
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Virtual Real., 05 October 2021
Sec. Virtual Reality in Medicine
Volume 2 - 2021 | https://doi.org/10.3389/frvir.2021.719681
This article is part of the Research TopicVirtual Reality Applications in Military and Veteran Medicine and HealthcareView all 8 articles
Objectives: The primary objective of this evaluation is to determine the impact of virtual reality (VR) distraction on acute and chronic pain in Veterans within the Veterans Affairs Health Care System (VA). A secondary objective is to determine the impact of VR on the experience of stress and anxiety in Veterans utilizing VR for the indication of pain. A third objective is to develop an understanding of the Veteran experience of using VR in a healthcare setting.
Methods: This prospective, pretest-posttest mixed methods assessment was performed at a VA medical center from August 30, 2019 to November 23, 2020. VR experiences lasted between 10 and 30 min utilizing an immersive head-mounted display with multiple, autonomously chosen virtual environments. Qualitative data was collected concurrently to provide context to quantitative measures which included pain scores and stress/anxiety levels. Data from 79 participants was included in this analysis. Data included pre- and post-VR session Defense and Veterans Pain Rating Scale and stress/anxiety levels.
Results: Results for the cohort demonstrated a statistically significant decrease in pain intensity (p <0 .001) with an average 12% decrease in pain levels and an 92% reduction in anxiety for those in concurrent pain.
Conclusion: VR as a non-pharmacological adjunct or alternative modality, appears to be a viable option for improving pain management and reducing anxiety in Veteran populations across various age ranges, and levels of acuity and chronicity. VR was found to be an effective distraction from pain, a pleasurable experience for the majority, and opened the door to other non-pharmacological modalities in a Veteran population.
There is a growing interest in virtual reality (VR) interventions as a non-pharmacological adjunct or alternative for pain management (Trost et al., 2021). VR immerses users in computer-generated, three-dimensional interactive environments by simultaneously engaging visual, auditory, and sometimes tactile senses (Hoffman et al., 2006; Indovina et al., 2018; Tack, 2019). As a distraction therapy, VR technology provides a sense of immersion (sensorial fidelity of the technology) and presence (the perception of being physically present in the virtual environment) to decrease adverse outcomes such as pain and anxiety (Hoffman et al., 2006; Indovina et al., 2018; Tack, 2019).
Pain has a significant effect on health and wellbeing and prolonged pain results in substantial psychological distress (Gureje, 1999). Patients in pain experience stress, anxiety, and depression (Sündermann et al., 2018). An estimated 20% of the world’s population lives in chronic pain (Goldberg and McGee, 2011) and 17.6% of those in chronic pain in the U.S. rate their pain as severe (Nahin, 2015; Becker et al., 2017). Traditional treatments for pain have relied on medications, in particular opioids, or invasive interventions, such as nerve blocks or epidural injections, each with their own risk profile (Benyamin et al., 2008; Bellini and Barbieri, 2013; Jung et al., 2014; Teater, 2014; Webster, 2017; Liberman et al., 2019; Chuan et al., 2020; Smith et al., 2020). In light of the current opioid overdose death crisis, there is an urgent need for implementation of noninvasive complementary and alternative modalities for the treatment of pain, both acute and chronic.
VR was first effectively used to treat pain in burn patients (Hoffman, 1998; Hoffman et al., 2000). Subsequently, VR has demonstrated effectiveness as a pain treatment modality in surgical and procedural settings (Abhinav et al., 2019; Chan et al., 2018; Hoffman et al., 2006; Mallari et al., 2019; Pourmand et al., 2018), wound care (Chan et al., 2018; Hoffman et al., 2000, 2001, 2011; Maani et al., 2011; Mallari et al., 2019), phantom limb (Fowler et al., 2019; Mallari et al., 2019; Pourmand et al., 2018), headaches (Pourmand et al., 2018), spinal injuries (Ahern et al., 2020; de Araujo et al., 2019), and cancer (Ahmad et al., 2020). Virtual environments began with simple computer-rendered graphics in labs looking at the effect on evoked pain and have since evolved into complex virtual environments providing everything from interactive games to realistic relaxation spaces providing meditation, hypnosis, mindfulness or even pain education. The accelerated advancement of virtual environments and VR technology creates a plethora of potential interventions for pain management. Studies, similar to this evaluation, assessed the utility of VR for pain but within a civilian patient population (Dascal et al., 2017; Chan et al., 2018; Spiegel et al., 2019; Chuan et al., 2020). Dascal et al. (2017) and Chan et al. (2018) completed systematic reviews of randomized controlled trials (RCT) and crossover studies assessing VR for pain management, acute and/or chronic, and the 27 combined studies included in their analyses used interactive and non-interactive virtual environments. The studies utilized either a single visual analogue, color analogue, graphic rating, numeric or functional pain rating scale as a measure of efficacy, with an average sample size of 40, with 18 out of 27 reporting significant decreases in pain. Most of these studies included younger, civilian patient populations with only 7 of 27 studies including patients at the median Veteran age or older. Understanding the utilization and efficacy of VR in an older population is still unclear.
VR has been utilized in military and Veteran populations to improve function (Fowler et al., 2019; Sheehan et al., 2020), treat procedural discomfort (Walker et al., 2014), and address post-traumatic stress disorder (Kramer et al., 2013; Norr et al., 2018) but the evidence is lacking for VR in the treatment of acute and chronic pain in the Veteran population. This is an important gap as Veterans experience pain more frequently and at greater levels of severity than non-Veterans (U.S. Department of Veterans Affairs, 2020; National Center for Complementary and Integrative Health, 2016). Our primary objective in this evaluation is to determine the effect of VR distraction on acute and chronic pain in Veterans in VHA settings. The secondary objective is to determine the impact of VR distraction on the experience of stress and anxiety in Veterans utilizing VR for the indication of acute or chronic pain. The third objective is to develop an understanding of the Veteran experience and applicability of using VR in a healthcare setting.
As part of our ongoing quality improvement and assessment efforts to enhance care, this prospective, pretest-posttest mixed methods evaluation was performed at the Western North Carolina Veterans Affairs Health Care System (WNC VA HCS) in Asheville, North Carolina from August 30, 2019 to November 23, 2020. Qualitative data was collected concurrently to provide context to quantitative measures. This evaluation received a Determination of non-research from the WNC VA HCS Institutional Review Board.
This project includes a convenience sample of Veterans receiving care who were experiencing acute or chronic pain in inpatient (medical, surgical, mental health, and intensive care), community living center (short term rehab, long-term care, and hospice), and outpatient (infusion and wound care clinics) settings. All Veterans were invited to utilize the VR system if available unless they were unable or had a contraindication. Veterans with blindness, severe hearing impairment, recent or active history of seizures or epilepsy; head, neck, facial injury and/or surgery in the prior 6 weeks; stroke and/or head trauma in the prior 6 weeks, implanted medical device(s) potentially subject to electromagnetic interference; severe frailty; active psychosis or delirium; and active nausea or dizziness were excluded.
