- 1Naval Submarine Medical Research Laboratory, Naval Submarine Base New London, Groton, CT, United States
- 2Design Interactive, Inc., Orlando, FL, United States
Editorial on the Research Topic
Cybersickness in Virtual Reality and Augmented Reality
Introduction
Early virtual reality (VR) systems introduced abnormal visual-vestibular integration and vergence-accommodation, causing cybersickness (McCauley and Sharkey, 1992) reminiscent of simulator sickness reported by military pilots, e.g., having some shared causes and overlapping (Lawson, 2014a) but distinguishable symptoms (Stanney et al., 1997). Improved processing, head tracking, and graphics were expected to overcome cybersickness (Rheingold, 1991), yet it persists in today’s much-improved VR (Stanney et al., 2020a, 2020b). This must be resolved, because VR and Augmented Reality (AR)1 are proliferating for training for stressful tasks, exposure therapy for post-traumatic stress, remote assistance/control, and operational situation awareness (Hale and Stanney, 2014; Beidel et al., 2019; Stanney et al., 2020b, 2021; NATO Science and Technology Office, 2021).
Experts considered the cybersickness problem recently at a 2019 Cybersickness Workshop2 and a 2020 Visually-Induced Motion Sensations meeting.3 Military aspects were discussed during 2019–2021 meetings of a Cybersickness Specialist Team (NATO Science and Technology Office, 2021). The Bárány Society’s Classification Committee just developed relevant international symptom standards for visually-induced motion sickness (VIMS; Cha et al., 2021). Finally, >40 authors produced twelve articles comprising this Frontiers Research Topic initiated by Dr. Stanney. Below, we summarize their work and provide recommendations.
Comments on the 12 Topic Articles
Three Articles Explored The Benefits Of Ambient Or Earth-Referenced Visual Cues
1) Hemmerich et al. found that an Earth-fixed visual horizon (but not a non-horizon cue) significantly reduced cybersickness.4 2) Shahnewaz Ferdous et al. posited that Earth-stable cues introduced into VR or AR (via a partial virtual frame) should improve balance and lessen cybersickness. They discussed two small studies of balance-impaired VR/AR users. Their VR study detected a cueing difference for two balance measures and the Simulator Sickness (SSQ) Disorientation measure5, while their AR study (which allowed sight of the room) detected a difference in one balance measure but no SSQ measures. Benefits were seen only with balance-impaired subjects. While the findings were mixed, an appropriately-designed Earth-referenced cue should aid orientation. Expanded studies of this type should compare similar VR-versus-AR fields of view. Finally, 3) Cao et al. provided VR users with Earth-stable granulated peripheral cues that allowed some peripheral vision, which improved visual target searching better than restricting field-of-view (FOV), a typical countermeasure. Could this approach also mitigate cybersickness better than FOV restriction?
Two Articles Discussed Aspects Of Tracking Latency As A Cybersickness Contributor
4) Stauffert et al. explored cybersickness implications of latency between the movement of a tracked object and its movement on a head-worn display. They provided information to assist in assessing latency, and stressed the need for comparable assessments. 5) Palmisano et al. posited that a key (and readily quantifiable) contributor to cybersickness is a large, temporally inconsistent difference between actual and virtual head position. Their findings are relevant to Moss et al. (2011), who found that varying head tracking latency was sickening. As many studies have observed that visually-moving fields elicit symptoms even when the head is still (e.g., Webb and Griffin, 2002), however, the contribution of visual field motion versus head position/motion conflict should be studied.
Three Articles Explored Additional Effects Of Head Motion, Head Orientation, Or Head-Mounting Of Displays
6) Kim et al. posited that linear head oscillations increase sensory conflict in VR devices that only track angular motion. While they failed to detect device-related differences in perceived scene stability, spatial presence, or cybersickness, this was a creative pilot study exploring implications of different tracking devices. 7) Wang et al. confirmed that vection (the illusion of self-motion) elicited by viewing a rotating dot pattern was stronger when concordant with expected graviceptive cues. VR/AR designers should know that when vection is desired, its direction should not contradict somatosensory/vestibular cues that would be present during real motion. Also, specific motion/orientation perceptions will tend to be altered to minimize sensory conflict (Young et al., 1975; Lackner and Teixeira, 1977; Dizio and Lackner, 1986; Howard et al., 1987; Golding, 1996; Tanahashi et al., 2012). The notion that vection can reduce sickening conflict is better supported than vection as a cause of sickness (Lawson, 2014a; Stanney et al., 2020b). Finally, 8) Hughes et al. evaluated head-worn versus tablet-based AR during tactical combat casualty training. They observed greater sickness with head-worn AR, but symptoms for both devices were mostly limited to the Oculomotor cluster of the SSQ, with little Nausea. Moreover, while subjects in the head-worn condition completed fewer training scenarios in the time allotted, they had more correct responses in completed scenarios. AR could be a less-sickening training approach, and solutions to mitigate oculomotor disturbances would make it even better.
