- INTEGRIS Health, Oklahoma City, OK, United States
The study explored the potential benefits of virtual reality as a psychological intervention to induce positive emotions and reduce pain levels in participants receiving IV chemotherapy treatment. Participants in the study had the opportunity to select a nature theme of their choosing during their treatment session. The study provided a noninvasive solution that promoted relaxation to reduce anxiety by shifting an individual’s mood positively during treatment. The objective was met by measuring participants' mood and pain levels before and after the virtual reality experience and participant satisfaction with the use of the technology. The study was conducted in the chemotherapy treatment area at the INTEGRIS Cancer Institute and consisted of a mixed demographic of cancer diagnosed patients. Results of this study showed that participants felt more calm, relaxed, and content, as well as less tense after the use of VR. Participants showed high ratings of feeling immersed and distracted by feeling like they were visiting the places displayed and paid more attention to the said environment than their own thoughts. There was no significant difference in blood pressure, pain levels, feeling upset, or worried. A majority of participants preferred to have VR as part of their future experiences during treatment time.
Introduction
The purpose of this study is to investigate the impact of nature scenes in a 3D virtual reality environment on patients receiving chemotherapy treatment. Virtual reality environments use a multi-sensory distraction technique that can help divert a person’s attention away from painful or negative stimuli (Hoffman et al., 2003; Gershon et al., 2004; Gold et al., 2007; Jones et al., 2016; Maples-Keller et al., 2017). Focusing one’s attention on pleasant, natural environments has shown to promote relaxation and enhance positive emotions, which can be influential in managing stress and decreasing feelings of anxiety (Carrougher et al., 2009; Chen et al., 2009; Banos et al., 2013; Shah et al., 2015; Flavian et al., 2019). Virtual reality has the potential to be more effective than other traditional methods due to its utilization of exposure-based therapy and immersion techniques (Powers and Emmelkamp, 2007; Opris et al., 2012; McCann et al., 2014; Fodor et al., 2018). The existing literature on virtual reality indicates that we know nature scenes can reduce anxiety for individuals. We also know that virtual reality serves as a distraction for patients to reduce pain levels, but we don’t know how virtual nature scenes impact chemotherapy patients while receiving treatment. The research study will test three hypotheses that expand on the use of virtual reality technology. Hypothesis 1: There is a statistically significant reduction in pain and blood pressure levels for patients who use a virtual reality intervention undergoing IV chemotherapy treatment than those levels before the VR session. Hypothesis 2: The use of virtual reality intervention provides an immersive atmosphere for cancer patients undergoing IV chemotherapy treatment. Hypothesis 3: Patients diagnosed with cancer undergoing IV chemotherapy treatment feel calmer and less anxious after using virtual reality than before the VR session.
Background
Attention Restoration Theory
The Attention Restoration Theory categorizes attention into two types: directed and involuntary. Directed attention involves “hard fascination,” a higher-order, top-down mental processing that fully captures one’s attention (Berman et al., 2008; Valtchanov and Ellard, 2015; Ohly et al., 2016; Basu et al., 2019). In contrast, involuntary attention utilizes “soft fascination” via bottom-up processing and is less cognitively demanding (Berman et al., 2008; Gamble et al., 2013; Berto, 2014; Valtchanov and Ellard, 2015; Gerber et al., 2017; Basu et al., 2019). Attention is susceptible to fatigue, which can lead to adverse cognitive effects that, in turn, impact one’s physical and emotional well-being (Ohly et al., 2016; Gerber et al., 2017). One way to combat attention fatigue is through attention restoration, which involves activating involuntary attention while allowing directed attention to recover (Berman et al., 2008; Ohly et al., 2016). Research has shown that natural environments are an effective method to achieve attention restoration (Berman et al., 2008; Berto, 2014; Gamble et al., 2014; Ohly et al., 2016; Gerber et al., 2017; Navarro-Haro et al., 2017).
Anxiety and Chemotherapy
While receiving chemotherapy, patients are exposed to various objects, medications, and environments that can elicit negative emotions and symptoms, such as anxiety, nausea, vomiting, pain, and fatigue. Techniques to help patients cope with these stressors can improve their experience during chemotherapy sessions and increase the likelihood of adherence to their treatment regimens (Schneider and Hood, 2007). Several studies support that the use of virtual reality has far better outcomes than traditional evidence-based interventions (cognitive-behavioral therapy, in vivo exposure, ad imaginal exposure) for treating anxiety disorders. due to the accessibility, control of content, customization options, and cost-effectiveness (Powers and Emmelkamp, 2007; Opris et al., 2012). Powers and Emmelkamp’s (2007) study strengthen the conclusion of the effectiveness of virtual reality exposure therapy (VRET) by analyzing several case studies to explore the effectiveness of VRET compared to other forms of existing treatments and conclude that VRET has a larger effect on cognitive outcome measures than other control conditions (waitlist, in vivo, relaxation, attention control, and bibliotherapy) with Cohen’s d = 1.11 (SE = 0.15, 95% CI: 0.82–1.39). Opris et al. (2012) highlight the advantages of VRET over traditional exposure specifically related to flexibility in the environment, the ability to repeat exposure as much as needed, and content selection per patient and anxiety disorder. When making a choice on type of treatment, PTSD patients highly preferred VRET over in vivo therapy which could be due to the patient’s perceptions of in vivo therapy and feeling threatened to confront fears in real life situations, objects, or activities (Opris et al., 2012).
