
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Virtual Real., 31 January 2024
Sec. Virtual Reality in Medicine
Volume 4 - 2023 | https://doi.org/10.3389/frvir.2023.1304155
This article is part of the Research TopicMixed Reality in Palliative careView all 5 articles
Introduction: As the global population continues to age, the demand for palliative care is progressively increasing. This growing trend highlights the pressing need for groundbreaking interventions that can effectively manage palliative symptoms and improve the quality of end-of-life care. We present a brief, structured, personalized, and innovative psychological intervention named Flourishing-Life-Of-Wish Virtual Reality Therapy (FLOW-VRT)®, which capitalizes on the distinctiveness of virtual reality (VR) as an advanced technology for symptom management. FLOW-VRT is theoretically based on self-determination theory, stress coping theory, flow theory, and attention restoration theory. With a special focus on relaxation, “FLOW-VRT-Relaxation” is designed to enhance end-of-life coping through personalized VR relaxation. As most studies on the use of VR in palliative care have been feasibility or pilot studies with small sample sizes, there is a need for a randomized controlled trial with sufficient statistical power.
Methods: The current study used a randomized controlled trial (n = 128) to test the efficacy of FLOW-VRT-Relaxation by comparing it to traditional relaxation practice in palliative care.
Results: Our results showed that following a FLOW-VRT-Relaxation session, the symptoms of distress that patients in palliative care have to endure significantly reduced, whether physical or emotional in nature.
Discussions: The current findings provide promising results regarding the therapeutic potential of using FLOW-VRT-Relaxation as a cost-effective, scalable, and personalized VR relaxation for patients in palliative care.
Palliative care is considered a basic human right for all patients with chronic and life-threatening illnesses (Ezer et al., 2018). This applies particularly to patients with cancer (Heins et al., 2018)- a leading cause of mortality resulting in 10 million deaths in 2020 (World Health Organization, 2020). The objective of palliative care is to manage symptoms and improve the quality of life of patients in the physical, psychological, spiritual, and psychosocial domains (Khater et al., 2021). Despite the provision of palliative care, several unmet needs remain for patients with advanced illnesses (World Health Organization, 2020). A systematic review finds that psychological, physical, and healthcare information and services are the three most commonly reported domains of unmet needs among Chinese patients with advanced cancer (Wu et al., 2022). Another systematic review (Wang et al., 2018) specifically identifies the unmet care needs of patients with terminal cancer. These needs include the appropriate management of physical pain as an example of an unmet physical need, and perceived reduction in autonomy as an example of unmet psychological need, often expressed as “not being able to do the things I used to do,” “I can do less than before,” and “experiencing loss of control over my life.” Additionally, unmet social needs for companionship include lack of “family and friends’ support”, not “having one member of hospital staff with whom I can talk to,” and “support in coping.” These unmet needs have been documented to have a detrimental effect on the progression of illnesses and consequently the quality-of-life of patients with terminal diseases (Spitzer et al., 1995; Katon, 2003; Cohen, 2004; Fink et al., 2004).
Evidence-based medical treatment and non-pharmacological interventions have both been used to manage symptoms in palliative care. Without the side effects of medical treatment, psychological interventions are widely delivered. Relaxation plays a central role in cognitive-behavioral therapy and has been found to be an effective tool for psychological interventions (Barlow et al., 1989; Norton and Price, 2007; Tsitsi et al., 2017). They are cost-effective, practical, and free of side effects (McCallie et al., 2006; Lin et al., 2011). Numerous studies have confirmed the effectiveness of relaxation techniques for managing cancer-related symptoms (Simeit et al., 2004; de Carvalho et al., 2007; Kwekkeboom et al., 2008; Matsuda et al., 2014; Stoerkel et al., 2018; Berkman and Akan, 2019; Dikmen and Terzioglu, 2019). Diaphragmatic breathing is an example of such a technique. It refers to a breathing technique that involves the contraction and relaxation of the diaphragm muscle. Unlike shallow chest breathing, diaphragmatic breathing intentionally expands the abdomen for deeper inhalation and exhalation, resulting in physiological and psychological benefits. It can relax the autonomic nervous system by enhancing parasympathetic activity (Lazarus and Mayne, 1990). It is found to improve attention, reduce negative affect, and alleviate stress responses (Ma et al., 2017).
Despite the abundance of evidence indicating the effectiveness of relaxation for symptom management, most studies concentrate solely on traditional techniques. Only a few studies have integrated advanced technologies, such as virtual reality (VR), with traditional relaxation methods (Chirico et al., 2016). VR is a cutting-edge technology that has the potential to make up for the shortcomings of traditional approaches in palliative care settings. It creates an immersive experience that can generate a sense of presence in a virtual environment (Malloy and Miling, 2010; Cummings and Bailenson, 2016; Berkman and Akan, 2019). It has become increasingly popular in complementary medicine because its unique characteristics can overcome certain limitations of traditional therapy (Stetz et al., 2011; Morina et al., 2015). First, VR offers an immersive environment that blocks patients from seeing their physical surroundings while instead inducing a sense of presence (“being there”) in a controlled, virtual environment (Slater, 2009). One of the most important cognitive-behavioral techniques for reducing pain is distraction, as suggested by gate control theory (Melzack and Wall, 1965). The sense of presence within the virtual environment can provide a high level of distraction from reality, which is likely one of the reasons why VR has been shown to be effective in reducing pain (Hoffman et al., 2006). Various studies have provided further evidence that consistently reported on patients’ feelings of being distanced from their current suffering during VR experiences (Schneider et al., 2004; Baños et al., 2013; Lloyd and Haraldsdottir, 2019; Niki et al., 2019; Weingarten et al., 2019; Ferguson et al., 2020; Johnson et al., 2020; Brungardt et al., 2021). Given its therapeutic potential in pain and mood management, VR has been further considered a potential substitute for analgesia (Bani Mohammad and Ahmad, 2019; Wittkopf et al., 2020). Second, VR allows a customized selection of virtual environments that can be tailored to meet the individual needs of patients (Perna et al., 2021). This personalized approach allows VR to overcome certain limitations of traditional therapy. For example, it enables patients to select their preferred VR content for relaxation purpose or even fulfill their wishes of traveling, albeit virtually. A case report (Woo and Lee, 2023) reported the therapeutic potential of using freely available videos from the internet as relaxation material to fulfill the participant’s last wishes of traveling to Japan to enjoy the blossoming season of sakura. Third, VR can induce positive emotions in patients faced with existential challenges. Lloyd and Haraldsdottir’s (2019) pilot study reported on patients’ positive experiences, such as joy and happiness, while using VR as a means to temporarily escape from their real and current situation. Since VR is able to simulate a wide range of environments and sensory experiences with remarkable accuracy, it allows patients to select the virtual environment that maximizes their positive emotions (Woo and Lee, 2023).