VR hardware utilized included the tethered Samsung Odyssey Plus virtual reality head-mounted display (HMD) and the stand-alone PICO Neo 2 HMD. Both devices are six degrees of freedom HMDs, which signifies a high-quality HMD capable of translating all possible movements and allowing for a substantially immersive experience. The tethered HMD was utilized when building architectural elements at our medical center prevented wireless Bluetooth connectivity.
A VR software platform created by Wellovate, Inc. © was utilized with both HMDs. Interactive virtual environments included the program modules titled treasure hunt, snowball fun, music and art museum, Waya®brush (virtual painting), memory recall, and speed punch. Stationary or relaxation options consisted of guided relaxation or panoramic views (mountains and beach scenes).
Three registered nurses (RN) trained to utilize the VR system offered the VR intervention to Veterans experiencing acute and/or chronic pain. After Veterans verbally agreed to the VR intervention, they autonomously selected a VR environment based on a standard explanation by the RN. Freedom to independently choose from a select collection of modules fosters autonomy, respects individual preferences, and follows the successful strategies of other individualized non-pharmacologic distraction interventions, such as music, in demonstrating positive effects in clinical studies including randomized controlled trials (Gerdner, 2000; Masada et al., 2018; Ridder et al., 2013; Spiegel et al., 2019). Additionally, older adults have been found to more readily accept technological interventions when autonomy is retained; acceptance is crucial to enabling the sense of presence necessary for efficacy of VR interventions (Hoffman et al., 2006; Hawley-Hague et al., 2014). Sessions were intended to last approximately 30 min, depending on participant preference. In the acute and long-term care settings, Veterans experienced the VR intervention in a private or semi-private room, either seated in a chair or in bed. Veterans in the outpatient clinics experienced the VR intervention in a treatment chair.
The RNs utilized a standardized Electronic Health Record (EHR) VR note template to document their observations, interventions, Veteran responses to treatment, and spontaneous comments from Veterans regarding their VR experience.
All data utilized for the final assessment was extracted from the EHR.
Demographic data included gender, age, history of a surgery or procedure in the prior 6 weeks, and location at the time of VR session. Veterans were categorized into acute and subacute status based on location of care. Acute care locations include medical/surgical, intensive care, and inpatient mental health units. Subacute settings include community living center (short-term rehabilitation, long-term care, hospice) and outpatient clinics.
Pain was documented as acute if less than 6 months in duration, and chronic if greater than 6 months in duration. It was also noted whether the patient had undergone surgery in the 6 weeks leading up to the VR session. A pre and post pain intensity score was assessed and documented using the Defense and Veterans Pain Rating Scale (DVPRS) (Polomano et al., 2016; Ackerman and Stevens, 1989).
The DVPRS is a validated scale of pain intensity that includes biopsychosocial and functional impacts of pain. It measures the change in functional status with each pain rating number on a 0–10 scale and includes enhanced features such as word descriptors, color coding, and facial expressions. DVPRS categorizes pain level as: 0—no pain; 1–3—mild pain (green); 4–6—moderate pain (yellow); 7–10 (red). When utilizing this scale, Veterans are asked to look at the DVPRS, read descriptions under each number, and rate the severity of their current pain by choosing the corresponding number between 0 and 10. A decrease in pain rating on the DVPRS signifies not only a decrease in pain intensity, but also a decrease in functional limitations and emotional distress, which implies an improvement in wellbeing.
Stress/anxiety level was collected utilizing a scale developed by WNC VA HCS for use with CIH modalities. The options were verbalized to the Veteran in the following order to indicate a worsening of stress/anxiety: Calm, Concerned, Worried, Upset, Out of Control.
Length of VR session and noted difficulty with VR equipment was collected. RNs asked Veterans to describe their experience with, “How was that for you?” after each session. RNs recorded Veteran responses and their observations of the Veteran.
Data were analyzed using Oneway Anova for each pre and post question. Additionally, the Wilcoxon Ranked Sums test was utilized to determine statistical significance of the pre/post changes for each group (i.e., the acute pain group and the chronic pain group). The tables contain the statistically significant results.
Veteran comments and RN observations were analyzed using qualitative descriptive analysis, a flexible and structured method of organizing and interpreting non-numerical data (Miles et al., 2014). Comments and observations were read through in their entirety to gain an overall sense of the data, then each statement was carefully evaluated and inductively coded as an initial interpretation. Like codes were condensed and grouped into categories as data patterns emerged. Categories were then combined to generate themes and sub-themes. The VR coordinator confirmed the coding process and resultant themes.
Seventy-nine patients that completed a pre and post pain rating were included in this analysis. VR sessions ranged from 10 to 30 min (average 26.8 min).
Table 1 provides baseline demographic and clinical characteristics of the cohort. The average age was 47.5, with a range of 29–83, and the majority were male (92%). A larger sample of Veterans in the 40–59 and 60–79 age groups was expected based on the national median ages for both genders. The median age for a male Veteran is 65, and 51 for a female Veteran (U.S. Department of Veterans Affairs, 2017). Additionally, Veterans age 40 to 85 + account for 85% of the entire Veteran population nationally (U.S. Department of Veterans Affairs. Veteran Population, 2018). This cohort had pain patterns similar to the general VA population (Clancy, 2015) with 40% experiencing acute pain and 58% chronic pain. Overall, the cohort is a representative sample of a Veteran population receiving care at a Veterans Affairs medical facility (Clancy, 2015; U.S. Department of Veterans Affairs, 2017).
Veterans reported a mean pre-pain level of 5.3, indicating moderate pain. After VR, Veterans reported a mean pain rating of 4.1. This decrease in pain intensity resulted in a statistically significant (p <0 .001) 12% (1.2) decrease in pain levels, according to the Wilcoxon Signed Rank test (Table 2). Of the 79 participants experiencing pain prior to the VR session, 48 (60.75%) experienced a decrease of 1 or more points on the DVPRS pain scale.
To understand if the VR session impacted specific Veterans groups differently, the pre and post DVPRS pain scale was grouped by age (20–39, 40–59, etc), gender, level of care, acute/chronic pain designation, recent surgery designation, and pre-VR pain category.
Age did not significantly impact pre-VR pain levels (p = 0.53) (Table 3). The post-pain rating demonstrated improvement (p = 0.07), indicating variance among age groups, though the result was not statistically significant. There were statistically significant changes between pre and post VR analysis among three age groups, with the youngest (21–39) being the most dramatic, with a 26% decrease in pain. The 80–99 age group was omitted from this analysis due to small sample size (n = 2).
Gender did not play a significant role in pain level change and both groups improved their DVPRS pain rating by 12% after the demonstration.
Veterans were classified as “acute” or “sub-acute” status depending on their unit location and health status. There was a significant difference (p < 0.001) in pre-VR pain levels, with acute status being 13% higher (5.8) than sub-acute status (4.5). The VR intervention had a slightly larger impact on the acute status Veterans, who reported a 13% improvement in pain compared to 11% for sub-acute status. (Table 4).
Of the 78 Veterans classified as having either chronic or acute pain, there was no significant difference in the pre-VR pain rating or response to intervention (Table 5). One Veteran was omitted due to having status designated as acute and chronic pain.