Virtual reality utilizes distraction techniques by creating a greater sense of presence in the virtual environment, focusing a patient’s attention away from stressors and negative stimuli associated with treatment. Previous studies have identified a relationship between higher levels of distraction and lower levels of negative moods in chemotherapy and oncology patients (Schneider and Hood, 2007; Banos et al., 2013). An extensive literature review revealed only three studies that examined the effects of virtual reality on anxiety and pain levels in patients receiving chemotherapy treatment (Schneider et al., 2004; Schneider and Hood, 2007; Banos et al., 2013). Two of the three studies found a reduction in anxiety levels, whereas only one study found a reduction in both anxiety and pain levels (Schneider and Hood, 2007; Banos et al., 2013). Therefore, additional studies are needed to examine the effects of both anxiety and pain levels in chemotherapy patients. The following study will expand upon the existing body of research on anxiety and pain levels.
Virtual Reality in Pain Management
Existing literature shows that virtual reality can serve as a distractor and reduce pain levels for patients in the ICU, the inpatient environment, the emergency department, and in the outpatient setting (Schneider et al., 2004; Jones et al., 2016; Sikka et al., 2018; Tanja-Dijkstra et al., 2018; Spiegel et al., 2019; Ong et al., 2020). Distraction is widely accepted as a nonpharmacological intervention for pain relief and can be an effective adjunctive therapy to compliment pain management protocols (Schneider et al., 2004; Jones et al., 2016; Sikka et al., 2018; Tanja-Dijkstra et al., 2018; Spiegel et al., 2019; Ong et al., 2020). Immersive experiences can distract from a noxious stimulus by using multiple sensory systems, making it difficult to focus on stimuli outside the field of attention (Schneider et al., 2004; Sikka et al., 2019; Spiegel et al., 2019). This view supports the Multiple Resources Theory, which indicates that sensory systems function independently, and Gate Theory of Attention, which helps to explain that pain perceptions are reduced given the distraction of VR and the diversion of attention from pain (Jones et al., 2016; Sikka et al., 2019). The effects of VR can improve the patient’s experience in several healthcare settings by reducing pain levels at the moment and specifically reducing unavoidable discomforts involving ICU care (Ong, 2020).
Nature Scenes and Virtual Reality
Exposure to natural environments helps restore and improve attention by activating soft fascination, which has shown to have positive effects on mood and provide relief from psychological stressors (Felnhofer et al., 2015; Herrero et al., 2015; Valchanov and Ellard, 2015; Gerber et al., 2017; Golding et al., 2018; Tanja-Dikkstra et al., 2018). Virtual reality provides the opportunity to simulate nature scenes and immerse the user in its environment, directing a patient’s attention away from treatment-induced