- 1Menzies Health Institute Queensland, Griffith University, Gold Coast, QLD, Australia
- 2School of Allied Health Sciences, Griffith University, Gold Coast, QLD, Australia
- 3Wearable Computer Lab, Australian Centre for Interactive and Virtual Environments, University of South Australia, Adelaide, SA, Australia
- 4La Trobe Sport and Exercise Medicine Centre, School of Allied Health, College of Science, Health and Engineering, La Trobe University, Melbourne, VIC, Australia
- 5Amsterdam Movement Sciences, Faculty of Behavioural and Movement Sciences, Vrije Universiteit Amsterdam, Amsterdam, Netherlands
Background: Virtual reality (VR) allows people to embody avatars that are different from themselves in appearance and ability. These experiences provide opportunities to challenge bodily perceptions. We devised a novel VR Body Image Training (VR-BIT) approach to target self-perceptions and pain in people with persistent pain.
Methods: A 45-year old male with a 5-year history of disabling chronic low back pain participated in a 4-week VR-BIT intervention. Pain began following a fall from a first-floor deck. Pain was central and on the right side of his lower back, radiating to his right buttock and thigh. Pain was constant and varying at a 5/10 average intensity. The 4-week intervention consistent of three face-to-face sessions 1-week apart, followed by 1-week of in-home VR-BIT. During the first face-to-face session, the participant embodied three athletic avatars: a superhero (Incredible Hulk), a boxer, and a rock climber. Since the participant strongly identified with the boxer, only boxing experiences were subsequently used. Primary outcomes relating to body image (self-perceived strength, vulnerability, agility, and confidence with activity) and pain intensity were assessed using numerical rating scales (0–10 NRS). Disability, kinesiophobia, overall change, and self-efficacy were assessed as secondary outcomes. Outcomes were assessed during each face-to-face session, and at 1-week and 3-month follow-up.
Results: The participant reported a high degree of engagement. Positive changes were noted during and after VR for all body image and pain assessments. Improvements were retained at 3-months for body image ratings (mean change: 4.5/10 NRS) and average pain intensity (change: 2/10 NRS). Improvements in disability (45% improvement); self-efficacy (pre: 2/12; post: 10/12); and overall change (“Very much improved”) were noted at 3-month follow-up. No change in kinesiophobia was detected. No adverse advents were recorded.
Conclusion: The participant engaged strongly with the intervention and showed clinically meaningful changes in body image, pain, disability, and self-efficacy. Despite his long history of pain and rapid improvements, reported changes may be due to non-treatment effects. Nonetheless, VR-BIT clearly warrants further investigation as a potential addition to usual care.
Introduction
Body perception is remarkably plastic and susceptible to states where it is out-of-step with reality (Moseley et al., 2012). The flagship example is the rubber hand illusion, where an in-view rubber hand and an out-of-view real hand are simultaneously brushed, causing touch to be perceived as arising from the rubber hand that begins to feel like one's own hand (Botvinick and Cohen, 1998). The advent of virtual reality (VR) has made it possible to extend such illusions to the entire body, such as where a virtual body is presented in place of one's own body, resulting in the illusion of “body swapping,” commonly termed “embodiment” (Slater et al., 2010; Serino et al., 2016).
Distorted body perception is possible, because brain-held representations of the body are continuously updated in line with new information (Moseley et al., 2012). Modern theories explain this by positing that perception is the result of maximum-likelihood estimations, derived from available multisensory information and prior expectation, in a way that aims to minimize perceptual errors (Samad et al., 2015). As such, when sufficiently congruent multisensory information is presented on a virtual display, body perception is updated, and illusory body ownership results. In VR, an avatar is substituted for the participants real body from a first-person perspective. Illusory body ownership is then supported through visuomotor synchrony, where real-time motion tracking enables the virtual and real bodies to in tandem (Kokkinara and Slater, 2014).
