
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Sports Act. Living, 07 June 2021
Sec. Injury Prevention and Rehabilitation
Volume 3 - 2021 | https://doi.org/10.3389/fspor.2021.637516
This article is part of the Research TopicHighlights in Injury Prevention and Rehabilitation: 2021/22View all 9 articles
The primary purpose of this study was to examine how the type and magnitude of changes in running behavior, as a consequence of COVID-19 pandemic restrictions, influence running-related injuries. Secondarily, we aimed to examine how lifestyle and psychosocial well-being measures may influence running behavior change. An online survey was advertised to individuals over the age of 18 that currently run or have previously participated in running for exercise. The survey questions examined injury history and new injuries sustained during COVID-19 restrictions, as well as changes related to training behavior changes, training environment changes, social behaviors, and psychosocial well-being. Changes reflected differences in running behaviors prior to COVID-19 restrictions (1 month prior to COVID-19 restrictions being imposed) and during COVID-19 restrictions (May 5 to June 10, 2020). A total of 1,035 runners were included in the analysis. Current injuries sustained during COVID-19 occurred in 9.5% of the runners. Injured runners made a greater number of total changes (p = 0.031) as well as training-related (p = 0.042) and environment-related (p = 0.017) changes compared with uninjured runners. A significant relationship was found between injury and those that reported less time to exercise to changes in work environment (p = 0017). This study highlights the multi-dimensional nature of running-related injuries and the need to consider the interaction of multiple changes in running behavior, rather than isolating single factors. Greater understanding of the underlying causes of running-related injuries can help reduce the risk of future injury.
Running is one of the most accessible and popular forms of exercise, requiring minimal equipment and facilities. Over 60 million people worldwide participated in running in 2017 (Ham et al., 2009; Bureau of Labor Statistics, U.S. Department of Labor, The Economics Daily, 2016). Importantly, physical activity and running can protect and enhance physical, mental, and social components of health (Greist et al., 1979; Chan and Grossman, 1988; Penedo and Dahn, 2005; Eime et al., 2013; Xie et al., 2020). Running has been related to a 30 to 45% lower risk of mortality and a 45 to 70% lower risk of cardiovascular disease-related mortality (Lee et al., 2017). Not only can running benefit physical health but also psychological health is reported to be higher in runners and worsens when habitual runners are prevented from running (Chan and Grossman, 1988; Trost et al., 2002). Maintaining the accessibility of running is essential for achieving optimal physical and mental health benefits.
One threat to maintaining optimal running for exercise is sustaining a running-related injury (RRI), a common risk at all levels of running. In novice and recreational runners, RRI rates per 1,000 h of running range from 7 to 79.3% (Blair et al., 1987; Jakobsen et al., 1994; van Gent et al., 2007; Buist et al., 2010; Videbæk et al., 2015; Hespanhol Junior et al., 2016; Bertelsen et al., 2017). This broad range of RRI incidence may highlight inadequacies in identifying RRI risk factors. Some research indicated that specific running behaviors, like high training distance, frequencies, and intensities, are associated with running RRIs (Nielsen et al., 2012; Ramskov et al., 2018, Hulme et al., 2017). However, results remain inconsistent, with some studies that indicated no association with higher training distance and RRI, and others that reported higher training distance to be protective against RRIs (Wen et al., 1998; Kelsey et al., 2007). Changes in running behaviors also have had conflicting evidence in how they associate with RRIs (Johnston et al., 2003; Nielsen et al., 2014,?; Hulme et al., 2017). One study indicated that 25% of individuals that started a running routine sustained an RRI within their first 37 km of running (Nielsen et al., 2014). Training progressions limited to 10% weekly increases in running duration or intensity have commonly and anecdotally been proposed to minimize injury, but with inconclusive evidence (Johnston et al., 2003; Nielsen et al., 2014). One study indicated differences in injury risk between 10 and 30% with increases in weekly running distance (Nielsen et al., 2014), while another research has reported that injured runners, on average, increased weekly running distances by 32%, whereas uninjured runners increased by 22% (Nielsen et al., 2013). Inconsistencies in the validity of this recommendation could result from the same increase in external load factors, like running distance, and, thus, lead to different increases in internal mechanical load factors (e.g., tissue strain and stress) and physiological response (e.g., perceived effort), especially in the presence of fatigue (Johnston et al., 2003; Nielsen et al., 2014; Paquette et al., 2020). Therefore, it is likely that running injuries are not exclusively influenced by a change in a single training-related factor such as distance.
Indeed, to comprehensively understand RRIs, it could be less pertinent to assess isolated running behaviors and more important to identify the influence of multiple changes in a more complex framework (Bertelsen et al., 2017). For example, one study identified that 53% of injured runners made variations in running behaviors (velocity, distance, volume, and frequency) compared with 32% of uninjured runners (Ferreira et al., 2012). This complex framework can extend past running-related behaviors and into factors like physical, social, and psychological environments that influence human behavior. Thus, to better understand how multiple changes in running behavior influence RRI, it is also crucial to consider how psychological, social, and environmental factors may influence running behaviors (Paluska and Schwenk, 2000; Trost et al., 2002). For example, running offers positive social interaction, to help individuals form and maintain social relationships and promote social identity (Shipway et al., 2012; Robinson et al., 2014; Hindley, 2020; Xie et al., 2020). Engagement in physical activity, such as running, has also long been shown to be an effective treatment for social isolation, social anxiety, and depression (Petruzzello et al., 1993; Paluska and Schwenk, 2000; Barber et al., 2005; Blumenthal et al., 2012; Anderson and Shivakumar, 2013; Liu et al., 2015). Furthermore, environmental factors like access to facilities and safe running environments have impacted activity behavior, with the Centers for Disease Control and Prevention previously reporting a significant positive association between perceived neighborhood safety and physical activity (From the Centers for Disease Control and Prevention, 1999). For example, activity levels in urban areas have been significantly higher than in rural areas (Bauman et al., 1999; Brown et al., 1999; Brownson et al., 2000). It is plausible that fluctuations in an individual's psychological and social well-being, as well as environmental changes, may present an influence in running behaviors. Thus, knowing that alterations in running behaviors have potential to influence RRI risk, environmental, social, and psychological factors should be considered.
With the recent worldwide pandemic of coronavirus disease 2019 (COVID-19), individuals have been forced to alter their daily lifestyle and exercise behaviors due to changes such as closures of fitness facilities, changes in work and home obligations, and novel isolation protocols. For example, recent work studying youth long-distance runners found that COVID-19 social distancing restrictions impacted training habits (Bazett-Jones et al., 2020). Furthermore, recent studies have illustrated that physical activity levels during the COVID-19 global pandemic have decreased (Castañeda-Babarro et al., 2020; Gallè et al., 2020; Eek et al., 2021; Fearnbach et al., 2021; Puccinelli et al., 2021; Wilke et al., 2021). Self-reported moderate physical activity levels have been reported to decrease by 41%, while Eek and colleagues depicted that more than 65% of the participants reported changes in their physical activity (Eek et al., 2021; Wilke et al., 2021). Such forced changes from a known, habitual lifestyle to novel pandemic restrictions provided a unique scenario to investigate how new environmental, social, and psychological barriers influence running behaviors and RRI risk in a large sample. The primary purpose of this study was to identify (1) if COVID-19 restrictions influenced the magnitude, direction of change (increase, decrease, and no change), and total quantity of changes in running behavior (volume, intensity, surface type, route location, and running schedule) relate to RRIs, and (2) how lifestyle, psychological and demographic factors may influence changes in running behaviors due to COVID-19 restrictions. We first hypothesized that (1) larger magnitudes of change and more total changes in volume, intensity, route variability, and surface type would relate to RRIs, and (2) increased loneliness and negative affect may relate to RRIs.
Participants qualified for this study if they were over 18 years of age and if they were currently running for exercise. Participants also qualified if they were not currently running, but had recent, previous history of running within the past year. We aimed to collect these individuals with recent, previous history of running for exercise to identify if individuals stopped running due to COVID-19. This study was approved by Auburn University's Institutional Review Board (protocol number: 20-221 EX 2004), and only responses from participants who consented to participate were recorded and used for analysis. Participants were recruited through snowball sampling via social media platforms and running communities on social media platforms (Twitter, Instagram, Facebook), email, and word of mouth.
