- 1Department of Social and Preventive Medicine, Medical University of Vienna, Vienna, Austria
- 2Department of Science and Technology Studies, University of Vienna, Vienna, Austria
- 3Department of Environmental Health, Medical University of Vienna, Vienna, Austria
Telehealth is a valuable tool for reminding transgender-persons to undergo HIV testing, hormone injections, and voice training. Despite increased awareness of the unique health needs of transgender-individuals in recent years, effectively addressing their concerns remains challenging. The COVID-19 pandemic has negatively affected socioeconomic status, mental health, and access to gender-affirming treatment. To better understand how individuals and their specific health issues are addressed in telehealth solutions, we conducted a scoping review using PubMed and Scopus, spanning from 2000 to 2021. We screened eligible articles following the PRISMA checklist, extracted the data, and performed a thematic analysis of 100 reports. For control purposes, we double-checked the ratings during the screening and coding. Our results show that telehealth is primarily used for healthcare access, sexual and reproductive health, and mental health. Since 2020, the overall number of publications has greatly increased, with only nine reports explicitly referring to COVID-19-related challenges. The latter relate exclusively to clinical purposes such as healthcare access. We found that transgender-women were researched more often than transgender-men, particularly in the field of sexual and reproductive health research. Some studies included groups other than transgender-persons, such as parents or clinicians, who might be relevant for advancing telehealth use. The review’s findings highlight the need for more research that considers the diversity of transgender-groups and the adapted use of diverse technological tools beyond pandemics and public health crises.
1 Introduction
Telehealth is a healthcare delivery method using telecommunication technology such as video conferencing to provide healthcare services and information remotely (Haluza et al., 2020), allowing individuals to connect with healthcare professionals from the comfort of their own homes or on the go when applying mobile applications. It is currently used in a wide range of healthcare services, including consultations, diagnosis, treatment, monitoring, and education (Haluza and Jungwirth, 2018). Telehealth is particularly useful for patients in remote or rural areas, those with mobility or transportation issues, and those experiencing difficulty accessing traditional healthcare services—such as transgender-persons being confronted with stigma, discrimination, and violence while seeking healthcare (Smith et al., 2018; Reisner et al., 2016). It has the potential to improve access to healthcare, increase patient engagement and satisfaction, and reduce costs (Radix et al., 2022; Restar et al., 2021; Russell et al., 2022; Shipherd et al., 2016). The COVID-19 pandemic profoundly impacted healthcare systems worldwide, with vulnerable groups, such as transgender-persons, being particularly affected (Restar et al., 2021). During a crisis, when many people stay at home and have limited in-person interactions, telehealth has become increasingly popular (Doraiswamy et al., 2020).
Despite recent efforts to address transgender-persons’ unique healthcare needs, the provision of adequate care remains challenging. In complex interdisciplinary settings, in which transgender-persons and healthcare workers interact, telehealth has been used to support healthcare needs, such as reminding users to conduct HIV tests or voice training (Jarrett et al., 2021; Wang et al., 2020; McGregor et al., 2023). Familiarity with the needs of transgender-individuals has grown in recent years, particularly in developed Western nations, and progress has been made. However, addressing specific health issues is challenging, given that people living under different political and social conditions depend on their home country and socioeconomic status (Asaad et al., 2020). Thus, the terminology (e.g., hijra, kathoey, travesties, and waria) used to describe transgender-populations worldwide across different socio-cultural settings is constantly evolving (Reisner et al., 2016).
Moreover, transgender-individuals face significant health disparities and stressors, which can lead to negative health outcomes if not addressed adequately (MacCarthy et al., 2015). This is translated in higher rates of mental health issues, such as depression and anxiety in the transgender-community than in the general population (Pinna et al., 2022). Transgender-persons may also face barriers to healthcare, such as a lack of knowledge among healthcare providers about their specific health needs or a lack of insurance coverage for gender-affirming treatments (Reisner et al., 2016), which encompass a range of social, psychological, behavioral, and medical interventions “designed to support and affirm an individual’s gender identity” (World Health Organization (WHO), 2024) when it conflicts with the gender they were assigned at birth.
Therefore, exploring this population’s health issues in telehealth research is crucial as little is known about the services that are used to provide health care and information remotely, also beyond the clinic and other medical institution (Roy et al., 2022). Putting telehealth for transgender-persons at the center of this review is of immense importance, as several studies have shown that the COVID-19 pandemic has negatively affected transgender-individuals´ lives worldwide, including their socioeconomic conditions, access to gender affirmation services, and mental health outcomes (Restar et al., 2021; Jarrett et al., 2021; Wang et al., 2020). Puckett et al. (2019) highlighted the importance of community support for individuals and the negative impact of its absence on mental health during the COVID-19 pandemic. Delays in accessing gender-affirming healthcare, including hormonal treatment and surgical care, detrimentally affected individuals’ health status additionally (van der Miesen et al., 2020). Hence, the focus of this research was the period from 2000 to the COVID-19 pandemic.
According to Radix et al., technological solutions for healthcare purposes can be categorized as telehealth or mobile health (Radix et al., 2022). As previously demonstrated, technology meant to facilitate healthcare, such as practitioner-patient communication, might also produce disparities, such as disparities between younger (i.e., “digital natives”) and older generations (i.e., “digital migrants”) (Haluza and Hofer, 2020; Naszay et al., 2018), as younger individuals are highly engaged online and well connected within online communities (Russell et al., 2022; McGregor et al., 2023; Mintz et al., 2022) compared to older populations.
Telehealth has emerged as an increasingly important tool for healthcare delivery, particularly in the wake of the COVID-19 pandemic (Monaghesh and Hajizadeh, 2020). However, the extent telehealth solutions address people’s specific health concerns remains unclear, as recent reviews have focused on aspects of accessibility and the quality of telehealth-enabled healthcare services (McGregor et al., 2023; Mintz et al., 2022). Our current review aimed to address this research knowledge gap and provide a more conclusive understanding of the health issues addressed in research on telehealth use. In this context, our research explored what kind of technological solutions are in use and investigated, what health issues they address, and how transgender-persons are addressed in scientific literature across multiple disciplines.
2 Methods
The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) framework supported a clear presentation of data sources, screening stages, and inclusion criteria, aligning with the scoping nature of our study by providing a structured and comprehensive overview of the available literature. Therefore, we employed the PRISMA framework to structure the data selection and reporting processes to ensure transparency and reproducibility in study selection (Tricco et al., 2018).
2.1 Eligibility criteria
For our literature review, we included articles that investigated telehealth focusing on or intended for transgender-persons, published since 2000 in peer-reviewed journals in German and English, and presented original data. Aside gender-affirming treatments we also included all the other specific health concerns of transgender-persons. Review articles as well as articles in other languages and those without a full text were not included in our literature search.
2.2 Literature search
We searched PubMed and Scopus databases in cooperation with the Library of the Medical University of Vienna. In the first query, we also included the search term trans, resulting in the exclusion of more than 30,000 records from further processing. The search terms used were transsex*, transgender, eHealth, mHealth, telehealth, mobile applications, and apps. Since research on this topic began predominantly in the early 21st century, the search encompassed more than two decades of publication data (2000–2021). Consequently, our analysis included information gathered from January 1, 2000, to December 31, 2021.
2.3 Selection process
Before initiating the literature search, we thoroughly examined online academic sources to determine whether a similar review had already been undertaken. Although we conducted a scoping review, we used the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist for reporting purposes (Page et al., 2021). Since transgender-persons were not clearly specified or the focus was limited to sexual practice in several studies, we investigated telehealth solutions focused on transgender-persons rather than other groups of people, even if they may intersect.
The term “Intersectionality” was coined by the racial theorist Kimberlé Crenshaw (1989) and describes how identities and movements are discussed as separated and constructed if they were standing alone. Intersectionality, however, describes how “systems of inequality intersect to ´create´ unique dynamics and effects “(TGEU (Trans Europe and Central Asia), 2024) which shape individuals’ experiences, opportunities, and forms of discrimination or privilege (Hammarström and Hensing, 2018). For this review, we considered the following systems of inequality: gender, race, ethnicity, sexual orientation, gender identity, disability, and class. Nevertheless, we did not consider studies that recruited along sexual practice, as numerous studies have recruited men who have sex with men but reported transgender-persons as a separate group, thus frequently reduced being transgender to sexual practices.
2.4 Data collection and analysis
Data were extracted using Excel (version 16.6). Our data grid contained the following variables: consecutive number; first author; article type; year of publication; rating within the screening (three to five stars records); COVID-19 pandemic virus-related (yes/no); study type and methods used; country and region; addressing transgender-persons in the study (e.g., transgender, trans-women); abbreviations used (e.g., TGNB, meaning trans-gender and non-binary and describes people whose gender does not match that assigned to them at birth); number and age of transgender-persons included in the study; intersectionality (e.g., young, black, or recently incarcerated); diagnosis, treatment, and intervention; control and comparison; and study outcome.
Recognizing the profound influence of diverse writing styles on vulnerable populations, we conscientiously chose to employ a hyphen in “trans-” during the analysis of the specific groups under consideration in our studies. This deliberate choice reflected our commitment to sensitivity and precision in addressing language nuances, particularly when discussing and representing vulnerable communities (Stryker et al., 2008). This analytical concept allowed us to analyze how transgender-persons intersect with other groups and categories (e.g., women, men, sex, gender, or young/old, ethnicity) to reflect on diversity aspects and aspects of intersectionality without being reductive towards transgender-individuals.
We used thematic analysis for establishing themes to describe the different health issues we identified in our review. Coding followed a five-step approach, assigning single codes to each category (Braun and Clarke, 2006; Braun and Clarke, 2014). We also conducted control steps in terms of intercoder reliability.