Remarkably, the occupant of a virtual avatar can express new behaviors, perceptions, and attitudes reflective of the character of the avatar (Slater and Sanchez-Vives, 2014). For example, after flying above a virtual city as a superhero, participants are more likely to help an experimenter pick up a jar of “accidentally” spilled pens than if they flew in a virtual helicopter (Rosenberg et al., 2013). Participants have even been shown to perform better on cognitive tasks when embodying Einstein (Banakou et al., 2018). This close relationship between mind and (perceived) body has been described as embodied cognition (Costa et al., 2013).
Altered body perception has been associated with a range of clinical conditions. These include body dysmorphias (Kaplan et al., 2013; Gadsby, 2017), body integrity disorder (Giummarra et al., 2011), and distorted phantom limbs (Foell et al., 2014). Much interest has emerged in targeting misrepresentations of the body using multisensory illusions (Riva et al., 2019). For example, some studies have shown that participants with anorexia have more accurate body size estimations after embodying healthy-weight avatars (Keizer et al., 2016; Serino et al., 2017, 2019; Ziser et al., 2018).
Some chronic pain states may also be regarded as conditions of altered body perception—if symptoms persist in the absence of pathology (Moseley et al., 2012). This mismatch between symptoms (perceived body state) and actual bodily state may result from brain-held representations of the body that adapted to pain/injury but failed to normalize with healing. These adaptations may be expressed in conscious impressions of the body—referred to as body image. These conscious impressions may include body-related attitudes, emotions, and sensations including pain. Chronic low back pain (LBP) has been associated with body image-related impairments including negative body-related attitudes such as reduced physical efficacy (i.e., low levels of perceived strength and skill; Levenig et al., 2019), and impressions of the body as malfunctioning or at risk of (re)injury (Crombez et al., 2012; Levenig et al., 2019). In the perceptual domain, disrupted conscious impressions of the body may extend not only to pain, other perceptual phenomena such as stiffness (Stanton et al., 2017). Considering the view of pain as a protective response, it is conceivable that impressions of the body as vulnerable may enhance pain (Moseley, 2003). By this theory, targeting vulnerability-related aspects of body image may reduce pain.
A recent study asked two participants with LBP to view a live video feed of their own back modified in real-time to appear hyper-muscular (Nishigami et al., 2019). In one participant, a change in pain and perceived strength was induced (Nishigami et al., 2019). However, no follow-up was included, only one session was delivered, and the avatar was viewed from a third person perspective. In this paper, we present a case report where a participant with chronic LBP undertook a 4-week VR Body Image Training (VR-BIT) program, involving the embodiment of athletically enhanced avatars, with the goal of targeting negative self-perceptions and pain.
Case Description
A participant was identified through a local physiotherapy clinic and was selected on the basis of having moderate-to-severe chronic LBP pain of >6-months duration and the absence of red flags (Verhagen et al., 2016). The participant was a 45-year old male with a 5-year history of chronic LBP following a fall on to the side of a trailer from a first-floor deck while at work in the construction industry. No fracture was identified. Due to pain, the participant was unable to return to normal duties. Approximately 3 years ago, his LBP became progressively worse following an ankle injury that the participant reported significantly impaired walking ability and induced an asymmetrical limp. Over the last 2 years his pain has been relatively constant, with occasional episodes of lower back “spasms” resulting in emergency admissions. The participant reported that the pain was due to L4/5 damage and sciatic nerve impingement revealed on MRI reports. No dysthesias or neurological signs were present. Current aggravating factors included any physical activity, sitting, reaching up, and lying flat. Previous management had included a 3-month outpatient gym program in 2018 that resulted in improvements, but not resolution. Pain was primarily central and right sided lower back, with radiation to his right buttock into his mid-lateral thigh. Pain was described as constant and varying, with a 5/10 on average, and 9/10 at its worst. The participant was unable to work in physical jobs searching for alternative work. He was not engaging in concurrent rehabilitation, however had been managing symptoms by pacing activity levels over the last 2 years. The patient was not on analgesic medication at the time of the study.
Intervention Details
Overview
The participant undertook a 4-week intervention, involving three face-to-face VR sessions 1-week apart, followed by 1-week of in-home VR. Across the sessions, the participant embodied three different avatars: a superhero (Incredible Hulk), a boxer, and a rock climber. Primary outcomes relating to body image and pain intensity were assessed using a number of numerical rating scales (NRS) relating to self-perceived strength, vulnerability, agility, and confidence with activity and pain intensity. Secondary outcomes relating to disability, kinesiophobia, overall change, and self-efficacy were also assessed. Outcomes were assessed during each face-to-face session, and at 1-week and 3-month follow-up. The project was approved by Griffith University HREC (2019/763).
