- 1Cambridge Centre for Sport and Exercise Sciences, Anglia Ruskin University, Cambridge, United Kingdom
- 2Department of Cancer Epidemiology and Prevention Research, Cancer Control Alberta, Alberta Health Services, Calgary, AB, Canada
- 3Departments of Oncology and Community Health Sciences, University of Calgary, Calgary, AB, Canada
- 4Department of Behavioural Science and Health, University College London, London, United Kingdom
- 5Division of Psychology and Mental Health, University of Manchester, Manchester, United Kingdom
- 6NICM Health Research Institute, Western Sydney University, Westmead, NSW, Australia
- 7Centre for Youth Mental Health, University of Melbourne, Melbourne, VIC, Australia
- 8Cognitive Sports Therapy, Cambridge, United Kingdom
- 9Cambridge Private Doctors, Nuffield Hospital, Cambridge, United Kingdom
- 10RC Psych Sports and Exercise Psychiatry Special Interest Group, London, United Kingdom
- 11Positive Ageing Research Institute (PARI), Anglia Ruskin University, Cambridge, United Kingdom
- 12Physiotherapy Department, South London and Maudsley NHS Foundation Trust, London, United Kingdom
- 13Department of Psychological Medicine, Institute of Psychiatry, Psychology and Neuroscience, King's College London, London, United Kingdom
Despite the many benefits of regular, sustained exercise, there is evidence that exercise can become addictive, to the point where the exerciser experiences negative physiological and psychological symptoms, including withdrawal symptoms upon cessation, training through injury, and the detriment of social relationships. Furthermore, recent evidence suggests that the etiology of exercise addiction is different depending on the presence or absence of eating disorders. The aim of this study was to explore to what extent eating disorder status, body dysmorphic disorder, reasons for exercise, social media use, and fitness instructor status were associated with exercise addiction, and to determine differences according to eating disorder status. The key findings showed that the etiology of exercise addiction differed according to eating disorder status, with variables including social media use, exercise motivation, and ethnicity being uniquely correlated with exercise addiction only in populations with indicated eating disorders. Furthermore, body dysmorphic disorder was highly prevalent in subjects without indicated eating disorders, and could be a primary condition in which exercise addiction is a symptom. It is recommended that clinicians and practitioners working with patients who present with symptoms of exercise addiction should be screened for eating disorders and body dysmorphic disorder before treatments are considered.
Introduction
Exercise can be defined as “structured, intentional physical activity for improving health and fitness” (Garber et al., 2011). Benefits of regular exercise in adults (18 years and over) include lower risk of all-cause mortality, improved cognitive function, and improvements in several areas of mental health (Ashdown-Franks et al., 2019; Powell et al., 2019).
There is evidence, however, that exercise can become obsessive, compulsive, or addictive, to the point where the exerciser experiences negative physiological and psychological symptoms, including withdrawal symptoms upon cessation, training through injury, and the detriments of social relationships (Symons Downs et al., 2019; Szabo et al., 2019). Several different terms have been used to label this phenomenon, including exercise addiction, exercise dependence, compulsive exercise, and obligatory exercise. For this study, we use the term exercise addiction (EA), as it encompasses aspects of both dependence and compulsion (Szabo et al., 2015). Overall prevalence of exercise addiction appears to be 3–14% of the exercising population; however, this varies depending on the population and method of exercise addiction measurement tool (Di Lodovico et al., 2019; Marques et al., 2019; Trott et al., 2020a).
Many theoretical models have been proposed to explain EA, including the Sympathetic Arousal Hypothesis [(Thompson and Blanton, 1987), the Cognitive Appraisal Hypothesis (Szabo, 1995), the IL-6 model (Hamer and Karageorghis, 2007), Four Phase model (Freimuth et al., 2011), and the Biopsychosocial model (McNamara and McCabe, 2012)]. Most recently, Egorov and Szabo (2013) updated the Cognitive Appraisal Hypothesis with their Interactional Model of EA (Figure 1), which describes a broad range of variables being conducive to developing EA, along with the acknowledgment that several variables' connection may be two-way.
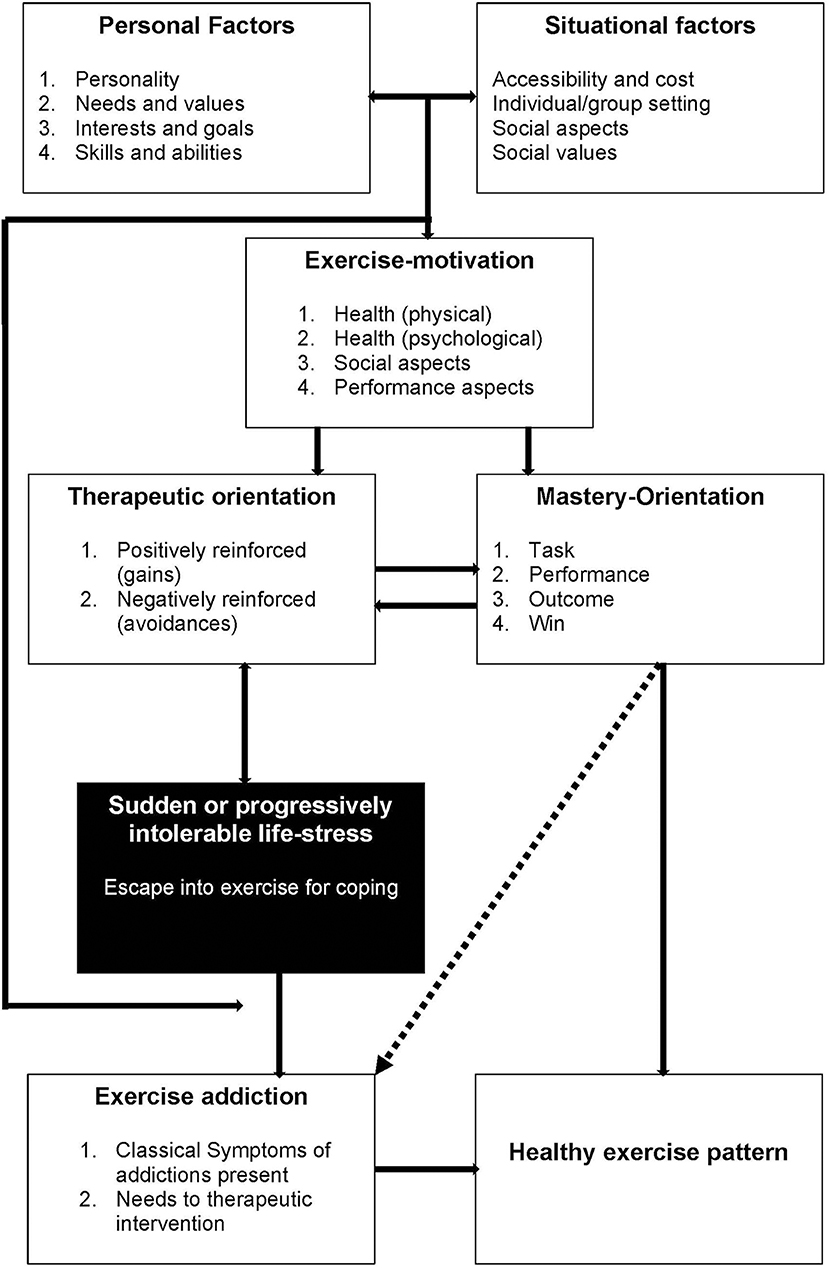
Figure 1. The interactional model of exercise addiction (Egorov and Szabo, 2013).
