- 1School of Social Work, Bar Ilan University, Ramat Gan, Israel
- 2Sonarion Ltd., Jerusalem, Israel
- 3Neuropsychiatry Unit, Jerusalem Mental Health Center, The Hebrew University, Jerusalem, Israel
Introduction: Research examining the prevention of Posttraumatic Stress Disorder (PTSD) has shown that selective treatments to those with high symptom levels, using trauma focused CBT are relatively successful in reducing symptoms and preventing chronic PTSD. However, uptake of these early treatments is often low. This study aimed to provide an internet based Virtual Reality treatment to overcome some of these barriers to early treatment.
Method: The study received IRB approval from Hadassah Hospital (HMO 0056-013); its ClinicalTrials.gov identifier is NCT01760213. Recent survivors of motor vehicle accidents (N = 1,500) were assessed by telephone and online questionnaires. Patients meeting study criteria were randomly assigned to a Virtual Reality internet-based trauma-focused cognitive behavioral therapy (CBT) or waitlist control.
Results: the majority of subjects recruited did not meet study criteria or were unwilling to participate. 14 subjects were randomly assigned to treatment or waitlist control. Results indicate that both groups show a decline in PTSD symptoms at follow up, with no significant differences between groups.
Discussion: prevention of PTSD is a challenging goal, and internet-based interventions may play a role in this. The current study was not able to recruit sufficient participants to draw conclusions regarding the efficacy of the treatment. Proving services via the internet may not reduce barriers to care in this population.
Clinical Trial Registration: https://clinicaltrials.gov/ct2/show/NCT01760213?term=Freedman&cond=PTSD&cntry=IL&draw=2&rank=2, identifier NCT01760213.
1 Introduction
Posttraumatic stress disorder (PTSD) is unique in psychiatry in that it has a known starting point (exposure to a traumatic event) and its development has been well described (Shalev et al., 1996). This literature indicates that whilst the majority of exposed individuals will express symptoms of distress in the immediate aftermath of an event, these will wane over time. This natural recovery means that up to 80% of these exposed to a traumatic event will not develop PTSD (Kashdan and Kane, 2011).
Since most natural recovery takes place close to the event, it seems likely that this time period represents a window of opportunity, where interventions may be more successful. Early interventions for PTSD thus are an attempt to prevent the development of the disorder. Prevention methods are important since treatment for chronic PTSD is not helpful for everyone. Recommended treatments for PTSD include EMDR, cognitive processing therapy and exposure-based therapy (Lewis et al., 2020). All these interventions reduce PTSD levels in approximately 60–70% of patients. However, barriers to treatment remain, since many patients do not come for treatment, or dropout of treatment early. This combined with those who do not respond to treatment, means that a substantial proportion of people with PTSD do not recover (Hoge et al., 2004; Shalev et al., 2011).
Similar barriers to treatment are relevant for PTSD prevention and in order to attempt to overcome these, it is important to examine non-traditional methods of treatment delivery, for instance delivering treatment via an alternative platform (Kazdin and Blase, 2011). Internet based treatments for PTSD include a range of formats, from completely self-guided online treatments through mixed online and therapist assisted interventions to therapist/patient meeting weekly online. A recent meta-analysis concludes that there is emerging evidence for therapist guided internet treatments, showing it to be superior to waitlist (Lewis et al., 2019). However, little data exists, and the results regarding long term outcome are less positive.
An additional barrier to treatment for PTSD within exposure-based therapies regards the challenge to the patient in reconstructing the narrative of the traumatic event, and exposure to the reminders of the event. In certain circumstances it can be hard to carry out in vivo exposures, for instance when treating a patient with PTSD following a car crash in a snowstorm, when snow falls in the area only once every few years. Several studies have shown the conducting exposure using virtual reality is effective and helpful (Rothbaum et al., 2010). However, as far as these authors are aware, early interventions have not included VR, and until now, Virtual Reality treatment has taken place in the traditional setting of the therapist’s office.
The aim of this randomized controlled study was to examine the effectiveness and efficacy of an internet-based Virtual Reality treatment for preventing PTSD, as compared to a non-treatment control group. The intervention, Internet-Virtual Reality (i-VR), was specifically designed as an intervention for PTSD that combines a Virtual Reality environment that can be accessed via the Internet. The five-session intervention included evidence-based components for PTSD, such as breathing retraining, exposure and cognitive restructuring.
