- 1Research Centre for Digital Mental Health Services, Division of Psychiatry, Haukeland University Hospital, Bergen, Norway
- 2Centre for Psychiatry Research, Department of Clinical Neuroscience, Stockholm Health Care Services, Karolinska Institutet, Stockholm, Sweden
- 3Department of Global Public Health and Primary Care, Faculty of Medicine, University of Bergen, Bergen, Norway
Objective: Public Speaking Anxiety is highly prevalent among adolescents. However, few interventions have been developed specifically for this group. This four-armed randomized trial addressed the following research questions regarding interventions for adolescents with public speaking anxiety (PSA): 1) is Virtual Reality exposure therapy (VRET) more efficacious than online psychoeducation or waitlist, and 2) is VRET followed by online exposure therapy more efficacious than VRET alone or online psychoeducation followed by online exposure therapy?
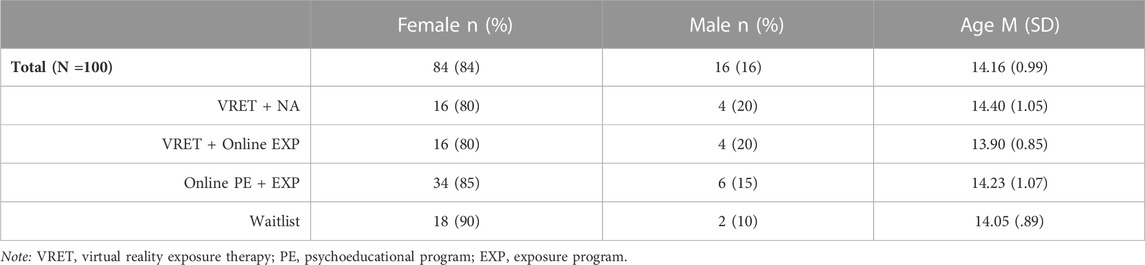
Methods: Adolescents, aged 13–16 with PSA were randomized to four groups: 1) VRET + no additional intervention (n = 20); 2) VRET + online exposure program (n = 20); 3) online psychoeducation program + exposure program (n = 40); or 4) waitlist (n = 20). Self-rated PSA symptoms served as primary outcome measure, with secondary outcomes covering other social anxiety symptoms.
Results: Linear mixed models revealed that there was a significant difference in the decrease in PSA symptoms among adolescents receiving VRET compared with waiting list (p = 0.015), but no significant difference to the online psychoeducation program (p = 0.056). However, online psychoeducation program yielded smaller within-group effect sizes compared to VRET, d = 0.33 vs. d = 0.83 respectively. VRET + online exposure program had a significant decrease in PSA symptoms (p = 0.013), but no significant difference from VRET + no additional intervention or online psychoeducation + online exposure program. Symptom reduction remained stable at 3-month follow-up.
Conclusion: The study shows the potential of delivering both gamified VRET as well as online psychoeducation and exposure programs as self-guided interventions for adolescents with PSA.
Clinical trial registration: clinicaltrials.gov, identifier: NCT04396392
1 Introduction
Public Speaking Anxiety (PSA) is the most common type of anxiety reported in the general population, and involves the fear of being negatively evaluated when performing in front of others (American Psychiatric Association, 2013). Symptoms typically onset during adolescence, with a higher prevalence among girls than boys (Essau et al., 2014). PSA can cause severe impairment in everyday functioning, including a negative impact on education (Ferreira Marinho et al., 2017), which may lead to occupational (Stein et al., 1996) and financial (Wittchen et al., 1999) difficulties in adulthood. PSA is also associated with depression and other anxiety disorders (Grant et al., 2005). While PSA has been recognized as a distinct “performance-only” subgroup of social anxiety disorder (SAD) (Blöte et al., 2009), around one-third of adolescents with PSA also experience difficulties in other social situations, and are at risk of developing generalized SAD (Wittchen et al., 1999). Thus, there is a need to develop efficacious interventions targeting adolescents with PSA.
Cognitive behavioral therapy (CBT) is recommended by the National Institute for Health and Care Excellence (NICE) guidelines (National Institute for Health and Care Excellence, 2013) and involves controlled exposure to the feared stimuli with a goal of disproving and thereby replacing the catastrophic beliefs that maintain the vicious cycle of avoidance (Craske et al., 2008). Exposure therapy for phobias is typically conducted using real-life (in-vivo) stimuli; however, in the case of PSA, this presents a logistic challenge since it requires an actual audience, hindering dissemination of an evidence-based treatment.
Technology-delivered interventions, such as Virtual Reality (VR) technology, offers an apparent solution to this issue. By having the user wear a head-mounted display interactive to head and even body movements, an immersive experience of being in a virtual environment (e.g., in front of an audience) can be simulated. This immersive experience can be put in to therapeutic use (Lindner, 2020). The VR format can be delivered through a computer-generated virtual environment or through 360° videos (Brivio et al., 2021). This format has the benefit of providing fully customizable virtual environments and the possibility of designing interventions as attractive, user-friendly and engaging serious games (Halldorsson et al., 2021). A meta-analysis of randomized controlled trials showed that VRET is an efficacious way of treating adults with anxiety and related disorders with large effect sizes when compared with waitlist controls, and with equal effect sizes when comparing with in vivo control groups (Carl et al., 2019). Another systematic review of 22 studies on adults showed equal efficacy of VRET and in vivo exposure (Horigome et al., 2020). The latest systematic review identified 27 studies targeting SAD, and found VRET as superior to waitlist in most studies, but not to in vivo control groups (Wiebe et al., 2022). Importantly, anxiety symptoms continue to decrease among adults who received VRET in the years that follow, even without continued VR use (Anderson et al., 2017).
Technological advances now make it possible to develop self-guided or even automated VR interventions (Lindner et al., 2019; Premkumar et al., 2021; Zainal et al., 2021), increasing the dissemination potential. Among adults, there is growing evidence for efficacy: one study showed that self-guided VRET for PSA had similar reduction in PSA symptoms when compared with therapist-led VRET (Lindner et al., 2019), and another study showed that self-guided VRET with 360-videos led to a reduction in SAD severity when compared with waiting list (Zainal et al., 2021). A study on adolescents aged 17–18 years old measured self-reported anxiety levels before each presentation (Valls-Ratés et al., 2022). The study found that the VR group presenting in front of a VR audience had a similar reduction in anxiety when compared to a non-VR group who conducted the oral presentations alone in a classroom. However, the VR group reported higher satisfaction rate at post-intervention.
Computer-generated, automated VR interventions may feature virtual therapists (Miloff et al., 2020), and allow manipulation of certain variables such as audience size, audience reaction and exposure tasks (Premkumar et al., 2021). Recently, self-guided VRET interventions have taken the form of “Applied Games” (Fleming et al., 2017). Applied games include gamification elements such as challenges, rewards, progression levels, star ratings or goals. Such gamification elements may increase adherence (Freeman et al., 2018; Goldenhersch et al., 2020; De Croon et al., 2021), and promote user behavior and intrinsic motivation (Mekler et al., 2013). Studies on VRET in an Applied games format for adults have shown promising results (Fleming et al., 2017), e.g., for spider phobia (Miloff et al., 2019).
Given its playful elements, VR has a great potential as an intervention for adolescents with PSA (Meyerbröker and Morina, 2021), who will likely be familiar to the game framework. VRET in a Applied games format has the potential of reaching out to adolescents who would otherwise not seek help, as adolescents would regard it as a game rather than psychotherapy (Fleming et al., 2017), which could result in less stigma and embarrassment. The literature on VRET for PSA has however almost exclusively featured adults (Ebrahimi et al., 2019; Kothgassner and Felnhofer, 2020; Reeves et al., 2021), with only three published feasibility or pilot studies (Parrish et al., 2016; Kahlon et al., 2019; Sülter et al., 2022), and two randomized controlled trials targeting children and adolescents with PSA (Gutiérrez-Maldonado et al., 2009; Valls-Ratés et al., 2022). None of the studies featured VRET in an Applied Games format.
As PSA often goes untreated (Wittchen et al., 1999), there is a need to intervene at an early stage in order to reduce PSA symptoms they experience currently and its negative impact on their education (Grant et al., 2005). Self-guided, technology-delivered interventions may be a possible solution to lower their threshold in seeking mental health advice (Conley et al., 2022). The main aim of the intervention developed for the current study was to target debilitating levels of PSA and was designed as a direct intervention for PSA. As PSA can cause severe negative consequences in adolescents’ school life, the overall aim was to reduce ongoing PSA symptoms. The current study investigates two research questions through a two-phased design: 1) Is self-guided, gamified, and automated VRET for adolescents with PSA more efficacious than online psychoeducation or waitlist in phase one? And 2) Is VRET followed by online exposure therapy more efficacious than VRET alone or online psychoeducation followed by online exposure program in phase two?
2 Materials and methods
2.1 Trial design and ethics
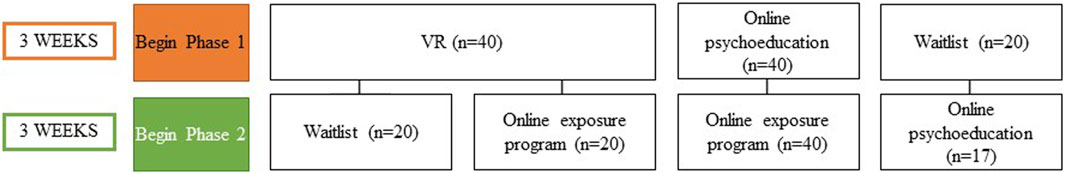
The current study, YoungSpotlight, was part of the larger INTROMAT research project, a collaboration with health researchers, ICT researchers, industrial partners, and adolescents (Nordgreen et al., 2021; Lamo et al., 2022). The study was a two-phased, four-armed randomized controlled trial (Figure 1), with each active phase lasting 3 weeks, including three active interventions and one waitlist control: 1) VRET + no additional intervention (VRET + NA) (n = 20), 2) VRET + online exposure program (VRET + online EXP) (n = 20), 3) online psychoeducation program + exposure program (online PE + EXP) (n = 40), or 4) waitlist (WL) (n = 20). For the first research question, the VRET groups were combined into one group and compared with online psychoeducation program and waitlist in phase one. For the second research question, VRET + online exposure program was compared to VRET + no additional intervention and online psychoeducational + online exposure program in phase two. Participants were assessed using self-report measures pre and post treatment, weekly during treatment phases, as well as at 3-month follow-up.