Participant Preparation
The participant received verbal information and provided written consent. A short video was used to explain the treatment intention (https://youtu.be/YnSs3SxwnYg). A detailed explanation about pain was avoided, in order to focus the study on VR, rather than education.
Hardware
For the face-to-face sessions, an Oculus Rift S head mounted display with connected Touch controllers (Oculus, Facebook Technologies, LCC, Menlo Park, USA) and Windows computer (Alienware 17 R4, with NVIDIA GTX1080 GPU, Dell Technologies Inc., Round Rock, Texas, USA). For the in-home sessions, an Oculus Quest was used because of its portability.
Software Applications
Three applications were used. All applications were available on the Oculus store for less than USD$50/46€ each: oculus.com/experiences/rift/. The applications allowed the participant to embody a boxer (Creed: Rise to Glory), a superhero (Incredible Hulk, Avengers Powers Unite), and a rock climber (The Climb) (see Figure 1). The hardware and software afforded six degrees of freedom for head and hand movement. Full-body tracking was not available with these applications, however CREED and The Avengers included full body avatars, that were animated in response to head and hand tracking and “best guess” algorithms. This approach resulted in a high degree of visuomotor congruence for the upper body. This was limited for the lower limbs, however the interactions primarily involved the upper body.
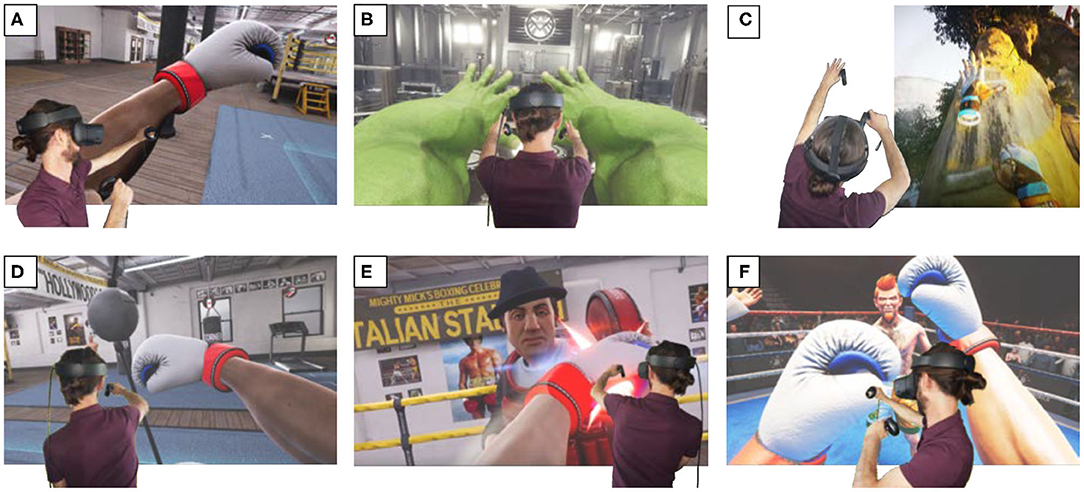
Figure 1. A screen shot from each of the VR applications. (A) “Creed: Rise to Glory”; (B) “Avengers Powers Unite”; (C) “The Climb”; (D–F) “Creed: Rise to Glory”.
Face-to-Face Sessions
The intervention was facilitated by a physiotherapist experienced in managing people with chronic pain. All three face-to-face sessions were completed in standing and involved ~15-min of time in VR. During the first face-to-face session, the participant engaged with the three applications for 5-min each. The physiotherapist guided embodiment of the avatars, by instructing the participant to observe and move their virtual body. The subsequent experiences depended on the application used. For the boxing application (Figure 1A) the participant was instructed to make muscle poses, throw air punches, and punch a virtual punching bag. In Avengers Powers Unite (Figure 1B), the participant became the Incredible Hulk. Here, the participant was again instructed to throw air punches, and adopt various muscle poses, all with their attention fixed on their newly adopted musculature. In The Climb (Figure 1C), the participant the participant scaled a virtual cliff, while being instructed to notice their strength and effortlessness.