One of the key determinants of EA in the Interactional Model is “sudden or progressively intolerable life-stress.” The most researched of these is the presence (or absence) of eating disorders, with recent evidence concluding that subjects with indicated eating disorders have 3.5x higher risk of developing EA than subjects without indicated eating disorders (Trott et al., 2020b) broadly supporting this model. Further evidence to support this hypothesis, however, is sparse, mainly because the majority of EA literature fails to screen for the presence of eating disorders (Di Lodovico et al., 2019; Marques et al., 2019; Symons Downs et al., 2019). Another condition that could be characterized as an “intolerable life-stress” is the presence of Body Dysmorphic Disorder (BDD), a condition in which a person is concerned about real or perceived physical defects (such as body shape, skin, or hair) as repulsive (Buhlmann et al., 2009; American Psychiatric Association, 2013). Previous studies have shown BDD to be a predictor of exercise addiction in populations without indicated eating disorders (Grandi et al., 2011); however, the strength of this association in populations with indicated eating disorders is unknown. Several other correlates have been shown to associate with BDD, including social media use and sexuality, both of which have been shown to yield more negative body image feelings, with a positive relationship between time spent on social media and negative body feelings (Fardouly and Vartanian, 2016), and heterosexual women and homosexual men demonstrating higher levels of body dissatisfaction (Conner et al., 2004), indicating a potential link between EA, social media use, sexuality, and BDD. These links, however, have not been empirically explored to date.
Another key component of the Interactional Model of EA is “exercise-motivation,” although few studies have explored reasons for exercise in exercise addicted populations. Serier et al. (2018) explored reasons for exercise in subjects with high levels of body dissatisfaction and found that EA subjects scored significantly higher in measures for “exercising for mood” and “enjoyment” compared to non-exercise addicted subjects, broadly supporting the Interactional Model. It has also been suggested that subjects with EA exercise for different reasons depending on the presence or absence of an eating disorder, with subjects with no indicated eating disorders exercising “as an end to itself,” and indicated eating disordered subjects exercising to achieve another goal, such as weight loss (de Coverley Veale, 1987). Evidence to support these differing exercise motivations, however, has not been explored to date.
Further at the beginning of the Interactional Model is “personal” and “situational” factors. Of these, the amount of leisure time physical activity has been consistently shown to positively correlate with exercise addiction risk (Kovacsik et al., 2018). One unique job that could be related to EA is being a fitness instructor (especially group fitness instructors), as they are regularly required to exercise as part of their job, and have been noted at being at higher risk of fitness related injuries, especially when coupled with obligatory exercise tendencies (Thompson et al., 2001); however, whether this directly correlates with increased exercise addiction risk is yet to be explored.
Identifying the extent to which these variables are associated with EA has the potential to support, refute, or suggest modifications to the Interactional Model of EA. Furthermore, identifying how much these associations differ between subjects with and without indicated eating disorders is important, as it allows researchers to understand if there are any differences in the two populations, and therefore have suggested different etiology. The aim of this study, therefore, was to answer the following questions:
1. To what extent is eating disorder status, BDD, reasons for exercise, social media use, and fitness instructor status associated with exercise addiction in line with the Interactional Model?
Based on the Interaction Model, it is hypothesized that eating disorder and BDD status (conditions that could be considered a “sudden or progressively intolerable life-stresses”) have the strongest association with EA. Exercise-motivations are hypothesized to have a smaller association, with the personal and situational factors (fitness instructor status and social media use) showing the smallest associations.
2. Do the associations between these psychological and social variables and exercise addiction differ according to eating disorder status?
We hypothesize that some correlates will differ according to eating disorder status.
Not only will this expand the understanding of exercise addiction, its relationship with eating disorders, and its relationship with the multiple variables described above, it has the potential to inform practitioners working with potentially “at risk” groups, such as physicians and fitness industry workers. Furthermore, this study will either support or refute the most recent model of EA, which will steer the direction of future research.
Measures and Methods
Study participants were recruited via an international group fitness e-newsletter and through Facebook, Instagram, and Twitter from 8/4/19 to 31/7/19 through social media influencers and through the authors' personal social media accounts. Participants provided informed consent prior to taking part in the survey, including the right to withdraw and access to further support if any of the topics were distressing. To be eligible for the study, participants were required to be adult (>18 years) health club users. Participants were oriented to an online battery of questions hosted through an academic survey website (Jisc Online Surveys, 2020), including measures of age, sex, ethnicity, socio-economic status, life-limiting illness status, exercise addiction, leisure-time physical activity frequency, reasons for exercise, eating disorders, BDD, social media use, body mass index (BMI), and sexuality. Ethical approval was obtained from the Anglia Ruskin University Sport and Exercise Sciences Departmental Ethics Panel (ESPGR-03).
Participants
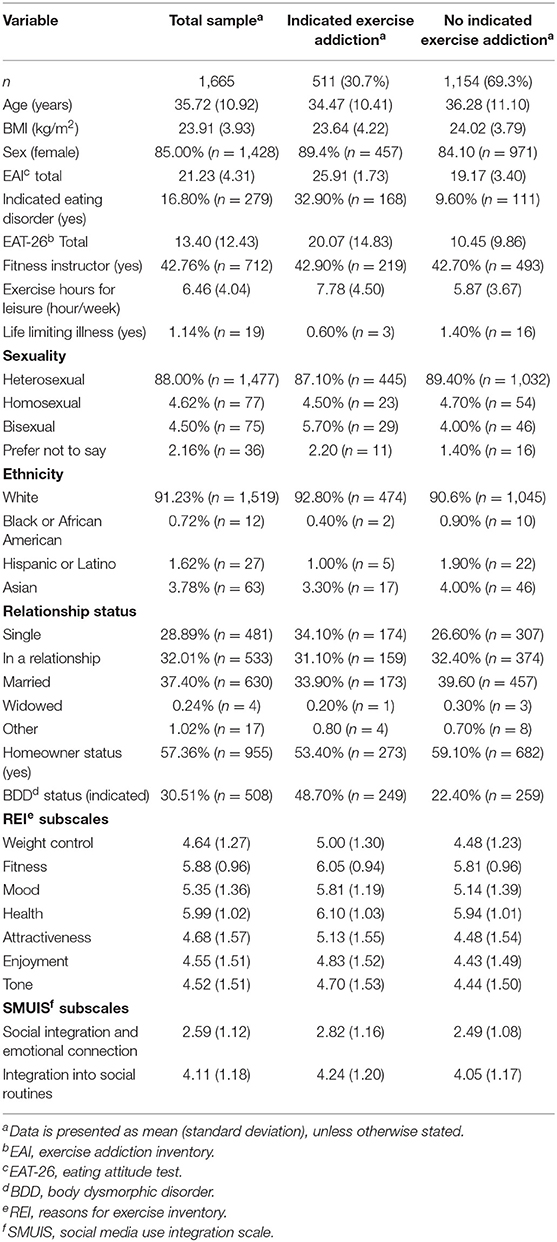
Total, 1,864 participants completed the questionnaire. Of these, 199 (10.7%) failed to confirm that they were health club users and were excluded from further analysis. Of the remaining 1,665 participants, the mean age was 35.7 years (SD = 10.9), mean self-reported BMI was 23.9 kg/m2 (SD = 3.9), and 1,428 (85.0%) subjects were female. Full demographic information is shown in Table 1.
