- 1Special Research Group Arts & Psychomotor Therapies/Master of Arts Therapies, HAN University of Applied Sciences, Nijmegen, Netherlands
- 2Karakter Child and Adolescent Psychiatry, University Center, Nijmegen, Netherlands
- 3GGNet, Centre for Mental Health, Scelta, Expert Centre for Personality Disorders Apeldoorn, Warnsveld, Netherlands
- 4KenVaK, Research Centre for the Arts Therapies, Hogeschool Zuyd, Heerlen, Netherlands
Background: Virtual Reality (VR) holds much promise for online offering of arts and psychomotor therapies. As these therapies use bodily experiences, expressive/artistic media, materials, movement, music, and (role) play, VR is more suitable than online/video consultations.
Objectives: This study was set up to improve VR possibilities for arts and psychomotor therapies, with the primary aim of redeveloping and rebuilding a VR application.
Methods: Using Lewin’s paradigm of Action Research in conjunction with the Lean Start up Method to develop Minimal Viable Products, we developed and built the Virtual Reality Health Experience (VRhExp), a full body multiplayer VR space providing online arts and psychomotor therapies. The Action Research concerned a one-year co-creation project involving 17 arts and psychomotor therapists (Mean age 44.1 years, SD 11.3) together with input from media designers in education and technical VR developers. The Action Research consisted of five cycles. All cycles were held in groups.
Results: We redeveloped an initial multiplayer full body VRhExp application based on users’ preferences, and ideas. Our participants reported becoming more proficient in using VR than at the start. Training and workshops held with arts and psychomotor therapists enhanced their knowledge of and skills in using the VRhExp. They provided input for the patient journey which was then used to develop a roadmap with the prerequisites for the implementation of the VRhExp in clinical practice. All participants indicated that the current version of VRhExp is not yet ready for use in clinical practice but appreciated that a great step forward had been made. Of the arts and psychomotor therapists who participated in the workshops, four out of five acknowledged the potential of acting and experiencing with the VRhExp (79%).
Conclusion: The VRhExp is a promising tool for patients with psychological disorders as it enables the continuity of care provision by therapists. The VRhExp is a first step towards developing a broader landscape for offering online experiential arts and psychomotor therapies.
Introduction
Prior to the COVID-19 pandemic, online therapy for psychological disorders had been shown to be a valuable aid to patient care (Betts, 2020; Deng et al., 2019; Hoppe et al., 2020; Maarsingh et al., 2019; Mozgai et al., 2020; Riva, 2005; Shamri Zeevi, 2021). However, the COVID-19 pandemic led to an increasing awareness among mental health professionals of the importance of being able to ensure continuity of care, and new routes to online healthcare provision became available.
During the COVID-19 pandemic, the majority of mental health professionals encountered both personal and technical barriers to providing online healthcare. While psychotherapy was achievable through online/video consultations, arts and psychomotor therapists faced greater barriers to providing online healthcare. Both arts and psychomotor therapists treat patients in an experiential manner; their therapies involve (visual) art, music, dance, drama, and psychomotor activities. Accommodating these therapies is more difficult in online video situations than in the more typical verbal interactions which characterize psychotherapy (Haeyen et al., 2020). A survey conducted among 281 arts and psychomotor therapists confirmed this; of the respondents, 91% indicated they lacked experience with providing online therapy (Haeyen, 2020).
Virtual Reality (VR) has much promise regarding applying these key properties of arts and psychomotor therapies. VR goes beyond video consultation as it provides a three-dimensional (3-D) artificially created environment which can be explored by patients (Riva, 2005). Patients become part of the virtual world in which they can interact with their therapist, manipulate objects, and perform action sequences. To date, the use of VR technology has been minimal among psychotherapists and arts and psychomotor therapists. VR applications are becoming trending in the field of psychotherapy (Shamri Zeevi, 2021; Gregg and Tarrier, 2007; Li and Shen, 2022) and now include a range of applications for amongst others treating fear of heights (Freeman et al., 2018; Krupić et al., 2021), anxiety (Carl et al., 2019) and psychosis (Pot-Kolder, 2021). VR is thus a potential vehicle for incorporating the key properties of arts and psychomotor therapies in online healthcare provision (Hacmun et al., 2018). However, VR has not yet been applied to the therapies typical of this professional field (Hacmun et al., 2021; Marks et al., 2017).
To address this lack of online provision of arts and psychomotor therapy, in 2019, our research group developed an initial multiplayer full body VR application: the VR Health Experience (Haeyen et al., 2021a; van den Berg, 2019). Dependent on a stable internet connection, patients and therapists could meet online and choose a full body avatar. Initial experiences with this multiplayer full body VR application were positive, as shown in a first study (Haeyen et al., 2021b). The participating arts and psychomotor therapists reported that VR enabled their patients to experience their possibilities, to practice new skills, and to achieve personal therapeutic aims.
However, limitations of the VR application became apparent as well. The principal concern was that most arts and psychomotor therapists indicated that they lacked the basic knowledge and skills to apply VR. This reflected their low perceived self-efficacy of their ability to apply VR in online therapy (Bandura, 1997). Therapists perceived self-efficacy as a cornerstone to successful patient treatment (Hacmun et al., 2018; Haeyen et al., 2021b; Békés and Aafjes-van Doorn, 2020). Other limitations concerned the VR application and its content. The first VR application was mainly developed based on psychomotor therapy and therefore included moving exercises, ball games, and the possibility to pick up objects. Consequently, there were limited exercises related to visual art, music, dance and drama therapies. To overcome this, arts and psychomotor therapists recommended extending the modalities in order to make the VR environment inclusive for all arts and psychomotor therapists (Haeyen et al., 2021a). Secondly, there were some technical limitations. Therapists could not create their own “private” session if other arts and psychomotor therapists and patients were present. Moreover, the scale-up capacity was insufficient; there was a need for extra spaces, changing avatars, implementing new game elements, and the ability to save a session for re-entry in the VR environment. Despite these limitations, the initial VR application showed great promise for developing arts and psychomotor therapies and mental healthcare.