Although the three most recent systematic reviews support the potential use of VR in palliative care (Carmont and McIlfatrick, 2022; Martin et al., 2022; Mo et al., 2022), there remains a significant gap in research and clinical practices. Martin et al. (2022) report that most VR studies are related to feasibility or are pilot studies with a small sample size and thus call for a randomized controlled trial with adequate power. The importance of delivering meaningful VR interventions to participants is also highlighted in this review, noting that VR activities that are meaningful for the patient are associated with better outcomes. Ma et al. (2021) similarly stress the importance of conducting high-quality randomized controlled trials to validate the effectiveness of VR as a modality of treatment. They also emphasize the necessity of standardizing programs and procedures to promote the widespread adoption of VR in palliative care. Carmont and McIlfatrick (2022) advocate for a comparison between VR therapy and complementary therapies within the context of palliative care. Geraets et al. (2021) express a similar viewpoint, stating that well-designed studies are necessary to explore the efficacy, efficiency, and cost-effectiveness of VR interventions in comparison to existing treatments.
To fill the gap in both clinical practice and research, we developed a novel VR psychological intervention called Flourishing-Life-Of-Wish Virtual Reality Therapy (FLOW-VRT)®. FLOW-VRT is a structured and personalized psychological intervention specially designed for patients in need of palliative care. Its theoretical foundations are based on flow theory (Csikszentmihalyi, 1975), which proposes the psychological state of flow “in which an individual is completely absorbed in activity without reflective self-consciousness but with a deep sense of control” (Engeser et al., 2021, p.2); self-determination theory, which promotes autonomy and sense of control (Deci and Ryan, 2000); stress coping theory, which advocates the employment of various cognitive and behavioral strategies to adapt to stressful conditions (Lazarus and Folkman, 1984); and attention restoration theory, which posits that an exposure to natural environments helps replenish cognitive resources and enhance wellbeing (Kaplan, 1995; Kaplan, 2001). The primary objective of FLOW-VRT is to address patients’ palliative needs by alleviating physical and emotional distress as well as enhancing the quality of end-of-life. “FLOW-VRT-Relaxation” refers to a specialized version of our FLOW-VRT intervention that focuses on relaxation. It allows patients to choose their preferred VR relaxation experience. In a recent case report (Woo and Lee, 2023), we found initial evidence supporting its feasibility and therapeutic potential. Using a randomized controlled trial, the current study compares FLOW-VRT-Relaxation with traditional relaxation practice. We aim to test the efficacy of FLOW-VRT-Relaxation in effective symptom control, i.e., improved emotional and physical symptoms, when compared with traditional relaxation practice.
This was a single-centered, prospective, randomized, single-blind, controlled trial conducted in Hong Kong. The present trial was pre-registered on 6th June 2022 with the Open Science Framework (OSF) registry. The pre-registration can be accessed through https://doi.org/10.17605/OSF.IO/4FJUP. The trial was approved by the Departmental Research Ethics Committee, Department of Psychology, the University of Hong Kong and the Joint CUHK-NTEC CREC (Reference Number: 2022.435-T).
A total of 128 patients with terminal cancer from an adult palliative care ward of Shatin Hospital, a public hospital in Hong Kong, were recruited. Eligible participants were all adults aged 18 or over, Cantonese-speaking, able to give informed consent, and diagnosed with cancer. Exclusion criteria were visual and hearing impairment, severe cognitive impairment, diagnosed epilepsy or having had a seizure in the past 6 weeks, hypersensitivity to motion, active nausea or vomiting, physical disability such as neck injury, a clinically depressed or unstable mood, delirium symptoms, or a history of dissociative disorders. Exclusion criteria are set to minimize the potential physical and psychological risks as delineated in the article of Woo and Lee (2023). A neutral script was used to introduce the study, which is included in Figure 1. Eligible participants who gave informed consent were randomly assigned following simple randomization procedures in a 1:1 ratio to the experimental or control group, using computer-generated randomization (https://www.randomizer.org). The randomization process was concealed until allocation. The sample size calculation was based on efficacy analysis. In order to achieve 80% power in detecting a medium effect size estimate of 0.25 between the two groups at a significance level of 5%, a sample size of 128 was estimated.
In the FLOW-VRT-Relaxation treatment group, a need assessment was first conducted by the primary investigator, who is both a registered clinical psychologist and a certified thanatologist, using a need assessment schedule specifically developed for the purpose of this study. The primary investigator presented the participants with a list of the most popular VR relaxation content (see Table 1), which was compiled based on the results of a survey conducted among patients in palliative care. The 360° VR videos were located in the YouTube VR app. YouTube VR is a free VR application that utilizes 360-degree video playback and spatial audio technologies to provide an immersive viewing experience, allowing users to navigate YouTube content in a virtual environment using VR headsets. The eight YouTube 360° VR videos were selected based on the following criteria:
1. VR content that promotes relaxation through serene environments, comforting sounds, and calming visuals;
2. VR content filmed with steady or stationary cameras to minimize sudden motions that can induce cybersickness;
3. VR content with a lower intensity of visual disturbances, such as minimal use of rapid transitions;
4. VR content that allows patients to focus on a fixed point or provides a stationary viewing experience.
After showing the list of VR content, the participants were asked to select their preferred relaxation video. The primary investigator then assisted in a 10-min session using the chosen relaxation VR video and the Meta Quest 2 VR headset. The Meta Quest 2 is a standalone VR headset with high-quality graphics through a resolution of 1832 × 1920 pixels per eye, providing an immersive viewing experience. During the VR experience, the primary investigator coached on diaphragmatic breathing by inviting the participant to inhale slowly by expanding the belly while focusing on the breathing process, then exhale slowly. Most of the participants spontaneously expressed their feelings and thoughts upon VR exposure. Sufficient time (around 1–2 min) was then provided for their adaptation to the virtual environment and verbal expressions before relaxation coaching. To standardize the procedure, FLOW-VRT-Relaxation was implemented following treatment procedures developed as part of the study and specified in a manual.