3 Results
3.1 Study selection
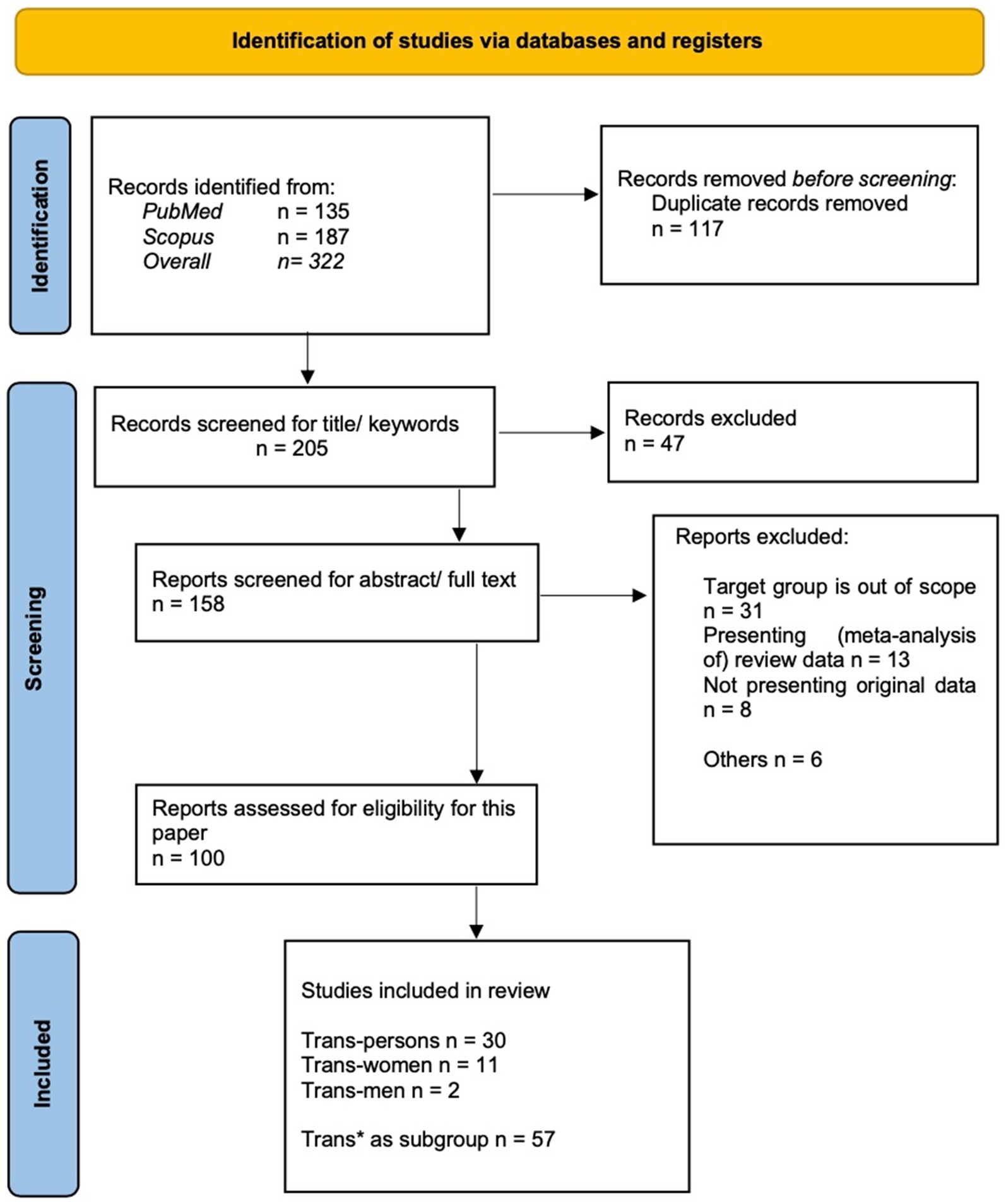
In total, 100 records were included in the final analysis. Overall, we identified 322 articles: 187 from Scopus and 135 from PubMed (Figure 1). The search records were exported to EndNote (Version X9.3.3) for screening purposes. After removing 117 duplicates, 205 records were screened by title and keywords. Each record was initially screened on the 5-star scale in Endnote, and 3- to 5-star records were considered for further analyses. For this purpose, we focused on the key term “telehealth” and excluded all the technological tools, that did not focus on health issues, such as geographical networking apps or technological tools whose focus was not the health of transgender-persons. To be precise about the inclusion thresholds, we checked 2- and 3-stars ratings twice. Furthermore, 47 records were excluded from the analysis because they were outside the scope of this study, such as not being peer-reviewed articles, being published in a Spanish-language journal, or not adequately covering our literature search. Ultimately, 158 records were downloaded for retrieval.
After screening the abstracts and full-text of these records, 57 reports were excluded from further analysis, as 31 records addressed groups that were outside the study scope (e.g., sex workers or people living with HIV not specified as transgender-persons), 21 records did not present original data, and 6 were excluded for other reasons (e.g., presenting an English abstract but the article text in Turkish, or outside the scope of the study). The screening and exclusion of records was double-checked by the authors.
3.2 Study characteristics
We found that the first article on telehealth for transgender-persons was published in 2009. Since then, the number of articles published a year ranged between 1 and 13. In 2020, with the outbreak of the COVID-19 pandemic crisis, this number increased: more than a half of the reports were published since then (n = 61) even though just a few of them (n = 9) directly refer their findings to the pandemic situation (Table 1). Geographically, the majority of the studies was conducted in the US and Canada (n = 68). Only four of these publications referred to the COVID-19 virus pandemic explicitly. Only one of the ten studies conducted in Asia did not refer to sexual health, such as testing for sexually transmitted infections, minimizing risks of sexual behavior, or health promotion in general (Table 1).
