- 1Department of Psychology, University of Ghana, Accra, Ghana
- 2School of Psychology, University of Leeds, Leeds, United Kingdom
Background: A growing body of evidence from high-income contexts suggests a strong association between sexual violence victimisation and self-harm and eventual suicide. However, both sexual violence and self-harm among adolescents are still less researched in sub-Saharan African countries, including Ghana.
Objectives: To estimate the 12-month prevalence of self-harm, and to describe the associated factors and reported reasons for self-harm among school-going adolescent survivors of sexual violence victimisation during the previous 12 months in urban Ghana.
Methods: Analytic data came from a regional-based representative cross-sectional survey including in-school youth (N = 1,723) conducted in 2017 within the Greater Accra Region of Ghana. Of these, 297 (17.2%) self-reported sexual violence victimisation in the previous 12 months; this proportion of the participants (n = 297) was the focus of the current study. Items measuring sexual violence victimisation, self-harm, and correlates were adopted from the 2012 Ghana WHO–Global School-based Student Health Survey and the Child and Adolescent Self-harm in Europe Study. Data analysis involved multivariable logistic regression models.
Results: The estimate of self-harm ideation during the previous 12 months was 45.8% (95% CI: 40–52), whereas the estimate of self-harm behaviour was 38.7% (95% CI: 33–44). About two in five of the participants who reported self-harm wanted to die by their last episode of the behaviour. While bullying victimisation was associated with increased odds of self-harm ideation (aOR = 1.97, 95% CI 1.17, 3.31, p = 0.010) and behaviour (aOR = 2.76, 95% CI 1.59, 4.80, p < 0.001), weekly alcohol use (aOR = 2.56, 95% CI 1.32, 4.93, p = 0.005), conflict with parents (aOR = 2.30, 95% CI 1.28, 4.12, p = 0.005), and physical abuse victimisation (aOR = 1.80, 95% CI 1.03, 3.15, p = 0.037) showed strong associations with increased odds of self-harm behaviour in the past 12 months.
Conclusions: The evidence underscores the need for both universal and targeted multi-level intervention and prevention programmes to mitigate the offence of sexual violence and reduce the chances of self-harm among adolescent survivors of sexual violence in urban Ghana.
Introduction
According to the World Health Organisation (WHO), sexual violence1 is “any sexual act, attempt to obtain a sexual act, unwanted sexual comments or advances, or acts to traffic, or otherwise directed, against a person's sexuality using coercion, by any person regardless of their relationship to the victim, in any setting, including but not limited to home and work” (Krug et al., 2002). The United Nations Children's Fund (UNICEF) estimates that across the world, about 13 million girls (representing one in every 20 girls) aged 15–19 years have experienced forced sex in their lifetime (UNICEF, 2014). As has been reported in high-income countries (UNICEF, 2014; UNICEF, UN Women, and Plan International, 2020), evidence from low- and middle-income countries (LAMICs), including those in sub-Saharan Africa suggests that boys are not exempt from sexual violence victimisation, even though girls are mostly abused (Veenema et al., 2015; Adjei and Saewyc, 2017). For example, in sub-Saharan Africa, self-reported lifetime prevalence estimates of sexual violence range between 33.5 and 36.2% among females and between 19.5 and 21.0% among males (Brown et al., 2009; Nguyen et al., 2019; Seff and Stark, 2019). In Ghana, a national household survey of sexual abuse victimisation has reported lifetime estimates of 38.2% among females and 19.4% among males, and 12-month estimates of 22.1% among females and 19.4% among males aged 15–19 years (Institute of Development Studies, 2016).
Besides poor academic outcomes and negative social and interpersonal problems, sexual violence victimisation among adolescents is associated with a wide-range of negative mental and physical health outcomes, including HIV and other sexually transmitted infections, broken bones, head trauma, depression, anxiety, and post-traumatic stress disorder (Wells et al., 1997; Daignault and Hebert, 2009; UNICEF, 2014; McLaughlin and Sheridan, 2016; Oram et al., 2017; McTavish et al., 2019; Nguyen et al., 2019; Seff and Stark, 2019). A growing body of evidence (mostly from high-income contexts) suggests that sexual violence victimisation is a strong risk for self-harm2, suicidal ideations, and eventual suicide among adolescents (Brown et al., 1999; Beautrais, 2000; Martin et al., 2004; Ystgaard et al., 2004; Klonsky and Moyer, 2008; Miller et al., 2013; Seff and Stark, 2019; Alix et al., 2020; Baiden et al., 2020). For example, evidence from Australia indicates that 54% of sexually abused (compared with 17% non-abused) adolescents report ever intentionally self-harming, while 32% of sexually abused adolescents versus 2% non-abused adolescents ever tried to take their own life five or more times (Martin et al., 2004).
A recent systematic review of the literature on self-harm, generally, among adolescents in sub-Saharan Africa reports a 12-month median prevalence estimate of 16.9% (interquartile range [IQR] = 11.5–25.5%) (Quarshie et al., 2020). However, thus far, only a few studies from countries in sub-Saharan Africa have reported self-harm specifically among adolescents with a history of sexual violence victimisation. An earlier study from Nigeria reported a 12-month prevalence estimate of suicidal ideation (40.8%) and suicidal attempt (24.2%) among in-school adolescents (Omigbodun et al., 2008). Recently, a cross-national survey has reported lifetime prevalence estimates of suicidal ideation and self-injury among adolescent victims of coerced or forced sexual initiation in three countries – Nigeria, Uganda, and Zimbabwe (Nguyen et al., 2019). Suicidal ideation ranged between 5.4 and 32% [Nigeria = 10.0% (5.4–14.7), Uganda = 23.8% (15.5–32.0), Zambia = 19.6% (11.9–27.3)], and self-injury ranged from 7.8 to 29.2% [Nigeria = 13.8% (7.8–19.8), Uganda = 13.3% (7.0–19.6), and Zambia = 20.9% (12.7–29.2)] (Nguyen et al., 2019).
Besides sexual violence victimisation being a single important risk factor for self-harm among adolescents, evidence from high-income countries suggests that sexually abused adolescents who are also exposed to negative school and peer-related factors (e.g., bullying), family dysfunctions (e.g., parent-child conflict), and mental health problems (e.g., anxiety, depression, alcohol, and substance use) are at an elevated risk of self-harm and even suicide (Yeo and Yeo, 1993; Boudewyn and Liem, 1995; Romans et al., 1995; Martin et al., 2004; Ystgaard et al., 2004). Compared to high-income countries, little is still known from African countries about other correlates in the form of adverse experiences that are associated with self-harm among sexually abused adolescents, while no published evidence exists from the region on self-reported reasons for self-harm among adolescent victims of sexual violence (Brown et al., 2009; Gage, 2013; Cluver et al., 2015; Nguyen et al., 2019; Seff and Stark, 2019; Quarshie et al., 2020). Taken together, given that the target to reduce suicide-related deaths has been prioritised in the sustainable development goals (UN Statistical Commission, 2016; Patel et al., 2018) and self-harm represents that single strongest risk for suicide (WHO, 2014; Naghavi and Global Burden of Disease Self-Harm Collaborators, 2019), it has become imperative to contribute sound and timely evidence through self-harm research, to inform intervention and prevention efforts, particularly, among young vulnerable groups including adolescent survivors of sexual violence in LAMICs, where 78% of the global suicide mortalities are reported from Bachmann (2018).
Aims of Study
(i) Estimate the self-reported 12-month prevalence of self-harm ideation and behaviour among school-going adolescent3 survivors of sexual violence victimisation in urban Ghana.
(ii) Identify the self-reported reasons/motivations for self-harm among school-going adolescent survivors of sexual violence victimisation.
(iii) Describe some of the factors associated with self-harm among school-going adolescent survivors of sexual violence victimisation in urban Ghana.