The current study was therefore set up to improve VR possibilities for arts and psychomotor therapies based on our previous experiences. Our primary aim was to redevelop and rebuild the initial multiplayer full body VR application. We designated this new application the VR Health Experience (VRhExp). Moreover, we aimed to examine whether arts and psychomotor therapists’ knowledge and skills in using VRhExp could be enhanced using online training programs. Finally, we aimed to formulate a roadmap with the prerequisites for implementing VRhExp in clinical practice.
Methods
Design - Methodological framework
The VRhExp development and build was achieved in close co-creation with arts and psychomotor therapists (recruited through own network), media designers in education, and technical VR developers. With that goal, we adopted Action Research (AR). We applied established methods of Action Research as described by Lewin’s paradigm of Action Research (Lewin, 1946). AR addresses problems encountered by healthcare providers in busy clinical practice by intertwining action-taking with conducting research. In this way, AR promotes the interplay between different stakeholders. We followed Lewin’s core principles that AR is: 1) Participatory, in example, healthcare providers are actively involved as fellow researchers; 2) Cyclical, in example, the principle that acting occurs in multiple successive cycles; 3) Reflective, in example, the need to review whether the step in the previous cycle contributed to the intended development and building goals; 4) Context aware, in example, it accounts for both barriers and facilitators in the clinical setting; 5) Educational, in example, it develops healthcare providers’ knowledge and skills.
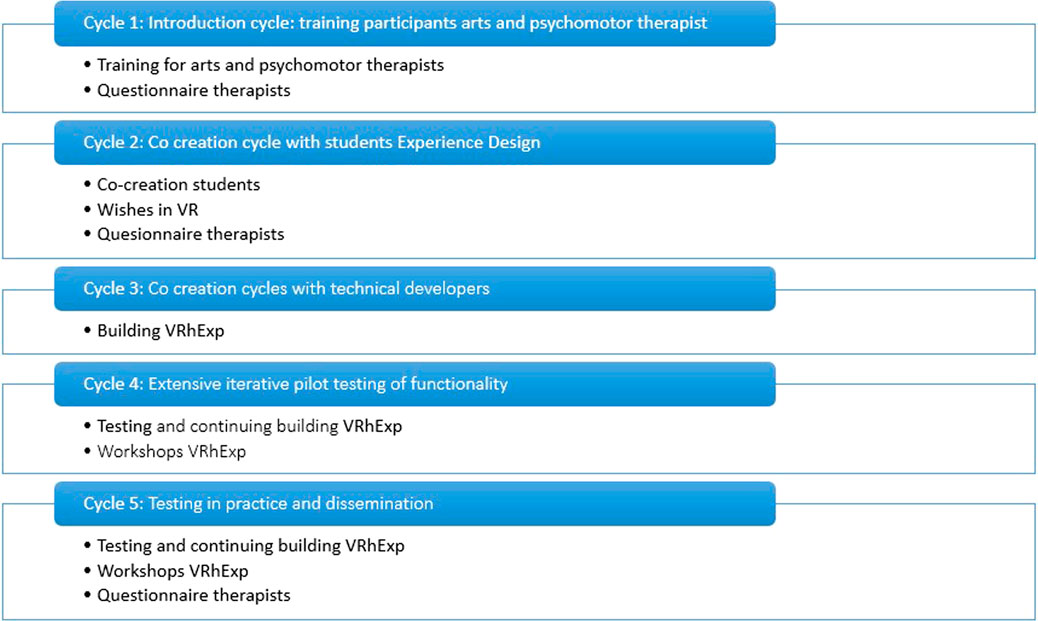
Our specific AR comprised the five cycles (Figure 1). We used the cycle-writing scale as previously described and adopted by Derks (Derks, 2022) to describe the objectives and intended results of each cycle (see below). This approach complements the related Lean Start up Method to develop Minimal Viable Products [MVP, (Onken and Campeau, 2016)]. Stakeholders were arts and psychomotor therapists who understood which VR application needed to be developed, and Information Technology (IT) technicians capable of building the VR application. All cycles were held in online groups; individual meetings were held with participants who were unable to participate in the online group meetings. The eligibility criteria for participants were to be an arts and psychomotor therapist or at least passed the first year of studying arts and psychomotor therapists.
Cycle 1: introduction cycle: training participating arts and psychomotor therapists
The aim of the first cycle was to enhance 17 arts and psychomotor therapists’ skills in using VR for online therapy. We also sought to foster awareness about valuable online therapy skills which therapists had not yet acquired. We thus initiated a training program to improve VR proficiency amongst arts and psychomotor therapists. This included practice sessions to explore the barriers and facilitators of using VR for online therapy. The therapists were asked to express the prerequisites of online arts and psychomotor therapy with VR. This information led to developing a patient journey which described the steps which patients would need to take in order to initiate and familiarize themselves when using the VRhExp.