More than a half of the publications (n = 57) presented transgender-persons as a subsample in a larger sample, sometimes even including only a few persons in samples larger than 1,000 (Table 1). In these samples, transgender-persons were rather addressed as “trans-women” or “transgender-women” (n = 33) than as “trans-men,” who were only addressed in one report (n = 1). Eleven articles examined “trans-(gender-) men and -women” or “trans-gender” persons/individuals equally as cis persons (male or female) and/or lesbian/gay/bi persons/individuals or as those living with HIV. A further eleven reports recruited participants along minority groups or acronyms, such as “sexual and gender minorities” or “LGBT*” (i.e., lesbians, gays, bisexuals, and transgender). Hence, transgender-persons were part of the study samples but not the focus of these studies (Table 1).
3.3 Telehealth for transgender-persons, transgender-women, and transgender-men
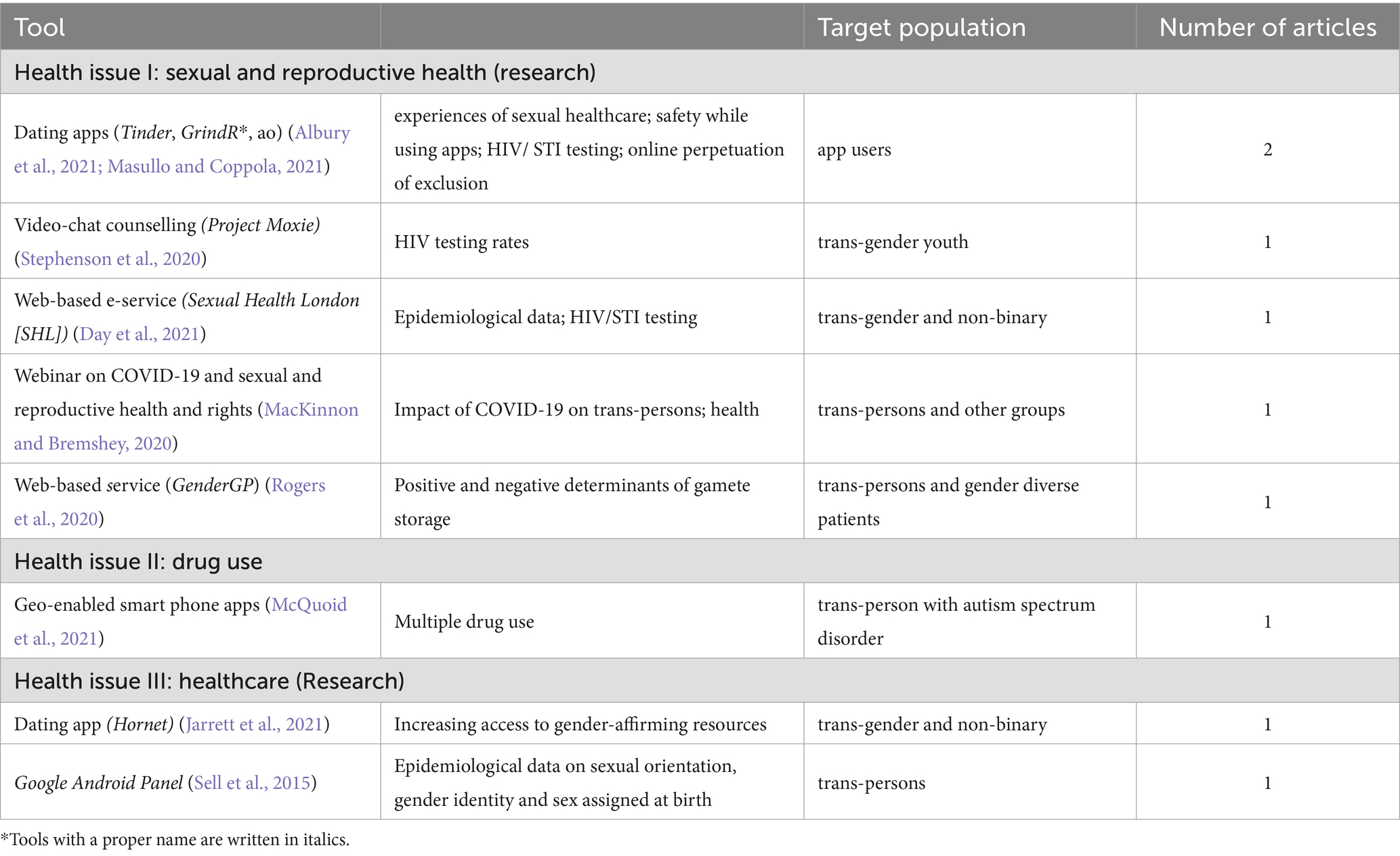
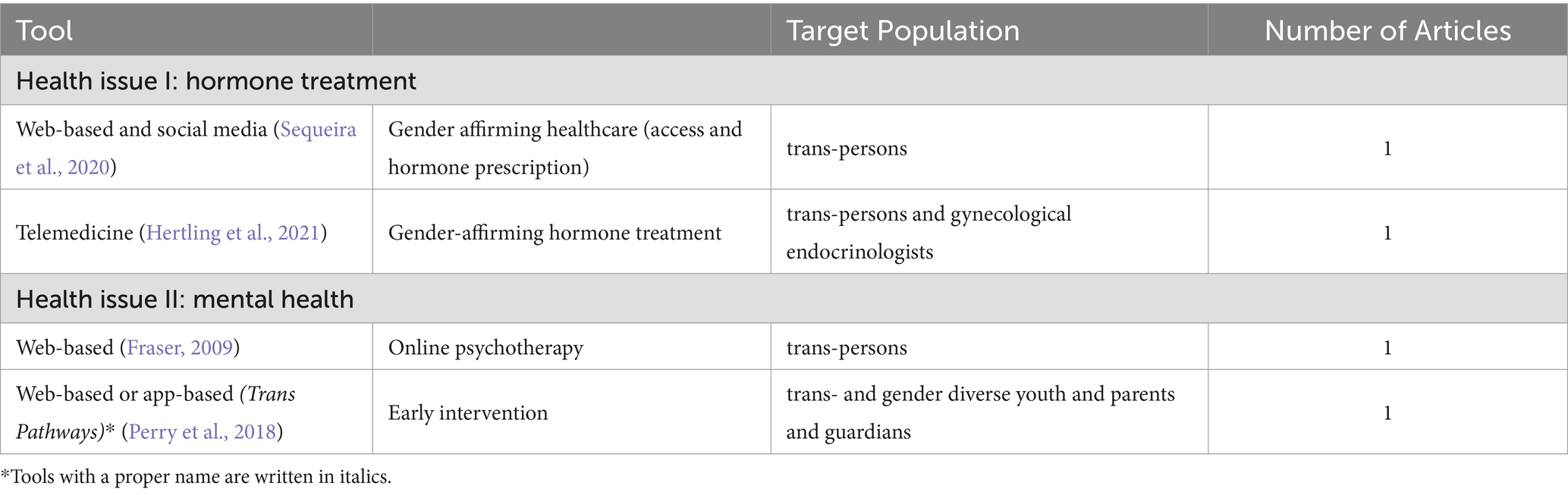
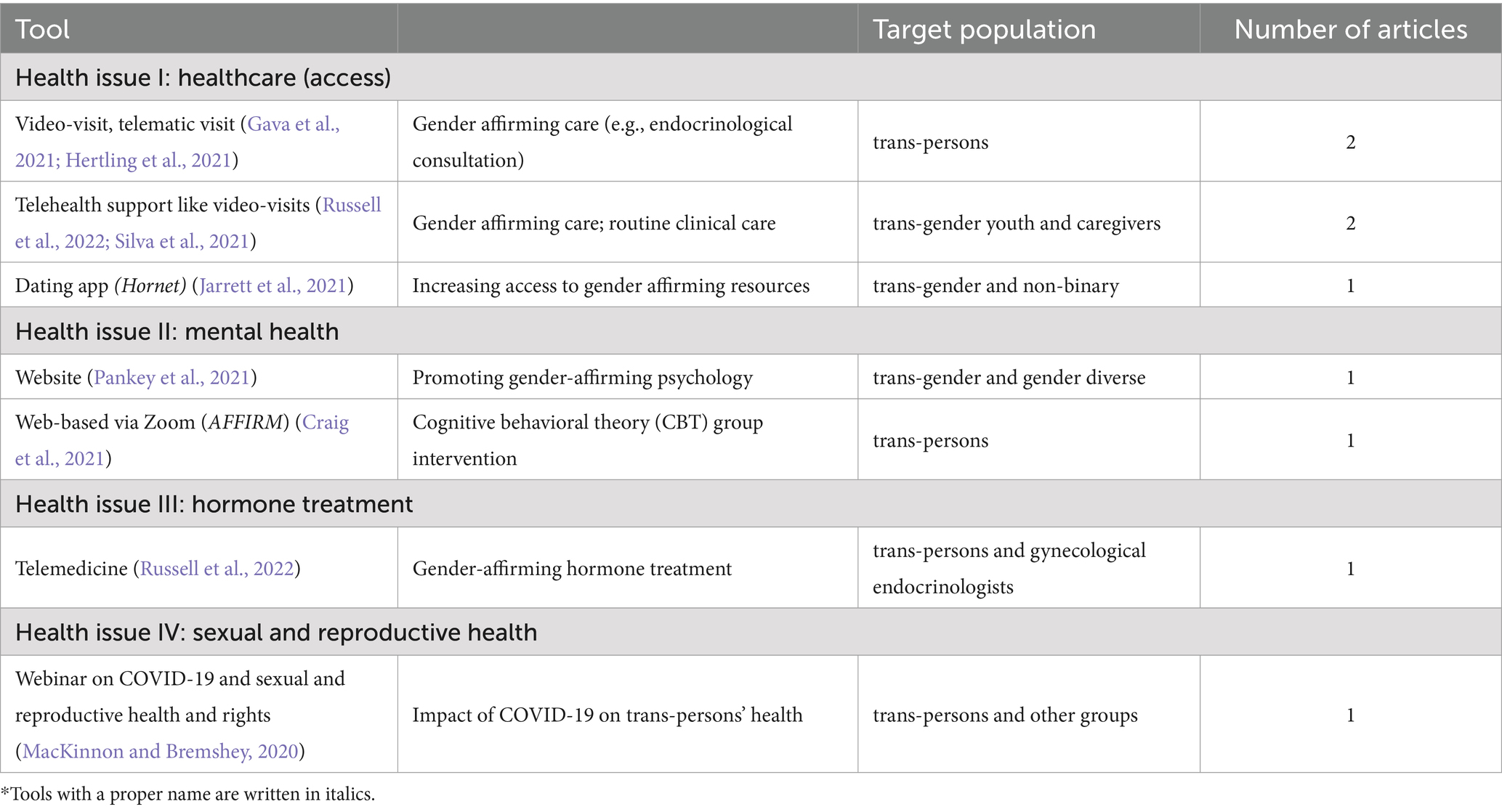
Telehealth can be used for both clinical and nonclinical purposes (World Health Organisation, 2010). Clinical use refers to patient management and diagnostics, whereas nonclinical use refers to education, mentoring, supervision, research, and health promotion. Hence, we sorted our study outcomes into clinical and nonclinical telehealth and observational studies (Tables 2–7, respectively). Table 2 shows the clinical telehealth tools for healthcare (e.g., access), sexual health, mental health, and health communication as well as the specific target population described in each of the included articles.
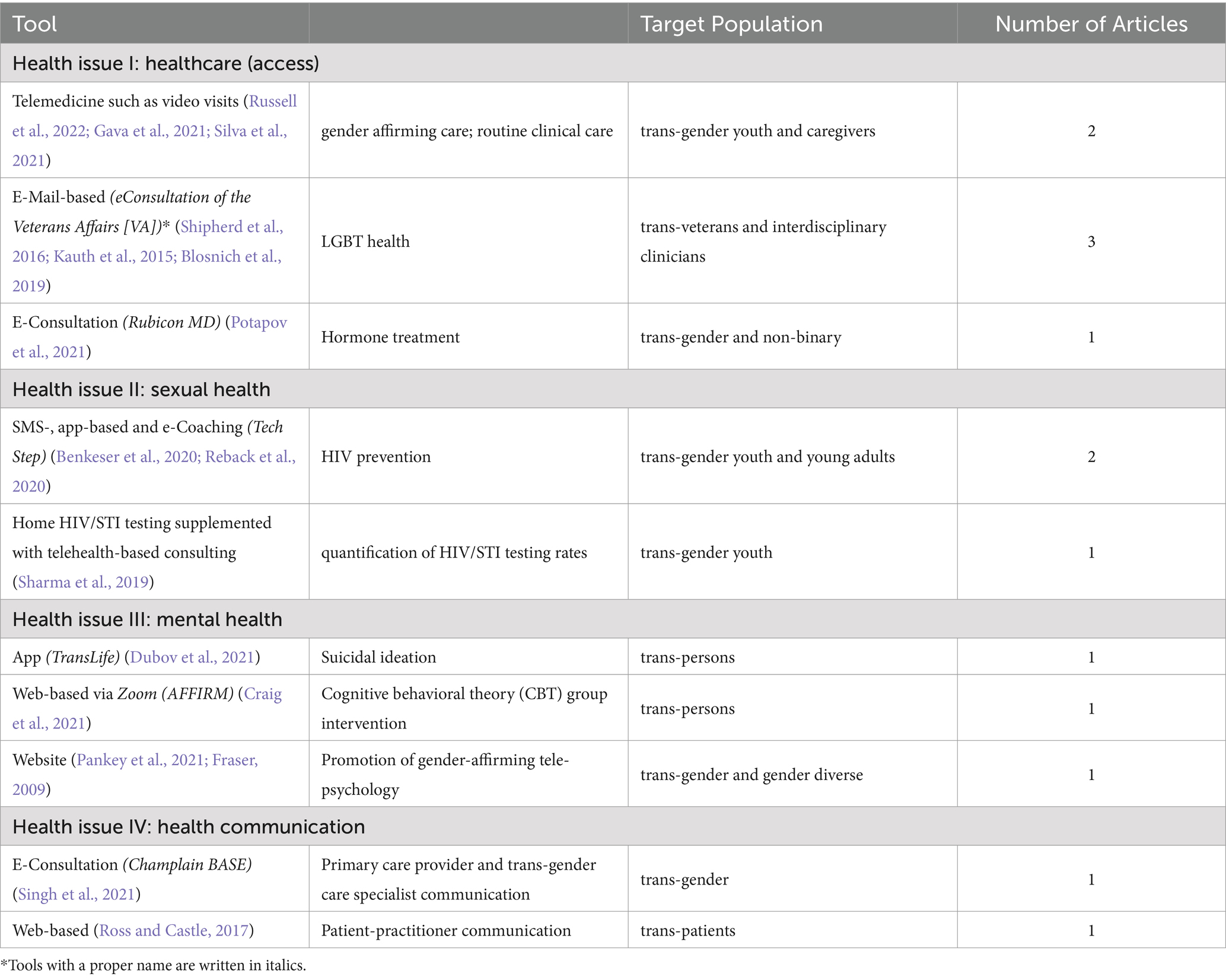
Table 2. Clinical telehealth tools and health issues, namely healthcare (access), sexual health, mental health, and health communication.

Table 5. Research on non-clinical telehealth tools: research purpose, methodologies, and sample sizes, settings.
