
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Virtual Real. , 15 July 2022
Sec. Virtual Reality and Human Behaviour
Volume 3 - 2022 | https://doi.org/10.3389/frvir.2022.915332
This article is part of the Research Topic VR/AR and Wellbeing: The Use of Immersive Technologies in Promoting Health Outcomes View all 6 articles
Most physical therapists would agree that physical rehabilitation is difficult to perform remotely. Consequently, the global COVID-19 pandemic has forced many physical therapists and their clients to adapt to telehealth, especially with video conferencing. In this article, we ask: How has telehealth for physical rehabilitation evolved with the global pandemic and what are the largest technological needs, treatment methodologies, and patient barriers? With the increased widespread use of telehealth for physical therapy, we present a qualitative study towards examining the shortcomings of current physical therapy mediums and how to steer future virtual reality technologies to promote remote patient evaluation and rehabilitation. We interviewed 130 physical rehabilitation professionals across the United States through video conferencing during the COVID19 pandemic from July—August 2020. Interviews lasted 30–45 min using a semi-structured template developed from an initial pilot of 20 interviews to examine potential barriers, facilitators, and technological needs. Our findings suggest that physical therapists utilizing existing telehealth solutions have lost their ability to feel their patients’ injuries, easily assess range of motion and strength, and freely move about to examine their movements when using telehealth. This makes it difficult to fully evaluate a patient and many feel that they are more of a “life coach” giving advice to a patient rather than a traditional in-person rehabilitation session. The most common solutions that emerged during the interviews include: immersive technologies which allow physical therapists and clients 1) to remotely walk around each other in 3D, 2) enable evidence-based measures, 3) automate documentation, and 4) provider clinical practice operation through the cloud. We conclude with a discussion on opportunities for immersive virtual reality towards telehealth for physical rehabilitation.
In 2020, the global COVID-19 pandemic halted existing models of physical rehabilitation care in the United States (Wikipedia, 2021). Social distancing guidelines required therapists to develop new protocols for patient care and often adoption of new technology for remote care (Yonter et al. (2020)). As a result, the global pandemic has deepened existing inequities and gaps in modern healthcare (Ndumbe-Eyoh et al. (2021)). These challenges sparked widespread adoption of telehealth, a service once ignored by many physical therapists due to its lack of hands on evaluation capabilities. The American Physical Therapy Association (APTA) notes “Telehealth is a well-defined and established method of health services delivery [and supports] Advancement of physical therapy telehealth practice, education, and research to enhance the quality and accessibility of physical therapist services” (APTA, 2019). Subsequently, the practice of telehealth for physical rehabilitation has seen an explosive adoption to mitigate the impact of the pandemic. In this paper, we examine the effects of telehealth adoption: it is challenges for physical rehabilitation, successes and practices during the pandemic, and professional views of how telehealth will transform physical rehabilitation beyond the pandemic.
In 2000, VandenBos and Williams (2000) defined telehealth as a “real-time service that occurs when the patient and the provider are physically separated at the time the service is rendered and some communication device is used in the exchange between the parties”. The best communication device then was a telephone. With advancements and accessibility of video camera technology, the internet provides a more capable choice for telehealth visits. In recent years, telehealth has proven to be an effective way to provide certain medical services. In a study by Axelsson et al. (2020), cognitive behavior therapy delivered via the internet “appeared to be noninferior to face-to-face [cognitive behavior therapy] for health anxiety, while incurring lower net societal costs.” Moreover, online therapy has the capability to increase evidence-based treatment. Another study in 2016 established that telehealth has potential to provide more accessible services to “vulnerable patient groups,” especially those who have transportation or financial barriers (Reed et al. (2020)).
Similarly, Telehealth Physical Therapy (TelePT) has been making its way onto online services; however, it is uncertain if telehealth can be truly effective for physical rehabilitation. First, what is TelePT? Building upon VanderBos, TelePT is a service that occurs when the patient and the physical therapist are physically separated at the time the service is rendered and some communication device is used in the exchange of rehabilitative exercises and consultation. The growing effectiveness of TelePT is supported by ongoing research. A study from Northeastern University examining virtual environment based systems for upper extremity mobility rehabilitation for post stroke patients found improvements even after physical therapy was discontinued (Shaw (2009)). Another study recorded upper and lower extremity movements with images and sent them to a hospital whose physical therapists provided feedback. This study determined that tech for rehabilitation was effective for storing data and referencing back later (Shaw (2009)). Reed et al. (2020) compared TelePT at home versus in-clinic rehabilitation and found that “telerehabilitation has the potential to substantially increase access to rehabilitation therapy on a large scale”. Other studies have shown that there is good agreement between telerehabilitation and face-to-face care for assessment of patients including lower back pain and hamstring flexibility (Palacín-Marín et al. (2013); Moral-Muñoz et al. (2015)) Additionally, telerehabilitation was shown to be effective following primary total hip or knee arthroplasty that did not compromise quality compared to face-to-face care and had high patient satisfaction (Kuether et al. (2019)). When contemplating telerehabilitation physical therapists (PT) should consider patient preference, assessment requirements, culutural needs, environment, cost, access, and confidence using technology (Zischke et al. (2021)). These studies show the results for online physical therapy have been effective with long term benefits to both the patient and the therapist.