Thirty five Veterans were classified as “Recent Surgery” (yes/no), indicating that their inpatient or community living center stay is related to a surgery within the prior 6 weeks; there was no significant difference in their pre-VR pain rating or response to intervention (Table 6).
Based on the DVPRS, Veterans were grouped into four categories based on their pre-demonstration pain levels (0: No Pain, 1–3: Mild Pain, 4–6: Moderate Pain, 7–10: Severe Pain). Veterans with “severe” pain improved their DVPRS rating by 16%, compared to a 9% improvement in Veterans who reported a “mild” pain level. Due to the wide confidence intervals, this did not meet a statistical significance of p < 0.05 (Table 7).
To understand if the type of VR hardware utilized had an impact on the participants’ pain outcomes, each group’s pre/post pain ratings were analyzed. There were no statistically significant differences in outcomes between the two HMDs used (p = 0.32).
Thirty-nine participants also completed the pre/post question for stress/anxiety; 36 classified their pre-stress/anxiety levels as concern, worry, or upset [Table 8]. After the demonstration, 33 of those 36 Veterans (92%) reported an improvement in their stress/anxiety level, with 31 of those reporting their stress/anxiety level as “calm” (2 Veterans had a decrease in anxiety from “worry” to “concern”).
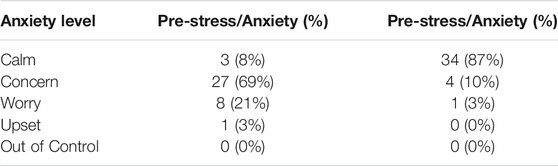
TABLE 8. VR Effect on Stress/Anxiety Level (Worsening level Calm, Concern, Worry, Upset, Out of Control).
VR-trained RNs documented short narrative descriptions for 97% of VR experiences (3% did not provide post-session statements). Five major themes emerged from the data.
Statements from 45 Veterans attributed the VR experience as a distraction from pain, even as, “a way to deal with the time until the next pill.” Common responses included, “I did not even notice my pain while doing that,” and, “it took my mind off my back pain a bit.” Distraction was mentioned not only in the context of pain relief, but also as a “good way to pass time” and as a “nice escape.” Beyond distraction, several Veterans expressed an even stronger level of immersion and presence with VR that transcended their current situation as though they were transported to a different reality, such as, “I felt like I was in the forest”, and, “it’s like a different reality–it feels more free”. One Veteran noted, “I wasn’t even thinking of my pain, I was in the zone.”
The conception of VR as a pleasurable experience emerged from the data as a distinct theme. Veterans and clinicians expressed this most often (n = 31) through enjoyment, such as, “I enjoyed that”. More impressive were the 26 responses that expressed an even greater enthusiasm for the VR experience, such as, “awesome”, “I love that, and “that made my day”. One Veteran who was new to VR stated, “That was like going to see a good movie, I didn’t want it to end!” Veterans conveyed not only enjoyment, but fun, as in (VR) “makes coming in here for something difficult fun.” Veterans also expressed a sense of accomplishment in the games such as, “I beat my score from yesterday,” and “I’m doing better at the memory game, I can tell I was faster this time.” Veterans noted that VR gave them “something to look forward to.”
Veterans conveyed a sense of relaxation (n = 14) and distraction from stress (n = 3) after VR, particularly after the beach and mountain scenes where two Veterans recounted falling asleep. Participants reported VR positively impacting both pain and anxiety, “that really helped bring my anxiety down, and my headache.” VR distraction appeared to ease anxiety, as stated, “It took my mind off my upcoming procedure,” and, “that didn’t do much for my pain, but it did help with my anxiety so it was worth it.” In addition to a reduction in anxiety, a sense of wellbeing and improved mood shone through, “I feel better, I feel really good.” There were expressions of gratitude for time spent by clinicians, with the power of human connection. One Veteran said his breathing was better while he was using VR and remained better afterward.
VR awakened Veterans to the possibility of expanding their use of non-pharmacologic therapies. First, Veterans commonly stated that they would like to have another VR session, would like to have their own VR unit at home, or suggested other Veteran populations that would also benefit from VR. Of greater importance, clinicians noted Veterans exhibited a “greater curiosity for new things” and an “expanded willingness to discuss other non-pharmacologic strategies for pain management or wholistic growth, such as meditation apps.” As one Veteran stated, “it helped me relax and make it easier to talk about things.”
Although infrequently noted, three challenges emerged surrounding the use of VR. There appears to be a learning curve for some Veterans new to VR, as they struggled to gain mastery over the games. A few participants appeared self-conscious, judging themselves for not performing better. “I need more practice”, “Gathering coins in the forest was stressful,” and, “It went pretty smooth for me this time.” Additionally, a clinician noted that VR was “frustrating at times for a Veteran with dementia.” Lastly, bothersome physical symptoms when experiencing VR were reported, namely nausea, this was specifically mentioned for only three Veterans, “this isn’t for me, it makes me a little nauseous.” Tired eyes were also reported.
Our findings demonstrate that VR distraction decreases pain levels in a Veteran population. Other studies using VR to treat pain in Veterans have shown no or small improvements in pain intensity but a large effect for patient-specific functioning (Fowler et al., 2019). Our findings are encouraging considering the difficulty Veterans experience with pain control compared to the general population (U.S. Department of Veterans Affairs, 2020), signifying VR has the potential to treat pain with equal effectiveness in Veteran populations as in civilian populations, and for multiple pain-related indications (Benham, 2019; Pourmand et al., 2018; Chan et al., 2018). The Gate Control, Multiple Resource, and Neuromatrix Theories of Pain explain the mechanism of action of VR in pain reduction. These theories purport that pain is influenced by sensory, affective, and cognitive inputs (Basil, 1994; Indovina et al., 2018; Smith et al., 2020). Since the human brain has a finite processing capacity, VR saturates the brain with engaging positive stimuli thus blocking/distracting from the pain signals resulting in pain reduction (Kahneman, 1973; Eccleston, 1999, 2001; Hoffman et al., 2007, 2011; Tack, 2019; Hoffman, 2021). We posit that the success of VR in our setting was likely the result of several factors.
Choice and control are important components in health care. Choices are limited in long-term and acute care environments, therefore we designed a program that fostered autonomy by allowing participants to independently choose a VR environment congruent with their preferences, physical ability, mental status, as well as cultural background, following the successful strategies of other non-pharmacologic pain programs (Hawley-Hague et al., 2014; Roberts et al., 2018; Won et al., 2017). Furthermore, in a systematic review, Hawley-Hague et al. (2014) discovered older adults were more receptive to technology if it was relevant to them, if they were given control, if they had autonomy related to the technology and components, and if already adopted by their peers. In addition, person-centered care approaches to non-pharmacologic interventions such as individualized music listening have similarly demonstrated positive outcomes in mood, behavior, and quality of life along with reductions in agitation and decreased use of psychotropic medication (Bakerjian et al., 2020; Huber et al., 2021; Maseda et al., 2018; Ridder et al., 2013). An additional factor believed to contribute to the success of our program includes the use of state of the art equipment which provides multisensory immersion/presence and therefore distraction.
