- 1Mass General Brigham, Somerville, MA, United States
- 2Department of Statistics, Harvard University, Cambridge, MA, United States
- 3Erasmus Medical Center, Rotterdam, Netherlands
Trauma and orthopedic surgery commonly rely on intraoperative radiography or fluoroscopy, which are essential for visualizing patient anatomy and safely completing surgical procedures. However, these imaging methods generate ionizing radiation, which in high doses carries a potential health risk to patients and operating personnel. There is an established need for formal training in obtaining precise intraoperative imaging while minimizing radiation exposure. Virtual reality (VR) simulation serves as a promising tool for orthopaedic trainees to develop skills in safe intraoperative imaging, without posing harm to patients, operating room staff, or themselves. This paper aims to provide a brief overview of literature surrounding VR training for intraoperative imaging in orthopaedic surgery. In addition, we discuss areas for improvement and future directions for development in the field.
Introduction
Trauma and orthopedic surgery commonly rely on intraoperative radiography or fluoroscopy. Orthopaedic surgeons and other members of the surgical team face the risk of exposure to ionizing radiation during intraoperative radiography or fluoroscopy (Mehlman and DiPasquale, 1997; Matityahu et al., 2017; Rashid et al., 2018; Hurley et al., 2022; Dorman et al., 2023). Patients and personnel assisting in, or performing fluoroscopically guided procedures may be exposed to high doses of radiation, with the highest dosage affecting the hands and wrist (Hafez et al., 2005; Singer, 2005). This exposure carries potential health risks, including cancer and cardiovascular disease (Chou et al., 2022; Gogos et al., 2022; Ko et al., 2018; Lai et al., 2020; Little et al., 2023). In particular, orthopaedic procedures involve the most frequent use of intraoperative fluoroscopy compared to other surgical fields (Lee et al., 2015; Visci et al., 2022).
The need for precise intraoperative imaging in orthopaedic surgery is unquestionable. However, the associated health risks are also a cause for concern. When using fluoroscopy, it is crucial for surgeons and technicians to utilize the C-arm in an efficient and effective manner to obtain the necessary anatomical information while minimizing radiation exposure (Kaplan et al., 2016). Literature has shown that angle of the imaging device influences in the amount of radiation, and that surgical experience decreases the amount of radiation (Magee et al., 2021; Yamashita et al., 2023).
To address these concerns, it is essential to assess the training and education provided to orthopaedic surgeons, both during residency and in practice. Despite the critical role of intraoperative fluoroscopy in assessing fracture reduction and implant positioning, there is a significant gap in formal education surrounding intraoperative imaging, for both residents and practicing orthopaedic surgeons (Ames et al., 2020). Orthopaedic and trauma surgeons at all levels acknowledge the need for training in obtaining optimal high-quality intraoperative images (Vetter et al., 2021).
