- 1School of Psychology, Dublin City University, Dublin, Ireland
- 2Department of Psychology, Faculty of Science and Engineering, Maynooth University, Maynooth, Ireland
- 3Aristotle University of Thessaloniki, Thessaloniki, Greece
- 4WITA, Trento, Italy
Augmented and virtual reality (AR/VR) technologies are regularly used in psychology research to complement psychological interventions and to enable an individual to feel as if they are in an environment other than that of their immediate surroundings. A scoping review was performed to identify how AR/VR was being used with older adult populations to impact their physical and mental health. The review also sought to determine whether the terminology used in AR/VR research was consistent. The results show that 65 studies have been published in the last 20 years that meet the inclusion criteria (virtual/augmented reality) technology to impact older adults’ physical/mental health and wellbeing. Participants included healthy, physically, and cognitively impaired, and emotionally vulnerable older adults. We argue that over 70% of the studies included in this review were mislabeled as VR and only six papers included fully immersive VR/AR. The remaining studies use less immersive variants of virtual reality with their populations, and only one study made use of AR, which prompted the suggestion of a new definition for virtual reality. This paper also calls for an updated taxonomy of augmented and virtual reality definitions to address the lack of consistency found in studies that identify themselves as AR/VR when they are using less immersive technical set-ups, including displaying non-interactive videos on 2D screens.
Background
The development and impact of virtual and augmented technologies has been examined since the early 60s (Eckert et al., 2019, p. 2). In their current evolution, they provide digital interaction in space. There are many complementary definitions of both terms though the most comprehensive are from McCoy and Stone (2001) and Botella et al. (2015). Virtual reality is “a collection of technologies that allow people to interact efficiently with 3D computerized databases in real time using their natural senses and skills” (McCoy and Stone, 2001, p. 912), whereas augmented reality “combines the real world with virtual elements, using computer graphics mixed with the real world in real time” (Botella et al., 2015, p. 2). Both definitions emphasize the importance of real-time interaction while also establishing their fundamental differences. Virtual reality immerses the user in a digital environment whereas augmented reality enhances the world around the user. Virtual technologies (hereafter referred to as AR/VR), have been incorporated into many areas of psychological research including exposure therapy (Riva et al., 2019, p. 82), pain management (Wiederhold, 2016, p. 577), and even diagnostic proficiency (Tarnanas et al., 2015, p. 12).
The use of AR/VR in older adult populations is often used as a form of Positive technology. This is the application of creative technologies for the benefit of personal experience (Botella et al., 2012, p. 78) through its structuring, augmentation and/or replacement” (Kitson et al., 2018, p. 3). When used to support user engagement, it enhances the environment and supports a person in new ways that better reflect their needs (Graffigna et al., 2013, p. 1). Functions of positive technologies include, encouraging positive emotions, promoting engagement and self-empowerment, and increasing social integration and connectedness (Wiederhold and Riva, 2012, p. 67). Each area can be promoted, affected, and facilitated by AR/VR and, the more interesting or compelling the virtual environment, the greater the enjoyment which can lead directly to increase motivation (Rizzo and Kim, 2005). Given that the population of adults over 65 in the EU27 (member states of the European Union) is expected to increase by 8.9% (Eurostat, 2020) by 2050, new and innovative ways to use AR/VR has become a tenet of research to support older adults to live independently at home for as long as possible (Wiederhold, 2020, p. 141). AR/VR physical activity programs have been successful in terms of increasing physical activity and strength and by influencing the motivations that drive these positive behaviors (Ng et al., 2019, p. 280). These interventions, underpinned by social cognitive theory, can effectively act as supplementary supports to physical actions. Through the observation of “others” or “oneself” in the digital environment, the user can learn and reinforce behaviors. Further research of the effects of intrinsic and extrinsic motivations in AR/VR interventions, is needed. While there are many studies that use AR/VR to impact physical and social factors in varied populations (Tarnanas et al., 2015, p. 2; Wiederhold, 2016; Riva et al., 2019, p. 82, p. 577), there is very little standardization or consistency in the terminology used to describe the technology. This has led to a call to unify definitions by (Kardong-Edgren et al., 2019, p. 29) and this review aims to address some of the gaps highlighted by the researchers.
“Virtual” Behavior Change Theory
Over the last decade virtual reality research has made the leap from “toy” to serious research tool (Stadler et al., 2019, p. 207). Several theories (Riva et al., 2016, p. 2–3) can be used to justify the inclusion and success of virtual interventions and this is important as many interventions have been found to provide inadequate theoretical support for their behavior change interventions (Michie et al., 2014). Perceptual Control Theory (Parker et al., 2020, p. 616) argues that participants occupied with a goal state interact with a digital environment and receive perceptual updates of their progress. Until their current perceptual state matches their goal state, they will receive “error” feedback, prompting them to continue until congruence is achieved. Self-affirmation theory (Velez and Hanus, 2016, p. 721–722) also supports the effectiveness of virtual interventions. During a virtual intervention, participants are often faced with negative information relevant to themselves. Researchers will prompt participants to change these behaviors in response to the intervention, but this can threaten the positive aspects of self-identity so virtual interventions often include positive encouragement to bolster important aspects of self-identity. This positive reinforcement facilitated by the virtual environment (e.g., gaining points in a virtual game) allows participants to fully engage with, and internalize the purpose of, the intervention. The Transtheoretical Model of Behavior Change (Yu-Leung et al., 2019, p. 287) states that there are six stages of health-related behavior change that hold true in both physical and virtual settings. These shifts in attitude are a useful indicator to researchers developing virtual interventions when compared to participants’ prior experience and interest. Finally, Transformative Learning Theory (Huth et al., 2020, p. 1026), unlike self-affirmation theory, suggests that a pre-existing view evolves in response to a conflicting situation. The participant can reflect and engage with the situation in the virtual environment and experience a fundamental shift in perspective.
Rationale for Scoping Review
To date, approximately 19 meta-analyses and systematic reviews (See Supplementary Table S1) have examined the effects of VR on older populations, yet none have investigated the impact of AR in this population. Smart health technologies can benefit the cognitive, emotional, physical, and social domains of day-to-day living (Guisado-Fernández et al., 2019, p. 7–8). As such, illuminating the relationship between AR/VR, older adults and physical and mental health is essential.
Two research questions were posed in this scoping review.
1. How is AR/VR technology currently used in research with older adults to assess and/or improve physical and mental health and general wellbeing?
2. Is consistent terminology used across these studies and if not, what are the inconsistencies, and can this evaluation identify (or construct) a definition that will advance or improve understanding?
Methods
Protocol
The PRISMA Extension for Scoping Reviews (Tricco et al., 2018, p. 4) was guides this review. We selected this framework given the variety of AR/VR technologies in research use, the numerous ways the technology is described, and the need to establish what and how research is conducted to enable appropriate systematic reviews to take place. Our aim is to create a resource for researchers interested in conducting AR/VR research with older adult populations in physical and mental health settings. As AR/VR terminology is multi-varied and (often) used interchangeably, this paper will summarize how these terms are being used and offer a rationale for why they are/are not being used correctly.
Search Keywords and Databases
A comprehensive list of search terms was created to address the three areas of interest in this review: AR/VR, older adults, physical/mental health, and wellbeing. The literature search was conducted on March 24th, 2020 across the following licenced databases: Academic Search Complete, CINAHL, PsycINFO, PsycArticles and Medline. Primary studies with all types of designs were included along with all types of reviews. Table 1 illustrates the key and related search terms used. Terms were combined using the Boolean Operators.
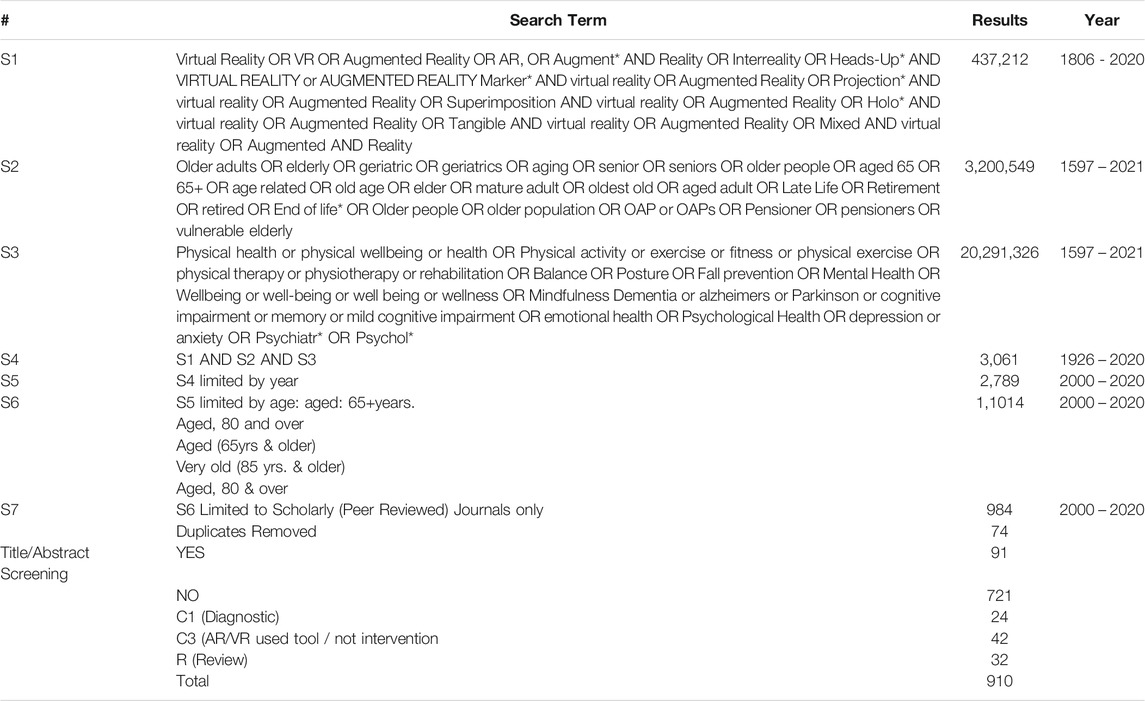
TABLE 1. Academic Search Complete + CINAHL Complete + MEDLINE + PsychArticles + PsychINFO – 24/03/2020
Inclusion and Exclusion Criteria
Articles were included if the target group were aged 60+°years, a common threshold for research in this field. If a study had participants of various ages, data relating to the older adults must have been presented separately to be included. All articles using terms such as “virtual,” “augmented” and/or “mixed” reality where included. Finally, articles were only included if they investigated physical/mental health, wellbeing and AR/VR was used as part of their intervention. Articles were excluded if they did not meet the above criteria, if they did not include an active intervention or if they were published abstracts (where no paper was submitted), book reviews, opinion articles, commentaries, letters, editorials, interviews, lectures, legal cases, newspaper articles, or patient education handouts. Articles published from January 1999 to March 2020 were considered so that the review would not only contain recent studies, but also those from the early 2000s (the emergence of modern 3D virtual and augmented reality technologies) and the 00s (when Virtools VR Pack was released, which supported development of virtual environments in immersive spaces such as CAVE’s and HMD’s such as the Oculus Rift). Finally, only articles published in English were included as accurate translation would not be possible in the review timeframe.