An anonymous online survey was created and hosted on the survey platform Qualtrics (Qualtrics Labs Inc). Qualtrics is a university-approved and secure survey platform that allows participants to enter the survey through a link on their home browsers or mobile devices. The survey was created by three researchers experienced in data collection, running and locomotion research, and running exercise, allowing for comprehensive collaboration, distribution, and interpretation of the survey. All researchers and other researchers in respective laboratories looked over the survey for clarity. The survey was reviewed by three experts and pilot tested in 20 individuals similar to the target group to ensure clarity of questions and rating scales. No major changes were suggested.
The survey included questions examining injury details, training-related changes, environment-related changes, social-related changes, and psychosocial well-being (Supplementary Material). To identify the changes in injuries and running behaviors, participants were asked in reference to before and after major COVID-19 lockdown restrictions in their geographical area. This survey was administered during the first COVID-19 lockdown procedures; meaning, individuals were largely transitioning from prior normalcy to first shift in lifestyle changes. Data reflecting “during COVID-19” were collected from May 5, 2020, through June 10, 2020, and data reflecting “before COVID-19” were collected 1 month prior to the introduction of COVID-19 restrictions. To explore changes in running behaviors that may have been imposed by environmental and social restrictions, questions reflected current behaviors (during COVID-19 restrictions) and behaviors in the month immediately before COVID-19 restrictions. Current behaviors were reflective of the period between May 5, 2020, and June 10, 2020, which included the presence of COVID-19 restrictions.
The survey also contained questions that examined participant demographics, which can be found in Table 1. These included measures such as age, sex assigned at birth, race and ethnicity, and details concerning occupation status. Sex assigned at birth was included as per APA recommendations. Racial and ethnic categories were chosen to reflect and match census categories. Occupation status included examining the proportion of participants that reported as being in full-time or part-time employment, participants that reported as unemployed or seeking employment, and the proportion of participants that reported as students or retired. We also examined to what extent (completely, partially, or not changed) work had transitioned to a remote workplace.
All RRIs were self-reported using a list of common RRIs and the same definition of RRI: “Musculoskeletal pain in the lower limbs that causes a restriction on or stoppage of running (distance, speed, duration, or training) for at least 7 days or three consecutive scheduled training sessions, or that requires the runner to consult a physician or other health professional” (Messier et al., 2018). Participants were asked, “During COVID-19, have you gotten injured running?” If the participant selected “Yes,” they could select which injury from the same list of RRIs. If the participant selected “Yes” they were classified in the injured group, indicating that they had sustained a new RRI during COVID-19. If the participant selected “No,” they were classified in the uninjured group, indicating that they had not sustained a new RRI during COVID-19. There were options for participants to write in an injury that was not listed. Participants were also asked if they had a history of RRIs. The full list of injuries and questions can be found in the Survey Document in the Supplementary Material. Participants' history of RRIs and RRIs sustained during the study period were obtained.
Questions investigating training-related running behaviors included examining the number of runs per week, weekly distance run, duration of the longest run per week, and the number of light, moderate, hard, or maximal intensity runs completed per week. The proportion of runs completed at each intensity was also calculated by dividing the number of runs at a particular intensity per week by the overall number of runs that week to provide an insight into the relative intensity load. Participants were asked to provide training-related running behaviors for the month leading up to the COVID-19 lockdown procedures in their geographic area and their training-related running behaviors currently during the first COVID-19 lockdown. The difference between current training-related running behaviors and before COVID-19 training-related behaviors was calculated to determine a change score, categorized as a decrease, increase, or no change for that specific running behavior.
Environment-related running behaviors included questions examining both running routes and running surface types. Participants were asked if they ran on mostly different routes, sometimes ran on different routes, or never ran on different routes before and during COVID-19 procedures. Participants were also asked how many times per week, they ran on different surface types before and during COVID-19 procedures. These surface types included the treadmill, inside and outside running tracks, outside rural and urban roads, outside on trails, and outside on the grass. Typical running routes and running surface types were asked regarding both the month leading up to COVID-19 restrictions and current environment-related running behaviors. Change scores, reflecting the difference between current and before COVID-19 environment-running behaviors were calculated to determine increases, decreases, or no change in particular running behaviors.
Social-related running behaviors before and during COVID-19 procedures included examining if participants ran on their own or with other people or objects. Participants were asked if they ran with members of their household, ran with teammates or a social group, ran alone inside on a treadmill, or ran alone. Responses were categorized into solidarity (ran alone inside on a treadmill and ran alone) and group-based running behaviors (they ran with members of their household, ran with teammates or a social group, ran with dog, and ran with stroller). Social-related running behaviors were asked both before COVID-19 restrictions and current social running behaviors during COVID-19. A shift from any group-based running behaviors to solidarity running behaviors was classified as a decrease in social-related running behaviors, and a shift from solidary running behaviors to group-based running behaviors was classified as an increase in social-related running behaviors.
The 20-item self-report Positive and Negative Affect Schedule (PANAS) (Watson et al., 1988) was used to measure psychological well-being. The PANAS measures emotions or feelings that an individual may experience and how they may influence actions and decision making. Positive affect refers to positive emotions and positive interactions with the environment, whereas negative affect refers to negative expressions and is associated with fear and sadness. The psychometric questionnaire contains 10 items that measure positive affect and 10 items that measure negative affect. Average positive and negative affect scores are derived from a five-point Likert scale that is used for scoring. The Likert scale offered responses of agreement, including “Very slightly or not at all, A Little, Moderately, Quite a bit, and Extremely” for each feeling or emotion, and participants were asked to “Indicate the extent you have felt this way during COVID-19.” The structure validity of the PANAS through confirmatory factor analyses have indicated overall good fit with minimal misspecification of the model regarding negative affect measures (Crocker, 1997). However, PANAS scores have previously been reported as having good internal consistency (positive affect α = 0.90, negative affect α = 0.91) and test–retest reliability (DeVellis, 2003; Serafini et al., 2016). The Three-Item Loneliness Scale, adapted from the Revised—UCLA Loneliness Scale (Russell et al., 1980) was used to measure the degree of loneliness and social isolation. Participants responded to three items indicating how often they felt a lack of companionship, felt left out, or felt isolated from others. Scores were summed for each item to garner an overall loneliness score, with higher scores indicating greater loneliness. The Three-Item Loneliness Scale has been shown to display good reliability (α = 0.72) and concurrent and discriminative validity, and depict strong correlations to the full and standard measure of loneliness, the R-UCLA (DeVellis, 2003; Hughes et al., 2004).
The survey also contained questions to examine what barriers running participants may or may not have experienced. Barriers may have been reflective of restrictions put in place to mitigate the spread of COVID-19, such as reduced access to workout facilities or arisen from changes in school and work environments resulting in increased obligations and decreased time for exercise. The survey also contained questions relating to potential psychological barriers such as apprehension in exercising and lack of motivation to exercise.
All survey responses are located in the Supplementary Table. Distance, frequency, and duration per week were reported in ranges (i.e., 0–10, 10–20 miles). Intensity and surface type were reported in number of days per week. Any increase or decrease in training, and environmental and social running behaviors, regardless of magnitude, was calculated from before to after COVID-19 isolation procedure (i.e., if a participant ran 0–10 miles before COVID-19 procedures and 10–20 miles during COVID-19 procedures, this was coded as an increase). Calculating proportions allowed interval data for statistical analysis. Data on intensity and surface types were collected in days out of the week (i.e., participant ran at a moderate intensity 2 days a week, or a participant ran on an outdoor track surface 2 days a week). Because we had discrete data and not data ranges for these outcome measures, we calculated proportions of intensity and surface type by the number of reported times per week running a certain intensity or on a certain surface divided by the total number of reported days (i.e., 2 days running at moderate intensity of a total 4 days running would equate to a proportion of 0.5). A change in proportions was calculated by the difference between the value during COVID-19 procedures and the value reported during the month prior to COVID-19 procedures. All statistical analyses were performed using IBM SPSS Statistics software program version 26 (SPSS Inc. Chicago, IL, USA), and level of significance was set to p < 0.05.