While telehealth was not initially the norm, it is use skyrocketed when people were required to abstain from physical contact with non-household members. During the 2020 pandemic, Smith et al. (2020) argued that telehealth requires “a significant change in management effort and the redesign of existing care models of care. Implementing telehealth proactively rather than reactively is more likely to generate greater benefits in the long-term, and help with the everyday (and emergency) challenges in healthcare”. The pandemic forced many providers and small health businesses to switch to virtual visits in order to deliver care. Dantas et al. (2020) says that TelePT “offers the possibility to continue providing some physical therapy services to patients, but regulations and implementation barriers are extremely heterogeneous around the world”. Lee (2020) also notes the benefits of using TelePT for building strong relationships between the patient and provider while maintaining a safe environment.
Telehealth cannot replace all forms of medical care. COVID-19 has deepened struggles for patients who require constant treatment or cancer patients who have compromised immune systems (Bland et al. (2020)). While it is a significant resource with growing adaptations, telehealth can not provide blood withdrawal, chemotherapy, or physical examinations. Still, COVID-19 has elevated the relevance of TelePT and its efficacy. As technology remains a huge part of daily life, TelePT might offer new opportunities for regular care practice. Policies have hindered the adoption of telehealth, but the COVID-19 pandemic caused a temporary policy relaxation with respect to physician licensure, geographic location, and eligible sites for reimbursement to help increase access to care as many clinics were unable to see their patients face-to-face (Albanese et al. (2021)). It is unclear how long these relaxations will last. Remaining challenges to facilitate adoption include the need for standardized telehealth practices and studies that address the efficacy of telehealth compared to in-person care. Furthermore, the uncertainty of insurance coverage for TelePT may be a significant barrier.
In this study we find rehabilitation via telehealth is sustainable and increases accessibility especially for under-served communities. While research on telehealth telepresence for physical well-being are largely reviews or perspectives, this article is based on primary research across the whole country. Furthermore, we have sought direct feedback from PTs, a group that is often not heard in telehealth research. While physicians can often make diagnoses using video, PTs find it hard to evaluate injuries with video only as they are accustomed to hands-on evaluation. COVID and social distancing protocols have limited patient’s access to care. As video therapists and TelePTs continue to practice in this global pandemic it is critical to learn what works, and doesn’t work, in order to provide effective remote care beyond the global COVID pandemic.
This study used a 2-stage sampling design. First, we purposefully selected three states (California, New York, and Florida) with the largest spikes of COVID19 cases to start. Within each state, we identified regional chapters of the American Physical Therapy Association (APTA) and reached out to professionals using LinkedIn, an online business social network platform. Two of us (A.E. and M.P.) identified 18 chapter leaders and requested informational interviews or recommendations for interviewees. The second stage involved a snowball sampling procedure that involved Question 6 from the box interview (Figure 1) responses of chapter leaders combined with LinkedIn searches of related physical therapy professionals including physical therapists, clinic owners, policy makers, leadership, and technology influencers (those who significantly impact technology adoption at their practice).
Additionally, this study received an Institutional Review Board (IRB) exemption from the University of California Santa Cruz (UCSC) Office of Research Compliance Administration (ORCA) under protocol #HS3573. No compensation was provided to the participants. In total, we sent 800 LinkedIn message requests resulting in a response/interview rate of about 16.25% (˜130/800). Our inclusion criteria were as follows:
• Practicing in a physical rehabilitation setting within the past 3 years.
• Able to consent to participate and join a remote video call.
• 18 years or older.
We developed a 30–45 min semi-structured interview guide based on an initial pilot study conducted in May 2020 with 20 physical therapists from the California Bay Area through phone interviews or web-conferencing. The interview protocol was iteratively updated to explore questions about potential barriers, facilitators, and technological needs for implementing remote physical rehabilitation with telehealth. This led to the final box interview template in Figure 1. Two researchers (A.E. and M.P.) then conducted interviews during 07 July 2020—18 August 2020. The researchers were trained to perform these interviews through the CITI Human Subjects Research (HSR) program (Braunschweiger and Hansen (2010)) and the National Science Foundation Innovation Corps (NSF I-CORPS) program (Nnakwe et al. (2018)). A.E. and M.P. also performed the pilot interviews to derive the initial codebook—this was done through unstructured interviews focused about current technology practices during and before the pandemic, technology usage and satisfaction, and stakeholder ecosystem mapping. Pilot interviews were excluded from the analysis of this study as they did not follow the box interview guide from Figure 1. Communication was achieved through face-to-face video conferencing with the Zoom platform.