stressors. Natural settings have a more significant restorative potential than other environments because they require greater activation of involuntary attention (Berman et al., 2008; Gamble et al., 2014). These restorative effects of nature scenes can increase relaxation and peacefulness, decrease psychological stress, and improve cognitive function and attention (Berman et al., 2008; Gamble et al., 2014; Valtchanov and Ellard, 2015; Navarro-Haro et al., 2017).
Methods
Design
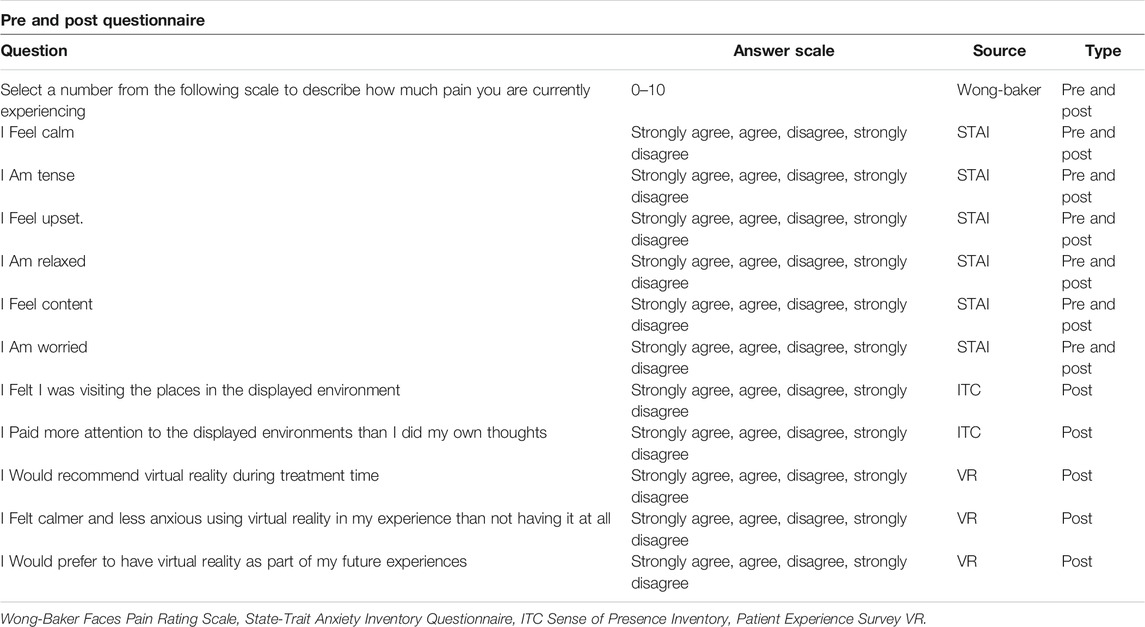
Before beginning the VR session, each participant completed a pre-assessment of their pain and mood levels using a modified version of the State-Trait Anxiety Inventory (STAI) questionnaire. Developed in 1970 by Spielberger, Gorsuch, and Lushene, the STAI is a validated assessment that consists of 40 statements that address state and trait anxiety feelings (Rubin et al., 2009). For this study, a condensed version of the STAI was used using six questions that focus on state components that gauged the intensity of feelings of anxiety in the particular moment. The feelings related to the condensed STAI were: (calm, tense, upset, relaxed, content, and worried on a scale of “strongly agree,” “agree,” “disagree,” and “strongly disagree.” The pre and post assessments include assessing level of pain using the Wong-Baker scale of 0–10 (see Table 1). The Wong-Baker face-pain scale was selected given its wide use in the healthcare industry, high usage as a study measure, and psychometric properties (McGrath, 2017). During this time, the investigator and study coordinator captured participant heart rates and blood pressure rates. After completing the pre-assessment, the VR headset was then given to the participant to place on their head and adjust as needed. The VR application used in this study, Applied VR, allows the participant to choose from 26 different nature scenarios that range from 2–30 min in duration (Figure 1). Each scenario contains relaxing music or interactive audio that is played through speakers built into the headset, providing an immersive audio-visual experience. Participants could adjust the volume to their desired level. Participants then navigated the 360-degree simulation by moving their eyes and head position. Participants were seated throughout the session and were informed they could stop at any time for any reason. Once the VR session ended, the headset was removed from the participant, and their heart rate and blood pressure were re-measured. The headsets and equipment were sanitized after each participant using the protocol provided by Applied VR. A post-assessment was then completed using the Wong-Baker faces and STAI questionnaire to evaluate pain and mood levels, as well as obtain patient satisfaction feedback regarding the overall VR experience.
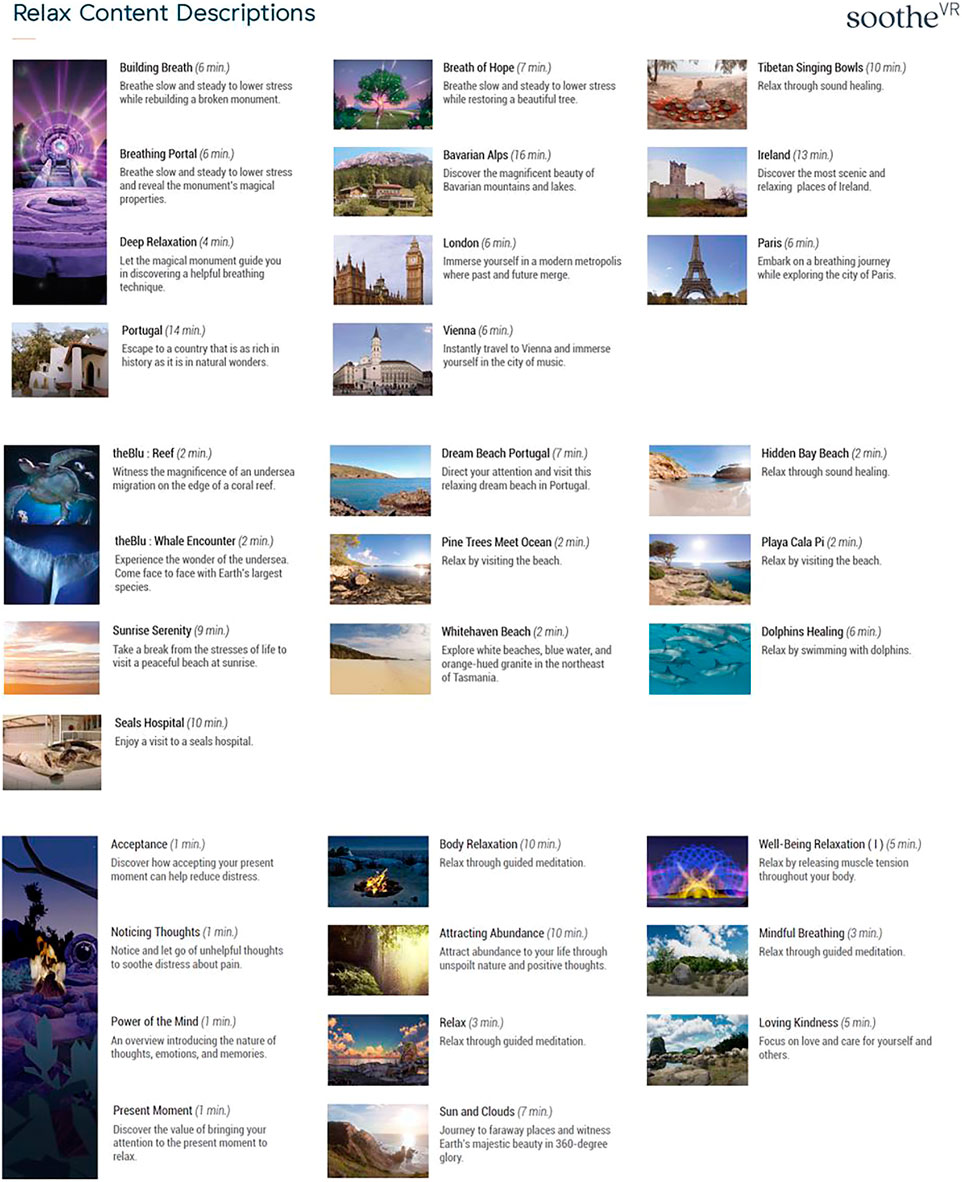
FIGURE 1. Screenshots, titles, durations, and descriptions of VR experiences available to patients in study. Complete list of content provided, with permission, from AppliedVR (2021).