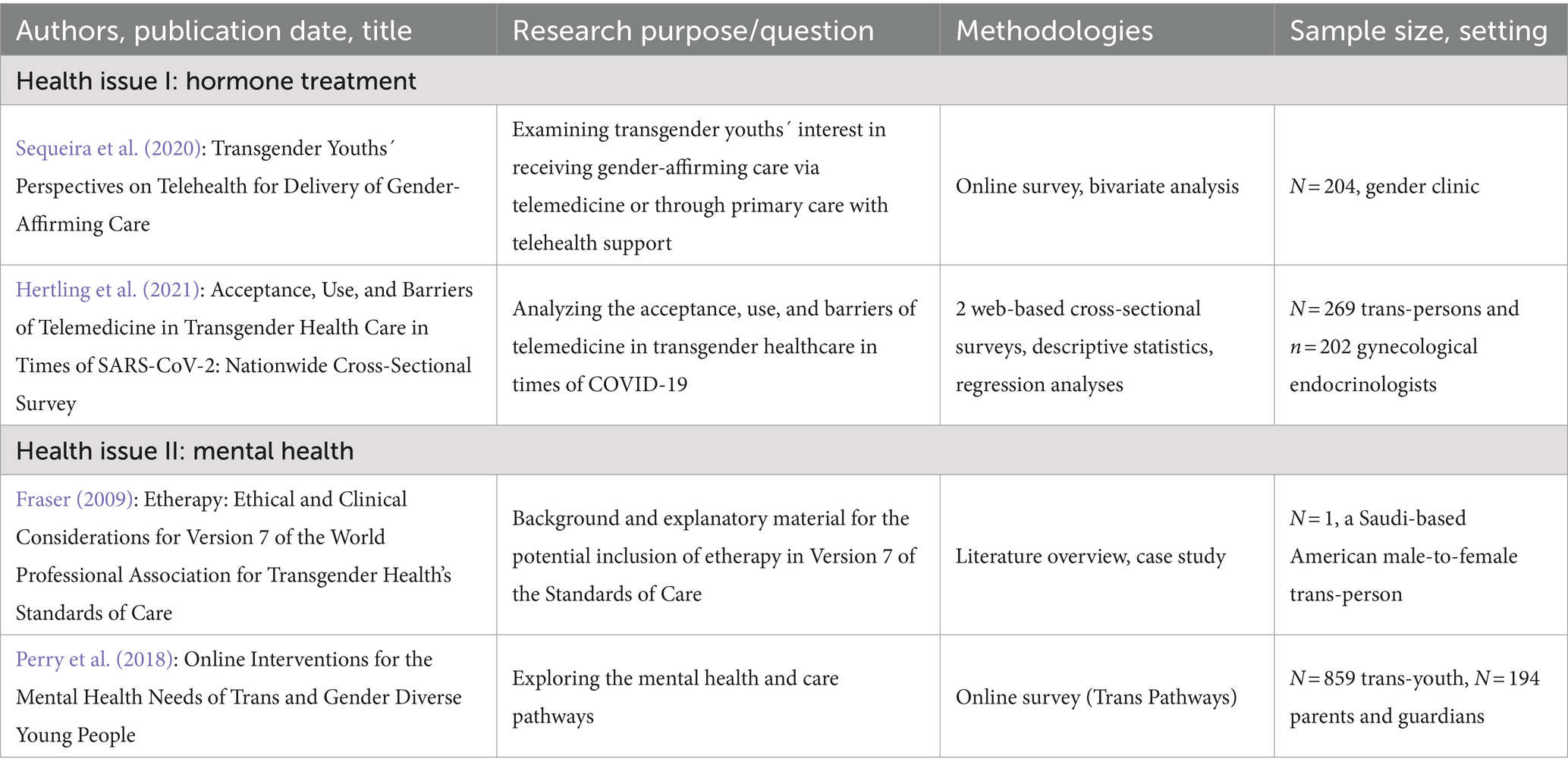
Table 7. Observational research on telehealth: research purpose, methodologies, and sample sizes, settings.
Table 3 presents the clinical telehealth tools used for healthcare (access), sexual health, mental health, and health communication, along with each study’s research purpose, methodology, sample size, and study setting.
As shown in Table 2, most publications (n = 16) referred to the clinical use of telehealth, such as the tool AFFIRM (affirmative cognitive behavioral therapy group intervention), while nine focused on nonclinical use (Table 4), such as investigating experiences in sexual healthcare or creating epidemiological data from very large existing data samples (e.g., the Google Android Panel). Furthermore, four were observational studies measuring the acceptance of telehealth tools. The most frequently discussed topics were sexual and reproductive health issues (n = 9) and healthcare access and research (n = 8), whereas mental health was discussed in only five. The less-discussed topics were health communication (n = 2) and drug use (n = 1).
Table 5 shows details of the included research articles on nonclinical telehealth tools for sexual and reproductive health (e.g., research), drug use, and healthcare (research), along with each study’s research purpose, methodology, sample size, and study setting.
Regarding age groups, we found that in seven articles, transgender-persons were recruited in adolescence, ranging from 14 to 18 years. In four publications, other groups were included, such as parents and caregivers, gynecological endocrinologists, and interdisciplinary clinicians, but were each analyzed and reported as a separate group. In two articles (Albury et al., 2021; Masullo and Coppola, 2021) transgender-persons were recruited via the telehealth intervention itself, thus, through addressing transgender-persons among the group of transgender-dating app users. Using an intersectional approach (Hammarström and Hensing, 2018), two studies focused on transgender-veterans (Shipherd et al., 2016) or a transgender-person with autism spectrum disorder (McQuoid et al., 2021). Table 6 summarizes observational studies on telehealth for hormone treatment and mental health, along with the respective groups addressed in this study.
Table 7 shows details of the observational research articles on telehealth tools for hormone treatment and mental health along with each study’s research purpose, methodology, and sample size, and study setting.
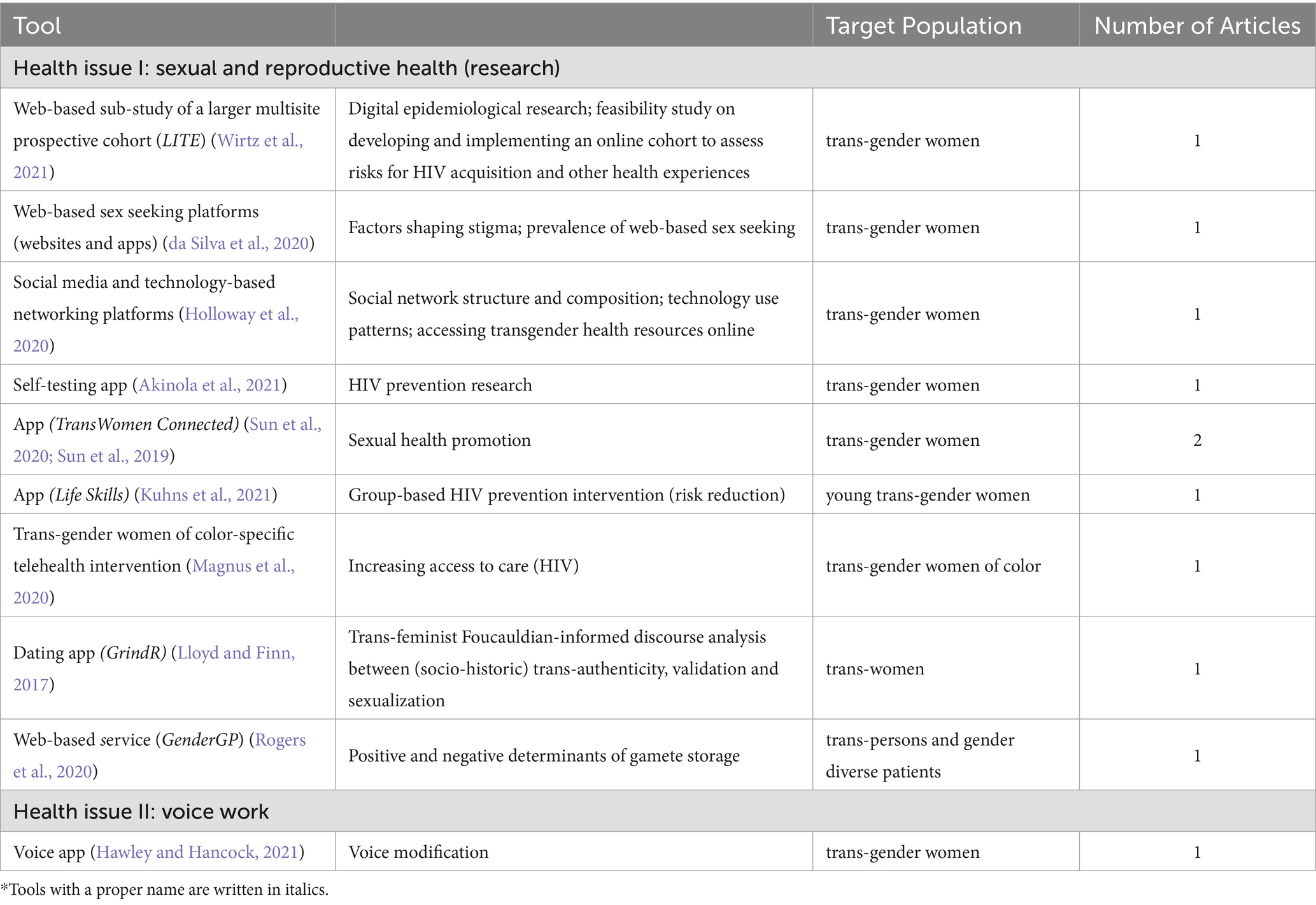
We also clustered the reported telehealth solutions stratified by group (i.e., women and men). Table 8 shows telehealth tools focusing on transgender-women that encompassed sexual and reproductive health and voice work.
Table 9 shows details of the studies focusing on transgender-women, along with each study’s research purpose, methodology, sample size, and setting.