Materials and Methods
Study Design and Participants
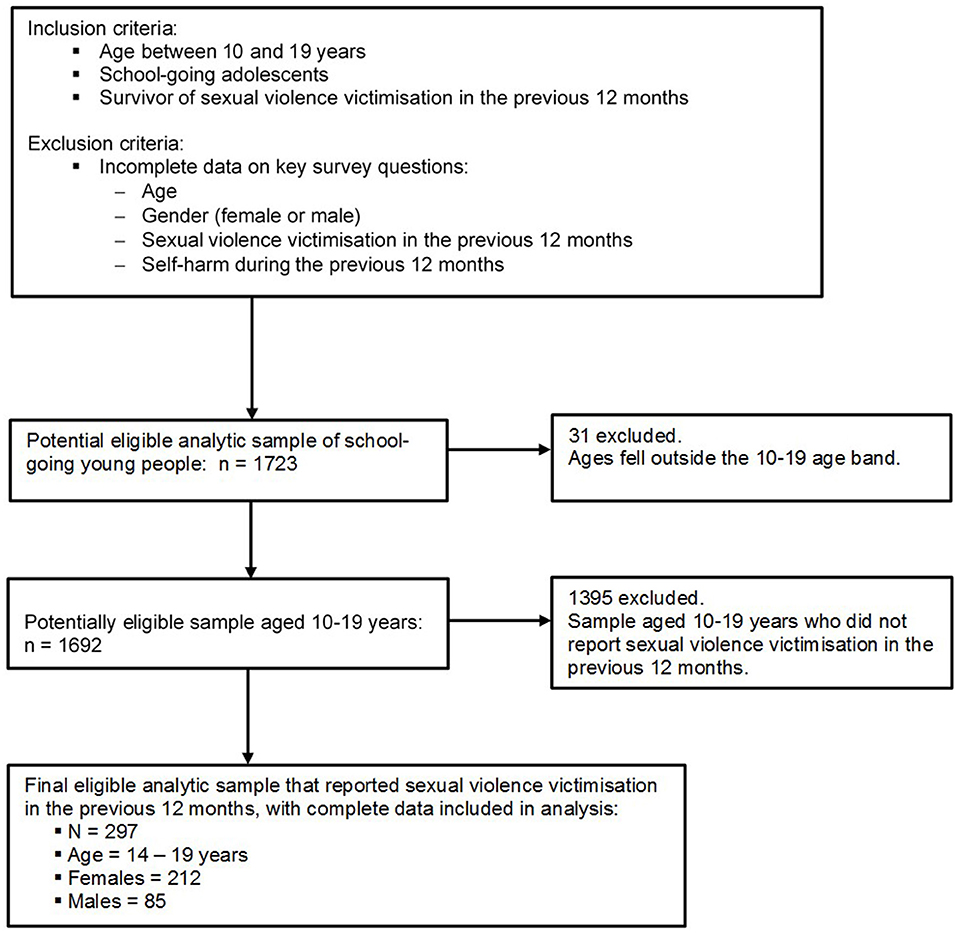
This study draws data from a regionally representative large cross-sectional self-report school-based survey data collected in 2017 in the Greater Accra Region of Ghana—details of the methods and ethical issues have been reported elsewhere (Quarshie, 2019). In short, the design of the survey followed the community-agreed recommendations of Strengthening the Reporting of Observational Studies in Epidemiology—STROBE (Vandenbroucke et al., 2007). A two-stage cluster sampling approach was used. Firstly, 20 schools were selected, with probability proportional to their student population size. Secondly, classes were selected randomly also with probability proportional to class enrolment size, and all students in each selected class were invited to respond to the survey. Across the 20 schools, 1,723 students aged 13–21 years answered the questionnaire, although 1,928 students were invited to participate in the study—representing a response rate of 89.4%. Figure 1 shows the analytic sample selection procedure and the inclusion and exclusion criteria applied in the current study.
Of the 1,723 students, 1,692 fell within the adolescent age band criterion of 10–19 years. The survey assessed sexual violence victimisation with a binary-response (No or Yes) single-item: “Has anyone forced you (i.e., physically or verbally) to engage in sexual activities against your will during the past 12 months?” Two hundred and ninety-seven (297) of the 1,692 adolescent participants reported sexual violence victimisation during the 12 months preceding the survey—this represented the analytic sample for the current study (Figure 1).
Measures
The questionnaire for the survey was in English, the language of instructions in schools in Ghana and the official language and lingua franca of the country. The measures included in this study covered demographic variables, lifestyle and social adversity factors, and outcome variables. The list of variables and specific questions used to assess them in the survey are provided in the Supplementary Table 1.
Exposures
Lifestyle Factors and Social Adversity
Nine binary (No or Yes) response rated lifestyle factors and variables assessing the experience of social and interpersonal adversities, adopted mainly from the 2012 WHO–Global School-based Student Health Survey (WHO-GSHS) questionnaire used in Ghana (WHO, 2015) were included. These included weekly alcohol use (In a typical week, how many times do you have at least one alcoholic drink?), parental separation/divorce (Have your parents separated or divorced during the past 12 months?), conflict with parents (Have you had any serious arguments or fights with either or both of your parents during the past 12 months?), conflict between parents (Have your parents had any serious arguments or fights during the past 12 months?), bullying victimisation (During the past 12 months, how many days were you bullied?), and physical abuse victimisation (Have you been seriously physically beaten during the past 12 months?)—see Supplementary Table 1.
Demographic Variables
Nine socio-demographic variables were included: gender (female or male), age, family structure (measured by father's number of wives), living arrangement, primary caretaker, caretaker's employment status, religious group, romantic relationship status, and sexual orientation—see Supplementary Table 1.
Outcomes
Self-harm during the previous 12 months was the main outcome variable in this study. This was assessed with a dichotomous (No = 0 or Yes = 1) response rated single item: “Have you, actually, intentionally harmed yourself (e.g., cutting, burning, or poisoning yourself, or tried to harm yourself in some other way, for example, hanging, jumping from height etc.) during the past 12 months?” This study also assessed the experience of self-harm ideation4 in the previous 12 months: “Have you thought about harming yourself (e.g., cutting, burning, or poisoning yourself, or considered harming yourself in some other way, for example, hanging, jumping from height etc.) during the past 12 months?” (No = 0 or Yes = 1). Given the lack of contextually developed measures of self-harm from LAMICs (Aggarwal and Berk, 2015; Aggarwal et al., 2017; Quarshie et al., 2020), the current study adopted the items measuring self-harm—behaviour and ideation—from the Child and Adolescent Self-harm in Europe studies (Hawton et al., 2002; Madge et al., 2008).
Similarly, a 15-item checklist of frequently reported reasons or motivations for self-harm were adopted from the WHO/EURO Multicentre Study on self-harm (Hjelmeland et al., 2002) and the Child and Adolescent Self-harm in Europe studies (Madge et al., 2008). A previous study from Africa has found the checklist to yield satisfactory consistency between Uganda and Norway (Hjelmeland et al., 2008). Some of the reasons on the checklist include “I wanted others to pay for the way they treated me,” “I wanted to die,” and “I wanted to persuade someone to change his/her mind” (see Supplementary Table 2). Drawing on the African cosmological worldview of aetiology—which attributes events to forces beyond the control of the individual—(Gyekye, 1995, 2003; Assimeng, 2010; Mbiti, 2015) the survey included an additional reason, “It was the work of the devil.”
Data Collection Procedure
The questionnaire was expert-reviewed prior to the survey by a child-and-adolescent-health researcher, a developmental [child] psychologist, and a suicidologist in Ghana. In each participating school, the students were gathered in a larger classroom or assembly hall designated for the survey, with sitting arrangement spaced by reasonable distance to ensure participants had privacy while answering the questionnaire. On average, the completion of the questionnaire lasted between 22 and 45 min, after which each student placed their answered questionnaire in a box. The survey was conducted between May and September 2017.
Ethics
The Ethics Committee for the Humanities, University of Ghana, Accra, Ghana approved this study (Ref. No: ECH078/16-17). In keeping with the research ethics of the Ghana Education Service, permissions were sought from the heads and management of all the participating schools. Prior to responding to the survey, each participant signed an actual written consent; parents and guardians of underage participants provided consent, while participants aged 17 years and younger assented prior to taking part in the study.
Statistical Analysis
All statistical analyses were conducted using SPSS (version 26.0 for Windows). Missing responses were deleted list-wise during the analysis, as the loss of cases due to missing data was <5% (Graham, 2012). The Supplementary Table 1 shows the proportion of missing data for each variable included in the analysis. Frequencies and proportions were used to estimate the 12-month prevalence of self-harm (ideation and behaviour) and to assess the distribution of the socio-demographic variables, lifestyle and adversity factors, and reported reasons for self-harm. Similar to key evidence in self-harm research (Scoliers et al., 2009; Edmondson et al., 2016; Rasmussen et al., 2016; Taylor et al., 2018), the reported reasons for self-harm were grouped into “intrapersonal5” and “interpersonal6” (see Supplementary Table 2). Bivariable analysis using Chi square test was performed to assess the relationship between each of the exposure variables and self-harm (ideation and behaviour); Fisher's exact test was applied where the expected count of a cell was <5. Considering that age was a continuous variable, point-biserial correlation (rpb) test (Prematunga, 2012) was used to examine the possible bivariate relationship between age and self-harm (ideation and behaviour).