Cycle 2: co-creation cycle with media designers in education
The aim of the second cycle was to build a markedly improved version of the VRhExp. Three Media designers in education and technical VR developers participated in this phase. As aspirant designers, media designers in education critically reflected on the prerequisites of the VRhExp described by the therapists in Cycle 1. In multiple co-creation sessions, the media designers in education collected all viewpoints and presented these to the Technical VR developers.
Cycle 3: co-creation cycles with technical VR developers
The aim of the third cycle was to build a large and solid foundation from which VRhExp could emerge. The technical VR developers took a stepwise approach. Every month, technical VR developers provided an update to the arts and psychomotor therapists and asked for their input. Specifically, the therapists then consulted the initial list of potential new elements as gathered by the media designers in education in cycle 2. The VR developers then updated the VRhExp by adding a new element, one at a time. The therapists then tested each update with the added element. The therapists were encouraged to share their ideas for potential elements which were then added to the initial topic list. Building and testing each update took a month. Several meetings were organized for the therapists to practice together to gain and improve their knowledge and skills in operating the VRhExp.
Cycle 4: extensive iterative pilot testing of functionality
In the fourth cycle, the AR participants conducted several pilots with the prototype VRhExp during therapy sessions with their patients, as well as with colleagues and acquaintances. Two final meetings were organized with the arts and psychomotor therapists to evaluate the VRhExp building process and determine opportunities for the therapists and for therapies. This in turn contributed to an ongoing optimization of the VRhExp build process. Furthermore, 3 workshops were held among arts and psychomotor therapists, (inter)national arts and psychomotor therapy. The workshop participants were introduced to the latest version of VRhExp in a low-threshold manner. Using the feedback of workshop participants, the VRhExp could be further developed, and knowledge was shared.
Cycle 5: testing in practice and dissemination
In the fifth cycle, the dissemination of the VRhExp to arts and psychomotor therapists continued at national and international workshops and presentations at professional network meetings.
Data collection
In the first and fourth cycle, arts and psychomotor therapists who participated in the AR were asked to complete questionnaires about their perceptions, and their experiences of VR. Due to the difficulty of endorsing a negative or negatively formulated statement, all statements were positive (Baarda et al., 2016). These included the following statements:
1) I am positive about providing online arts and psychomotor therapy.
2) I feel sufficiently competent to provide online arts and psychomotor therapy.
3) I have an affinity with digital technology.
4) Doing and experiencing is possible in an online (VR) environment.
5) The treatment techniques I am familiar with can be applied well through online arts and psychomotor therapy.
6) I experience a high workload when I have to offer online arts and psychomotor therapy.
7) I have learned new skills since I started providing online arts and psychomotor therapy.
Two focus groups then took place with the AR participants to collect their viewpoints and experiences concerning opportunities to apply VR for online art therapy. Workshop participants in the fourth cycle were also asked to complete this questionnaire. All responses from the questionnaires are posted on the research team secured drive (at the University of Applied Sciences Arnhem and Nijmegen).
Analysis
Demographic and clinical characteristics of participating arts and psychomotor therapists were summarized with descriptive statistics. The main findings for each cycle were described. Data from the questionnaires were summarized with descriptive statistics, while data from the focus groups were reported qualitatively. Inferential statistical analyses were not conducted as the goal of the action research was not to generalize findings from a finite sample to the population, and the sample size was not determined by an a priori power analysis.
Ethical considerations
This research complies with the criteria of the Declaration of Helsinki on Ethical Principles for Medical Research Involving Human Subjects, applicable national laws (like the General Data Protection Regulation), and the Dutch Code of Conduct for Research Integrity. Participation in this research was fully voluntarily. Participants were provided verbally and written information. They signed an informed consent and had a reflection period. At any time they were free to end their participation.
Results
A total of 17 arts and psychomotor therapists participated in cycles 1-5 of the AR of whom 3 were men and 14 were women, and whose mean age was 44.1 years (SD 11.3). Of them, 8 were psychomotor therapists, 3 were visual art therapists, 2 were dance therapists, 3 were music therapists, and 1 was a drama therapist. Four had less than 5 years of working experience, two had 5–10 years of working experience, while eleven had over 10 years of working experience. Participating art and psychomotor therapists provided care to diverse patient groups ranging from children, adolescents, adults and the elderly. These included patients with depression and anxiety, trauma, personality disorders, psychotic disorders, pervasive developmental disorders, eating disorders, addiction, traumatic brain injury and dementia. At cycle 4, another 34 arts and psychomotor therapists participated in three workshops. Of them 10 were men and 24 were women, and their mean age was 41.7 years (SD 11.1).
Descriptive results based on the cycles
Cycle 1: introduction cycle: training arts and psychomotor therapist participants
Regarding the modes of online healthcare provision, seven of the participating arts and psychomotor therapists noted that they had never used VR for treatment and eight had never used gaming in therapy. Ten of them used e-mail, chat, and/or (video) calling as a mode of online healthcare provision. Telerobot and VR were rarely used. Fourteen of the arts and psychomotor therapists indicated to have some/much capacity in using online tools. The participating arts and psychomotor therapists were introduced to VR by a 3-h training and created skills and a foundation for the next phases. It is important to guide users in developing the digital skills they need to work with VRhExp with sufficient confidence. In all skill development, investing time is crucial. On average, this means 4 h of participation in onboarding sessions for participants, 4 h of self-practice, and 1 to 2 additional hours of individual support from the trainer. Time and support are key factors in this process.