Population and Sample
The theoretical population is chemotherapy patients undergoing treatment in an outpatient setting. The accessible population for this study is patients undergoing chemotherapy treatment at the INTEGRIS Cancer Institute. The population consists of male and female individuals who are actively undergoing chemotherapy treatment with a current cancer diagnosis. The minimum age range for the population is 18 years old. All races will be open to inclusion in this study, with a breakdown of all demographic information.
The sample for this study is a convenience sample of available patients at the INTEGRIS Cancer Institute who had an appointment based on the investigator’s availability to recruit patients for the study between May 7, 2019, and February 20, 2020. The sampling frame is the daily clinic schedule provided by EPIC. Patients are identified by name, date of birth, and appointment time.
Eligibility criteria for inclusion in this study are that subjects must be 18 years of age or older, male or female, and currently receiving chemotherapy treatment. Exclusion criteria would be an individual with a history of epilepsy, seizures, vertigo, or motion sickness. The virtual reality setting could possess potential side effects, specifically visually-induced motion sickness (VIMS), for individuals with a history of one of the clinical conditions (Lorenz, 2017).
Ethical Considerations
From a beneficence standpoint, the focus is not to harm while maximizing benefits to participants with little to no risk (Belmont, 2007). As mentioned in the sampling plan, specific patients with the exclusion criteria will not participate in the study. The study's benefits are not justifiable to individuals who would be more susceptible to VIMS, given the underlying preexisting health conditions (Lorenz et al., 2017). Given the exclusion of such individuals, the research study to the proposed population would not expose participants to greater than normal daily risks. Integris Health Institutional Review Board (IRB) ensures the ethical concerns in all proposed research are addressed before approving such research. An essential step in this study is to comply with all the regulations for all institutional review boards. For INTEGRIS Health IRB, an IRB application consisting of consent to participate, confidentiality agreements, and rights protection will be submitted. IRB submission also includes informed consent, conflict of interest disclosure, protocol, ethical considerations, subject and recruitment methods, and research procedures. The protection of the participant's privacy will also be considered by ensuring all identifying information will be blinded, and all documents related to assessments will be anonymous. The anonymity technique is coding the pre and post assessments by completion date and using a randomly assigned letter of the alphabet to identify the patient.
Results
Patient Characteristics
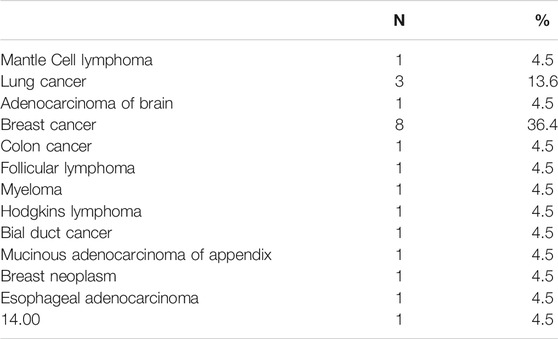
A total of 22 participants were recruited for the study. Table 2 shows the types of diagnosis for the sample with the majority of the sample having a diagnosis of breast cancer. Tables 3, 4 provide the ethnicity and gender demographics for the sample of the research study. From a gender standpoint, 59% were female, and 41% were male. The median age was 61, and the range was between 32 and 78 years of age. The demographic consisted of Caucasian (86%), African American (9%), and Asian (5%) participants.