Adjusted and unadjusted multivariable logistic regression models were used to explore the possible associations between the exposures and the binary outcome variables, self-harm ideation and behaviour in the past 12 months. Variables included in the logistic regression models were considered regardless of the statistical significance of their bivariate relationships with the outcome variables (Sun et al., 1996; Babyak, 2004). The socio-demographic variables were included in the models as covariates. It must be noted though that in the initial models, “sexual orientation” was associated with very high or infinite odds ratios and confidence intervals, suggesting an existence of sparse data bias (Greenland et al., 2000, 2016a); thus, for a stable model, sexual orientation was excluded from the final logistic regression models. Results of the logistic regression were reported as odds ratios with 95% CIs (Greenland et al., 2016b) and p < 0.05 was used to determine statistically significant results.
Results
Characteristics of Participants
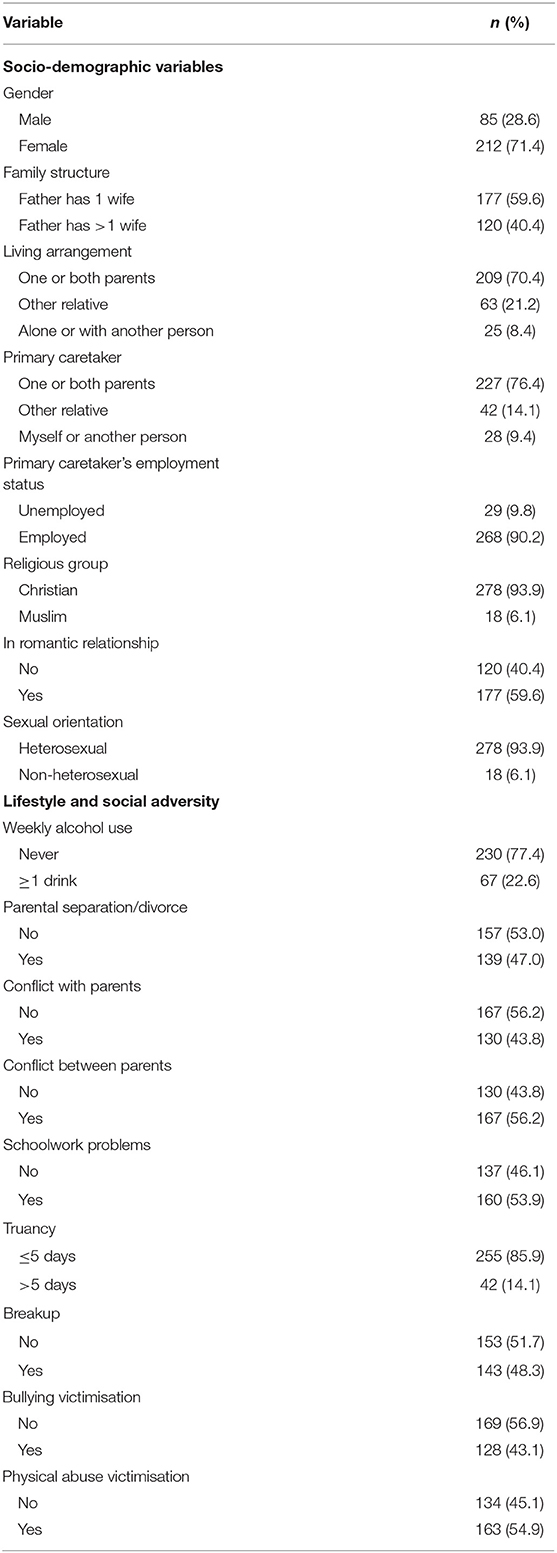
Table 1 presents the characteristics of the final analytic sample (n = 297); the participants were aged between 14 and 19 years (mean = 17.1; standard deviation = 1.1). There were more females (n = 212; 71.4%) than males (n = 85; 28.6%). Most participants (n = 177; 59.6%) reported having a father who had more than one wife.
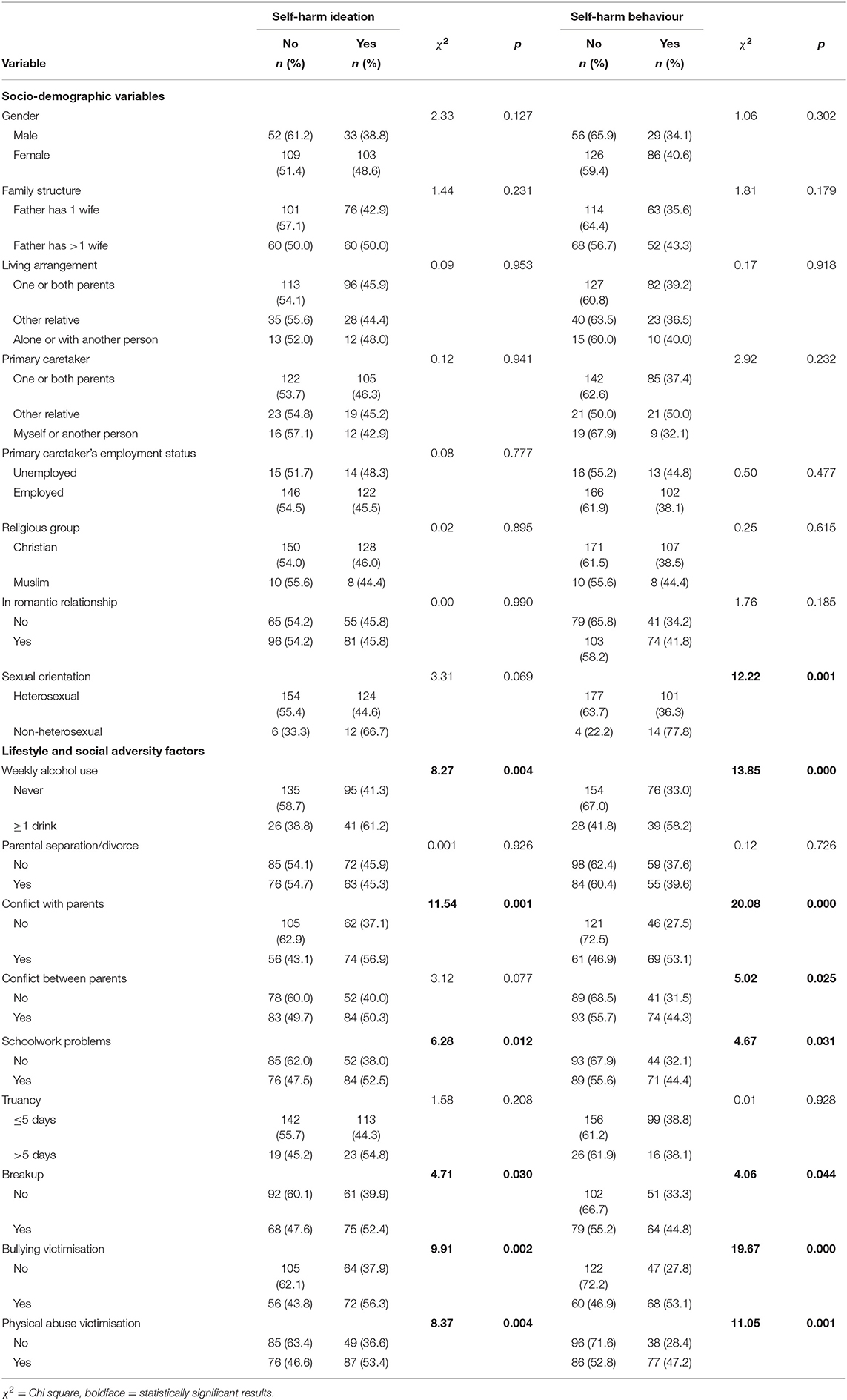
Prevalence Estimates of Self-Harm and Bivariate Associations
The estimate of self-harm ideation during the previous 12 months was 45.8% (95% CI: 40–52), whereas the estimate of self-harm behaviour was 38.7% (95% CI: 33–44). As shown in Table 2, the estimates of self-harm ideation and behaviour were comparable between females and males; the differences did not reach statistical significance. Also, Table 2 shows that adolescent survivors of sexual violence victimisation who reported conflict with their parents were likely than those who reported no conflict with their parents to experience self-harm ideation [ = 11.54, p = 0.001]. Bullying victimisation [ = 9.91, p = 0.002], physical abuse victimisation [ = 8.37, p = 0.004], and alcohol use [ = 8.27, p = 0.004] showed significant bivariate relationships with self-harm ideation.