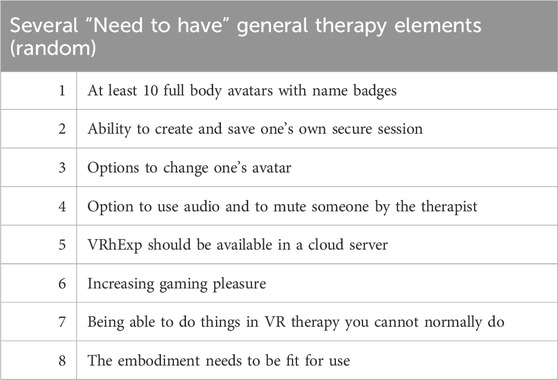
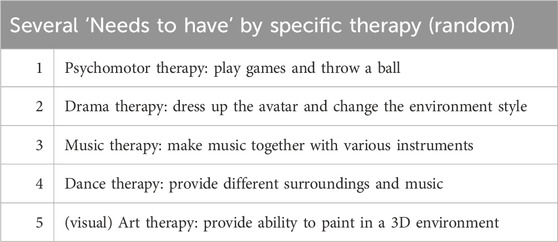
An overview of required elements like visuals and audio was developed. In addition, the therapists created their own list of preferences for each different arts and psychomotor therapy to be developed. Table 1 shows the required elements and Table 2 lists the arts and psychomotor therapy specific elements; the listed items are regarded as indispensable.
This resulted in a patient journey in which each therapeutical step to be taken was clarified. Prior to a therapy session, participants needed a standard explanation of how to use the controllers’ how to make contact, and the ability to see your own avatar with name badges, which took around 10 min at least. In addition, the ‘therapy’ room could not be disturbed by anyone without approved access. Breakout rooms, a slightly vibrating controller when the patient reaches an edge of the VR playing field, and the possibility to immediately clean-up their session was required during the sessions. Of particular value, participants noted that the therapy room should be saved for later use. If working in a group, some form of 3D audio would help participants identify where the sound would be coming from.
Cycle 2: co-creation cycle with media designers in education
Co-creation started in the second phase based on the wish lists and patient journeys created in the first cycle. The collaboration with media designers in education provided several examples which the Technical VR developers were able to use in cycle 3. For example, different atmospheres in terms of space were viewed, asset sets were compared, and participants were interviewed individually about their needs regarding features and VR. The media designers in education developed a patient journey and created a film showing what VRhExp could look like and delivered a full report of their findings to the research team and the technical VR developers.
Cycle 3: co-creation cycle with technical VR developers
The technical VR developers incorporated elements such as synchronous movement of at least 10 of the avatars (people), the ability to play audio everywhere throughout the VR environment and being able to communicate with multiple and different avatars at once. This included interacting with the environment, objects, and fellow players, and the ability to reserve space for future VR expansion of VR. The goal was that the VRhExp should run independently and safely in the online cloud for many users, without involving a technical VR-developer.
Technical VR developers then developed a new interactive VR space as a ‘telepresence tool’ for arts and psychomotor therapists called the VRhExp in this cycle and the fourth and the fifth cycle. In these cycles, they started with the basics in the form of one small space where initially people could only stack blocks. A monthly update was developed with new features such as: adding interactive objects like a ball, a paint sprayer, blocks, musical instruments and soft toys; different spaces; decorating the room such as “laying a floor” and “wallpapering” and a life-size mirror; creating a whole house allowing “inside” and “outside” views; adding a button for changing the avatar and clearing the entire space at once; games; and enabling opportunities to have restricted areas using personal codes.
Cycle 4: extensive iterative pilot testing of functionality
Perceptions and experiences of action research participants
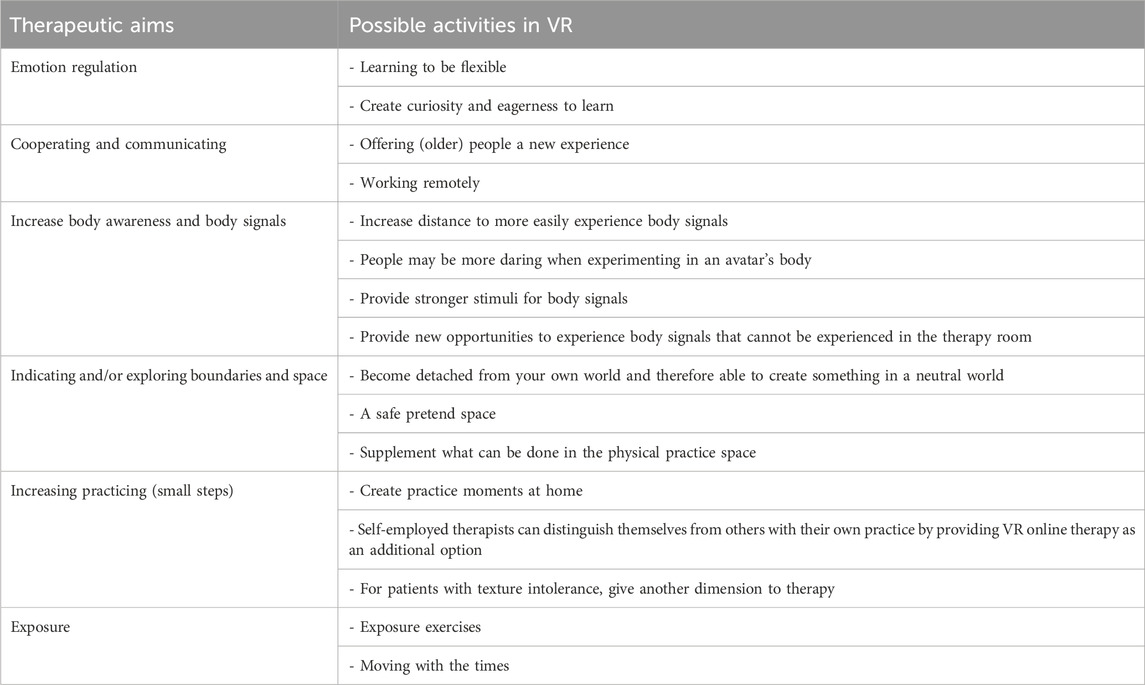
Arts and psychomotor therapists who participated in the Action Research noted a variety of therapeutic goals for online therapy. Referring to psychological and physical function, they identified improving somatosensory perceptions, psychomotor skills, regulation of distress and emotions, fostering creativity, playfulness, joy. Regarding clinical syndrome level, they identified reducing general anxiety and specific anxiety (for example phobia through exposure), psychoeducation and Young´s Schema therapy. For social-cognitive and interpersonal functioning, they identified strengthening self-worth and assertiveness and practicing social, communication, and collaboration skills. In focus groups, arts and psychomotor therapists shared ideas about possible activities for VRhExp related to the therapeutic aims (Table 3). One art therapist did not see therapeutic goals for online therapy.