The study was approved by Regional Ethical Committee South-East (REK 60628) and was registered at Clinicaltrials.gov (NCT04396392). Informed consent was obtained at first login by both parents and adolescents younger than 16 years through a secure, digital platform, by using a secure, digital two-factor authentication signature, equivalent to those used in digital healthcare and bank services. Participants younger than 16 years old logged in via one of their parents. Adolescents aged 16 years logged in via their own, secure, digital two-factor authentication and signed informed consent without obtaining parental consent.
2.2 Participants
Adolescents were recruited from Bergen Municipality and surrounding areas. Information about the study was distributed via study website, school visits, e-mail, Facebook and Instagram profile, and posters. A collaboration with Bergen Municipality’s school health services was also established to facilitate the recruitment process. Inclusion criteria were: 1) Reporting symptoms of 55 or more on the self-reported Public Speaking Anxiety Scale (PSAS; Bartholomay and Houlihan, 2016), 2) answering yes to both questions “Are you afraid of speaking in front of your class?” and “Do you avoid speaking in front of your class if possible? 3) aged between 13–16 years old, 4) residing in Bergen Municipality, and 5) leaving contact information. Inclusion was automatically determined in the online screening. As no cut-off score exists for PSAS for Norwegian youth population, the cut-off score was determined by the previous feasibility and pilot study (Kahlon et al., 2019) by using the median score from the pre-assessment. Exclusion criteria were assessed in the phone interview: 1) reading difficulties, 2) balance and/or stereoscopic vision problems, 3) ongoing treatment for mental health disorders which could cause difficulties or extra burden for completing the training program.
2.3 Recruitment and screening
Adolescents were invited to the study by accessing the study website and filling out an online screening assessment. Eligible participants were then contacted by telephone within 1 week. A member of the study team conducted the phone interview with parents and/or the adolescents. During the phone interview, inclusion criteria were again assessed, and participants were asked to elaborate on the impact of PSA and had to confirm that their PSA resulted in avoidance behavior or interfered in their school functioning. A final decision regarding inclusion was made at the end of the phone interview. In case of inclusion uncertainty, the participants were discussed in a study team meeting and a final decision was made collectively.
Eligible participants were randomized to one of the four arms and given information about the group they had been allocated to during the same phone interview. For technical reasons, the randomization was conducted prior to the pre-assessment. After signing informed consent, the participants filled out the pre-assessments before starting the intervention.
All participants received weekly assessments in a period of 6 weeks and received a notification by text message/email when a new assessment had been assigned to them. For the post and follow-up measurements they also received an extra personalized message in order to increase adherence. To proceed to the next assessment, it was mandatory to answer each item, leaving no missing data at item level. Participants who filled out the post 2 and 3 months follow up assessments received two gift cards equivalent to 20 USD.
2.4 Interventions
The interventions were developed in collaboration with psychologists, psychology students and industry partners YouWell and Attensi. In the developmental process of the VR intervention, four adolescents provided initial ideas for the VR scenario, including design ideas for the classroom and the audience. Moreover, they tested the VR scenarios during the developmental phase and provided user feedback. Six adolescents did a usability test of all interventions in a fast-speed, 2-week period. Any bugs and errors with a negative impact on user experience were taken note of and adjusted before commencing recruitment. The user involvement was conducted by adolescents familiar to the research team and their peers. All of them had relatable experience to PSA occasionally.
2.4.1 Virtual Reality
The VR intervention was designed to be self-guided and used at home for 3 weeks, focusing on conducting speech exercises (exposure framed as training) in front of a virtual audience sitting in a classroom (see Figure 2 for VR application screenshots). Multiple components were included, enabling content variation in the form of audience mood, number of audience members, speech types and durations. The application included 15 predefined speech tasks, with a duration of 1–2 min per task, in addition to evaluation forms. Prior to each task, the participant received written instructions for the speech task (e.g., one of the speech task was to count down loud from 60 to 0), and had to select the most accurate statements among several regarding their catastrophic beliefs. After the task they answered the degree of anxiety experienced on a scale from 1 (no anxiety) to 100 (extreme anxiety), whether their catastrophic beliefs occurred or not and what they have learned from the task. The VR intervention included several gamification elements, including 1) levels (giving a sense of progression), 2) star rating and achievements when completing a level, 3) clear goals for each level, 4) performance feedback after completing a level, 5) varying difficulty for each level, 6) time constraints for each level, and 7) offering choices by setting up their own tasks (Hammady and Arnab, 2022).

FIGURE 2. Screenshot from the VR app ‘UngSpotlight’ adapted with permission from Attensi (2021). (A) Participant sitting by their desk and reading out loud from a text in English or Norwegian, (B) Participant standing in front of the audience and presenting, (C) Overview of the progression mode, which includes 15 predefined levels. (D) Overview of the practice mode where they can practice and construct their own exposure situations based on the same components in the progression mode.
The participants received a star rating, derived from predefined threshold levels based on speech performance and eye contact (indicated by head movement) with the virtual audience, A star rating 4 out of 5 was required to proceed to the next level. The predefined threshold levels were set by the research team through thorough testing of the virtual exposure tasks, including varying voice pitch and eye contact with the audience. Informed by user testing, final threshold levels were set based on clinical expertise and experience.
2.4.1.1 Procedure
As soon as the participants filled out the informed consent and the pre assessments, a member of the study team met with participants allocated to the VRET groups to hand out the VR-equipment, an Oculus Quest 1. In addition, the VRET groups received a handout with instructional text about the VR intervention and how to use the VR device. The group were told to do weekly training, at least three times a week or five exposure tasks weekly, estimated to approximately 30–60 min of weekly training. After 3 weeks of training, a member of the study team met with the participant or the parent of the participant again to collect the VR equipment. They were advised to contact a member of the study team by telephone in case they experienced any technical issues during the training period. There were no contact during the interventions unless initiated by the adolescents.
2.4.2 Online psychoeducation
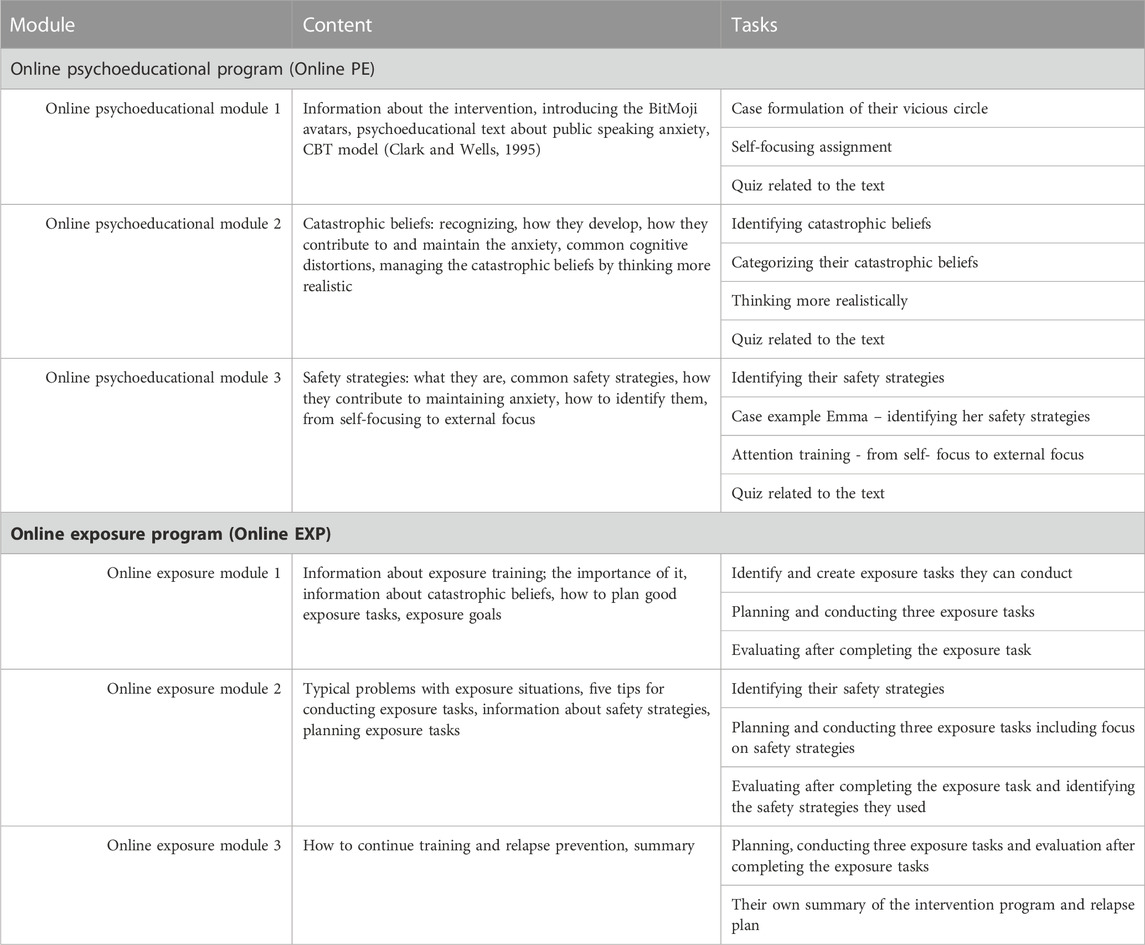
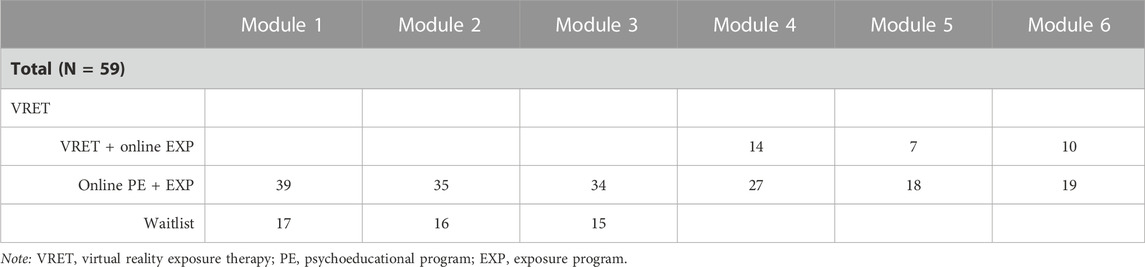
The online Psychoeducation (online PE) program included three Bitmoji avatars (Emma, Lucas, and Samira) who shared how they experienced their PSA with relatable examples. The avatars provided guidance in how to work with the online modules and the participants followed the avatars throughout the intervention. The online PE program included educative information about PSA, and CBT elements involved identifying their catastrophic beliefs and safety strategies and how they maintain their PSA. The online psychoeducation program did not encourage to conduct exposure tasks, but only educated the adolescents about how catastrophic beliefs and safety strategies/avoidance behavior can maintain their anxiety level. See Table 1 for overview of the modules.