Similarly, adolescent survivors of sexual violence victimisation who reported conflict with their parents were likely than those who reported no conflict with their parents to report self-harm behaviour [ = 20.08, p < 0.001]. Participants who experienced bullying victimisation [ = 19.67, p < 0.001], reported alcohol use [ = 13.85, p < 0.001], and physical abuse victimisation [ = 11.05, p = 0.001], and those who identified as non-heterosexual [ = 12.22, p = 0.001] were also likely to report self-harm behaviour during the previous 12 months. Age showed no statistically significant bivariate relationship with neither self-harm ideation (rpb = −0.045, N = 297, p = 0.438) nor self-harm behaviour (rpb = −0.14, N = 297, p = 0.808).
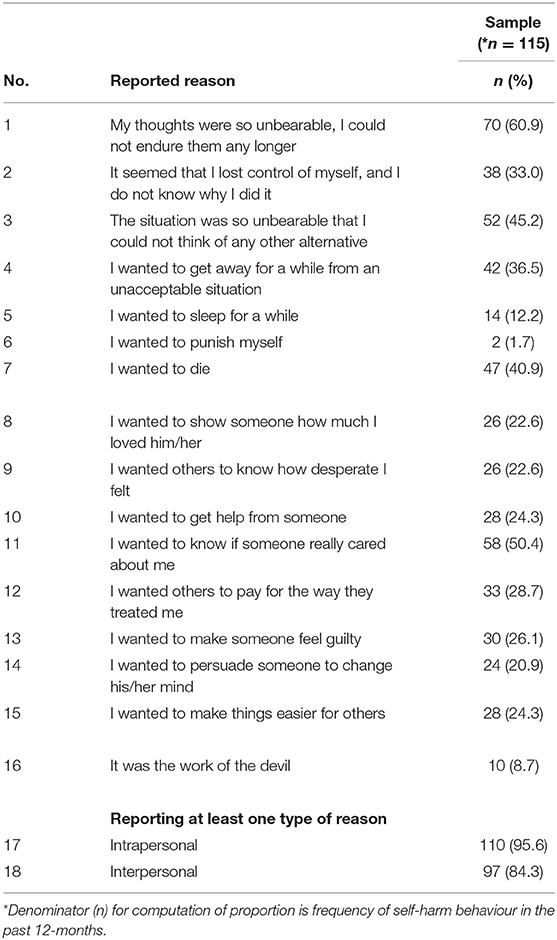
Reported Reasons/Motivations for Last Episode of Self-Harm
The participants reported multiple reasons, including both intrapersonal and personal motives, for their last episode of self-harm—see Table 3.
Generally, the participants checked more intrapersonal (95.6%) than interpersonal (84.3%) reasons for their self-harm behaviour. Specifically, the intrapersonal reason “My thoughts were so unbearable, I could not endure them any longer” was most frequently reported (60.9%), while the most frequently reported interpersonal reason was “I wanted to know if someone really cared about me” (50.4%). Notably, 40.9% of the 115 participants who reported self-harm behaviour indicated their motivation as “I wanted to die.” In other words, about two in five wanted to die by their self-harm.
Associations of Self-Harm
Self-Harm Ideation
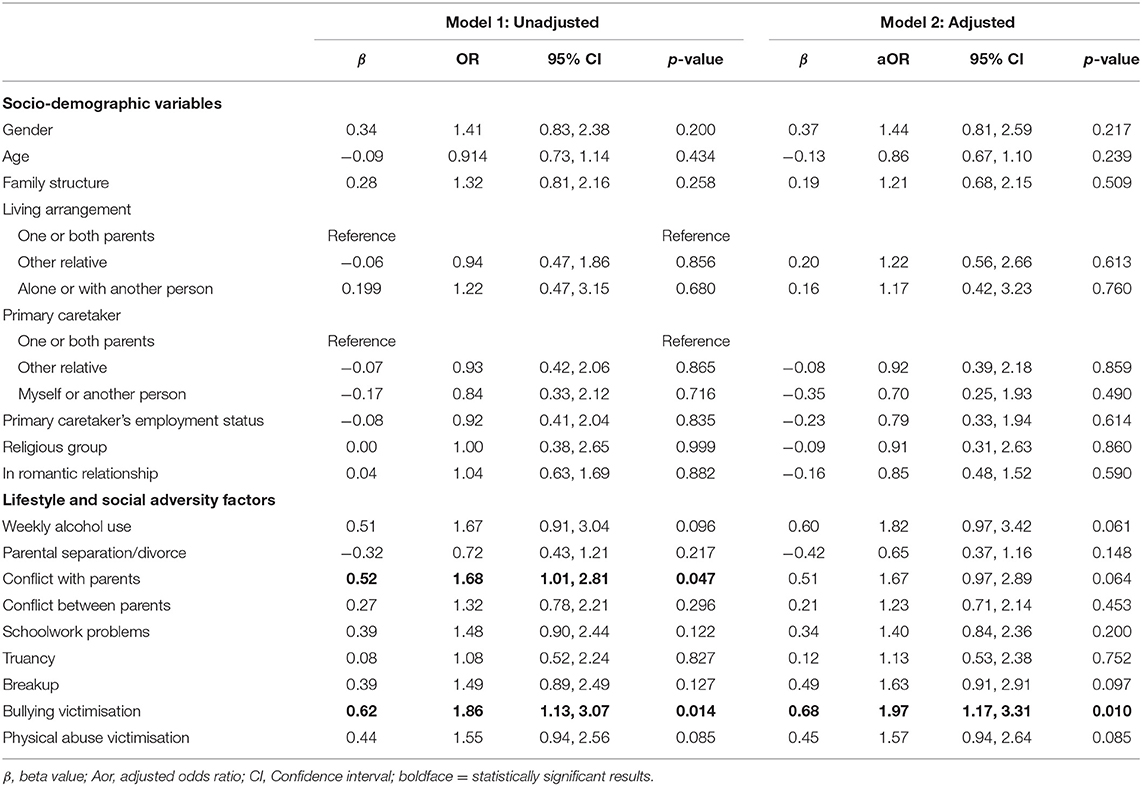
As shown in Table 4, no socio-demographic factor was observed to have a statistically significant association with neither increased nor reduced odds of self-harm ideation in both the unadjusted and adjusted models.
However, conflict with parents was associated with increased odds of self-harm ideation (OR = 1.68, 95% CI 1.01, 2.81, p = 0.047), while bullying victimisation was associated with increased odds of self-harm ideation in both the unadjusted (OR = 1.86, 95% CI 1.13, 3.07, p = 0.014) and adjusted (aOR = 1.97, 95% CI 1.17, 3.31, p = 0.010) models.
Self-Harm Behaviour
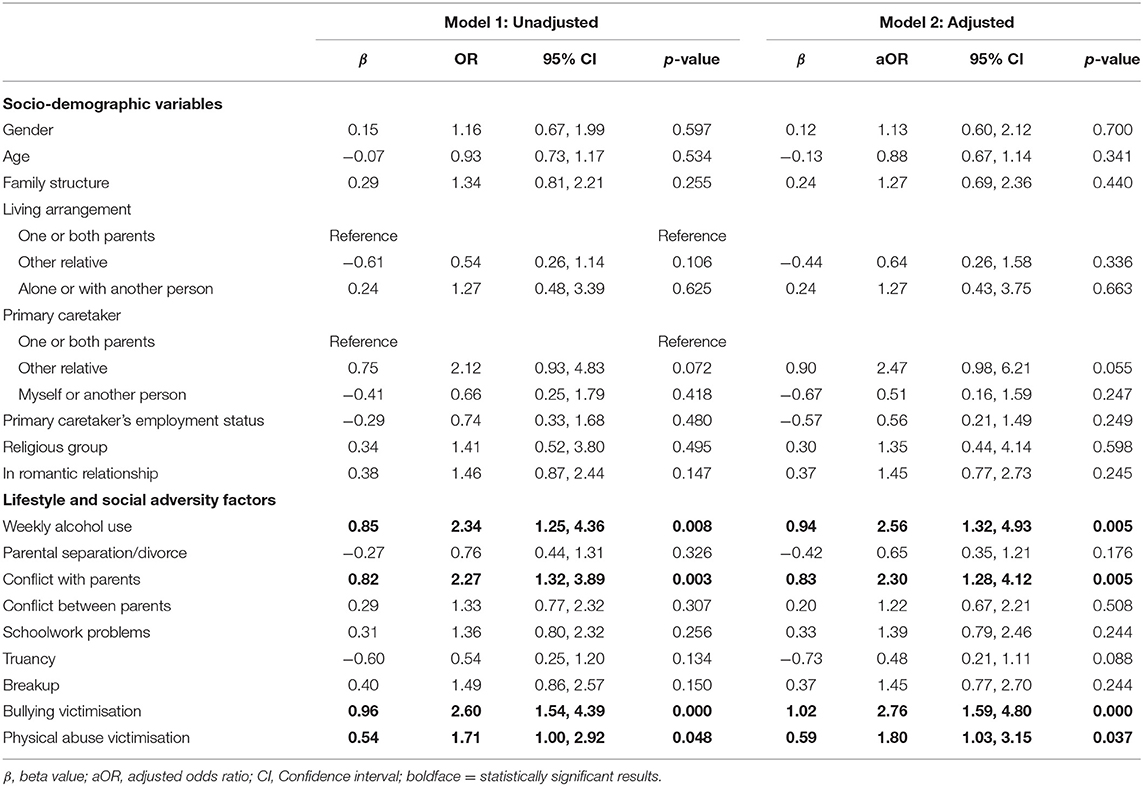
In the unadjusted model, bullying victimisation (OR = 2.60, 95% CI 1.54, 4.39, p < 0.001), weekly alcohol use (OR = 2.34, 95% CI 1.25, 4.36, p = 0.008), conflict with parents (OR = 2.27, 95% CI 1.32, 3.89, p = 0.003), and physical abuse victimisation (OR = 1.71, 95% CI 1.00, 2.92, p = 0.048) showed strong associations with increased odds of self-harm behaviour in the past 12 months—see Table 5.