Learning to use it themselves
Following the 1-year project, AR participants reported becoming more proficient in using VR than at the start. The differences in degree of proficiency may be due to some participants practicing more than others; the various group meetings and practice times were valuable in their becoming more proficient. The research team support was experienced as pleasant by the participants; any individual problems could be resolved quickly. Participants were generally satisfied with the project’s progress, however they expressed regret that the software was not fully operational, for example user satisfaction was low due to the bugs in software, and that more steps had to be taken before VRhExp can actually be used in therapy.
“When I wanted to practice and I did not succeed directly, I stopped” (psychomotor therapist, participant 8).
Own experience
VRhExp invited the participants to play and explore, despite the fact that the options were still fairly limited. One participant indicated that being busy discovering made her less connected to other participants. The addition of name tags was specifically mentioned as a major improvement regarding the degree of contact by one participant. Participants did experiments with VRhExp with people in their private circles and colleagues, and found this to be positive.
“I feel like a kind of child who gets to try everything,” (drama therapist, participant 3).
“The musical opportunities already offer some perspective, when I saw people dancing to the music I thought, I want to join in!” (music therapist, participant 5).
Deploying with patients
Most participants did not use VRhExp with their patients for a variety of reasons. The overarching reason was that VRhExp was not sufficiently stable at the time, and basic elements such as picking up and fluid movement were not sufficiently evolved. A single therapist did introduce a patient to VRhExp, where the patient had been informed that not everything was already working perfectly. Participants experienced that it takes a patient a relatively long time to become proficient in VRhExp, which means that substantive steps cannot yet be taken. Most participants did recognize the potential of the VRhExp, and could foresee transdiagnostic themes like distance proximity, cooperation, resilience, and boundaries. Therapists also saw the potential of VR as an intermediate solution to working in a physical space with their patient. Participants indicated that they could not foresee using VRhExp with patients who could quickly dissociate, hyperventilate, get into crisis, with schizophrenia, or perhaps not with elderly people. Moreover, they indicated that VRhExp could not be immediately used with new patients; they first had to build a relationship.
“Everything still works too woodenly and it's still in its infancy” (dance-movement therapist, participant 9).
“There are definitely treatment goals to be achieved online, you have to be creative for it yourself” (visual art therapist, participant 6).
Reflection on the development process
All participants indicated that the current version of VRhExp was not yet ready for use in clinical practice but appreciated that a great step forward had been made. They mentioned that a priority is to make the base more “smooth,” especially regarding picking up elements. The avatars could also be improved; the avatars in the current version still felt a bit strange. They proposed several ideas such as being able to create an avatar in the VR glasses themselves (thick, thin, big, small, young, old, freckles, no freckles, etc.). This was also indicated earlier in the wish list made by the participants in phase 2.
“I still do not feel as many body sensations as when using the previous version of VR Health Experience” (psychomotor therapist, participant 8)
Looking forward
While using the VRhExp, arts and psychomotor therapists saw that their patients literally got moving, however they experienced difficulties because of the limited space where a person can walk. Participants noted that it was precisely the things that were different from a normal therapy space that created an opportunity for change when adding VR as an additional element. Participants mentioned the value of developing new modules and specific themes in a follow-up version of VRhExp, noting that the motivated group of researchers and practitioners were helpful in this regard. Most participants indicated that they would like to stay involved and contribute to future VRhExp development.
“Not everything has to be realistic,” (music therapist, participant 5).
Perceptions and experiences of workshop participants
Of the arts and psychomotor therapists who participated in the workshops, four out of five acknowledged the potential of acting and experiencing with the VRhExp (79%) and three out of five indicated to have affinity with digital technology (62%). At the same time, fewer of them were ready to provide online therapy with the VRhExp. Half were positive about providing online therapy (47%). One out of four respondents thought that arts and psychomotor interventions known to them could be applied online (24%), while slightly more than one out of ten considered themselves capable to offer online therapy (12%).
Cycle 5: testing in practice and dissemination
Participants tested VRhExp the app together to test the new features, generating new arts and psychomotor therapy exercises, for example the collection and description of arts and psychomotor therapy exercises in VRhExp within the various arts and psychomotor therapy disciplines. Workshop participants also indicated that they would like to be kept up to date on VRhExp progress through a newsletter. To date, 5 newsletters have been sent to 92 people interested in the VRhExp, disseminating knowledge in an attractive format. This format has been enthusiastically received by the participants, leading to them proposing many new ideas on how to expand VRhExp even further. Another form of dissemination was to raise VRhExp awareness by conducting workshops and sharing knowledge in training sessions, introducing more arts and psychomotor therapists to opportunities for using VR in arts and psychomotor therapy.