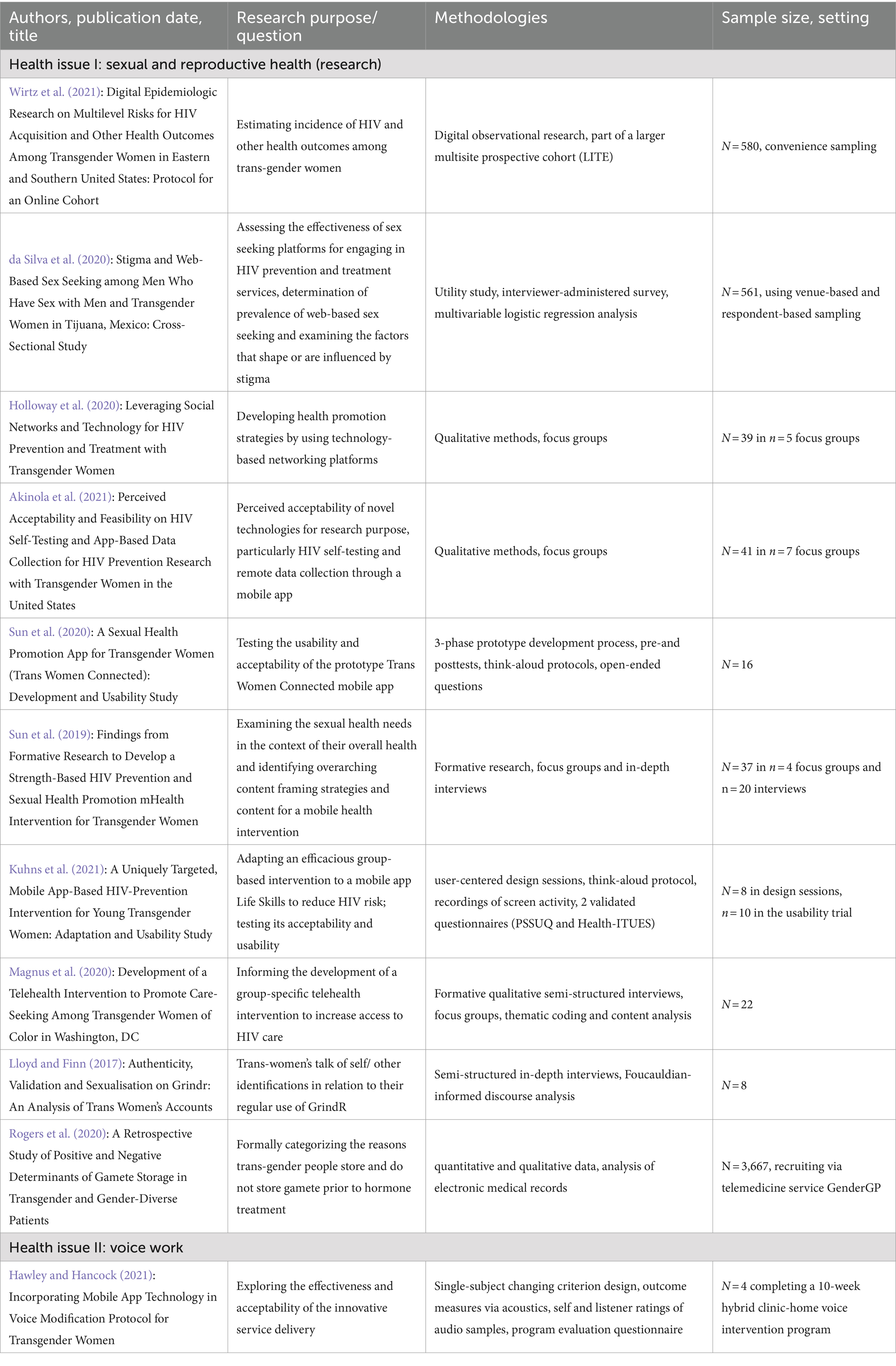
Table 9. Studies focused on transgender-women: research purpose, methodologies, and sample sizes, settings.
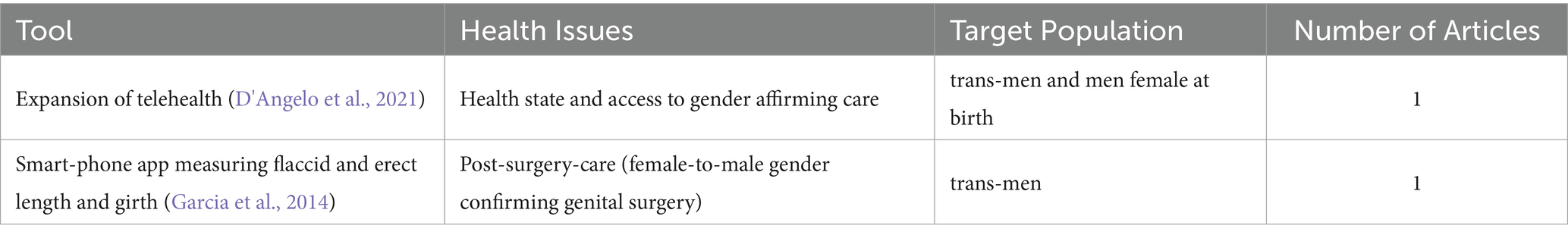
When examining telehealth solutions addressed to transgender-individuals, we found that more articles focused on transgender-women and that transgender-women were frequently included in study samples exclusively comprised of transgender-persons. Eleven studies discussed transgender-women (Kuhns et al., 2021; Lloyd and Finn, 2017), whereas only two studies discussed transgender-men (Table 10) (D'Angelo et al., 2021; Garcia et al., 2014). This discrepancy is particularly noticeable in studies on sexual and reproductive health. Ten tools addressed transgender-women and one transgender-men. Within the two groups, we also found unique research topics, such as post-surgery care for transgender-men and voice modification for transgender-women. Table 11 shows details of the reviewed studies focusing on transgender-men and each study’s research purpose, methodology, sample size, and setting.
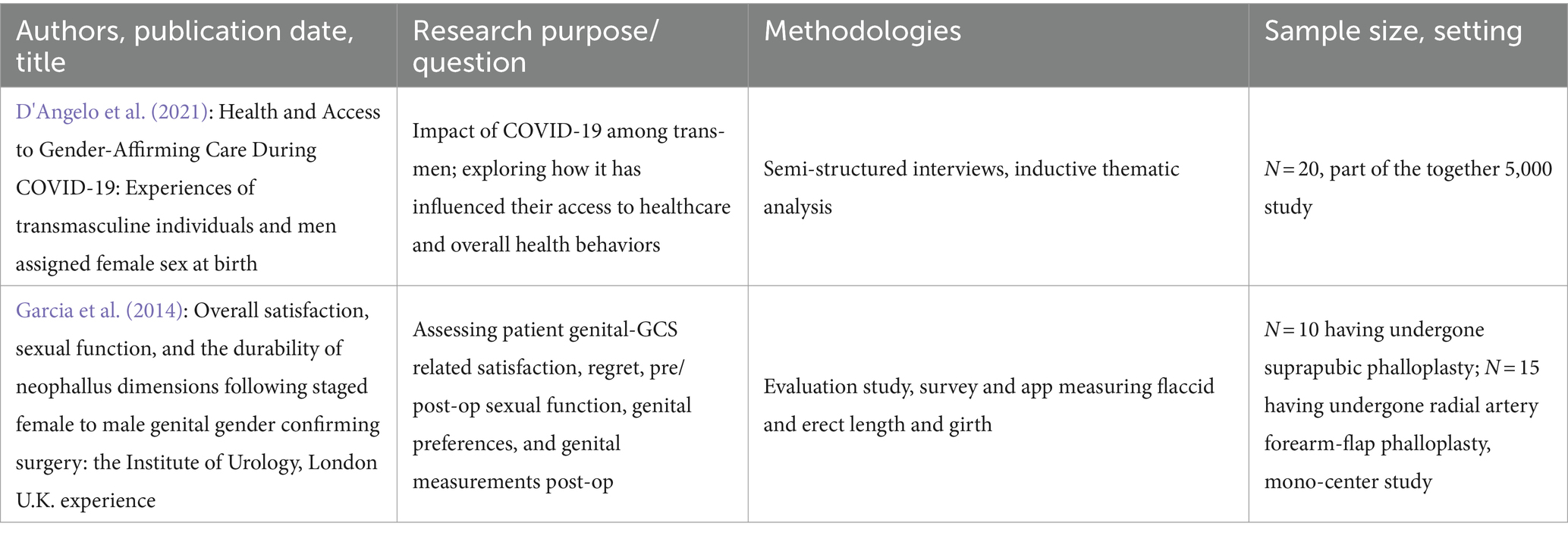
Table 11. Telehealth studies addressed at transgender-men: research purpose, methodologies, and sample sizes, settings.
3.4 Telehealth for transgender-persons during the COVID-19 pandemic
Even prior to the COVID-19 public health crisis, researchers emphasized the importance of utilizing 21st-century technological innovations for groups with existing access (Asaad et al., 2020). As previously published (Gahbauer and Haluza, 2022), the COVID-19 public health crisis resulted in the uptake of telehealth interventions for transgender-persons. More than half of the articles were published since 2020, although not all referred to the COVID-19 pandemic. Within our sample, we found 17 articles explicitly referring to the COVID-19 public health crisis, of which nine that were analyzed in this chapter as they addressed transgender-persons, transgender-men, or transgender-women.
As Table 12 shows, the pandemic rather supported the use of telehealth for maintaining health and healthcare access (Russell et al., 2022), especially in the younger groups than in older groups. Further health issues addressed in the reports at hand were mental, endocrinological, and sexual health. The tool AFFIRM translated an effective behavioral group therapy into an online environment. The authors of the respective article also examined the telehealth learning effects resulting from the COVID-19 pandemic, such as the learning effects of online adaptations of clinical skills (Craig et al., 2021).
Table 13 summarizes the telehealth tools that addressed transgender-persons and explicitly referred to the COVID-19 pandemic, along with each study’s research purpose, methodology, sample size, and setting.
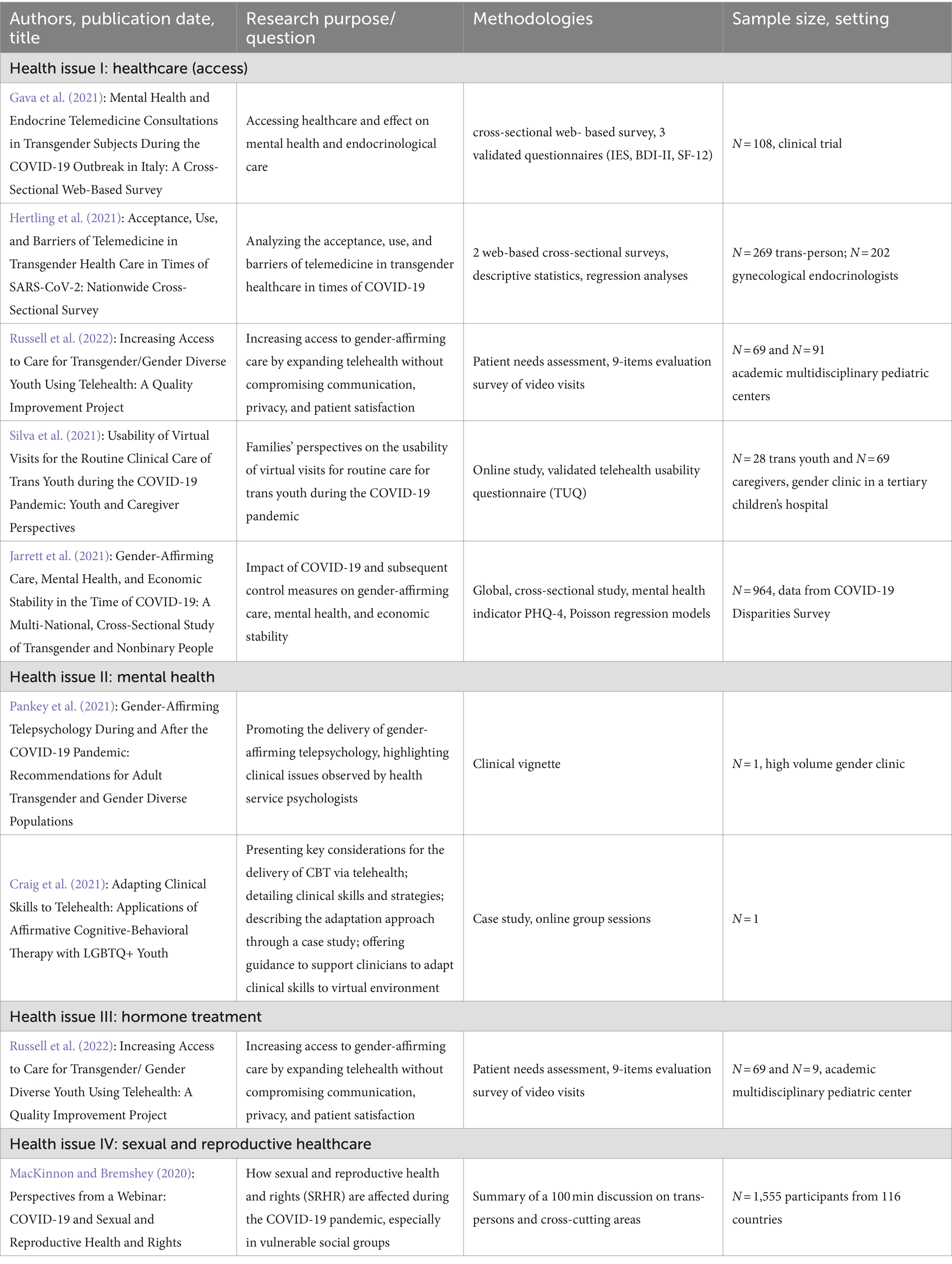
Table 13. Telehealth tools explicitly referring to COVID-19 and their research purpose, methodologies, sample sizes, and settings.