Use of VR significantly reduced average pain intensity. The average pain intensity rating without VR was 5.3 (moderate pain). This dropped to 4.1 (mild pain) post-VR. A moderate pain intensity level on the DVPRS signifies that the pain either interrupts some activities or is hard to ignore, causing the Veteran to avoid usual activities. A decrease of pain intensity to the mild category of DVPRS is associated functionally with pain that is distracting but does not prevent participation in usual activities, an important distinction in the potential for improved wellbeing or quality of life (Polomano et al., 2016). The ability to transform moderate pain to mild pain can allow Veterans to feel less impaired by their disability and may help to decrease or prevent any associated psychological distress.
Although not statistically significant, results showed a valuable pattern. Even Veterans reporting severe pain reported a 21% reduction in pain after VR. Other studies have found that VR-based distraction is more effective for high levels of pain intensity and for those with higher levels of dysfunction (Hoffman et al., 2011; Lee et al., 2016; Maani et al., 2011; Spiegel et al., 2019; Ahern et al., 2020). This is clinically important as the highest levels of pain may be the most debilitating and often require the highest levels of pharmacological treatment. For the few participants who did not state a decrease in pain intensity following a VR session, many of them expressed that they did not feel pain during the session as evidenced by the documented qualitative statements. Some evidence indicates the effect of VR on pain to be significantly less post-session in comparison to intra-session (Jones et al., 2016). VR may be more effective at reducing pain while participants are still in VR, whereas the current study measured their “current pain” shortly after a VR session, i.e. no longer in the virtual environment. Most previously published studies have investigated memory for pain during a session recently completed, whereas the current study measures perception of current pain. Future studies should include an intra-VR session DVPRS rating in addition to the pretest-posttest scores to determine VR’s effect on pain during a VR session.
The cohort was placed into the following age categories: 20–39 (N = 5); 40–59 (N = 21), and 60–79 (N = 51). While there were no significant differences amongst the three age groups in their pretest pain scores, there was statistical significance found in the pretest-posttest analysis of each group. The 21–39 (n = 5) age group experienced the largest decrease in pain at 26%, followed by 60–79 (n = 51) with 13%, and 40–59 (n = 21) with 9%. The differences could signify that younger patients are more likely to be impacted by VR as a modality, but due to the small sample size, additional data is required. Numerous studies demonstrate that VR is effective amongst older adults, so the difference in age groups may be related to sample size alone (Roberts et al., 2018; Brown, 2019; Huygelier et al., 2019; Syed-Abdul et al., 2019). There were no significant gender differences regarding the effect of VR on pain, although the female sample size was considerably smaller (n = 6).
While the literature on VR use in both acute and chronic pain has grown rapidly in the past decade, our knowledge of the efficacy of VR in the treatment of chronic pain remains particularly lacking (Honzel et al., 2019; Mallari et al., 2019; Trost et al., 2021). However, in this assessment, VR did not demonstrate greater effectiveness in one group over the other (i.e., acute vs. chronic pain groups). The incidence of Veterans experiencing chronic pain is significantly higher (50–60%) than the civilian population (30%) and most experiencing acute pain are experiencing acute on chronic pain (Clancy, 2015; NCCIH, 2016). VR’s impact on chronic pain in this evaluation demonstrates its potential to improve overall pain levels amongst Veteran populations.
Both acute and chronic pain can lead to varying levels of functional disability and the experience of pain may take on different meaning to patients (Williamson & Higgart, 2005). Clinically, acute pain is more readily affected by VR as a distraction modality and VR may have more impact on chronic pain if used to alter “pain related movement patterns” and through integration with behavioral interventions such as meditation or exposure therapy (Chuan et al., 2020; Keefe et al., 2012; Trost, 2021). This assessment measured the analgesic effects of VR distraction on chronic pain during VR sessions or shortly after removing the VR HMD only. Due to this constraint, the authors agree with the recommendation by Ahmad et al. (2020) for utilization of VR as an adjunctive therapy to standard care for chronic pain due to the lack of evidence for a sustained decrease in pain. However, our findings, along with studies by Hoffman et al. (2007) and Shahrbanian et al. (2009), support clinical VR use with acute pain as an alternative or adjunct, non-pharmacological option.
Participants were classified into two levels of acuity subgroups of “acute” or “subacute” based on location and health status at the time of intervention. Though the pre-intervention pain scores were significantly higher in acute care patients, VR appeared to be equally effective in the acute and subacute populations. Additionally, no significant difference in pain intensity was found between those who had experienced a surgery in the past 6 weeks and those who had not. This may be due to Veterans often experiencing acute on chronic pain following surgeries and VR has been found to affect each group similarly in this assessment (acute vs. chronic pain designation).
Hardware and software play an important role in the effectiveness of VR related to level of immersion and presence, which may be affected by the degrees of freedom, field of view, interactivity, sound quality, frame rate, and other characteristics (Hoffman et al., 2006; Hoffman, 2021). In our assessment, we utilized two similar 6DoF HMDs, one tethered and one standalone, due to Bluetooth connectivity issues within the facility, but found no statistically significant difference between the two in regard to impact on pain or anxiety.
Anxiety and stress, whether caused by pain or the fear of pain, has been shown to have a positive correlation with pain, to worsen the experience of perceived pain, and decrease the threshold for pain (Theunissen et al., 2012). The understanding that anxiety and pain often overlap is supported in our results: 92% of the Veterans who reported anxiety pre-VR felt a decrease in their stress /anxiety following VR, including an improved mood. As with pain, the underlying mechanism of how VR reduces anxiety is thought to be VR’s effect on the neuromatrix (Indovina et al., 2018). VR directs attention to pleasant or engaging stimuli, thus interrupting the focus on symptoms of stress and anxiety (Firoozabadi et al., 2020; Ong et al., 2020; Piskorz & Czub, 2018; Smith et al., 2020). As anxiety can exacerbate pain, VR’s ability to act as an anxiolytic may contribute to its efficacy as an analgesic. Li et al. (2017) found that VR was more effective with those experiencing a higher level of anxiety, which is analogous to the studies stating an increased analgesic effect in those experiencing higher pain severity. This relationship is supported in our findings of 22 of the 33 Veterans (67%) who experienced a decrease in anxiety level also experienced a decrease in pain.
The analysis of Veteran comments and RN observations provided insight into participants’ experience of VR. Findings support VR as an effective distraction from pain and other negative stressors through compelling reports of immersion and presence during their session. Furthermore, VR was reported by Veterans as effective for reducing anxiety and improving their mood. This effect for some lasted several hours. Overall, the VR experience was also an enjoyable experience for our patients, with varying levels of enthusiasm described, and minimal or no side effects. Side effects in this cohort occurred in only three participants, described as nausea or eye tiredness. Although the direct association between enjoyment and a decrease in pain or anxiety is unclear, other studies also support “enjoyment” as a correlated finding (Ong et al., 2020; Appel et al., 2020). Veterans also expressed VR as a fun and novel intervention to combat boredom frequently encountered in health care settings. There were a few patient challenges noted with hardware, namely lack of initial mastery of wireless controllers due to physical or cognitive limitations. Part of these challenges are now being addressed with the introduction of “gaze control,” or eye and head tracking that allows the viewer to have a hands-free experience (Pai et al., 2018; Al-Ghamdi et al., 2020). Consideration of participant preferences and functional abilities in choosing the VR environment and level of difficulty may affect their experience. Unexpectedly, Veterans were found to have an increased willingness to explore other non-pharmacological interventions for pain and anxiety after participating in VR. This finding suggests that VR utilization may be beneficial in transforming patients’ viewpoints and expectations on how their pain and anxiety can and should be treated.