The study used a non-treatment control group since prevention methods need to be more effective than natural recovery. Additionally, only patients with a high likelihood of developing PTSD were included, since previous studies has shown that preventative methods work best with this population.
2 Materials and methods
2.1 Participants
Adult patients, aged 18–65 who arrived at a Level I Emergency Room following a motor vehicle accident (MVA) were recruited to the study. Inclusion criteria included PTSD symptoms (apart from the time criteria) 2 weeks post trauma and ability to give informed consent. Exclusion criteria included suffering from, or have suffered from in the past, bipolar disorder, psychotic disorder or substance abuse; suffering from chronic PTSD; loss of consciousness on arrival to the ER; suffering from another Axis I anxiety disorder that requires immediate treatment; and suicide risk.
2.2 Study design
In this randomized controlled trial, patients were randomized to one of two conditions. The first was the i-VR treatment, consisting of five sessions; the second was waitlist control. The study received IRB approval from Hadassah Hospital (HMO 0056-013); its ClinicalTrials.gov identifier is NCT01760213. Patients signed informed consent, and were able to leave the study at any point. Patients still symptomatic at the end of the research were referred to the Outpatient Psychiatry Department, Hadassah Hospital. The Internet environment ensured patient confidentiality. All data was stored with subject numbers only, without identifying data.
2.3 Intervention
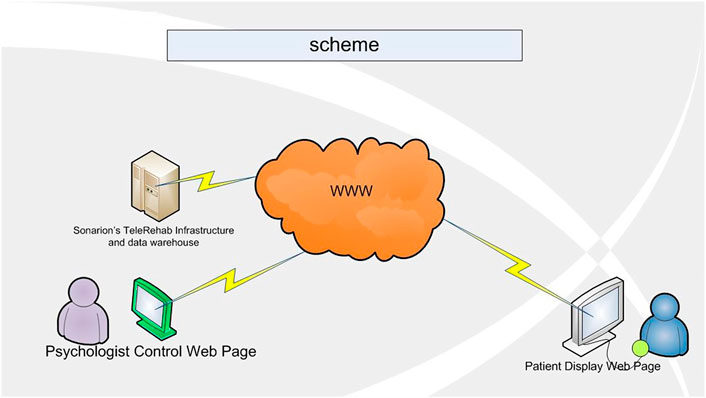
The treatment protocol consisted of five sessions. All interventions described were available in multi-formats: the therapist’s verbal explanation, a written text that appears in the ‘therapy room’, animation of examples and metaphors used, video clips, and Virtual Reality scenarios. All these were available between sessions for the patient to use. In the initial session, the therapist built rapport with the patient, provided education regarding both common reactions following traumatic events, and the therapy, and agreed a problem list. At the end of the session the therapist taught the patient anxiety reducing breathing retraining. In session II, the rationale for in vivo exposure was given-the patient learnt why fear reduces when we expose ourselves to avoided, although safe, stimuli. The therapist and patient then built a hierarchy of avoided situations. One situation was chosen, and the patient carried out exposure using the library of images and media components that are stored in the i-VR Argaman environment. The therapist and patient monitored SUDS ratings. The patient continued this exposure task in the i-VR Argaman space as homework. In the third and fourth sessions, the rationale for building a trauma narrative was given, and the patient narrated the trauma using the Virtual Reality components of the environment. This included two scenes, showing a car crash from above and from the first-person perspective. In session IV the patient was also introduced to the importance of thoughts and the therapist showed the patient how to record their thoughts. In the final session, the patient and therapist worked on thought challenging, discussed the intervention, identified areas that the patient should continue to work on, and discussed techniques for relapse prevention (Figures 1–3).
2.4 Procedure
The telephone interview team called suitable ER patients within 2 weeks of their traumatic event, and an initial telephone assessment determined whether the individual met study criteria. After receiving verbal informed consent, participants were given the details of a secure internet site, where they were asked to fill out questionnaires including the PCL-5 assessing PTSD symptoms. Subjects with a PCL-5 score greater than 33 or K6 over five were invited for a second telephone assessment. During this assessment, the patient was assessed with the SCID I and CAPS-5. Patients who fulfilled the inclusion criteria were invited to join the randomized controlled trial. Subjects who entered the trial received a detailed description of the study, and if interested in participating, they signed informed consent. All clinical interviews were carried out by the telephone interview team, who remained blind to treatment condition.