Three Articles Explored The Role Of Active Sensorimotor Engagement Or Maintenance Of Postural Equilibrium
9) Curry et al. evaluated participants in a head-worn racing game. They did not detect main differences in cybersickness between active drivers versus passengers. The reasons for this should be explored, as a difference has been observed in other contexts (Rolnick and Lubow, 1991; Stanney and Hash, 1998; Seay et al., 2002; Sharples et al., 2008). 10) Weech et al. found a correlation between visually-influenced body sway (reflected by the center-of- pressure [COP] ratio)6 and SSQ Disorientation and Oculomotor sub-scores in a VR. It makes sense for the Disorientation score to be related to sway; expanded studies should determine if COP ratio correlates with SSQ Total Sickness or Nausea scores, as these are likely to predict quitting a training session. Finally, 11) Jasper et al. evaluated the efficacy of different cybersickness recovery strategies. Their study elicited sufficient cybersickness (Stanney et al., 2003). Greatest recovery was observed for resting with the VR off (real natural decay), while doing a virtual hand-eye task yielded the least recovery. We agree with the authors’ implication that administration of the SSQ during VR/AR should be explored further.
Three Studies Addressed The Role Of Individual Cybersickness Susceptibility (Two Of Which Were Mentioned Immediately Above)
12) Golding et al. found that sickness severity in a moving visual surround is predicted by history of susceptibility to motion sickness, migraine, and fainting. They did not detect a relationship between sickness and vection, adding to the many studies failing to find this relation (Lawson, 2014a; Stanney et al., 2021).7 Consistent with the literature (Lawson, 2014a; Stanney et al., 2020a), the aforementioned article #11 by Jasper et al. and #9 by Curry et al. observed mixed findings concerning sex as a factor in cybersickness susceptibility. Jasper et al. observed that women reported more cybersickness, but this was confounded by women having less experience with video games. The sex difference detected in Curry et al. was solely among the subset of subjects who discontinued participation early, wherein women quit earlier when driving, but not when passengers. Future studies of individual cybersickness differences should estimate variance accounted for by experience with motion sickness, driving, video games, and head-worn displays.
Causal Hypotheses Relevant to the 12 Topic Articles
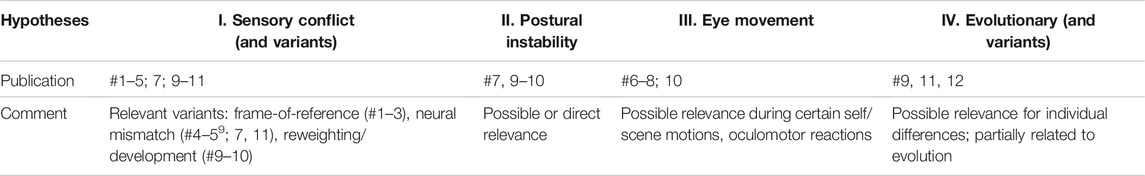
While the explanatory capabilities of a complete motion/simulator/cybersickness theory have been described (Lawson, 2014a), there is no universally accepted theory. Six hypotheses were discussed by Stanney et al. (2021) and ten by Keshavarz et al. (2014). Most of these can be grouped into four established categories (Table 26.1, Keshavarz et al.), which in Table 1 are linked to the 12 articles in this Research Topic. This taxonomy may aid further literature inquiries concerning theoretical implications.8
Concluding Recommendations to the Research Community
We thank the authors for contributing many provocative studies. As is common in research, as many questions were raised as were answered. Answering the key cybersickness questions requires controlled, labor-intensive research entailing:
1. Assessment of relevant stimulus experiences (Jasper et al.) and past susceptibility (Golding et al.): This is vital to interpretation and such measures can be used as covariates to improve analyses.