Data Analysis
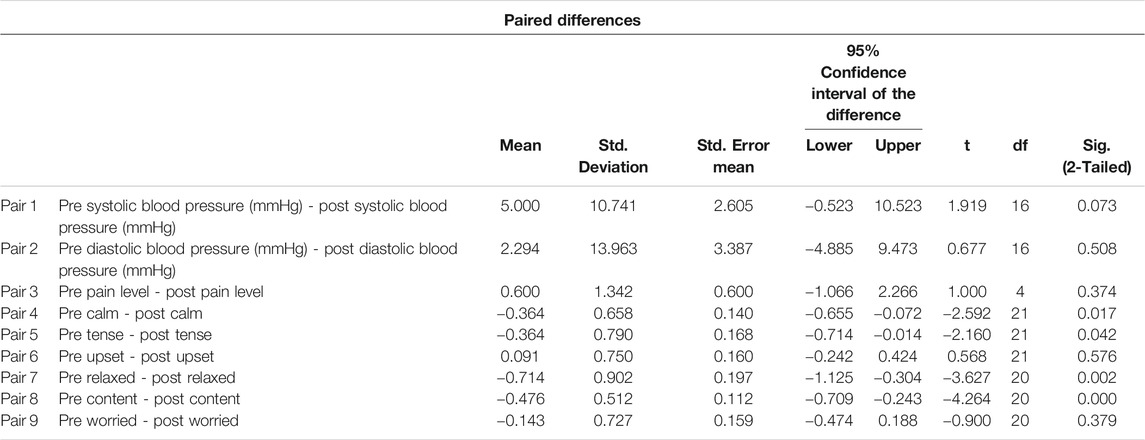
Following data collection, the data was entered into an SPSS data file for analysis. A paired T-test was used to determine the significance level, and the p-value was set at p > 0.05. According to Table 5, there was no significant difference in blood pressure (Pair 1 p = 0.073, Pair 2 = 0.508), pain levels (Pair 2 p = 0.374), feeling upset (Pair 6 p = 0.576, or worried (Pair 9 p = 0.379). The data supports the rejection of Hypothesis one since there was no significant reduction in blood pressure or pain levels. Even though there was no statistically significant difference in blood pressure for the sample, it is worth noting that out of the 22 participants, 12 participants had a decrease in systolic blood pressure levels. Additionally, six participants had a reduction in diastolic blood pressure levels. In regard to feeling calm, the T-test in Table 5, a T-test showed a p-value of 0.017, indicating that participants felt calmer after the virtual reality experience. In Table 5, a p-value of 0.042 indicates the significance of feeling less tense after the use of VR. The effect of VR was more pronounced in the feelings of being relaxed (p = 0.002) and content (p = 0.000).
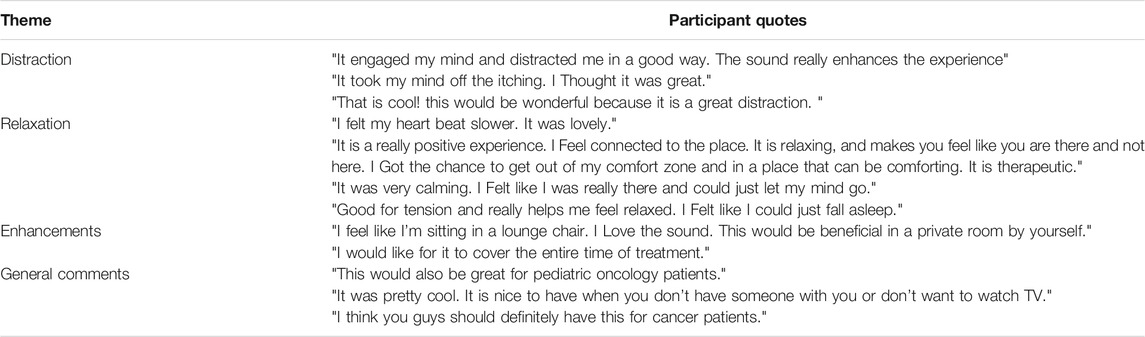
To assess the distraction quality of the intervention, participants were asked to rate their level of feeling distracted and immersed on a Likert scale with the following ratings: strongly agree (4), agree (3), disagree (2), and strongly disagree (1). The average score of feeling distracted was 3.68. According to Table 6, the average score of feeling immersed was 3.33, concluding that most patients strongly agreed to feeling like they were visiting the places displayed and paid more attention to the said environment than their own thoughts which validates Hypothesis 2. The feeling of distraction is validated through the qualitative feedback received from participants provided in Table 1. Participants reported the VR provided a distraction from their chemotherapy treatment and contributed to their positive experience, stating: “It engaged my mind and distracted me in a good way. The sound really enhances the experience”; “It took my mind off the itching. I thought it was great”; and “That is cool! This would be wonderful because it is a great distraction.”
Upon completion of the VR session, participants were asked if they felt calmer and less anxious using the virtual reality in their chemotherapy experience than not having it at all. In Table 6, an average score of 3.18 indicates that participants felt calmer and less anxious than before using VR, which validates Hypothesis 3. The qualitative feedback from participants further validates the feeling of relaxation, which is associated with lower levels of anxiousness and feeling calmer. A majority of participants found the VR to be an overall positive experience. Several participants commented on the ability of the VR to induce relaxation, stating: “I felt my heartbeat slower. It was lovely”; “It is a really positive experience. I feel connected to the place. It is relaxing and makes you feel like you are there and not here. I got the chance to get out of my comfort zone and in a place that can be comforting. It is therapeutic”; “It was very calming. I felt like I was really there and could just let my mind go”; and “Good for tension and really helps me feel relaxed. I felt like I could just fall asleep.”