Runners were grouped into an injured group (indicating that they had sustained a new RRI since COVID-19 restrictions), and an uninjured group (indicating they had not sustained a new RRI since COVID-19 restrictions). For the purposes of comparing continuous scores (such as proportions, PANAS, and loneliness scores) between runners who had sustained and who had not sustained a new RRI during COVID-19, the Mann–Whitney U was conducted. This test is a non-parametric counterpart to the independent samples t-test and is more appropriate in cases of unbalanced design and where parametric assumptions are unlikely to be met (Strunk and Mwavita, 2020). In the present study, the group sizes were heavily imbalanced, making this test the more appropriate choice. For analyses testing association of categorical variables, such as yes/no questions, with injury status, we used chi-square tests of independence. This tests the independence of group membership on two categorical variables and is thus appropriate to those questions. An ordinary least squared (OLS) regression analysis was conducted to assess the relationship between PANAS and loneliness scores and changes in the various domains (training, environmental, and social) of running behavior. Finally, to test the association of continuous variables with one another, we used Pearson product-moment correlation coefficients.
Data collection took place from May 5, 2020, through June 10, 2020. A total of 1,158 participants completed the survey; however, only 1,035 participants were included in the main analysis identifying associations among running behaviors, psychological well-being, and RRIs. One hundred nineteen participants were excluded as they reported that they were not currently running for exercise, and a further four participants were removed as their responses to open-ended items were clearly derogatory, non-sensical, or indicated they did not intend to provide a valid response. Of the participants who were not currently running for exercise, 13% (n = 16) had stopped running due to changes induced by COVID-19.
During COVID-19, 9.5% of the participants sustained a new injury. Prior history of injury was associated with reported new RRIs (χ21 = 20.396, p < 0.001), with those with a history of prior injuries overrepresented in the injured group [standardized residual (SR) = 3.10]. Of injured participants, 70.7% had history of prior injuries compared with only 46.7% of uninjured participants. Six percent of injured participants sustained a stress fracture or reaction type injury. Injuries were sustained to the foot (10.1%), ankle (10.1%), lower leg (24.2%) lower back (4%), pelvis or hip (10.1%), thigh (13.1%), and knee (13.1%). The types of injuries reported can be observed in Table 2.
There were no significant differences in Pre-COVID training-related running behavior such as frequency (Z = −0.723, p = 0.470), distance (Z = −0.810, p = 0.418), duration (Z = −0.711, p = 0.477), light intensity (Z = −0.611, p = 0.541), moderate intensity (Z = −0.533, p = 0.594), hard intensity (Z = −1.023, p = 0.306), and maximal intensity (Z = −0.966, p = 0.334) between those that got injured and those that did not get injured. There was also no difference in the proportion of days training at light duration (Z = −1.255, p = 0.210), moderate (Z = −0.964, p = 0.335), hard (Z = −0.993, p = 0.321), or maximal (Z = −1.003, p = 0.316) intensities between the injured and uninjured. Furthermore, there was no significant difference in the proportion of days running on a particular surface type, including treadmill (Z = −0.363, p = 0.717), indoor track (Z = −0.715, p = 0.474), outdoor track (Z = −1.377, p = 0.168), rural road (Z = −0.415, p = 0.678), urban road (Z = −1.230, p = 0.219), trails (Z = −0.464, p = 0.643), or grass (Z = −0.637, p = 0.524) between the injured and uninjured runners.
We found that runners who sustained a new injury during COVID-19 made a significantly greater number of total running behavior changes (encompassing training, environment, and social factors) compared with uninjured runners (Z = −2.153, p = 0.031) (Table 3, Figure 1). Injured runners also exhibited significantly greater number of training (Z = −2.036, p = 0.042) and environmental (Z = −2.393, p = 0.017) changes in running behavior compared with uninjured runners. No significant difference between injured and uninjured runners were observed in the number of social changes in running behavior (Z = −1.712, p = 0.087).
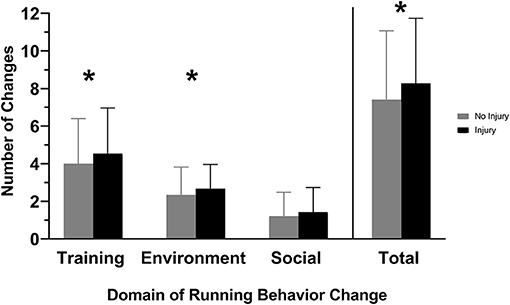
Figure 1. Injured refers to runners who sustained a new running-related injury (RRI) during COVID-19 restrictions. Uninjured refers to runners who did not sustain a new RRI during COVID-19 restrictions. Injured runners exhibited a greater number of changes in training and environment-related running behaviors, as well as cumulative overall changes. *p < 0.05.
There was a significant relationship with changes in maximal intensity (χ22 = 6.382, p = 0.041) with those increasing maximal intensity overrepresented in the group that experienced new injuries (SR = 2.289) (Figure 2). However, there was no significant relationship between those with and without new injuries with changes in distance run per week (χ22 = 0.394, p = 0.821), days run per week (χ22 = 0.507, p = 0.776), minutes of longest run (χ22 = 1.505, p = 0.471), in light intensity (χ22 = 4.807, p = 0.090), moderate intensity (χ22 = 2.380, p = 0.304), hard intensity (χ22 = 2.997, p = 0.223). When examining proportional changes in training-related running behaviors, there was a significant difference between injured and uninjured runners in proportional change in light intensity (Z = −2.296, p = 0.022) and hard intensity (Z = −2.565, p = 0.010) (Table 4, Figure 3). There was no significant difference between those with and without new injuries in proportional change in moderate intensity (Z = −0.063, p = 0.949) or maximal intensity (Z = −1.215, p = 0.224).
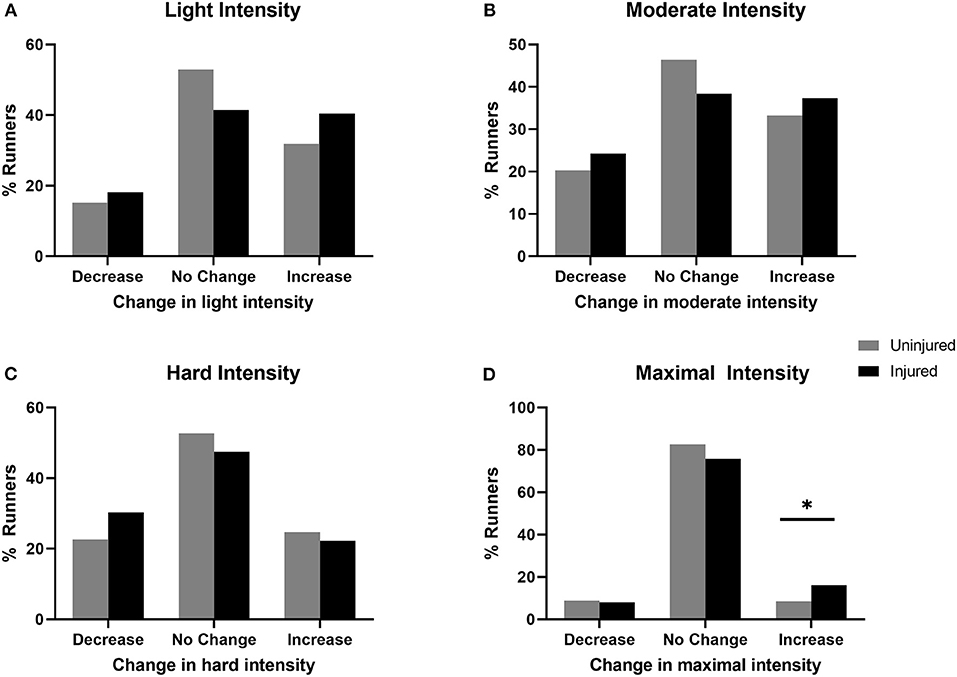
Figure 2. Injured refers to runners who sustained a new RRI during COVID-19 restrictions. Uninjured refers to runners who did not sustain a new RRI during COVID-19 restrictions. Changes in the number of days per week training at (A) light intensity, (B) moderate intensity, (C) hard intensity, and (D) maximal intensity. Chi-square test of independence revealed significant association between maximal intensity and injury group, with those increasing maximal intensity overrepresented in the injured runners. *p < 0.05.