As a notable strength, these preliminary data suggest that VR as a distraction modality is a value to Veteran populations for aiding in pain management, both acute and chronic, as well as offering anxiolytic effects and an increase in overall “pleasant” experience. To the authors’ knowledge, no prior assessment offers support of this idea for Veteran populations specifically.
Our cohort size is similar to several studies in civilian settings, that were focused on evoked, experimental pain in healthy adults. However, by design, those studies are not generalizable to the clinical care of Veterans who in addition are a statistically older population with multiple co-morbidities (Chan et al., 2018; Chuan et al., 2020; Dascal et al., 2017; Spiegel et al., 2019). Our cohort size is larger than studies with other clinical pain-related indications for use, such as for burn pain, procedural use, chronic pain, and phantom limb pain (22 studies, mean n = 25 vs. n = 79 on our cohort) (Honzel et al., 2019; Chan et al., 2018). In addition, the VA patient population is predominantly male (90%) which is considered a limitation related to generalizing knowledge for all genders, but not a limitation for generalizing to the usual Veteran population.
Participant choice of environment was not tracked in our assessment. Future studies that assess outcomes related to choice of environment may help to guide future strategies for specific indications such as for acute and/or chronic pain with or without anxiety. However, it may also be that it is the immersive nature of the VR experience, and not the specific module, that drives effectiveness. Furthermore, one’s preference is likely related to social and cultural preference which may be uncoupled from the general pain mediating effectiveness of a specific module.
Another limitation is that the data set of this assessment included only a first session with each Veteran. It is possible the novelty of the experience can enhance the efficacy of the initial session. However, other studies have shown evidence to suggest VR distraction continues to reduce pain when utilized over several, consecutive days (Hoffman et al., 2019).
Heterogeneity of the sample regarding level and focus of care within the facility may also be considered a limitation, however it served as a strength due to insights gained regarding VR feasibility in more than one Veteran clinical area.
The rating scale used to measure anxiety in this assessment, though different from others’ approach and not yet tested for validity, was more operationally efficient and practical for clinical use in comparison to validated anxiety scales requiring lengthy assessment.
Though this assessment and others provide the groundwork for feasibility and initial outcome data regarding the value of VR analgesia for Veterans, future studies will require larger cohorts, randomization, and specific assessment in relationship to type of pain to more confidently determine the efficacy of VR for all indications for use.
Future studies of VR in clinical and home settings should evaluate the potentially varying level of immersion and presence felt by participants in different virtual environments, which may shed light on the impact of different environments on specific indications for use, age groups, or gender.
Evidence suggests integration of VR into standards of care as an early non-pharmacological option for acute pain management and as an adjunct to current treatments for chronic pain could be beneficial and feasible (Trost, 2021; Honzel et al., 2019). In addition, future studies are needed to determine whether VR has long-term analgesic effects for chronic pain that extend to daily activities when not wearing a VR HMD (Keefe et al., 2012). The authors intend to explore the use of VR for various clinical use-cases, including Veteran populations during outpatient procedures for pain management and anxiety.
Our assessment demonstrates that VR is an effective non-pharmacological adjunct or alternative modality for improving pain management and reducing anxiety in Veteran populations across various age ranges, and levels of acuity and chronicity. This assessment also found VR to be a beneficial distraction from pain, a pleasurable experience, and one that opens the door to utilization of other non-pharmacological modalities. VR as an adjunct or alternative modality has the potential to offer a clinically efficacious, noninvasive intervention for pain management and anxiety with few to no side effects.
The datasets presented in this article are not readily available because they cannot be shared without IRB and VA authorization and approval. Data may be available for researchers who meet the criteria for access to confidential data after evaluation from affiliated IRB and VA Research and Development Committees. As per VA national legal policy (VHA Directive1605.01), these national policies and standards also apply to deidentified data. VHA Directive 1605.01, states that deidentification certification needs to be met by Expert Determination. The expert determination requires independent assessment from an experienced master or PhD in biostatistics. Requests to access the datasets should be directed to Y2FpdGxpbi5yYXdsaW5zQHZhLmdvdg==.
The studies involving human participants were reviewed and approved by Western North Carolina Veterans Affairs Health Care System Institutional Review Board and approved for Non-Research Designation. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
CR, contributed to project design, implementation, data collection, writing, and review of the manuscript. ZV contributed to data analysis. CH contributed to data analysis, writing, and review of the manuscript. CC contributed to review of the manuscript. TO contributed to the structure, writing, and review of the manuscript.
This project was funded in part by the Nursing Services of the WNC VA HCS. External funding included monies awarded for the 2019 American Nurses Credentialing Center Pathway Award® sponsored by Cerner® and financial support received as an investee of the VHA Innovators Network for Fiscal Year 2020.
The contents do not represent the view of the Veterans Health Administration (VHA) or the United States Government.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations or those of the publisher, the editors, and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
The authors would like to thank Annette Racer, BSN, RN HNB-BC and Lynn Mennin, BSN, RN, HTP-A at Charles George VA Medical Center in the WNC VA HCS for their continued assistance with implementation, support of the project, and for co-writing the EHR template. Thank you also to Amanda Graves, BSN, RN–Nurse Manager; David Przestrzelski, MS, RN–Chief Nurse Executive/ADPCS; Linda Bugg, MSN, RN–Chief Nurse of Operations and Acute Care; and Natalie Parce, MSN, RN, CNS - Clinical Nurse Specialist of the WNC VA HCS for their support and guidance in the design, implementation, and sustainability of this work. This material is the result of work supported by the use of facilities at the Charles George VA Medical Center of the WNC VA HCS.
CIH, Complementary and Integrative Health; DVPRS, Defense and Veterans Pain Rating Scale; HMD, Head mounted display; VA, Veterans Affairs; VHA, Veterans Health Administration; VR, Virtual Reality; WNCVAHCS, Western North Carolina Veterans Affairs Health Care System.