In the treatment-as-usual group, a need assessment was first conducted to assess participants’ need for relaxation. In this group, patients received 10-min coaching on diaphragmatic breathing by the primary investigator, as is usual practice in relaxation-based palliative care. Using the same approach as in the treatment group, diaphragmatic breathing was coached by inviting the participant to inhale slowly by expanding the belly while focusing on the breathing, then exhaling slowly. Pre-selected soothing music was played during relaxation.
The outcome measure of the current study is the Chinese version of the Edmonton Symptom Assessment System (CESAS) (Bruera et al., 1991; Dong et al., 2015). It is a questionnaire used to rate the intensity of nine common symptoms experienced by patients diagnosed with cancer. Research has demonstrated the reliability of using it as a tool to assess symptoms in patients undergoing palliative care (Watanabe et al., 2012). The CESAS demonstrated acceptable internal consistency with a Cronbach’s alpha 0.72, strong test-retest reliability with Pearson correlation coefficients ranging from 0.47 to 0.92 between baseline and after 2 h, and good concurrent validity with Spearman correlation ranging from 0.66 to 0.96 between CESAS and the Chinese version of the M. D. Anderson Symptom Inventory (Dong et al., 2015). Demographic and clinical variables such as age, sex, education, medical diagnosis, and current treatment were collected by retrieving information from the medical records with informed consent from the participants.
Upon recruitment, one of our research assistants blinded to study group allocation administered the pre-test measurement, after which another assistant performed the computer-generated randomization and notified the principal investigator of the group allocations. The principal investigator was not blinded to the group allocation due to the nature of the study; however, participants were blinded to study group allocation during the intervention. The research assistant, who was blinded to the study group allocation, administered the post-test measurement.
A comparison between the FLOW-VRT-Relaxation and Treatment-as-Usual groups was performed using Analysis of Covariance (ANCOVA). Pre-test measurements were included as covariates in the ANOVA model to control for their effects on the dependent variable. Statistical analysis was performed using the statistical analysis software Jamovi (The Jamovi Project, 2023), choosing p < 0.05 as indicating statistical significance. The statistical analysis was conducted on an intention-to-treat basis, including all participants irrespective of whether they completed the entire intervention or not (Gupta, 2011). The assumption check of the ANCOVA was assessed using Shapiro-Wilk tests for the normality and Levene’s test for the homogeneity of variances.
Eligible participants from a palliative care unit in a public hospital were recruited from November 2022 to September 2023. During the recruitment period, 140 patients were eligible and approached for the study, with 128 (91%) agreeing to participate. Through randomization, 64 were assigned to the experimental group, and 64 were assigned to the control group. The overall completion rate is 93%, with 59 [92.2%] participants from the experimental group and 60 [93.8%] participants from the control group completing the session. Reasons for incomplete sessions include lack of interest in continuing VR intervention, unfavorable physical conditions such as coughing and tiredness, interruptions such as family visits and early discharge, and needs assessed to be null for VR intervention. The mean and standard deviation ages of the 128 randomized participants are 66.6 and 11.5 years, respectively. 90 of 128 recruited participants [70%] are female, while 38 [30%] are male. The majority of participants completed at least primary education (120 participants [93.8%]). There are no significant differences between groups in terms of age [t(126) = 0.183, p = 0.855], education [χ2(4) = 1.24, p = 0.871], gender [χ2 (1) = 0.599, p = 0.439] and medical treatment [χ2 (4) = 7.43, p = 0.115]. Similarly, there are no significant differences between groups at baseline in CESAS-Total score [t(117) = 0.695, p = 0.488], CESAS-Physical Subscale score [t(117) = 0.401, p = 0.689], and CESAS-Emotional Subscale score [t(117) = 0.324, p = 0.746]. Please refer to Figure 2 for the CONSORT study flow diagram and Table 2 for the baseline characteristics of participants. ANCOVA with the baseline assessment as covariates was conducted to determine if FLOW-VRT-Relaxation would bring about more symptom reduction when compared with a traditional relaxation practice. The ANOVA assumptions were assessed for the total score, physical subscale score, and emotional subscale score. The results of Shapiro-Wilk tests show that the total score (p = 0.112) and physical subscale score (p = 0.182) are normally distributed, but not the emotional subscale score (p < 0.05). Kruskal-Wallis test, as a non-parametric test, was then conducted to analyze the emotional subscale score. The assumption of homogeneity of variances was examined using Levene’s test, which indicates no significant differences for the total score [F(1, 117) = 0.634, p = 0.427], emotional subscale score [F(1, 117) = 0.007, p = 0.934], and physical subscale score [F(1, 117) = 1.88, p = 0.173].