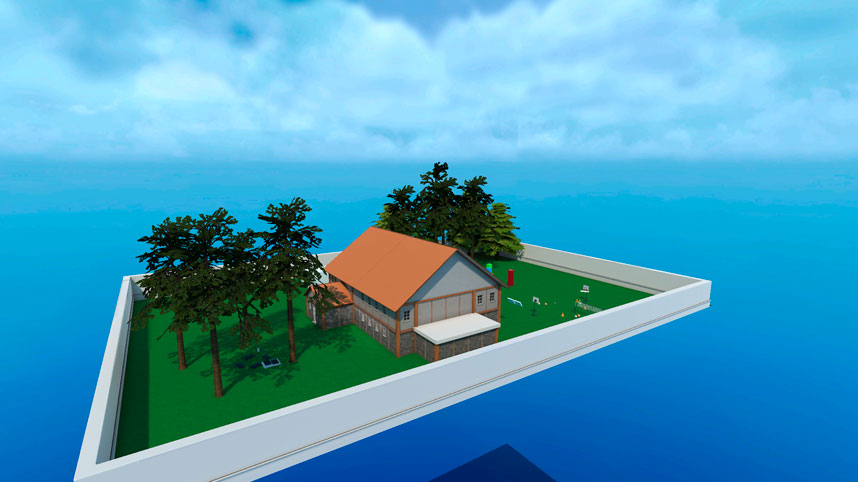
Figures 2, 3 show images of parts of the VRhExp.
Discussion
Principal findings
In this study we redeveloped, rebuilt, and pilot tested the full body multiplayer application: the VR Health Experience (VRhExp), a virtual reality space for online arts and psychomotor therapies. The input from arts and psychomotor therapists and other mental healthcare professionals laid the foundations for the make process for the technical VR developers using an Action Research design. We formulated a roadmap with the prerequisites for implementing VRhExp in clinical practice. The VRhExp provides the opportunity for treatment continuity, especially in cases where being on location with the patient are limited.
Participants reported potential in using VR in arts and psychomotor therapy. However, at the completion of the project, the application was not sufficiently developed to actually use it in arts and psychomotor therapy. However, many suggestions were made by the participants that would allow VRhExp to be further developed in the future. Other arts and psychomotor therapists who heard about the existence of the application were enthusiastic about the possibilities.
Strengths and limitations
This study had a number of strengths. First, the VRhExp offers the possibility for treatment continuity in cases of social distancing, hospitalization, or when either the therapist or patient(s) are at distant locations where normally, therapy would come to a halt. As such the VRhExp contributes to sustainable healthcare. Second, this study fits in with a current trend in healthcare as the use of VR in psychotherapy is increasing. This will benefit the popularity of using VR within arts and psychomotor therapy (Shamri Zeevi, 2021; Gregg and Tarrier, 2007; Hacmun et al., 2018). Third, to our knowledge we are the first to develop an application like this for arts and psychomotor therapists working in the field of mental health. Second, the VRhExp uses a full body multiplayer application in therapy. So far, most VR-applications for therapy offer a pre-structured VR situation in which the patient works individually on personal therapeutic goals, with the therapist outside the VR environment. However, in our VRhExp, the therapist and the patient and/or patient group (up to 9 persons) can meet together online, each as their own avatar, and are able to communicate and interact with each other. This makes the VRhExp inclusive, on an equal level, as well as including the specific attunement essential for delivering person tailored therapy. The VRhExp environment provides this group of therapists with special opportunities for their professional development. A fourth methodological strength pertains to the study design. The cyclical approach of Action Research allowed arts and psychomotor therapists to adapt to the situation, and timely adjustments could be made. Arts and psychomotor therapists with diverse backgrounds, demographics and experience were involved in the VRhExp co-creation during the Action Research process. This diversity contributed to the representativeness of the study and the usability of the VRhExp.
Also a number of potential shortcomings deserve to be mentioned as well. First, this study was a pilot study. While the cycles were extensive, the number of participants in these cycles were limited and inferential statistics were not computed. However, statistical inference was not the principal goal of this study. Second, it took participating arts and psychomotor therapists more time than expected to familiarize themselves with the VRhExp and becoming proficient in its use. However, we have now created a pool of arts and psychomotor therapists proficient in using VR. The same applied to patients who needed time to practice the skills to operate the VR application. The participating arts and psychomotor therapists reported that teaching a patient a new skill was a therapeutic process in itself.
Future directions
We can conclude that next steps are to develop specific content such as working methods related to arts and psychomotor therapies to be used in the VRhExp based on existing therapeutic approaches as well as innovative working methods.
VRhExp provides opportunities for the continuity of treatment by arts and psychomotor therapists. We recommend developing alternatives for the “live on location therapy’ as other pandemics like the COVID-19 pandemic may reoccur, and remote working may be valuable in other situations. Moreover, reducing travel is sustainable in itself, for example less travel costs and time, reduced emissions etcetera, while working in a digital space may also lead to a reduction of workplace accommodation. This study demonstrates that arts and psychomotor therapists can continue to work and offer experiential and interactive therapies, despite social distancing. It must be noted that VRhExp is not a complete substitute for live on location arts and psychomotor therapies, but it provides an innovative adjunct for both therapists and patients.