2.4.2.1 Procedure
The participants received access to the online PE program within a few days after the phone interview, immediately after providing informed consent and completing the pre assessment. The intervention lasted for 3 weeks, with one short text module assigned weekly with a notification on SMS or e-mail. In addition, they received notifications every 4 days if they remained inactive. They were advised to complete one module per week. Participants were informed that it would take approximately 30–60 min to read each module and complete the assignments.
2.4.3 Online exposure program
The online exposure program (online EXP) focused on how to do exposure training and how to create good in vivo exposure tasks, including typical problems one might encounter with exposure situations. They were advised to plan each exposure task as specific as possible using SMART goal criteria (Bovend'Eerdt et al., 2009): Specific, Measurable, Achievable, Relevant, and Time-bound. Participants were encouraged to do weekly exposure training related to public speaking situations. The program provided the participants with some examples of exposure tasks, e.g., asking a question in the classroom when knowing/not knowing the answer, reading out loud in the classroom, volunteer as group leader in a school project and lead a group discussion. Each exposure task included filling out planning and evaluation forms. When planning an exposure task, participants had to write what they were going to do, when they were going to do it (day and time), their catastrophic beliefs related to the exposure task, how they were going to notice whether their catastrophic beliefs occur, and the likelihood of their catastrophic beliefs occurring. The evaluation form included questions regarding whether their catastrophic beliefs occurred, how they could notice it, whether they used safety strategies and what they had learned. The respective forms were based on the inhibitory learning model focusing on disproving catastrophic beliefs (Craske et al., 2008). At the end of the online exposure program, they received an introduction on how to continue their training and relapse prevention. The participants followed the same Bitmoji avatars as in the online PE. See Table 1 for overview of the modules.
2.4.3.1 Procedure
Allocated participants began the online exposure program in phase two. The intervention lasted for 3 weeks, and one text module was assigned weekly. They were advised to complete one module per week. It would take approximately 30–60 min to read each module and complete the assignments. Moreover, they were advised to conduct at least three public speaking related exposure tasks per week. The participants received notifications in the same manner as in the online PE.
2.4.4 Waitlist
No intervention was provided during the first 3 weeks of the waitlist period. Those in the waitlist group received access to the online psychoeducation program after 3 weeks.
2.5 Measures
2.5.1 Primary outcome measure
Public Speaking Anxiety Scale (PSAS; Bartholomay and Houlihan, 2016) is a 17-items questionnaire, measuring symptoms of PSA on a 5-point Likert Scale, ranging from 1 (not at all) to 5 (extremely). The scale covers behavioral, cognitive, and physiological aspects of PSA, and was originally developed for adults. However, user testing with adolescents did not present any misinterpretations of the scale and it performed well in previous research (Kahlon et al., 2019). Internal consistency at screening was a satisfactory α = 0.76.
2.5.2 Secondary outcome measure
The self-rated Social Interaction Anxiety Scale (SIAS) 6-item, and the Social Phobia Scale (SPS) 6-item is validated (Peters et al., 2012) and measure social interaction and performance anxiety (respectively), both with a 0–4 item response format. Internal consistency at screening was α = 0.84 for the SIAS-6 and α = 0.90 for the SPS-6.
2.5.3 Clinically significant improvement and deterioration
There is little evidence regarding deterioration rates in Virtual Reality interventions. Few studies investigate symptoms of deterioration in treatment, and majority of the evidence relies on results from face-to-face treatment (Fernández-Álvarez et al., 2019). However, an individual patient data meta-analysis from both VR studies (Fernández-Álvarez et al., 2019) and internet guided treatment (Karyotaki et al., 2018) showed that both treatment approaches have lower deterioration rates than waitlist control.
In the current study, reliable change index was calculated for the primary outcome measure PSAS by the formula
where〖SE〗_diff is the standard error for pre-treatment, S_ks is the standard deviation and r is the reliability coefficient. A score difference of +10 was categorized as a significant positive change, and a score of −10 was categorized as a significant deterioration.
2.6 Sample size
Sample size was calculated and determined a priori by using mixed effects model power calculation (Magnusson, 2018). Power in phase one, corresponding to the first research questions, was used to guide sample size calculations. In phase one, two contrasts were of a priori interest, with different presumed between-group effect sizes. Sample sizes were adjusted accordingly: VRET vs. waiting list, and VRET vs. online psychoeducation. The contrast VRET (n = 40) vs. waiting list (n = 20) provided 82% power to detect a symptom trajectory difference corresponding to Cohen’s d > 0.8, assuming an ICC of 0.6, a variance ratio of 0.02, and cumulative dropout rates of 20% in the VRET arm and 30% in the waitlist arm. The study expected to find large differences between VRET vs. waitlist based on the extant VRET literature (Carl et al., 2019; Meyerbröker and Morina, 2021; Reeves et al., 2021), including an assumption of little spontaneous symptom reduction in the waitlist arm (Patterson et al., 2016). Based on this, a smaller sample size was required for the waitlist group, as done in other studies (Schuurmans et al., 2006; Berger et al., 2009). A higher dropout rate was also expected for the waitlist, as the VR intervention was believed to be more appealing. The contrast VRET (n = 40) vs. online psychoeducation (n = 40) provided 79% power to detect a Cohen’s d > 0.60 (with an assumption of 20% dropout in both arms), which was deemed satisfactory due to the complexities of powering an advanced study design.
2.7 Randomization
The randomization was generated via the website randomization.org using a block randomization strategy, with 10 participants in each block, which randomly assigned the participants to the four groups. Block randomization strategy ensured that the sample size in each group was kept equal over time.
2.8 Statistical analyses
A chi-square test for gender and ANOVA tests for age, and outcome measures were conducted in order to investigate group differences pre-treatment. In addition, the VRET groups were compared to each other using the same analysis.
Outcomes were examined according to the intention-to-treat principle, using linear mixed effect models. Analyses included a numeric (sequential) time predictor and were separated by phase: in phase one, the two VRET arms were collapsed into one (since they received the exact same intervention), which served as reference for pairwise model contrasts. In phase two, all four arms were included, with VRET + online EXP serving as reference. Within-group effect sizes were calculated by the formula (M1 –M2)/SD1. Between effect sizes were calculated by (Mgroup1 – Mgroup2)/SD Pooled. As the data were assumed to be missing at random, effect sizes were calculated based on observed data.
3 Results
3.1 Participants and adherence
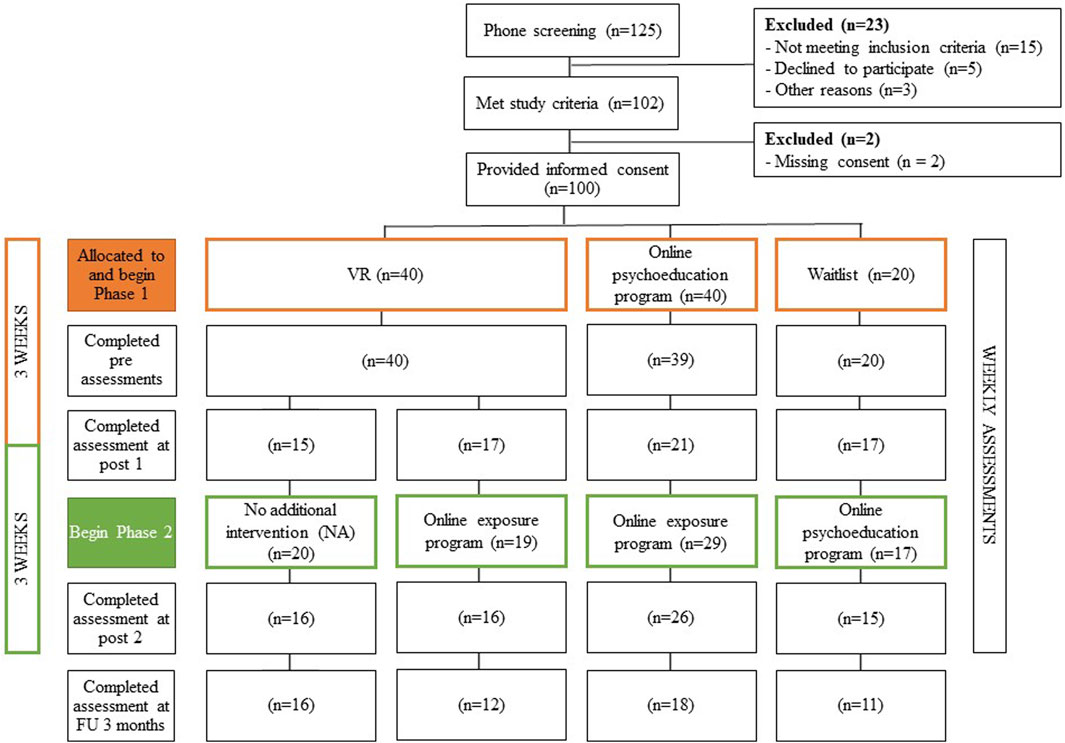
The recruitment window covered approximately 7 months and started 7th September 2020 and the last participant was enrolled on 15 March 2021. During this period, COVID-19 restrictions were in effect in Norway. A total of 253 accessed the online survey, whereas 59 adolescents did not leave their contact information. See Figure 3 for study flowchart. In the total sample of 100 adolescents, 16 were males and 84 females, with an average age of 14.2 years (SD = 0.99). See Table 2 for more sample characteristics and Tables 3, 4 for observed means, standard deviations and n missing at each time point for phase one and phase two.