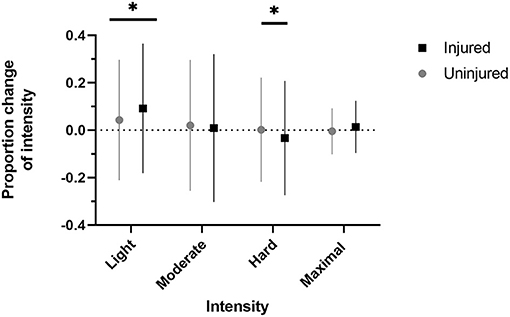
Figure 3. Injured refers to runners who sustained a new RRI during COVID-19 restrictions. Uninjured refers to runners who did not sustain a new RRI during COVID-19 restrictions. Change in the number of days spent running at a specific intensity proportional to total running intensities per week. Injured runners exhibited a relative increase in the proportion of light intensity runs and a relative decrease in the proportion of hard intensity runs. Dotted line indicates no change. *p < 0.05.
There was a significant relationship with outdoor trail running (χ22 = 6.350, p = 0.012), where those with new injuries were overrepresented among those increasing outdoor trail running (SR = 1.9) and underrepresented among those with no change in outdoor trail running (SR = −1.4) (Table 5). There were no significant relationships with changes in indoor treadmill running (χ22 = 0.151, p = 0.698), indoor track running (χ22 = 0.850, p = 0.357), outdoor track running (χ22 = 0.245, p = 0.620), outdoor rural running (χ22 = 0.158, p = 0.691), outdoor urban running (χ22 = 1.302, p = 0.254), outdoor grass running (χ22 = 0.202, p = 0.653), or changes in routes (χ22 = 3.364, p = 0.067) (Table 5).
When examining proportional changes in environment-related running behaviors, there was no significant difference between those with and without new injuries in proportional change in treadmill use (Z = −0.359, p = 0.719), indoor track running (Z = −1.312, p = 0.190), outdoor track running (Z = −0.176, p = 0.860), rural road running (Z = −1.090, p = 0.276), urban road running (Z = −0.971, p = 0.331), trail running (Z = −0.533, p = 0.594), and grass running (Z = −1.269, p = 0.205).
Regarding social running behaviors, we found no significant relationship between new injuries and changes in running alone strictly (χ22 = 1.057, p = 0.304), running alone (χ2= 0.818, p = 0.366), running in a group (χ22 = 0.781, p = 0.377), running with a dog (χ22 = 2.135, p = 0.144), or running with a stroller (χ22 = 1.911, p = 0.167).
We found a significant relationship between those that sustained a new injury and those that reported less time to exercise due to changes in work environment (χ21 = 5.716, p = 0.017). No significant relationship was reported between injury and any additional barriers, including not having access to running group (χ21 = 1.104, p = 0.294), apprehension in running alone (χ21 = 0.457, p = 0.499), lacking motivation (χ21 = 2.603, p = 0.107), stress or anxiety in leaving the home (χ21 = 0.817, p = 0.366), less time obligations (χ21 = 0.780, p = 0.378), limited access to running routes (χ21 = 0.218, p = 0.641), limited access to safe environments (χ21 = 3.574, p = 0.059), and having no access to workout facilities (χ21 = 2.249, p = 0.134).
We found no significant differences between those that sustained a new injury and uninjured runners in positive affect (Z = −0.494, p = 0.622), negative affect (Z = −1.622, p = 0.105), or loneliness scores (Z = −0.59, p = 0.953) (Figure 4). Loneliness scores were positively associated with total changes in running behaviors (r = 0.168, p <0.001, R2 = 0.028), as were negative affect scores (r = 0.072, p = 0.030, R2 = 0.005). Loneliness was positively correlated with training changes (r = 0.096, p = 0.002, R2 = 0.009), environmental changes (r = 0.141, p < 0.001, R2 = 0.020), and social changes (r = 0.119, p < 0.001, R2 = 0.014). There was no relationship between positive affect scores and total changes (r = −0.004, p = 0.913, R2 <.001). Positive affect scores were not related to training changes (r = −0.023, p = 0.476, R2 < 0.001), environmental changes (r = −0.015, p = 0.635, R2 < 0.001), or social changes (r = −0.052, p = 0.115, R2 = 0.002). Negative affect scores were not related to training changes (r = 0.039, p = 0.218, R2 = 0.002), environmental changes (r = 0.060, p = 0.063, R2 = 0.004), or social changes (r = 0.058, p = 0.078, R2 = 0.003).
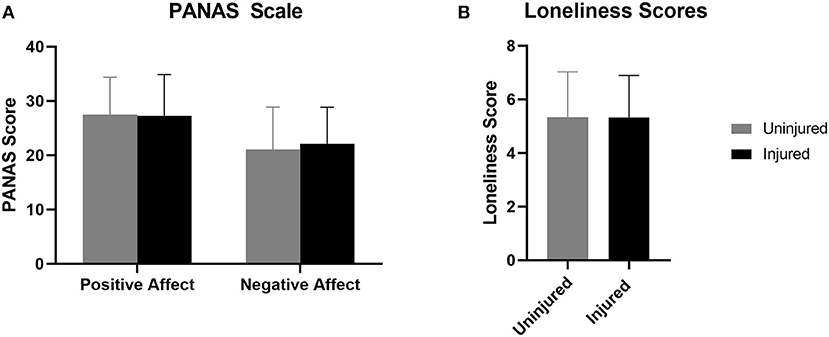
Figure 4. Injured refers to runners who sustained a new RRI during COVID-19 restrictions. Uninjured refers to runners who did not sustain a new RRI during COVID-19 restrictions. (A) Positive and negative affect and (B) measures of loneliness were not different between injured and uninjured runners.
The results of the OLS regression revealed that the combination of PANAS and loneliness scores significantly explained changes in light intensity running that were observed in response to COVID-19 restrictions [F(3, 973) = 2.838, p = 0.037], and explained about 1% of the variance in proportional changes in light intensity running (R2 = 0.009, Adj. R2 = 0.006, SE = 0.257). Positive affect scores were a significant predictor (B = 0.081, β = −0.070, t = −2.115, p = 0.035) of proportional changes in light intensity running, indicating that higher positive affect scores were negatively related to proportional changes in light intensity running during COVID-19 restrictions. Neither negative affect scores (B = 0.000, β = 0.000, t = 0.004, p = 0.996) nor loneliness scores (B = 0.007, β = 0.048, t = 1.226, p = 0.221) were significant predictors. The combination of PANAS and loneliness scores did not significantly explain changes in hard intensity running [F(3, 973) = 2.534, p = 0.056, R2 = 0.008, Adj. R2 = 0.005, SE = 0.218].
Loneliness scores were positively associated with apprehension to running alone (r = 0.163, p < 0.001, R2 = 0.027), lack of motivation (r = 0.237, p < 0.001, R2 = 0.056), and stress and anxiety of leaving home (r = 0.170, p < 0.001, R2 = 0.029). Positive affect scores were negatively associated with lack of motivation (r = −0.320, p < 0.001, R2 = 0.102), and stress and anxiety of leaving home (r = −0.140, p < 0.001, R2 = 0.020). Negative affect scores were positively associated with apprehension to running alone (r = 0.134, p < 0.001, R2 = 0.018), lack of motivation (r = 0.135, p < 0.001, R2 = 0.018), and stress and anxiety of leaving home (r = 0.313, p < 0.001, R2 = 0.10).
We report three main findings: (1) the total number of changes in running behaviors, regardless of the category of running behavior, and direction of change (increase or decrease), and changes in training and environmental running behaviors were associated with the occurrence of RRI, (2) less time to exercise, due to changes in work environment, was associated with RRIs, and (3) feelings of loneliness and positive and negative affect were associated with running behaviors and barriers linked to RRI.