During the initial face-to-face session, the participant mentioned that he had prior experience with boxing. As a result of its relatability, subsequent face-to-face sessions focussed exclusively on this application. Across these sessions, the intervention was altered to simulate increasing strength, capability, agility, and physical resilience. In the second session, two new boxing experiences were introduced. In the first, a suspended punching bag was punched in various directions in order to strike specific targets (Figure 1D). In the second, the participant spared with a virtual coach (Figure 1E). In the third session, these experiences were repeated, then extended to a virtual boxing match (Figure 1F).
In-Home Sessions
For the in-home sessions, the participant was given autonomy to explore the boxing application. Prior to taking the device home, the participant rehearsed set-up of the physical environment, creating a virtual safety boundary, and navigating the interface. The participant was instructed to complete 15-min of training on five separate days during the week of in-home VR-BIT.
Outcome Assessments
Baseline Assessments
Prior to the intervention, a patient interview was conducted to gather demographic data (such as age, sex, and occupation) and clinical data (such as location of pain and history of injury/pain). The participant then completed a digital questionnaire (LimeSurvey online survey tool; Schmitz, 2012), to gather baseline outcome data.
Primary Outcomes
Primary outcomes relating to body image and pain were assessed using six 0–10 numerical rating scales (NRS). The body image scales assessed four dimensions of body image. For each body image scale, the participant was asked “Using the following scale, rate how your body feels (not how it might actually be).” The four rating scales related to self-perceived strength, vulnerability, agility and confidence with activity (see body image scales in Appendix 1). Current pain and average pain over the past week were measured using a NRS using the anchors: 0 = no pain, and 10 = the worst imaginable pain.
Secondary Outcomes
Secondary outcomes relating to disability, kinesiophobia, overall change, and self-efficacy were also assessed using recommended questionnaires (Sleijser-Koehorst et al., 2019). Disability was quantified using the Roland-Morris Disability Questionnaire (Stratford et al., 1996), fear of movement was measured using the Tampa Scale of Kinesiophobia (TSK-11) (Vlaeyen J. et al., 1995), and Self-efficacy was measured using the Pain Self-efficacy Questionnaire (PSEQ-2) (Nicholas et al., 2015). Overall perceived change was measured using the Patient Global Impression of Change scale (PGIC) (Fischer et al., 1999). The PGIC is a seven-point scale with descriptors anchored to each point (1: Very much improved, 2: Much improved; 3: Minimally improved; 4: No change; 5: Minimally worse; 6: Much worse; 7: Very much worse). The participant selected the response (in the LimeSurvey questionnaire) which best matched his status relative to the start of the study.
Assessment Timing
Current pain and body image assessments were acquired at baseline, during VR-BIT, and at the end of each face-to-face session, and at 1-week and 3-month following the conclusion of the week of in-home VR sessions. Kinesiophobia, self-efficacy, average pain over the last week and disability were assessed at the beginning of each face-to-face session, and at 1-week and 3-months follow-up. Overall change was assessed at the beginning of face-to-face sessions two and three, and at 1-week and 3-months follow-up. The body image and pain ratings acquired during the VR experiences were given verbally, otherwise outcomes were acquired through LimeSurvey.
Results
Across the 4-week intervention, the participant attended the three face-to-face sessions 1-week apart, and completed six sessions of in-home VR-BIT. Thus, rather than the instructed five sessions, the participant undertook training on an additional day by his own volition. In each face-to-face session, the participant spent ~15-min in VR. During the in-home sessions, the participant reported completing 15 to 25-min per day. The sessions were well-tolerated, and no adverse advents or motion sickness were experienced for face-to-face or in-home sessions. The participant reported a high degree of engagement and enjoyment with the therapy, and reported the experience of being able to move more freely in VR. There was no change to analgesic medication use across the experiment.