4 Discussion
On a global scale, the demand for comprehensive and inclusive healthcare is rapidly increasing. This growing recognition highlights the importance of adopting a thoughtful approach that addresses various dimensions of transgender-persons´ lives and their specific health requirements (Pinna et al., 2022; Puckett et al., 2019; Kirby, 2016). Hence, we reviewed the pertinent literature to shed light on what kind of technological solutions are in use and investigated, what health issues they address, and how transgender-persons are addressed within tools and applications.
We found that the most often discussed health issue was healthcare (e.g., access), particularly during the COVID-19 public health crisis. Further important themes were sexual and reproductive health issues and mental health issues. The first is strictly tied to with sexually transmitted infectious diseases (STIs) and related to their prevention through risk management. When addressing mental health issues, we found several tools that were exclusively produced to support issues experienced by transgender-persons, such as Trans-Pathways and AFFIRM.
The review further showed that, especially for sexual health concerns, the clinic is extended through the use of technological tools that aren’t initially designed for health purposes. Dating apps, for instance, support the discussion of risky behavior and, have potential to collect epidemiological data on transgender-persons, amongst others. As other studies have shown, non-clinical tools such as social media, have great potential to support public health purposes, in particular health promotion efforts (Wernhart et al., 2019). On the other hand, it is difficult to select scientifically informed offers in non-clinical tools (de Vere and Linos, 2022).
The heterogeneity of groups and practices in the existing research limits the endeavor to provide accurate and appropriate guidance for transgender-specific initiatives. This also ties into the fact that some treatments are more relevant for only one particular group of transgender-persons: a masculinization of voice, for instance, is much easier to realize than a feminization, which could require surgical support (Gahbauer, 2019). Nevertheless, the aim of addressing a broadly defined population group while simultaneously reflecting on intersectionality might not adequately address group vulnerabilities. The concept of intersectionality is highly relevant to the current field of research on transgender-persons. By recognizing and addressing the interconnected nature of individuals’ identities and experiences, researchers can foster a more comprehensive understanding of their diverse health needs and develop inclusive approaches to meet those needs.
Notably, our literature review highlighted the emphasis on transgender-women within the realm of telehealth research. This was especially obvious in sexual health research (MacCarthy et al., 2015), in which sexual practice was seen as common ground. For further research, we would first suggest to address the data gap in transgender-men, and to consider their higher proportion of the sexual orientation ´gay´ and ´queer´ also in studies on telehealth (Reisner et al., 2023). And second, we assume that this fact is consistent with studies showing that women are objectified (Mol and Law, 2004; Gahbauer, 2015) and sexualized in medical practice and beyond (Lloyd and Finn, 2017). Hence, further investigation is necessary to determine whether transgender-women and transgender-men are treated differently in telehealth, not because one treatment is more relevant for one of the two groups but because of their association with the traditional binary categories of men/women and male/female. Similarly, a study by Rudin et al. demonstrated that even in completely different settings, transgender-women face greater discrimination than transgender-men (Rudin et al., 2023).
Since practitioners and other groups within and outside the healthcare system may not always feel comfortable discussing transgender-identity-related health issues, telehealth could be valuable for transgender-persons when not directly focusing on transgender-persons (Asaad et al., 2020; Craig et al., 2021). Within our data, we also found interventions aimed at practitioners, such as e-consultation programs connecting with a specialist in transgender-health, or involving parents of transgender-adolescents in an intervention program for mental health. The latter includes persons outside the healthcare system but might be crucial for the success of a medical intervention (Russell et al., 2022). Our review revealed a lack of established telehealth programs that targeted different populations working with transgender-persons. Yet, many of the included studies did not explicitly mention the COVID-19 public health crisis. Instead, it appeared to be a case of the “normative power of the factual,” such as adapting clinical skills to an online environment. We expect a steep increase in the implementation of established telehealth programs as a result of the COVID-19 pandemic in clinical contexts.
Despite the COVID-19 pandemic providing valuable insights for all stakeholders in the healthcare system, these insights have yet to translate into legal and policy progress (Coleman et al., 2022). Viewing telehealth as a risk, gender-affirming health services might become rather a question of economic power rather than of subjective body experience (Jarrett et al., 2021; McGregor et al., 2023; van der Miesen et al., 2020). Hence, for improving telehealth offers for transgender-persons it might be necessary to foster cooperation between industries and healthcare systems in order to provide state-of-the-art health technology and scientifically informed health services to all transgender-persons.
Due to the wide range of health issues, tools, and in particular methods presented in our data, conducting a quantitative meta-analysis was not possible. Therefore, we provided detailed information on individual reports. The diversity of the reports was reflected in the various settings where transgender-groups were recruited, including clinical settings, community centers, and through the use of apps or at local venues, such as a gay resort, for instance. Additionally, some reports presented secondary analyses of big data. This diversity suggests the numerous technological possibilities for addressing health concerns, particularly for nonclinical and public health purposes. Hence, for future research we also suggest to consider a more in-depth quantitative exploration of how telehealth mitigated or failed to address health care gaps, particularly in clinical areas like hormone therapy delays and mental health support or in time frames such as pandemics.
Belonging to a gender minority group is likely to activate different stressors that are also relevant for health conditions and healthcare needs of different populations, and must be considered also for the use of telehealth tools (Frost et al., 2015). Thus, there is a crucial need for more focused and comprehensive research that encompasses diverse transgender-populations and encompasses various practices, enabling a more informed approach to developing suitable offerings for this community.
4.1 Limitations
It is important to acknowledge the limitations of this study. The findings of the current review might not be generalized to all transgender-persons or all healthcare contexts, as our search strategy in terms of language and search terms focused on specific populations or settings and did not represent the full spectra of cultural understandings of transgender-persons, such as the Samoan fa’afafine (Poasa, 1992). This limitation in our search strategy might have led to an overrepresentation of geographical regions, such as US and Canada. Their particular healthcare contexts might differ from underrepresented healthcare contexts in terms of access to the internet, of access to healthcare in general as well as to gender-affirming healthcare. However, we included all age groups to provide a comprehensive overview that considers the various experiences and challenges across different age demographics within the transgender-community. Our database selection might have excluded further records in literature search. For instance, we did not consider the database PsycInfo, as we wanted to focus on the relation between transgender-persons and the technological aspect of telehealth research. Our search strategy was also limited to a specific timeframe (2000–2021) and may have missed more recent studies that were not available at the time of the search. Our study only analyzed peer-reviewed articles, which may have excluded relevant research in other types of publications, such as conference proceedings, books, or reports.
Notably, this review did not address ways how telehealth advances transgender-persons’ healthcare needs and inequities. Herein, we rather summarized the current evidence on transgender-individuals’ health issues discussed in research on telehealth use, which we estimated to be a relevant aspect for future research, including systematic literature reviews.
5 Conclusion
The telehealth tools we analyzed during our scoping review primarily discussed health issues that were also discussed to be impacted by the COVID-19 pandemic. Some tools also focused on the lack of knowledge among healthcare providers, who may need education and training on the diversity of non-binary groups and appropriate care for gender affirming treatments. Although telehealth solutions for transgender-persons may attempt to be inclusive of diverse groups of transgender-persons and make efforts to address the specific health issues of transgender-men and transgender-women, a risk of objectifying transgender-persons exists, in particular transgender-women. Future research should focus on intersectionality in transgender-persons’ experiences without reducing to sexual practices for instance. In this regard, investigating the interactions between technology and transgender-persons, as well as including groups outside of the healthcare system, might help to advance the development of telehealth tools for transgender-persons and explore possibilities of an adaptive use of existing tools.