Measures
Exercise Addiction
The Exercise Addiction Inventory (EAI) (Terry et al., 2004) is a six-item questionnaire that assesses each component of Brown's theory of addiction (Brown, 1993) in an exercise context. Each question is scored on a Likert scale of 1–5, with a higher score indicating higher risk of exercise addiction. Subjects who score ≥24 are classified as “at risk” of exercise addiction (Terry et al., 2004). The EAI has been shown to have good reliability and validity across physically active populations (Terry et al., 2004; Griffiths et al., 2015; Lichtenstein and Jensen, 2016) and shows good internal reliability in the current study (α = 0.74).
Note: Despite having a cut-off score, the EAI was used as a continuous variable indicting severity of exercise addiction risk because there are no clinically recognized diagnostic criteria for exercise addiction (American Psychiatric Association, 2013).
Social Media Use
Social media use was measured using the Social Media Use Integration Scale (SMUIS) (Jenkins-Guarnieri et al., 2013), a 10-item questionnaire with two sub-scales: social integration and emotional connection and integration into social routines. Each question is scored on a Likert scale of 1–6, with higher scores in each sub-scale indicating higher levels of its respective sub-scale. The SMUIS has shown good validity across several age ranges (Jenkins-Guarnieri et al., 2013; Maree, 2017) and shows excellent internal consistency in the current study (social integration and emotional connection sub-scale Cronbach's α = 0.88; integration into social routines sub-scale Cronbach's α = 0.81).
Reasons for Exercise
Reasons for exercise was measured using the Reasons for Exercise Inventory (REI) (Silberstein et al., 1988), a 24-item questionnaire with seven sub-scales: weight control, fitness, mood, health, attractiveness, enjoyment, and tone. Each question is scored on a Likert scale of 1–7, with higher scores in each sub-scale indicating higher levels in the respective sub-scale. The REI has been validated across several populations (Silberstein et al., 1988; Cash et al., 1994) and in the current study shows good internal consistency (Cronbach's αs: weight control α = 0.61; fitness α = 0.83; mood α = 0.86; health α = 0.86; attractiveness α = 0.85; enjoyment α = 0.82; tone α = 0.79).
BDD
BDD was measured using the Body Dysmorphic Disorder Questionnaire (BDDQ) (Phillips, 2005), a questionnaire based on the DSM-IV (American Psychiatric Association, 2000) diagnostic criteria for BDD. Classification of BDD is made based on answering positively to questions 1 and 2, at least one part of question 3, and indicating spending one or more hours each day thinking about their appearance. The questionnaire has excellent reported sensitivity (94%) and specificity (90%) in non-clinical community populations (Brohede et al., 2013).
Eating Disorder Symptoms
Eating disorder symptomology was measured using the Eating Attitudes Test 26 (EAT-26) (Garner et al., 1982), a 26-item questionnaire scored on a Likert scale of 1–6. A score of ≥20 is sufficient to be classified as having possible pathological eating behaviors. The EAT-26 has been well-validated in athletic populations (Doninger et al., 2005; Pope et al., 2015) and has shown excellent internal consistency in the current study (Cronbach's α = 0.91).
Health Club User
Participants were required to answer yes/no to indicate whether they were a current health club user.
Fitness Instructor
Participants were required to answer yes/no to indicate if they were currently a fitness instructor.
Leisure-Time Physical Activity
Participants were required to indicate how many hours per week they participated in physical activity (if the subject was a fitness instructor, this did not include exercise hours as part of work).
Data Analysis
All data were analyzed using SPSS Version 26 (IBM Corp., 2019).
Exercise addiction prevalence was also calculated in all the total sample and both indicated and non-indicated eating disorder populations.
A hierarchical multiple linear regression was run on the total sample to determine if the addition of variables significantly added to the total model with EAI score (as a continuous variable) as the dependent variable. The variables were added to the previous models in the following order:
Model 1: Age, gender, BMI, ethnicity, life limiting illness
Model 2: Eating disorder status
Model 3: BDD status
Model 4: Reasons for exercise (all items)
Model 5: Fitness instructor status
Model 6: Social media use (all items)
Model 7: Sexuality
Model 8: Exercise hours for leisure
Model 9: Relationship status
Furthermore, a linear regression was used to analyse associations between exercise addiction score (as a continuous variable) and: age, sex, BMI, ethnicity, eating disorder status, homeowner status, relationship status, both subscales of the SMUIS, all subscales of the REI, being a fitness instructor, leisure time physical activity, sexuality, and BDD status in two populations:
1. Indicated eating disorders (defined as scoring ≥20 in the EAT-26)
2. No indicated eating disorders (defined as scoring <20 in the EAT-26)
Any missing data was tested for randomness via Little's MCAR test (Little, 1988), and if confirmed random, deleted listwise from all regression analyses.
In order to explore whether associations varied according to eating disorder status, we repeated the multivariable analysis (model 9) in a series of linear regression models adding the interaction term (eating disorder status*respective variable) between eating disorder status and each potential correlate in turn (e.g., in the first analysis we included all variables in model 9 with the addiction of the variable “eating disorder status*age”; in the second analysis we included all variables in model 9 with the addiction of the variable “eating disorder status*gender”, etc.).
Results
Exercise Addiction Prevalence
The prevalence of exercise addiction, as defined by a score of ≥24 on the EAI (Terry et al., 2004), in the total sample was 30.7% (95%CI = 28.5–33.0%), 60.2% (95%CI = 54.2–66.0%) in the population who had an indicated eating disorders, and 24.7% (95%CI = 22.5–27.1%) in the population who had no indicated eating disorders.
Regression Assumption Testing
There was linearity in all samples as assessed by partial regression plots and a plot of studentized residuals against the predicted values. There was independence of residuals in all populations, as assessed by a Durbin-Watson statistic of 2.108, 1.087, and 2.036 in the total sample, indicated ED and no indicated ED samples, respectively. Homoscedasticity was as assessed by visual inspection of a plot of studentized residuals vs. unstandardized predicted values, with evidence of homoscedasticity in all three samples. There was no evidence of multicollinearity in any sample, as assessed by tolerance values >0.1. There were 23 studentized deleted residuals >±3 standard deviations, which were kept in the analysis. The assumption of normality was met, as assessed by a Q-Q Plot. The Little's MCAR test confirmed that all missing data was random (p = 0.07), and therefore were listwise deleted from all regression analyses.