Abhinav, R., Sweta, V., and Ramesh, A. (2019). Role of Virtual Reality in Pain Perception of Patients Following the Administration of Local Anesthesia. Ann. Maxillofac. Surg. 9 (1), 110. doi:10.4103/ams.ams_263_18
Ackerman, M. D., and Stevens, M. J. (1989). Acute and Chronic Pain: Pain Dimensions and Psychological Status. J. Clin. Psychol. 45 (2), 223–228. doi:10.1002/1097-4679(198903)45:2<223:aid-jclp2270450208>3.0.co;2-y
Ahern, M. M., Dean, L. V., Stoddard, C. C., Agrawal, A., Kim, K., Cook, C. E., et al. (2020). The Effectiveness of Virtual Reality in Patients with Spinal Pain: A Systematic Review and Meta‐Analysis. Pain Pract. 20, 656–675. doi:10.1111/papr.12885
Ahmad, M., Bani Mohammad, E., and Anshasi, H. A. (2020). Virtual Reality Technology for Pain and Anxiety Management Among Patients with Cancer: A Systematic Review. Pain Manag. Nurs. 21, 601–607. doi:10.1016/j.pmn.2020.04.002
Al-Ghamdi, N. A., Meyer, W. J., Atzori, B., Alhalabi, W., Seibel, C. C., Ullman, D., et al. (2020). Virtual Reality Analgesia with Interactive Eye Tracking during Brief thermal Pain Stimuli: A Randomized Controlled Trial (Crossover Design). Front. Hum. Neurosci. 13. 467. doi:10.3389/fnhum.2019.00467
Appel, L., Appel, E., Bogler, O., Wiseman, M., Cohen, L., Ein, N., et al. (2020). Older Adults with Cognitive And/or Physical Impairments Can Benefit from Immersive Virtual Reality Experiences: A Feasibility Study. Front. Med. 6. 329. doi:10.3389/fmed.2019.00329
Bakerjian, D., Bettega, K., Cachu, A. M., Azzis, L., and Taylor, S. (2020). The Impact of Music and Memory on Resident Level Outcomes in california Nursing Homes. J. Am. Med. Directors Assoc. 21 (8), 1045–1050e2. doi:10.1016/j.jamda.2020.01.103
Basil, M. D. (1994). Multiple Resource Theory I. Commun. Res. 21 (2), 177–207. doi:10.1177/009365094021002003
Becker, W. C., Dorflinger, L., Edmond, S. N., Islam, L., Heapy, A. A., and Fraenkel, L. (2017). Barriers and Facilitators to Use of Non-pharmacological Treatments in Chronic Pain. BMC Fam. Pract. 18 (1). 41. doi:10.1186/s12875-017-0608-2
Bellini, M., and Barbieri, M. (2013). Systemic Effects of Epidural Steroid Injections. Anaesthesiol Intensive Ther. 45 (2), 93–98. doi:10.5603/ait.2013.0021
Benham, S., Kang, M., and Grampurohit, N. (2019). Immersive Virtual Reality for the Management of Pain in Community-Dwelling Older Adults. OTJR: Occup. Participation Health 39 (2), 90–96. doi:10.1177/1539449218817291
Benyamin, R., Trescot, A. M., Datta, S., Buenaventura, R., Adlaka, R., Sehgal, N., et al. (2008). Opioid Complications and Side Effects. Pain Physician 11 (2 Suppl. l), S105–S120. doi:10.36076/ppj.2008/11/s105
Brown, J. A. (2019). An Exploration of Virtual Reality Use and Application Among Older Adult Populations. Gerontol. Geriatr. Med. 5, 233372141988528. doi:10.1177/2333721419885287
Chan, E., Foster, S., Sambell, R., and Leong, P. (2018). Clinical Efficacy of Virtual Reality for Acute Procedural Pain Management: A Systematic Review and Meta-Analysis. PLOS ONE 13 (7), e0200987. doi:10.1371/journal.pone.0200987
Chuan, A., Zhou, J. J., Hou, R. M., Stevens, C. J., and Bogdanovych, A. (2020). Virtual Reality for Acute and Chronic Pain Management in Adult Patients: A Narrative Review. Anaesthesia 76, 695–704. doi:10.1111/anae.15202
Clancy, C. (2015). Department of Veterans Affairs (VA) before the Committee on Veteran’s Affairs United States Senate. Available at: https://www.veterans.senate.gov/imo/media/doc/VA%20Clancy%20Testimony%203.26.20151.pdf.
Dascal, J., Reid, M., Ishak, W. W., Spiegel, B., Recacho, J., Rosen, B., et al. (2017). Virtual Reality and Medical Inpatients: A Systematic Review of Randomized, Controlled Trials. Innov. Clin. Neurosci. 14 (1-2), 14–21.
Eccleston, C., and Crombez, G. (1999). Pain Demands Attention: A Cognitive-Affective Model of the Interruptive Function of Pain. Psychol. Bull. 125 (3), 356–366. doi:10.1037/0033-2909.125.3.356
Eccleston, C. (2001). Role of Psychology in Pain Management. Br. J. Anaesth. 87 (1), 144–152. doi:10.1093/bja/87.1.144
Firoozabadi, R., Elhaddad, M., Drever, S., Soltani, M., Githens, M., Kleweno, C. P., et al. (2020). Case Report: Virtual Reality Analgesia in an Opioid Sparing Orthopedic Outpatient Clinic Setting: A Case Study. Front. Virtual Real. 1. 553492. doi:10.3389/frvir.2020.553492
Fowler, C. A., Ballistrea, L. M., Mazzone, K. E., Martin, A. M., Kaplan, H., Kip, K. E., et al. (2019). Virtual Reality as a Therapy Adjunct for Fear of Movement in Veterans with Chronic Pain: Single-Arm Feasibility Study. JMIR Form Res. 3 (4), e11266. doi:10.2196/11266
Gerdner, L. A. (2000). Effects of Individualized versus Classical "Relaxation" Music on the Frequency of Agitation in Elderly Persons with Alzheimer's Disease and Related Disorders. Int. Psychogeriatr. 12 (1), 49–65. doi:10.1017/S1041610200006190
Goldberg, D. S., and McGee, S. J. (2011). Pain as a Global Public Health Priority. BMC Public Health 11 (1). 770. doi:10.1186/1471-2458-11-770
Gureje, O., Von Korff, M., Simon, G. E., and Gater, R. (1999). Persistent Pain and Well Being: A World Health Organization Study in Primary Care. Surv. Anesthesiology 43 (3), 174–175. doi:10.1097/00132586-199906000-00054
Hawley-Hague, H., Boulton, E., Hall, A., Pfeiffer, K., and Todd, C. (2014). Older Adults' Perceptions of Technologies Aimed at Falls Prevention, Detection or Monitoring: A Systematic Review. Int. J. Med. Inform. 83 (6), 416–426. doi:10.1016/j.ijmedinf.2014.03.002
Hoffman, H. G., Chambers, G. T., Meyer, W. J., Arceneaux, L. L., Russell, W. J., Seibel, E. J., et al. (2011). Virtual Reality as an Adjunctive Non-pharmacologic Analgesic for Acute Burn Pain during Medical Procedures. Ann. Behav. Med. 41 (2), 183–191. doi:10.1007/s12160-010-9248-7