The ANCOVA results show significant differences between the experimental and control groups on the total score [F(1, 116) = 11.3, p = 0.001,
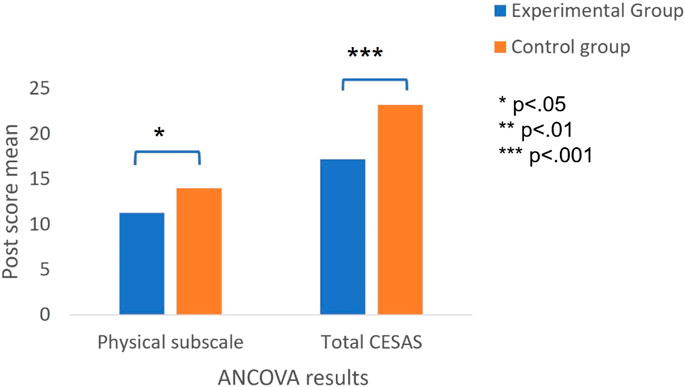
FIGURE 3. ANOVA results under the between-group comparisons on physical subscale score and total score.
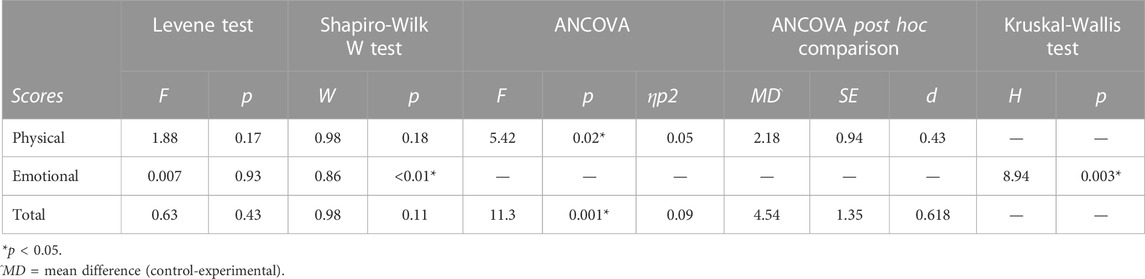
TABLE 4. ANCOVA with post hoc comparisons or Kruskal-Wallis test results, following results from Levene’s test and Shapiro-Wilk W test.
The current study compares the efficacy of FLOW-VRT-Relaxation with respect to traditional relaxation practice in a palliative care setting. FLOW-VRT-Relaxation shows a significant difference in the reduction of the total score [F(1, 116) = 11.3, p = 0.001,
The therapeutic elements of FLOW-VRT-Relaxation that are particularly useful in reducing the emotional and physical symptoms among patients with terminal illnesses may relate to its theoretical frameworks. First, FLOW-VRT-Relaxation may have the potential to enhance patients’ self-determination, which requires future investigations to establish the potential relationship. Self-determination theory is “centrally concerned with the social conditions that facilitate or hinder human flourishing” (Ryan and Deci, 2017, p. 6). It is a psychological theory that appraises behavior as a function of motives, taking the form of desires, values, and goals (Deci and Ryan, 2000). Research shows that autonomy-supportive interactions are effective in motivating individuals to adopt healthier behaviors, in contrast to methods that aim to control or regulate the person (Ryan et al., 2008; Ryan et al., 2011). The therapeutic benefits of FLOW-VRT may relate to customization, allowing patients to choose the content used during the experience according to their desires and values. The findings of a systematic review by Martin et al. (2022) resonate with the current study, revealing the therapeutic potential of customized content. Specifically, the review highlights a pattern across the statistical results in which significant somatic and psychological symptom improvement was observed when the VR experience was personally meaningful. Second, FLOW-VRT-Relaxation incorporates VR technology, which has been shown to be flow-inducing (Gaggioli et al., 2003). Although limited studies are exploring the direct effect of flow experiences induced by VR on symptom control in palliative care, it is known that flow is associated with both physical and psychological wellbeing (Persson, 1996; Heo et al., 2010; Hirao et al., 2012; Heo et al., 2013). Future research is, therefore, recommended to substantiate the role of flow in symptom management among patients with terminal illnesses. Lastly, FLOW-VRT-Relaxation may offer opportunities for patients to explore and cultivate adaptive stress coping. The stress coping theory posits the existence of two coping strategies: problem-focused coping, which refers to a coping style concentrating on the management of stressful situations by operating on the stressor, and emotion-focused coping, which aims to manage one’s emotions when facing that stressor (Lazarus and Folkman, 1984). FLOW-VRT-Relaxation allows patients to experience positive emotions derived from the virtual experience, which is clinically meaningful when the stressful condition of being terminally ill may not allow room for problem-focused coping. Such emotion-focused coping is further supported by the findings of Carmont and McIlfatrick’s (2022) systematic integrative review. Their study highlights the potential of VR to foster emotional connection, particularly in the context of patients dealing with terminal illnesses and the accompanying physical and emotional decline.
A possible limitation of the current study is that only the immediate effect of FLOW-VRT-Relaxation is measured. Since a follow-up assessment, such as in one-day or one-week time, is not conducted, the maintenance of the treatment effect of relaxation is not ascertained. Given the fact that the death of patients in palliative care can be imminent, i.e., within a few hours or days (General Medical Council of the United Kingdom, 2010), the short-term therapeutic effect of FLOW-VRT-Relaxation on patients is regarded as clinically meaningful, not to mention the virtual fulfillment of their last wishes. Although the current study investigates only the immediate effects, long-term benefits are worthy of further investigation and research. Another limitation refers to the fact that all the VR videos are drawn from pre-existing online sources, limiting the degree of personalization. As meaningful VR for patients is important, as highlighted in the systematic review of Martin et al. (2022), future research that focuses on the advancement of personalized and meaningful VR content for the needs of patients in palliative care is recommended. The participation of various stakeholders, such as patients, families, ward staff, and therapists, in the curation process would be favorable. Lastly, since FLOW-VRT-Relaxation is carried out by one registered clinical psychologist who is also a certified thanatologist with years of clinical experience of VR delivery in palliative care settings, results may not reflect the skills of other VR therapists or facilitators. Appropriate training may be needed for the VR therapists-to-be to ensure quality delivery of VR interventions in palliative care.