This project is relevant to the profession in several aspects. As western society becomes increasingly digital, so does mental healthcare, which makes the step of implementing VR in therapy appropriate. Through this innovation, arts and psychomotor therapists can profile themselves with the potential (expansion) opportunities of remote, experiential work. VRhExp is currently still in a starting phase, providing many opportunities for developing (relatively) easily implementable applications.
Many arts and psychomotor therapists in the field have expressed their interest in learning about the VRhExp. Therefore, the training program developed for arts and psychomotor therapists is now available to the field. The large network built up while working on this and the previous projects forms a broad support base for further VRhExp development and implementation. Moreover, a number of arts and psychomotor education programs are interested in adding the VRhExp to their curriculum. For example, the HAN University of Applied Sciences in Nijmegen, the Netherlands, has already integrated VRhExp in part of the curricular program. These developments will result in future arts and psychomotor therapists with skills in using VR for therapy purposes.
The professional field’s willingness to adopt VR applications has led to the development of a VRhExp training program. This so-called ‘telepresence tool’ may also be valuable for other disciplines in the field of mental healthcare. Once VRhExp has been sufficiently developed, then therapeutic goals set by therapists can be more easily achieved as patients can continue with these therapies in their daily lives.
Our main recommendation for future research on the VRhExp is to develop specific working methods and treatment modules directly applicable to arts and psychomotor therapies. In addition, continuing (technical) developments in the field of VR should be a focus of follow-up projects, as rapid innovation will resolve some of the issues addressed in this paper.
Conclusion
Using this VR-tool in arts and psychomotor therapies provides several possibilities that contribute to the further development of eHealth. Arts and psychomotor therapists were positive when using the app and see many possibilities for the future. The developed roadmap with arts and psychomotor therapists” wish list is a valuable step in further developing VRhExp. The VRhExp project contributes to developing the profession of arts and psychomotor therapists, as well as raising the profile of arts and psychomotor therapies. The combination of a full body multiplayer VR-application to be used in (arts and psychomotor) therapy is innovative on a global level. We note the high interest in this project shown by practitioners, those involved in educational programs, as well as from other mental healthcare professions. The participating arts and psychomotor therapists felt that the VRhExp was sufficiently connected to practice and valued their participation in this project. Furthermore, the project addresses the issue of increasing health expenditure in mental healthcare by introducing possible savings. The VRhExp is a promising tool for fostering the continuity of experiential and interactive treatment by arts and psychomotor therapists, tailored for and attuned to patients with psychological problems. This VR space is the first step in the landscape of online experiential arts and psychomotor therapies.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
NJ: Writing–original draft, Writing–review and editing. HW: Data curation, Writing–review and editing. JK: Investigation, Software, Visualization, Writing–review and editing. SH: Conceptualization, Funding acquisition, Methodology, Supervision, Writing–review and editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This project was funded through the KIEM grant (SVB/KIEM. K21.01.007). We kindly acknowledge the following private practices for their time and efforts: Praktijk Lijfzijn, Praktijk Scit, Zin-Ergie, Praktijk Vena, PMT praktijk Apeldoorn and Manon Zandbergen Praktijk voor Psychomotorische Therapie) and GGNet, Mental Healthcare institution. The Special Research Group, the Academy of Health and Vitality, as well as the HAN department of Arts and Psychomotor Therapies invested in this study.
Acknowledgments
We thank the participating arts and psychomotor therapists for their enthusiastic contribution, the technical VR developers from VREE who helped build the application, and the Media designers in education from HAN University of Applied Sciences. We also thank Arjan Doolaar for checking the bibliographical references.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
3-D, three-dimensional; AR, Action Research; IT-specialists, Information Technology specialists; MVP, Minimal Viable Products; VR, Virtual Reality; VRhExp, Virtual Reality Health Experience
References
Baarda, B., Kalmijn, M., and de Goede, M. P. M. (2016). Basisboek enquêteren: handleiding voor het maken van een vragenlijst en het voorbereiden en afnemen van enquêtes, Vierde druk. Groningen: Noordhoff Uitgevers.
Békés, V., and Aafjes-van Doorn, K. (2020). Psychotherapists’ attitudes toward online therapy during the COVID-19 pandemic. J. Psychother. Integr. 30 (2), 238–247. doi:10.1037/int0000214
Betts, D. (2020). Advances in Creative Forces® clinical research and applications of the creative arts therapies for treating PTSD and TBI in military-connected populations. Creat. Forces Natl. Resour. Cent.