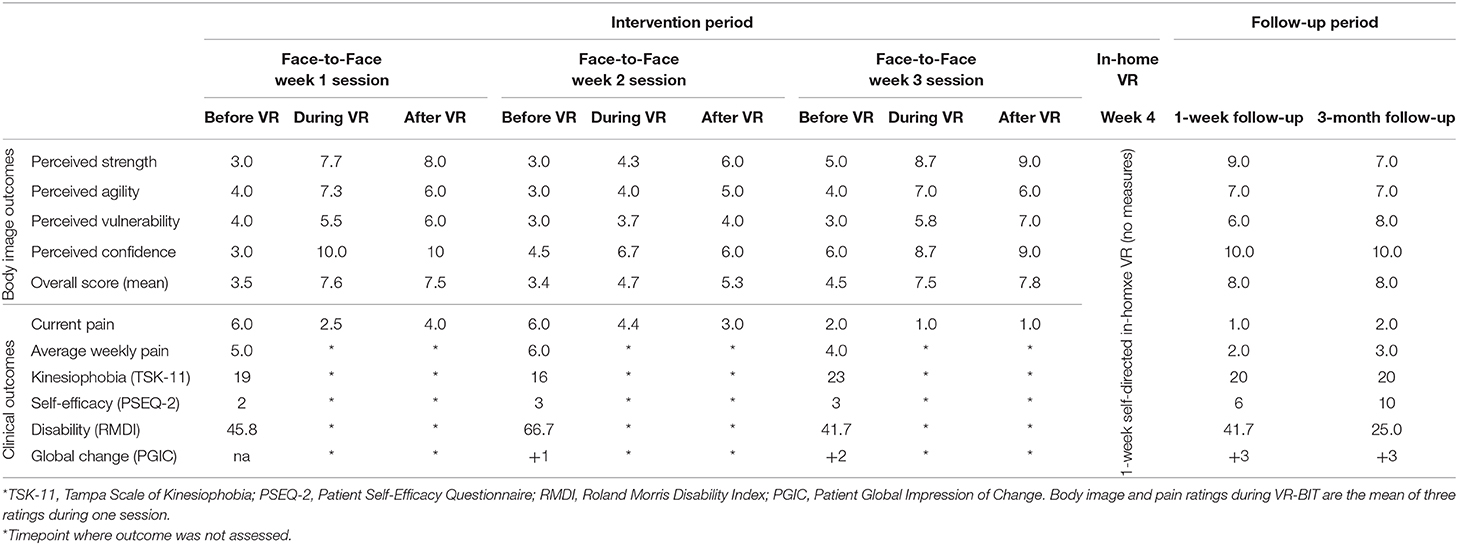
Overall, the participant improved in body image ratings (from 3.5/10.0 to 8.0/10.0) and showed improvement across each of the associated dimensions (Table 1 and Figure 2). Average weekly pain improved from 5/10 at baseline, to 2/10 at 1-week follow-up, and 3/10 at 3-month follow-up, thus exceeding the minimally important difference of 2/10 or 30% (Farrar et al., 2001; Table 1 and Figure 3). Using the PGIC scale, the participant indicated that he was much improved by the third face-to-face session, and very much improved at 1-week and 3-month follow-up. Positive changes in self-efficacy were apparent at 1-week and 3-month follow-up, however no meaningful change was detected in kinesiophobia (Table 1). While disability was not improved at 1-week follow-up, a 45% reduction in disability score became apparent at 3-month follow-up (Table 1). Changes in body image appeared to parallel changes in current pain (Pearson's r = −0.78, p = 0.005) and average pain over the last week (Pearson's r = −0.93, p = 0.024; Figure 3).