Data Sorting and Analysis
Two reviewers screened for title and abstract, and full text reviews. Each reviewer conducted their screening individually, conflicts were discussed, and a final decision made. If any articles were not agreed upon, they were sent to a third party for arbitration. Data from full-text review was charted using the following headings: Title, citation, hypothesis, research question, aim, study design, participant details, methodology, procedure, country, results, conclusions, hardware used, software used, classification of AR/VR and, definitions used. Following the same procedure, reviewers also classified each article as: 1) Immersive VR; 2) Non-Immersive VR; 3) 2D VR; or 4) AR. Classifications were determined separately and a consensus was achieved through discussion.
Results
The literature revealed 984 studies. From this, 74 duplicates were removed. After screening titles and abstracts of the remaining 910 articles, 91 articles were brought forward for full-text review. After review, 52 studies were included in this study (See Figure 1). A further 13 articles were incorporated into this study based on a review of the references included in three systematic reviews identified in our search. The final number of articles included in this review was 65. The most common reasons for exclusion were participants under the age of 60 and studies that did not include an active intervention. Two reviewers screened results at all stages of screening and disagreements were found in approximately 7.5% of cases on average.
Characteristics of the Participants
For a detailed overview of the virtual and augmented reality characteristics included in the 65 studies, please see Table 2. Across the 65 studies identified, there was an average of 65 participants (Range 7–664) with a mean age of 67.63 (SD 8.45). Each study investigated older populations except three that compared older and younger adults. Four studies provided a participant age range (60–90+) and just one study specified a population over 60. Most studies included male and female participants however 13 investigated only male (N = 1), female (N = 5) populations or, did not specify participant gender (N = 7). The majority of studies included healthy participants however others included participants prone to falling (N = 5), participants in hospital (N = 2) or long-term living facilities (N = 3), participants with osteopenia (N = 2), neurological issues (N = 15), PTSD (N = 1) or diabetes (N = 1), participants who had experienced a stroke (N = 1) or persistent dizziness (N = 2), veterans (N = 2), those who were recently bereaved (N = 1) and those with depression (N = 1). Finally, three studies were systematic reviews containing multiple populations.
Study Designs
Of the included studies, 24 were randomized controlled trials, four were non-randomized controlled trials one was an exploratory study, two were observational two were qualitative, and one was an open label trail. The remaining studies were quasi-experimental (see Table 2).
Research Focus (Measures)
The measures used across the 65 studies were categorized into seven main themes, with most research examining two or more (See Table 3). Themes included physical activity, general health, balance and falls, cognition, affect, wellbeing and user experience (UX). One measure looked at a person’s motivations within a natural or therapeutic environment and was categorized as other.
AR/VR Equipment
The 65 studies included a combination of custom-made and commercially available virtual technologies. Custom systems usually consisted of a specially designed virtual environment displayed on a monitor or projector and interacted with using keyboard/mouse (N = 5), joystick/controller (N = 10) or, exercise equipment such as treadmills (N = 4) or stationary bicycles (N = 3). Other customized equipment included the BARCO™ (N = 2) and IREX™ (N = 3) systems. Commercially available systems included use of Xbox Console™ and Kinect Cameras™ (N = 10), PlayStation™ and EyeToy™ Cameras (N = 2) or, Wii Console™ (N = 11) with Wii Remote™ (N = 4) and Wii Balance Board™ (N = 9). Only six studies used HMDs to immerse users in a virtual (N = 5) or augmented (N = 1) environment. Alternate set-ups included: 1) a two custom scenarios where participants “rowed” along with a first person video displayed on screen (N = 1) or where participants memories a route (N = 1), 2) a bereavement study where the participants interacted with each other through “Second Life,” a massively multiplayer online roleplaying game (MMORPG) (N = 1); 3), studies that looked at the impact of using dance platforms (N = 2); and 4) a study that looked at cybersickness and drop-out rates in a driving simulator (N = 1).
Virtual Reality Characteristics
This scoping review aimed to identify AR/VR technology used to support older adults’ physical and/or mental health. However, only one augmented reality study (Korsgaard et al., 2019) was identified. As described earlier this paper categorized the technology used in each study as either: 1) 2D VR, 2) Non-Immersive VR, 3) Immersive VR and 4) AR. Despite self-identifying as Immersive VR, 16 of 21 studies were in fact 2D VR. The remaining five studies correctly identified themselves as either a “virtual environment” (Liu, 2010; Fasilis et al., 2018; Lokka et al., 2018), a video game (Studenski et al., 2010) and a virtual avatar (Sun et al., 2019). This review categorized 35 studies as non-immersive VR but, only seven of these studies did not include the phrasing “Immersive VR” or “virtual reality” in their interventions. Five papers described themselves as “exergames” (Rosenberg et al., 2010; Franco et al., 2012; Karahan et al., 2015; Padala et al., 2017a; Padala et al., 2017b), one as a videogame (Laver et al., 2012), one as a “virtual environment” (Merriman et al., 2015) and one only described the type of console used (Padala et al., 2012). Finally, five studies can be categorized as “Immersive VR” (Gamito et al., 2010; Optale et al., 2010; Corno et al., 2014; Parijat et al., 2014; Lokka et al., 2018) and each study accurately described itself as such. Despite the large number of studies included in this review, only 16 provided a definition for virtual reality (See Table 4), one offered a definition for virtual reality exposure therapy (Barbosa et al., 2019) and one described “mixed reality” (Korsgaard et al., 2019).
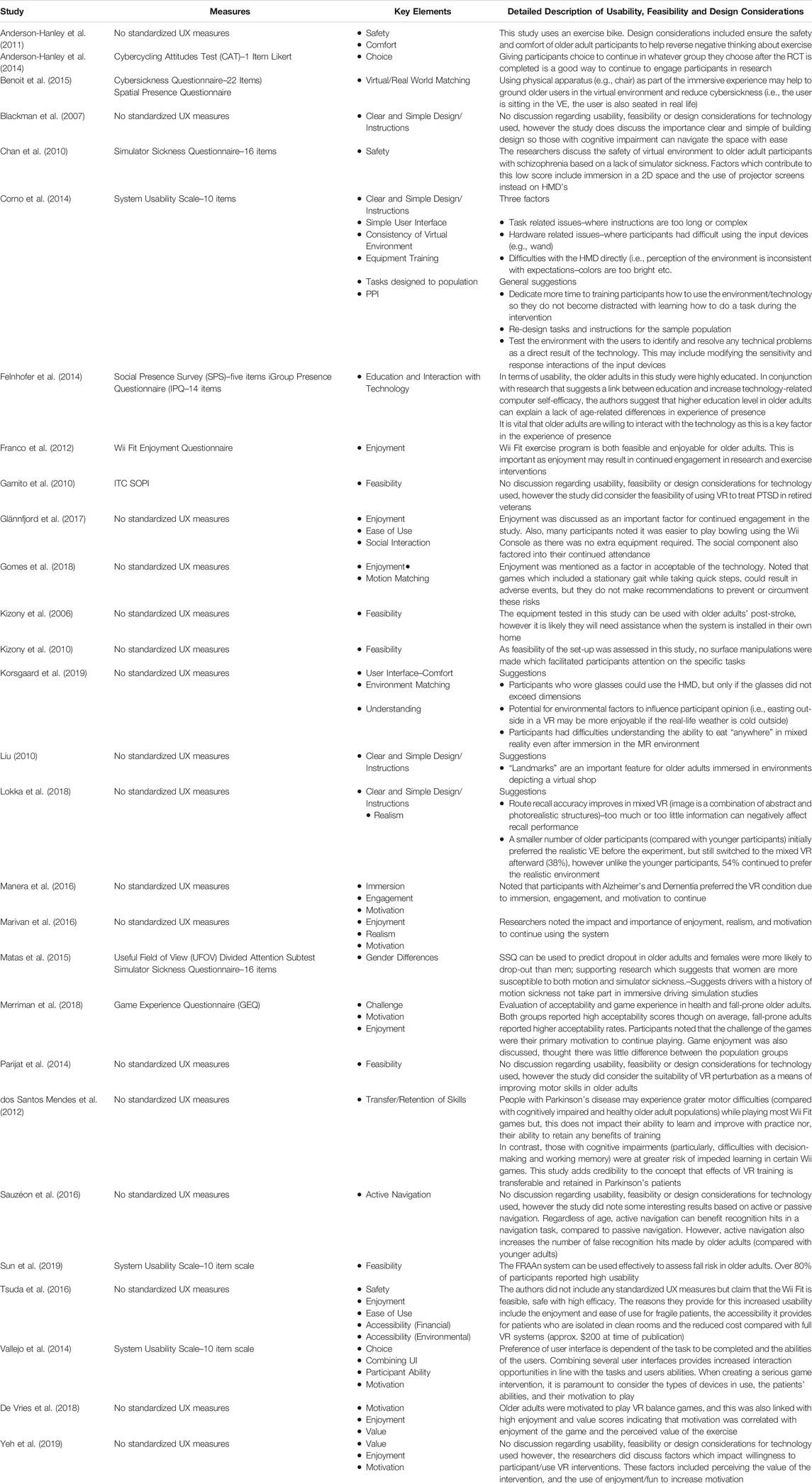
Usability and Virtual/Augmented Technologies
Over a third of the studies included in this review directly investigated the usability and feasibility of various AR/VR systems for use with older populations to support physical and mental health and wellbeing. However, only ten of these studies used standardized questionnaires (see Table 3) to evaluate participants’ sense of presence and the usability of each system. The remaining studies that included evaluations of usability or design provided their participants with bespoke questionnaires tailored to fit their purpose. Key findings from this group of studies indicated that there were no age differences (between older and younger users) in physical and social presence (Felnhofer et al., 2014), or in experience of cybersickness (Sauzéon et al., 2016). One study demonstrated a reduction in cybersickness with older adults with schizophrenia (Chan et al., 2010), another indicated that most of their PTSD patients reported no negative effects after exposure to a virtual environment displayed in an HMD. Despite this, research still maintains that older adults are a high-risk group for cybersickness (Matas et al., 2015). One study did find a gender difference in level of presence, where men were more likely to experience a greater sense of presence (Felnhofer et al., 2014).