Based on our clinical experience in administering VR-based interventions in a palliative care setting, we suggest taking a few precautions to minimize potential adverse effects associated with the use of this technology. First, patients’ needs, values, and preferences should be respected at all times, following the ethical principle of patient autonomy (Beauchamp and Childress, 2001). One of the participants who withdrew from our research shared that he wished to watch war-related VR content instead of what the therapist had selected as relaxing, while another participant rejected VR exposure due to a lack of interest. Encouraging patients to try such a novel technology further may impose unnecessary stress or psychological pressure. Second, exclusion criteria should be crafted with care in preparation for future clinical or research applications. Given the physical and emotional vulnerability of the target users, patients with symptoms of depression or suffering from low morale may be susceptible to psychological distress. Indeed, engaging in virtual travel involving (virtual) physical activities may backfire as it can increase awareness of one’s actual physical limitations. The patient may experience a sense of loss regarding their physical abilities or their past identity, such as being an energetic hiker or scuba diver. This heightened awareness of limitations can lead to emotional disturbances and potentially pose psychological risks. Therefore, it is essential to screen a patient’s mood at all times, including their readiness to enter the virtual and ideal world. Lastly, our study shows a high female-to-male ratio (70%–30%) in the recruited participants. We observe that males show higher rates of rejection towards research participation and are more often physically unable to join the VR research, i.e., males are observed to be more tired, more often with life-supporting devices, and more often sleeping upon approach when compared with females. Based on the clinical sensitivity and experiences of VR therapists or researchers, it is important to decide whether or not to proceed with recruitment to avoid unnecessary pressure or burden on patients who are either psychologically or physically unready for VR.
Our results show that following a FLOW-VRT-Relaxation session, the symptoms of distress that patients in palliative care have to endure significantly reduce, whether physical or emotional in nature. The novel and distinctive features of FLOW-VRT-Relaxation include prior assessment of individual needs for VR relaxation, customized VR relaxation content, and live coaching of relaxation techniques by a clinical psychologist during VR. Instead of being limited to coaching diaphragmatic breathing, as is the case in traditional clinical settings, FLOW-VRT-Relaxation includes an immersive virtual experience using “relaxation content” previously selected by the patients themselves. Their improvement in mood and physical symptoms may be explained by the capacity of this innovative technology to address not only the physical symptoms (e.g., through relaxation induced by a powerful and distracting immersive experience) but also the psychological needs (e.g., through virtual fulfillment of wishes, sense of control). Addressing these physical and psychological needs is particularly important for patients with terminal illnesses who often suffer from their physical constraints (e.g., bedbound conditions, unfavorable ward environments, unresolved pain, negative side-effects of medications) and emotional fragility (e.g., unfulfilled wishes of traveling to a comfortable place, barriers to escape from current suffering). FLOW-VRT-Relaxation appears to be a superior form of relaxation than the traditional approach, as the former potentially addresses the high prevalence of palliative symptoms and further improves the quality of end-of-life care. In future follow-up studies, we will explore whether FLOW-VRT can lead to greater senses of presence, flow, and, restoration that contribute to symptom control, which hopefully provides further evidence to support our claims about the positive effects of our intervention on adaptive stress-coping.
The current study tested the efficacy of FLOW-VRT-Relaxation by comparing it to traditional relaxation practice in palliative care. Our results show that following a FLOW-VRT-Relaxation session, the symptoms of distress that patients in palliative care typically report significantly reduce, whether physical or emotional in nature. It provides promising evidence that the newly developed FLOW-VRT-Relaxation is preferable as a novel relaxation practice in palliative care. It is hitherto the first personalized VR relaxation intervention guided by theories and clinical considerations on the purpose and content of VR, how VR is to be delivered, and by whom it is delivered. It is also the first VR relaxation intervention empirically tested in a randomized controlled trial with an adequate sample size and compared with traditional relaxation practice in a palliative care setting. The encouraging result of the current research may shed light on the potential application of FLOW-VRT-Relaxation in wider adoption, such as elderly homes and rehabilitation centers. With its optimal use, FLOW-VRT-Relaxation hopefully serve as a complementary therapeutic tool that effectively improves end-of-life care in face of the mounting need of palliative care.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by the Departmental Research Ethics Committee, Department of Psychology, the University of Hong Kong and the Joint CUHK-NTEC CREC (Reference Number: 2022.435-T). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
OW: Conceptualization, Data curation, Formal Analysis, Investigation, Writing–original draft. AL: Conceptualization, Investigation, Supervision, Writing–review and editing. RN: Writing–review and editing. DE: Writing–review and editing. RL: Writing–review and editing. AC: Funding acquisition, Writing–review and editing, Validation, Resources.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research was funded by the CityU Strategic Research Grant (SRG-Fd) (Grant no. 7006120).
The authors would like to thank all the participants that took part in the study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Bani Mohammad, E., and Ahmad, M. (2019). Virtual reality as a distraction technique for pain and anxiety among patients with breast cancer: a randomized control trial. Palliat. Support. Care 17 (1), 29–34. doi:10.1017/S1478951518000639
Baños, R. M., Espinoza, M., García-Palacios, A., Cervera, J. M., Esquerdo, G., Barrajón, E., et al. (2013). A positive psychological intervention using virtual reality for patients with advanced cancer in a hospital setting: a pilot study to assess feasibility. Support. Care Cancer 21 (1), 263–270. doi:10.1007/s00520-012-1520-x
Barlow, D. H., Craske, M. G., Cerny, J. A., and Klosko, J. S. (1989). Behavioral treatment of panic disorder. Behav. Ther. 20 (2), 261–282. doi:10.1016/s0005-7894(89)80073-5
Beauchamp, T. L., and Childress, J. F. (2001). Principles of biomedical ethics. 5th ed. Oxford University Press.