Patients were randomly assigned by computer to one of the two treatment arms. Patients in the Waitlist condition filled out questionnaires via the secure internet site once a week. These were checked by a team member dedicated to this task, who was able to contact these patients should a specific need arrive. Patients in the i-VR arm received a laptop computer for the duration of the treatment, with the i-VR Argaman program loaded on. They received training in how to access it, and a time for the first i-VR session was made. The five i-VR sessions were carried out by experienced CBT therapists, all of whom were trained in TF-CBT, had extensive experience in protocol driven research trials, and received weekly supervision from SF.
Follow up assessment was conducted by the telephone interview team in clinical telephone interviews, 2 weeks following the end of treatment, and again 6, and 12 months later (CONSORT diagram).
2.5 Research tools
2.5.1 Self-report questionnaires (these were administered via a secure internet site)
K6: (Mewton et al., 2015): This is a six-item questionnaire designed to assess levels of non-specific distress. A cut-off score of five indicates moderate mental distress (Prochaska et al., 2012).
PCL-5 (Blevins et al., 2015) This is a 20-item self-report questionnaire, assessing PTSD symptoms according to DSM 5 (American Psychiatric Association, 2013). A cut off score of 33 indicates probable PTSD.
2.5.2 Clinical interviews
Patients were assessed by telephone, before treatment and after treatment, and 6, and 12 months following the end of treatment. These interviews were carried out by trained psychologists, who remained blind to treatment condition. The following instruments were used:
SCID I: The Structured Clinical Interview for DSM-IV (First and Gibbon, 2004) is used to evaluate the current and lifetime presence or absence of Axis I disorders. The Hebrew version (Shalev et al., 1996) has been used in many studies. The SCID is considered to be the gold standard when evaluating Axis I Disorders.
CAPS 5: The Clinicians’ Administered PTSD Scale (CAPS 5, (Weathers et al., 2018), is a 30 item semi-structured interview that confers a diagnosis of PTSD according to DSM 5 (American Psychiatric Association, 2013) and a continuous measure of PTSD symptoms’ frequency and intensity.
3 Results
3.1 Recruitment
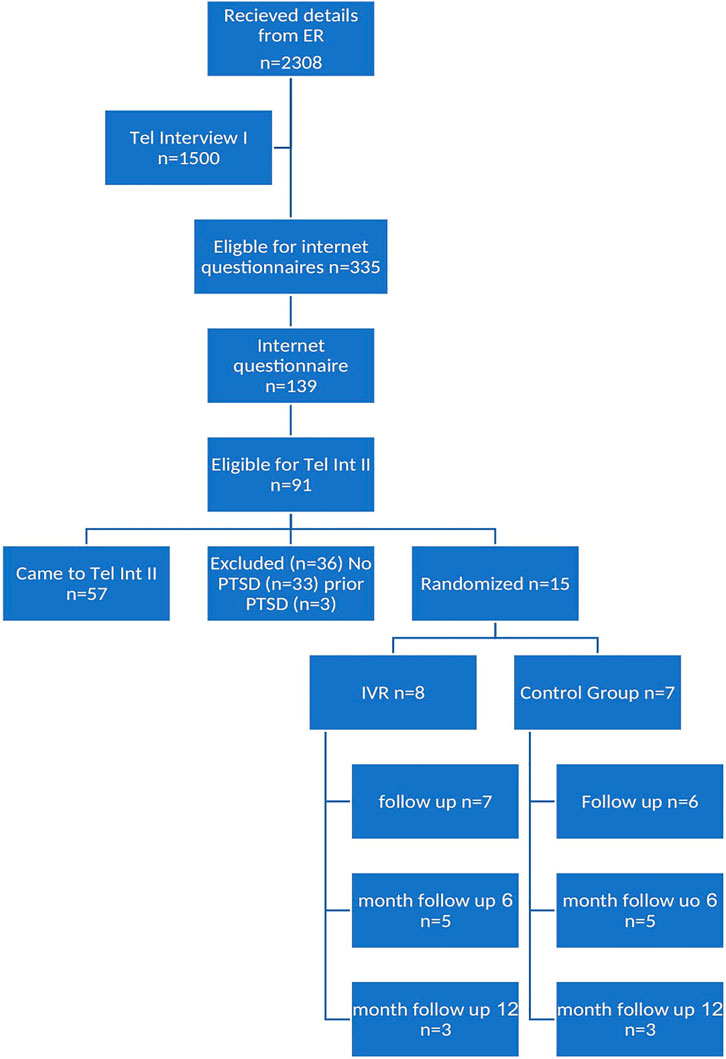
As can been see in the CONSORT diagram (Figure 4), over 2000 patients who came to the Emergency Room following a motor vehicle accident were identified as potential subject. The research team were able to carry out the first telephone interview with 1,500 (65%).