Hierarchical Multiple Regression
In the total sample, each model significantly added to the total R2, apart from models 5, 7, and 9 (the respective addition of fitness instructor status, sexuality, and relationship status into the previous model). The final multiple regression model (model 9) was statistically significant [F(29, 1, 500) = 16.227, p ≤ 0.001, adj. R2 = 0.224]. The variables BMI, life limiting illness, being a fitness instructor, exercise hours for leisure, eating disorder status, REI “mood” and “enjoyment” subscales, SMUIS social integration and emotional connection subscale, BDD status, ethnicity black and Asian (vs. white) added significantly to the prediction (p ≤ 0.05). Full coefficient results and changes in R2 are shown in Table 2.
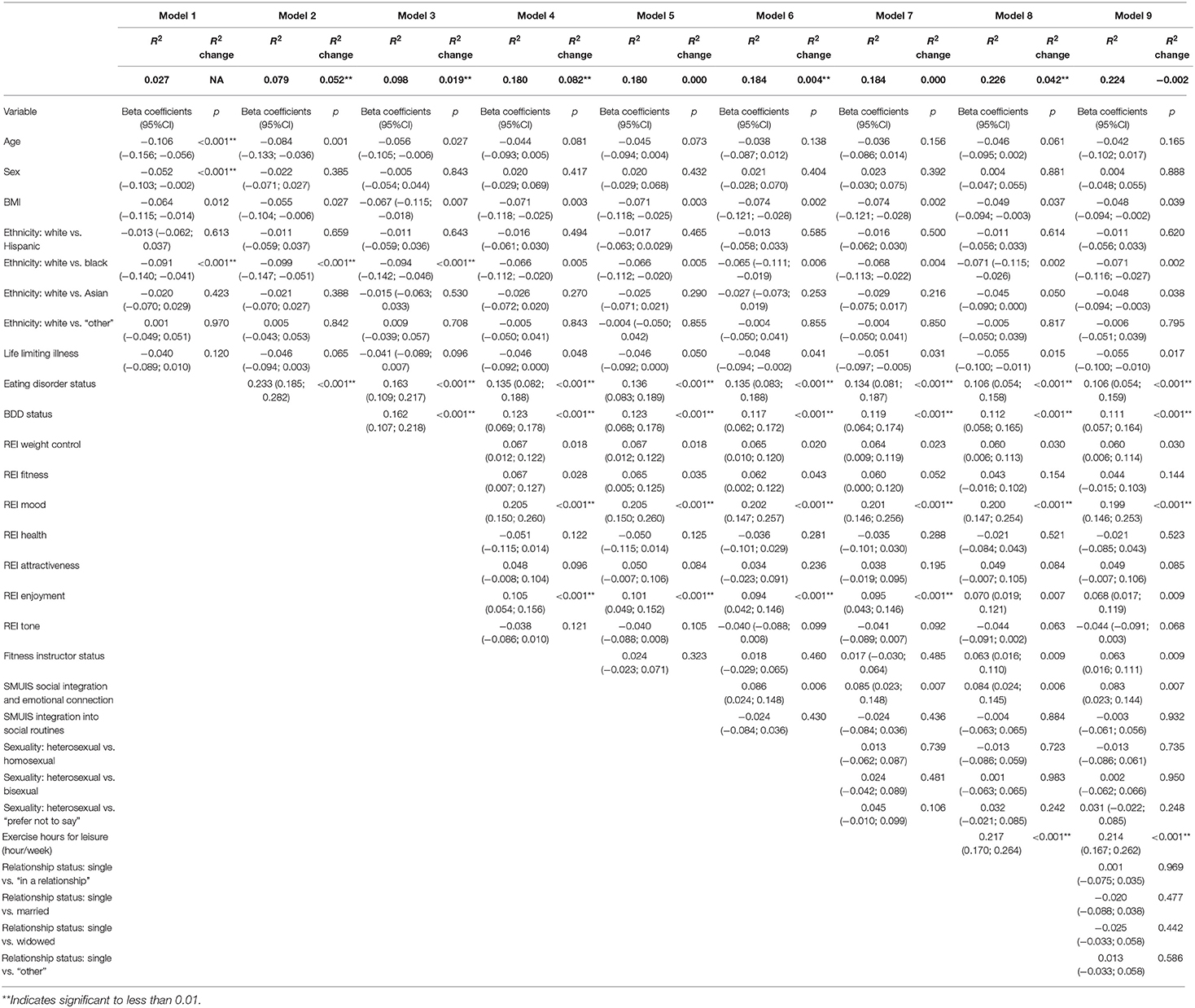
Table 2. Hierarchical regression in the total sample (exercise addiction inventory scores as the dependent variable).
Indicated vs. No-Indicated Eating Disorders Sub-groups Multiple Regression
Both populations' full regression models were statically significant [indicated eating disorders = F(27, 231) = 2.995, p ≤ 0.001, adj. R2 = 0.173; no indicated eating disorders = F(28, 1, 242) = 12.383, p ≤ 0.001, adj. R2 = 0.201]. In the indicated eating disorders population, the variables BMI, SMUIS social integration, and emotional connection subscale, and ethnicity black and Asian (vs. white) added significantly to the regression model (p ≤ 0.05). In the no indicated eating disorders population, the variables REI “mood” and “enjoyment” subscales, being a fitness instructor, exercise hours per week, and BDD status added significantly to the regression model (p ≤ 0.05). Full coefficients for both populations are shown in Table 3.
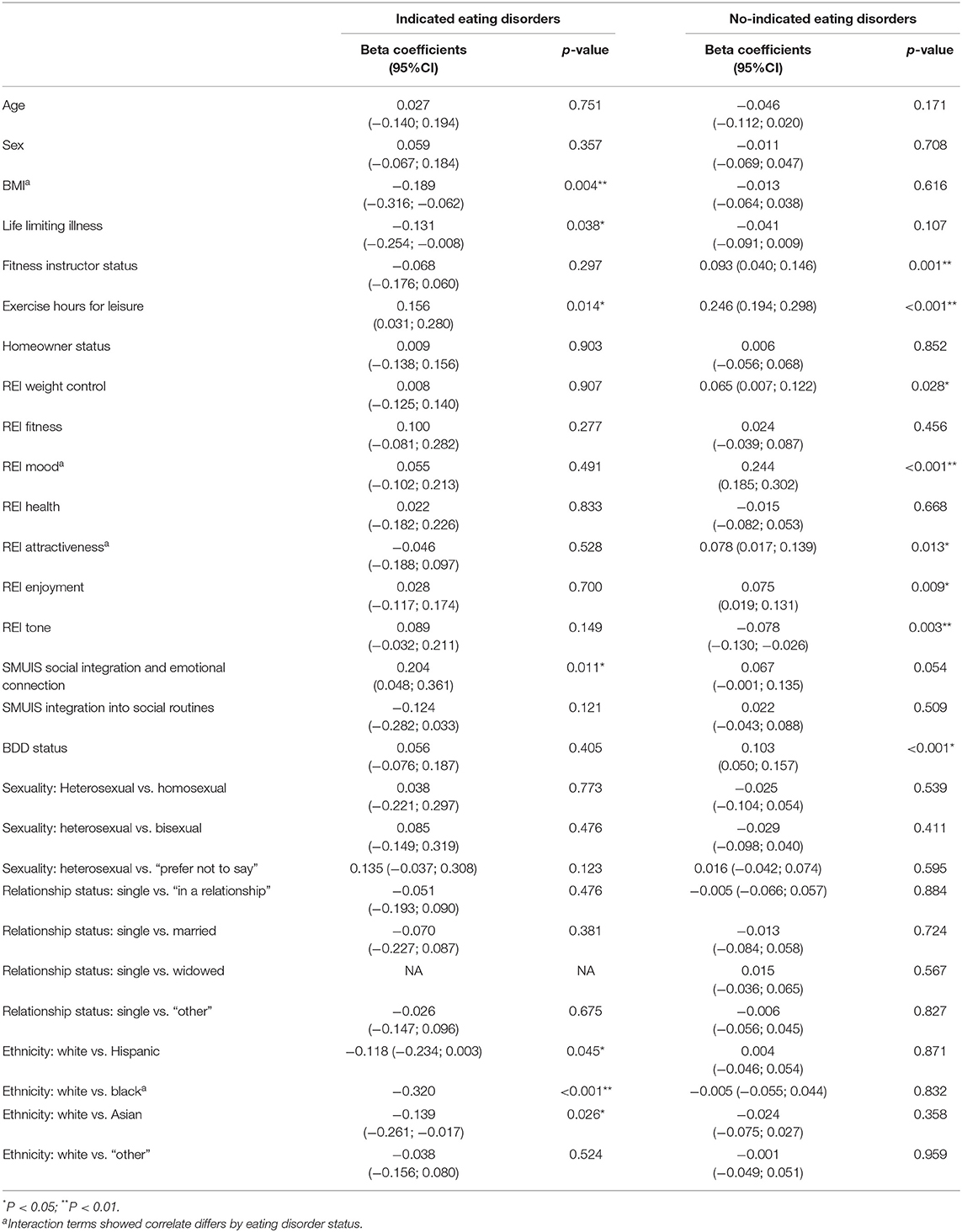
Table 3. Multiple linear regression summary of independent variables (dependent variable = exercise addiction inventory total score).