Table 6 shows that a majority of participants preferred to have VR as part of their future experiences, with a mean score of 3.68. Participant feedback in Table 7 validates the continued use of VR for future treatment sessions: “I feel like I’m sitting in a lounge chair. I love the sound. This would be beneficial in a private room by yourself”; and “I would like for it to cover the entire time of treatment.” A mean score of 3.86 indicates that most participants would recommend having virtual reality as an option during chemotherapy treatment sessions. Open comments that validate recommending VR include: “This would also be great for pediatric oncology patients”; “It was pretty cool. It is nice to have when you don’t have someone with you or don’t want to watch TV”; and “I think you guys should definitely have this for cancer patients.”
Summary, Discussion, and Limitations
Results of this study show that although there was not a statistically significant decrease in blood pressure, we do know that 12 participants in the study had lower systolic blood pressure levels, and six participants had a lower diastolic blood pressure after their virtual reality session. The ability of virtual reality to reduce pain levels while receiving chemotherapy treatment remains inconclusive. The results of this research study suggest that further research using a larger sample size to measure pain levels and blood pressure is warranted to validate if virtual reality impacts the two variables.
Participants indicated a significant reduction in levels of feeling tense, as well as an increase in levels of feeling calm, relaxed, and content. These findings support Stress Reduction Theory, which states that nature scenes contribute to the restoration of attention and improvement in mood (Golding et al., 2018). Results support the ability of virtual reality nature scenes to distract participants from their thoughts and surroundings, allowing for restoration of attention and improvement in cognitive functioning, which supports Attention Restoration Theory.
Previous literature has expressed concern regarding visually-induced motion sickness (VIMS), and virtual reality equipment could contribute or lead to cybersickness (Schneider et al., 2004; Lorenz et al., 2017). None of the study participants experienced unusual symptoms such as dizziness, nausea, vomiting, headache, or visual disturbances. As with any treatment, the intervention should be used with caution and safety parameters. Virtual reality should be discontinued if adverse reactions are experienced.
There are several limitations to this study. The number of participants is a limiting factor due to the difficulties in recruitment, COVID-19, and the restrictions that led to the inability to be involved in direct patient care areas. To expand the sample size for future studies, a randomized recruiting method for any potential participant within the population should be considered. The study did not include a control group with which to compare the outcomes. A control group would help to validate if VR is an effective intervention for chemotherapy patients. Levels of pain and anxiety were not measured on a longitudinal scale, so it is difficult to determine the impact of virtual reality over extended periods or multiple chemotherapy treatments. Distraction interventions are typically available as individualized experiences that generally require a quiet environment. Some of the factors that could have caused distractions for the participant during the intervention include background noises from medical equipment such as monitors, staff coming in and out of the room, televisions, and family members engaging with participants at the bedside during treatment.
A possible confounder to this study is that the principal investigator and study coordinator conducted the VR sessions and collected the outcome data from participants. Experimenter bias could have been introduced through this process. A recommendation would be to have future sessions in which an unaffiliated person could assess the presence of this bias. Additionally, participants were aware of the study's purpose, which could have resulted in a biased effect.
Data Availability Statement
The datasets generated and/or analyzed during the current study are not publicly available to protect patient confidentiality but are available from the corresponding author on reasonable request.
Ethics Statement
The studies involving human participants were reviewed and approved by the INTEGRIS IRB. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
KW was the Primary Investigator, and GS was the study coordinator for the presented research study. KW conceived of the presented idea, submitted the application for grant funding, managed all expenses, composed the protocol, created consent forms, prepared the assessment forms, performed computations, and verified the analytical methods for the research study. GS heavily investigated background literature and existing work to help formalize the theoretical foundation and provided critical feedback in the data analysis. KW and GS contributed jointly to the following; carrying out the study, sample preparation, data collection, interpretation of results, conducting the literature review, and drafting the manuscript.