Similarly, in the adjusted model, bullying victimisation (aOR = 2.76, 95% CI 1.59, 4.80, p < 0.001), weekly alcohol use (aOR = 2.56, 95% CI 1.32, 4.93, p = 0.005), conflict with parents (aOR = 2.30, 95% CI 1.28, 4.12, p = 0.005), and physical abuse victimisation (aOR = 1.80, 95% CI 1.03, 3.15, p = 0.037) showed strong associations with increased odds of self-harm behaviour in the past 12 months. However, in both unadjusted and adjusted models, no socio-demographic variable was observed to have a statistically significant association with self-harm behaviour.
Notably, bullying victimisation emerged as the only factor with a strong association with both self-harm ideation and behaviour across both unadjusted and adjusted models (Tables 4, 5).
Discussion
Taken together, the findings of this study show that: (1) about four out of 10 school-going adolescent survivors of sexual violence victimisation reported self-harm ideation, while three out of 10 reported self-harm behaviour in the previous 12 months; (2) school-going adolescent survivors of sexual violence victimisation reported more intrapersonal reasons for their last episode of self-harm, about two in five wanted to die by their self-harm; and (3) lifestyle and social adversity factors were associated with increased odds of self-harm ideation and behaviour; in particular, bullying victimisation showed a strong association with both self-harm ideation and behaviour.
The 12-month prevalence estimate of self-harm among adolescent survivors of sexual violence in the present study (38.7% [95% CI: 33–44%]) is higher, relative to the estimates of self-harm among the general population of adolescents across the region of sub-Saharan Africa [median: 16.9%; IQR = 11.5–25.5%] (Quarshie et al., 2020), and LAMICs [11.5–33.8%] (Aggarwal et al., 2017; Mannekote Thippaiah et al., 2020); it is still higher than the global estimates among the general population of adolescents [10.1–19.5%] (Lim et al., 2019). However, the estimate of self-harm in the present study is comparable to what has been reported among adolescent survivors of sexual violence in high-income countries; for example, Australia, where 54% intentionally self-harmed and 24% attempted suicide (Martin et al., 2004). Possibly, this evidence of higher prevalence estimates could be underscoring the importance of sexual violence victimisation as a critical risk for self-harm among adolescents (Klonsky and Moyer, 2008; Brown et al., 2009; Miller et al., 2013; UNICEF, 2014). The high prevalence estimate could also be supportive of the evidence that adolescent survivors of sexual violence experience significant emotional problems and psychological disturbance, which in turn lead up to self-harm (Brown et al., 1999; Beautrais, 2000).
In the light of both the African and global literature, the current study represents the first effort at reporting evidence on the motivations of school-going adolescent survivors of sexual violence for engaging in self-harm. Many of the participants reported constriction of thought and inability to generate alternative courses of action, but also experienced the motivation to die. About two in five wanted to die by their self-harm. This finding is comparable to evidence from high-income countries, where many adolescent survivors have reported death-intended self-harm behaviours (Brown et al., 1999; Beautrais, 2000; Martin et al., 2004; Ystgaard et al., 2004; Klonsky and Moyer, 2008; Miller et al., 2013; Seff and Stark, 2019; Alix et al., 2020; Baiden et al., 2020). For example, evidence from Australia indicates that 32% of sexually abused adolescents, compared to 2% non-abused adolescents, ever tried to take their own life five or more times (Martin et al., 2004).
Furthermore, this evidence supports the findings of earlier studies that, apart from clinically symptomatic depression and other internalising symptoms, the offence of sexual violence generates suicidal tendencies in adolescent survivors, as the abuse gravely affects the self-esteem and global self-worth of survivors (Serafini et al., 2015; McLaughlin and Sheridan, 2016; Mutavi et al., 2018a,b). Additionally, the finding that many of the adolescent survivors of sexual violence victimisation reported interpersonal reasons for their self-harm is to be expected, as many also had the motive of wanting “others to pay for the way they treated me.” This seeming vengeful motive could be indicative of the negative emotional responses and anger that are often experienced by survivors of sexual violence victimisation (Coyle et al., 2014; Boyle and Clay-Warner, 2018). However, further studies (involving qualitative approaches) are needed to explore the meanings of the self-harm motive “I wanted to make things easier for others” as reported by the adolescent survivors of sexual violence in the current study. While further research is needed to expand our understanding of this finding, the evidence is critical for the design and planning of intervention and prevention programmes against the onset of self-harm ideation and transition to self-harm behaviour among this vulnerable population of young people.
Regarding factors associated with self-harm among school-going adolescent survivors of sexual violence, this study has shown that lifestyle factors (such as weekly alcohol use) and adverse social experiences (i.e., bullying victimisation, conflict with parents, and physical abuse victimisation) have strong associations with increased odds of self-harm. This evidence is consistent with findings from a longitudinal study from South Africa (Cluver et al., 2015) and a global systematic review (Serafini et al., 2015) that multiple or cumulative exposures to adverse experiences among adolescents is associated with an elevated risk of self-harm. The dimension of adversity theory posits that exposure to multiple adverse experiences could fall between threat and deprivation, both of which could potentially compromise the (later) emotional well-being, cognitive development, and mental health of the individual (McLaughlin and Sheridan, 2016). Threat experiences (e.g., weekly alcohol use, sexual abuse victimisation, conflict with parents, bullying victimisation, and physical abuse victimisation) involve harm or threat of harm, while deprivation experiences involve absence of expected input from the environment (e.g., neglect, poverty). Each of these experiences of threat and deprivation are varied in severity and frequency, but they all involve (threat of) harm (McLaughlin and Sheridan, 2016; Lambert et al., 2017). In the current study, possibly, weekly alcohol use, conflict with parents, and physical abuse victimisation were threats that simultaneously compromised the resilience and resistance of the adolescents, thereby leading up to self-harm.
The finding that bullying victimisation was uniquely associated with both self-harm ideation and behaviour is worth some comments. This finding is worrying but not totally surprising, considering that sexual abuse is stigmatised and connotes unpleasant social labels and victim-blaming (UNICEF, 2014; Williamson and Serna, 2018). Evidence from Ghana indicates that entrenched patriarchal beliefs and rape myth acceptance tend to allow victim-blaming to fester (Boakye, 2009a,b). Thus, compared to non-abused adolescents, adolescent survivors of sexual violence victimisation tend to be at increased vulnerability to bullying and its attendant negative mental health outcomes, including self-blame, self-dislike, and potentially self-destructive behaviours (Hébert et al., 2016).
Relatedly, conflict between parents and their adolescent survivors of sexual violence victimisation is also of concern but not totally surprising, as there is evidence to suggest that some parents are less supportive of their child who has been sexually abused (Elliott and Carnes, 2001; Ullman, 2002). Recent evidence from Ghana suggests that some families of sexually abused children tend to misconstrue the abuse as a consequence of failed parenting and as a betrayal by their abused child; this often leads up to conflict between some parents and their sexually abused child (Tetteh and Markwei, 2018). The emergence of parent-child conflict in the context of child sexual abuse could lead to self-blame and other self-directed negative emotions and impulses on the part of the abused child, which in turn may lead up to self-harm.