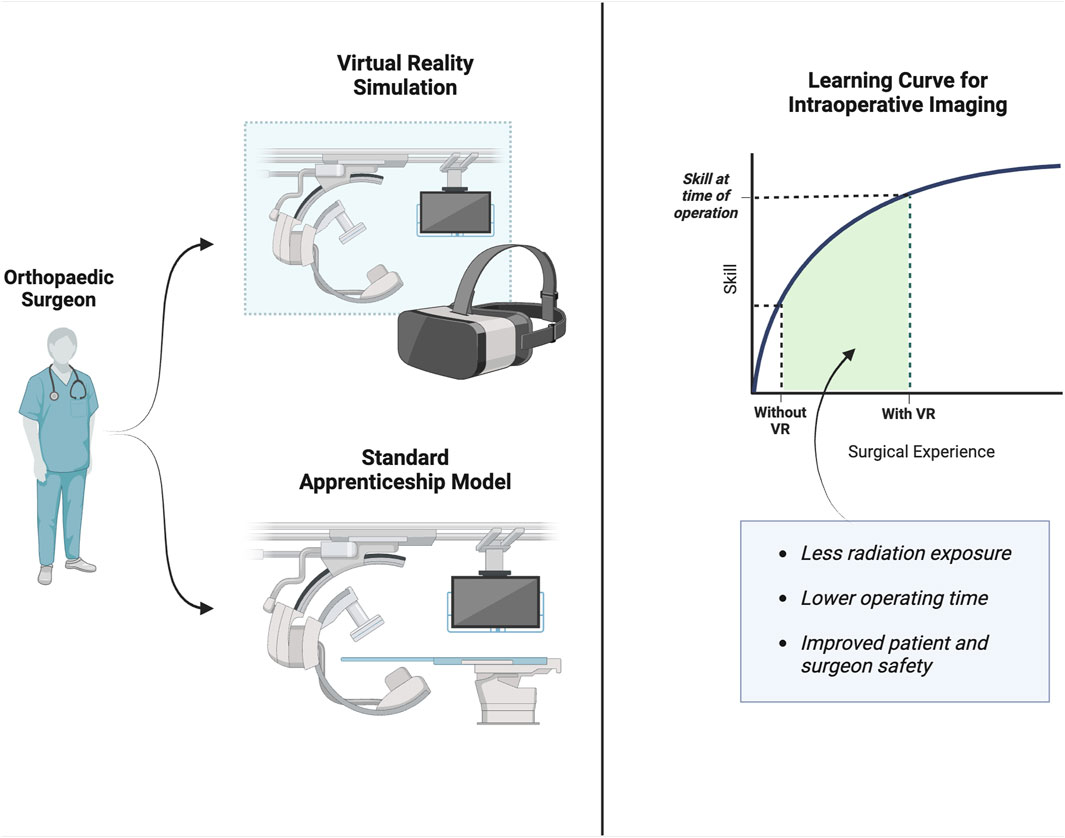
The predominant training structure in surgical specialties, including orthopaedic surgery, is apprenticeship. However, orthopaedic procedures increasingly require intense technical skills which have a steep learning curve (Lee et al., 2013; Hoppe et al., 2014). This calls for a training structure that allows trainees to develop skills without posing harm to trainees or patients. One way to improve proficiency in the use of fluoroscopy during orthopaedic procedures may be through the use of virtual reality simulation.
Virtual reality (VR) is increasingly used for surgical skills learning and training (Izard et al., 2018; Khan et al., 2019; Bielsa, 2021; Hasan et al., 2021). In recent years, a large body of work has been published describing the implementation and efficacy of VR training systems across a range of surgical specialties. The use of VR has improved the efficiency and quality of performance in laparoscopic surgical practice in comparison to traditional training (Guedes et al., 2019; Portelli et al., 2020). VR applications can be executed repeatedly, are cost-effective, are able to provide objective feedback, and create a safe-environment to make mistakes (Bielsa, 2021). VR may be an ideal technique to teach intraoperative imaging skills to orthopaedic trainees (Figure 1). This paper aims to provide an overview of virtual reality training for intraoperative imaging in orthopaedic surgery, addressing the current progress, evidence, and future directions for development.