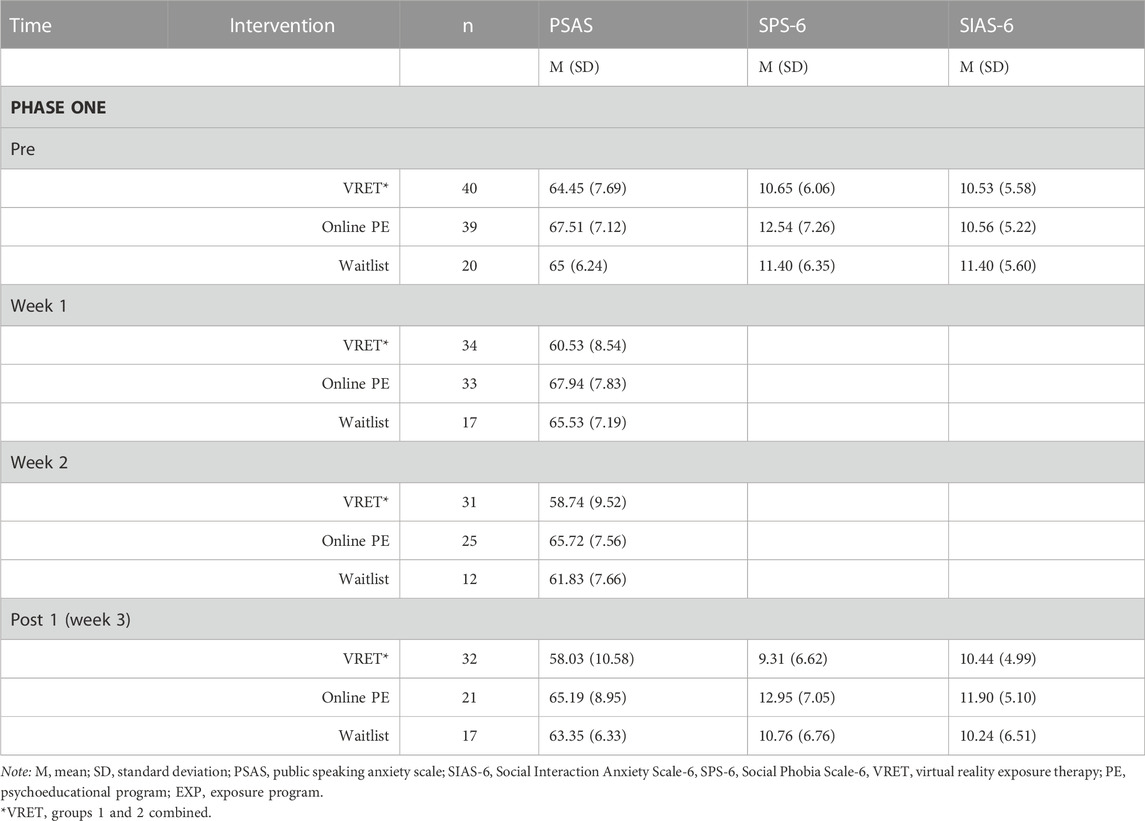
TABLE 3. Observed means, standard deviations and n missing for primary and secondary outcome measure in phase one from pre to post 1.
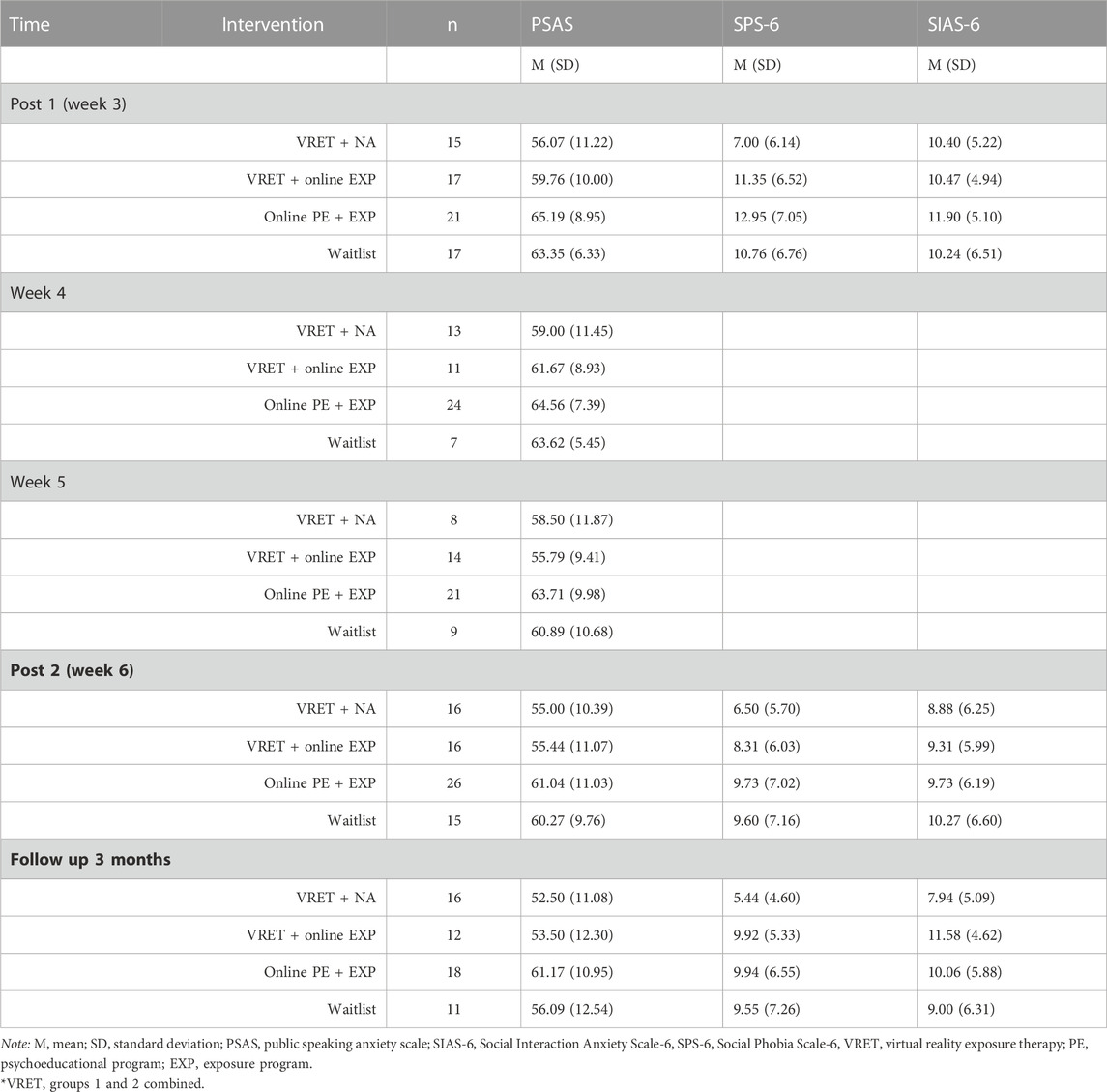
TABLE 4. Observed means, standard deviations and n missing for primary and secondary outcome measure in phase two from post 1 (baseline) to post 2, and follow up 3 months.
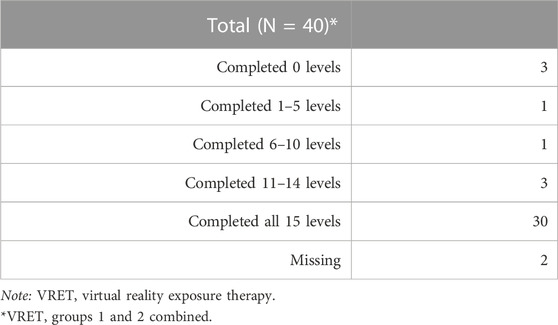
Adherence in VRET groups combined was high, with 75% completing all 15 levels, and 50% of the participants in the VRET + online EXP group completing all three modules in the online exposure program. Around 49% of the participants in the online PE + EXP group completed all six modules. Waitlist group also had a high adherence to the online psychoeducation program with 75% of the participants completing all three modules. See Tables 5, 6 for adherence to the interventions.
3.2 Randomization
No significant differences between the four groups were identified at pre-intervention with regards to gender (x2 (1) = 1.042, p = 0.791), age (F (3, 96) = 0.987, p = 0.402)), PSAS (F (3, 95) = 1.354, p = 0.262), SPS (F (3, 95) = 0.732, p = 0.535), or SIAS scores (F (3, 95) = 0.133, p = 0.940). The two VRET arms were combined in phase one as both groups received the exact same intervention. When comparing the VRET arms with each other, no significant differences were identified at pre-measurement in gender (x2 (1) = 0.00, p = 1.00), nor age (t (38) = 1.657, p = 0.106), PSAS (t (38) = 0.448, p = 0.657), SPS (t (38) = −0.831, p = 0.411), or SIAS scores (t (38) = 0.084, p = 0.934).