Based on the pilot study with 20 PTs, we developed an codebook centered around value propositions as shown in shown in Figure 3. Our goal was to capture at least 100 interviews to reach significant thematic saturation of values over the 2 month period, as often a standard practice in the NSF I-CORPS training program (Braunschweiger and Hansen (2010)). The interviews began with variety of professionals in the physical rehabilitation field and as the needs were understood the interviews tend towards the need of one archetype with the greatest need, resulting in our focus of Physical Therapists. Interviewers took iterative notes, transcriptions, and labeled emergent themes from interviewees as the interviews progressed. Data was analyzed in a procedure where A.E. and M.P. identified interview themes and codes using constant comparative analysis as an ongoing measure (Fram (2013))—interviews were coded and disagreements were verbally discussed within 1 week of each interview to resolve any disagreements between all A.E. and M.P. with S.K. acting as a tie breaker. Through this process, we identified a range of risks and benefits based from participant experiences, this is shown in the sub-themes of Figure 3. Our final codebook categorized telehealth physical therapy and VR interventions by seven different value propositions: analytics, interaction, practice, gamification, documentation, access, and usability in order of frequency of codes appearing in interviews. We further breakdown these values in Section 3.1.
We conducted 130 in-depth interviews in face-to-face live video interviews across 26 states, with most interviews conducted in Northern California (38), Southern California (16), New York (11), Florida (6), and Texas (6) as shown in Figure 2. Interviewees identified as physical therapists (96) with a subset identifying as occupational therapists (4), physical therapy assistants/technicians (5), or physical rehabilitation management experts (25). Participants included 74 doctors of physical therapy with specializations in outpatient (27), sports (18), orthopedic (16), home health (14), neurological (13), travel (4), and geriatrics (2). Additionally, 40 interviews were clinic owners, 55 had experience in care management roles, 50 considered themselves to be technology influencers in their workplace, 15 PTs went through physical rehabilitation for their own injuries as a patient during the pandemic, and 18 were actively involved in leadership or rehabilitation policy. The top most reoccurring locations, specializations, and roles can be seen in Table 1. Interviewee healthcare institutions ranged from large hospitals to small independent clinics.
The interviews identified key trends for physical rehabilitation showing that many PTs we interviewed had similar experiences with their patients. Physical Therapy typically consists of the patient going to the clinic 1–2 times per week for several weeks, months, or even years. The patient is often given exercises to do at home, which studies show have low compliance rates (Sluijs et al. (1993); Chen et al. (1999)). After in-person treatment, depending on the type of insurance, the patient is discharged from clinical therapy and advised to continue exercises at home to further the recovery. Most fail to continue with at-home exercises due to lack of motivation, repetitive exercises, and lack of accountability. In many areas, there are not enough therapists to meet the demand of all surrounding patients leading to difficult scheduling and less frequent clinic visits.
With shelter in place orders across the nation, clinics responded with a range of options: discontinued care for patients altogether, implemented social distancing, or adopted teletherapy using video conferencing. These responses impacted low income and rural communities especially in medical deserts with fewer health professionals relative to more affluent areas. Video conferencing enables communication, but lacks interpersonal connections between physician and patient that stems from interaction. Additionally, the physician is unable to obtain functional health metrics that help monitor progression of conditions such as heart rate or joint angles and forces for physical movement.
Several themes emerged from the interviews including: therapists believe that telehealth will be a part of physical therapy beyond the COVID-19 pandemic, current telehealth systems don’t allow for accurate patient evaluation, insurance coverage for telehealth in the future is unclear, telehealth increases accessibility for patients, telehealth may help with preventative care, and therapists want telehealth platforms to provide accurate measures and 3D interaction. Subsequently, resulting themes can be seen in Figure 3.