Eating Disorder Interaction Effects
There were significant interactions between eating disorder status and BMI, exercising for mood, exercising for attractiveness, and ethnicity (black vs. white). Full interaction data are shown in Table 4.
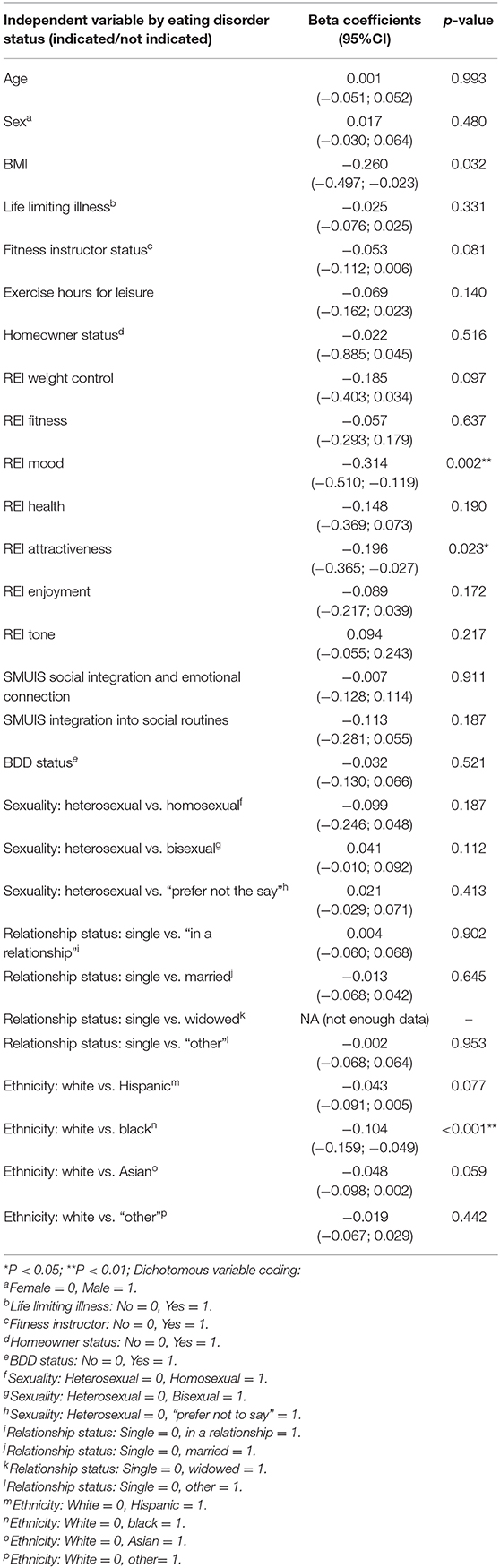
Table 4. Interaction effects between independent variables and eating disorder status (dependent variable = exercise addiction inventory total score).
Discussion
The present study explored the prevalence of exercise addiction among fitness club users, the extent to which age, BMI, gender, sexuality, social media use, BDD, fitness instructor status, eating disorder status, and reasons for exercise were associated with exercise addiction scores, and whether these correlates differed according to eating disorder status. The prevalence of exercise addiction in the total sample was 30.7%, with prevalence rates differing largely according to eating disorder status (indicated eating disorders 60.2%; no indicated eating disorders 24.7%). Characteristics associated with higher exercise addiction scores in multivariable models included: indicated eating disorder, being a fitness instructor, leisure-time physical activity, exercising to improve mood, enjoyment, and for weight control, indicated BDD, and using social media for social integration and emotional connection. Characteristics associated with lower exercise addiction scores included: a higher BMI, reporting a life-limiting illness, and ethnicity (black vs. white and Asian vs. white). There were significant interactions between eating disorder status and BMI, exercising for mood, exercising for attractiveness, and ethnicity (black vs. white).
Total Sample
The hierarchical regression showed that the addition of all variables into the model significantly increased the R2, apart from the addition of fitness instructor status, sexuality, and relationship status, indicting their limited significance in explaining the total variance in EAI scores.
As hypothesized, the strength of associations of the two variables that could be interpreted as “sudden or progressively intolerable life-stress” (eating disorder status and BDD status) in the Interactional Model of EA were among the strongest. This concurs with several studies that have shown that eating disordered subjects suffer from higher EA (Fietz et al., 2014; Trott et al., 2020b), and several studies that show that negative self-body image is positively correlated with exercise addiction (Klein et al., 2004; Ertl et al., 2018). Moreover, this provides initial evidence that these two conditions could be listed in the Interactional Model as possible intolerable life-events. Another variable that had one of the strongest associations with EA was exerting to modify mood. Although this could be interpreted as “psychological health” on the Interactional Model, it also could be dealing with a sudden or progressively intolerable life stress, such as depression or anxiety, which would place this variable into this part of the model. Furthermore, this association broadly concurs with previous studies that have found that exercising for mood is positively correlated with exercise addiction (Serier et al., 2018). Due to this, we propose a modification to the Interactional Model: adding a direct link between “exercise motivation” and “sudden or progressive intolerable life-stress.”