Hoffman, H. G., Doctor, J. N., Patterson, D. R., Carrougher, G. J., and Furness, T. A. (2000). Virtual Reality as an Adjunctive Pain Control during Burn Wound Care in Adolescent Patients. Pain 85 (1), 305–309. doi:10.1016/s0304-3959(99)00275-4
Hoffman, H. G. (2021). Interacting with Virtual Objects via Embodied Avatar Hands Reduces Pain Intensity and Diverts Attention. Sci. Rep. 11 (1). 10672. doi:10.1038/s41598-021-89526-4
Hoffman, H. G., Patterson, D. R., Carrougher, G. J., and Sharar, S. R. (2001). Effectiveness of Virtual Reality-Based Pain Control with Multiple Treatments. The Clin. J. Pain 17 (3), 229–235. doi:10.1097/00002508-200109000-00007
Hoffman, H. G., Richards, T. L., Van Oostrom, T., Coda, B. A., Jensen, M. P., Blough, D. K., et al. (2007). The Analgesic Effects of Opioids and Immersive Virtual Reality Distraction: Evidence from Subjective and Functional Brain Imaging Assessments. Anesth. Analgesia 105 (6), 1776–1783. doi:10.1213/01.ane.0000270205.45146.db
Hoffman, H. G., Rodriguez, R. A., Gonzalez, M., Bernardy, M., Peña, R., Beck, W., et al. (2019). Immersive Virtual Reality as an Adjunctive Non-opioid Analgesic for Pre-dominantly Latin American Children with Large Severe Burn Wounds during Burn Wound Cleaning in the Intensive Care Unit: A Pilot Study. Front. Hum. Neurosci. 13. 262. doi:10.3389/fnhum.2019.00262
Hoffman, H. G., Seibel, E. J., Richards, T. L., Furness, T. A., Patterson, D. R., and Sharar, S. R. (2006). Virtual Reality Helmet Display Quality Influences the Magnitude of Virtual Reality Analgesia. The J. Pain 7 (11), 843–850. doi:10.1016/j.jpain.2006.04.006
Hoffman, H. (1998). Virtual Reality: A New Tool for Interdisciplinary Psychology Research. CyberPsychology Behav. 1 (2), 195–200. doi:10.1089/cpb.1998.1.195
Honzel, E., Murthi, S., Brawn-Cinani, B., Colloca, G., Kier, C., Varshney, A., et al. (2019). Virtual Reality, Music, and Pain: Developing the Premise for an Interdisciplinary Approach to Pain Management. PAIN 160 (9), 1909–1919. doi:10.1097/j.pain.0000000000001539
Huber, A., Oppikofer, S., Meister, L., Langensteiner, F., Meier, N., and Seifert, A. (2021). Music & Memory: The Impact of Individualized Music Listening on Depression, Agitation, and Positive Emotions in Persons with Dementia. Activities, Adaptation & Aging 45 (2), 70–84. doi:10.1080/01924788.2020.1722348
Huygelier, H., Schraepen, B., van Ee, R., Vanden Abeele, V., and Gillebert, C. R. (2019). Acceptance of Immersive Head-Mounted Virtual Reality in Older Adults. Sci. Rep. 9 (1). 100141. doi:10.1038/s41598-019-41200-6
Indovina, P., Barone, D., Gallo, L., Chirico, A., De Pietro, G., and Giordano, A. (2018). Virtual Reality as a Distraction Intervention to Relieve Pain and Distress during Medical Procedures. Clin. J. Pain 34 (9), 858–877. doi:10.1097/AJP.0000000000000599
Jones, T., Moore, T., and Choo, J. (2016). The Impact of Virtual Reality on Chronic Pain. PLOS ONE 11 (12), e0167523. doi:10.1371/journal.pone.0167523
Jung, J. H., Ignatius, M. I., Davis, J. M., and Jim, L. (2014). Long-Term Complications of Epidural Steroid Injections. Curr. Phys. Med. Rehabil. Rep. 2 (1), 55–60. doi:10.1007/s40141-013-0038-6
Keefe, F. J., Huling, D. A., Coggins, M. J., Keefe, D. F., Rosenthal, Z. M., Herr, N. R., et al. (2012). Virtual Reality for Persistent Pain: A New Direction for Behavioral Pain Management. Pain 153 (11), 2163–2166. doi:10.1016/j.pain.2012.05.030
Kramer, T. L., Savary, P. E., Pyne, J. M., Kimbrell, T. A., and Jegley, S. M. (2013). Veteran Perceptions of Virtual Reality to Assess and Treat Posttraumatic Stress Disorder. Cyberpsychology, Behav. Soc. Networking 16 (4), 293–301. doi:10.1089/cyber.2013.1504
Lee, M., Suh, D., Son, J., Kim, J., Eun, S.-D., and Yoon, B. (2016). Patient Perspectives on Virtual Reality-Based Rehabilitation after Knee Surgery: Importance of Level of Difficulty. J. Rehabil. Res. Dev. 53 (2), 239–252. doi:10.1682/jrrd.2014.07.0164
Li, L., Yu, F., Shi, D., Shi, J., Tian, Z., Yang, J., et al. (2017). Application of Virtual Reality Technology in Clinical Medicine. Am. J. Transl Res. 9 (9), 3867–3880. doi:10.4247/am.2017.abh187
Liberman, J. S., Samuels, L. R., Goggins, K., Kripalani, S., Roumie, C. L., Bachmann, J., et al. (2019). Opioid Prescriptions at Hospital Discharge Are Associated with More Postdischarge Healthcare Utilization. Jaha 8 (3). e010664. doi:10.1161/jaha.118.010664
Maani, C. V., Hoffman, H. G., Morrow, M., Maiers, A., Gaylord, K., McGhee, L. L., et al. (2011). Virtual Reality Pain Control during Burn Wound Debridement of Combat-Related Burn Injuries Using Robot-like Arm Mounted VR Goggles. J. Trauma Inj. Infect. Crit. Care 71 (Suppl. ment), S125–S130. doi:10.1097/ta.0b013e31822192e2
Mallari, B., Spaeth, E. K., Goh, H., and Boyd, B. S. (2019). Virtual Reality as an Analgesic for Acute and Chronic Pain in Adults: A Systematic Review and Meta-Analysis. Jpr 12, 2053–2085. doi:10.2147/jpr.s200498
Maseda, A., Cibeira, N., Lorenzo-López, L., González-Abraldes, I., Buján, A., de Labra, C., et al. (2018). Multisensory Stimulation and Individualized Music Sessions on Older Adults with Severe Dementia: Effects on Mood, Behavior, and Biomedical Parameters. Jad 63 (4), 1415–1425. doi:10.3233/jad-180109
Miles, M. B., Huberman, A. M., and Saldaña, J. (2014). Qualitative Data Analysis : A Methods Sourcebook. Thousand Oaks: Sage.
Nahin, R. L. (2015). Estimates of Pain Prevalence and Severity in Adults: United States, 2012. J. Pain 16 (8), 769–780. doi:10.1016/j.jpain.2015.05.002
National Center for Complementary and Integrative Health (2016). Pain: U.S. Military and Veterans. Bethesda: NCCIH; National Institutes of Health. Available at: https://www.nccih.nih.gov/health/pain/veterans.