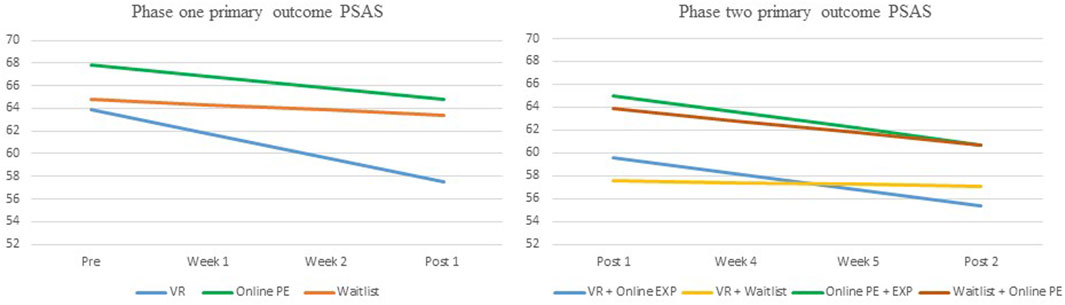
3.3 Is virtual reality exposure therapy (VRET) more efficacious than waitlist and online psychoeducation?
The linear mixed model analysis revealed a significant reduction for the VRET arms combined on the primary outcome measure PSAS with an average of 2.14 points reduction per week during the 3-week intervention period (95% CI = −2.92 ─ −1.37, p < 0.001), and a large within-group effect size of d = 0.83. The VRET arms had a significantly greater reduction in PSAS scores compared to the waiting list arm (95% CI VRET vs WL = 0.34 ─ 3.02, p = 0.015), with a moderate between effect size d = 0.61. Reduction in PSAS over time was not statistically significant different from the online PE arm (95% CI = −0.03 – −2.29, p = 0.06) (Table 7; Figure 4). However, the online PE arm yielded a smaller within group-effect size of d = 0.33.
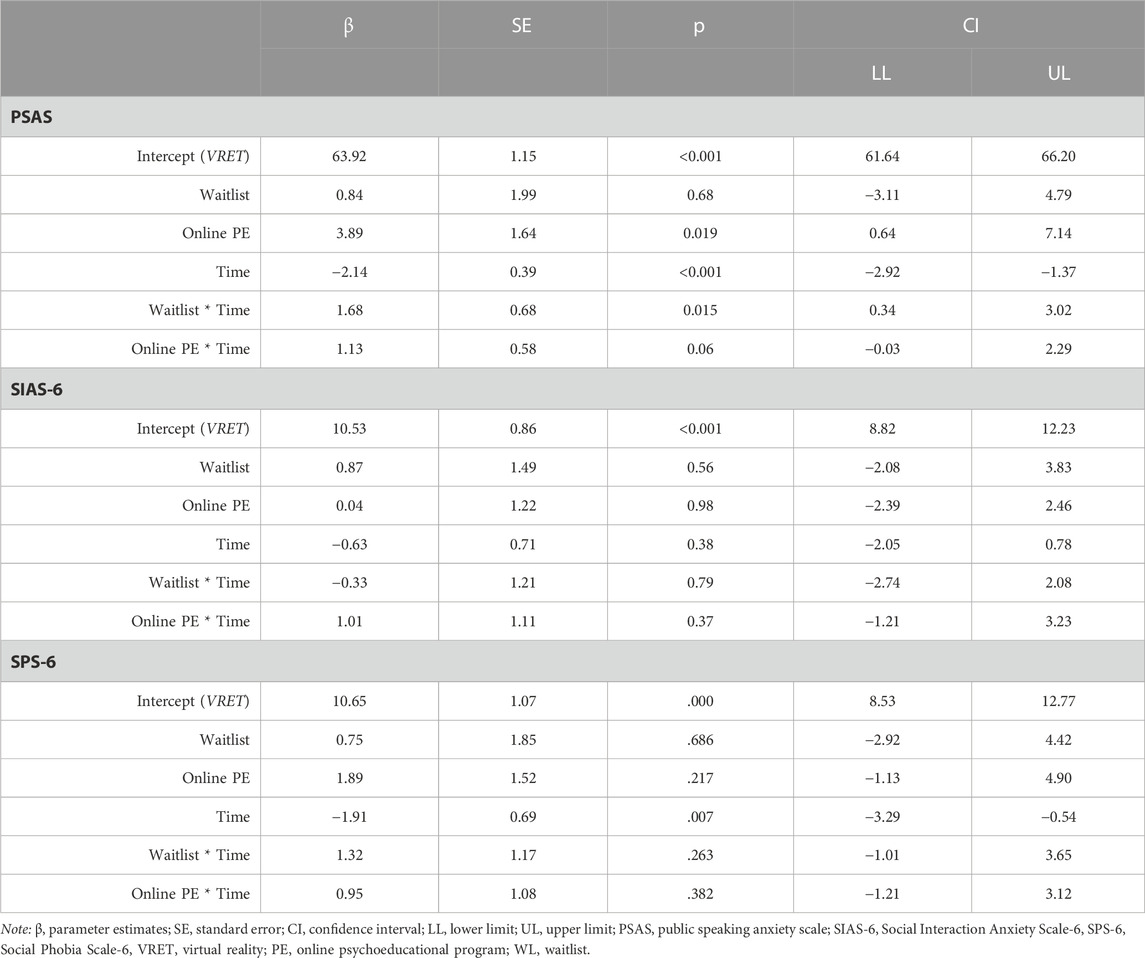
TABLE 7. Linear mixed models’ analysis for Phase one from pre to post 1: VRET vs. 1) online PE and 2) Waitlist.
Linear mixed modeling of secondary outcome measure SPS-6 revealed a significant reduction for the VRET arms combined with 1.91 points reduction per week during the intervention period (95% CI = −3.29 ─ −0.54, p = 0.007) and a small within-group effect size of d = 0.22. There were no statistically significant group differences. Linear mixed modelling of the secondary outcome measure SIAS-6 showed no reduction over time for the VRET arms, nor any group differences (See Table 7).
3.4 Is a combination of VRET + online exposure therapy more efficacious than VRET alone or online psychoeducation and online exposure program?
The linear mixed model analysis revealed a significant reduction for the VRET + online EXP arm on the primary outcome measure PSAS, with an average of 1.42 points reduction per week during the intervention period (95% CI = −2.53 ─ −0.31, p = 0.013) and a small within-group effect size d = 0.43. The linear mixed model analysis revealed no statistically significant group differences (see Table 8; Figure 4).
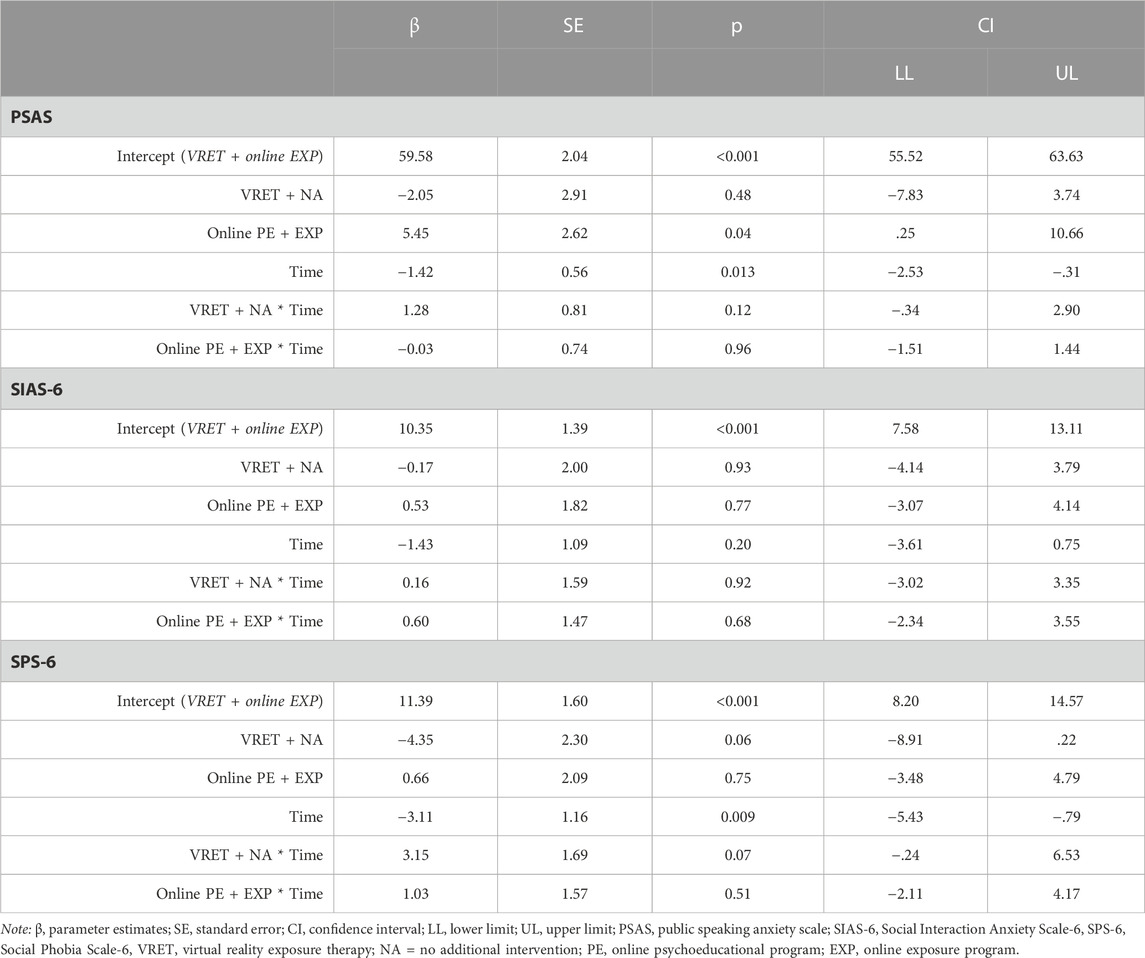
TABLE 8. Linear mixed models’ analysis for Phase two from post 1 (baseline) to post 2: VRET + online EXP vs. 1) VRET + NA, and 2) online PE + EXP.
Linear mixed modeling of secondary outcome measure SPS-6 showed a significant reduction for the VRET + online EXP arm with 3.11 points reduction during the intervention period (95% CI = −5.43 ─ −0.79, p = 0.009), and a small within-group effect size of d = 0.36. There were no significant group differences. The results showed no significant reduction on the secondary outcome measure SIAS-6 for the VRET + online EXP arm, nor any group differences (See Table 8).