Bruera, E., Kuehn, N., Miller, M., Selmser, P., and Macmillan, K. (1991). The Edmonton Symptom Assessment System (ESAS): a simple method for the assessment of palliative care patients. J. Palliat. Care 7, 6–9. doi:10.1177/082585979100700202
Brungardt, A., Wibben, A., Tompkins, A. F., Shanbhag, P., Coats, H., LaGasse, A. B., et al. (2021). Virtual reality-based music therapy in palliative care: a pilot implementation trial. J. Palliat. Med. 24 (5), 736–742. doi:10.1089/jpm.2020.0403
Carmont, H., and McIlfatrick, S. (2022). Using virtual reality in palliative care: a systematic integrative review. Int. J. Palliat. Nurs. 28 (3), 132–144. doi:10.12968/ijpn.2022.28.3.132
Charalambous, A., Giannakopoulou, M., Bozas, E., Marcou, Y., Kitsios, P., and Paikousis, L. (2016). Guided imagery and progressive muscle relaxation as a cluster of symptoms management intervention in patients receiving chemotherapy: a randomized control trial. PloS One 11 (6), e0156911. doi:10.1371/journal.pone.0156911
Chirico, A., Lucidi, F., De Laurentiis, M., Milanese, C., Napoli, A., and Giordano, A. (2016). Virtual reality in health system: beyond entertainment. a mini-review on the efficacy of VR during cancer treatment. J. Cell. Physiology 231 (2), 275–287. doi:10.1002/jcp.25117
Cohen, J. (1988). Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, N.J: L. Erlbaum Associates.
Cohen, S. (2004). Social relationships and health. Am. Psychol. 59 (8), 676–684. doi:10.1037/0003-066x.59.8.676
Cummings, J. J., and Bailenson, J. N. (2016). How immersive is enough? A meta-analysis of the effect of immersive technology on user presence. Media Psychol. 19 (2), 272–309. doi:10.1080/15213269.2015.1015740
de Carvalho, E. C., Martins, F. T. M., and dos Santos, C. B. (2007). A pilot study of a relaxation technique for management of nausea and vomiting in patients receiving cancer chemotherapy. Cancer Nurs. 30 (2), 163–167. doi:10.1097/01.ncc.0000265007.87311.d0
Deci, E. L., and Ryan, R. M. (2000). The “what” and “why” of goal pursuits: human needs and the self-determination of behavior. Psychol. Inq. 11, 227–268. doi:10.1207/s15327965pli1104_01
Dikmen, H. A., and Terzioglu, F. (2019). Effects of reflexology and progressive muscle relaxation on pain, fatigue, and quality of life during chemotherapy in gynecologic cancer patients. Pain Manag. Nurs. 20 (1), 47–53. doi:10.1016/j.pmn.2018.03.001
Dong, Y., Chen, H., Yuanyu, G., Ying, K., Jung, H., et al. (2015). Psychometric validation of the Edmonton symptom assessment system in Chinese patients. J. Pain Symptom Manag. 50 (5), 712–717.e2. doi:10.1016/j.jpainsymman.2015.05.018
Engeser, S., Schiepe-Tiska, A., and Peifer, C. (2021). “Historical lines and an overview of current research on flow,” in Advances in flow research (Springer International Publishing), 1–29. doi:10.1007/978-3-030-53468-4_1
Ezer, T., Lohman, D., and de Luca, G. B. (2018). Palliative care and human rights: a decade of evolution in standards. J. Pain Symptom Manag. 55 (2), S163–S169. doi:10.1016/j.jpainsymman.2017.03.027
Ferguson, C., Shade, M. Y., Blaskewicz Boron, J., Lyden, E., and Manley, N. A. (2020). Virtual reality for therapeutic recreation in dementia hospice care: a feasibility study. Am. J. Hospice Palliat. Med. 37 (10), 809–815. doi:10.1177/1049909120901525
Fink, A. K., Gurwitz, J., Rakowski, W., Guadagnoli, E., and Silliman, R. A. (2004). Patient beliefs and tamoxifen discontinuance in older women with estrogen receptor—positive breast cancer. J. Clin. Oncol. 22 (16), 3309–3315. doi:10.1200/JCO.2004.11.064
Gaggioli, A., Bassi, M., and Delle Fave, A. (2003). “Quality of experience in virtual environments,” in Being there: concepts, effects and measurement of user presence in synthetic environments. Editors G. Riva, W. IJsselsteijn, and F. Davide (Amsterdam: IOS Press), 121–135.
General Medical Council of the United Kingdom (2010). Treatment and care towards the end of life: good practice in decision making. Available at: https://www.gmc-uk.org/-/media/documents/treatment-and-care-towards-the-end-of-life---english-1015_pdf-48902105.pdf?la=en&hash=41EF651C76FDBEC141FB674C08261661BDEFD004.