Methods
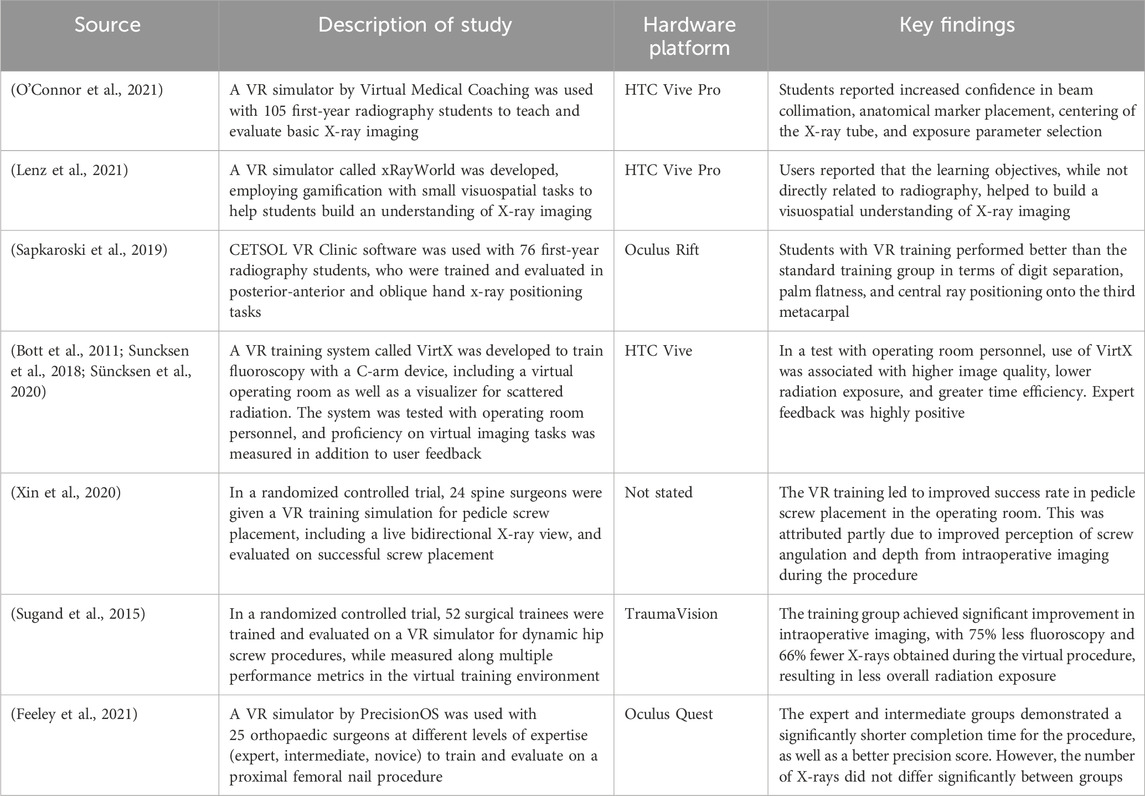
We conducted a PubMed literature search to identify publications related to orthopaedic imaging and virtual reality, using the following search terms: (virtual reality OR VR) AND (orthopaedic* OR orthopedic*) AND (surgery) AND (train*). We identified 309 papers, of which 41 papers were relevant to our broader review topic. Of these, 17 papers involved intraoperative imaging as a discussion point or outcome, leading us to select 10 primary research studies (randomized controlled trials, methods papers), and 7 reviews (systematic reviews, meta-analyses) for discussion. Selected findings are outlined in Table 1 and discussed below.
Using VR training for intraoperative imaging
There is a sparsity of literature evaluating VR training for intraoperative imaging. To understand the utility of VR for training intraoperative imaging, we also evaluated the progress of VR training systems in adjacent imaging tasks as well.
In a study involving first-year radiology students (O’Connor et al., 2021), an immersive 3D virtual radiography simulation tool was integrated into the curriculum, which guided students to X-ray virtual patients in a VR suite with instant feedback. Within a learning period of only 60 min, students reported increased confidence in radiography skills, including beam collimation, marker placement, centering the X-ray tube, and exposure parameter selection.
In a similar vein, xRayWorld (Lenz et al., 2021) is a VR simulator that employs gamification with small visuospatial tasks to help students build an understanding of X-ray imaging. User responses indicated that the learning objectives may not have been directly useful for learning radiography, but rather to build a basic visuospatial understanding of X-ray imaging.
A radiography VR simulator by CETSOL VR was built and evaluated for training patient positioning for hand X-ray capture (Sapkaroski et al., 2019). The study showed that students trained on the VR platform performed significantly better in the quality of captured hand radiographs (digit separation, palm flatness, and central ray positioning), compared to students who underwent standard real-world clinical training for the same task. This shows promise for the pedagogical potential of VR in patient positioning if it can be extended to intraoperative imaging as well.