Analysis of the 28 studies that considered UX design of AR/VR environments (See Table 5), and the technologies used has established three main categories, each with further sub-categories, to describe the factors by. These include usability, feasibility, and tailored design.
Usability
Enjoyment (N = 8) and Motivation (N = 6) are the most common themes with researchers identifying them as vital to user engagement. Additional themes included, clear and simple design/instructions (N = 4), Matching (N = 3), Value (N = 2), Ease of Use (N = 2), Comfort (N = 2) and Choice (N = 2). The remaining themes within the category of Usability each had one mention and they included, Accessibility, Challenge, Combining UI, Consistency of Virtual Environment, Engagement, Simple UI and Social Interaction.
Feasibility
Feasibility (N = 5), Safety (N = 3), Gender Differences (N = 1), Participants Ability (N = 1), Tasks Designed to Population (N = 1) and Understanding (N = 1) were sub-categories identified across the research studies.
Tailored Design
Finally, there were seven suggestion/outcome sub-categories identified. These included, Realism (N = 2), Active Navigation (N = 1), Education and Interaction with Technology (N = 1), Equipment Training (N = 1), Immersion (N = 1), Public and Patient Involvement (PPI) (N = 1), and Transfer/Retention of Skills (N = 1).
Intervention-Based Theories
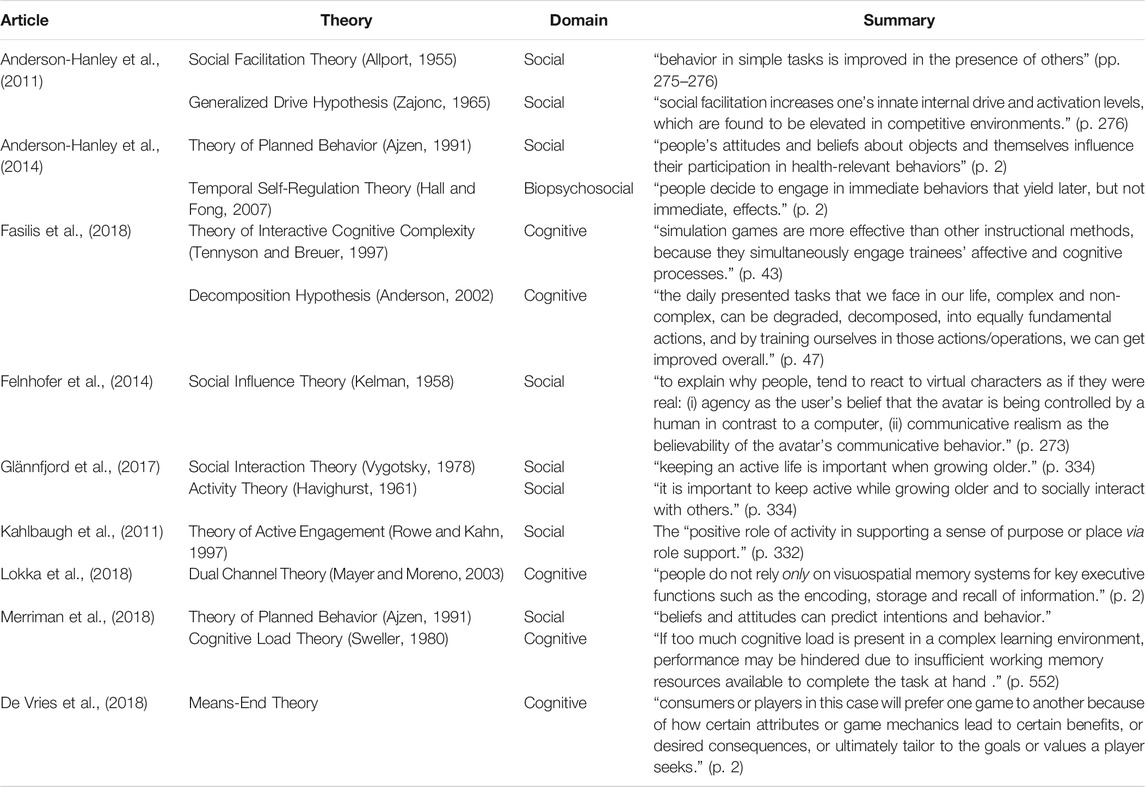
This paper outlines four popular theories that can be applied to AR/VR research; perceptual control theory, Self-affirmation theory, the transtheoretical model of behavior change and the transformative learning theory. However, none of these theories were considered by the studies included in review. Instead, 13 additional theories were used to support the AR/VR methodologies used in those papers (See Table 6) and only the theory of planned behavior (Anderson-Hanley et al., 2012; Merriman et al., 2018) was cited twice. Overall, the theories that were cited focused on either the impact of the surrounding environment (Anderson-Hanley et al., 2011; Felnhofer et al., 2014; Glännfjord et al., 2017), the intrinsic motivations of the individual (Anderson-Hanley et al., 2011; Kahlbaugh et al., 2011; Anderson-Hanley et al., 2014; Glännfjord et al., 2017; De Vries et al., 2018) or the complex cognitive processes occurring in the unconscious (Fasilis et al., 2018; Lokka et al., 2018; Merriman et al., 2018).
Discussion
This scoping review was undertaken to assess the variety and scale of AR/VR in use with older adults in relation to physical and mental health and wellbeing. As this study was completed in the first half of 2020, it includes the most recent relevant articles from 2019. Findings from this review, indicate that AR is not readily being used with this population in a health setting. More studies are using non-immersive VR (53%) compared to 2D VR (32%), but research of this kind is less likely to define VR before including it in the methodology.
Designing AR/VR Environments
As described in the results above, over a third of papers identified in this review are investigating the usability, feasibility, and design considerations important for AR/VR environments aimed at assisting older adults in their physical/mental health and general wellbeing. Despite the large number of papers investigating this area, very few used standardized measures. This impedes reviews such as this as comparisons and developments are more difficult to evaluate. However, three primary categories were identified including usability, feasibility, and tailored design (See Table 7). Within those categories there were many themes, which will now be discussed.
Usability
The most common factors identified as vital to usability were enjoyment and motivation. Many of the articles noted that participants reported either feeling enjoyment or a need to enjoy the activity to continue with the interventions. Similarly, motivation was identified as essential to continued engagement with the interventions over time. The remaining themes were not identified as often but were nonetheless important. Usability was dependent on participants receiving clear and simple instructions (Corno et al., 2014) and/or taking part in environments that were designed with clear and simple layouts (Blackman et al., 2007; Liu, 2010; Lokka et al., 2018). The concept of “matching” came up in three separate studies, though each with a different emphasis. Benoit et al. (2015) identified the importance of creating an environment where both the virtual and the real-world mirror each other (e.g., sitting at a table in a virtual environment, and sitting a table of similar height in the real-world) to help reduce the symptoms of cybersickness. Gomes et al. (2018) discusses the impact of games where the user/avatar appears stationary, but the user is required to take quick steps in the real-world and how this could result in adverse effects for the user. However, despite identifying this concern, they made no attempt to prevent or propose solutions. Finally, Korsgaard et al. (2019) considered the potential to increase use and willingness to use VR technology and applications through weather matching, or rather “miss-matching.” The ability of VR environments to provide a warm comfortable outside environment for exercise and other activities may entice older adult users into engaging with the technology on cold, wet days when they are unable to leave their homes. Perceived value of an intervention also had an impact on the usability of a piece of technology or virtual environment. Participants who could see how the exercise would help them were more likely to continue an intervention to the end and they were more likely to link it with their motivation to continue. How easy the technology was to use (Tsuda et al., 2016; Glännfjord et al., 2017) also played a part in the usability of the system; however, it was surprising that this factor was not mentioned more across the identified studies. Participant comfort considered both the equipment being used (Anderson-Hanley et al., 2011) and the features of users (e.g., eyeglasses) (Korsgaard et al., 2019), though again, not many findings or observations were identified. Other factors which played a part in the overall usability of a system included providing participants with a challenge (Merriman et al., 2018), choice of different user interfaces (Vallejo et al., 2014) so their motions/interactions are identified/picked-up, providing an environment that is consistent (Corno et al., 2014) with expectations (e.g., colors are not too bright etc.), easy to engage with (Manera et al., 2016), using simple user interfaces (Corno et al., 2014) and social interaction (Glännfjord et al., 2017) where the ability to compete and take part with others influenced participants decisions to continue engaging with the interventions.