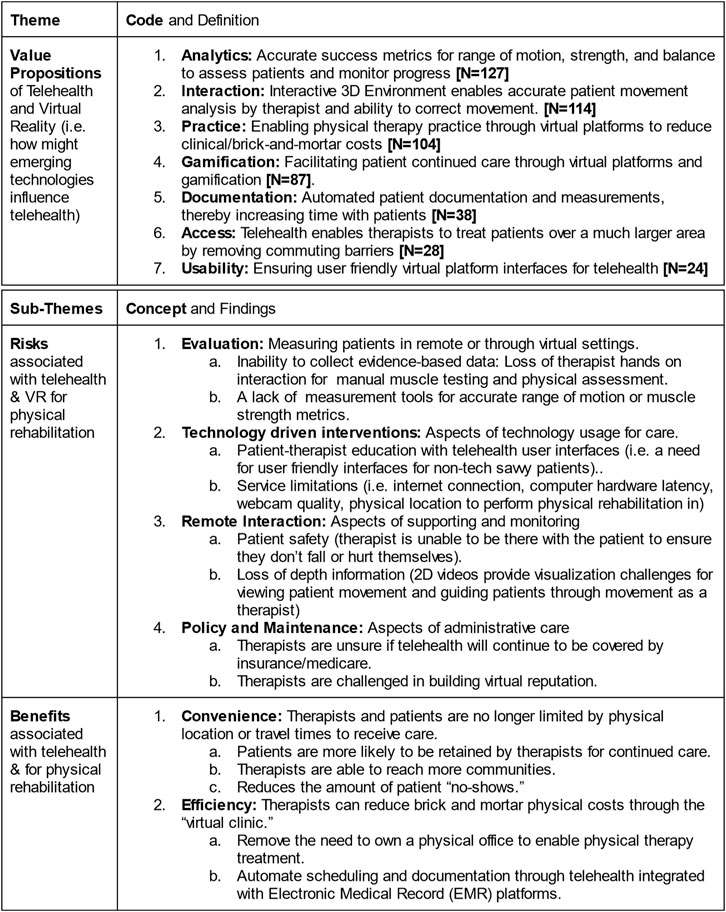
FIGURE 3. Codebook and themes generated from interviews around technological challenges and opportunities for physical therapy telehealth. N indicates number of occurrences from interviews per top-level themes.
A recurring theme was the severe concern of integrating telehealth for physical therapy both during and after the COVID-19 pandemic. Many physical therapists and outpatient rehabilitation clinic owners perceived telehealth adoption to be accelerated by the impact of the pandemic, noting that telehealth for physical therapy is here to stay. Therapists explained their biggest concerns with telehealth was the lack of hands-on evaluation (e.g., manual muscle testing) and obtaining evidence-based measures of recovery such as goniometer measurements for range of motion. Most clinics turned to remote video conferencing solutions to facilitate physical therapy; however, therapists shared frustration with 2D video displays: an inability to properly observe evaluative tests such as berg balance or time-up-and-go due to limited space in the patient’s home, technical difficulties in setting up webcams, and being unable to tilt the camera around the patient to view their movements as needed. Therapists shared that “all [video] telehealth can do is functional testing. I need to get a range of motion and strength assessments” with many PTs feeling that they have become “virtual life coaches instead of physical therapists” due to the limitations of phone-based or video physical therapy. Another large concern was the uncertainty of Medicare coverage in telehealth, where many clinics providing Medicare services felt indecision in investing towards telehealth without a guarantee that treatment will be reimbursed without pay cuts.
On the other hand, many interviewees noted benefits of incorporating physical therapy through telehealth. One clinical director shared “Telehealth is like [the food delivery app] Uber Eats, you can reinforce it as it’s convenient and patients know it exists now. They’ve gotten used to the convenience of telehealth and it’s really here to stay thanks to COVID.” Other physical therapists noted that patient no-shows were reduced, follow-up appointment retention increased, and patient visit throughput for therapists was increased due to travel time being removed and greater autonomy with online scheduling and web conference systems.
Interviewees shared many perspectives about insurance and concierge based physical therapy. Key pain points regarding insurance were noted: uncertainty of future medicare policies, perceived lowering standards of treatment due to insurance evidence requirements, and turning clinics into “patient mills” where therapists per patient are increased with minimal visit time to get enough revenue to keep their clinics afloat. Patient mills were a recurring concern between in-patient and out-patient physical therapists where pay cuts in insurance appeared to be one of the largest causes amplified by the global pandemic. Consequently, clinical directors and traveling therapists conveyed that out-of-network coverage is a growing trend where physical therapists who are suffering from burnout and insurance are turning instead towards concierge based physical therapy. Another self-practicing physical therapist shared “every physical therapist that opens a clinic dreams of getting their patients into fully cash-based [payment methods], insurance is a means to an end to get more patients, but the dream is fully cash-based to give us the freedom to help our patients as they need it.”
Thus, a majority of interviewees, self-practicing or clinical owning physical therapists, are actively searching for new business models to support preventative treatment, with cash-based or concierge physical therapy as an avenue to support this model. Interviewees argued that insurance based physical therapy is largely a rehabilitative market, reacting to injury without emphasizing or recognizing the need of preventive rehabilitation (prehab). One therapist shared “physical therapy should last years, become a lifestyle [for the patient], but in reality the minimum is done for patients who often fall back into cycles of treatment.” This perspective was amplified by the rapid adoption of telehealth, especially for continued care. Many were laid off at the start of the pandemic due to clinics closing due to decreased patient visits or lack of infrastructure to adopt telehealth as a business model. A majority of therapists in this situation turned towards self-practicing concierge services and preventative care, effectively becoming traveling physical therapists through a hybrid mix of occasional visits to patients home and conducting check-ins with video conferencing. Many self-practicing and clinic owning therapists believed that after the pandemic, their practices will likely continue with telehealth or hybrid models of video visits with in person. Many emphasized moving away from injury to preventative care, where follow up visits can be conducted through telehealth for a lower cost but at a higher visit rate. Telehealth was often seen as a solution to facilitating prehab through continued care: getting the tools into the hands of patients before they even become patients with video visits, asynchronous messaging between therapist-patients, and a greater rate of visits.