Geraets, C. N. W., van der Stouwe, E. C. D., Pot-Kolder, R., and Veling, W. (2021). Advances in immersive virtual reality interventions for mental disorders: a new reality? Curr. Opin. Psychol. 41, 40–45. doi:10.1016/j.copsyc.2021.02.004
Gupta, S. K. (2011). Intention-to-treat concept: a review. Perspect. Clin. Res. 2 (3), 109–112. doi:10.4103/2229-3485.83221
Heins, M., Hofstede, J., Rijken, M., Korevaar, J., Donker, G., and Francke, A. (2018). Palliative care for patients with cancer: do patients receive the care they consider important? A survey study. BMC Palliat. Care 17 (1), 61–67. doi:10.1186/s12904-018-0315-3
Heo, J., Lee, Y., Pedersen, P. M., and McCormick, B. P. (2010). Flow experience in the daily lives of older adults: an analysis of the interaction between flow, individual differences, serious leisure, location, and social context. Can. J. Aging/La Revue Can. Du Vieillissement 29 (3), 411–423. doi:10.1017/s0714980810000395
Heo, J., Stebbins, R. A., Kim, J., and Lee, I. (2013). Serious leisure, life satisfaction, and health of older adults. Leis. Sci. 35 (1), 16–32. doi:10.1080/01490400.2013.739871
Hirao, K., Kobayashi, R., Okishima, K., and Tomokuni, Y. (2012). Flow experience and health related quality of life in community dwelling elderly Japanese. Nurs. Health Sci. 14 (1), 52–57. doi:10.1111/j.1442-2018.2011.00663.x
Hoffman, H. G., Richards, T. L., Bills, A. R., Van Oostrom, T., Magula, J., Seibel, E. J., et al. (2006). Using fMRI to study the neural correlates of virtual reality analgesia. CNS Spectrums 11 (1), 45–51. doi:10.1017/s1092852900024202
Johnson, T., Bauler, L., Vos, D., Hifko, A., Garg, P., Ahmed, M., et al. (2020). Virtual reality use for symptom management in palliative care: a pilot study to assess user perceptions. J. Palliat. Med. 23 (9), 1233–1238. doi:10.1089/jpm.2019.0411
Kaplan, S. (1995). The restorative benefits of nature: toward an integrative framework. J. Environ. Psychol. 15, 169–182. doi:10.1016/0272-4944(95)90001-2
Kaplan, S. (2001). Meditation, restoration and the management of mental fatigue. Environ. Behav. 33, 480–506. doi:10.1177/00139160121973106
Katon, W. J. (2003). Clinical and health services relationships between major depression, depressive symptoms, and general medical illness. Biol. Psychiatry 54 (3), 216–226. doi:10.1016/s0006-3223(03)00273-7
Khater, W. A., Akhu-Zaheya, L. M., Al-Nabulsi, H. W., Shattnawi, K. K., Shamieh, O., and Joseph, R. (2021). Barriers to implementing palliative care in intensive care units: perceptions of physicians and nurses in Jordan. Int. J. Palliat. Nurs. 27 (2), 98–106. doi:10.12968/ijpn.2021.27.2.98
Kwekkeboom, K. L., Hau, H., Wanta, B., and Bumpus, M. (2008). Patients’ perceptions of the effectiveness of guided imagery and progressive muscle relaxation interventions used for cancer pain. Complementary Ther. Clin. Pract. 14 (3), 185–194. doi:10.1016/j.ctcp.2008.04.002
Lazarus, A. A., and Mayne, T. J. (1990). Relaxation: some limitations, side effects, and proposed solutions. Psychotherapy Theory, Res. Pract. Train. 27 (2), 261–266. doi:10.1037/0033-3204.27.2.261
Lin, K.-Y., Hu, Y.-T., Chang, K.-J., Lin, H.-F., and Tsauo, J.-Y. (2011). Effects of yoga on psychological health, quality of life, and physical health of patients with cancer: a meta-analysis. Evidence-Based Complementary and Alternative Medicine, 659876. doi:10.1155/2011/659876
Lloyd, A., and Haraldsdottir, E. (2019). P-165 observations of immersive virtual reality sessions in a hospice. BMJ Support. Palliat. Care 9 (Suppl. 4), A71. doi:10.1136/bmjspcare-2019-HUKNC.187
Ma, L., Mor, S., Anderson, P., Baños, R., Botella, C., Bouchard, S., et al. (2021). Integrating virtual realities and psychotherapy: SWOT analysis on VR and MR based treatments of anxiety and stress-related disorders. Cogn. Behav. Ther. 50 (6), 509–526. doi:10.1080/16506073.2021.1939410
Ma, X., Yue, Z.-Q., Gong, Z.-Q., Zhang, H., Duan, N.-Y., Shi, Y.-T., et al. (2017). The effect of diaphragmatic breathing on attention, negative affect and stress in healthy adults. Front. Psychol. 8, 874. doi:10.3389/fpsyg.2017.00874
Malloy, K. M., and Milling, L. S. (2010). The effectiveness of virtual reality distraction for pain reduction: a systematic review. Clin. Psychol. Rev. 30 (8), 1011–1018. doi:10.1016/j.cpr.2010.07.001
Martin, J. L., Saredakis, D., Hutchinson, A. D., Crawford, G. B., and Loetscher, T. (2022). Virtual reality in palliative care: a systematic review. Healthc. (Basel) 10 (7), 1222. doi:10.3390/healthcare10071222
Matsuda, A., Yamaoka, K., Tango, T., Matsuda, T., and Nishimoto, H. (2014). Effectiveness of psychoeducational support on quality of life in early-stage breast cancer patients: a systematic review and meta-analysis of randomized controlled trials. Qual. Life Res. 23, 21–30. doi:10.1007/s11136-013-0460-3
McCallie, M. S., Blum, C. M., and Hood, C. J. (2006). Progressive muscle relaxation. J. Hum. Behav. Soc. Environ. 13 (3), 51–66. doi:10.1300/j137v13n03_04
Melzack, R., and Wall, P. D. (1965). Pain Mechanisms: a New Theory: a gate control system modulates sensory input from the skin before it evokes pain perception and response. Science 150 (3699), 971–979. doi:10.1126/science.150.3699.971
Mo, J., Vickerstaff, V., Minton, O., Tavabie, S., Taubert, M., Stone, P., et al. (2022). How effective is virtual reality technology in palliative care? A systematic review and meta-analysis. Palliat. Med. 36 (7), 1047–1058. doi:10.1177/02692163221099584
Morina, N., Ijntema, H., Meyerbröker, K., and Emmelkamp, P. M. (2015). Can virtual reality exposure therapy gains be generalized to real-life? A meta-analysis of studies applying behavioral assessments. Behav. Res. Ther. 74, 18–24. doi:10.1016/j.brat.2015.08.010
Niki, K., Okamoto, Y., Maeda, I., Mori, I., Ishii, R., Matsuda, Y., et al. (2019). A novel palliative care approach using virtual reality for improving various symptoms of terminal cancer patients: a preliminary prospective, multicenter study. J. Palliat. Med. 22 (6), 702–707. doi:10.1089/jpm.2018.0527
Norton, P. J., and Price, E. C. (2007). A meta-analytic review of adult cognitive-behavioral treatment outcome across the anxiety disorders. J. Nerv. Ment. Dis. 195 (6), 521–531. doi:10.1097/01.nmd.0000253843.70149.9a
Perna, M. S. C, Msw, L., Lund, S., White, N., and Minton, O. (2021). The potential of personalized virtual reality in palliative care: a feasibility trial. Am. J. Hospice Palliat. Med. 38 (12), 1488–1494. doi:10.1177/1049909121994299
Persson, D. (1996). Play and flow in an activity group—a case study of creative occupations with chronic pain patients. Scand. J. Occup. Ther. 3, 33–42. doi:10.3109/11038129609106680
Ryan, R. M., and Deci, E. L. (2017). Self-determination theory: basic psychological needs in motivation, development, and wellness. The Guilford Press. doi:10.1521/978.14625/28806
Ryan, R. M., Lynch, M. F., Vansteenkiste, M., and Deci, E. L. (2011). Motivation and autonomy in counseling, psychotherapy, and behavior change: a look at theory and practice. Couns. Psychol. 39 (2), 193–260. doi:10.1177/0011000009359313
Ryan, R. M., Patrick, H., Deci, E. L., and Williams, G. C. (2008). Facilitating health behaviour change and its maintenance: interventions based on self-determination theory. Eur. Health Psychol. 10, 2–5.