3.5 Improvement and deterioration
During phase one, 11 out of 32 (28%) respondents in the VRET groups combined, and 5 out of 16 (31%) respondents in the online PE group reported a clinical reliable change on the primary outcome PSAS. The difference in reliable change between these two groups was not significant, X2 (1, N = 53) = 0.672, p = .41. The remaining participants remained unchanged. All respondents (n = 17) in the waitlist arm remained stable in symptoms during phase one (See Table 9).
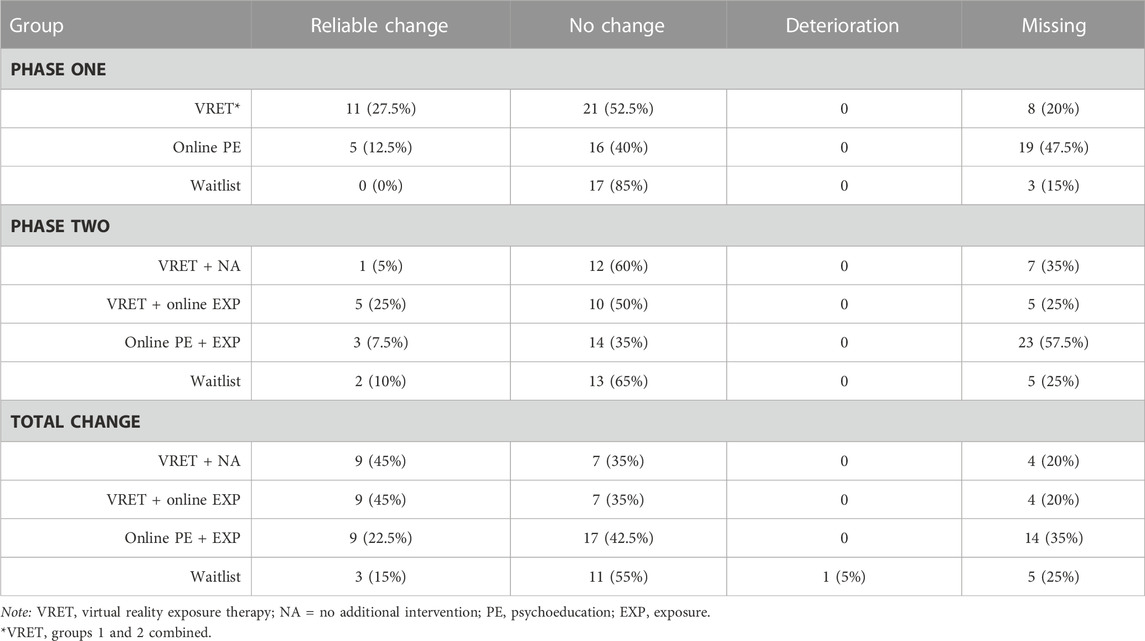
TABLE 9. Clinical reliable change in symptoms on the primary outcome measure Public Speaking Anxiety Scale (PSAS) for Phase one, Phase two and Total Change from pre-intervention to post 2-intervention.
During phase two, 5 out of 15 (33%) of the respondents in the VRET + online EXP group, and 3 out of 17 (18%) respondents in the online PE + EXP group reported a clinical reliable change. The difference in reliable change between these two groups was not significant X2 (1, N = 32) = 1.046, p = .31. None of the participants reported deterioration following the interventions in phase two (See Table 9).
3.6 Long-term results
The linear mixed model (random intercept only) analysis for long term results revealed a non-significant change in PSAS score of −2.80 points from post 2–3 months follow up measurement for the VRET + online EXP (95% CI = −7.17 ─ 1.57, p = 0.205). The analysis did not show any time*group interaction effects for online PE + EXP (95% CI VRET+EXP vs PE+EXP = −3.59 ─ 7.77, p = 0.464), VRET + NA (95% CIVRET+EXP vs VRET+NA = −4.57 ─ 7.19, p = 0.657), nor for waitlist (95% CIVRET+EXP vs WL+PE = −8.02 ─ 4.83, p = 0.621).
The linear mixed model on the secondary outcome SPS-6 did not reveal a significant reduction in PSAS for VRET + online EXP (95% CI = −1.26 ─ 4.44, p = 0.27), nor any time*group interaction effects for online PE + EXP (95% CI VRET+EXP vs PE+EXP = −5.06 ─ 2.35, p = 0.47), VRET + NA (95% CIVRET+EXP vs VRET+NA = −5.78 ─ 1.91, p = 0.32), and waitlist (95% CIVRET+EXP vs WL+PE = −6.87─ 1.50, p = 0.20).
The results revealed no significant reduction in symptoms on the secondary outcome SIAS-6 for VRET + online EXP (95% CI = −0.56 ─ 4.34, p = 0.13). The analysis did however find a significant higher reduction in symptoms for the waitlist group compared with VRET + online EXP (95% CIVRET+EXP vs WL+PE = −7.29 ─ −.0.09, p = 0.045). The interaction effects time*group for online PE + EXP (95% CI VRET+EXP vs PE+EXP = −5.92 ─ 0.45, p = 0.09) and VRET + NA (95% CIVRET+EXP vs VRET+NA = −5.84 ─ 0.76, p = 0.13) was not significant.
Univariate analysis of variance did not identify any between-group differences at the 3 months follow up on the PSAS (p = 0.424), SPS-6 (p = 0.772), or SIAS-6 (p = 0.544).
4 Discussion
To our knowledge, this is the first randomized trial of an automated, gamified VR intervention for public speaking anxiety (PSA) for adolescents, with comparison to both a waiting-list control and another technological-delivered intervention.
The first research question investigated whether VRET was more efficacious when compared to 1) waitlist group, and 2) online psychoeducational program. The results showed that the VRET group had a significantly greater reduction in PSA symptoms compared with the waitlist group. The results are congruent with a recent VRET study on children demonstrating that VRET was more efficacious when compared to a control condition who practiced on their public speaking skills as usual (Sülter et al., 2022), as well as a meta-analysis which concluded that VRET interventions targeting PSA were more efficacious than waitlist (Reeves et al., 2021). Moreover, our results replicate studies conducted on adults and adolescents with PSA showing that self-guided VRET intervention is efficacious in reducing PSA symptoms (Lindner et al., 2019; Premkumar et al., 2021; Zainal et al., 2021; Valls-Ratés et al., 2022). However, contrary to our expectations, the results from the study showed that there was no significant difference in symptom reduction when comparing VRET against online psychoeducation. A meta-analysis found that psychoeducational interventions can be efficacious in reducing symptoms of anxiety, however, with smaller effect sizes (Donker et al., 2009). This is also found in the current study as VRET yielded a large within-group effect size d = 0.83, whereas the online psychoeducation yielded a smaller within-group effect size of d = 0.33. Thus, VRET has more practical implications compared to online psychoeducation program, which should be considered when targeting adolescents with PSA.
The second research question investigated whether VRET followed by online exposure program is more efficacious than VRET alone or online psychoeducation + exposure program. The results showed that VRET + online exposure program was not statistically significant different when compared with VRET + no additional intervention and online psychoeducation + exposure program. However, all groups had a significant decrease in PSA symptoms over time. Moreover, treatment effects remained stable at 3-month follow-up for all groups. One reason for the non-significant difference between the groups may be due to COVID-19. COVID-19 pandemic was in effect during the recruitment period, leading to home-schooling, lockdowns, and quarantines, thus resulting in a decreased social contact. This may have affected their exposure opportunities and resulted in less exposure training during the online exposure program. Future studies should therefore continue to investigate whether VRET as a stand-alone intervention is equally efficacious as VRET together with another intervention focusing on real life exposure. Of note, the trial was primarily powered to detect difference between VRET and waitlist or online psychoeducation in phase one. The results of phase two comparing VRET + online exposure program against the other intervention groups should therefore be considered as exploratory as there may be a type II error involved. Nevertheless, these results may be comparable to other studies comparing VRET with in vivo control groups (Carl et al., 2019; Horigome et al., 2020; Reeves et al., 2021). A meta-analysis also found no significant differences when comparing VRET against other treatment methods (Lim et al., 2022). However, as there is limited evidence on VRET compared with other active intervention groups on adolescents, more studies are still needed to conclude on its efficacy compared to other intervention modalities in this target group with sufficient powered design.
The results also showed that the active control group online psychoeducation + exposure program was efficacious in reducing PSA symptoms with no significant difference in clinical reliable improvement when compared with the group receiving VRET + online exposure program. This provides an opportunity to deliver different intervention modalities based on the adolescents’ preferences. More research on VRET using active comparison arms, including non-inferiority trials (Miloff et al., 2019), is required to elucidate what intervention works for what patient group. Moreover, more studies investigating the efficacy of automated, gamified VR intervention compared to other intervention modalities for adolescents are still needed.
All groups had a reduction in social phobia symptoms, measured by the Social Phobia Scale (SPS; Mattick and Clarke, 1998). SPS measure social fears while being at center of attention, such as eating in front of other, performing in front of people (Mattick and Clarke, 1998), thus capturing the performance only subtype of SAD (American Psychiatric Association, 2013). Thus, there may be due to a slight overlap in measurement construct between the Public Speaking Anxiety Scale (PSAS; Bartholomay and Houlihan, 2016), and SPS (Mattick and Clarke, 1998) as both measure performance related fears.
Even though the main purpose of the present study was to recruit adolescents with performance anxiety, we also wished to explore whether intervening on PSA had a spillover effect on social interaction anxiety symptoms. This has been reported by previous studies (i.e., Hindo and González-Prendes, 2011; Hofmann et al., 2006). The adolescents in this study did, however, not report any reduction in social interaction anxiety symptoms from pre to post intervention. To promote improvement related to social interaction symptoms, the VRET intervention would benefit by including interaction elements, and the online exposure program should encourage the adolescent to expose themselves to various social interaction situations. Moreover, a longer follow-up assessment is also needed to identify potential preventive effects for developing generalized SAD.
The participants receiving VRET had a high adherence to the intervention, with 75% of the participants completing all 15 levels. The gamification elements, combined with the playful elements of VR itself may have contributed to a higher treatment uptake, as reported by other studies (Freeman et al., 2018; Goldenhersch et al., 2020; De Croon et al., 2021). A lower adherence was identified for the online PE + EXP group with 49% of the participants completing all six modules during the intervention period. Of note, the participants had access to the online psychoeducation and exposure programs during the follow-up assessment period. Some of the participants completed the modules following the 6 weeks intervention period, however, these data were not included.