Some clinics took the opportunity to incorporate high-tech solutions into facilitating telehealth: this included smartphone based patient videos for exercises, wearable sensors with IMUs to track range of motion, and exoskeletons for at-home supported movements and exercises. Interviewees were encouraged to speculate about possible improvements for telehealth beyond video based interaction. Therapists were asked “what if you could stand in the same room with your patient, walk around them in 3D, but be unable to touch them?” Many top themes were revealed (1—analytics) the ability to gather evidence-based measures of patient performance remotely through patient motion capture, (2—interaction) enhancing therapist perception with immersive 3D technologies to effectively enable therapists and patients to be in the same room and walk around each other remotely, (3—practice) provide a means for therapists to run their own practice or clinic through the cloud to reduce the overhead costs of starting their own practice or running a practice during the pandemic, (4—gamification) a means to increase compliance and adherence of remote exercises through making therapy prescriptions more playful or game-based in VR, and (5—documentation) automating documentation and measurements to give the therapist more one-on-one time with the patient. Further themes, values, and sub-findings are shown in Figure 3. Followup questions were centered around usability concerns (how would the technology need to function for patients to be able to use it at home), success metrics (what metrics does a therapist need to see with this technology to evaluate a patient and see they are improving), and patient involvement (when should patients use or not use this type of technology). The resulting wordclouds from these queries is illustrated in Figure 4.
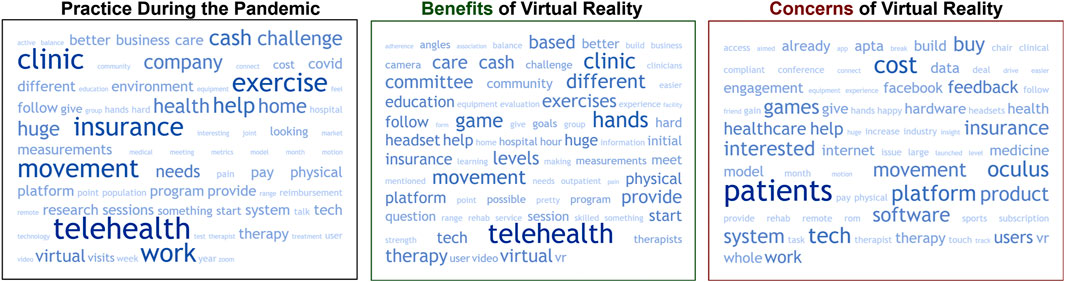
FIGURE 4. Wordclouds generated from interviews on practice during the pandemic, perceived benefits and concerns of VR.
Common concerns included an easy to use technology with an intuitive user design, need and validation of accurate metrics for range of motion, strength, and balance, and that this type of technology should not be used for any patients who are at medium or high risk of falling. On concerns of usability and patient involvement with VR, four primary risks were identified (1—evaluation) the application will need to be validated for accuracy with alternative measurement tools that do not require hands-on intervention, (2—technology intervention) the VR application will need to be user-friendly and intuitive enough to work with non-tech savvy populations that may have service limitations in internet connectivity and physical space, (3—remote interaction) the VR technology should primarily be used in safe situations (e.g., outpatient populations) that don’t require therapist or caretaker monitoring of the patient or close observation to reduce immediate injury, and (4—policy and maintenance) the VR application will need to be covered by insurance and integrate with electronic medical records (EMRs) for full-adoption outside of concierge practices. While many therapists were worried about the technology savviness of their patients, many referred to previous experiences of utilizing hardware such as the Nintendo Wii (e.g., Wii Sports and Balance Board) and Microsoft Xbox Kinect in clinics with relatively easy patient adoption.
The global COVID-19 pandemic has vastly accelerated the adoption of telehealth for physical rehabilitation. Many therapists shared that this event has fast tracked the technological remodeling of modern clinics as both patients and therapists have become used to the technical needs of living in a virtual-social workplace with sheltering in place. While telehealth was initially viewed as a flawed practice for physical therapy, clinicians have found strengths in remote healthcare such as increased patient retention, reduced travel time, and less operating costs. The largest challenges of telehealth was the inability to collect evidence-based success measures and evaluate patient movements. Metrics of capturing range of motion, muscle strength, and balance risk were all common measures for in-person physical therapy, but these were lost in telehealth. Nonetheless, a common consensus was that telehealth in physical rehabilitation is here to stay. Beyond the pandemic, many practitioners shared they would switch to a hybrid model of in-person treatment and telehealth or entirely adopt telehealth practices to run “physical therapy clinics in the cloud.” In examining future approaches for mitigating limitations in telehealth, immersive virtual environments were found to be one promising solution: enabling 3D virtual worlds for patients and therapists to meet, walk around one another, and examine exercise movements.