Unsurprisingly, leisure-time physical activity was a significant correlate of higher scores of exercise addiction, which concurs with the literature (Hausenblas and Downs, 2002; Adams et al., 2003; Allegre et al., 2007; Costa et al., 2013). One possible mechanism of this relationship could be the desire to increase levels of β-endorphins through increasing amounts of exercise, leading to a relative feeling of euphoria post-exercise (Leuenberger, 2006). Studies in other addictions have suggested that the endogenous opioid system is a key factor in generating addictions (O'Brien, 2004).
Analysis According to Eating Disorder Status
Lower BMI, using social media for social integration and emotional connection, and ethnicity (white vs. black, Hispanic, and Asian) were only positively associated with higher exercise addiction scores among health club users with indicated eating disorders, and fitness instructor status, exercising to improve mood, attractiveness, exercising for enjoyment, and BDD status were only associated with higher exercise addiction scores among health club users without an indicated eating disorder.
Lower BMI was a correlate of higher exercise addiction scores only in health club users who had an indicated eating disorder. This is consistent with the eating disorder literature which states that striving for a lower body weight (and therefore a lower BMI) via excessive exercise is a common symptom of both anorexia and bulimia nervosa (Abraham, 2016), adding to the evidence that exercise levels should be closely monitored in subjects with indicated eating disorders.
Participants who identified as fitness instructors had a slightly higher risk of higher exercise addiction scores than health club users who did not identify as fitness instructors; however, in the sub-populations this was only present in participants who showed no indicated eating disorders. One possible reason is because of the expectation of fitness instructors to exercise as part of their role, and the expectation of superior levels of fitness compared to regular health club users (Thompson et al., 2001); more research is needed to test this hypothesis. A recent study reported that fitness instructors are frequently worried about members in their centers who exhibit EA tendencies but are unsure on how to deal with these people (Colledge et al., 2020). These results suggest that fitness instructors should monitor their peers as well as their members.
Participants who reported exercising to improve their mood, to be more attractive, weight control, tone, and for enjoyment had higher exercise addiction scores; however, this was only seen in participants who had no indicated eating disorders. This is broadly consistent with previous studies that have found that exercising for mood, appearance, and enjoyment is positively correlated with exercise addiction (Serier et al., 2018). The finding that exercising for these reasons was only significant in participants without an indicated eating disorder was interesting as previous studies have found that people who exercise for mood and appearance reasons are more likely to demonstrate eating pathology (Macfarlane et al., 2016). This adds initial evidence that the links between exercise motivation and EA are different according to eating disorder status, and therefore indicates differing etiology for EA for the two sub-populations. This is important as if the two sub-populations have differing EA etiologies, then it is possible that therapeutic interventions would need to be different. Further research exploring potential mediating relationships between reasons for exercise, eating disorders, and exercise addiction would greatly add to the knowledge in this area.
Participants with indicated BDD were significantly more likely to yield higher exercise addiction scores, but only in participants without indicated eating disorders. Although this concurs with several studies that have shown that negative self-body image is positively correlated with exercise addiction (Klein et al., 2004; Ertl et al., 2018), this is the first study to our knowledge to show that this is not the case in populations with indicated eating disorders. This suggests that BDD is a primary condition in which exercise addiction is a symptom. This is important, as if BDD is a primary condition where EA is a symptom, then the treatment of BDD should yield lower levels of EA. It is therefore recommended that patients presenting with EA symptoms (who do not show evidence of eating disorders) should be screened for BDD before any treatments can be considered.
In the group with indicated eating disorders, participants from ethnic minorities (black, Hispanic, and Asian vs. being white) yielded higher exercise addiction scores. This is the first time such a finding has been reported, and this could be because of the long-recognized limited treatment barriers to eating disorders that subjects from ethnic minorities face (Cachelin et al., 2001; Becker et al., 2003; Coffino et al., 2019). Confirmatory and causal exploration is needed to confirm this relationship and explore interventions to address this.
Exercise Addiction Prevalence
The prevalence of exercise addiction was high in this sample, with 30.7% being classified as at risk of exercise addiction. Prevalence rates differed largely according to eating disorder status, with participants with indicated eating disorders yielding more than double the prevalence rates than those with no indicated eating disorders. These results are broadly in agreement with a recent meta-analysis that showed subjects with indicated eating disorders are over 3.5 times more likely to also have exercise addiction (Trott et al., 2020b). The overall exercise addiction prevalence rate is higher than in several reviews that have estimated prevalence between 3 and 14% (Di Lodovico et al., 2019; Marques et al., 2019). One potential reason could be because of the recruitment strategy and specific population group; this study used social media as a means of recruitment and was restricted to health club users, which is unique in this area of research. This is supported by our finding that using social media for social integration and emotional connection was a significant predictor for higher exercise addiction scores. Social media use has been shown to elicit feelings of negative body image (Perloff, 2014; Fardouly and Vartanian, 2016), which has been shown to be associated with exercise addiction. Social media is an appropriate platform to recruit from, however, primarily due to the number of people who routinely engage in social media. Recent data suggests that 2.2 billion people use social media on a daily basis (Facebook, 2019). The role of social media's influence in the etiology of exercise addiction warrants further exploration.
Limitations and Strengths
This study had several limitations. Firstly, due to the cross-sectional nature of the study design, the direction of correlation (and therefore causality) is impossible to determine. Further longitudinal analysis is required to determine the direction of the observed correlations. Secondly, it has been reported that the EAI can yield false-positive results in elite athletes (Szabo et al., 2015), and it is unknown whether the EAI over-estimates exercise addiction prevalence in other highly active populations who exercise as part of their job, such as fitness instructors. Further validation of this questionnaire in this sub-population is warranted. Thirdly, the variables accounted for a low percentage of the total variation. Moreover, the sample was restricted to health club users who were recruited via social media, making the generalization of the findings across populations difficult. Despite these limitations, the large sample size, novelty of measured correlates, and our findings that significant variables of EA vary according to eating disorder status mean that this study adds significant knowledge to the current EA literature.
Conclusion
The key findings from this study suggest a direct link between exercise motivations and EA, especially if the reason for exercising is to modify mood state. It is suggested that exercising to modify mood state, eating disorder status, and BDD status be included in the intolerable life-stress section of the Interactional Model of EA.
Furthermore, this study shows that the etiology of EA differs according to eating disorder status, with variables including social media use, exercise motivation, and ethnicity being uniquely correlated with EA only in populations with indicated eating disorders. Furthermore, BDD is also highly prevalent in subjects without indicated eating disorders and could be a primary condition in which exercise addiction is a symptom. It is recommended that clinicians and practitioners working with patients who present with symptoms of EA should be screened for eating disorders and BDD before treatments are considered, as both eating disorders and BDD have considerably higher co-morbid outcomes than EA, and therefore need to be treated as a primary condition. Furthermore, treatment programs already exist for these two primary conditions and therefore can be implemented easier. The development of screening tools that are able to stratify these populations would be beneficial to both researchers and practitioners.