Certainly, further expansive research is needed to extend the clarification of the evidence on the association between sexual violence victimisation and self-harm among adolescents in Ghana, but also across other countries in sub-Saharan Africa. Put together, the evidence of the current study highlights the need for universal and targeted multi-level intervention and prevention programmes at the individual level (e.g., teaching adolescents self-defence for reduced risk of sexual violence and bullying victimisation, helping adolescents to avoid alcohol and substance use, and teaching them emotional and social skills), family context (e.g., teaching effective parent-child communication characterised by emotional disclosure, and teaching supportive parenting skills), and the school environment (e.g., training school staff on promoting pro-mental health school climate, and enforcing existing child protection policies to stop bullying, sexual violence, and physical abuse of students). At the macro-level, it is strongly recommended that the government of Ghana and its stakeholder agencies (e.g., Ghana Education Service, Department of Social Welfare, Ministry of Gender, Children and Social Protection) continue to give full cooperation to the support lend by UNICEF toward the effective implementation of various child protection policies and social intervention programmes (National Development Planning Commission, UNICEF, and Ghana Statistical Service, 2020; UNICEF, 2020a,b).
Broadly, this study is in response to the recommendation for further evidence on self-harm among sexually abused young people, particularly, in LAMICs (Klonsky and Moyer, 2008; Miller et al., 2013; UNICEF, 2014; WHO, 2014; Nguyen et al., 2019). This study is the first from Ghana to report estimates of self-harm among adolescent survivors of sexual violence, and the first to contribute evidence to the global literature on reported reasons or self-reported motives for self-harm by adolescent survivors of sexual violence. Nonetheless, the interpretation and adoption of the evidence presented in this study must be done cautiously, owing to some notable limitations.
There is evidence from Ghana to suggest that the general non-supportive social environment precludes survivors of sexual violence from disclosing their abuse (Boakye, 2009b), and the criminalised and highly stigmatised status of self-harm (attempted suicide) also leads to increased non-disclosure and socially desirable responses among research participants (Osafo et al., 2015). The implication could be an underestimation of both self-reported sexual violence victimisation and self-harm. Notably though, the position of the current study is that, plausible non-reporting and underestimation might be low, as participants in the current study were allowed reasonable privacy in responding to the survey: a self-report anonymous questionnaire was used, teachers were not allowed into the location of the survey, and participants sat far apart from one another during the survey.
Furthermore, in this cross-sectional survey both the outcome and exposure variables were measured at the same point in time; this means that the findings reported in this study cannot support causal interpretations. It is also important to point out that the current study failed to include some key variables related to mental health—for example, depression, hopelessness, and anxiety—which have been found to mediate the association between sexual violence victimisation and self-harm (Martin et al., 2004; Klonsky and Moyer, 2008; Miller et al., 2013; Serafini et al., 2017). Whereas, the evidence of this study may be generalisable across urban in-school adolescents, they may not necessarily be applicable to adolescents in rural Ghana. Also, it is plausible that the single-item measure used in this study to assess sexual violence victimisation might have been partly inadequate in capturing the full nuances of sexual violence victimisation; similarly, even though single-item measures of self-harm facilitate the screening of larger research participants at a time, potentially, such measure could lead to misclassification of self-harm behaviours (Millner et al., 2015; Hom et al., 2016). Future, studies may consider applying validated checklist or multi-item measures with satisfactory ecological validity and relevance. Lastly, of the 297 adolescent survivors of sexual violence included in this study, 71.4% (n = 212) were females. While this disproportionate distribution potentially skews the results to be more applicable to females, it also precluded meaningful stratification and sub-group analysis of the data in terms of gender. Notably however, this observation is not intended to mean that the effects of sexual violence victimisation on females is more harmful than on males; sexual violence victimisation is troubling for both females and males in the immediate and long-terms.
Relatively, the estimates of self-harm among school-going adolescent survivors of sexual violence victimisation are higher; the motivations for self-harm are intrapersonal, including the motive to die. Social adversities in the family and school contexts present as strong factors associated with self-harm among school-going adolescent survivors of sexual violence victimisation. The evidence underscores the need for both universal and targeted multi-level intervention and prevention programmes to mitigate the offence of sexual violence and reduce the chances of self-harm among adolescent survivors of sexual violence in urban Ghana.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by The Ethics Committee for the Humanities, University of Ghana, Accra, Ghana approved this study (Ref. No: ECH078/16-17). Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author Contributions
The author confirms being the sole contributor of this work and has approved it for publication.
Funding
This study was supported by the Leeds International Research Scholarship (LIRS) at the University of Leeds, School of Psychology, in the form of a doctoral scholarship to the author (Grant No: CFN/sy/200631403). The funding did not cover cost of (open access) publication. The funder of the study had no role in the study design, data collection, data analysis, data interpretation, or writing of the report.
Disclaimer
The views expressed in this paper are those of the author and not necessarily those of the Leeds International Research Scholarship (LIRS).
Conflict of Interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The author thanks all the heads of the participating schools, the Director of the Greater Accra Regional Office of the Ghana Education Service, the Head of the Department of Social Welfare Headquarters, Accra, and parents/guardians of the study participants. Also, the author thanks all the participants who contributed data about their sexual violence victimisation and self-harm for this study.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsoc.2021.605865/full#supplementary-material
Footnotes
1. ^In the current study, “sexual violence”, “sexual abuse”, and “coerced sex” have been used interchangeably to mean the same phenomenon.
2. ^Self-harm is used in the current study to mean any intentional “act of self-poisoning or self-injury carried out by an individual irrespective of motivation” [National Institute for Health and Care Excellence (NICE), 2012, p.14].
3. ^This study applies WHO's chronological definition of an adolescent: an individual aged between 10 and 19 years (WHO, 2009).
4. ^Self-harm ideation is taken to mean having thoughts to engage in self-harm (self-harm behaviour).
5. ^Intrapersonal reasons for self-harm are related to attaining emotional or cognitive relief or punish self, etc.
6. ^Interpersonal reasons for self-harm are related to seeking help, communicating distress, punishing others, or influencing the behaviour of others.
References
Adjei, J. K., and Saewyc, E. M. (2017). Boys are not exempt: sexual exploitation of adolescents in sub-Saharan Africa. Child Abuse Negl. 65, 14–23. doi: 10.1016/j.chiabu.2017.01.001
Aggarwal, S., and Berk, M. (2015). Nonsuicidal self-injury in Indian adolescents: nonexistent or unacknowledged? Int. J. Soc. Psychiatry 61, 516–517. doi: 10.1177/0020764015579739
Aggarwal, S., Patton, G., Reavley, N., Sreenivasan, S. A., and Berk, M. (2017). Youth self-harm in low-and middle-income countries: systematic review of the risk and protective factors. Int. J. Soc. Psychiatry 63, 359–375. doi: 10.1177/0020764017700175
Alix, S., Cossette, L., Cyr, M., Frappier, J.-Y., Caron, P.-O., and Hébert, M. (2020). Self-blame, shame, avoidance, and suicidal ideation in sexually abused adolescent girls: a longitudinal study. J. Child Sex. Abus. 29, 432–447. doi: 10.1080/10538712.2019.1678543
Assimeng, M. (2010). Religion and Social Change in West Africa. An Introduction to the Sociology of Religion, 2nd Edn. Accra: Woeli Publishing Services.