Similar principles can be applied to fluoroscopy: virtX is a VR training system for fluoroscopy with a C-arm device (Bott et al., 2011; Suncksen et al., 2018). This system employs gamification and realistic simulation of intraoperative image capture. It received excellent feedback in a pilot test with experts who were tasked to take radiographs of different body parts. Experts agreed on the merits of the approach for clinical education, but complained of issues with the virtual C-arm handling, the angle precision, and the quality of the virtual radiograph (Suncksen et al., 2018).
The virtX system was also repurposed to build a system that visualized scattered radiation during intraoperative imaging (Süncksen et al., 2020), with the purpose of educating surgeons and operating room personnel on the safe usage of the C-arm imaging device, in a way that minimizes scattered radiation exposure. Similar to the previous study, experts who used the system agreed on the merits of the tool to help trainees understand intraoperative radiation exposure, but they had issues with interaction and visualization which limited the utility of the system.
The strongest evidence for VR training, specifically for intraoperative imaging, comes from clinical trials evaluating specific VR programs and their outcome on surgeon performance. In a randomized controlled trial, spine surgeon trainees were given a VR training simulation for pedicle screw placement and evaluated on successful screw placement (Xin et al., 2020). The program improved the success rate of the procedure compared to basic video training; furthermore, the researchers interpreted that the presence of a simulated spinal X-ray view improved the trainees’ perception of screw angle and depth during the procedure, leading to the improved outcomes.
Another randomized controlled trial evaluated a VR simulator for dynamic hip screw procedures, measuring surgical trainees along multiple performance metrics in the training environment (Sugand et al., 2015). Compared to a control group with only one attempt, a training group achieved drastic improvements in intraoperative imaging, with 75% less fluoroscopy and 66% fewer X-rays obtained during the procedure. As the researchers note, this corresponds to a much lower risk of patient exposure to ionizing radiation. It also corresponds to increased efficiency in assessing proper screw fixation.
A debated topic is the level of clinical realism that is necessary within VR simulations, specifically with respect to intraoperative imaging. A common attribute of such simulations is the presence of assistive prompts: these prompts may aid a trainee in completing a procedure and can also serve as a useful outcome measure. For example, a study evaluating the efficacy of a VR simulation for total hip replacement (Logishetty et al., 2020) found that VR training led to a 70% reduction in assistive prompts from the orthopaedic residents being evaluated. However, this feature is not available in a real operating room, and even within a simulation, it may nullify the use of intraoperative imaging as a feedback method.
The issue of assistive prompts is most evident in a study assessing a VR simulation for a proximal femoral nail procedure, tested on orthopaedic surgeons at different levels of expertise (Feeley et al., 2021). The number of intraoperative X-rays was measured in all cohorts, but ultimately—as admitted by the researchers—it was not a useful metric in determining expertise, due to all groups being given a feature for assistive prompts that gave direct feedback at any time in the simulation. In addition, there was no option for continuous live fluoroscopy, which is a common clinical practice for such procedures, which may have affected the number of single X-rays taken during the procedure: the researchers note that this should be heavily considered in future developments of the technology.
Discussion and future developments
While the existing literature demonstrates the potential of VR training in radiography and intraoperative imaging, there are several limitations and areas for future development.
Firstly, the available studies primarily focus on preoperative and radiography training, with relatively less work surrounding VR training for intraoperative imaging in orthopaedic surgery. There are reported deficiencies in the quality of the VR simulations examined, including the simulated radiographs, as well as the means by which the surgical trainee interacts with the virtual patient and environment (Suncksen et al., 2018). For example, the link between patient positioning and image quality appears to be poorly executed in the current VR simulators available for intraoperative fluoroscopy. Patient positioning is a crucial skill for intraoperative fluoroscopy, and orthopaedic trainees could benefit greatly from learning to acquire quality C-arm images in a precise and efficient manner that minimizes radiation exposure. This may be resolved by VR simulations that track user input more precisely using more sophisticated equipment, allowing for trainees to better learn the visuospatial intuition underlying patient positioning.