Funding
INTEGRIS Foundation Grant BG-2021-045 for publication INTEGRIS Foundation Grant BG-2020-031 INTEGRIS Foundation Grant BG-2019-051.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Baños, R. M., Espinoza, M., García-Palacios, A., Cervera, J. M., Esquerdo, G., Barrajón, E., et al. (2013). A Positive Psychological Intervention Using Virtual Reality for Patients with Advanced Cancer in a Hospital Setting: A Pilot Study to Assess Feasibility. Support Care Cancer 21 (1), 263–270. doi:10.1007/s00520-012-1520-x
Basu, A., Duvall, J., and Kaplan, R. (2019). Attention Restoration Theory: Exploring the Role of Soft Fascination and Mental Bandwidth. Environ. Behav. 51 (9-10), 1055–1081. doi:10.1177/0013916518774400
Berman, M. G., Jonides, J., and Kaplan, S. (20080956-7976). The Cognitive Benefits of Interacting with Nature. Psychol. Sci. 19 (12), 1207–1212. doi:10.1111/j.1467-9280.2008.02225.x
Berto, R. (2014). The Role of Nature in Coping with Psycho-Physiological Stress: A Literature Review on Restorativeness. Behav. Sci. 4 (4), 394–409. doi:10.3390/bs4040394
Carrougher, G. J., Hoffman, H. G., Nakamura, D., Lezotte, D., Soltani, M., Leahy, L., et al. (2009). The Effect of Virtual Reality on Pain and Range of Motion in Adults with Burn Injuries. J. Burn Care Res. 30 (5), 785–791. doi:10.1097/BCR.0b013e3181b485d3
Chen, C.-H., Jeng, M.-C., Fung, C.-P., Doong, J.-L., and Chuang, T.-Y. (2009). Psychological Benefits of Virtual Reality for Patients in Rehabilitation Therapy. J. Sport Rehabil. 18 (2), 258–268. doi:10.1123/jsr.18.2.258
Felnhofer, A., Kothgassner, O. D., Schmidt, M., Heinzle, A.-K., Beutl, L., Hlavacs, H., et al. (2015). Is Virtual Reality Emotionally Arousing? Investigating Five Emotion Inducing Virtual Park Scenarios. Int. J. Human-Computer Stud. 82, 48–56. doi:10.1016/j.ijhcs.2015.05.004
Flavián, C., Ibáñez-Sánchez, S., and Orús, C. (2019). The Impact of Virtual, Augmented and Mixed Reality Technologies on the Customer Experience. doi:10.1016/j.jbusres.2018.10.050
Fodor, L. A., Coteț, C. D., Cuijpers, P., Szamoskozi, Ş., David, D., and Cristea, I. A. (2018). The Effectiveness of Virtual Reality Based Interventions for Symptoms of Anxiety and Depression: A Meta-Analysis. Sci. Rep. 8 (1), 1–13. doi:10.1038/s41598-018-28113-6
Gamble, K. R., Howard, J. H., and Howard, D. V. (2014). Not just Scenery: Viewing Nature Pictures Improves Executive Attention in Older Adults. Exp. Aging Res. 40 (5), 513–530. doi:10.1080/0361073X.2014.956618
Gerber, S. M., Jeitziner, M.-M., Wyss, P., Chesham, A., Urwyler, P., Müri, R. M., et al. (2017). Visuo-acoustic Stimulation that Helps You to Relax: A Virtual Reality Setup for Patients in the Intensive Care Unit. Sci. Rep. 7 (1), 13228–13310. doi:10.1038/s41598-017-13153-1
Gershon, J., Zimand, E., Pickering, M., Rothbaum, B. O., and Hodges, L. (2004). A Pilot and Feasibility Study of Virtual Reality as a Distraction for Children with Cancer. J. Am. Acad. Child Adolesc. Psychiatry 43 (10), 1243–1249. doi:10.1097/01.chi.0000135621.23145.05
Gold, J. I., Belmont, K. A., and Thomas, D. A. (2007). The Neurobiology of Virtual Reality Pain Attenuation. CyberPsychology Behav. 10 (4), 536–544. doi:10.1089/cpb.2007.9993
Golding, S. E., Gatersleben, B., and Cropley, M. (2018). An Experimental Exploration of the Effects of Exposure to Images of Nature on Rumination. Int. J. Environ. Res. Public Health 15 (2), 300. doi:10.3390/ijerph15020300
Herrero, R., García-Palacios, A., Castilla, D., Molinari, G., and Botella, C. (2014). Virtual Reality for the Induction of Positive Emotions in the Treatment of Fibromyalgia: A Pilot Study over Acceptability, Satisfaction, and the Effect of Virtual Reality on Mood. Cyberpsychology, Behav. Soc. Networking 17 (6), 379–384. doi:10.1089/cyber.2014.0052
Hoffman, H. G., Garcia-Palacios, A., Kapa, V., Beecher, J., and Sharar, S. R. (2003). Immersive Virtual Reality for Reducing Experimental Ischemic Pain. Int. J. Human-Computer Interaction 15 (3), 469–486. doi:10.1207/s15327590ijhc1503_10
Jones, T., Moore, T., and Choo, J. (2016). The Impact of Virtual Reality on Chronic Pain. PLoS One 11 (12), e0167523. doi:10.1371/journal.pone.0167523
Lorenz, J., Gomes, P., Prang, J., Jamshidirad, A., and Tolg, B. (2017). Subjective and Autonomic Responses to a 3D-Virtual Reality Game. Reading: Academic Conferences International LimitedRetrieved from Available at: http://library.capella.edu/login?qurl=https%3A%2F%2Fsearch. proquest.com%2Fdocview%2F1967758474%3Faccountid%3D27965.