Babyak, M. A. (2004). What you see may not be what you get: a brief, nontechnical introduction to overfitting in regression-type models. Psychosom. Med. 66, 411–421. doi: 10.1097/01.psy.0000127692.23278.a9
Bachmann, S. (2018). Epidemiology of suicide and the psychiatric perspective. Int. J. Environ. Res. Public Health 15:1425. doi: 10.3390/ijerph15071425
Baiden, P., Xiao, Y., Asiedua-Baiden, G., LaBrenz, C. A., Boateng, G. O., Graaf, G., et al. (2020). Sex differences in the association between sexual violence victimization and suicidal behaviors among adolescents. J. Affect. Disord. Rep. 1:100011. doi: 10.1016/j.jadr.2020.100011
Beautrais, A. L. (2000). Risk factors for suicide and attempted suicide among young people. Aust. N. Z. J. Psychiatry 34, 420–436. doi: 10.1080/j.1440-1614.2000.00691.x
Boakye, K. E. (2009a). Attitudes toward rape and victims of rape: a test of the feminist theory in Ghana. J. Interpers. Violence 24, 1633–1651. doi: 10.1177/0886260509331493
Boakye, K. E. (2009b). Culture and nondisclosure of child sexual abuse in Ghana: a theoretical and empirical exploration. Law Soc. Inquiry 34, 951–979. doi: 10.1111/j.1747-4469.2009.01170.x
Boudewyn, A. C., and Liem, J. H. (1995). Childhood sexual abuse as a precursor to depression and self-destructive behavior in adulthood. J. Trauma. Stress 8, 445–459. doi: 10.1002/jts.2490080307
Boyle, K. M., and Clay-Warner, J. (2018). Shameful “victims” and angry “survivors”: emotion, mental health, and labeling sexual assault. Violence Vctims 33, 436–452. doi: 10.1891/0886-6708.v33.i3.436
Brown, D. W., Riley, L., Butchart, A., Meddings, D. R., Kann, L., and Harvey, A. P. (2009). Exposure to physical and sexual violence and adverse health behaviours in African children: results from the Global School-based Student Health Survey. Bull. World Health Organ. 87, 447–455. doi: 10.2471/BLT.07.047423
Brown, J., Cohen, P., Johnson, J. G., and Smailes, E. M. (1999). Childhood abuse and neglect: specificity of effects on adolescent and young adult depression and suicidality. J. Am. Acad. Child Adolesc. Psychiatry 38, 1490–1496. doi: 10.1097/00004583-199912000-00009
Cluver, L., Orkin, M., Boyes, M. E., and Sherr, L. (2015). Child and adolescent suicide attempts, suicidal behavior, and adverse childhood experiences in South Africa: a prospective study. J. Adolesc. Health 57, 52–59. doi: 10.1016/j.jadohealth.2015.03.001
Coyle, E., Karatzias, T., Summers, A., and Power, M. (2014). Emotions and emotion regulation in survivors of childhood sexual abuse: the importance of “disgust” in traumatic stress and psychopathology. Eur. J. Psychotraumatol. 5:23306. doi: 10.3402/ejpt.v5.23306
Daignault, I. V., and Hebert, M. (2009). Profiles of school adaptation: social, behavioral and academic functioning in sexually abused girls. Child Abuse Negl. 33, 102–115. doi: 10.1016/j.chiabu.2008.06.001
Edmondson, A. J., Brennan, C. A., and House, A. O. (2016). Non-suicidal reasons for self-harm: a systematic review of self-reported accounts. J. Affect. Disord. 191, 109–117. doi: 10.1016/j.jad.2015.11.043
Elliott, A. N., and Carnes, C. N. (2001). Reactions of nonoffending parents to the sexual abuse of their child: a review of the literature. Child Maltreat. 6, 314–331. doi: 10.1177/1077559501006004005
Gage, A. J. (2013). Association of child marriage with suicidal thoughts and attempts among adolescent girls in Ethiopia. J. Adolesc. Health 52, 654–656. doi: 10.1016/j.jadohealth.2012.12.007
Graham, J. W. (2012). Missing Data: Analysis and design. New York, NY: Springer. doi: 10.1007/978-1-4614-4018-5
Greenland, S., Mansournia, M. A., and Altman, D. G. (2016a). Sparse data bias: a problem hiding in plain sight. BMJ 352:i1981. doi: 10.1136/bmj.i1981
Greenland, S., Schwartzbaum, J. A., and Finkle, W. D. (2000). Problems due to small samples and sparse data in conditional logistic regression analysis. Am. J. Epidemiol. 151, 531–539. doi: 10.1093/oxfordjournals.aje.a010240
Greenland, S., Senn, S. J., Rothman, K. J., Carlin, J. B., Poole, C., Goodman, S. N., et al. (2016b). Statistical tests, P values, confidence intervals, and power: a guide to misinterpretations. Eur. J. Epidemiol. 31, 337–350. doi: 10.1007/s10654-016-0149-3
Gyekye, K. (1995). An Essay on African Philosophical Thought: The Akan Conceptual Scheme. Philadelphia, PA: Temple University Press.
Gyekye, K. (2003). African Cultural Values. An Introduction. Washington, DC: Sankofa Publishing Company.
Hawton, K., Rodham, K., Evans, E., and Weatherall, R. (2002). Deliberate self harm in adolescents: self report survey in schools in England. BMJ 325, 1207–1211. doi: 10.1136/bmj.325.7374.1207
Hébert, M., Cénat, J. M., Blais, M., Lavoie, F., and Guerrier, M. (2016). Child sexual abuse, bullying, cyberbullying, and mental health problems among high schools students: a moderated mediated model. Depress. Anxiety 33, 623–629. doi: 10.1002/da.22504
Hjelmeland, H., Hawton, K., Nordvik, H., Bille-Brahe, U., De Leo, D., Fekete, S., et al. (2002). Why people engage in parasuicide: a cross-cultural study of intentions. Suicide Life-Threat. Behav. 32, 380–393. doi: 10.1521/suli.32.4.380.22336
Hjelmeland, H., Knizek, B. L., Kinyanda, E., Musisi, S., Nordvik, H., and Svarva, K. (2008). Suicidal behavior as communication in a cultural context: a comparative study between Uganda and Norway. Crisis 29, 137–144. doi: 10.1027/0227-5910.29.3.137
Hom, M. A., Joiner Jr, T. E., and Bernert, R. A. (2016). Limitations of a single-item assessment of suicide attempt history: implications for standardized suicide risk assessment. Psychol. Assess. 28, 1026–1030. doi: 10.1037/pas0000241
Institute of Development Studies, Ghana Statistical Services, and Associates (2016). Domestic Violence in Ghana: Incidence, Attitudes, Determinants and Consequences. Brighton: Institute of Development Studies.
Klonsky, E. D., and Moyer, A. (2008). Childhood sexual abuse and non-suicidal self-injury: meta-analysis. Br. J. Psychiatry 192, 166–170. doi: 10.1192/bjp.bp.106.030650
Krug, E. G., Dahlberg, L. L., Mercy, J. A., Zwi, A. B., and Lozano, R., (eds.). (2002). World Report on Violence and Health. Geneva: World Health Organization. doi: 10.1016/S0140-6736(02)11133-0
Lambert, H. K., King, K. M., Monahan, K. C., and McLaughlin, K. A. (2017). Differential associations of threat and deprivation with emotion regulation and cognitive control in adolescence. Dev. Psychopathol. 29, 929–940. doi: 10.1017/S0954579416000584
Lim, K.-S., Wong, C. H., McIntyre, R. S., Wang, J., Zhang, Z., Tran, B. X., et al. (2019). Global lifetime and 12-month prevalence of suicidal behavior, deliberate self-harm and non-suicidal self-injury in children and adolescents between 1989 and 2018: a meta-analysis. Int. J. Environ. Res. Public Health 16:4581. doi: 10.3390/ijerph16224581
Madge, N., Hewitt, A., Hawton, K., Wilde, E. J. d., Corcoran, P., et al. (2008). Deliberate self-harm within an international community sample of young people: comparative findings from the Child and Adolescent Self-harm in Europe (CASE) Study. J. Child Psychol. Psychiatry 49, 667–677. doi: 10.1111/j.1469-7610.2008.01879.x
Mannekote Thippaiah, S., Shankarapura Nanjappa, M., Gude, J. G., Voyiaziakis, E., Patwa, S., Birur, B., et al. (2020). Non-suicidal self-injury in developing countries: a review. Int. J. Soc. Psychiatry. doi: 10.1177/0020764020943627. [Epub ahead of print].
Martin, G., Bergen, H. A., Richardson, A. S., Roeger, L., and Allison, S. (2004). Sexual abuse and suicidality: gender differences in a large community sample of adolescents. Child Abuse Negl. 28, 491–503. doi: 10.1016/j.chiabu.2003.08.006
McLaughlin, K. A., and Sheridan, M. A. (2016). Beyond cumulative risk: a dimensional approach to childhood adversity. Curr. Direc. Psychol. Sci. 25, 239–245. doi: 10.1177/0963721416655883
McTavish, J. R., Sverdlichenko, I., MacMillan, H. L., and Wekerle, C. (2019). Child sexual abuse, disclosure and PTSD: a systematic and critical review. Child Abuse Negl. 92, 196–208. doi: 10.1016/j.chiabu.2019.04.006
Miller, A. B., Esposito-Smythers, C., Weismoore, J. T., and Renshaw, K. D. (2013). The relation between child maltreatment and adolescent suicidal behavior: a systematic review and critical examination of the literature. Clin. Child Fam. Psychol. Rev. 16, 146–172. doi: 10.1007/s10567-013-0131-5
Millner, A. J., Lee, M. D., and Nock, M. K. (2015). Single-item measurement of suicidal behaviors: validity and consequences of misclassification. PLoS ONE 10:e0141606. doi: 10.1371/journal.pone.0141606
Mutavi, T., Obondo, A., Kokonya, D., Khasakhala, L., Mbwayo, A., Njiri, F., et al. (2018a). Incidence of depressive symptoms among sexually abused children in Kenya. Child Adolesc. Psychiat. Mental Health 12:40. doi: 10.1186/s13034-018-0247-y
Mutavi, T., Obondo, A., Mathai, M., Kokonya, D., and Dako-Gyeke, M. (2018b). Incidence of self-esteem among children exposed to sexual abuse in Kenya. Glob. Soc. Welfare 5, 39–47. doi: 10.1007/s40609-017-0107-3
Naghavi, M., and Global Burden of Disease Self-Harm Collaborators. (2019). Global, regional, and national burden of suicide mortality 1990 to 2016: systematic analysis for the Global Burden of Disease Study 2016. BMJ 364:l94. doi: 10.1136/bmj.l94
National Development Planning Commission, UNICEF, and Ghana Statistical Service (2020). Multi-Dimensional Child Poverty in Ghana. Accra: National Development Planning Commission.