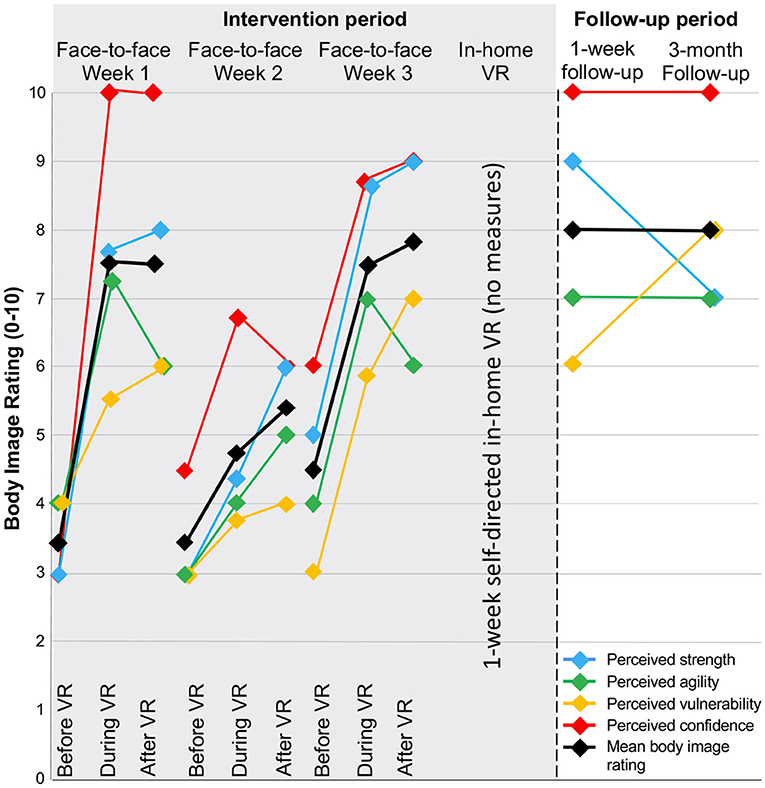
Figure 2. Body image ratings assessed before, during, and immediately after each weekly face-to-face session, at 1-week following the in-home VR-BIT training, and at 3-month follow-up. Lines represent each of the assessed components of body image, and the average across dimensions.
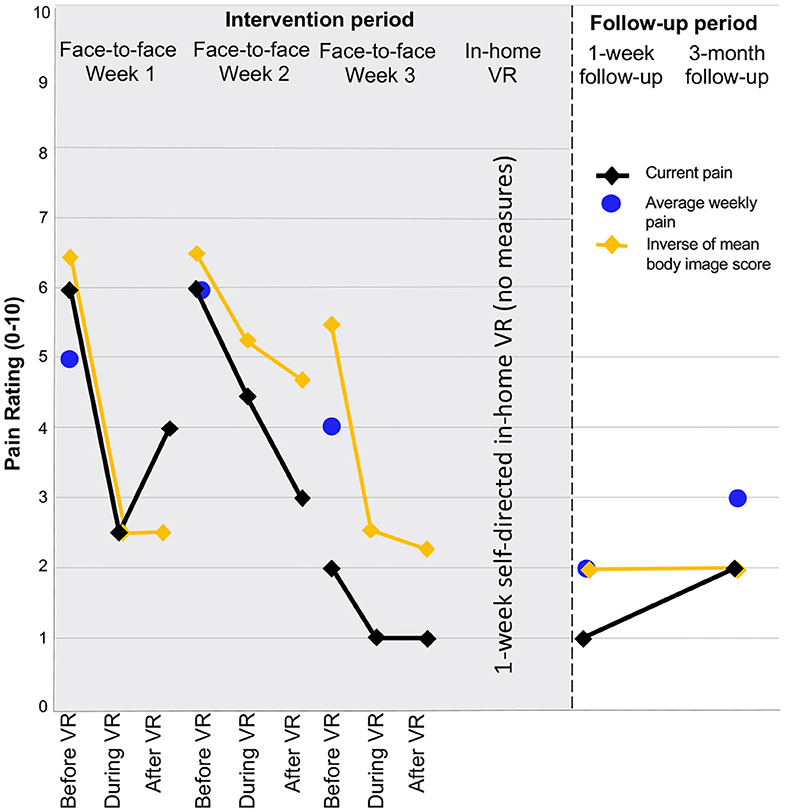
Figure 3. Current pain intensity ratings assessed before, during, and after VR-BIT at each face-to-face session, and at 1-week and 3-month follow-up. Average pain ratings “over the past week” are shown as discrete points. The overall body image rating is also shown but inversed in order to easily appreciate correlations between body image and pain.