Author contributions
SG: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Validation, Visualization, Writing – original draft, Writing – review & editing. DH: Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We want to thank Eva Chwala from the University Library for her support in identifying relevant literature and Editage for English language editing.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Akinola, M., Wirtz, A. L., Chaudhry, A., Cooney, E., and Reisner, S. L. (2021). Perceived acceptability and feasibility of HIV self-testing and app-based data collection for HIV prevention research with transgender women in the United States. AIDS Care 33, 1079–1087. doi: 10.1080/09540121.2021.1874269
Albury, K., Dietzel, C., Pym, T., Vivienne, S., and Cook, T. (2021). Not your unicorn: trans dating app users’ negotiations of personal safety and sexual health. Health Soc Rev. 30, 72–86. doi: 10.1080/14461242.2020.1851610
Asaad, M., Rajesh, A., Vyas, K., and Morrison, S. D. (2020). Telemedicine in transgender care: a twenty-first-century beckoning. Plast. Reconstr. Surg. 146, 108e–109e. doi: 10.1097/PRS.0000000000006935
Benkeser, D., Horvath, K., Reback, C. J., Rusow, J., and Hudgens, M. (2020). Design and analysis considerations for a sequentially randomized HIV prevention trial. Stat. Biosci. 12, 446–467. doi: 10.1007/s12561-020-09274-3
Blosnich, J. R., Rodriguez, K. L., Hruska, K. L., Kavalieratos, D., Gordon, A. J., Matza, A., et al. (2019). Utilization of the veterans affairs' transgender e-consultation program by health care providers: mixed-methods study. JMIR Med. Inform. 7:e11695. doi: 10.2196/11695
Braun, V., and Clarke, V. (2006). Using thematic analysis in psychology. Qual. Res. Psychol. 3, 77–101. doi: 10.1191/1478088706qp063oa
Braun, V., and Clarke, V. (2014). What can “thematic analysis” offer health and wellbeing researchers? Int. J. Qual. Stud. Health Well Being 9:26152. doi: 10.3402/qhw.v9.26152
Coleman, E., Radix, A. E., Bouman, W. P., Brown, G. R., de Vries, A. L. C., Deutsch, M. B., et al. (2022). Standards of Care for the Health of transgender and gender diverse people, version 8. Int. J. Transgend. Health 23, S1–S259. doi: 10.1080/26895269.2022.2100644
Craig, S. L., Iacono, G., Pascoe, R., and Austin, A. (2021). Adapting clinical skills to telehealth: applications of affirmative cognitive-behavioral therapy with LGBTQ+ youth. Clin. Soc. Work. J. 49, 471–483. doi: 10.1007/s10615-021-00796-x
Craig, S. L., Leung, V. W. Y., Pascoe, R., Pang, N., Iacono, G., Austin, A., et al. (2021). Affirm online: Utilising an affirmative cognitive–behavioural digital intervention to improve mental health, access, and engagement among LGBTQA+ youth and young adults. Int. J. Environ. Res. Public Health 18, 1–18. doi: 10.3390/ijerph18041541
Crenshaw, K. (1989). Demarginalizing the intersection of race and sex: A black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. Univ. Chic. Leg. Forum 1, 139–167.
da Silva, C. E., Smith, L. R., Patterson, T. L., Semple, S. J., Harvey-Vera, A., Nunes, S., et al. (2020). Stigma and web-based sex seeking among men who have sex with men and transgender women in Tijuana, Mexico: cross-sectional study. JMIR Publ. Heal Surveil. 6:e14803. doi: 10.2196/14803
D'Angelo, A. B., Argenio, K., Westmoreland, D. A., Appenroth, M. N., and Grov, C. (2021). Health and access to gender-affirming care during COVID-19: experiences of transmasculine individuals and men assigned female sex at birth. Am. J. Mens Health 15:15579883211062681. doi: 10.1177/15579883211062681
Day, S., Smith, J., Perera, S., Jones, S., and Kinsella, R. (2021). Beyond the binary: sexual health outcomes of transgender and non-binary service users of an online sexual health service. Int. J. STD AIDS 32, 896–902. doi: 10.1177/0956462420982830
de Vere, H. I., and Linos, E. (2022). Social Media for Public Health: framework for social media–based public health campaigns. J. Med. Internet Res. 24:e42179. doi: 10.2196/42179
Doraiswamy, S., Abraham, A., Mamtani, R., and Cheema, S. (2020). Use of telehealth during the COVID-19 pandemic: scoping review. J. Med. Internet Res. 22:e24087. doi: 10.2196/24087
Dubov, A., Fraenkel, L., Goldstein, Z., Arroyo, H., McKellar, D., and Shoptaw, S. (2021). Development of a smartphone app to predict and improve rates of suicidal ideation among transgender persons (TransLife): a qualitative study. J. Med. Internet Res. 23:e24023. doi: 10.2196/24023
Fraser, L. (2009). Etherapy: ethical and clinical considerations for version 7 of the world professional association for transgender health's standards of care. Int. J. Transgend. 11, 247–263. doi: 10.1080/15532730903439492
Frost, D. M., Lehavot, K., and Meyer, I. H. (2015). Minority stress and physical health among sexual minority individuals. J. Behav. Med. 38, 1–8. doi: 10.1007/s10865-013-9523-8
Gahbauer, S. (2015). “Body images in medical teaching: A gender sensitive use” in Gender summit Europe 7 - mastering gender in research performance, contexts, and outcomes (Berlin: Gender Summit Europe).
Gahbauer, S. Voice work as a public health tool for trans* persons. Sustainable Health - 22nd Conference of the Austrian Society for Public Health (ÖGPH); (2019), Austria: Austrian Society for Public Health (ÖGPH).
Gahbauer, S., and Haluza, D. (2022). eHealth solutions for trans* persons: a systematic literature review of research from 2000 till 2021. Eur. J. Pub. Health 32:ckac131.508. doi: 10.1093/eurpub/ckac131.508
Garcia, M. M., Christopher, N. A., De Luca, F., Spilotros, M., and Ralph, D. J. (2014). Overall satisfaction, sexual function, and the durability of neophallus dimensions following staged female to male genital gender confirming surgery: the Institute of Urology, London U.K. experience. Transl. Androl. Urol. 3, 156–162. doi: 10.3978/j.issn.2223-4683.2014.04.10
Gava, G., Fisher, A. D., Alvisi, S., Mancini, I., Franceschelli, A., Seracchioli, R., et al. (2021). Mental health and endocrine telemedicine consultations in transgender subjects during the COVID-19 outbreak in Italy: a cross-sectional web-based survey. J. Sex. Med. 18, 900–907. doi: 10.1016/j.jsxm.2021.03.009
Haluza, D., and Hofer, F. (2020). Exploring perceptions on medical app use in clinical communication among Austrian physicians: results of a validation study. Health Informatics J. 26, 1659–1671. doi: 10.1177/1460458219888420
Haluza, D., and Jungwirth, D. (2018). ICT and the future of healthcare: aspects of pervasive health monitoring. Inform. Health Soc. Care 43, 1–11. doi: 10.1080/17538157.2016.1255215
Haluza, D., Saustingl, M., and Halavina, K. (2020). Perceptions of practitioners on telehealth and app use for smoking cessation and COPD care—an exploratory study. Medicina 56:698. doi: 10.3390/medicina56120698
Hammarström, A., and Hensing, G. (2018). How gender theories are used in contemporary public health research. Int. J. Equity Health 17:34. doi: 10.1186/s12939-017-0712-x
Hawley, J. L., and Hancock, A. B. (2021). Incorporating Mobile app Technology in Voice Modification Protocol for transgender women. J. Voice 7:21. doi: 10.21037/mhealth-20-43
Hertling, S., Hertling, D., Martin, D., and Graul, I. (2021). Acceptance, use, and barriers of telemedicine in transgender health Care in Times of SARS-CoV-2: Nationwide cross-sectional survey. JMIR Public Health Surveill. 7:e30278. doi: 10.2196/30278
Holloway, I. W., Jordan, S. P., Dunlap, S. L., Ritterbusch, A., and Reback, C. J. (2020). Leveraging social networks and technology for HIV prevention and treatment with transgender women. AIDS Educ. Prev. 32, 83–101. doi: 10.1521/aeap.2020.32.2.83
Jarrett, B. A., Peitzmeier, S. M., Restar, A., Adamson, T., Howell, S., Baral, S., et al. (2021). Gender-affirming care, mental health, and economic stability in the time of COVID-19: a multi-national, cross-sectional study of transgender and nonbinary people. PLoS One 16:e0254215. doi: 10.1371/journal.pone.0254215
Kauth, M. R., Shipherd, J. C., Lindsay, J. A., Kirsh, S., Knapp, H., and Matza, L. (2015). Teleconsultation and training of VHA providers on transgender care: implementation of a multisite hub system. Telemed. J. E Health 21, 1012–1018. doi: 10.1089/tmj.2015.0010
Kirby, T. (2016). Sari Reisner - making transgender health visible. Lancet 388:332. doi: 10.1016/S0140-6736(16)30839-X
Kuhns, L. M., Hereth, J., Garofalo, R., Hidalgo, M., Johnson, A. K., Schnall, R., et al. (2021). A uniquely targeted, Mobile app-based HIV prevention intervention for young transgender women: adaptation and usability study. J. Med. Internet Res. 23:e21839. doi: 10.2196/21839
Lloyd, C. E. M., and Finn, M. D. (2017). Authenticity, validation and sexualisation on Grindr: an analysis of trans women’s accounts. Psychol. Sex. 8, 158–169. doi: 10.1080/19419899.2017.1316769
MacCarthy, S., Reisner, S. L., Nunn, A., Perez-Brumer, A., and Operario, D. (2015). The time is now: attention increases to transgender health in the United States but scientific knowledge gaps remain. LGBT Health 2, 287–291. doi: 10.1089/lgbt.2014.0073
MacKinnon, J., and Bremshey, A. (2020). Perspectives from a webinar: COVID-19 and sexual and reproductive health and rights. Sex Reprod. Health Matters 28:1763578. doi: 10.1080/26410397.2020.1763578
Magnus, M., Edwards, E., Dright, A., Gilliam, L., Brown, A., Levy, M., et al. (2020). Development of a telehealth intervention to promote care-seeking among transgender women of color in Washington, DC. Public Health Nurs. 37, 262–271. doi: 10.1111/phn.12709
Masullo, G., and Coppola, M. (2021). Scripts and sexual Markets of Transgender People on online dating apps: a Netnographic study. Ital Sociol Rev. 11, 319–341. doi: 10.13136/isr.v11i4S.437
McGregor, K., Williams, C. R., Botta, A., Mandel, F., and Gentile, J. (2023). Providing essential gender-affirming telehealth services to transgender youth during COVID-19: a service review. J. Telemed. Telecare 29, 147–152. doi: 10.1177/1357633X221095785
McQuoid, J., Thrul, J., Lopez-Paguyo, K., and Ling, P. M. (2021). Exploring multiple drug use by integrating mobile health and qualitative mapping methods - an individual case study. Int. J. Drug Policy 97:103325. doi: 10.1016/j.drugpo.2021.103325