Telehealth was seen as a possible solution to therapist burnout and barriers to entry in starting independent clinics. While therapists pointed out limitations in video and text based communication platforms, there was growing disconnect with returning “back to normal” after the pandemic subsided. Many therapists shared that medicare based clinics can often feel like “patient mills”—treatment overloaded by patient size and conforming to insurance restrictions (e.g., medicare compliance). Many therapists that shared the desire to start their own clinics or switch to independent practitioners, but were deterred by student debt or clinic startup costs. When speculating about the future, therapists viewed the cash-based physical therapy market as a potential entry point to mitigate the startup costs without the burnout from adhering to insurance restrictions.
Telehealth’s largest challenge with physical rehabilitation was the loss of hands-on evaluation tools. Many therapists never received formal training for conducting remote treatment during the pandemic, and the loss of hand-based evaluation (e.g., manual muscle testing) was often referred to as the largest challenge. Throughout the interviews, four recurring tests were often discussed: 1) Range of Motion (e.g., Goniometer), 2) Strength (e.g., manual muscle testing, or Isokinetic Dynamometers), 3) Coordination (e.g., Timed up and Go), and 4) Balance (e.g., Berg Balance Assessment). With the loss of these measures, therapists resorted to having patients self-test or became “life coaches,” meeting virtually to provide advice rather than treatment. While some therapists acclimated to utilizing digital measurement tools (e.g., virtual goniometers from video), many struggled to obtain proper lighting, full depth of movements, and or camera quality to perform a visual evaluation. This informed our speculative component of the interview to determine how emerging technology could mitigate these challenges.
Immersive virtual environments offer a powerful opportunity to transform physical rehabilitation telehealth. In discussing the incorporation of 3D virtual environments for treating patients, therapists saw opportunity for capturing range of motion and strength assessments utilizing head-mounted display motion capture. The incorporation of a 3D virtual room in which patients and therapists could meet virtually through avatars seemed to be a potential solution to the existing limitations of video based telehealth. While the loss of hands-on evaluation was a barrier, therapists believed such an approach would enhance continued care, retention, and reliability of patient progression. Therapists did note many possible risks with such an environment: 1) patients with unstable balance risk injury without in person supervision, 2) virtual representation of the patient’s movements must be accurate in order to reduce movement bias, and 3) motion sickness from the headset may cause discomfort. While there is still much research to be done on the effectiveness and best practices of rehabilitation and virtual environments, studies have shown increases in motivation, reduction in discomfort, high patient satisfaction, and functional improvements to be comparable to face-to-face care (Gromala et al. (2015); Hoffman et al. (2011); Schröder et al. (2019)). Virtual reality head-mounted display systems provide the added benefit of motion capture of the user so that the PT can potentially use this data for predicting a patient’s range of motion or joint torques (Powell et al. (2022)). Virtual reality systems are continuously improving and prices are being driven down by the industry making this technology more accessible and a possible platform for remote physical rehabilitation (Elor and Kurniawan (2020)).
As with any study, there are some limitations of our work that need to be taken into account. The COVID-19 lockdown forced us to reconfigure interviewing as video conferences rather than in person. This limited the fidelity of the demonstrations we can witness from the health care professionals we interviewed. Second, with our sample states, our results might not be as relevant to states with different regulations or practices. Third, personal demographics were not collected and all recorded data was de-identified to follow our IRB exemption protocol. This inhibits us from drawing any interpretation related to personal demographics, which can definitely be expanded upon in future work as the majority of our interviewees were outpatient physical therapists. Our results might differ if the professionals were different and or focus on sampling by unique demographics. Finally, our speculative portion of the therapist interviews were framed through immersive virtual reality, while modern head-mounted display systems are becoming increasingly more accurate at combining virtual and augmented reality experiences, it would be important to consider smartphone and handheld based virtual reality systems in future work. While we must consider these limitations, we believe that the results we report provide a starting point to engage upon future research towards supporting telehealth and physical therapy with immersive technologies such as virtual reality.
In this research on the uses of telehealth in physical rehabilitation throughout COVID-19 restrictions, our empirical study with physical therapists offers insights into new directions for telehealth after the pandemic. Common themes emerged regarding potential solutions for working around issues of presence or measurement data collection. These include: immersive 3D technologies which allow PTs and clients to walk around each other remotely, evidence-based measures, automating documentation and measurements, provide a means for therapists to run their own practice or clinic through the cloud, and more. These approaches may enable PTs to reduce the overhead costs of starting or maintaining practice in event that future pandemics require limited in person care or therapeutic treatment. In summary, the knowledge gained from these interviews indicate significant opportunities with virtual reality to expand the capabilities and reach of physical therapists for rehabilitation and preventative care via telehealth.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by University of California, Santa Cruz (UCSC) Office of Research Compliance Administration (ORCA). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
AE and SC wrote the first draft of the article. AE and MP led the interviews with physical therapists while AR and SK supported. AS and SC supported secondary analysis. NC and SK advised on methods and analysis while also supporting with article revisions. All authors contributed to the final article draft through group writing working sessions.