With regards to improving user input, a key point of improvement in VR simulations is haptic feedback. Surgical procedures may require precise forces to be applied by the surgeon, with limited visual feedback. An example is total hip replacement, in which milling of the hip acetabulum must be done precisely with limited visualization: a VR simulation was created and validated for the acetabulum milling step of this procedure, including both haptic feedback and simulated X-ray imaging (Kaluschke et al., 2018; Pelliccia et al., 2020). Other works have explored haptic feedback in VR simulations for endoscopic surgery (Tavakoli et al., 2006) and dental training (Al-Saud, 2020). An important consideration for future work is to integrate haptic feedback and visual feedback in the form of intraoperative imaging. By training a surgeon to operate using multiple forms of feedback, VR simulations have the potential to become more effective and realistic for complex surgical procedures.
Expert feedback from the C-arm simulation studies (Suncksen et al., 2018; Süncksen et al., 2020) has highlighted issues related to the quality of virtual radiographs obtained from the imaging. The current approach for the examined VR radiography simulators is based on generation of synthetic radiographs from a perspective projection of a 3D volume (Nilsson et al., 2004). This can lead to a disparity in the quality and appearance of the simulated image, compared to the true appearance of intraoperative images. In addition, this is only useful if there is a 3D volume obtained from the patient; in many surgical cases, it is difficult to obtain accurate volumes due to CT artifacts, and in turn, this hinders the performance of VR simulators that depend on perspective projection. Future developments could aim to enhance the realism of virtual imaging using computational methods, making it more faithful to real-world scenarios.
Finally, multiple studies acknowledged that the patient and surgery scenarios were highly limited. For VR training to be integrated into orthopaedic training programs, it is essential that it is paired with a curriculum that exposes students to a variety of patients and surgeries. In the current literature, all imaging challenges are performed as stand-alone tasks, on a homogenous set of patient models. It would be extremely beneficial for the trainees if the imaging were assessed on a diverse set of patients and presentations, alongside other surgical skills in real-time. This would suggest the development of a VR platform that can support multiple surgical tasks and intraoperative imaging, and function with multiple cases and patient models. This versatility would be a large step towards integrating VR into orthopaedic education.
Conclusion
This paper highlights the promising role of VR training in addressing the challenges of intraoperative imaging for orthopaedic surgeons. In our literature review, we survey the effectiveness of VR training for radiography skills, patient positioning, and intraoperative fluoroscopy. We propose that future developments ought to prioritize the quality of the virtual environment and the way that trainees interact with the simulations. In addition, integrating VR into orthopaedic training programs would be supported by a curriculum exposing trainees to diverse clinical scenarios.
Author contributions
JP: Writing–original draft, Writing–review and editing, Conceptualization, Investigation, Methodology. CL: Conceptualization, Investigation, Methodology, Writing–original draft, Writing–review and editing. NC: Conceptualization, Funding acquisition, Resources, Supervision, Writing–review and editing. AB: Conceptualization, Funding acquisition, Resources, Supervision, Writing–review and editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Al-Saud, L. M. (2020). The utility of haptic simulation in early restorative dental training: a scoping review. J. Dent. Educ. 85 (5), 704–721. doi:10.1002/jdd.12518