Discussion
Embodying athletic avatars in VR to assist in overcoming persistent body image impairments and pain following injury is an intriguing possibility. With this prospect in mind, we explored a novel application of VR in a participant with chronic LBP. The therapy aimed to induce the experience of a strong, capable body, that would conflict with negative self-perceptions—such a sense of having a vulnerable body. Positive gains were made in body image (perceptions of strength, vulnerability, agility, and confidence with movement) and pain. These gains were noted during VR, after VR, and at 1-week and 3-month follow-ups. Positive changes were also seen in some secondary outcomes, including self-efficacy and overall change at 1-week and 3-month follow-up. No meaningful change was detected in kinesiophobia and improvements in disability only appeared at 3-month follow-up.
To date, there are no cohort studies or clinical trials investigating a treatment similar to that outlined here in people with persistent pain. Although others have attempted to use embodiment approaches to treat pain (Matamala-Gomez et al., 2019a,b) only one conceptually similar, single-session, case series of two-participants has been reported (Nishigami et al., 2019). During their study, one participant experienced changes in pain and perceived strength while viewing a manipulated live-video of their own back appearing hyper-muscular (Nishigami et al., 2019). In contrast to our study, the experience was a third-person perspective rather than first-person, and no follow-up measures were taken after the experience. The current case report is the first documented intervention for chronic LBP based on the embodiment of athletic avatars across multiple sessions, with sufficient follow-up, and using a first-person embodiment approach.
Case studies cannot support efficacy or imply causality. Nonetheless, the participant showed gains that were clinically meaningful. All body image ratings (perceived strength, agility, vulnerability, and confidence with activity) showed gains of 3/10–7/10 across the study. Reductions in “average pain over the last week” of 40% was noted at 3-month follow-up and overall improvement was rated as “Very much improved.” Moreover, self-efficacy was reported at “2” at the beginning of the study (<5 = low confidence with physical functioning in the presence of pain) at “6” at 1-week and “10” at 3-month follow-up (>8 reflects desirable self-efficacy) (Nicholas et al., 2015). While disability did not show improvement at initial follow-up, a 44% improvement in the RMDQ was apparent at 3-month follow-up. While these improvements may be due to non-specific effects or natural history, other cognition targeting treatments have also demonstrated a delayed effect on function. For example, change in pain knowledge following a pain education intervention is associated with late (6 to 12-month) improvements in function in people with chronic pain (Lee et al., 2016).
Potential Mechanisms
Disruption of body image has been observed in people with chronic pain (Moseley and Flor, 2012; Moseley et al., 2012; Levenig et al., 2016; Wand et al., 2016). These disruptions include changes in perceived body dimensions (Wand et al., 2016) and perceptions of vulnerability and fear of (re)injury (Vlaeyen J.W. et al., 1995; Levenig et al., 2016). Authors have highlighted the possibility that addressing body image disruptions may be therapeutic (Moseley, 2004; Moseley and Flor, 2012; Riva et al., 2017, 2019). For example, anorexia may be the outcome of a failure to update old memories of the body (Riva et al., 2019). Thus, following weight loss, the experience of, and attitudes toward, his/her body may persist following (Riva et al., 2019). If a similar failure to update body representations persists following injury, then it follows that injury-related behaviors and perceptions may persist. VR may allow the (mis)representation of the body to be disrupted and updated through illusory ownership of a virtual body with vastly different characteristics in domains such as shape, size, and capability. In this way, a limited amount of time in VR, could mediate sustained improvements. Sustained improvements might also depend on post-VR reengagement with movement and activity reinforcing the updated body image. In this case, this could be an increase in activity without re-injury or significant pain.
Researchers also suggest that having experiences from another perspective/body may result in implicit learning (Slater, 2017). For example, becoming a body that reflects a different ethnicity reduces implicit racial bias (Hasler et al., 2017) and alters in-group behaviors (Banakou et al., 2016). In a similar way, experiencing an athletic avatar may result in implicit changes to self-perception in domains such as perceived strength and resilience.