Feasibility
Three studies considered the importance of safety in regards to the feasibility of their intervention. One study considered how the intervention itself provided additional safety to its participants when compared to completing a similar intervention in a real-world setting (Anderson-Hanley et al., 2011), another considered the impact simulator sickness may have on individuals with schizophrenia and determined there set-up was a safe alternative to HMD’s (Chan et al., 2010) and another considered the increased safety VR systems could provide to chemotherapy patients required to remain in clean-rooms (Tsuda et al., 2016). One study noted gender differences as a feasibility consideration (Matas et al., 2015); women were more prone to both motion and simulator sickness and the authors went on to suggest that drivers with a history of motion sickness should not take part in any immersive driving simulations. Participants inherent abilities should also be taken into consideration of the feasibility of a AR/VR set-up (Vallejo et al., 2014) as overly mismatching their ability to the task could pre-dispose participants to reduced motivation and incompletion of the intervention. This is in-line with research that argues that tasks themselves be tailored to the population (Corno et al., 2014). The final theme identified in this category related to older adults ability to understand the combining of virtual and real aspects of a mixed reality setting; for example, understanding that they could eat “anywhere” within the virtual environment even though no tables were visible despite having spent time in that environment while seated at their own table (Korsgaard et al., 2019). This is of particular importance as older adults and those with cognitive impairment must understand the environments they are immersed in so as to avoid any upset or negative effects on the participant.
Tailored Design
The final category could be broken into seven themes. Realism was identified as an important factor in continued use of a system (Marivan et al., 2016) but it was also worth noting that the level of realism was important for older adult populations (Lokka et al., 2018). Older adults initially preferred the realistic environment and a small percentage switched to using a mixed reality environment. However, despite the switch, over 50% of the older adults’ participants continued to prefer the realistic environment compared with a younger population. This is interesting as this research suggests that the mixed environment produced better recall (both long and short-term) in younger and older adult populations. This poses an interesting ethical dilemma that merits further examination; if personal choice and preference is important in establishing and retaining participant trust, comfort, and engagement until the end of an intervention, but researcher selected equipment and environments are expected to demonstrate greater efficacies, is it justifiable to remove those choices? Are the potential results, the expected savings in study finance, resources, and time acceptable reasons for limiting interventions with these vulnerable populations?
Many studies using AR/VR use navigation tasks to assess memory and attention in cognitively impaired populations. Active navigation is an interesting factor to consider as it requires the participant to navigate a virtual environment themselves using some form of UI, whereas passive navigation typically demonstrates a route or direction through pre-recorded video. Active navigation increases recognition hits in older adults, however it also increases false positives in older adult populations (Sauzéon et al., 2016). Often it is both necessary and preferred that participants actively engage in a virtual intervention, but if there is a possibility that the subsequent results are Type 1 errors, then checks and controls should be built into the intervention procedures. An interesting interaction between education level and computer self-efficacy was also reported (Felnhofer et al., 2014). Older adults with higher education were better able and more confident in using the virtual environments. Many current older adults may have missed educational opportunities due to historic circumstance, however as education levels in the global aging population increase, progressively more and more older adults will be proficient technology users. Researchers should no longer assume older populations are technologically illiterate. Older adults are more capable than ever at interacting with complex technology, but there is still a learning curve. It has been suggested that when instructing participants on the procedure of an intervention or task, they should first be introduced to the technology and allowed to interact with it (Corno et al., 2014). Adjustment periods ensure that participants do not become distracted by the technology during the data collection period. The level of immersion is also an important factor to consider for Alzheimer’s and Dementia populations. There may be an assumption that these populations can become confused with high levels of immersion or through the use of 3D glasses but Manera et al. (2016) found that participants preferred the 3D environment when compared with a 2D paper task. Similarly, research with Parkinson’s patients (dos Santos Mendes et al., 2012) has noted that also they can have difficulty with virtual games due to increased motor difficulties, this does not prevent them from learning, improving and retaining the positive effects of exergaming. In contrast, those with cognitive impairment are more likely to experience inhibited learning.
The key take home message across these studies is the importance of positive user experience influencing the usability and feasibility of AR/VR environments and technologies (Vallejo et al., 2014, p. 24; Yeh et al., 2019, p. 10).
Increasingly, research is being conducted with the assistance of experts by experience (public, patient involvement; PPI). The is an important paradigm shift for researchers. By asking living experts to help design (make suggestions), and evaluate virtual environments as they are created you increase the likelihood that your intervention will meet the needs and requirements necessary for that population group (Corno et al., 2014). By including PPI researchers will address two vital factors for feasibility of AR/VR research interventions, designing tasks with a population in mind and matching the abilities of the participants to the task.
The Lack of Augmented Reality
This review indicates that AR is rarely being used as a form of digital intervention. There are many reasons for this. When the original articles were screened for title and abstract two main clusters of articles were identified that closely matched the current search but were different enough to warrant exclusion. These included articles where AR/VR were used as either a means of diagnosis or studies that used virtual technology as a convenient alternative to a potentially dangerous real-world setting; the effects of the virtual environment or equipment was not itself examined. A greater number of AR papers may have fallen into these alternate categories. Another reason AR technology may have been absent from these results is the current focus of AR studies. Much of the research employs smart-phone applications (such as Pokémon Go), which older adults are less likely to engage with. AR also features in research in the areas of education, tourism, and advertising; areas where digital interventions are not always targeted toward older adults. In comparison to VR, many AR studies may still be in their infancy and while they would suit an older population, research tends not to be directed to those 60°years and above. Finally, several studies in this review include samples where younger participants were present, but where older adults’ results were reported separately. AR research may not yet categorize their samples to the degree required by this review.
VR-Based Interventions
This review has identified several sub-populations and areas of interest where virtual reality technology is being used to affect the physical/mental health and wellbeing of older adults. Populations include healthy, physically, and cognitively impaired, and emotionally vulnerable older adults (Tarnanas et al., 2015, p. 3; Wiederhold, 2016, p. 577–578; Riva et al., 2019, p. 82–88). VR technology has demonstrated its positive impacts using immersive environments that can display games, exercises and true-to-life digitally created surroundings. The environments in the 65 studies in this review were used to increase physical activity, improve balance, memory, attention, and quality of life, and to reduce falls, anxiety, and depression. The most common limitations described included small sample sizes not representative of the larger populations (including limited gender balances), a lack of control groups, limited access to technical (gameplay) data and short intervention periods often due to a lack of time/resources. Future research in this area should look at large scale studies with interventions capable of being personalized and meeting the recommended length of time for behavior change (12 weeks). Participants should be more representative of the general population with gender, education level, ethnicity and socioeconomic status all taken into consideration. Technical interventions should include neurobiological assessments as control measures to further support physical and cognitive change assessments. Areas needing further exploration include, active identify of older adults and its role in influencing VR related exercise behavior (Anderson-Hanley et al., 2011), acceptance of VR supported interventions in hospital-bound populations (Korsgaard et al., 2019), the experience of immersion and flow in 3D VR training (Lee et al., 2017), and investigating natural user interfaces to allow for simultaneous dual motion input (Vallejo et al., 2014).
Theories in Practice
This review drew attention to four well known theories (Riva et al., 2016) that can be applied to AR/VR research. The authors expected to find these theories being used to support the methodologies used by the identified articles but only nine papers used psychological theory to support their intervention. Unexpectedly, none of the theories put forth by Riva and colleagues (2016) were used. However, the 13 theories adopted by researchers to support AR/VR research (see Table 6 above) were also based on social, cognitive, and biopsychosocial frameworks. Most of the theories were social, and a common theme included the influence of others of behavior (38%). Other areas of effect included impact of the surrounding environment (23%), intrinsic motivation of the individual (7%) and interaction with cognitive processes (38%). These studies clearly demonstrate the psychological underpinnings related to and influencing the effects of AR/VR methodological design. However, most studies evaluated in this review offered no theoretical support for their experimental design. Behavior change research is complex and often interventions designed to effect change are activating many interconnected components that work together to produce a response. Even when an intervention is successful, the lack of appropriate theoretical supports means there is no way to accurately determine what underpinned this success (Michie et al., 2014). Future researchers must reconsider incorporating psychological theory to provide strong foundations from which to develop effective, lasting and, impactful AR/VR interventions.
Specific Domains
Within the social domain, the theories addressed the impact of others on the behaviors of the individual during interventions. The transformative Learning Theory model was also based in a social framework and while it was not referenced specifically, common aspects of this theory included, recognition of the self and revision of beliefs leading to behavior change. The cognitive domain was more prominent in the theories presented by Riva et al. (2016) but these theories were less frequent in the identified literature. However, these theories are similar in that the place the self at the forefront and behavior change is influenced by our perceptions. Socio-cognitive and biopsychosocial models were presented as explanations for behavior change and while these models were the least incorporated, they are the most complex supporting explanations for behavior changes because of complex interconnections between the environment, cognition, social influences, biological predispositions, and psychological health.