Ames, S. E., Ponce, B. A., Marsh, J. L., and Hamstra, S. J. (2020). Orthopaedic surgery residency milestones: initial formulation and future directions. J. Am. Acad. Orthop. Surg. 28 (1), E1–E8. doi:10.5435/jaaos-d-18-00786
Bielsa, V. F. (2021). Virtual reality simulation in plastic surgery training. Literature review. J. Plast. Reconstr. Aesthet. Surg. 74 (9), 2372–2378. doi:10.1016/j.bjps.2021.03.066
Bott, O. J., Dresing, K., Wagner, M., Raab, B.-W., and Teistler, M. (2011). Informatics in radiology: use of a C-arm fluoroscopy simulator to support training in intraoperative radiography. RadioGraphics 31 (3), E65–E75. doi:10.1148/rg.313105125
Chou, L. B., Johnson, B., Shapiro, L. M., Pun, S., Cannada, L. K., Chen, A. F., et al. (2022). Increased prevalence of breast and all-cause cancer in female orthopaedic surgeons. J. Am. Acad. Orthop. Surg. Glob. Res. Rev. 6 (5), e22.00031. doi:10.5435/jaaosglobal-d-22-00031
Dorman, T., Drever, B., Plumridge, S., Gregory, K., Cooper, M., Roderick, A., et al. (2023). Radiation dose to staff from medical X-ray scatter in the orthopaedic theatre. Eur. J. Orthop. Surg. Traumatol. 33 (7), 3059–3065. doi:10.1007/s00590-023-03538-6
Feeley, A., Feeley, I., Merghani, K., and Sheehan, E. (2021). A pilot study to evaluate the face and construct validity of an orthopaedic virtual reality simulator. Injury 52 (7), 1715–1720. doi:10.1016/j.injury.2021.04.045
Gogos, S., Touzell, A., and Lerner, L. B. (2022). What we know about intra-operative radiation exposure and hazards to operating theatre staff: a systematic review. ANZ J. Surg. 92, 51–56. doi:10.1111/ans.17160
Guedes, H. G., Câmara Costa Ferreira, Z. M., Ribeiro de Sousa Leão, L., Souza Montero, E. F., Otoch, J. P., and Luiz de Almeida Artifon, E. (2019). Virtual reality simulator versus box-trainer to teach minimally invasive procedures: a meta-analysis. Int. J. Surg. 61, 60–68. doi:10.1016/j.ijsu.2018.12.001
Hafez, M. A., Smith, R. M., Matthews, S. J., Kalap, G., and Sherman, K. P. (2005). Radiation exposure to the hands of orthopaedic surgeons: are we underestimating the risk? Arch. Orthop. Trauma Surg. 125 (5), 330–335. doi:10.1007/s00402-005-0807-5
Hasan, L. K., Haratian, A., Kim, M., Bolia, I. K., Weber, A. E., and Petrigliano, F. A. (2021). Virtual reality in orthopedic surgery training. Adv. Med. Educ. Pract. 12, 1295–1301. doi:10.2147/amep.s321885
Hoppe, D. J., de Sa, D., Simunovic, N., Bhandari, M., Safran, M. R., Larson, C. M., et al. (2014). The learning curve for hip arthroscopy: a systematic review. Arthroscopy 30 (3), 389–397. doi:10.1016/j.arthro.2013.11.012
Hurley, R. J., McCabe, F. J., Turley, L., Maguire, D., Lucey, J., and Hurson, C. J. (2022). Whole-body radiation exposure in Trauma and Orthopaedic surgery. Bone Jt. open 3 (11), 907–912. doi:10.1302/2633-1462.311.bjo-2022-0062.r1
Izard, S. G., Juanes, J. A., García Peñalvo, F. J., Estella, J. M. G., Ledesma, M. J. S., and Ruisoto, P. (2018). Virtual reality as an educational and training tool for medicine. J. Med. Syst. 42 (3), 50. doi:10.1007/s10916-018-0900-2
Kaluschke, M., Weller, R., Zachmann, G., Pelliccia, L., Lorenz, M., Klimant, P., et al. (2018). “A virtual hip replacement surgery simulator with realistic haptic feedback,” in 2018 IEEE Conference on Virtual Reality and 3D User Interfaces (VR). 2018 IEEE Conference on Virtual Reality and 3D User Interfaces (VR) (IEEE).