Considering all categories of running behaviors (training, environmental, and social), we observed that a greater number of total changes in running behavior were associated with the occurrence of RRIs. The total changes are reflective of a combination of increases or decreases across the various categories of running behaviors (training, environmental, or social running behaviors). Total changes averaged 8.2 for injured runners, whereas uninjured runners averaged 7.4 total changes. Analyzing changes in running frequency, distance, and duration in isolation did not reveal any significant associations with RRIs. Furthermore, although the total changes were significantly different between injured and uninjured runners, the difference was, on average, approximately one behavior change. Therefore, the lack of differences among commonly reported running behaviors (frequency, distance, and duration), along with the sensitivity in total running behavior changes across training, environmental, and social behaviors, support the need to analyze RRIs in a more complex framework with many interacting components. The interaction of commonly measured running behaviors (frequency, intensity, and duration) is crucial when investigating RRIs (Nielsen et al., 2012; Bittencourt et al., 2016; Bertelsen et al., 2017). Prior research has shown that changes in training-related running behaviors may inadvertently predispose individuals to injury, while external parameters such as running surface have also been shown to influence RRIs (Buist et al., 2010; Nielsen et al., 2013). Our study outcomes reinforce recent findings from Fredette and colleagues, who reported that 75.7% of Canadian military members that suffered an RRI had made recent changes to their running behavior, just prior to injury onset (Fredette et al., 2020). Therefore, our results build upon previous findings, highlighting the need to analyze RRI risk in a complex framework, incorporating a range of training, environment, and social domains of running behaviors and internal and external factors like psychological well-being and barriers to running routines.
We observed that training and environment changes, but not social changes, were associated with the occurrence of new RRIs sustained during COVID-19 restrictions. Running intensity was the only training-related running behavior that influences the occurrence of new RRIs. In fact, ~50% more of our participants that sustained new RRI, compared with uninjured participants, increased the number of maximal intensity per week. Although high-intensity running has been previously associated with RRIs, the reporting of intensity is inconsistent (Nielsen et al., 2012). Studies identifying how running intensity influences RRIs commonly use running pace as an indicator of intensity (Nielsen et al., 2012). In our study, participants ranked perceived intensity from light, moderate, hard, and maximal. Despite the participants that sustained a new RRI reporting an increase in the number of weekly maximal intensity workouts (Figure 2D), injured participants also decreased the proportion of hard workouts and increased the proportion of light intensity workouts significantly more than uninjured runners (Figure 3). Newly injured runners, on average, decreased the proportion of hard intensity workouts by 3.3%, whereas uninjured runners increased by a slight 0.1%. Furthermore, runners that experienced a new injury increased the proportion of light intensity workouts by ~9%, whereas uninjured runners only increased by ~4%. Before COVID restrictions, there were no significant differences in any training behaviors between injured and uninjured runners. Our findings on intensity may be a product of study design. For example, it is possible that newly injured runners depicted increases in the proportion of light intensity runs in response to injury. However, our results are consistent with previous literature relating RRI with increased intensity. Specifically, identifying the injured group's increase in the number of maximal intensity workouts per week corroborates prior literature depicting an increased risk of RRI with higher-intensity running (Jacobs and Berson, 1986; Hootman et al., 2002; Nielsen et al., 2012).
Regarding environmental changes in running behavior, more injured runners reported either increasing or not changing the number of runs per week they ran on trails. In fact, 25.3% of injured runners reported increasing the number of runs per week on trails compared with 18.6% of uninjured runners. Considering that surface type is vital in considering external load factors, different surfaces can alter mechanics (Dixon et al., 2000; Bertelsen et al., 2017). Differences among surface types are associated with alterations in ground reaction forces, leg stiffness, and joint kinematics during running (Dixon et al., 2000). Furthermore, running on a grass surface, as opposed to asphalt or concrete can reduce peak pressure in the rearfoot by 16% and by 12% in the forefoot (Tessutti et al., 2012). Previous work has shown that running on concrete and asphalt can influence injury risk, showing that runners with back and thigh injuries spent less percentage of their training running on concrete and asphalt surfaces (Macera et al., 1989; Wen et al., 1997). Specifically, well-trained female runners exhibit a decrease in average loading rate while running on rubber-modified asphalt (e.g., outdoor track surfaces) compared with running on conventional asphalt (Dixon et al., 2000). Trail running has been associated with RRIs, with one study reporting one in five trail runners injured at one time (Hespanhol Junior et al., 2017). Interestingly, our injured and uninjured runners were no different in the changes of the proportion of workouts run on each surface, indicating that the absolute change, rather than the change in the proportion of trail running days relative to all running days, may be of importance when considering RRIs.
In addition to changes in running intensity and running surface types, less time to run due to changes in the work environment was significantly associated with the occurrence of RRIs. In fact, 56% of injured runners reported that they had less time to run due to changes in work environments. Our findings support recent work that examined adults' exercise levels in response to the COVID-19 lockdown, in which adults reported lack of time as a primary contributor to decreased activity levels (Constandt et al., 2020). Furthermore, the lack of time has also been a significant external barrier to exercise among University students (Gómez-López et al., 2010). Perhaps the lack of time to run due to work changes is associated with the increased total number of maximal-intensity runs observed in the injured runners. Due to time constraints, it is possible that runners sought to maximize the limited time they have by increasing the intensity of their runs. This could perhaps help explain why we observe an increase in the absolute number of maximal-intensity runs.
Contrary to our hypothesis, running-related injuries were not associated with positive and negative affect or loneliness scores. However, we did find associations between these psychosocial measures and changes in running behavior. Our results indicate that negative affect and loneliness scores were associated with a greater number of total changes in running behavior, while there was no such association with positive affect scores. These findings support recent literature highlighting alterations in physical activity behaviors in response to the COVID-19 outbreak and their association with increased adverse psychological outcomes (Duncan et al., 2020; Stanton et al., 2020). For example, it has been shown that those reporting a negative change in physical activity were more likely to have higher depression, anxiety, and stress (Stanton et al., 2020). In our study, we identified moderate effect relationships among positive affect and decreased lack of motivation, and between negative affect and increased stress and anxiety leaving the home, both with implications on psychological well-being and potential influences on physical activity behavior. Not only is it pertinent to consider the impact of alterations in physical activity behavior on measures of psychological well-being but also the relationship is bi-directional. It is plausible that subjective well-being and psychological well-being measures can also lead to changes in physical activity behavior. Therefore, it is crucial to consider both elements when analyzing running behavior change.
Strategies aimed at mitigating the spread of the virus, such as social isolation and physical distancing, shelter in place, and quarantine, despite being necessary measures to help combat the spread of the virus, can have adverse psychological impacts (Brooks et al., 2020; Duncan et al., 2020; Stanton et al., 2020; Tian et al., 2020; Wang et al., 2020). In our study, we identified small, but significant relationships among increased loneliness and increased stress and anxiety of leaving the home. Research examining the immediate psychological response to the outbreak of COVID-19 reports that 70% of participants experienced moderate–severe psychological symptoms (Tian et al., 2020). Further literature depicts that 33% of the respondents report having moderate to severe anxiety in response to the COVID-19 outbreak (Wang et al., 2020). These psychological symptoms can directly impact negative affect, which describes experiencing the world in a negative manner and is highly influenced by stress and anxiety (McIntyre et al., 1990; Magyar-Moe, 2009). Therefore, the negative psychological impact of the COVID-19 global pandemic may indirectly influence RRIs by impacting the overall number of running behavior changes.
Loneliness scores were positively associated with changes in training, environmental, and social behaviors. Social network processes and social interactions with peers and friends are highly influential factors in determining physical activity behaviors (Macdonald-Wallis et al., 2012; Montgomery et al., 2020). However, strategies to combat COVID-19 have largely compromised these factors, through the closure of public workout facilities and limiting interactions with those outside of one's household. Therefore, such policies may have caused alterations in running behaviors and forced individuals to adapt to the unprecedented circumstances. It is possible that the resultant social isolation and subsequent alterations in training, environmental, and social running behaviors may have contributed to increasing the risk of RRI.
Therefore, when examining the underlying mechanisms of running-related injuries, it is crucial to consider measures of psychological well-being. In the face of stress or adversity, such as COVID-19, or other major life stressors, many turn to exercise as means of coping strategy (Cairney et al., 2014). The moderating role of emotional competencies has the ability to influence various aspects of running behavior.