This article is based upon work supported by the National Science Foundation under Grant No #2037917. Such work was also supported by the 2020 Seed Fund Award 2020-0000000044 from CITRIS and the Banatao Institute at the University of California, a statewide research institute operated by the University of California to facilitate the real-world application of technological research. Additionally, AE was supported by the University of California, Santa Cruz Global Community Health Wellbeings 2020 Fellows Program. Any opinions, findings, and conclusions or recommendations expressed in this material are those of the author(s) and do not necessarily reflect the views of the National Science Foundation, University of California, and or the ARCS Foundation.
AE received a 2020 University of California Global and Community Health Fellowship from the University of California, Santa Cruz and an ARCS Fellowship from the United States ARCS Foundation Non-profit. Additionally, AE, MP, and AR joined and co-founded Immergo Labs in September 2021.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Dana Seth, DPT, of the Austin Physical Therapy Clinics, provided assistance and feedback during the early stages of the study design. Greg Gewickey provided feedback throughout the study and recommended key individuals and stakeholders to interview.
Albanese, S., Gupta, A., Shah, I., and Mitri, J. (2021). Medicare Telehealth Pre and Post-covid-19: Interstate Framework, Regulations, Licensure, and Hipaa. Telehealth Med. Today 6, 299. doi:10.30953/tmt.v6.299
APTA (2019). Position on Telehealth. Available at: https://www.apta.org/apta-and-you/leadership-and-governance/policies/telehealth.
Axelsson, E., Andersson, E., Ljótsson, B., Björkander, D., Hedman-Lagerlöf, M., and Hedman-Lagerlöf, E. (2020). Effect of Internet vs Face-To-Face Cognitive Behavior Therapy for Health Anxiety. JAMA Psychiatry 77, 915. doi:10.1001/jamapsychiatry.2020.0940
Bland, K. A., Bigaran, A., Campbell, K. L., Trevaskis, M., and Zopf, E. M. (2020). Exercising in Isolation? the Role of Telehealth in Exercise Oncology during the COVID-19 Pandemic and beyond. Phys. Ther. 100, 1713–1716. doi:10.1093/ptj/pzaa141
Braunschweiger, P., and Hansen, K. (2010). Collaborative Institutional Training Initiative (Citi). J. Clin. Res. Best. Pract. 6, 1–6.
Chen, C.-Y., Neufeld, P. S., Feely, C. A., and Skinner, C. S. (1999). Factors Influencing Compliance with Home Exercise Programs Among Patients with Upper-Extremity Impairment. Am. J. Occup. Ther. 53, 171–180. doi:10.5014/ajot.53.2.171
Dantas, L. O., Barreto, R. P. G., and Ferreira, C. H. J. (2020). Digital Physical Therapy in the COVID-19 Pandemic. Braz. J. Phys. Ther. 24, 381–383. doi:10.1016/j.bjpt.2020.04.006
Elor, A., and Kurniawan, S. (2020). The Ultimate Display for Physical Rehabilitation: A Bridging Review on Immersive Virtual Reality. Front. Virtual Real. 1, 585993. doi:10.3389/frvir.2020.585993
Fram, S. M. (2013). The Constant Comparative Analysis Method outside of Grounded Theory. Qual. Rep. 18.
Gromala, D., Tong, X., Choo, A., Karamnejad, M., and Shaw, C. D. (2015). “The Virtual Meditative Walk: Virtual Reality Therapy for Chronic Pain Management,” in Proceedings of the 33rd Annual ACM Conference on Human Factors in Computing Systems (New York, NY, United States: ACM), 521–524.