Kaplan, D. J., Patel, J. N., Liporace, F. A., and Yoon, R. S. (2016). Intraoperative radiation safety in orthopaedics: a review of the ALARA (As low as reasonably achievable) principle. Patient Saf. Surg. 10 (1), 27. doi:10.1186/s13037-016-0115-8
Khan, R., Plahouras, J., Johnston, B. C., Scaffidi, M. A., Grover, S. C., and Walsh, C. M. (2019). Virtual reality simulation training in endoscopy: a Cochrane review and meta-analysis. Endoscopy 51 (7), 653–664. doi:10.1055/a-0894-4400
Ko, S., Kang, S., Ha, M., Kim, J., Jun, J. K., Kong, K. A., et al. (2018). Health effects from occupational radiation exposure among fluoroscopy-guided interventional medical workers: a systematic review. J. Vasc. Interv. Radiol. 29, 353–366. doi:10.1016/j.jvir.2017.10.008
Lai, C. H., Finlay, A., Cannada, L. K., Chen, A. F., and Chou, L. B. (2020). Radiation exposure and case characteristics in national sample of female orthopaedic trauma and arthroplasty surgeons. Iowa Orthop. J. 40 (1), 5–11.
Lee, Y.-K., Ha, Y.-C., Hwang, D.-S., and Koo, K.-H. (2013). Learning curve of basic hip arthroscopy technique: CUSUM analysis. Knee Surg. Sports Traumatol. Arthrosc. 21 (8), 1940–1944. doi:10.1007/s00167-012-2241-x
Lee, Y. S., Lee, H. K., Cho, J. H., and Kim, H. G. (2015). Analysis of radiation risk to patients from intra-operative use of the mobile X-ray system (C-arm). J. Res. Med. Sci. 20 (1), 7–12.
Lenz, F., Fock, M., Kramer, T., Petersen, Y., and Teistler, M. (2021). “A virtual reality game to support visuospatial understanding of medical X-ray imaging,” in 2021 IEEE 9th International Conference on Serious Games and Applications for Health(SeGAH), 1–6.
Little, M. P., Azizova, T. V., Richardson, D. B., Tapio, S., Bernier, M. O., Kreuzer, M., et al. (2023). Ionising radiation and cardiovascular disease: systematic review and meta-analysis. BMJ 380, e072924. doi:10.1136/bmj-2022-072924
Logishetty, K., Gofton, W. T., Rudran, B., Beaulé, P. E., and Cobb, J. P. (2020). Fully immersive virtual reality for total hip arthroplasty. J. Bone Jt. Surg. 102 (6), e27. doi:10.2106/jbjs.19.00629
Magee, L. C., Karkenny, A. J., Nguyen, J. C., Fazal, F. Z., Talwar, D., Zhu, X., et al. (2021). Does surgical experience decrease radiation exposure in the operating room? J. Pediatr. Orthop. 41 (6), 389–394. doi:10.1097/bpo.0000000000001825
Matityahu, A., Duffy, R. K., Goldhahn, S., Joeris, A., Richter, P. H., and Gebhard, F. (2017). The Great Unknown-A systematic literature review about risk associated with intraoperative imaging during orthopaedic surgeries. Injury 48 (8), 1727–1734. doi:10.1016/j.injury.2017.04.041
Mehlman, C. T., and DiPasquale, T. G. (1997). Radiation exposure to the orthopaedic surgical team during fluoroscopy: “how far away is far enough?”. J. Orthop. Trauma 11 (6), 392–398. doi:10.1097/00005131-199708000-00002
Nilsson, T., Ahlqvist, J., Johansson, M., and Isberg, A. (2004). Virtual reality for simulation of radiographic projections: validation of projection geometry. Dentomaxillofacial Radiol. 33 (1), 44–50. doi:10.1259/dmfr/22722586
O’Connor, M., Stowe, J., Potocnik, J., Giannotti, N., Murphy, S., and Rainford, L. (2021). 3D virtual reality simulation in radiography education: the students’ experience. Radiography 27 (1), 208–214. doi:10.1016/j.radi.2020.07.017
Pelliccia, L., Lorenz, M., Heyde, C.-E., Kaluschke, M., Klimant, P., Knopp, S., et al. (2020). A cadaver-based biomechanical model of acetabulum reaming for surgical virtual reality training simulators. Sci. Rep. 10 (1), 14545. doi:10.1038/s41598-020-71499-5
