, Badiola A, Iturricastillo A, Otero M, Olasagasti J, et al. Anthropometry and performance in wheelchair basketball. J Strength Cond Res. (2015) 29(7):1812–20. doi: 10.1519/JSC.0000000000000817
15. Hutzler Y. Physical performance of elite wheelchair basketball players in armcranking ergometry and in selected wheeling tasks. Paraplegia. (1993) 31(4):255–61. doi: 10.1038/sc.1993.45
16. Iturricastillo A, Granados C, Los Arcos A, Yanci J. Objective and subjective methods for quantifying training load in wheelchair basketball small-sided games. J Sports Sci. (2017) 35(8):749–55. doi: 10.1080/02640414.2016.1186815
17. Iturricastillo A, Granados C, Yanci J. Changes in body composition and physical performance in wheelchair basketball players during a competitive season. J Hum Kinet. (2015) 48:157–65. doi: 10.1515/hukin-2015-0102
18. Iturricastillo A, Granados C, Reina R, Sarabia JM, Romarate A, Yanci J. Velocity and power-load association of bench press exercise in wheelchair basketball players and their relationships with field-test performance. Int J Sports Physiol Perform. (2019) 14(7):880–6. doi: 10.1123/ijspp.2018-0123
19. Iturricastillo A, Yanci J, Granados C. Neuromuscular responses and physiological changes during small-sided games in wheelchair basketball. Adapt Phys Act Q. (2018) 35(1):20–35. doi: 10.1123/apaq.2016-0139
20. Marszalek J, Kosmol A, Morgulec-Adamowicz N, Mroz A, Gryko K, Klavina A, et al. Laboratory and non-laboratory assessment of anaerobic performance of elite male wheelchair basketball athletes. Front Psychol. (2019) 10:514. doi: 10.3389/fpsyg.2019.00514
21. Tachibana K, Mutsuzaki H, Shimizu Y, Doi T, Hotta K, Wadano Y. Influence of functional classification on skill tests in elite female wheelchair basketball athletes. Med. (2019) 55(11):740. doi: 10.3390/medicina55110740
22. Yanci J, Granados C, Otero M, Badiola A, Olasagasti J, Bidaurrazaga-Letona I, et al. Sprint, agility, strength and endurance capacity in wheelchair basketball players. Biol Sport. (2015) 32(1):71–8. doi: 10.5604/20831862.1127285
23. Yüksel MF, Sevindi T. Examination of performance levels of wheelchair basketball players playing in different leagues. Sports. (2018) 6(1):18. doi: 10.3390/sports6010018
24. Vanlandewijck YC, Daly DJ, Theisen DM. Field test evaluation of aerobic, anaerobic, and wheelchair basketball skill performances. Int J Sports Med. (1999) 20(8):548–54. doi: 10.1055/s-1999-9465
25. Wang YT, Chen S, Limroongreungrat W, Change LS. Contributions of selected fundamental factors to wheelchair basketball performance. Med Sci Sports Exerc. (2005) 37(1):130–7. doi: 10.1249/01.MSS.0000150076.36706.B2
26. Weissland T, Faupin A, Borel B, Berthoin S, Leprêtre PM. Effects of modified multistage field test on performance and physiological responses in wheelchair basketball players. Biomed Res Int. (2015) 2015:245378. doi: 10.1155/2015/245378
27. Weissland T, Faupin A, Borel B, Leprêtre PM. Comparison between 30 and 15 intermittent fitness test and multistage field test on physiological responses in wheelchair basketball players. Front Physiol. (2015) 6:380. doi: 10.3389/fphys.2015.00380
28. Castagna C, Impellizzeri FM, Rampinini E, D’Ottavio S, Manzi V. The Yo–Yo intermittent recovery test in basketball players. J Sci Med Sport. (2008) 11(2):202–8. doi: 10.1016/j.jsams.2007.02.013
29. Bangsbo J, Iaia FM, Krustrup P. The Yo–Yo intermittent recovery test. Sports Med. (2008) 38(1):37–51. doi: 10.2165/00007256-200838010-00004
30. Gorostiaga EM, Llodio I, Ibáñez J, Granados C, Navarro I, Ruesta M, et al. Differences in physical fitness among indoor and outdoor elite male soccer players. Eur J Appl Physiol. (2009) 106(4):483–91. doi: 10.1007/s00421-009-1040-7
31. De Groot S, Balvers IJ, Kouwenhoven SM, Janssen TW. Validity and reliability of tests determining performance-related components of wheelchair basketball. J Sport Sci. (2012) 30(9):879–87. doi: 10.1080/02640414.2012.675082
32. Molik B, Laskin JJ, Kosmol A, Marszałek J, Morgulec-Adamowicz N, Frick T. Relationships between anaerobic performance, field tests, and functional level of elite female wheelchair basketball athletes. Hum Mov. (2013) 14(4):366–71. doi: 10.2478/humo-2013-0045
33. Artero EG, Espana-Romero V, Castro-Pinero J, Ortega FB, Suni J, Castillo-Garzon MJ, et al. Reliability of field-based fitness tests in youth. Int J Sports Med. (2011) 32(3):159–69. doi: 10.1055/s-0030-1268488
34. Artero EG, Espana-Romero V, Castro-Pinero J, Ruiz J, Jimenez-Pavon D, Aparicio V, et al. Criterion-related validity of field-based muscular fitness tests in youth. J Sports Med Phys Fitness. (2012) 52(3):263–72.22648464
35. Suni JH, Oja P, Miilunpalo SI, Pasanen ME, Vuori IM, Bos K. Health-related fitness test battery for adults: associations with perceived health, mobility, and back function and symptoms. Arch Phys Med Rehabil. (1998) 79(5):559–69. doi: 10.1016/S0003-9993(98)90073-9
36. Suni JH, Oja P, Laukkanen RT, Miilunpalo SI, Pasanen ME, Vuori IM, et al. Health-related fitness test battery for adults: aspects of reliability. Arch Phys Med Rehabil. (1996) 77(4):399–405. doi: 10.1016/S0003-9993(96)90092-1
37. Dewhurst S, Bampouras TM. Intraday reliability and sensitivity of four functional ability tests in older women. Am J Phys Med Rehab. (2014) 93(8):703–7. doi: 10.1097/PHM.0000000000000078
39. Lamb KLB DA, Roberts K. Physical fitness and health-related fitness as indicators of a positive health state. Health Promot Int. (1988) 3(2):171–82. doi: 10.1093/heapro/3.2.171
Keywords: standard operating procedure (SOP), evaluation, disability, sport, performance
Citation: Petrigna L, Pajaujiene S and Musumeci G (2022) Physical fitness assessment in wheelchair basketball: A mini-review. Front. Sports Act. Living 4:1035570. doi: 10.3389/fspor.2022.1035570
Received: 2 September 2022; Accepted: 16 November 2022;
Published: 9 December 2022.
Edited by:
Donatella Di Corrado, Kore University of Enna, ItalyReviewed by:
Natasja Bosma, University of Groningen, NetherlandsElvira Padua, Università telematica San Raffaele, Italy
© 2022 Petrigna, Pajaujiene and Musumeci. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Luca Petrigna bHVjYS5wZXRyaWduYUB1bmljdC5pdA==
Specialty Section: This article was submitted to Movement Science and Sport Psychology, a section of the journal Frontiers in Sports and Active Living
 Luca Petrigna
Luca Petrigna Simona Pajaujiene
Simona Pajaujiene Giuseppe Musumeci
Giuseppe Musumeci