2. Larger samples (e.g., Moss and Muth, 2011) than have commonly been employed (e.g., Kim et al.; Shahnewaz Ferdous et al.), in order to deal with high individual variability in susceptibility (Lawson, 2014a).
3. Stimuli that elicit functionally relevant cybersickness (Stanney et al., 201410), to avoid basement effects or detection of statistical differences lacking clear functional significance (e.g., Hemmerich et al.).
4. Managing sessions and session intervals to reduce carry-over effects which may confound studies with many cybersickness sessions held closely together (e.g., Hemmerich et al.; Kim et al.). Sickening VR or simulator studies should ideally limit the number of sessions to three (Lawson et al., 200911) and allow 1 week of recovery between sessions, to reduce visual-vestibular and vergence-accommodation carry-over effects due to adaptation (Dai et al., 2011) or sensitization (Dizio and Lackner, 2000), as well as learning, fatigue, classical conditioning, subject attrition, and ultradian variation (Lawson et al., 2009; Lawson, 2014a) (Comparable session guidelines need to be established for AR studies.)
5. Careful establishment of measures, e.g., whenever “objective” indicators of cybersickness are considered (Stauffert et al.; Shahnewaz Ferdous et al.; Hemmerich et al.); researchers should realize that specificity needs more emphasis (Bos and Lawson, 2021), and an established symptom scale is required for validation (Lawson, 2014b).
Author Contributions
All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
Author Disclaimer
The views expressed in this document are those of the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, nor the US. Government. Dr. Lawson is an employee of the US. Government. This work was prepared as part of his official duties. Title 17 US. C. 1O5 provides that “Copyright protection under this title is not available for any work of the United States Government.”
Conflict of Interest
KS was employed by the Design Interactive, Inc.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors thank fellow editors Charles M. Oman, Ph.D. (Mann-Vehicle Laboratory, Massachusetts Institute of Technology), Stephan Palmisano (University of Wollongong, Australia), and Douglas A. Bowman (Virginia Tech) for ably shepherding some of the papers in this research topic.
Footnotes
1AR overlays virtual images on a partial view of the real world. While AR often causes less visual-vestibular conflict, vergence-accommodation problems may persist.
2https://s2019.siggraph.org/conference/programs-events/organization-events/frontiers-workshops/cybersickness-causes-and-solutions/
3https://ieda.ust.hk/dfaculty/so/VIMS2020/
4A VR was used. Our recommendations for futures studies of this type are at the end of this editorial.
5Four measures are yielded by SSQ (Total Sickness Score, Disorientation score, Nausea Score, and Oculomotor score) (Kennedy et al., 1993). Five within-device balance-related measures were tried (two sway measures, one sway-driven dodgeball task, and one questionnaire).
6Defined as the amount of sway associated with visual scene oscillation, where a high ratio implies an inability to down-weigh visual information and is a hypothesized cybersickness contributor.
7Curry et al. (#9) also posit that their findings are (indirectly) inconsistent with a causal cybersickness role for vection.
8Stanney et al. and Keshavarz et al. provide (and evaluate) the source materials.
9Palmisano et al. (#5) hypothesize a new conflict between virtual versus physical head pose.
10Moderate-to-medium cybersickness severity occurs at 20–28 SSQ points (Table 31.3), and 20 points is where some subjects would quit (personal communication, Dr. Stanney, 1 May 2020).
11See p. 16–17.
References
Beidel, D. C., Frueh, B. C., Neer, S. M., Bowers, C. A., Trachik, B., Uhde, T. W., et al. (2019). Trauma Management Therapy with Virtual-Reality Augmented Exposure Therapy for Combat-Related PTSD: A Randomized Controlled Trial. J. Anxiety Disord. 61, 64–74. doi:10.1016/j.janxdis.2017.08.005
Bos, J. E., and Lawson, B. D. (2021). “Symptoms and Measurement, in NATO Science and Technology Office,”. Peer-reviewed Final Report of the Human Factors and Medicine Panel/Modeling & Simulations Group in Guidelines for Mitigating Cybersickness in Virtual Reality Systems. Brussels, Belgium: NATO Science and Technology Organization. Activity Number 323 (NATO STO-TR-HFM-MSG-323). Chapter 4.