Hoffman, H. G., Chambers, G. T., Meyer, W. J., Arceneaux, L. L., Russell, W. J., Seibel, E. J., et al. (2011). Virtual Reality as an Adjunctive Non-pharmacologic Analgesic for Acute Burn Pain during Medical Procedures. Ann. Behav. Med. 41, 183–191. doi:10.1007/s12160-010-9248-7
Kuether, J., Moore, A., Kahan, J., Martucci, J., Messina, T., Perreault, R., et al. (2019). Telerehabilitation for Total Hip and Knee Arthroplasty Patients: A Pilot Series with High Patient Satisfaction. HSS Journal® 15, 221–225. doi:10.1007/s11420-019-09715-w
Lee, A. C. (2020). COVID-19 and the Advancement of Digital Physical Therapist Practice and Telehealth. Phys. Ther. 100, 1054–1057. doi:10.1093/ptj/pzaa079
Moral-Muñoz, J. A., Esteban-Moreno, B., Arroyo-Morales, M., Cobo, M. J., and Herrera-Viedma, E. (2015). Agreement between Face-To-Face and Free Software Video Analysis for Assessing Hamstring Flexibility in Adolescents. J. Strength & Cond. Res. 29, 2661–2665. doi:10.1519/jsc.0000000000000896
Ndumbe-Eyoh, S., Muzumdar, P., Betker, C., and Oickle, D. (2021). ‘Back to Better’: Amplifying Health Equity, and Determinants of Health Perspectives during the COVID-19 Pandemic. Glob. Health Promot. 28 (2), 7–16. doi:10.1177/17579759211000975
Nnakwe, C. C., Cooch, N., and Huang-Saad, A. (2018). Investing in Academic Technology Innovation and Entrepreneurship: Moving beyond Research Funding through the Nsf I-corpsTM Program. Technol. Innovation 19, 773–786. doi:10.21300/19.4.2018.773
Palacín-Marín, F., Esteban-Moreno, B., Olea, N., Herrera-Viedma, E., and Arroyo-Morales, M. (2013). Agreement between Telerehabilitation and Face-To-Face Clinical Outcome Assessments for Low Back Pain in Primary Care. Spine 38, 947–952. doi:10.1097/brs.0b013e318281a36c
Powell, M. O., Elor, A., Robbins, A., Kurniawan, S., and Teodorescu, M. (2022). Predictive Shoulder Kinematics of Rehabilitation Exercises through Immersive Virtual Reality. IEEE Access 10, 25621–25632. doi:10.1109/access.2022.3155179
Reed, M. E., Huang, J., Graetz, I., Lee, C., Muelly, E., Kennedy, C., et al. (2020). Patient Characteristics Associated with Choosing a Telemedicine Visit vs Office Visit with the Same Primary Care Clinicians. JAMA Netw. Open 3, e205873. doi:10.1001/jamanetworkopen.2020.5873
Schröder, J., Van Criekinge, T., Embrechts, E., Celis, X., Van Schuppen, J., Truijen, S., et al. (2019). Combining the Benefits of Tele-Rehabilitation and Virtual Reality-Based Balance Training: a Systematic Review on Feasibility and Effectiveness. Disabil. Rehabilitation Assistive Technol. 14, 2–11. doi:10.1080/17483107.2018.1503738
Shaw, D. K. (2009). Overview of Telehealth and its Application to Cardiopulmonary Physical Therapy. Cardiopulm. Phys. Ther. J. 20, 13–18. doi:10.1097/01823246-200920020-00003
Sluijs, E. M., Kok, G. J., and van der Zee, J. (1993). Correlates of Exercise Compliance in Physical Therapy. Phys. Ther. 73, 771–782. doi:10.1093/ptj/73.11.771
Smith, A. C., Thomas, E., Snoswell, C. L., Haydon, H., Mehrotra, A., Clemensen, J., et al. (2020). Telehealth for Global Emergencies: Implications for Coronavirus Disease 2019 (COVID-19). J. Telemedicine Telecare 26, 309–313. doi:10.1177/1357633X20916567
VandenBos, G. R., and Williams, S. (2000). The Internet versus the Telephone: What Is Telehealth Anyway? Prof. Psychol. Res. Pract. 31, 490–492. doi:10.1037/0735-7028.31.5.490
Wikipedia (2021). COVID-19 Pandemic. Page Version ID: 1027893345. Available at: https://en.wikipedia.org/w/index.php?title=COVID-19_pandemicoldid=102789334.
Yonter, S. J., Alter, K., Bartels, M. N., Bean, J. F., Brodsky, M. B., González-Fernández, M., et al. (2020). What Now for Rehabilitation Specialists? Coronavirus Disease 2019 Questions and Answers. Archives Phys. Med. Rehabilitation 101, 2233–2242. doi:10.1016/j.apmr.2020.09.368
Keywords: physical rehabilitation, physical therapy, immersive virtual reality, extended reality, metaverse, telehealth, remote care, COVID19
Citation: Elor A, Conde S, Powell M, Robbins A, Chen NN and Kurniawan S (2022) Physical Therapist Impressions of Telehealth and Virtual Reality Needs Amidst a Pandemic. Front. Virtual Real. 3:915332. doi: 10.3389/frvir.2022.915332
Received: 07 April 2022; Accepted: 22 June 2022;
Published: 15 July 2022.
Edited by:
Benjamin J Li, Nanyang Technological University, SingaporeCopyright © 2022 Elor, Conde, Powell, Robbins, Chen and Kurniawan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Aviv Elor, YWVsb3JAdWNzYy5lZHU=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.