3.2 Telephone interview I
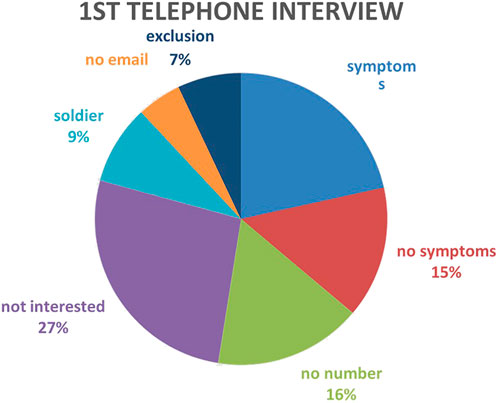
Figure 5 illustrates the outcome of the telephone call with these subjects: 249 (16.6%) did not have any symptoms of PTSD and therefore were not followed up further. 729 subjects (48.6%) met other exclusion criteria: 424 (28.3%) did not speak Hebrew fluently, 120 (0.08%) did not have access to email, 185 (12.3%) were soldiers. A further 182 subjects (12%) did not want to participate in the research. A total of n = 335 (22.3%) were symptomatic and fit inclusion criteria. A link to the online questionnaires was sent to all these subjects.
3.3 Online assessment (within 3 weeks of the traumatic event)
Subjects who met study criteria were given a link to a secure internet site where there was a link to answer questionnaires. Each subject (n = 335) who was given the link to the online questionnaires was also given up to three reminders to answer them, in the 2 weeks following the telephone interview. 196 subjects (58.5%) did not fill in the online questionnaires. 139 subjects (41.4%) filled out the PCL5.
3.4 Telephone interview II
91 subjects were invited to a clinical interview. n = 41 (41.8%) declined to participate. Of those who did participate (n = 57, 58.2%), 33 (57.9%) did not meet criterion for PTSD. Three patients had PTSD related to a prior event. 21 subjects (36.8%) had PTSD. At the beginning of the study, six patients were not randomized—one dropped out before randomization, two were referred elsewhere for longer term treatment, and three were treated by iVR as pilot patients.
3.5 Treatment in the RCT
Fourteen subjects were randomized to the two arms of the study: seven to the control group, and seven to the intervention group. The control group were contacted by a member of the research team and completed weekly online questionnaires. The treatment group received the intervention as described above.
3.6 Follow up
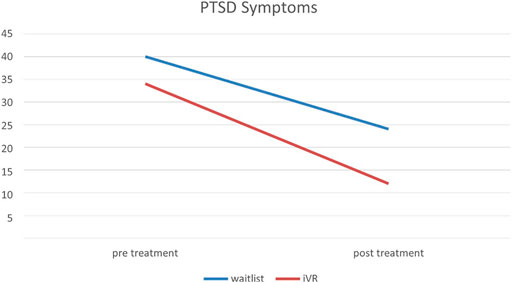
All subjects completed a post treatment clinical assessment. As can be seen in the CONSORT diagram, few subjects came to follow up assessments, these are therefore not reported here. A repeated analysis of variance, examining CAPS total scores at time 1 (pre treatment) and time 2 (post treatment) show a significant effect of Time [F (8) = 9.35, p < 0.05] but no significant effect of group [F (8) = 0.001, ns] (Figure 6).
4 Discussion
This study aimed to examine the feasibility and effectiveness of an internet based Virtual Reality treatment to prevent PTSD. As far as these authors are aware, this is the first time VR treatment for PTSD has been delivered remotely.
The results indicate that internet based VR treatment is acceptable: only one patient did not complete all five sessions, and none dropped out. This is very unusual for a treatment for PTSD, where conventional treatment can be rejected by as many as 40% of recruited subjects (Shalev et al., 2012).