Data Availability Statement
The datasets generated for this study are available on request to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by Anglia Ruskin University Sport and Exercise Sciences Departmental Ethics Panel (ESPGR-03). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
MT and LS: study design, data collection, data analysis, and write up. BS, JF, SJ, and LY: study design, data analysis, and write up. CG: study design and write up. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Adams, J. M., Miller, T. W., and Kraus, R. F. (2003). Exercise dependence: diagnostic and therapeutic issues for patients in psychotherapy. J. Contemp. Psychother. 33, 93–107. doi: 10.1023/A:1022883104269
Allegre, B., Therme, P., and Griffiths, M. (2007). Individual factors and the context of physical activity in exercise dependence: a prospective study of “ultra-marathoners. Int. J. Ment. Health Addict. 5, 233–243. doi: 10.1007/s11469-007-9081-9
American Psychiatric Association (2000). Diagnostic and Statistical Manual of Mental Disorders, 4th Edn. Washington, DC: American Psychiatric Association.
American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders (DSM-5®). Washington, DC: American Psychiatric Association. doi: 10.1176/appi.books.9780890425596
Ashdown-Franks, G., Sabiston, C. M., and Stubbs, B. (2019). The evidence for physical activity in the management of major mental illnesses: a concise overview to inform busy clinicians' practice and guide policy. Curr. Opin. Psychiatry 32, 375–380. doi: 10.1097/YCO.0000000000000526
Becker, A. E., Franko, D. L., Speck, A., and Herzog, D. B. (2003). Ethnicity and differential access to care for eating disorder symptoms. Int. J. Eat. Disord. 33, 205–212. doi: 10.1002/eat.10129
Brohede, S., Wingren, G., Wijma, B., and Wijma, K. (2013). Validation of the body dysmorphic disorder questionnaire in a community sample of Swedish women. Psychiatry Res. 210, 647–652. doi: 10.1016/j.psychres.2013.07.019
Brown, R. I. F. (1993). “Some contributions of the study of gambling to the study of other addictions,” in Gambling Behavior and Problem Gambling, eds W. Eadington and J. Cornelius (Nevada: Commercial Gaming, University of Nevada, 241–272.
Buhlmann, U., Teachman, B. A., Naumann, E., Fehlinger, T., and Rief, W. (2009). The meaning of beauty: implicit and explicit self-esteem and attractiveness beliefs in body dysmorphic disorder. J. Anxiety Disord. 23, 694–702. doi: 10.1016/j.janxdis.2009.02.008
Cachelin, F. M., Rebeck, R., Veisel, C., and Striegel-Moore, R. H. (2001). Barriers to treatment for eating disorders among ethnically diverse women. Int. J. Eat. Disord. 30, 269–278. doi: 10.1002/eat.1084
Cash, T. F., Novy, P. L., and Grant, J. R. (1994). Why do women exercise? Factor analysis and further validation of the reasons for exercise inventory. Percept. Mot. Skills 78, 539–44. doi: 10.2466/pms.1994.78.2.539
Coffino, J. A., Udo, T., and Grilo, C. M. (2019). Rates of help-seeking in US adults with lifetime DSM-5 eating disorders: prevalence across diagnoses and differences by sex and ethnicity/race. Mayo Clin. Proc. 94, 1415–1426. doi: 10.1016/j.mayocp.2019.02.030
Colledge, F., Cody, R., Pühse, U., and Gerber, M. (2020). Responses of fitness center employees to cases of suspected eating disorders or excessive exercise. J. Eat. Disord. 8:8. doi: 10.1186/s40337-020-0284-9
Conner, M., Johnson, C., and Grogan, S. (2004). Gender, sexuality, body image and eating behaviours. J. Health Psychol. 9, 505–15. doi: 10.1177/1359105304044034
Costa, S., Hausenblas, H. A., Oliva, P., Cuzzocrea, F., and Larcan, R. (2013). The role of age, gender, mood states and exercise frequency on exercise dependence. J. Behav. Addict. 2, 216–223. doi: 10.1556/JBA.2.2013.014
de Coverley Veale, D. M. (1987). Exercise dependence. Br. J. Addict. 82, 735–740. doi: 10.1111/j.1360-0443.1987.tb01539.x
Di Lodovico, L., Poulnais, S., and Gorwood, P. (2019). Which sports are more at risk of physical exercise addiction: a systematic review. Addict. Behav. 93, 257–262. doi: 10.1016/j.addbeh.2018.12.030
Doninger, G. L., Enders, C. K., and Burnett, K. F. (2005). Validity evidence for eating attitudes test scores in a sample of female college athletes. Meas. Phys. Educ. Exerc. Sci. 9, 35–49. doi: 10.1207/s15327841mpee0901_3
Egorov, A. Y., and Szabo, A. (2013). The exercise paradox: an interactional model for a clearer conceptualization of exercise addiction. J. Behav. Addict. 2, 199–208. doi: 10.1556/JBA.2.2013.4.2
Ertl, M. M., Longo, L. M., Groth, G. H., Berghuis, K. J., Prout, J., Hetz, M. C., et al. (2018). Running on empty: high self-esteem as a risk factor for exercise addiction. Addict. Res. Theory 26, 205–211. doi: 10.1080/16066359.2017.1347257
Fardouly, J., and Vartanian, L. R. (2016). Social media and body image concerns: current research and future directions. Curr. Opin. Psychol. 9, 1–5. doi: 10.1016/j.copsyc.2015.09.005
Fietz, M., Touyz, S., and Hay, P. (2014). A risk profile of compulsive exercise in adolescents with an eating disorder: a systematic review. Adv. Eat. Disord. 2, 241–263. doi: 10.1080/21662630.2014.894470
Freimuth, M., Moniz, S., and Kim, S. R. (2011). Clarifying exercise addiction: differential diagnosis, co-occurring disorders, and phases of addiction. Int. J. Environ. Res. Public. Health 8, 4069–4081. doi: 10.3390/ijerph8104069
Garber, C. E., Blissmer, B., Deschenes, M. R., Franklin, B. A., Lamonte, M. J., Lee, I.-M., et al. (2011). Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med. Sci. Sports Exerc. 43, 1334–59. doi: 10.1249/MSS.0b013e318213fefb
Garner, D. M., Olmsted, M. P., Bohr, Y., and Garfinkel, P. E. (1982). The eating attitudes test: psychometric features and clinical correlates. Psychol. Med. 12, 871–878. doi: 10.1017/S0033291700049163
Grandi, S., Clementi, C., Guidi, J., Benassi, M., and Tossani, E. (2011). Personality characteristics and psychological distress associated with primary exercise dependence: an exploratory study. Psychiatry Res. 189, 270–275. doi: 10.1016/j.psychres.2011.02.025
Griffiths, M. D., Urbán, R., Demetrovics, Z., Lichtenstein, M. B., de la Vega, R., Kun, B., et al. (2015). A cross-cultural re-evaluation of the exercise addiction inventory (EAI) in five countries. Sports Med. Open 1:5. doi: 10.1186/s40798-014-0005-5
Hamer, M., and Karageorghis, C. I. (2007). Psychobiological mechanisms of exercise dependence. Sports Med. 37, 477–484. doi: 10.2165/00007256-200737060-00002
Hausenblas, H. A., and Downs, D. S. (2002). How much is too much? The development and validation of the exercise dependence scale. Psychol. Health 17, 387–404. doi: 10.1080/0887044022000004894
Jenkins-Guarnieri, M. A., Wright, S. L., and Johnson, B. (2013). Development and validation of a social media use integration scale. Psychol. Pop. Media Cult. 2, 38–50. doi: 10.1037/a0030277
Jisc Online Surveys (2020). Available online at: https://www.onlinesurveys.ac.uk/ (accessed April 22, 2020).