This study comes with limitations. Through the nature of the survey design, it is possible that running injuries themselves influenced changes in running behaviors. We addressed this by analyzing training-specific running variables prior to injury between injured and uninjured runners and assessing questions that addressed COVID-19 as a specific influence on running behaviors. Running related injuries were self-reported. Although we provided a valid definition of RRI, a comprehensive list of common RRIs, and the ability to report an RRI not listed, accuracy of injury type has the potential to be compromised through self-report data. Because the dates of COVID-19 lockdowns varied by geographic location, we did not collect the date of injury. However, this limits our ability to interpret the duration that training changes may influence RRI risk. Due to the nature of the survey, we did not capture exact increases or decreases in training distance, frequency, and duration. Furthermore, training run intensity was based on self-report intensity without any physiological measurements (i.e., heart rate) or scales (i.e., Borg Scale Rate of Perceived Exertion). Due to the broad sample demographics and reflective nature of the survey (i.e., reflecting on running behaviors in the month preceding COVID-19 protocols), it is likely that not all participants track their exact training metrics or have tools to measure intensity, making this method of data sampling most appropriate. There are also other aspects of training (nutrition, hydration, sleep, footwear, recovery, and warm-ups) that were not included in this survey that could influence RRI risk and also are associated with changes induced by COVID-19. Future analyses should focus on how other potential influencers of RRI are affected by psychosocial and training behaviors. Because participants spanned many locations across the United States, there is a likely variability within surface types. For example, trail surfaces may vary on how perturbed the surface is, which may influence injuries. Furthermore, although COVID-19 restrictions may have been similar in different geographic locations, it is possible that some areas were of higher risk than others, which may make specific barriers inconsistent across participants. Due to the novelties that COVID-19 presents, this survey was broad with many statistical analyses to understand the scope of associations among running behaviors, psychological well-being, and running injuries. Our survey was novel with the intentions to test during this unique time. We did not have statistics on survey validity for the running behavior portion of the survey. Future analyses should validate survey parameters and focus on particular relationships to build upon the complex nature of RRI frameworks. Due to the exploratory nature of this study and group sample sizes, we did not adjust for multiple comparisons (Keppel and Wickens, 2007; Pituch and Stevens, 2016; Strunk and Mwavita, 2020). Thus, interpretations can be taken with caution. Follow-up studies and future investigations would benefit from such analyses on multiple comparisons. Furthermore, due to the novel complications of COVID-19 on health and lifestyle, there is a possibility that results of this study may not be fully generalizable to changes in running behavior and psychological well-being outside of COVID-19.
A greater number of training, environmental, and social changes in running behaviors were associated with the occurrence of RRIs. The findings of our study highlight the importance of investigating all parameters of running (training-related, environment-related, social-related, and measures of psychological well-being), as opposed to isolating one specific aspect of running behavior. Our study highlights that individual barriers to exercise may also influence changes in running behavior. Understanding barriers associated with increased risk of injury may be useful for individuals undergoing various lifestyle changes. Runners may be forced to make multiple changes to their running routines dependent on life circumstances (i.e., moving, adjusted hours at work, new life stresses). Measures of psychological well-being were associated with running behavior and linked to RRI. Consideration of measures of psychological well-being are merited as they may serve a moderating role with respect to alterations in running behavior. Our findings highlight the importance of taking a multifactorial approach when examining RRI and suggests that exploring the impact of multiple changes may be more pertinent to garner a greater understanding of the causal mechanisms of RRI.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Participants provided consent via agreeing to the informed consent document online. The study, informed consent and method of obtaining informed consent was approved by Auburn University's Institutional Review Board.
HH, PM, and JR conceptualized the research question. HH, PM, MP, and JR distributed the survey to the participants. HH and PM wrote the first draft of the manuscript. KS conducted the statistical analysis. KS, MP, and JR contributed to the manuscript with their expertise, and read, edited, and approved the final version of manuscript. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors would like to thank those who participated in this study and all those who helped distribute and spread awareness of our study.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fspor.2021.637516/full#supplementary-material
Anderson, E., and Shivakumar, G. (2013). Effects of exercise and physical activity on anxiety. Front. Psychiatry 4:27. doi: 10.3389/fpsyt.2013.00027
Barber, B. L., Stone, M. R., and Eccles, J. S. (2005). Adolescent participation in organized activities, in What Do Children Need to Flourish? Conceptualizing and Measuring Indicators of Positive Development, eds K. A. Moore and L. H (Boston, MA: Lippman Springer), 133–146.
Bauman, A., Smith, B., Stoker, L., Bellew, B., and Booth, M. (1999). Geographical influences upon physical activity participation: evidence of a 'coastal effect'. Aust. N. Z. J. Public Health 23, 322–324. doi: 10.1111/j.1467-842X.1999.tb01265.x
Bazett-Jones, D. M., Garcia, M. C., Taylor-Haas, J. A., Long, J. T., Rauh, M. J., Paterno, M. V., et al. (2020). Impact of COVID-19 social distancing restrictions on training habits, injury, and care seeking behavior in youth long-distance runners. Front. Sports Active Living 2:179. doi: 10.3389/fspor.2020.586141
Bertelsen, M. L., Hulme, A., Petersen, J., Brund, R. K., Sørensen, H., Finch, C. F., et al. (2017). A framework for the etiology of running-related injuries. Scand. J. Med. Sci. Sports 27, 1170–1180. doi: 10.1111/sms.12883
Bittencourt, N. F. N., Meeuwisse, W. H., Mendonça, L. D., Nettel-Aguirre, A., Ocarino, J. M., and Fonseca, S. T. (2016). Complex systems approach for sports injuries: moving from risk factor identification to injury pattern recognition-narrative review and new concept. Br. J. Sports Med. 50, 1309–1314. doi: 10.1136/bjsports-2015-095850
Blair, S. N., Kohl, H. W., and Goodyear, N. N. (1987). Rates and risks for running and exercise injuries: studies in three populations. Res. Quarterly Exercise Sport 58, 221–228. doi: 10.1080/02701367.1987.10605453
Blumenthal, J. A., Smith, P. J., and Hoffman, B. M. (2012). Is exercise a viable treatment for depression? ACSM's Health Fitness J. 16, 14–21. doi: 10.1249/01.FIT.0000416000.09526.eb
Brooks, S. K., Webster, R. K., Smith, L. E., Woodland, L., Wessely, S., Greenberg, N., et al. (2020). The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 395, 912–920. doi: 10.1016/S0140-6736(20)30460-8
Brown, W. J., Young, A. F., and Byles, J. E. (1999). Tyranny of distance? The health of mid-age women living in five geographical areas of Australia. Aust. J. Rural Health 7, 148–154. doi: 10.1046/j.1440-1584.1999.00236.x
Brownson, R. C., Eyler, A. A., King, A. C., Brown, D. R., Shyu, Y. L., and Sallis, J. F. (2000). Patterns and correlates of physical activity among US women 40 years and older. Am. J. Public Health 90, 264–270. doi: 10.2105/AJPH.90.2.264
Buist, I., Bredeweg, S. W., Bessem, B., van Mechelen, W., Lemmink, K. A., and Diercks, R. L. (2010). Incidence and risk factors of running-related injuries during preparation for a 4-mile recreational running event. Br. J. Sports Med. 44, 598–604. doi: 10.1136/bjsm.2007.044677
Bureau of Labor Statistics U.S. Department of Labor The Economics Daily. (2016). Sports and exercise among Americans. Available onnline at: https://www.bls.gov/opub/ted/2016/sports-and-exercise-among-americans.htm (accessed May 04, 2021).
Cairney, J., Kwan, M. Y., Veldhuizen, S., and Faulkner, G. E. (2014). Who uses exercise as a coping strategy for stress? Results from a national survey of Canadians. J. Phys. Act. Health 11, 908–916. doi: 10.1123/jpah.2012-0107
Castañeda-Babarro, A., Arbillaga-Etxarri, A., Gutiérrez-Santamaría, B., and Coca, A. (2020). Physical activity change during COVID-19 confinement. Int. J. Environ. Res. Public Health 17:6878. doi: 10.3390/ijerph17186878
Chan, C. S., and Grossman, H. Y. (1988). Psychological effects of running loss on consistent runners. Perceptual Motor Skills 66, 875–883. doi: 10.2466/pms.1988.66.3.875
Constandt, B., Thibaut, E., De Bosscher, V., Scheerder, J., Ricour, M., and Willem, A. (2020). Exercising in times of lockdown: an analysis of the impact of COVID-19 on levels and patterns of exercise among adults in Belgium. Int. J. Environ. Res. Public Health 17:4144. doi: 10.3390/ijerph17114144
Crocker, P. R. E. (1997). A confirmatory factor analysis of the Positive Affect Negative Affect Schedule (PANAS) with a youth sport sample. J. Sport Exercise Psychol. 19, 91–97. doi: 10.1123/jsep.19.1.91
DeVellis, R. F. (2003). Scale Development: Theory and Applications (2nd ed. ed.). Thousand Oaks, CA: Sage.