Portelli, M., Bianco, S. F., Bezzina, T., and Abela, J. E. (2020). Virtual reality training compared with apprenticeship training in laparoscopic surgery: a meta-analysis. Ann. R. Coll. Surg. Engl. 102 (9), 672–684. doi:10.1308/rcsann.2020.0178
Rashid, M. S., Aziz, S., Haydar, S., Fleming, S. S., and Datta, A. (2018). Intra-operative fluoroscopic radiation exposure in orthopaedic trauma theatre. Eur. J. Orthop. Surg. Traumatol. 28 (1), 9–14. doi:10.1007/s00590-017-2020-y
Sapkaroski, D., Baird, M., Mundy, M., and Dimmock, M. R. (2019). Quantification of student radiographic patient positioning using an immersive virtual reality simulation. Simul. Healthc. 14 (4), 258–263. doi:10.1097/SIH.0000000000000380
Singer, G. (2005). Radiation exposure to the hands from mini C-arm fluoroscopy. J. Hand Surg. Am. 30 (4), 795–797. doi:10.1016/j.jhsa.2005.01.007
Sugand, K., Akhtar, K., Khatri, C., Cobb, J., and Gupte, C. (2015). Training effect of a virtual reality haptics-enabled dynamic hip screw simulator. Acta Orthop. 86 (6), 695–701. doi:10.3109/17453674.2015.1071111
Suncksen, M., Bendig, H., Teistler, M., Wagner, M., Bott, O. J., and Dresing, K. (2018). “Gamification and virtual reality for teaching mobile x-ray imaging,” in 2018 IEEE 6th International Conference on Serious Games and Applications for Health (SeGAH), 1–7.
Süncksen, M., Bott, O. J., Dresing, K., and Teistler, M. (2020). Simulation of scattered radiation during intraoperative imaging in a virtual reality learning environment. Int. J. Comput. Assisted Radiology Surg. 15 (4), 691–702. doi:10.1007/s11548-020-02126-x
Tavakoli, M., Patel, R. V., and Moallem, M. (2006). A haptic interface for computer-integrated endoscopic surgery and training. Virtual Real. 9, 160–176. doi:10.1007/s10055-005-0017-z
Vetter, S. Y., Kraus, M., Rikli, D., Pesantez Hoyos, R., Grützner, P. A., Cunningham, M., et al. (2021). Design, delivery, and evaluation of seminars and hands-on courses worldwide on intraoperative imaging in orthopedic trauma. Injury 52 (11), 3264–3270. doi:10.1016/j.injury.2021.06.031
Visci, G., Rizzello, E., Zunarelli, C., Violante, F. S., and Boffetta, P. (2022). Relationship between exposure to ionizing radiation and mesothelioma risk: a systematic review of the scientific literature and meta-analysis. Cancer Med. 11 (3), 778–789. doi:10.1002/cam4.4436
Xin, B., Huang, X., Wan, W., Lv, K., Hu, Y., Wang, J., et al. (2020). The efficacy of immersive virtual reality surgical simulator training for pedicle screw placement: a randomized double-blind controlled trial. Int. Orthop. 44 (5), 927–934. doi:10.1007/s00264-020-04488-y
Keywords: virtual reality, orthopaedic surgery, intraoperative image acquisition, computed tomography, simulation, computers, X-ray image
Citation: Pratap J, Laane C, Chen N and Bhashyam A (2024) Virtual reality training for intraoperative imaging in orthopaedic surgery: an overview of current progress and future direction. Front. Virtual Real. 5:1392825. doi: 10.3389/frvir.2024.1392825
Received: 28 February 2024; Accepted: 15 April 2024;
Published: 16 May 2024.
Edited by:
Danny Goel, University of British Columbia, CanadaReviewed by:
Philipp Klimant, Hochschule Mittweida, GermanyCopyright © 2024 Pratap, Laane, Chen and Bhashyam. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Abhiram Bhashyam, abhashyam@mgb.org
 Jayanth Pratap
Jayanth Pratap Charlotte Laane1,3
Charlotte Laane1,3