Defining Virtual and Augmented Reality
When searching the literature for virtual and augmented reality research it became clear that there was no single definition in use. Many studies used terms like virtual, augmented, and mixed reality to describe 3D virtual environments displayed onto 2D desktop environments. The “reality-virtuality continuum” (Eckert et al., 2019, p. 2) suggests that terms like “virtual environment” and “virtual reality” can be used to describe these two-dimensional displays. However, AR/VR technologies have advanced beyond the systems available in the 1990s and the continuum does not accurately differentiate digitally created environments. A desktop environment like Sims™ or Second Life™ can be called a “virtual environment” but so too can an immersive display in a HMD like the Oculus Rift™. Only 16 of 65 papers in this review provided a definition of VR. All 16 definitions considered the digitally created environment and real-time interaction, but only seven also mentioned the user (See Table 4) and only one defined “mixed reality;” a term often used to describe the combination of virtual and augmented reality technology elements. The remaining definitions described only the technical elements (e.g., computer simulated environment, interaction of computer-generated experience) required to create VR. This illustrates an interesting distinction between papers that focus solely on the technical components (50%) and those that consider the human interaction as a vital step in the virtuality process. There is no clear way to determine which approach is more successful in terms of reaching the objectives of the planned intervention however, future research could set out to identify the definitions/descriptions used in quantitative AR/VR research and complete a meta-analysis comparing the outcomes of the studies. In general, these findings support those of Kardong-Edgren et al. (2019), (p. 33) who identified 14 different VR definitions and six different AR definitions in their review. These combinations of ambiguity and opposing perspectives contributes to the complexity of true AR/VR and clearly demonstrates the need for a more robust taxonomy. This review also aimed to determine if consistent terminology was being used in AR/VR research. Only five studies using the term VR involved a fully immersive virtual environment. The remaining 57 studies used variations of “virtual reality” and “virtual environments” to describe their technology. Over 70% of studies in this analysis mislabeled themselves as “virtual reality” and this may be attributed to two main factors. First, very few studies provided an operational definition of virtual reality and this leads to ambiguities and misunderstandings as readers attempt to ascribe a label to the technology used. Second, while virtual (Milgram and Kishino, 1994, p. 8–12) and augmented reality (Grubert et al., 2017, p. 1711–1715; Hugues et al., 2011, p. 5–15) taxonomies exist, they do not accurately describe the modern technologies available (e.g., describing analogue or digital monitors), which adds further confusion to an already complex and quickly evolving area.
These inconsistent terms and definitions emphasize the need for more sophisticated terminology to describe virtual designs. In addition, one study described their set-up as a virtual reality, referring to a video they had taken as a virtual environment (Choi and Lee, 2019, p. 862). Under the “reality-virtuality continuum” (Eckert et al., 2019, p. 2) this identification is legitimate, but it is inaccurate. Asking participants to watch a video and follow along with the motions is not the same as a participant interacting in real-time within a 3D virtual environment that can track movement and provide an immersive user experience. While the definitions of McCloy and Stone (2001), (p. 912) Botella et al. (2015), (p. 2) used in planning this review are the most acceptable definitions that are currently available, greater nuance is required to convey fully the degree and level of immersion required in a virtual reality system. Based on the definitions identified in this review and those identified in the call for unification of virtual reality theories (Kardong-Edgren et al., 2019, p. 30–31), we have identified the following elements which are required to formulate a more complete definition. There must be reference to 3D graphics displayed in either 2-or-3 dimensions. This should include everything from projector screens, television sets, computer monitors and HMD’s. The second element of a new definition should address the level of interaction available to the users including multimodal systems combining the senses to create full-body experiences and increasing levels of user interfaces ranging from controllers and joysticks to motion control, position tracking and multi-modal interface in-puts. Finally, a new definition should include the ability to view the environment and any avatars in either first or third person perspective. This is a complicated task as even with these factors there are many levels of technology included. To fully address the insufficient language and terminology in this complex area, an updated taxonomy classifying virtual and augmented technologies is urgently required.
Strengths and Limitations
This review evaluated many studies to determine how AR/VR is used when aiming to improve physical/mental health and general wellbeing of older adults. The analysis clearly demonstrates the assortment of technologies available, but also the insufficient terminology available to categorize and identify them. Two researchers conducted the screening for this review ensuring consensus was reached on all points. Finally, three systematic reviews (Hugues et al., 2011; Miller et al., 2014; Coyle et al., 2015) identified in the screening process were used to supplement the initial search and an additional 13 studies were included in this review.
Two branches of AR/VR research were not included in this review (use as a diagnostic tool and use as a methodology rather than the factor under investigation) due to time constraints. Both areas are large enough to warrant their own review. Another limitation to this study is the lack of AR research found. This may be due to the focus on older adults in this review, or that AR research may not report the older participants as an individual group. Another factor may be the availability of AR technology. Newer models of smart phones and tablets may be AR compatible, but these may not be used to the same extent in an older population.
Conclusion
This scoping review aimed to identify how AR/VR technology was used within an older adult population to influence their physical, mental health and wellbeing. Only five studies were objectively classified as VR and only one study used AR. However, these studies encompassed a wide range of domains including improving physical activity, balance, memory, attention, and quality of life, and reducing falls, anxiety, and depression. A secondary aim of this study was to identify whether the terminology used across the studies was consistent. Findings have demonstrated that terms such as virtual reality and virtual environments are used to describe many levels of technology. Many of the papers discussed in this review provide no definition of virtual reality and those that do, lack consensus. Further, half of these definitions fail to include the user despite the user being central to the intervention being conducted. This review has proposed the elements necessary to construct an alternative definition. It also urgently calls for an updated taxonomy to address the varying levels of technology and immersion used in today’s virtual reality research. Similarly, there are many useful theories that can bring focus to the factors influencing behavior change. When designing these interventions, the authors urge researchers to do so with a strong theoretical foundation.
Author Contributions
The main body of research was conducted by JC supported by LH and AF. Contributors to the paper include, RL-V, PB, and EK.
Funding
This review was undertaken as part of the CAPTAIN Project–Horizon 2020: European Union Funding for Research and Innovation Call: S1-PM-15-2017.
Conflict of Interest
Author EK was employed by the company WITA.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frvir.2021.655338/full#supplementary-material
References
Agmon, M., Perry, C. K., Phelan, E., Demiris, G., and Nguyen, H. Q. (2011). A Pilot Study of Wii Fit Exergames to Improve Balance in Older Adults. J. Geriatr. Phys. Ther. 34 (4), 161–167. doi:10.1519/JPT.0b013e3182191d98
Ajzen, I. (1991). The Theory of Planned Behavior. Organiz. Behav. Human Dec. Proc. 50, 179–211. doi:10.1016/0749-5978(91)90020-T
Allport, F. (1995). The Influence of the Group upon Association and Thought (1920). In Small Groups: Studies in Social Interaction. Editors P. Hare, E. F. Borgatta, and R. F. Bales, 31–34.