Norr, A. M., Smolenski, D. J., Katz, A. C., Rizzo, A. A., Rothbaum, B. O., Difede, J., et al. (2018). Virtual Reality Exposure versus Prolonged Exposure for PTSD: Which Treatment for Whom. Depress. Anxiety 35 (6), 523–529. doi:10.1002/da.22751
Ong, T. L., Ruppert, M. M., Akbar, M., Rashidi, P., Ozrazgat-Baslanti, T., Bihorac, A., et al. (2020). Improving the Intensive Care Patient Experience with Virtual Reality-A Feasibility Study. Crit. Care Explorations 2 (6), e0122. doi:10.1097/cce.0000000000000122
Pai, Y. S., Dingler, T., and Kunze, K. (2018). Assessing Hands-free Interactions for VR Using Eye Gaze and Electromyography. Virtual Reality 23 (2), 119–131. doi:10.1007/s10055-018-0371-2
Piskorz, J., and Czub, M. (2018). Effectiveness of a Virtual Reality Intervention to Minimize Pediatric Stress and Pain Intensity during Venipuncture. J. Spec. Pediatr. Nurs. 23 (1), e12201. doi:10.1111/jspn.12201
Polomano, R. C., Galloway, K. T., Kent, M. L., Brandon-Edwards, H., Kwon, K. N., Morales, C., et al. (2016). Psychometric Testing of the Defense and Veterans Pain Rating Scale (DVPRS): A New Pain Scale for Military Population. Pain Med. 17 (8), 1505–1519. doi:10.1093/pm/pnw105
Pourmand, A., Davis, S., Marchak, A., Whiteside, T., and Sikka, N. (2018). Virtual Reality as a Clinical Tool for Pain Management. Curr. Pain Headache Rep. 22 (8). 53. doi:10.1007/s11916-018-0708-2
Ridder, H. M. O., Stige, B., Qvale, L. G., and Gold, C. (2013). Individual Music Therapy for Agitation in Dementia: An Exploratory Randomized Controlled Trial. Aging Ment. Health 17 (6), 667–678. doi:10.1080/13607863.2013.790926
Roberts, A. R., De Schutter, B., Franks, K., and Radina, M. E. (2018). Older Adults' Experiences with Audiovisual Virtual Reality: Perceived Usefulness and Other Factors Influencing Technology Acceptance. Clin. Gerontologist 42 (1), 27–33. doi:10.1080/07317115.2018.1442380
Shahrbanian, S., Ma, X., Korner-Bitensky, N., and Simmonds, M. J. (2009). Scientific Evidence for the Effectiveness of Virtual Reality for Pain Reduction in Adults with Acute or Chronic Pain. Stud. Health Technol. Inform. 144, 40–43. doi:10.3233/978-1-60750-017-9-40
Sheehan, R. C., Fain, A. C., Wilson, J. B., Wilken, J. M., and Rábago, C. A. (2020). Inclusion of a Military-specific, Virtual Reality-Based Rehabilitation Intervention Improved Measured Function, but Not Perceived Function, in Individuals with Lower Limb Trauma. Mil. Med 186(7-8):e777-e783. doi:10.1093/milmed/usaa483
Smith, V., Warty, R. R., Sursas, J. A., Payne, O., Nair, A., Krishnan, S., et al. (2020). The Effectiveness of Virtual Reality in Managing Acute Pain and Anxiety for Medical Inpatients: Systematic Review. J. Med. Internet Res. 22 (11), e17980. doi:10.2196/17980
Spiegel, B., Fuller, G., Lopez, M., Dupuy, T., Noah, B., Howard, A., et al. (2019). Virtual Reality for Management of Pain in Hospitalized Patients: A Randomized Comparative Effectiveness Trial. PLOS ONE 14 (8), e0219115. doi:10.1371/journal.pone.0219115
Sündermann, O., Rydberg, K., Linder, L., and Linton, S. J. (2018). "When I Feel the Worst Pain, I Look like Shit" - Body Image Concerns in Persistent Pain. Scand. J. Pain 18 (3), 379–388. doi:10.1515/sjpain-2017-0163
Syed-Abdul, S., Malwade, S., Nursetyo, A. A., Sood, M., Bhatia, M., Barsasella, D., et al. (2019). Virtual Reality Among the Elderly: A Usefulness and Acceptance Study from Taiwan. BMC Geriatr. 19 (1). 223. doi:10.1186/s12877-019-1218-8
Tack, C. (2019). Virtual Reality and Chronic Low Back Pain. Disabil. Rehabil. Assistive Tech. 16, 637–645. doi:10.1080/17483107.2019.1688399
Teater, D. (2014). The Psychological and Physical Side Effects of Pain Medications. Itasca: National Safety Council. Available at: https://hcpf.colorado.gov/sites/hcpf/files/Psycholigical%20and%20Physical%20Side%20Effects%20Teater%20NSC.pdf.
Theunissen, M., Peters, M. L., Bruce, J., Gramke, H.-F., and Marcus, M. A. (2012). Preoperative Anxiety and Catastrophizing. Clin. J. Pain 28 (9), 819–841. doi:10.1097/ajp.0b013e31824549d6
Trost, Z., France, C., Anam, M., and Shum, C. (2021). Virtual Reality Approaches to Pain: Toward a State of the Science. Pain 162 (2), 325–331. doi:10.1097/j.pain.0000000000002060
U.S. Department of Veterans Affairs (2017). Profile of Veterans: 2017 Highlights. Washington, D.C: U.S. Department of Veterans Affairs. Available at: https://www.va.gov/vetdata/docs/QuickFacts/2017_Veterans_Profile_Fact_Sheet.PDF.
U.S. Department of Veterans Affairs (2020). VA Research on Pain Management. Washington, D.C: U.S. Department of Veterans Affairs. Available at: https://www.research.va.gov/pubs/docs/va_factsheets/Pain.pdf.
U.S. Department of Veterans Affairs (2018). Veteran Population. Washington, D.C: VA.gov; National Center for Veterans Analysis and Statistics. Available at: https://www.va.gov/vetdata/veteran_population.asp.
Walker, M. R., Kallingal, G. J. S., Musser, J. E., Folen, R., Stetz, M. C., and Clark, J. Y. (2014). Treatment Efficacy of Virtual Reality Distraction in the Reduction of Pain and Anxiety during Cystoscopy. Mil. Med. 179 (8), 891–896. doi:10.7205/MILMED-D-13-00343
Webster, L. R. (2017). Risk Factors for Opioid-Use Disorder and Overdose. Anesth. Analgesia 125 (5), 1741–1748. doi:10.1213/ane.0000000000002496
Williamson, A., and Hoggart, B. (2005). Pain: A Review of Three Commonly Used Pain Rating Scales. J. Clin. Nurs. 14 (7), 798–804. doi:10.1111/j.1365-2702.2005.01121.x
Keywords: virtual reality, pain, anxiety, veteran, distraction, acute pain, chronic pain, immersive
Citation: Rawlins CR, Veigulis Z, Hebert C, Curtin C and Osborne TF (2021) Effect of Immersive Virtual Reality on Pain and Anxiety at a Veterans Affairs Health Care Facility. Front. Virtual Real. 2:719681. doi: 10.3389/frvir.2021.719681
Received: 02 June 2021; Accepted: 21 September 2021;
Published: 05 October 2021.
Edited by:
Rudolph. P Darken, Naval Postgraduate School, United StatesReviewed by:
Abdulaziz. M Alshaer, Umm al-Qura University, Saudi ArabiaCopyright © 2021 Rawlins, Veigulis, Hebert, Curtin and Osborne. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Caitlin R. Rawlins, Q2FpdGxpbi5SYXdsaW5zQHZhLmdvdg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.