Mintz, L. J., Gillani, B., and Moore, S. E. (2022). Telehealth in trans and gender diverse communities: the impact of COVID-19. Curr. Obstet. Gynecol. Rep. 11, 75–80. doi: 10.1007/s13669-022-00334-7
Mol, A., and Law, J. (2004). Embodied action, enacted bodies: the example of Hypoglycaemia. Body Soc. 10, 43–62. doi: 10.1177/1357034x04042932
Monaghesh, E., and Hajizadeh, A. (2020). The role of telehealth during COVID-19 outbreak: a systematic review based on current evidence. BMC Public Health 20, 1193–1199. doi: 10.1186/s12889-020-09301-4
Naszay, M., Stockinger, A., Jungwirth, D., and Haluza, D. (2018). Digital age and the public eHealth perspective: prevailing health app use among Austrian internet users. Inform. Health Soc. Care 43, 390–400. doi: 10.1080/17538157.2017.1399131
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., et al. (2021). The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. doi: 10.1136/bmj.n71
Pankey, T. L., Heredia, D. Jr., Vencill, J. A., and Gonzalez, C. A. (2021). Gender-affirming telepsychology during and after the COVID-19 pandemic: recommendations for adult transgender and gender diverse populations. J. Health Serv. Psychol. 47, 181–189. doi: 10.1007/s42843-021-00048-z
Perry, Y., Strauss, P., and Lin, A. (2018). Online interventions for the mental health needs of trans and gender diverse young people. Lancet Psychiatry 5:e6. doi: 10.1016/S2215-0366(18)30017-8
Pinna, F., Paribello, P., Somaini, G., Corona, A., Ventriglio, A., Corrias, C., et al. (2022). Mental health in transgender individuals: a systematic review. Int. Rev. Psychiatry 34, 292–359. doi: 10.1080/09540261.2022.2093629
Poasa, K. (1992). The Samoan fa'afafine: one case study and discussion of transsexualism. J. Psychol. Hum. Sex. 5, 39–51. doi: 10.1300/J056v05n03_04
Potapov, A., Olayiwola, J. N., Radix, A. E., Meacher, P., Sajanlal, S., and Gordon, A. (2021). Electronic consultations as an educational tool to improve the care of transgender patients in primary care. J. Health Care Poor Underserved 32, 680–687. doi: 10.1353/hpu.2021.0097
Puckett, J. A., Matsuno, E., Dyar, C., Mustanski, B., and Newcomb, M. E. (2019). Mental health and resilience in transgender individuals: what type of support makes a difference? J. Fam. Psychol. 33, 954–964. doi: 10.1037/fam0000561
Radix, A. E., Bond, K., Carneiro, P. B., and Restar, A. (2022). Transgender individuals and digital health. Curr. HIV/AIDS Rep. 19, 592–599. doi: 10.1007/s11904-022-00629-7
Reback, C. J., Rusow, J. A., Cain, D., Benkeser, D., Arayasirikul, S., Hightow-Weidman, L., et al. (2020). Technology-based stepped care to stem transgender adolescent risk transmission: protocol for a randomized controlled trial (TechStep). JMIR Res. Protoc. 9:e18326. doi: 10.2196/18326
Reisner, S. L., Choi, S. K., Herman, J. L., Bockting, W., Krueger, E. A., and Meyer, I. H. (2023). Sexual orientation in transgender adults in the United States. BMC Public Health 23:1799. doi: 10.1186/s12889-023-16654-z
Reisner, S. L., Poteat, T., Keatley, J., Cabral, M., Mothopeng, T., Dunham, E., et al. (2016). Global health burden and needs of transgender populations: a review. Lancet 388, 412–436. doi: 10.1016/S0140-6736(16)00684-X
Restar, A. J., Jin, H., Jarrett, B., Adamson, T., Baral, S. D., Howell, S., et al. (2021). Characterising the impact of COVID-19 environment on mental health, gender affirming services and socioeconomic loss in a global sample of transgender and non-binary people: a structural equation modelling. BMJ Glob. Health 6:e004424. doi: 10.1136/bmjgh-2020-004424
Rogers, C., Webberley, M., Mateescu, R., El Rakhawy, Y., Daly-Gourdialsing, A., and Webberley, H. (2020). A retrospective study of positive and negative determinants of gamete storage in transgender and gender-diverse patients. Int. J. Transgend. Health 22, 167–178. doi: 10.1080/26895269.2020.1848693
Ross, K. A., and Castle, B. G. (2017). A culture-centered approach to improving healthy trans-patient-practitioner communication: recommendations for practitioners communicating withTrans individuals. Health Commun. 32, 730–740. doi: 10.1080/10410236.2016.1172286
Roy, J., Levy, D. R., and Senathirajah, Y. (2022). Defining telehealth for research, implementation, and equity. J. Med. Internet Res. 24:e35037. doi: 10.2196/35037
Rudin, J., Billing, T., Farro, A., and Yang, Y. (2023). When are trans women treated worse than trans men? Equal. Divers. Inclus. 42, 723–736. doi: 10.1108/EDI-08-2021-0195
Russell, M. R., Rogers, R. L., Rosenthal, S. M., and Lee, J. Y. (2022). Increasing access to Care for Transgender/gender diverse youth using telehealth: a quality improvement project. Telemed. J. E Health 28, 847–857. doi: 10.1089/tmj.2021.0268
Sell, R., Goldberg, S., and Conron, K. (2015). The utility of an online convenience panel for reaching rare and dispersed populations. PLoS One 10:e0144011. doi: 10.1371/journal.pone.0144011
Sequeira, G. M., Kidd, K. M., Coulter, R. W. S., Miller, E., Fortenberry, D., Garofalo, R., et al. (2020). Transgender Youths' perspectives on telehealth for delivery of gender-affirming care. J. Adolesc. Health 68, 1207–1210. doi: 10.1016/j.jadohealth.2020.08.028
Sharma, A., Kahle, E., Todd, K., Peitzmeier, S., and Stephenson, R. (2019). Variations in testing for HIV and other sexually transmitted infections across gender identity among transgender youth. Transgend. Health 4, 46–57. doi: 10.1089/trgh.2018.0047
Shipherd, J. C., Kauth, M. R., and Matza, A. (2016). Nationwide interdisciplinary E-consultation on transgender Care in the Veterans Health Administration. Telemed. J. E Health 22, 1008–1012. doi: 10.1089/tmj.2016.0013
Silva, C., Fung, A., Irvine, M. A., Ziabakhsh, S., and Hursh, B. E. (2021). Usability of virtual visits for the routine clinical Care of Trans Youth during the COVID-19 pandemic: youth and caregiver perspectives. Int. J. Environ. Res. Public Health 18:11321. doi: 10.3390/ijerph182111321
Singh, J., Lou, A., Green, M., Keely, E., Greenaway, M., and Liddy, C. (2021). Evaluation of an electronic consultation service for transgender care. BMC Fam. Pract. 22:55. doi: 10.1186/s12875-021-01401-3
Smith, A. J., Hallum-Montes, R., Nevin, K., Zenker, R., Sutherland, B., Reagor, S., et al. (2018). Determinants of transgender individuals’ well-being, mental health, and suicidality in a rural state. J. Rural Ment. Health 42, 116–132. doi: 10.1037/rmh0000089
Stephenson, R., Todd, K., Kahle, E., Sullivan, S. P., Miller-Perusse, M., Sharma, A., et al. (2020). Project moxie: results of a feasibility study of a telehealth intervention to increase HIV testing among binary and nonbinary transgender youth. AIDS Behav. 24, 1517–1530. doi: 10.1007/s10461-019-02741-z
Stryker, S., Currah, P., and Moore, L. J. (2008). Introduction: trans-, trans, or transgender? Women's Stud. Q. 36, 11–22. doi: 10.1353/WSQ.0.0112
Sun, C. J., Anderson, K. M., Kuhn, T., Mayer, L., and Klein, C. H. (2020). A sexual health promotion app for transgender women (trans women connected): development and usability study. JMIR Mhealth Uhealth 8:e15888. doi: 10.2196/15888
Sun, C. J., Anderson, K. M., Mayer, L., Kuhn, T., and Klein, C. H. (2019). Findings from formative research to develop a strength-based HIV prevention and sexual health promotion mHealth intervention for transgender women. Transgend. Health 4, 350–358. doi: 10.1089/trgh.2019.0032
TGEU (Trans Europe and Central Asia). (2024). Intersectionality. Available at: https://www.tgeu.org/topics/trans-intersectionality/ (Accessed October 28, 2024).
Tricco, A. C., Lillie, E., Zarin, W., O'Brien, K. K., Colquhoun, H., Levac, D., et al. (2018). PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann. Intern. Med. 169, 467–473. doi: 10.7326/M18-0850
van der Miesen, A. I. R., Raaijmakers, D., and van de Grift, T. C. (2020). “You have to wait a little longer”: transgender (mental) health at risk as a consequence of deferring gender-affirming treatments during COVID-19. Arch. Sex. Behav. 49, 1395–1399. doi: 10.1007/s10508-020-01754-3
Wang, Y., Pan, B., Liu, Y., Wilson, A., Ou, J., and Chen, R. (2020). Health care and mental health challenges for transgender individuals during the COVID-19 pandemic. Lancet Diabetes Endocrinol. 8, 564–565. doi: 10.1016/S2213-8587(20)30182-0
Wernhart, A., Gahbauer, S., and Haluza, D. (2019). eHealth and telemedicine: practices and beliefs among healthcare professionals and medical students at a medical university. PLoS One 14:e0213067. doi: 10.1371/journal.pone.0213067
Wirtz, A. L., Cooney, E. E., Stevenson, M., Radix, A., Poteat, T., Wawrzyniak, A. J., et al. (2021). Digital epidemiologic research on multilevel risks for HIV acquisition and other health outcomes among transgender women in eastern and southern United States: protocol for an online cohort. JMIR Res. Protoc. 10:e29152. doi: 10.2196/29152
World Health Organisation (2010). Telemedicine: Opportunities and developments in member states: Report on the second global survey on eHealth. Geneva: World Health Organisation.
World Health Organization (WHO). (2024). Gender incongruence and transgender health in the ICD. Available at: https://www.who.int/standards/classifications/frequently-asked-questions/gender-incongruence-and-transgender-health-in-the-icd (Accessed June 17, 2024).
Keywords: transgender persons, transgender health, scoping review, COVID-19, telehealth, transgender men, transgender women
Citation: Gahbauer S and Haluza D (2024) Transgender health issues addressed in research on telehealth use: a scoping review. Front. Sociol. 9:1371524. doi: 10.3389/fsoc.2024.1371524
Edited by:
Rosa Fernández, University of A Coruña CICA-INIBIC Strategic Group, SpainReviewed by:
Meenakshi Khapre, All India Institute of Medical Sciences, IndiaSnehil Kumar Singh, UNICEF, Malawi
Copyright © 2024 Gahbauer and Haluza. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Susanne Gahbauer, c3VzYW5uZS5nYWhiYXVlckBtZWR1bml3aWVuLmFjLmF0
 Susanne Gahbauer
Susanne Gahbauer Daniela Haluza
Daniela Haluza