Dixon, S. J., Collop, A. C., and Batt, M. E. (2000). Surface effects on ground reaction forces and lower extremity kinematics in running. Med. Sci. Sports Exerc. 2, 1919–1926. doi: 10.1097/00005768-200011000-00016
Duncan, G. E., Avery, A. R., Seto, E., and Tsang, S. (2020). Perceived change in physical activity levels and mental health during COVID-19: findings among adult twin pairs. PLoS ONE 15:e0237695. doi: 10.1371/journal.pone.0237695
Eek, F., Larsson, C., Wisén, A., and Ekvall Hansson, E. (2021). Self-perceived changes in physical activity and the relation to life satisfaction and rated physical capacity in Swedish adults during the COVID-19 pandemic-a cross sectional study. Int. J. Environ. Res. Public Health 18:671. doi: 10.3390/ijerph18020671
Eime, R. M., Young, J. A., Harvey, J. T., Charity, M. J., and Payne, W. R. (2013). A systematic review of the psychological and social benefits of participation in sport for children and adolescents: informing development of a conceptual model of health through sport. Int. J. Behav. Nutr. Phys. Activity 10:98. doi: 10.1186/1479-5868-10-98
Fearnbach, S. N., Flanagan, E. W., Höchsmann, C., Beyl, R. A., Altazan, A. D., Martin, C. K., et al. (2021). Factors protecting against a decline in physical activity during the COVID-19 pandemic. Med. Sci. Sports Exercise. doi: 10.1249/MSS.0000000000002602. [Epub ahead of print].
Ferreira, A. C., Dias, J. M. C., Fernandes, R. d., M, Sabino, G. S., Anjos, M. T. S. d., et al. (2012). Prevalência e fatores associados a lesões em corredores amadores de rua do município de Belo Horizonte, MG. Revista Brasileira Med. Esporte 18, 252–255. doi: 10.1590/S1517-86922012000400007
Fredette, M. A., Roy, J. S., Esculier, J. O., and Perreault, K. (2020). Most military runners report recent changes in running parameters before lower limb injury onset. Mil Med. doi: 10.1093/milmed/usaa524
From the Centers for Disease Control and Prevention (1999). Neighborhood safety and the prevalence of physical inactivity— selected states, 1996. JAMA 281, 1373–1373. doi: 10.1001/jama.281.15.1373
Gallè, F., Sabella, E. A., Da Molin, G., De Giglio, O., Caggiano, G., Di Onofrio, V., et al. (2020). Understanding knowledge and behaviors related to CoViD-19 epidemic in italian undergraduate students: the EPICO study. Int. J. Environ. Res. Public Health 17:3481. doi: 10.3390/ijerph17103481
Gómez-López, M., Gallegos, A. G., and Extremera, A. B. (2010). Perceived barriers by university students in the practice of physical activities. J. Sports Sci. Med. 9, 374–381.
Greist, J. H., Klein, M. H., Eischens, R. R., Faris, J., Gurman, A. S., and Morgan, W. P. (1979). Running as treatment for depression. Compr. Psychiatry 20, 41–54. doi: 10.1016/0010-440X(79)90058-0
Ham, S. A., Kruger, J., and Tudor-Locke, C. (2009). Participation by US adults in sports, exercise, and recreational physical activities. J. Phys. Act. Health 6, 6-14. doi: 10.1123/jpah.6.1.6
Hespanhol Junior, L. C., de Carvalho, A. C., Costa, L. O., and Lopes, A. D. (2016). Lower limb alignment characteristics are not associated with running injuries in runners: prospective cohort study. Eur. J. Sport Sci. 16, 1137–1144. doi: 10.1080/17461391.2016.1195878
Hespanhol Junior, L. C., van Mechelen, W., and Verhagen, E. (2017). Health and economic burden of running-related injuries in dutch trailrunners: a prospective cohort study. Sports Med. 47, 367–377. doi: 10.1007/s40279-016-0551-8
Hindley, D. (2020). More Than Just a Run in the Park”: an exploration of parkrun as a shared leisure space. Leisure Sci. 42, 85–105. doi: 10.1080/01490400.2017.1410741
Hootman, J. M., Macera, C. A., Ainsworth, B. E., Martin, M., Addy, C. L., and Blair, S. N. (2002). Predictors of lower extremity injury among recreationally active adults. Clin. J. Sport Med. 12, 99–106. doi: 10.1097/00042752-200203000-00006
Hughes, M. E., Waite, L. J., Hawkley, L. C., and Cacioppo, J. T. (2004). A short scale for measuring loneliness in large surveys: results from two population-based studies. Res. Aging 26, 655–672. doi: 10.1177/0164027504268574
Hulme, A., Nielsen, R. O., Timpka, T., Verhagen, E., and Finch, C. (2017). Risk and protective factors for middle- and long-distance running-related injury. Sports Med. 47, 869–886. doi: 10.1007/s40279-016-0636-4
Jacobs, S. J., and Berson, B. L. (1986). Injuries to runners: a study of entrants to a 10,000 meter race. Am. J. Sports Med. 14, 151–155. doi: 10.1177/036354658601400211
Jakobsen, B. W., Krøner, K., Schmidt, S. A., and Kjeldsen, A. (1994). Prevention of injuries in long-distance runners. Knee Surg. Sports Traumatol Arthrosc. 2, 245–249. doi: 10.1007/BF01845597
Johnston, C. A. M., Taunton, J. E., Lloyd-Smith, D. R., and McKenzie, D. C. (2003). Preventing running injuries. Practical approach for family doctors. Can. Fam. Phys. 49, 1101–1109.
Kelsey, J. L., Bachrach, L. K., Procter-Gray, E., Nieves, J., Greendale, G. A., Sowers, M., et al. (2007). Risk factors for stress fracture among young female cross-country runners. Med. Sci. Sports Exerc. 39, 1457–1463. doi: 10.1249/mss.0b013e318074e54b
Keppel, G., and Wickens, T. D. (2007). Design and Analysis: A Researchers Handjournal. Upper Saddle River, NJ: Academic Internet Incorperated.
Lee, D. C., Brellenthin, A. G., Thompson, P. D., Sui, X., Lee, I. M., and Lavie, C. J. (2017). Running as a key lifestyle medicine for longevity. Prog. Cardiovasc. Dis. 60, 45–55. doi: 10.1016/j.pcad.2017.03.005
Liu, M., Wu, L., and Ming, Q. (2015). How does physical activity intervention improve self-esteem and self-concept in children and adolescents? Evidence from a meta-analysis. PLoS ONE 10:e0134804. doi: 10.1371/journal.pone.0134804
Macdonald-Wallis, K., Jago, R., and Sterne, J. A. (2012). Social network analysis of childhood and youth physical activity: a systematic review. Am. J. Prev. Med. 43, 636–642. doi: 10.1016/j.amepre.2012.08.021
Macera, C. A., Pate, R. R., Powell, K. E., Jackson, K. L., Kendrick, J. S., and Craven, T. E. (1989). Predicting lower-extremity injuries among habitual runners. Arch. Intern. Med. 149, 2565–2568. doi: 10.1001/archinte.149.11.2565
Magyar-Moe, J. L. (2009). Chapter 3 - positive psychological tests and measures, in Therapist's Guide to Positive Psychological Interventions, ed J. L. Magyar-Moe (San Diego, CA: Academic Press), 43–72.