National Institute for Health and Care Excellence (NICE) (2012). Self-harm: Longer-term management. The British Psychological Society and the Royal College of Psychiatrists.
Nguyen, K. H., Padilla, M., Villaveces, A., Patel, P., Atuchukwu, V., Onotu, D., et al. (2019). Coerced and forced sexual initiation and its association with negative health outcomes among youth: results from the Nigeria, Uganda, and Zambia violence against children surveys. Child Abuse Negl. 96:104074. doi: 10.1016/j.chiabu.2019.104074
Omigbodun, O., Dogra, N., Esan, O., and Adedokun, B. (2008). Prevalence and correlates of suicidal behaviour among adolescents in southwest Nigeria. Int. J. Soc. Psychiatry 54, 34–46. doi: 10.1177/0020764007078360
Oram, S., Khalifeh, H., and Howard, L. M. (2017). Violence against women and mental health. Lancet Psychiatry 4, 159–170. doi: 10.1016/S2215-0366(16)30261-9
Osafo, J., Akotia, C. S., Andoh-Arthur, J., and Quarshie, E. N.-B. (2015). Attempted suicide in Ghana: motivation, stigma, and coping. Death Stud. 39, 274–280. doi: 10.1080/07481187.2014.991955
Patel, V., Saxena, S., Lund, C., Thornicroft, G., Baingana, F., Bolton, P., et al. (2018). The Lancet Commission on global mental health and sustainable development. Lancet 392, 1553–1598. doi: 10.1016/S0140-6736(18)31612-X
Prematunga, R. K. (2012). Correlational analysis. Aust. Crit. Care 25, 195–199. doi: 10.1016/j.aucc.2012.02.003
Quarshie, E. N.-B. (2019). Self-harm in adolescents in Ghana. Doctoral Thesis. University of Leeds, Leeds, United Kingdom. Available online at: http://etheses.whiterose.ac.uk/25720/ (accessed January 10, 2020).
Quarshie, E. N. B., Waterman, M. G., and House, A. O. (2020). Self-harm with suicidal and non-suicidal intent in young people in sub-Saharan Africa: a systematic review. BMC Psychiatry 20, 1–26. doi: 10.1186/s12888-020-02587-z
Rasmussen, S., Hawton, K., Philpott-Morgan, S., and O'Connor, R. C. (2016). Why do adolescents self-harm? An investigation of motives in a community sample. Crisis 37, 176–183. doi: 10.1027/0227-5910/a000369
Romans, S. E., Martin, J. L., Anderson, J. C., Herbison, G. P., and Mullen, P. E. (1995). Sexual abuse in childhood and deliberate self-harm. Am. J. Psychiatry 152, 1336–1342. doi: 10.1176/ajp.152.9.1336
Scoliers, G., Portzky, G., Madge, N., Hewitt, A., Hawton, K., De Wilde, E. J., et al. (2009). Reasons for adolescent deliberate self-harm: a cry of pain and/or a cry for help? Soc. Psychiatry Psychiatr. Epidemiol. 44, 601–607. doi: 10.1007/s00127-008-0469-z
Seff, I., and Stark, L. (2019). A sex-disaggregated analysis of how emotional violence relates to suicide ideation in low-and middle-income countries. Child Abuse Negl. 93, 222–227. doi: 10.1016/j.chiabu.2019.05.008
Serafini, G., Canepa, G., Adavastro, G., Nebbia, J., Belvederi Murri, M., Erbuto, D., et al. (2017). The relationship between childhood maltreatment and non-suicidal self-injury: a systematic review. Front. Psychiatry 8:149. doi: 10.3389/fpsyt.2017.00149
Serafini, G., Muzio, C., Piccinini, G., Flouri, E., Ferrigno, G., Pompili, M., et al. (2015). Life adversities and suicidal behavior in young individuals: a systematic review. Eur. Child Adolesc. Psychiatry 24, 1423–1446. doi: 10.1007/s00787-015-0760-y
Sun, G.-W., Shook, T. L., and Kay, G. L. (1996). Inappropriate use of bivariable analysis to screen risk factors for use in multivariable analysis. J. Clin. Epidemiol. 49, 907–916. doi: 10.1016/0895-4356(96)00025-X
Taylor, P. J., Jomar, K., Dhingra, K., Forrester, R., Shahmalak, U., and Dickson, J. M. (2018). A meta-analysis of the prevalence of different functions of non-suicidal self-injury. J. Affect. Disord. 227, 759–769. doi: 10.1016/j.jad.2017.11.073
Tetteh, P. M., and Markwei, U. (2018). Situating the notion of “gbekεfOηs” in the discourse of child sexual abuse among the Ga in Accra, Ghana. J. Child Sex. Abus. 27, 510–522. doi: 10.1080/10538712.2018.1477225
Ullman, S. E. (2002). Social reactions to child sexual abuse disclosures: a critical review. J. Child Sex. Abus. 12, 89–121. doi: 10.1300/J070v12n,01_05
UN Statistical Commission (2016). Report of the Inter-Agency and Expert Group on Sustainable Development Goal Indicators (E/CN.3/2016/2/Rev.1), Annex IV. Available online at: https://unstats.un.org/sdgs (accessed March 13, 2018).
UNICEF (2020b). Goal Area 5: Every Child has an Equitable Chance in Life. Global annual results report, 2019. UNICEF.
UNICEF UN Women, and Plan International (2020). A New Era for Girls: Taking Stock of 25 Years of Progress. UNICEF.
Vandenbroucke, J. P., Von Elm, E., Altman, D. G., Gøtzsche, P. C., Mulrow, C. D., Pocock, S. J., et al. (2007). Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. PLoS Med. 4:e297. doi: 10.1371/journal.pmed.0040297
Veenema, T. G., Thornton, C. P., and Corley, A. (2015). The public health crisis of child sexual abuse in low and middle income countries: an integrative review of the literature. Int. J. Nurs. Stud. 52, 864–881. doi: 10.1016/j.ijnurstu.2014.10.017
Wells, R., McCann, J., Adams, J., Voris, J., and Dahl, B. (1997). A validational study of the structured interview of symptoms associated with sexual abuse (SASA) using three samples of sexually abused, allegedly abused, and nonabused boys. Child Abuse Negl. 21, 1159–1167. doi: 10.1016/S0145-2134(97)00091-4
WHO (2009). Strengthening the health sector response to adolescent health and development. Geneva, Switzerland: WHO.
WHO (2015). Global School-Based Student Health Survey (GSHS) - Ghana. Available online at: https://www.who.int/ncds/surveillance/gshs/ghana/en/ (accessed February 10, 2016).
Williamson, J., and Serna, K. (2018). Reconsidering forced labels: outcomes of sexual assault survivors versus victims (and those who choose neither). Violence Against Women 24, 668–683. doi: 10.1177/1077801217711268
Yeo, H. M., and Yeo, W. W. (1993). Repeat deliberate self-harm: a link with childhood sexual abuse? Emerg. Med. J. 10, 161–166. doi: 10.1136/emj.10.3.161
Keywords: adolescents, Ghana, self-harm, sexual abuse, sexual violence, social adversity, suicide attempt, suicide
Citation: Quarshie EN-B (2021) Self-Harm Among School-Going Adolescent Survivors of Sexual Violence Victimisation: A Cross-Sectional Study. Front. Sociol. 6:605865. doi: 10.3389/fsoc.2021.605865
Received: 13 September 2020; Accepted: 15 March 2021;
Published: 20 May 2021.
Edited by:
Godfrey Zari Rukundo, Mbarara University of Science and Technology, UgandaReviewed by:
John W. Yuen, Hong Kong Polytechnic University, Hong KongOluwabunmi Buhari, University of Ilorin, Nigeria
Copyright © 2021 Quarshie. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Emmanuel Nii-Boye Quarshie, ZW5xdWFyc2hpZUB1Zy5lZHUuZ2g=; ZW5xdWFyc2hpZUBnbWFpbC5jb20=
 Emmanuel Nii-Boye Quarshie
Emmanuel Nii-Boye Quarshie