Anderson-Hanley, C., Arciero, P. J., Barcelos, N., Nimon, J., Rocha, T., Thurin, M., et al. (2014). Executive Function and Self-Regulated Exergaming Adherence Among Older Adults. Front. Hum. Neurosci., 8(989) 1–8. doi:10.3389/fnhum.2014.00989
Anderson-Hanley, C., Arciero, P. J., Brickman, A. M., Nimon, J. P., Okuma, N., Westen, S. C., et al. (2012). Exergaming and Older Adult Cognition: A Cluster Randomized Clinical Trial. Am. J. Prev. Med., 42(2), 109–119. doi:10.1016/j.amepre.2011.10.016
Anderson-Hanley, C., Snyder, A. L., Nimon, J. P., and Arciero, P. J. (2011). Social Facilitation in Virtual Reality-Enhanced Exercise: Competitiveness Moderates Exercise Effort of Older Adults. Clin. interventions Aging 6, 275. doi:10.2147/CIA.S25337
Anderson, J. R. (2002). Spanning seven orders of magnitude: A challenge for cognitive modeling. Cognitive Sci. 26, 85–112. doi:10.1207/s15516709cog2601_3
Bacha, J. M. R., Gomes, G. C. V., de Freitas, T. B., Viveiro, L. A. P., da Silva, K. G., Bueno, G. C., et al. (2018). Effects of Kinect Adventures Games versus Conventional Physical Therapy on Postural Control in Elderly People: A Randomized Controlled Trial. Games Health J. 7 (1), 24–36. doi:10.1089/g4h.2017.0065
Barbosa, C. F. M., Pavanelli, I. L., Silva, T. D. O. S., Júnior, P. R. R., and do Nascimento, G. B. (2019). Effectof Virtual Reality on the Intensity of Dizziness and Quality of Life in the Elderly Withunilateral Vestibular Hypo-Function. Fisoterapia Brasil, 20 (2), 278 – 287. doi:10.33233/fb.v20i2.2846
Bell, C. S., Fain, E., Daub, J., Warren, S. H., Howell, S. H., Southard, K. S., et al. (2011). Effects of Nintendo Wii on Quality of Life, Social Relationships, and Confidence to Prevent Falls. Phys. Occup. Ther. Geriatr., 29(3), 213–221. doi:10.3109/02703181.2011.559307
Benoit, M., Petit, P. D., and Manera, V. (2015). Is it Possible to Use Highly Realistic Virtual Reality in the Elderly? a Feasibility Study with Image-Based Rendering. Neuropsychiatr. Dis. Treat., 11, 557–563. doi:10.2147/NDT.S73179
Bisson, E., Contant, B., Sveistrup, H., and Lajoie, Y. (2007). Functional Balance and Dual-Task Reaction Times in Older Adults Are Improved by Virtual Reality and Biofeedback Training. Cyberpsychology Behav. 10 (1), 16–23. doi:10.1089/cpb.2006.9997
Blackman, T., Van Schaik, P. A. U. L., and Martyr, A. (2007). Outdoor Environments for People with Dementia: an Exploratory Study Using Virtual Reality. Ageing Soc. 27 (6), 811. doi:10.1017/S0144686X07006253
Botella, C., Pérez-Ara, M. A., Bretón-López, J., Quero, S., García-Palacios, A., and Baños, R. M. (2015). In Vivo versus Augmented Reality Exposure in the Treatment of Small Animal Phobia: A Randomized Controlled Trial. PLOS ONE 11 (2). doi:10.1371/journal.pone.0148237
Botella, C., Riva, G., Gaggioli, A., Wiederhold, B. K., Alcaniz, M., and Baños, R. M. (2012). The Present and Future of Positive Technologies. Cyberpsychology, Behav. Soc. Networking 15 (2), 78–84. doi:10.1089/cyber.2011.0140
Cacciata, M., Stromberg, A., Lee, J. A., Sorkin, D., Lombardo, D., Clancy, S., et al. (2019). Effect of Exergaming on Health-Related Quality of Life in Older Adults: A Systematic Review. Int. J. Nurs. Stud., 93, 20 – 40. doi:10.1016/j.ijnurstu.2019.01.010
Chan, C. L., Ngai, E. K., Leung, P. K., and Wong, S. (2010). Effect of the Adapted Virtual Realitycognitive Training Program Among Chinese Older Adults with Chronic Schizophrenia: A Pilot Study. Int. J. Geriatr. Psychiatry A J. Psychiatry Late Life Allied Sci. 25 (6), 643–649. doi:10.1002/gps.2403
Choi, W., and Lee, S. (2019). The Effects of Virtual Kayak Paddling Exercise on Postural Balance, Musical Performance, and Cognitive Function in Older Adults with Mild Cognitive Impairment; a Randomized Controlled Trial. J. Aging Phys. Activity, 27(6), 861–870. doi:10.1123/japa.2018-0020
Corno, G., Bouchard, S., and Forget, H. (2014). Usability Assessment of the Virtual Multitasking Test (V-mt) for Elderly People. Annu. Rev. Cyberther. Telemed 199, 168–172. doi:10.3233/978-1-61499-401-5-168
Coyle, H., Traynor, V., and Solowij, N. (2015). Computerized and Virtual Reality Cognitive Training for Individuals at High Risk of Cognitive Decline: Systematic Review of the Literature. Am. J. Geriatr. Psychiatry, 23(4), 335–359. doi:10.1016/j.jagp.2014.04.009
De Vries, A. W., Van Dieën, J. H., Van Den Abeele, V., and Verschueren, S. M. (2018). Understanding Motivations and Player Experiences of Older Adults in Virtual Reality Training. Games Health J. 7 (6), 369–376. doi:10.1089/g4h.2018.0008
dos Santos Mendes, F. A., Pompeu, J. E., Lobo, A. M., da Silva, K. G., de Paula Oliveira, T., Zomignani, A. P., et al. (2012). Motor Learning, Retention, and Transfer after Virtual-Reality-Based Training in Parkinson's Disease–Effect of Motor and Cognitive Demands of Games: a Longitudinal, Controlled Clinical Study. Physiotherapy, 98(3), 217–223. doi:10.1016/j.physio.2012.06.001
Eckert, M., Volmerg, J. S., and Friedrich, C. M. (2019). Augmented Reality in Medicine: Systematic and Bibliographic Review. JMIR Mhealth Uhealth 7 (4), e10967. doi:10.2196/10967
Eggenberger, P., Schumacher, V., Angst, M., Theill, N., and de Bruin, E. D. (2015). Does Multicomponent Physical Exercise with Simultaneous Cognitive Training Boost Cognitive Performance in Older Adults? A 6-month Randomized Controlled Trial with a 1-year Follow-Up. Clin. Interventions Aging 10, 1335–1349. doi:10.2147/CIA.S87732
Eurostat(2020). Demographic Balances and Indicators by Type of Projection: Proportion of population aged 65 years or more [Data set]. Avaliable at: https://appsso.eurostat.ec.europa.eu/nui/submitViewTableAction.do dataset
Fasilis, T., Patrikelis, P., Siatouni, A., Alexoudi, A., Veretzioti, A., Zachou, L., et al. (2018). A Pilot Study and Brief Overview of Rehabilitation via Virtual Environment in Patients Suffering from Dementia. Psychiatriki = Psychiatriki 29 (1), 42–51. doi:10.22365/jpsych.2018.291.42
Felnhofer, A., Kothgassner, O. D., Hauk, N., Beutl, L., Hlavacs, H., and Kryspin-Exner, I. (2014). Physical and Social Presence in Collaborative Virtual Environments: Exploring Age and Gender Differences with Respect to Empathy. Comput. Hum. Behav., 31, 272–279. doi:10.1016/j.chb.2013.10.045
Franco, J. R., Jacobs, K., Inzerillo, C., and Kluzik, J. (2012). The Effect of the Nintendo Wii Fit and Exercise in Improving Balance and Quality of Life in Community Dwelling Elders. Tech. Health Care 20 (2), 95–115. doi:10.3233/THC-2011-0661
Gamito, P., Oliveira, J., Morais, D., Coelho, C., Santos, N., Alves, C., et al. (2019). Cognitive Simulation of Elderly Individuals with Instrumental Virtual Reality-Based Activities of Daily Life: Pre-post Treatment Study. Cyberpsychology, Behav. Soc. Networking 22 (1), 69–75. doi:10.1089/cyber.2017.0679
Gamito, P., Oliveira, J., Rosa, P., Morais, D., Duarte, N., Oliveira, S., et al. (2010). PTSD Elderly War Veterans: A Clinical Controlled Pilot Study. Cyberpsychology, Behav. Soc. Networking 13 (1), 43–48. doi:10.1089/cyber.2009.0237
Glännfjord, F., Hemmingsson, H., and Larsson Ranada, Å. (2017). Elderly People’s Perceptions of Using Wii Sports Bowling - A Qualitative Study. Scand. J. Occup. Ther. 24 (5), 329–338. doi:10.1080/11038128.2016.1267259
Gomes, G. C. V., do Socorro Simões, M., Lin, S. M., Bacha, J. M. R., Viveiro, L. A. P., Varise, E. M., et al. (2018). Feasibility, Safety, Acceptability, and Functional Outcomes of Playing Nintendo Wii Fit PlusTM for Frail Older Adults: A Randomized Feasibility Clinical Trial. Maturitas, 118, 20–28. doi:10.1016/j.maturitas.2018.10.002
Graffigna, G., Barello, S., and Riva, G. (2013). Technologies for Patient Engagement. Health Aff. 32 (6), 1172. doi:10.1377/hlthaff.2013.0279
Grubert, J., Langlotz, T., Zollmann, S., and Regenbrecht, H. (2017). Towards Pervasive Augmented Reality: Context-Awareness in Augmented Reality. IEEE Trans. Visualization Comp. Graphics 23 (6), 1706–1723. doi:10.1109/TVCG.2016.2543720
Guisado-Fernández, E., Giunti, G., Mackey, L. M., Blake, C., and Caulfield, B. M. (2019). Factors Influencing the Adoption of Smart Health Technologies for People with Dementia and Their Informal Caregivers: Scoping Review and Design Framework. JMIR Aging 2 (1), e12192. doi:10.2196/12192
Hall, P. A., and Fong, G. T. (2007). Temporal self-regulation theory: A model for individual health behavior. Psychol. Rev. 1, 6–52. doi:10.1080/17437190701492437
Hsieh, C. C., Kin, P. S., Hsu, W. C., Wang, J. S., Huang, Y. C., Lim, A. Y., et al. (2018). The Effectiveness of a Virtual Reality-Based Tai Chi Exercise on Cognitive and Physical Function in Older Adults with Cognitive Impairment. Demen. Geriatr. Cogn. Disord. 46 (5–6), 358–370. doi:10.1016/j.physio.2015.03.3418