McIntyre, C. W., Watson, D., and Cunningham, A. C. (1990). The effects of social interaction, exercise, and test stress on positive and negative affect. Bull. Psychonomic Soc. 28, 141–143. doi: 10.3758/BF03333988
Messier, S. P., Martin, D. F., Mihalko, S. L., Ip, E., DeVita, P., Cannon, D. W., et al. (2018). A 2-year prospective cohort study of overuse running injuries: the runners and injury longitudinal study (TRAILS). Am. J. Sports Med. 46, 2211–2221. doi: 10.1177/0363546518773755
Montgomery, S. C., Donnelly, M., Bhatnagar, P., Carlin, A., Kee, F., and Hunter, R. F. (2020). Peer social network processes and adolescent health behaviors: a systematic review. Prev. Med. 130:105900. doi: 10.1016/j.ypmed.2019.105900
Nielsen, R. O., Buist, I., Sørensen, H., Lind, M., and Rasmussen, S. (2012). Training errors and running related injuries: a systematic review. Int. J. Sports Phys. Ther. 7, 58–75.
Nielsen, R. O., Nohr, E. A., Rasmussen, S., and Sørensen, H. (2013). Classifying running-related injuries based upon etiology, with emphasis on volume and pace. Int. J. Sports Phys. Ther. 8, 172–179.
Nielsen, R. O., Rønnow, L., Rasmussen, S., and Lind, M. (2014). A prospective study on time to recovery in 254 injured novice runners. PLoS ONE 9:e99877. doi: 10.1371/journal.pone.0099877
Paluska, S. A., and Schwenk, T. L. (2000). Physical activity and mental health: current concepts. Sports Med. 29, 167–180. doi: 10.2165/00007256-200029030-00003
Paquette, M. R., Napier, C., Willy, R. W., and Stellingwerff, T. (2020). Moving beyond weekly ‘distance' - optimizing quantification of training load in runners. J Orthop Sports Phys Ther. 50, 564–569. doi: 10.2519/jospt.2020.9533
Penedo, F. J., and Dahn, J. R. (2005). Exercise and well-being: a review of mental and physical health benefits associated with physical activity. Curr. Opin. Psychiatry 18, 189–193. doi: 10.1097/00001504-200503000-00013
Petruzzello, S. J., Landers, D. M., and Salazar, W. (1993). Exercise and anxiety reduction: examination of temperature as an explanation for affective change. J. Sport Exercise Psychol. 15, 63–76. doi: 10.1123/jsep.15.1.63
Pituch, K. A., and Stevens, J. (2016). Applied Multivariate Statistics for the Social Sciences : Analyses With SAS and IBM's SPSS. New York, NY: Routledge.
Puccinelli, P. J., da Costa, T. S., Seffrin, A., de Lira, C. A. B., Vancini, R. L., Nikolaidis, P. T., et al. (2021). Reduced level of physical activity during COVID-19 pandemic is associated with depression and anxiety levels: an internet-based survey. BMC Public Health 21:425. doi: 10.1186/s12889-021-10684-1
Ramskov, D., Rasmussen, S., Sørensen, H., Parner, E. T., Lind, M., and Nielsen, R. O. (2018). Run Clever – No difference in risk of injury when comparing progression in running volume and running intensity in recreational runners: a randomised trial. BMJ Open Sport Exercise Med. 4:e000333. doi: 10.1136/bmjsem-2017-000333
Robinson, R., Patterson, I., and Axelsen, M. (2014). The “loneliness of the long-distance runner” no more. J. Leisure Res. 46, 375–394. doi: 10.1080/00222216.2014.11950333
Russell, D., Peplau, L. A., and Cutrona, C. E. (1980). The revised UCLA loneliness scale: concurrent and discriminant validity evidence. J. Personality Soc. Psychol. 39, 472–480. doi: 10.1037/0022-3514.39.3.472
Serafini, K., Malin-Mayor, B., Nich, C., Hunkele, K., and Carroll, K. M. (2016). Psychometric properties of the Positive and Negative Affect Schedule (PANAS) in a heterogeneous sample of substance users. Am. J. Drug Alcohol Abuse 42, 203–212. doi: 10.3109/00952990.2015.1133632
Shipway, R., Holloway, I., and Jones, I. (2012). Organisations, practices, actors, and events: Exploring inside the distance running social world. Int. Rev. Sociol. Sport 48, 259–276. doi: 10.1177/1012690212442135
Stanton, R., To, Q. G., Khalesi, S., Williams, S. L., Alley, S. J., Thwaite, T. L., et al. (2020). Depression, anxiety and stress during COVID-19: associations with changes in physical activity, sleep, tobacco and alcohol use in Australian Adults. Int. J. Environ. Res. Public Health 17:4065. doi: 10.3390/ijerph17114065
Strunk, K. K., and Mwavita, M. (2020). Design and Analysis in Educational Research: ANOVA Designs in SPSS® (1st ed.). New York, NY: Routledge. doi: 10.4324/9780429432798
Tessutti, V., Ribeiro, A. P., Trombini-Souza, F., and Sacco, I. C. (2012). Attenuation of foot pressure during running on four different surfaces: asphalt, concrete, rubber, and natural grass. J. Sports Sci. 30, 1545–1550. doi: 10.1080/02640414.2012.713975
Tian, F., Li, H., Tian, S., Yang, J., Shao, J., and Tian, C. (2020). Psychological symptoms of ordinary Chinese citizens based on SCL-90 during the level I emergency response to COVID-19. Psychiatry Res. 288:112992. doi: 10.1016/j.psychres.2020.112992
Trost, S. G., Owen, N., Bauman, A. E., Sallis, J. F., and Brown, W. (2002). Correlates of adults' participation in physical activity: review and update. Med. Sci. Sports Exerc. 34, 1996–2001. doi: 10.1097/00005768-200212000-00020
van Gent, R. N., Siem, D., van Middelkoop, M., van Os, A. G., Bierma-Zeinstra, S. M., and Koes, B. W. (2007). Incidence and determinants of lower extremity running injuries in long distance runners: a systematic review. Br. J. Sports Med. 41, 469–480; discussion 480. doi: 10.1136/bjsm.2006.033548
Videbæk, S., Bueno, A. M., Nielsen, R. O., and Rasmussen, S. (2015). Incidence of running-related injuries per 1000 h of running in different types of runners: a systematic review and meta-analysis. Sports Med. 45, 1017–1026. doi: 10.1007/s40279-015-0333-8
Wang, C., Pan, R., Wan, X., Tan, Y., Xu, L., Ho, C. S., et al. (2020). Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health 17:1729. doi: 10.3390/ijerph17051729
Watson, D., Clark, L. A., and Tellegen, A. (1988). Development and validation of brief measures of positive and negative affect: The PANAS scales. J. Personality Soc. Psychol. 54, 1063–1070. doi: 10.1037/0022-3514.54.6.1063
Wen, D. Y., Puffer, J. C., and Schmalzried, T. P. (1997). Lower extremity alignment and risk of overuse injuries in runners. Med. Sci. Sports Exerc. 29, 1291–1298. doi: 10.1097/00005768-199710000-00003
Wen, D. Y., Puffer, J. C., and Schmalzried, T. P. (1998). Injuries in runners: a prospective study of alignment. Clin. J. Sport Med. 8, 187–194. doi: 10.1097/00042752-199807000-00005
Wilke, J., Mohr, L., Tenforde, A. S., Edouard, P., Fossati, C., González-Gross, M., et al. (2021). A pandemic within the pandemic? Physical activity levels substantially decreased in countries affected by COVID-19. Int. J. Environ. Res. Public Health 18:2235. doi: 10.3390/ijerph18052235
Keywords: COVID-19, injury, environment, cross-country (XC), track and field, surface, intensity
Citation: Holmes HH, Monaghan PG, Strunk KK, Paquette MR and Roper JA (2021) Changes in Training, Lifestyle, Psychological and Demographic Factors, and Associations With Running-Related Injuries During COVID-19. Front. Sports Act. Living 3:637516. doi: 10.3389/fspor.2021.637516
Received: 03 December 2020; Accepted: 08 April 2021;
Published: 07 June 2021.
Edited by:
Pascal Edouard, Université Jean Monnet, FranceReviewed by:
Alexis Ruffault, Institut national du sport, de l'expertise et de la performance (INSEP), FranceCopyright © 2021 Holmes, Monaghan, Strunk, Paquette and Roper. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jaimie A. Roper, anJvcGVyQGF1YnVybi5lZHU=
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.