Cha, Y.-H., Golding, J., Keshavarz, B., Furman, J., Kim, J.-S., Lopez-Escamez, J. A., et al. (2021). Motion Sickness Diagnostic Criteria: Consensus Document of the Classification Committee of the Bárány Society. VES, 1–17. doi:10.3233/VES-200005
Dai, M., Raphan, T., and Cohen, B. (2011). Prolonged Reduction of Motion Sickness Sensitivity by Visual-Vestibular Interaction. Exp. Brain Res. 210 (3-4), 503–513. doi:10.1007/s00221-011-2548-8
Dizio, P. A., and Lackner, J. R. (1986). Perceived Orientation, Motion, and Configuration of the Body during Viewing of an Off-Vertical, Rotating Surface. Perception Psychophys. 39 (1), 39–46. doi:10.3758/BF03207582
Dizio, P., and Lackner, J. R. (2000). “Motion Sickness Side Effects and Aftereffects of Immersive Virtual Environments Created with Helmet-Mounted Visual Displays,”. Published in RTO MP-54 in Proceedings, RTO HFM Workshop on "The Capability of Virtual Reality, to Meet Military Requirements, April 20–25, 2002, Minneapolis, MN Available at: https://apps.dtic.mil/sti/pdfs/ADP010619.pdf.
Golding, J. F., and Markey, H. M. (1996). Effect of Frequency of Horizontal Linear Oscillation on Motion Sickness and Somatogravic Illusion. Aviat Space Environ. Med. 67 (2), 121–126.
Hale, K. S., and Stanney, K. M. (2014). Handbook of Virtual Environments: Design, Implementation, and Applications. Second edition. New York, NY: CRC Press. doi:10.1201/b17360
Howard, I. P., Cheung, B. S. K., and Landolt, J. (1987). Influence of Vection axis and Body Posture on Visually Induced Self-Rotation and Tilt. Advisory Group Aerospace Res. Develop. 433, 15-1–15-8.
Kennedy, R. S., Lane, N. E., Berbaum, K. S., and Lilienthal, M. G. (1993). Simulator Sickness Questionnaire: An Enhanced Method for Quantifying Simulator Sickness. Int. J. Aviation Psychol. 3, 203–220. doi:10.1207/s15327108ijap0303_3
Keshavarz, B., Hecht, H., and Lawson, B. D. (2014). “Ch 26: Visually Induced Motion Sickness: Causes, Characteristics, and Countermeasures,” In: Handbook of Virtual Environment: Design, Implementation, and Applications. Editors K. S. Hale, and K. M. Stanney Boca Raton, FL: CRC Press, 648–681.
Lackner, J. R., and Teixeira, R. A. (1977). Optokinetic Motion Sickness: Continuous Head Movements Attenuate the Visual Induction of Apparent Self-Rotation and Symptoms of Motion Sickness. Aviat Space Environ. Med. 48, 248–253.
Lawson, B. D. (2014a). “Motion Sickness Symptomatology and Origins,” in Handbook of Virtual Environments: Design, Implementation, and Applications. Editors K. S. Hale, and K. M. Stanney Second edition (New York, NY: CRC Press), 531–600.
Lawson, B. D. (2014b). “Motion Sickness Scaling,” in Handbook of Virtual Environments: Design, Implementation, and Applications. Editors K. S. Hale, and K. M. Stanney Second edition (New York, NY: CRC Press), 601–626.
Lawson, B. D., McGee, H. A., Castaneda, M. A., Golding, J. F., Kass, S. J., and McGrath, C. M. (2009). Evaluation Of Several Common Anti-motion Sickness Medications and Recommendations Concerning Their Potential Usefulness during Special Operations (NAMRL-09-15). Pensacola, FL: Naval Aerospace Medicine Research Laboratory.
McCauley, M. E., and Sharkey, T. J. (1992). Cybersickness: Perception of Self-Motion in Virtual Environments. Presence: Teleop. Vir. Environ. 1 (3), 311–318. doi:10.1162/pres.1992.1.3.311
Moss, J. D., Austin, J., Salley, J., Coats, J., Williams, K., and Muth, E. R. (2011). The Effects of Display Delay on Simulator Sickness. Displays 32 (4), 159–168. doi:10.1016/j.displa.2011.05.010
Moss, J. D., and Muth, E. R. (2011). Characteristics of Head-Mounted Displays and Their Effects on Simulator Sickness. Hum. Factors 53, 308–319. doi:10.1177/0018720811405196
NATO Science and Technology Office (2021). Guidelines for Mitigating Cybersickness in Virtual Reality Systems. Peer-reviewed Final Report of the Human Factors and Medicine Panel/Modeling & Simulations Group, Activity Number 323 (NATO STO-TR-HFM-MSG-323).