Klein, D. A., Bennett, A. S., Schebendach, J., Foltin, R. W., Devlin, M. J., and Walsh, B. T. (2004). Exercise “addiction” in anorexia nervosa: model development and pilot data. CNS Spectr. 9, 531–537. doi: 10.1017/S1092852900009627
Kovacsik, R., Griffiths, M. D., Pontes, H. M., Soós, I., Vega, R., Ruíz-Barquín, R., et al. (2018). The role of passion in exercise addiction, exercise volume, and exercise intensity in long-term exercisers. Int. J. Ment. Health Addict. 17, 1389–1400. doi: 10.1007/s11469-018-9880-1
Leuenberger, A. (2006). Endorphins, exercise, and addictions: a review of exercise dependence. Prem. J. Undergrad. Publ. Neurosci. 3, 1–9.
Lichtenstein, M. B., and Jensen, T. T. (2016). Exercise addiction in crossfit: prevalence and psychometric properties of the exercise addiction inventory. Addict. Behav. Rep. 3, 33–37. doi: 10.1016/j.abrep.2016.02.002
Little, R. J. A. (1988). A test of missing completely at random for multivariate data with missing values. J. Am. Stat. Assoc. 83, 1198–1202. doi: 10.1080/01621459.1988.10478722
Macfarlane, L., Owens, G., and Cruz, B. D. P. (2016). Identifying the features of an exercise addiction: a delphi study. J. Behav. Addict. 5, 474–484. doi: 10.1556/2006.5.2016.060
Maree, T. (2017). The social media use integration scale: toward reliability and validity. Int. J. Hum. Comput. Interact. 33, 963–972. doi: 10.1080/10447318.2017.1301041
Marques, A., Peralta, M., Sarmento, H., Loureiro, V., Gouveia, É. R., and Gaspar de Matos, M. (2019). Prevalence of risk for exercise dependence: a systematic review. Sports Med. 49, 319–330. doi: 10.1007/s40279-018-1011-4
McNamara, J., and McCabe, M. P. (2012). Striving for success or addiction? Exercise dependence among elite Australian athletes. J. Sports Sci. 30, 755–766. doi: 10.1080/02640414.2012.667879
O'Brien, C. P. (2004). The mosaic of addiction. Am. J. Psychiatry 161, 1741–1742. doi: 10.1176/ajp.161.10.1741
Perloff, R. M. (2014). Social media effects on young women's body image concerns: theoretical perspectives and an agenda for research. Sex Roles 71, 363–377. doi: 10.1007/s11199-014-0384-6
Phillips, K. A. (2005). The Broken Mirror: Understanding and Treating Body Dysmorphic Disorder. Oxford: Oxford University Press.
Pope, Z., Gao, Y., Bolter, N., and Pritchard, M. (2015). Validity and reliability of eating disorder assessments used with athletes: a review. J. Sport Health Sci. 4, 211–221. doi: 10.1016/j.jshs.2014.05.001
Powell, K. E., King, A. C., Buchner, D. M., Campbell, W. W., DiPietro, L., Erickson, K. I., et al. (2019). The scientific foundation for the physical activity guidelines for americans, 2nd edition. J. Phys. Act. Health 16, 1–11. doi: 10.1123/jpah.2018-0618
Serier, K. N., Smith, J. E., Lash, D. N., Gianini, L. M., Harriger, J. A., Sarafin, R. E., et al. (2018). Obligatory exercise and coping in treatment-seeking women with poor body image. Eat. Weight Disord. 23, 331–338. doi: 10.1007/s40519-018-0504-3
Silberstein, L. R., Striegel-Moore, R. H., Timko, C., and Rodin, J. (1988). Behavioral and psychological implications of body dissatisfaction: do men and women differ? Sex Roles 19, 219–232. doi: 10.1007/BF00290156
Symons Downs, D., MacIntyre, R. I., and Heron, K. E. (2019). “Exercise addiction and dependence,” in APA Handbook of Sport and Exercise Psychology, Vol. 2. Exercise Psychology, eds M. H. Anshel, S. J. Petruzzello, and E. E. Labbe (Washington, DC: American Psychiatric Association), 589–604. doi: 10.1037/0000124-030
Szabo, A. (1995). The impact of exercise deprivation on well-being of habitual exercisers. Aust. J. Sci. Med. Sport 27, 68–75.
Szabo, A., Griffiths, M. D., de La Vega Marcos, R., Merv,ó, B., and Demetrovics, Z. (2015). Methodological and conceptual limitations in exercise addiction research. Yale J. Biol. Med. 88, 303–308.
Szabo, A., Griffiths, M. D., and Demetrovics, Z. (2019). “Psychology and exercise,” in Nutrition and Enhanced Sports Performance, eds D. Bagchi, S. Nair, and C. Sen (London: Elsevier), 63–72. doi: 10.1016/B978-0-12-813922-6.00005-9
Terry, A., Szabo, A., and Griffiths, M. (2004). The exercise addiction inventory: a new brief screening tool. Addict. Res. Theory 12, 489–499. doi: 10.1080/16066350310001637363
Thompson, J. K., and Blanton, P. (1987). Energy conservation and exercise dependence: a sympathetic arousal hypothesis. Med. Sci. Sports Exerc. 19, 91–99. doi: 10.1249/00005768-198704000-00005
Thompson, S. H., Case, A. J., and Sargent, R. G. (2001). Factors influencing performance-related injuries among group exercise instructors. Women Sport Phys. Act. J. 10, 125–142. doi: 10.1123/wspaj.10.1.125
Trott, M., Jackson, S. E., Firth, J., Fisher, A., Johnstone, J., Mistry, A., et al. (2020a). Exercise addiction prevalence and correlates in the absence of eating disorder symptomology. A systematic review and meta-analysis. J. Addict. Med. doi: 10.1097/ADM.0000000000000664. [Epub ahead of print].
Keywords: exercise addiction, exercise dependence, eating disorder, social media, reasons for exercising, exercise, pathological exercise
Citation: Trott M, Yang L, Jackson SE, Firth J, Gillvray C, Stubbs B and Smith L (2020) Prevalence and Correlates of Exercise Addiction in the Presence vs. Absence of Indicated Eating Disorders. Front. Sports Act. Living 2:84. doi: 10.3389/fspor.2020.00084
Received: 14 February 2020; Accepted: 02 June 2020;
Published: 10 July 2020.
Edited by:
Sergio Machado, Salgado de Oliveira University, BrazilReviewed by:
Jennifer Cumming, University of Birmingham, United KingdomDonatella Di Corrado, Kore University of Enna, Italy
Copyright © 2020 Trott, Yang, Jackson, Firth, Gillvray, Stubbs and Smith. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mike Trott, bWlrZS50cm90dEBwZ3IuYW5nbGlhLmFjLnVr
†ORCID: Mike Trott orcid.org/0000-0001-5978-3407
 Mike Trott
Mike Trott Lin Yang
Lin Yang Sarah E. Jackson4
Sarah E. Jackson4 Joseph Firth
Joseph Firth Lee Smith
Lee Smith