One major challenge for treatment that attempts to prevent PTSD is that they have to be shown to be better than natural recovery (Freedman, 2019). In this study, both waitlist control and the iVR treatment led to significantly lower levels of PTSD. There were no significant differences between the groups, probably as a result of the small numbers of patients treated. Since the trend is in the right direction, this system needs to be further examined in a larger population, as well as with patients suffering from chronic PTSD. These results are similar to the only other study that has examined internet-based treatment for the prevention of PTSD (Mouthaan et al., 2013).
The small subject numbers can be attributed to a number of factors. Firstly, almost 13% of subjects initially contacted either had no email or internet-based interaction, and so were automatically disqualified from participating in the study, or were not interested in participating. Comparable trials with the same population for a non internet based intervention had significantly greater uptake. Secondly, when offering an internet-based intervention, we were anxious to exclude subjects who were not comfortable with using technology. As a result, we included an extra recruitment stage of online questionnaires. This was intended to identify those subjects who could not manage or want to participate in an internet-based project. We anticipated a relatively small percentage of subjects would not participate in this stage. The results of this study show unequivocally that these initial assumptions were incorrect: almost 60% of those sent a link to the online questionnaires did not fill them out. These data were unexpected and had the unfortunate result of reducing our potential pool of patients. However, these data are of utmost importance, since they indicate that therapy using the internet is not that acceptable in this population. Since this platform was expected to overcome barriers to treatment, it is important to note that this does not appear to be the case. Similar results have been found elsewhere, e.g., a large study in Australia (n> 7,000) showing 25% acceptance levels for an internet based intervention (Titov et al., 2015).
It is important to note, however, that this extra stage designed to identify those subjects who were suitable for internet-based intervention, was extremely effective. No subject dropped out at the stage of randomization. In most randomized controlled trials, including previous studies carried out on this population, a significant percentage of patients (up to 30%) decline treatment at this stage. In addition, only one patient did not complete all five sessions. This indicates that the recruitment strategy was successful in identifying patients who were suitable for this intervention.
This study succeeded in recruiting 1,050 potential patients, the iVR system is acceptable and works well. iVR treatment results in a reduction in PTSD symptoms. However, more work needs to be carried out regarding the acceptability of internet-based systems for intervention for psychological disorders, and further research is needed to examine the effectiveness of iVR versus other types of therapy or natural recovery.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Hadassah University Hospital Helsinki Committee. The patients/participants provided their written informed consent to participate in this study.
Author contributions
SF is the senior author on this paper. ED provided the software, contributed to the design of iVR and the overall running of the study, RE contributed to the writing of the paper.
Funding
This study received funding from the Israel Internet Association. The funder was not involved in the study design, collection, analysis, interpretation of data, the writing of this article or the decision to submit it for publication. All authors declare no other competing interests.
Conflict of interest
ED was employed by the Sonarion Ltd.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders. 5th Edn. Arlington, VA: Author.
Blevins, C. A., Weathers, F. W., Davis, M. T., Witte, T. K., and Domino, J. L. (2015). The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. J. Trauma. Stress 28, 489–498. doi:10.1002/jts.22059
First, M. B., and Gibbon, M. (2004). “The structured clinical interview for DSM-IV axis I disorders (SCID-I) and the structured clinical interview for DSM-IV axis II disorders (SCID-II),” in Comprehensive handbook of psychological assessment. Editors Hilsenroth, M. J., and Segal, D. L. Personality assessment. (John Wiley & Sons, Inc.), 2, 134–143.