Schneider, S. M., Prince-Paul, M., Allen, M. J., Silverman, P., and Talaba, D. (2004). Virtual reality as a distraction intervention for women receiving chemotherapy. Oncol. Nurs. Forum 31 (1), 81–88. doi:10.1188/04.ONF.81-88
Simeit, R., Deck, R., and Conta-Marx, B. (2004). Sleep management training for cancer patients with insomnia. Support. Care Cancer 12, 176–183. doi:10.1007/s00520-004-0594-5
Slater, M. (2009). Place illusion and plausibility can lead to realistic behaviour in immersive virtual environments. Philosophical Trans. R. Soc. B Biol. Sci. 364 (1535), 3549–3557. doi:10.1098/rstb.2009.0138
Spitzer, R. L., Kroenke, K., Linzer, M., Hahn, S. R., Williams, J. B., Degruy, F. V., et al. (1995). Health-related quality of life in primary care patients with mental disorders: results from the PRIME-MD 1000 Study. Jama 274 (19), 1511–1517. doi:10.1001/jama.274.19.1511
Stetz, M. M. C., Ries, R. I., and Folen, R. A. (2011). “Virtual reality supporting psychological health,” in Advanced computational intelligence paradigms in healthcare 6. Virtual reality in psychotherapy, rehabilitation, and assessment (Springer), 13–29.
Stoerkel, E., Bellanti, D., Paat, C., Peacock, K., Aden, J., Setlik, R., et al. (2018). Effectiveness of a self-care toolkit for surgical breast cancer patients in a military treatment facility. J. Altern. Complementary Med. 24 (9-10), 916–925. doi:10.1089/acm.2018.0069
The Jamovi Project (2023). jamovi. [Computer Software]. Available at: https://www.jamovi.org.
Tsitsi, T., Charalambous, A., Papastavrou, E., and Raftopoulos, V. (2017). Effectiveness of a relaxation intervention (progressive muscle relaxation and guided imagery techniques) to reduce anxiety and improve mood of parents of hospitalized children with malignancies: a randomized controlled trial in Republic of Cyprus and Greece. Eur. J. Oncol. Nurs. 26, 9–18. doi:10.1016/j.ejon.2016.10.007
Wang, T., Molassiotis, A., Chung, B., and Tan, J. (2018). Unmet care needs of advanced cancer patients and their informal caregivers: a systematic review. BMC Palliat. Care 17 (1), 96–29. doi:10.1186/s12904-018-0346-9
Watanabe, S., Nekolaichuk, C., and Beaumont, C. (2012). The Edmonton Symptom Assessment System, a proposed tool for distress screening in cancer patients: development and refinement. Psycho-oncology (Chichester, Engl. 21 (9), 977–985. doi:10.1002/pon.1996
Weingarten, K., Macapagal, F., and Parker, D. (2019). Virtual reality: endless potential in pediatric palliative care: a case report. J. Palliat. Med. 23 (1), 147–149. doi:10.1089/jpm.2019.0207
Wittkopf, P. G., Lloyd, D. M., Coe, O., Yacoobali, S., and Billington, J. (2020). The effect of interactive virtual reality on pain perception: a systematic review of clinical studies. Disabil. Rehabilitation 42 (26), 3722–3733. doi:10.1080/09638288.2019.1610803
Woo, K. L. O., and Lee, A. (2023). Case report: therapeutic potential of Flourishing-Life-Of-Wish Virtual Reality Therapy on Relaxation (FLOW-VRT-Relaxation)—a novel personalized relaxation in palliative care. Front. Digital Health 5, 1228781. doi:10.3389/fdgth.2023.1228781
Woo, O. K. L., and Lee, A. M. (2023). A perspective on potential psychological risks and solutions of using virtual reality in palliative care. Front. Virtual Real. 4, 1256641. doi:10.3389/frvir.2023.1256641
World Health Organization (2020). Palliative care fact sheet. Available at: http://www.who.int/mediacentre/factsheets/fs402/en/.
Keywords: virtual reality, palliative care, relaxation, FLOW-VRT, personalized, end-of-life care, symptom management, randomized controlled trial
Citation: Woo OKL, Lee AM, Ng R, Eckhoff D, Lo R and Cassinelli A (2024) Flourishing-Life-Of-Wish Virtual Reality Relaxation Therapy (FLOW-VRT-Relaxation) outperforms traditional relaxation therapy in palliative care: results from a randomized controlled trial. Front. Virtual Real. 4:1304155. doi: 10.3389/frvir.2023.1304155
Received: 29 September 2023; Accepted: 04 December 2023;
Published: 31 January 2024.
Edited by:
Marientina Gotsis, University of Southern California, United StatesCopyright © 2024 Woo, Lee, Ng, Eckhoff, Lo and Cassinelli. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Olive K. L. Woo, b2xpdmV3b29raXRsaW5nQGdtYWlsLmNvbQ==, b2xpdmV3b29AY29ubmVjdC5oa3UuaGs=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.