Rolnick, A., and Lubow, R. E. (1991). Why Is the Driver Rarely Motion Sick? the Role of Controllability in Motion Sickness. Ergonomics 34, 867–879. doi:10.1080/00140139108964831
Seay, A. F., Krum, D. M., Hodges, L., and Ribarsky, W. (2002). “Simulator Sickness and Presence in a High Field-Of-View Virtual Environment,” in Proceedings of the CHI’02 Extended Abstracts on Human Factors in Computing Systems, April 2002 (New York, NY: ACM), 784–785. doi:10.1145/506443.506596
Sharples, S., Cobb, S., Moody, A., and Wilson, J. R. (2008). Virtual Reality Induced Symptoms and Effects (VRISE): Comparison of Head Mounted Display (HMD), Desktop and Projection Display Systems. Displays 29, 58–69. doi:10.1016/j.displa.2007.09.005
Stanney, K., Fidopiastis, C., and Foster, L. (2020a). Virtual Reality Is Sexist: but it Does Not Have to Be. Front. Robot. AI 7, 4. doi:10.3389/frobt.2020.00004
Stanney, K., Kennedy, R., and Hale, K. (2014). “Virtual Environment Usage Protocols,” in Handbook of Virtual Environments: Design, Implementation, and Applications. Editors K. S. Hale, and K. M. Stanney Second edition (New York: NY: CRC Press), 797–809. doi:10.1201/b1736010.1201/b17360-38
Stanney, K., Lawson, B. D., Rokers, B., Dennison, M., Fidopiastis, C., Stoffregen, T., et al. (2020b). Identifying Causes of and Solutions for Cybersickness in Immersive Technology: Reformulation of a Research and Development Agenda. Int. J. Human Comput. Interaction 36 (19), 1783–1803. doi:10.1080/10447318.2020.1828535
Stanney, K. M., and Hash, P. (1998). Locus of User-Initiated Control in Virtual Environments: Influences on Cybersickness. Presence 7 (5), 447–459. doi:10.1162/105474698565848
Stanney, K. M., Kennedy, R. S., and Drexler, J. M. (1997). Cybersickness Is Not Simulator Sickness. Proc. Hum. Factors Ergon. Soc. Annu. Meet. 41 (2), 1138–1142. doi:10.1177/107118139704100292
Stanney, K. M., Nye, H., Haddad, S., Hale, K. S., Padron, C. K., and Cohn, J. V. (2021). “Extended Reality (Xr) Environments,” in Handbook of Human Factors and Ergonomics. Editors G. Salvendy, and W. Karwowski 5th edition (New York: John Wiley), 782–815. doi:10.1002/9781119636113.ch30
Stanney, K. M., Kingdon, K., Nahmens, I., and Kennedy, R. S. (2003). What to Expect From Immersive Virtual Environment Exposure: Influences of Gender, Body Mass Index, and Past Experience. Human Factors 45 (3), 504–522.
Tanahashi, S., Ujike, H., and Ukai, K. (2012). Visual Rotation axis and Body Position Relative to the Gravitational Direction: Effects on Circular Vection. I-Perception 3 (10), 804–819. doi:10.1068/i0479
Webb, N. A., and Griffin, M. J. (2002). Optokinetic Stimuli: Motion Sickness, Visual Acuity, and Eye Movements. Aviat Space Environ. Med. 73 (4), 351–358.
Keywords: cybersickness, virtual reality, augmented reality, postural instability, vection, adverse aftereffects, simulator sickness, visual acuity in head mounted displays
Citation: Lawson BD and Stanney KM (2021) Editorial: Cybersickness in Virtual Reality and Augmented Reality. Front. Virtual Real. 2:759682. doi: 10.3389/frvir.2021.759682
Received: 16 August 2021; Accepted: 20 September 2021;
Published: 13 October 2021.
Edited by:
Mel Slater, University of Barcelona, SpainReviewed by:
Joan Llobera, University of Barcelona, SpainCopyright © 2021 Lawson and Stanney. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ben D. Lawson, YmVudG9uLmQubGF3c29uLmNpdkBtYWlsLm1pbA==
 Ben D. Lawson
Ben D. Lawson Kay M. Stanney
Kay M. Stanney