Freedman, S. A. (2019). Psychological interventions to prevent PTSD. Psychiatr. Ann. 49 (7), 314–319. doi:10.3928/00485713-20190528-01
Hoge, C. W., Castro, C. A., Messer, S. C., McGurk, D., Cotting, D. I., Koffman, R. L., et al. (2004). Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N. Engl. J. Med. Overseas. Ed. 351, 13–22. doi:10.1056/NEJMoa040603
Kashdan, T. B., and Kane, J. Q. (2011). Posttraumatic distress and the presence of posttraumatic growth and meaning in life: Experiential avoidance as a moderator. Personality Individ. Differ. 50 (1), 84–89. doi:10.1016/j.paid.2010.08.028
Kazdin, A. E., and Blase, S. L. (2011). Rebooting psychotherapy research and practice to reduce the burden of mental illness. Perspect. Psychol. Sci. 6, 21–37. doi:10.1177/1745691610393527
Lewis, C., Roberts, N. P., Andrew, M., Starling, E., and Bisson, J. I. (2020). Psychological therapies for post-traumatic stress disorder in adults: Systematic review and meta-analysis. Eur. J. Psychotraumatol. 10, 1729633. doi:10.1080/20008198.2020.1729633
Lewis, C., Roberts, N. P., Simon, N., Bethell, A., and Bisson, J. (2019). Internet-delivered cognitive behavioural therapy for post-traumatic stress disorder: Systematic review and meta-analysis. Acta Psychiatr. Scand. 140, 508–521. doi:10.1111/acps.13079
Mewton, L., Kessler, R. C., Slade, T., Hobbs, M. J., Brownhill, L., Birrell, L., et al. (2015). The psychometric properties of the kessler psychological distress scale (K6) in a general population sample of adolescents. Psychol. Assess. 28, 1232–1242. doi:10.1037/pas0000239
Mouthaan, J., Sijbrandij, M., de Vries, G.-J., Reitsma, J. B., van de Schoot, R., Goslings, J. C., et al. (2013). Internet-based early intervention to prevent posttraumatic stress disorder in injury patients: Randomized controlled trial. J. Med. Internet Res. 15 (8), e165. doi:10.2196/jmir.2460
Prochaska, J. J., Sung, H. Y., Max, W., Shi, Y., and Ong, M. (2012). Validity study of the K6 scale as a measure of moderate mental distress based on mental health treatment need and utilization. Int. J. Methods Psychiatr. Res. 21 (2), 88–97. doi:10.1002/mpr.1349
Rothbaum, B. O., Rizzo, A. S., and Difede, J. (2010). Virtual reality exposure therapy for combat-related posttraumatic stress disorder. Ann. N. Y. Acad. Sci. 1208, 126–132. doi:10.1111/j.1749-6632.2010.05691.x
Shalev, A. Y., Peri, T., Canetti, L., and Schreiber, S. (1996). Predictors of PTSD in injured trauma survivors: A prospective study. Am. J. Psychiatry 153 (2), 219–225. http://www.ncbi.nlm.nih.gov/pubmed/8561202. doi:10.1176/ajp.153.2.219
Shalev, A. Y., Ankri, Y., Israeli-Shalev, Y., Peleg, T., Adessky, R., and Freedman, S. (2012). Prevention of posttraumatic stress disorder by early treatment: Results from the jerusalem trauma outreach and prevention study. Arch. Gen. Psychiatry 69 (2), 166. doi:10.1001/archgenpsychiatry.2011.127
Shalev, A. Y., Ankri, Y. L. E., Peleg, T., Israeli-Shalev, Y., and Freedman, S. (2011). Barriers to receiving early care for PTSD: Results from the jerusalem trauma outreach and prevention study. Psychiatr. Serv. 62 (7), 765–773. doi:10.1176/ps.62.7.pss6207_0765
Titov, N., Dear, B. F., Staples, L. G., Bennett-Levy, J., Klein, B., Rapee, R. M., et al. (2015). MindSpot clinic: An accessible, efficient, and effective online treatment service for anxiety and depression. Psychiatr. Serv. 66 (10), 1043–1050. doi:10.1176/appi.ps.201400477
Keywords: internet, PTSD, prevention, RCT, virtual reality
Citation: Freedman SA, Dayan E and Eitan R (2022) An internet based virtual reality intervention for preventing posttraumatic stress disorder. Front. Virtual Real. 3:831051. doi: 10.3389/frvir.2022.831051
Received: 07 December 2021; Accepted: 15 July 2022;
Published: 02 September 2022.
Edited by:
Raúl Duron-Figueroa, National Autonomous University of Mexico, MexicoReviewed by:
Laura E. Watkins, Emory University, United StatesAngelo Lavano, University of Magna Graecia, Italy
Copyright © 2022 Freedman, Dayan and Eitan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sara A. Freedman, c2FyYS5mcmVlZG1hbkBiaXUuYWMuaWw=
 Sara A. Freedman
Sara A. Freedman Ehud Dayan2
Ehud Dayan2 Renana Eitan
Renana Eitan