Carl, E., Stein, A. T., Levihn-Coon, A., Pogue, J. R., Rothbaum, B., Emmelkamp, P., et al. (2019). Virtual reality exposure therapy for anxiety and related disorders: a meta-analysis of randomized controlled trials. J. Anxiety Disord. 61, 27–36. doi:10.1016/j.janxdis.2018.08.003
Deng, W., Hu, D., Xu, S., Liu, X., Zhao, J., Chen, Q., et al. (2019). The efficacy of virtual reality exposure therapy for PTSD symptoms: a systematic review and meta-analysis. J. Affect. Disord. 257, 698–709. doi:10.1016/j.jad.2019.07.086
Derks, Y. P. M. J. (2022). Alexithymia in borderline personality pathology: from theory to a biosensor application. Enschede, Netherlands: University of Twente. PhD. doi:10.3990/1.9789464217896
Freeman, D., Haselton, P., Freeman, J., Spanlang, B., Kishore, S., Albery, E., et al. (2018). Automated psychological therapy using immersive virtual reality for treatment of fear of heights: a single-blind, parallel-group, randomised controlled trial. Lancet Psychiatry 5 (8), 625–632. doi:10.1016/S2215-0366(18)30226-8
Gregg, L., and Tarrier, N. (2007). Virtual reality in mental health: a review of the literature. Soc. Psychiatry Psychiatr. Epidemiol. 42 (5), 343–354. doi:10.1007/s00127-007-0173-4
Hacmun, I., Regev, D., and Salomon, R. (2021). Artistic creation in virtual reality for art therapy: a qualitative study with expert art therapists. Arts Psychother. 72, 101745. doi:10.1016/j.aip.2020.101745
Hacmun, I., Regev, D., and Salomon, R. (2018). The principles of art therapy in virtual reality. Front. Psychol. 9, 2082. doi:10.3389/fpsyg.2018.02082
Haeyen, S. (2020). Vaktherapie online: Het perspectief van vaktherapeuten: Resultaten van de enquête over online vaktherapie [Arts and psychomotor therapies online: The perspective of arts therapists: Results of the survey on arts and psychomotor therapies online]. Tijdschr. Voor Vaktherapie (4), 18–27.
Haeyen, S., Jans, N., Glas, M., and Kolijn, J. (2021a). VR health experience: a virtual space for arts and psychomotor therapy. Front. Psychol. 12, 704613. doi:10.3389/fpsyg.2021.704613
Haeyen, S., Jans, N., and Heijman, J. (2021b). The use of VR tilt brush in art and psychomotor therapy: an innovative perspective. Arts Psychother. 76, 101855. doi:10.1016/j.aip.2021.101855
Haeyen, S., Kolijn, J., Hoek, P., and van Hooren, S. (2020). Vaktherapie in coronatijd: Uitbraak van innovatie? Over online werken en de inzet van digitale middelen [Arts and psychomotor therapies during COVID: Outbreak of innovation? On working online and using digital resources]. Tijdschr. Voor Vaktherapie (4), 1–10.
Hoppe, A. H., Anken, J. K., Schwarz, T., Stiefelhagen, R., and Van De Camp, F. (2020). “CLEVR: a customizable interactive learning environment for users with low vision in virtual reality,” in The 22nd international ACM SIGACCESS conference on computers and accessibility (Virtual Event Greece: ACM), 1–4. doi:10.1145/3373625.3418009
Krupić, D., Žuro, B., and Corr, P. J. (2021). Anxiety and threat magnification in subjective and physiological responses of fear of heights induced by virtual reality. Personal. Individ. Differ. 169, 109720. doi:10.1016/j.paid.2019.109720
Lewin, K. (1946). Action research and minority problems. J. Soc. Issues 2 (4), 34–46. doi:10.1111/j.1540-4560.1946.tb02295.x
Li, B., and Shen, M. (2022). The psychological recovery of patients in the Context of virtual reality application by a complementary medicine scheme based on visual art. Evid. Based Complement. Altern. Med. 2022, 1–5. doi:10.1155/2022/7358597
Maarsingh, B. M., Bos, J., Van Tuijn, C. F. J., and Renard, S. B. (2019). Changing stress mindset through stressjam: a virtual reality game using biofeedback. Games Health J. 8 (5), 326–331. doi:10.1089/g4h.2018.0145
Marks, K., Marks, S., and Brown, A. (2017). Step into my (virtual) world: an exploration of virtual reality drawing applications for arts therapy. J. Creative Arts Ther. 1 (99), 99–111.
Mozgai, S., Hartholt, A., Leeds, A., and ‘Skip’ Rizzo, A. (2020). “Iterative participatory design for VRET domain transfer: from combat exposure to military sexual trauma,” in Extended abstracts of the 2020 CHI conference on human factors in computing systems (Honolulu HI USA: ACM), 1–8. doi:10.1145/3334480.3375219
Onken, M., and Campeau, D. (2016). Lean startups: using the business model canvas. J. Case Stud. (1), 95–101.
Riva, G. (2005). Virtual reality in psychotherapy: review. Cyberpsychol. Behav. 8 (3), 220–230. doi:10.1089/cpb.2005.8.220
Shamri Zeevi, L. (2021). Making art therapy virtual: integrating virtual reality into art therapy with adolescents. Front. Psychol. 12, 584943. doi:10.3389/fpsyg.2021.584943
van den Berg, J. (2019). VR body Lab. iXperium. Available at: https://www.ixperium.nl/vr-body-lab/.
Keywords: art therapies, psychomotor therapy, full body multiplayer, virtual reality, e-health, music therapy, dance therapy, drama therapy
Citation: Jans N, Wouters H, Kolijn J and Haeyen S (2025) Developing a virtual reality application for online arts and psychomotor therapies using action research. Front. Virtual Real. 6:1462775. doi: 10.3389/frvir.2025.1462775
Received: 10 July 2024; Accepted: 06 January 2025;
Published: 22 January 2025.
Edited by:
Anna Kobusinska, Poznań University of Technology, PolandReviewed by:
Stefan Marks, Auckland University of Technology, New ZealandXiangrong Jiang, Xihua University, China
Copyright © 2025 Jans, Wouters, Kolijn and Haeyen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nathalie Jans, bGVjdG9yYWF0LnZ0Z3pAaGFuLm5s
 Nathalie Jans
Nathalie Jans Hans Wouters1
Hans Wouters1 Joep Kolijn
Joep Kolijn Suzanne Haeyen
Suzanne Haeyen