4.1 Strength and limitations
The current study addresses key gaps in extant literature on VRET for adolescents, being the first randomized controlled study investigating VRET for adolescents with PSA in an Applied Games format, compared with waitlist and another technology-delivered intervention. Strengths include both passive and active control groups and a comparatively large sample size. Several limitations nonetheless apply. First, during the recruitment period, COVID-19 pandemic-related quarantine measures like homeschooling and lockdowns were in-effect. This varied across time and locations and may have affected the results of the study: by not being able to attend school, some might have experienced difficulties in conducting exposure training and practicing skills they have learned throughout the program. Originally, power calculations were made for both phases, resulting in a sample size of N = 160. However, due to covid-19 pandemic and recruitment delays, the sample size was reduced to N = 100, resulting in an underpowered phase two when comparing VRET + online exposure programs against the other intervention groups. These results therefore need to be interpreted with caution. Another limitation is that pre-treatment measures were collected after informing the adolescents about allocation. This could have had resulted in a bias, yet after careful consideration, this procedure was deemed inevitable due to technological factors which could otherwise have led to a participant confusion and increased attrition. Importantly, no group differences were observed at pre-assessment. A third limitation is that the data only relies on self-report measurements. Future studies should also include other assessments methods such as behavioral approach tests or physiological measurements. And fourth, the sample consists of a higher range of girls, which may affect the generalizability of the results.
4.2 Clinical implications
Clinical implications of the current study include demonstrating the potential of a scalable, self-guided VR intervention for adolescents with PSA. The intervention may serve as a stepwise treatment as self-guided as a first step, and those not benefiting from this solely may receive the intervention as part of a therapist-guided intervention as done in the previous feasibility study (Kahlon et al., 2019). The online psychoeducation and exposure program have a higher dissemination potential and is also more cost-effective. This is apparent as the online programs have now been implemented and is nationally available.
A barrier to scalability is the costs related to the development of VR exposure scenarios. Moreover, VR hardware and software is still expensive for the individual use, making it unaffordable for low-income countries, and may also be a barrier for individuals living in high-income countries (Morina et al., 2021). Thus, there is a need to continue to develop efficacious interventions and target adolescents with PSA through other modalities which can be implemented in both low and high-income countries, as well as to continue to explore its clinical efficacy on adolescents before implementation.
4.3 Conclusion
The study has explored the potential of utilizing VRET as a self-guided, automated, and gamified intervention to reduce PSA among adolescents and shows promising results. Future studies should continue investigating the efficacy of VR-based interventions for adolescents with PSA.
Data availability statement
The raw data supporting the conclusion of this article will be made available by the authors, without undue reservation.
Ethics statement
The study involving humans were approved by Regional Ethical Committee South-East. The study were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants or participants’ legal guardians/next of kin.
Author contributions
SK assessed and treated the participants, collected and prepared the data, and drafted the manuscript. The manuscript was revised in collaboration with PL and TN who also assisted with the analyses and interpretation of results. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Norwegian Research Council (NFR grant no 259293).
Acknowledgments
Anne Synnøve Thomassen and Pia Rygg Hauge contributed with the data collection. We acknowledge the work that has been done by the psychology students and industry partners who were involved in the development of the interventions and the adolescents who have contributed to the research.
Conflict of interest
PL has consulted for VR developer Mimerse, a company which has since seized operations. SK and PL receive minor royalties from sales of a textbook that includes a chapter on clinical VR use.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
American Psychiatric Association, (2013). Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC, USA, American Psychiatric Publishing.
Anderson, P. L., Edwards, S. M., and Goodnight, J. R. (2017). Virtual reality and exposure group therapy for social anxiety disorder: results from a 4–6 Year follow-up. Cognitive Ther. Res. 41 (2), 230–236. doi:10.1007/s10608-016-9820-y
Bartholomay, E. M., and Houlihan, D. D. (2016). Public speaking anxiety scale: preliminary psychometric data and scale validation. Personality Individ. Differ. 94, 211–215. doi:10.1016/j.paid.2016.01.026
Berger, T., Hohl, E., and Caspar, F. (2009). Internet-based treatment for social phobia: A randomized controlled trial. J. Clin. Psychol. 65 (10), 1021–1035. doi:10.1002/jclp.20603
Blöte, A. W., Kint, M. J., Miers, A. C., and Westenberg, P. M. (2009). The relation between public speaking anxiety and social anxiety: A review. J. Anxiety Disord. 23 (3), 305–313. doi:10.1016/j.janxdis.2008.11.007
Bovend'Eerdt, T. J., Botell, R. E., and Wade, D. T. (2009). Writing SMART rehabilitation goals and achieving goal attainment scaling: A practical guide. Clin. Rehabil. 23 (4), 352–361. doi:10.1177/0269215508101741
Brivio, E., Serino, S., Cousa, E. N., Zini, A., Riva, G., and De Leo, G. (2021). Virtual reality and 360° panorama technology: A media comparison to study changes in sense of presence, anxiety, and positive emotions. Virtual Real. 25 (2), 303–311. doi:10.1007/s10055-020-00453-7
Carl, E., Stein, A. T., Levihn-Coon, A., Pogue, J. R., Rothbaum, B., Emmelkamp, P., et al. (2019). Virtual reality exposure therapy for anxiety and related disorders: A meta-analysis of randomized controlled trials. J. Anxiety Disord. 61, 27–36. doi:10.1016/j.janxdis.2018.08.003
Clark, D. M., and Wells, A. (1995). “A cognitive model of social phobia,” in Social phobia: Diagnosis, assessment, and treatment. Editors R. G. Heimberg, M. R. Liebowitz, D. A. Hope, and F. R. Schneier (New York, NY, USA, The Guilford Press), 69–93.
Conley, C. S., Raposa, E. B., Bartolotta, K., Broner, S. E., Hareli, M., Forbes, N., et al. (2022). The impact of mobile technology-delivered interventions on youth well-being: systematic review and 3-level meta-analysis. JMIR Ment. Health 9 (7), e34254. doi:10.2196/34254
Craske, M. G., Kircanski, K., Zelikowsky, M., Mystkowski, J., Chowdhury, N., and Baker, A. (2008). Optimizing inhibitory learning during exposure therapy. Behav. Res. Ther. 46 (1), 5–27. doi:10.1016/j.brat.2007.10.003
De Croon, R., Geuens, J., Verbert, K., and Vanden Abeele, V. (2021). “A systematic review of the effect of gamification on adherence across disciplines,” in HCI in games: Experience design and game mechanics (Berlin, Germany: Springer).
Donker, T., Griffiths, K. M., Cuijpers, P., and Christensen, H. (2009). Psychoeducation for depression, anxiety and psychological distress: A meta-analysis. BMC Med. 7 (1), 79. doi:10.1186/1741-7015-7-79
Ebrahimi, O. V., Pallesen, S., Kenter, R. M. F., and Nordgreen, T. (2019). Psychological interventions for the fear of public speaking: A meta-analysis. Front. Psychol. 10 (488), 488. doi:10.3389/fpsyg.2019.00488
Essau, C. A., Lewinsohn, P. M., Olaya, B., and Seeley, J. R. (2014). Anxiety disorders in adolescents and psychosocial outcomes at age 30. J. Affect. Disord. 163, 125–132. doi:10.1016/j.jad.2013.12.033
Fernández-Álvarez, J., Rozental, A., Carlbring, P., Colombo, D., Riva, G., Anderson, P. L., et al. (2019). Deterioration rates in Virtual Reality Therapy: an individual patient data level meta-analysis. J. Anxiety Disord. 61, 3–17. doi:10.1016/j.janxdis.2018.06.005
Ferreira Marinho, A. C., Mesquita de Medeiros, A., Côrtes Gama, A. C., and Caldas Teixeira, L. (2017). Fear of public speaking: perception of college students and correlates. J. Voice 31 (1), 127.e7–127.e11. doi:10.1016/j.jvoice.2015.12.012
Fleming, T. M., Bavin, L., Stasiak, K., Hermansson-Webb, E., Merry, S. N., Cheek, C., et al. (2017). Serious games and gamification for mental health: current status and promising directions. Front. psychiatry 7, 215. doi:10.3389/fpsyt.2016.00215
Freeman, D., Haselton, P., Freeman, J., Spanlang, B., Kishore, S., Albery, E., et al. (2018). Automated psychological therapy using immersive virtual reality for treatment of fear of heights: A single-blind, parallel-group, randomised controlled trial. Lancet Psychiatry 5 (8), 625–632. doi:10.1016/S2215-0366(18)30226-8
Goldenhersch, E., Thrul, J., Ungaretti, J., Rosencovich, N., Waitman, C., and Ceberio, M. R. (2020). Virtual reality smartphone-based intervention for smoking cessation: pilot randomized controlled trial on initial clinical efficacy and adherence. J. Med. Internet Res. 22 (7), e17571. doi:10.2196/17571
Grant, B. F., Hasin, D. S., Blanco, C., Stinson, F. S., Chou, S. P., Goldstein, R. B., et al. (2005). The epidemiology of social anxiety disorder in the United States: results from the national epidemiologic survey on alcohol and related conditions. J. Clin. Psychiatry 66 (11), 1351–1361. doi:10.4088/jcp.v66n1102
Gutiérrez-Maldonado, J., Magallón-Neri, E., Rus-Calafell, M., and Peñaloza, C. (2009). Virtual reality exposure therapy for school phobia. Anu. Psicol. 40 (2), 223–236.