Hugues, O., Fuchs, P., and Nannipieri, O. (2011). “New Augmented Reality Taxonomy: Technologies and Features of Augmented Environment,” in Handbook of Augmented Reality. Editor B. Furht (New York: Springer-Verlag), 47–63. doi:10.1007/978-1-4614-0064-6_2
Huth, K., Amar-Dolan, L., Perez, J. M., Luff, D., Cohen, A. P., Glader, L., et al. (2020). Visiting Jack: Mixed Methods Evaluation of a Virtual home Visit Curriculum with a Child with Medical Complexity. Acad. Pediatr., 20(7), doi:10.1016/j.acap.2020.05.001
Kahlbaugh, P. E., Sperandio, A. J., Carlson, A. L., and Hauselt, J. (2011). Effects of Playing Wii on Well-Being in the Elderly: Physical Activity, Loneliness, and Mood. Activities. Adaptation & Aging 35 (4), 331–344. doi:10.1080/01924788.2011.625218
Karahan, A. Y., Tok, F., Taşkın, H., Küçüksaraç, S., Başaran, A., and Yıldırım, P. (2015). Effects of Exergames on Balance, Functional Mobility, and Quality of Life of Geriatrics versus home Exercise Programme: Randomized Controlled Study. Cent. Eur. J. Public Health, 23(Suppl. ment), S14–S18. doi:10.21101/cejph.a4081
Kardong-Edgren, S., Farra, S. L., Alinier, G., and Young, H. M. (2019). A Call to Unify Definitions of Virtual Reality. Clin. Simulation Nurs. 31. 28–34. doi:10.1016/j.ecns.2019.02.006
Kelman, H. C. (1958). Compliance, identification, and internalization three processes of attitude change. J. Conflict Resolut. 2, 51–60. doi:10.1177/002200275800200106
Kitson, A., Prpa, M., and Riecke, B. E. (2018). Immersive Interactive Technologies for Positive Change: A Scoping Review and Design Considerations. Front. Psychol. 9 1354. doi:10.3389/fpsyg.2018.01354
Kizony, R., Levin, M. F., Hughey, L., Pérez, C., and Fung, J. (2010). Cognitive Load and Dual-Task Performance during Locomotion Poststroke: A Feasibility Study Using a Functional Virtual Environment. Phys. Ther., 90, 252 – 260. doi:10.2522/ptj.20090061
Kizony, R., Weiss, P., Shahar, M., and Rand, D. (2006). TheraGame–a home Based Virtual Reality Rehabilitation System. Denmark: Esbjerg. doi:10.1515/IJDHD.2006.5.3.265
Knowles, L. M., Stelzer, E-M., Jovel, K. S., and O’Connor, M-F. (2017). A Pilot Study of Virtual Support for Grief: Feasibility, Acceptability, and Preliminary Outcomes. Comput. Hum. Behav., 73, 650 – 658. doi:10.1016/j.chb.2017.04.005
Korsgaard, D., Bjøner, T., and Nilsson, N. C. (2019). Where Would You like to Eat? A Formative Evaluation of Mixed-Reality Solitary Meals in Virtual Environments for Older Adults with Mobility Impairments Who Live Alone. Food Res. Int., 117, 30–39. doi:10.1016/j.foodres.2018.02.051
Laver, K., George, S., Ratcliffe, J., Quinn, S., Whitehead, C., Davies, O., et al. (2012). Use of an Interactive Video Gaming Program Compared with Conventional Physiotherapy for Hospitalised Older Adults: a Feasibility Trial. Disabil. Rehabil. 34 (21), 1802–1808. doi:10.3109/09638288.2012.662570
Lee, M., Son, J., Kim, J., and Yoon, B. (2015). Individualized Feedback-Based Virtual Reality Exercise Improves Older Women’s Self-Perceived Health: A Randomized Controlled Trail. Arch. Gerontol. Geriatr. 61(2), 154–160. doi:10.1016/j.archger.2015.06.010
Lee, S., and Shin, S. (2013). Effectiveness of Virtual Reality Using Video Gaming Technology in Elderly Adults with Diabetes Mellitus. Diabetes Technol. Ther. 15 (6), 489–496. doi:10.1089/dia.2013.0050
Lee, Y., Choi, W., Lee, K., Song, C., and Lee, S. (2017). Virtual Reality Training with Three-Dimensional Video Games Improves Postural Balance and Lower Extremity Strength in Community-Dwelling Older Adults. J. Aging Phys. Activity, 25(4), 621–627. doi:10.1123/japa.2015.2015-0271
Levy, F., Leboucher, P., Rautureau, G., Komano, O., Millet, B., and Jouvent, R. (2016). Fear of Falling: Efficacy of Virtual Reality Associated with Serious Games in Elderly People. Neuropsychiatr. Dis. Treat. 12, 877–881. doi:10.2147/NDT.S97809
Liu, C. L. (2010). The Impact of Goods-Classification and Landmarks for Spatial Knowledge and Goods-Finding in the Elderly within a 3D Virtual Store. Comput. Hum. Behav., 26(6), 1777–1786. doi:10.1016/j.chb.2010.07.005
Lokka, I. E., Çöltekin, A., Wiener, J., Fabrikant, S. I., and Röcke, C. (2018). Virtual Environments as Memory Training Devices in Navigational Tasks for Older Adults. Scientific Rep. 8 (1), 1–15. doi:10.1038/s41598-018-29029-x
Man, D. W., Chung, J. C., and Lee, G. Y. (2012). Evaluation of a Virtual Reality-Based Memory Training Programme for Hong Kong Chinese Older Adults with Questionable Dementia: a Pilot Study. Int. J. Geriatr. Psychiatry 27 (5), 513–520. doi:10.1002/gps.2746
Manera, V., Chapoulie, E., Bourgeois, J., Guerchouche, R., David, R., and Ondrej, J. (2016). A Feasibility Study with Image-Based Rendered Virtual Reality in Patients with Mild Cognitive Impairment and Dementia. PLoS ONE 11 (3), e0151487. doi:10.1371/journal.pone.0151487
Marivan, K., Boully, C., Benveniste, S., Reingewirtz, S., Rigaud, A.-S., Kemoun, G., et al. (2016). Rehabilitation of the Psychomotor Consequences of Falling in an Elderly Population: A Pilot Study to Evaluate Feasibility and Tolerability of Virtual Reality Training. Tech. Health Care 24 (2), 169–175. doi:10.3233/THC-151114
Matas, N. A., Nettelbeck, T., and Burns, N. R. (2015). Dropout during a Driving Simulator Study: a Survival Analysis. J. Saf. Res., 55, 159–169. doi:10.1016/j.jsr.2015.08.004
Mayer, R. E., and Moreno, R. (2003). Nine Ways to Reduce Cognitive Load in Multimedia Learning. Educ. Psychol. 38, 43–52. doi:10.1207/S15326985EP3801_6
McCloy, R., and Stone, R. (2001). Virtual Reality in Surgery. Bmj 323 (7318), 912–915. doi:10.1136/bmj.323.7318.912
Merriman, N. A., Roudaia, E., Romagnoloi, M., Orvieto, I., and Newell, F. N. (2018). Acceptability of a custom-designed game, CityQuest, aimed at improving balance confidence and spatial cognition in fall-prone and healthy older adults, Behav. Inf. Tech., 37(6), 538 – 557. doi:10.1080/0144929X.2018.1462402
Merriman, N. A., Whyatt, C., Setti, A., Craig, C., and Newell, F. N. (2015). Successful Balance Training Is Associated with Improved Multisensory Function in Fall-Prone Older Adults. Comput. Hum. Behav., 45, 192–203. doi:10.1016/j.chb.2014.12.017
Michie, P. S., West, P. R., Campbell, P. R., Brown, D. J., and Gainforth, D. H. (2014). ABC of Behaviour Change Theories. Silverback Publishing.
Milgram, P., and Kishino, F. (1994). A Taxonomy of Mixed Reality Visual Displays. IEICE Trans. Inf. Syst. E77 (12), 1321–1329. 10.1.1.102.4646
Miller, K. J., Adair, B. S., Pearce, A. J., Said, C. M., Ozanne, E., and Morris, M. M. (2014). Effectiveness and Feasibility of Virtual Reality and Gaming System Use at home by Older Adults for Enabling Physical Activity to Improve Health-Related Domains: a Systematic Review. Age and ageing, 43(2), 188–195. doi:10.1093/ageing/aft194
Mirelman, A., Maidan, I., Herman, T., Deutsch, J. E., Giladi, N., and Hausdorff, J. M. (2011). Virtual Reality for Gait Training: Can it Induce Motor Learning to Enhance Complex Walking and Reduce Fall Risk in Patients with Parkinson’s Disease?. The Journals Gerontol. Ser. A 66 (2), 234–240. doi:10.1093/Gerona/glq201
Monteiro-Junior, R. S., da Silva Figueiredo, L. F., de Tarso Maciel-Pinheiro, P., Abud, E. L. R., Braga, A. E. M. M., BarcaEngedal, M. L. K., et al. (2017). Acute Effects of Exergames on Cognitive Function of Institutionalized Older Persons: A Single-Blinded, Randomized and Controlled Pilot Study. Aging Clin. Exp. Res. 29 (3), 387–394. doi:10.1007/s40520-016-0595-5
Morone, G., Paolucci, T., Luziatelli, S., Iosa, M., Piermattei, C., Zangrando, F., et al. (2016). Wii Fit Is Effective in Women with Bone Loss Condition Associated with Balance Disorders: a Randomized Controlled Trial. Aging Clin. Exp. Res. 28 (6), 1187–1193. doi:10.1007/s40520-016-0578-6
Ng, Y. L., Ma, F., Ho, F. K., Ip, P., and Fu, K. W. (2019). Effectiveness of Virtual and Augmented Reality-Enhanced Exercise on Physical Activity, Psychological Outcomes, and Physical Performance: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Comput. Hum. Behav., 99, 278–291. doi:10.1016/j.chb.2019.05.026
Optale, G., Urgesi, C., Busato, V., Marin, S., Piron, L., Priftis, K., et al. (2010). Controlling Memory Impairment in Elderly Adults Using Virtual Reality Memory Training: a Randomized Controlled Pilot Study. Neurorehabil. Neural Repair 24 (4), 348–357. doi:10.1177/1545968309353328
Padala, K. P., Padala, P. R., Lensing, S. Y., Dennis, R. A., Bopp, M. M., Parkes, C. M., et al. (2017a). Efficacy of Wii-Fit on Static and Dynamic Balance in Community Dwelling Older Veterans: a Randomized Controlled Pilot Trial. J. Aging Res., 2017:4653635. doi:10.1155/2017/4653635