Maples-Keller, J. L., Bunnell, B. E., Kim, S.-J., and Rothbaum, B. O. (2017). The Use of Virtual Reality Technology in the Treatment of Anxiety and Other Psychiatric Disorders. Harv. Rev. Psychiatry 25 (3), 103–113. doi:10.1097/HRP.0000000000000138
McCann, R. A., Armstrong, C. M., Skopp, N. A., Edwards-Stewart, A., Smolenski, D. J., June, J. D., et al. (2014). Virtual Reality Exposure Therapy for the Treatment of Anxiety Disorders: An Evaluation of Research Quality. J. Anxiety Disord. 28 (6), 625–631. doi:10.1016/j.janxdis.2014.05.010
McGrath, P. J., Forgeron, P. A., and Huguet, A. (2017). Pain, Children and ☆. Reference Module in Neuroscience and Biobehavioral Psychology () Elsevier. doi:10.1016/B978-0-12-809324-5.04184-5
Navarro-Haro, M. V., López-del-Hoyo, Y., Campos, D., Linehan, M. M., Hoffman, H. G., García-Palacios, A., et al. (2017). Meditation Experts Try Virtual Reality Mindfulness: A Pilot Study Evaluation of the Feasibility and Acceptability of Virtual Reality to Facilitate Mindfulness Practice in People Attending a Mindfulness Conference. PLoS One 12 (11), e0187777. doi:10.1371/journal.pone.0187777
Ohly, H., White, M. P., Wheeler, B. W., Bethel, A., Ukoumunne, O. C., Nikolaou, V., et al. (2016). Attention Restoration Theory: A Systematic Review of the Attention Restoration Potential of Exposure to Natural Environments. J. Toxicol. Environ. Health B 19 (7), 305–343. doi:10.1080/10937404.2016.1196155
Ong, T. L., Ruppert, M. M., Akbar, M., Rashidi, P., Ozrazgat-Baslanti, T., Bihorac, A., et al. (2020). Improving the Intensive Care Patient Experience with Virtual Reality-A Feasibility Study. Crit. Care Explorations 2 (6), e0122. doi:10.1097/CCE.0000000000000122
Opris, D., Pintea, S., García-Palacios, A., Botella, C., Szamosközi, S., and David, D. (20121091-4269). Virtual Reality Exposure Therapy in Anxiety Disorders: A Quantitative Meta-Analysis. Depress. Anxiety 29 (2), 85–93. doi:10.1002/da.20910
Powers, M. B., and Emmelkamp, P. M. G. (2008). Virtual Reality Exposure Therapy for Anxiety Disorders: A Meta-Analysis. J. Anxiety Disord. 22 (3), 561–569. doi:10.1016/j.janxdis.2007.04.006
Rubin, R. B., Rubin, A. M., Graham, E., Perse, E. M., and Seibold, D. (2009). Anxiety: State-Trait Inventory. Abingdon-on-Thames, United Kingdom: Routledge, 463–469. doi:10.4324/9780203871539-76
Schneider, S. M., and Hood, L. E. (2007). Virtual Reality: A Distraction Intervention for Chemotherapy. Oncol. Nurs. Forum 34 (1), 39–46. doi:10.1188/07.onf.39-46
Schneider, S. M., Prince-Paul, M., JoAllen, M., Silverman, P., and Talaba, D. (2004). Virtual Reality as a Distraction Intervention for Women Receiving Chemotherapy. Oncol. Nurs. Forum 31 (1), 81–88. doi:10.1188/04.ONF.81-88
Shah, L. B. I., Torres, S., Kannusamy, P., Chng, C. M. L., He, H., and Klainin-Yobas, P. (2015). Efficacy of the Virtual Reality-Based Stress Management Program on Stress-Related Variables in People with Mood Disorders: The Feasibility Study. Available at: https://doi-org.library.capella.edu/10.1016/j.apnu.2014.09.003.
Sikka, N., Shu, L., Ritchie, B., Amdur, R. L., and Pourmand, A. (2019). Virtual Reality-Assisted Pain, Anxiety, and Anger Management in the Emergency Department. Telemed. e-Health 25 (12), 1207–1215. doi:10.1089/tmj.2018.0273
Spiegel, B., Fuller, G., Lopez, M., Dupuy, T., Noah, B., Howard, A., et al. (2019). Virtual Reality for Management of Pain in Hospitalized Patients: A Randomized Comparative Effectiveness Trial. PLoS One 14 (8), e0219115, doi:10.1371/journal.pone.0219115
Tanja-Dijkstra, K., Pahl, S., White, M. P., Auvray, M., Stone, R. J., Andrade, J., et al. (2018). The Soothing Sea: A Virtual Coastal Walk Can Reduce Experienced and Recollected Pain. Environ. Behav. 50 (6), 599–625. doi:10.1177/0013916517710077
Keywords: virtual reality, nature, chemotherapy, anxiety, pain, distraction, attention restoration theory, cancer
Citation: Wilson K and Scorsone G (2021) The Use of Virtual Reality Technologies to Reduce Anxiety and Improve Experience in Chemotherapy Patients During Treatment. Front. Virtual Real. 2:695449. doi: 10.3389/frvir.2021.695449
Received: 15 April 2021; Accepted: 17 June 2021;
Published: 30 June 2021.
Edited by:
David Joseph Brown, Nottingham Trent University, United KingdomReviewed by:
Laura E. Watkins, Emory University, United StatesAli Fardinpour, Wise Realities Institute for Healthcare Emerging Technologies Research, Australia
Copyright © 2021 Wilson and Scorsone. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kaylie Wilson, a3dpbHNvbjUxMjFAeWFob28uY29t
†ORCID: Kaylie Wilson, orcid.org/0000-0001-8653-6428; Grace Scorsone, orcid.org/0000-0003-2137-0572
 Kaylie Wilson
Kaylie Wilson Grace Scorsone
Grace Scorsone