Halldorsson, B., Hill, C., Waite, P., Partridge, K., Freeman, D., and Creswell, C. (2021). Annual research review: immersive virtual reality and digital applied gaming interventions for the treatment of mental health problems in children and young people: the need for rigorous treatment development and clinical evaluation. J. Child Psychol. Psychiatry 62 (5), 584–605. doi:10.1111/jcpp.13400
Hammady, R., and Arnab, S. (2022). Serious gaming for behaviour change: A systematic review. Information 13 (3), 142. https://www.mdpi.com/2078-2489/13/3/142. doi:10.3390/info13030142
Hindo, C. S., and González-Prendes, A. A. (2011). One-session exposure treatment for social anxiety with specific fear of public speaking. Res. Soc. Work Pract. 21 (5), 528–538. doi:10.1177/1049731510393984
Hofmann, S. G., Schulz, S. M., Meuret, A. E., Moscovitch, D. A., and Suvak, M. (2006). Sudden gains during therapy of social phobia. J. Consult. Clin. Psychol. 74 (4), 687–697. doi:10.1037/0022-006X.74.4.687
Horigome, T., Kurokawa, S., Sawada, K., Kudo, S., Shiga, K., Mimura, M., et al. (2020). Virtual reality exposure therapy for social anxiety disorder: A systematic review and meta-analysis. Psychol. Med. 50 (15), 2487–2497. doi:10.1017/S0033291720003785
Kahlon, S., Lindner, P., and Nordgreen, T. (2019). Virtual reality exposure therapy for adolescents with fear of public speaking: A non-randomized feasibility and pilot study. Child Adolesc. psychiatry Ment. health 13, 47. doi:10.1186/s13034-019-0307-y
Karyotaki, E., Kemmeren, L., Riper, H., Twisk, J., Hoogendoorn, A., Kleiboer, A., et al. (2018). Is self-guided internet-based cognitive behavioural therapy (iCBT) harmful? An individual participant data meta-analysis. Psychol. Med. 48 (15), 2456–2466. doi:10.1017/S0033291718000648
Kothgassner, O. D., and Felnhofer, A. (2020). Lack of research on efficacy of virtual reality exposure therapy (VRET) for anxiety disorders in children and adolescents: A systematic review. Neuropsychiatrie 35 (2), 68–75. doi:10.1007/s40211-020-00349-7
Lamo, Y., Mukhiya, S. K., Rabbi, F., Aminifar, A., Lillehaug, S. I., Tørresen, J., et al. (2022). Towards adaptive technology in routine mental health care. Digit. HEALTH 8, 205520762211286. doi:10.1177/20552076221128678
Lim, M. H., Aryadoust, V., and Esposito, G. (2022). A meta-analysis of the effect of virtual reality on reducing public speaking anxiety. Curr. Psychol. 42, 12912–12928. doi:10.1007/s12144-021-02684-6
Lindner, P. (2020). Better, virtually: the past, present, and future of virtual reality cognitive behavior therapy. Int. J. Cognitive Ther. 14, 23–46. doi:10.1007/s41811-020-00090-7
Lindner, P., Miloff, A., Fagernas, S., Andersen, J., Sigeman, M., Andersson, G., et al. (2019). Therapist-led and self-led one-session virtual reality exposure therapy for public speaking anxiety with consumer hardware and software: A randomized controlled trial. J. Anxiety Disord. 61, 45–54. doi:10.1016/j.janxdis.2018.07.003
Lindner, P., Rozental, A., Jurell, A., Reuterskiold, L., Andersson, G., Hamilton, W., et al. (2020). Experiences of gamified and automated virtual reality exposure therapy for spider phobia: qualitative study. JMIR Serious Games 8 (2), e17807. doi:10.2196/17807
Magnusson, K. (2018). Powerlmm: power analysis for longitudinal multilevel models. R package version 0.4.0. Available at: https://cran.r-project.org/src/contrib/Archive/powerlmm/.
Mattick, R. P., and Clarke, J. C. (1998). Development and validation of measures of social phobia scrutiny fear and social interaction anxiety11Editor’s note: this article was written before the development of some contemporary measures of social phobia, such as the Social Phobia and Anxiety Inventory (Turner et al., 1989). We have invited this article for publication because of the growing interest in the scales described therein. S.T. Behav. Res. Ther. 36 (4), 455–470. doi:10.1016/S0005-7967(97)10031-6
Mekler, E. D., Brühlmann, F., Opwis, K., and Tuch, A. N. (2013). “Do points, levels and leaderboards harm intrinsic motivation? An empirical analysis of common gamification elements,” in Proceedings of the First International Conference on Gameful Design, Research, and Applications, October 2013, Toronto, Canada. doi:10.1145/2583008.2583017
Meyerbröker, K., and Morina, N. (2021). The use of virtual reality in assessment and treatment of anxiety and related disorders. Clin. Psychol. Psychotherapy 28 (3), 466–476. doi:10.1002/cpp.2623
Miloff, A., Carlbring, P., Hamilton, W., Andersson, G., Reuterskiöld, L., and Lindner, P. (2020). Measuring alliance toward embodied virtual therapists in the era of automated treatments with the virtual therapist alliance scale (VTAS): development and psychometric evaluation. J. Med. Internet Res. 22 (3), e16660. doi:10.2196/16660
Miloff, A., Lindner, P., Dafgard, P., Deak, S., Garke, M., Hamilton, W., et al. (2019). Automated virtual reality exposure therapy for spider phobia vs. in-vivo one-session treatment: A randomized non-inferiority trial. Behav. Res. Ther. 118, 130–140. doi:10.1016/j.brat.2019.04.004
Morina, N., Kampmann, I., Emmelkamp, P., Barbui, C., and Hoppen, T. H. (2021). Meta-analysis of virtual reality exposure therapy for social anxiety disorder. Psychol. Med. 53, 2176–2178. doi:10.1017/S0033291721001690
National Institute for Health and Care Excellence, (2013). Social anxiety disorder: recognition, assessment and treatment. (NICE Quality Standard No. 159). Available at: https://www.nice.org.uk/guidance/cg159
Nordgreen, T., Rabbi, F., Torresen, J., Skar, Y. S., Guribye, F., Inal, Y., et al. (2021). Challenges and possible solutions in cross-disciplinary and cross-sectorial research teams within the domain of e-mental health. J. Enabling Technol. 15 (4), 241–251. doi:10.1108/JET-03-2021-0013
Parrish, D. E., Oxhandler, H. K., Duron, J. F., Swank, P., and Bordnick, P. (2016). Feasibility of virtual reality environments for adolescent social anxiety disorder. Res. Soc. Work Pract. 26 (7), 825–835. doi:10.1177/1049731514568897
Patterson, B., Boyle, M. H., Kivlenieks, M., and Van Ameringen, M. (2016). The use of waitlists as control conditions in anxiety disorders research. J. Psychiatric Res. 83, 112–120. doi:10.1016/j.jpsychires.2016.08.015
Peters, L., Sunderland, M., Andrews, G., Rapee, R. M., and Mattick, R. P. (2012). Development of a short form social interaction anxiety (SIAS) and social phobia scale (SPS) using nonparametric item response theory: the SIAS-6 and the SPS-6. Psychol. Assess. 24 (1), 66–76. doi:10.1037/a0024544
Premkumar, P., Heym, N., Brown, D. J., Battersby, S., Sumich, A., Huntington, B., et al. (2021). The effectiveness of self-guided virtual-reality exposure therapy for public-speaking anxiety. Front. psychiatry 12, 694610. doi:10.3389/fpsyt.2021.694610
Reeves, R., Curran, D., Gleeson, A., and Hanna, D. (2021). A meta-analysis of the efficacy of virtual reality and in vivo exposure therapy as psychological interventions for public speaking anxiety. Behav. Modif. 46, 937–965. doi:10.1177/0145445521991102
Schuurmans, J., Comijs, H., Emmelkamp, P. M. G., Gundy, C. M. M., Weijnen, I., van den Hout, M., et al. (2006). A randomized, controlled trial of the effectiveness of cognitive–behavioral therapy and sertraline versus a waitlist control group for anxiety disorders in older adults. Am. J. Geriatric Psychiatry 14 (3), 255–263. doi:10.1097/01.JGP.0000196629.19634.00
Stein, M. B., Walker, J. R., and Forde, D. R. (1996). Public-speaking fears in a community sample. Prevalence, impact on functioning, and diagnostic classification. Archives General Psychiatry 53 (2), 169–174. doi:10.1001/archpsyc.1996.01830020087010
Sülter, R. E., Ketelaar, P. E., and Lange, W.-G. (2022). SpeakApp-Kids! Virtual reality training to reduce fear of public speaking in children – a proof of concept. Comput. Educ. 178, 104384. doi:10.1016/j.compedu.2021.104384
Valls-Ratés, Ï., Niebuhr, O., and Prieto, P. (2022). Unguided virtual-reality training can enhance the oral presentation skills of high-school students. Front. Commun. 7. 196, doi:10.3389/fcomm.2022.910952
Wiebe, A., Kannen, K., Selaskowski, B., Mehren, A., Thöne, A.-K., Pramme, L., et al. (2022). Virtual reality in the diagnostic and therapy for mental disorders: A systematic review. Clin. Psychol. Rev. 98, 102213. doi:10.1016/j.cpr.2022.102213
Wittchen, H. U., Stein, M. B., and Kessler, R. C. (1999). Social fears and social phobia in a community sample of adolescents and young adults: prevalence, risk factors and co-morbidity. Psychol. Med. 29 (2), 309–323. doi:10.1017/S0033291798008174
Keywords: virtual reality exposure therapy, public speaking anxiety, self-guided, internet interventions, adolescents
Citation: Kahlon S, Lindner P and Nordgreen T (2023) Gamified virtual reality exposure therapy for adolescents with public speaking anxiety: a four-armed randomized controlled trial. Front. Virtual Real. 4:1240778. doi: 10.3389/frvir.2023.1240778
Received: 15 June 2023; Accepted: 15 August 2023;
Published: 29 August 2023.
Edited by:
Clint Bowers, University of Central Florida, United StatesReviewed by:
Christine Seaver, University of Central Florida, United StatesTomasz Kupka, Polish Dental Association, Poland
Copyright © 2023 Kahlon, Lindner and Nordgreen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Smiti Kahlon, c21pdGkua2FobG9uQGhlbHNlLWJlcmdlbi5ubw==
 Smiti Kahlon
Smiti Kahlon Philip Lindner
Philip Lindner Tine Nordgreen
Tine Nordgreen