Padala, K. P., Padala, P. R., Lensing, S. Y., Dennis, R. A., Bopp, M. M., Roberson, P. K., et al. (2017b). Home-based Exercise Program Improves Balance and Fear Offalling in Community-Dwelling Older Adults with Mild Alzheimer’s Disease: a Pilot Study. J. Alzheimer's Dis. 59 (2), 565–574. doi:10.3233/JAD-170120
Padala, K. P., Padala, P. R., Malloy, T. R., Geske, J. A., Dubbert, P. M., Dennis, R. A., et al. (2012). Wii-fit for Improving Gait and Balance in an Assisted Living Facility: a Pilot Study. J. Aging Res., 2012:597573, doi:10.1155/2012/597573
Parijat, P., Lockhart, T. E., and Liu, J. (2014). EMG and Kinematic Responses to Unexpected Slips after Slip Training in Virtual Reality. IEEE Trans. Biomed. Eng. 62 (2), 593–599. doi:10.1109/TBME.2014.2361324
Parker, M. G., Willett, A. B., Tyson, S. F., Weightman, A. P., and Mansell, W. (2020). A Systematic Evaluation of the Evidence for Perceptual Control Theory in Tracking Studies. Neurosci. Biobehavioral Rev., 112, 616–633. doi:10.1016/j.neubiorev.2020.02.030
Riva, G., Baños, R. M., Botella, C., Mantovani, F., and Gaggioli, A. (2016). Transforming Experience: The Potential of Augmented Reality and Virtual Reality for Enhancing Personal and Clinical Change. Front. Psychiatry 7, 164. doi:10.3389/fpsyt.2016.00164
Riva, G., Wiederhold, B. K., and Mantovani, F. (2019). Neuroscience of Virtual Reality: From Virtual Exposure to Embodied Medicine. Cyberpsychology, Behav. Soc. networking 22 (1), 82–96. doi:10.1089/cyber.2017.29099.gri
Rizzo, A., and Kim, G. J. (2005). Virtual Reality Rehabilitation and Therapy. PRESENCE: Teleoperators Virtual Environ. 14, 119–146. doi:10.1162/1054746053967094
Rodrigues, E. V., Gallo, L. H., Guimaraes, A. T. B., Melo Filho, J., Luna, B. C., and Gomes, A. R. S. (2018). Effects of Dance Exergaming on Depressive Symptoms, Fear of Falling,and Musculoskeletal Function in Fallers and Nonfallers Community-Dwelling Older Women. Rejuvenation Res. 21 (6), 518–526. doi:10.1089/rej.2017.2041
Rosenberg, D., Depp, C. A., Vahia, I. V., Reichstadt, J., Palmer, B. W., Kerr, J., et al. (2010). Exergames for Subsyndromal Depression in Older Adults: a Pilot Study of a Novel Intervention. Am. J. Geriatr. Psychiatry 18 (3), 221–226. doi:10.1097/JGP.0b013e3181c534b5
Rowe, J. W., and Kahn, R. L. (1997). Successful Aging1. The Gerontologist 37, 433–440. doi:10.1093/geront/37.4.433
Sápi, M., Domján, A., Fehérné Kiss, A., and Pintér, S. (2019). Is Kinect Training Superior to Conventional Balance Training for Healthy Older Adults to Improve Postural Control? Games Health J., 8(1), 41–48. doi:10.1089/g4h.2018.0027
Sauzéon, H., N’Kaoua, B., Arvind Pala, P., Taillade, M., and Guitton, P. (2016). Age and Active Navigation Effects on Episodic Memory: A Virtual Reality Study. Br. J. Psychol. 107 (1), 72–94. doi:10.1111/bjop.12123
Smaerup, M., Laessoe, U., Grönvall, E., Henriksen, J. J., and Damsgaard, E. M. (2016). The Use of Computer-Assisted home Exercises to Preserve Physical Function after a Vestibular Rehabilitation Program: a Randomized Controlled Study. Rehabil. Res. Pract., 2016:7026317, doi:10.1155/2016/7026317
Stadler, S., Cornet, H., Theoto, T. N., and Frenkler, F. (2019). “A Tool, Not a Toy: Using Virtual Reality to Evaluate the Communication between Autonomous Vehicles and Pedestrians,” in Augmented Reality and Virtual Reality (Cham: Springer), 203–216. doi:10.1007/978-3-030-06246-0_15,
Studenski, S., Perera, S., Hile, E., Keller, V., Spadola-Bogard, J., and Garcia, J. (2010). Interactive Video Dance Games for Healthy Older Adults. J. Nutr. Health Aging 14 (10), 850–852. doi:10.1007/s12603-010-0119-5
Sun, R., Aldunate, R. G., Paramathayalan, V. R., Ratnam, R., Jain, S., Morrow, D. G., et al. (2019). Preliminary Evaluation of a Self-Guided Fall Risk Assessment Tool for Older Adults. Arch. Gerontol. Geriatr., 82, 94–99. doi:10.1016/j.archger.2019.01.022
Sweller, J. (1980). Transfer Effects in a Problem Solving Context. Quart. J. Exp. Pyschol. 32, 233–239. doi:10.1080/14640748008401159
Tarnanas, I., Papagiannopoulos, S., Kazis, D., Wiederhold, M., Widerhold, B., and Tsolaki, M. (2015). Reliability of a Novel Serious Game Using Dual-Task Gait Profiles to Early Characterize aMCI. Front. Aging Neurosci. 7 (50), 1–15. doi:10.3389/fnagi.2015.00050
Tennyson, R. D., and Breuer, K. (1997). Psychological Foundations for Instructional Design Theory. In Instructional Design: International Perspectives I: Volume I: Theory, Research, and Models:volume Ii: Solving Instructional Design Problems. Editors R. D. Tennyson, F. Schott, N. M. Seel, & S. Dijkstra (Routledge). Available at: https://books.google.ie/books?hl=en&lr=&id=9dg6q9FO5H0C&oi=fnd&pg=PA113&ots=--htjWy83E&sig=MLn-G-31dDwcbFwuPxjsUdHSPlA&redir_esc=y#v=onepage&q&f=false
Tricco, A. C., Lillie, E., Zarin, W., O’Brien, K. K., Colquhoun, H., Levac, D., et al. (2018). PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 169 (7), 467–473. doi:10.7326/M18-0850
Tsuda, K., Sudo, K., Goto, G., Takai, M., Itokawa, T., Isshiki, T., et al. (2016). A Feasibility Study of Virtual Reality Exercise in Elderly Patients with Hematologic Malignancies Receiving Chemotherapy. Intern. Med., 55(4), 347–352. doi:10.2169/internalmedicine.55.5275
Vallejo, V., Tarnanas, I., Yamaguchi, T., Tsukagoshi, T., Yasuda, R., Müri, R., et al. (2014). Usability assessment of natural user interfaces during serious games: Adjustments for dementia intervention. Virtual Reality, 8. http://www.icdvrat.reading.ac.uk/2014/papers/ICDVRAT2014_S01N3_Vallejo_etal.pdf.
Velez, J. A., and Hanus, M. D. (2016). Self-affirmation Theory and Performance Feedback: When Scoring High Makes You Feel Low. Cyberpsychology, Behav. Soc. Networking 19 (12), 721–726. doi:10.1089/cyber.2016.0144
Vygotsky, L. S. (1978). Mind in Society: Development of Higher Psychological Processes. Harvard University Press. doi:10.2307/j.ctvjf9vz4
Wiederhold, B. K. (2020). How Virtual Reality Is Changing the Reality of Aging. Cyberpsychology, Behav. Soc. Networking 23 (3). doi:10.1089/cyber.2020.29176.bkw
Wiederhold, B. K. (2016). Lessons Learned as We Begin the Third Decade of Virtual Reality. Cyberpsychology, Behav. Soc. Networking 19 (10), 577–578. doi:10.1089/cyber.2016.29052.bkw
Wiederhold, B. K., and Riva, F. (2012). Positive Technology Supports Shift to Preventive, Integrative Health. Cyberpsychology, Behav. Soc. Networking 15 (2), 67–68. doi:10.1089/cyber.2011.1533
Williams, B., Doherty, N. L., Bender, A., Mattox, H., and Tibbs, J. R. (2011). The Effect of Nintendo Wii on Balance: A Pilot Study Supporting the Use of the Wii in Occupational Therapy for the Well Elderly. Occup. Ther. Health Care, 25 (2-3), 131–139. doi:10.3109/07380577.2011.560627
Yeh, T. M., Pai, F. Y., and Jeng, M. Y. (2019). The Factors Affecting Older Adults’ Intention toward Ongoing Participation in Virtual Reality Leisure Activities. Int. J. Environ. Res. Public Health 16 (3), 333. doi:10.3390/ijerph16030333
Yu-Leung, N., Flora, M., Frederick, H., Patrick, I., and King-Wa, F. (2019). Effectiveness of Virtual and Augmented Reality-Enhanced Exercise on Physical Activity, Psychological Outcomes, and Physical Performance: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Comput. Hum. Behav., 99, 278–291. doi:10.1016/j.chb.2019.05.026
Zajonc, R. B. (1965). Social Facilitation. Science 149, 269–274. https://www.jstor.org/stable/1715944
Keywords: virtual reality, augmented reality, older adults, physical/mental health, scoping review, psychology
Citation: Carroll J, Hopper L, Farrelly AM, Lombard-Vance R, Bamidis PD and Konstantinidis EI (2021) A Scoping Review of Augmented/Virtual Reality Health and Wellbeing Interventions for Older Adults: Redefining Immersive Virtual Reality. Front. Virtual Real. 2:655338. doi: 10.3389/frvir.2021.655338
Received: 18 January 2021; Accepted: 07 May 2021;
Published: 02 June 2021.
Edited by:
John Naslund, Harvard Medical School, United StatesReviewed by:
Vangelis Lympouridis, University of Southern California, United StatesSavita G Bhakta, University of California, San Diego, United States
Copyright © 2021 Carroll, Hopper, Farrelly, Lombard-Vance, Bamidis and Konstantinidis. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Joanne Carroll, am9hbm5lLmNhcnJvbGxAZGN1Lmll
 Joanne Carroll
Joanne Carroll Louise Hopper
Louise Hopper Aaron Mark Farrelly
Aaron Mark Farrelly Richard Lombard-Vance2
Richard Lombard-Vance2 Panagiotis D. Bamidis
Panagiotis D. Bamidis Evdokimos I. Konstantinidis
Evdokimos I. Konstantinidis