Limitations and Future Directions
Despite the long history of pain without resolution and relatively quick improvements, reported changes may be due to natural history, regression to the mean, and non-specific treatment effects. Nonetheless, this case report outlined a new potential therapeutic approach and highlighted a range of potential future directions that we hope will catalyse further research. As for any novel intervention, there was no existing support for a specific treatment dosage or timing. We note however, that the relatively small dosage of the intervention was both well-tolerated and did not appear to preclude benefit. Another limitation was the absence of whole-body-tracking which may have improved embodiment by virtue of greater visuomotor congruence. A further limitation of the study was its inability to differentiate the effects of VR, from the effects of movement and education. That is, because the intervention necessitated movement, we cannot rule out its effects; although a greater dose would likely be needed to induce meaningful physiological effects. Moreover, the intervention required a limited explanation of pain and the brain, which may have effected a change in pain-related cognitions and body image independent of VR. Finally, we note that our primary outcomes were custom likert scales that have not been formally validated. However, likert scales are widely used in psychology and social sciences and providing they have over four response categories are generally found to be reliable and valid (Lozano et al., 2008).
Among the considerations for future research, it is worth noting that the relatability of the boxing avatar may have been a factor in success. A further direction for future research is to identify clinical indicators that might predict treatment success or highlight barriers. For example, the effectiveness of the intervention may depend on body image impairments being part of the clinical picture. Future studies might consider the intervention as part of a broader biopsychosocial package of care.
Conclusions
Embodying athletic avatars in VR to assist in overcoming persistent body image impairments and pain following injury is an intriguing possibility. This study outlined a novel approach to treating chronic LBP, using relatively affordable, off-the-shelf technology. The intervention was well-received, and positive improvements were seen in body image and pain at 1-week follow-up. At 3-month follow-up, gains were retained and an apparent improvement in disability also emerged. Future research controlling for time and non-specific effects will be needed in order to investigate efficacy.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author Contributions
DH and MC developed the study concept. DH, MC, ER, NO, and RS contributed to design, data interpretation, and write-up. DH collected the data. All authors contributed to the article and approved the submitted version.
Funding
This project was supported by a Hopkins Centre seeding grant. DH was supported by an Early Career Research Fellowship from the National Health and Medical Research Council of Australia (APP1142929). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frvir.2020.00013/full#supplementary-material
References
Banakou, D., Hanumanthu, P. D., and Slater, M. (2016). Virtual embodiment of white people in a black virtual body leads to a sustained reduction in their implicit racial bias. Front. Hum. Neurosci. 10:601. doi: 10.3389/fnhum.2016.00601
Banakou, D., Kishore, S., and Slater, M. (2018). Virtually being Einstein results in an improvement in cognitive task performance and a decrease in age bias. Front. Psychol. 9:917. doi: 10.3389/fpsyg.2018.00917
Botvinick, M., and Cohen, J. (1998). Rubber hands ‘feel’touch that eyes see. Nature 391, 756–756. doi: 10.1038/35784
Costa, M. R., Kim, S. Y., and Biocca, F. (2013). “Embodiment and embodied cognition,” Paper Presented at the International Conference on Virtual, Augmented and Mixed Reality (Las Vegas, NV). doi: 10.1007/978-3-642-39405-8_37
Crombez, G., Eccleston, C., Van Damme, S., Vlaeyen, J. W., and Karoly, P. (2012). Fear-avoidance model of chronic pain: the next generation. Clin. J. Pain 28, 475–483. doi: 10.1097/AJP.0b013e3182385392
Farrar, J. T., Young, J. P. Jr., LaMoreaux, L., Werth, J. L., and Poole, R. M. (2001). Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain 94, 149–158. doi: 10.1016/S0304-3959(01)00349-9
Fischer, D., Stewart, A. L., Bloch, D. A., Lorig, K., Laurent, D., and Holman, H. (1999). Capturing the patient's view of change as a clinical outcome measure. JAMA 282, 1157–1162. doi: 10.1001/jama.282.12.1157
Foell, J., Bekrater-Bodmann, R., Diers, M., and Flor, H. (2014). Mirror therapy for phantom limb pain: brain changes and the role of body representation. Eur. J. Pain 18, 729–739. doi: 10.1002/j.1532-2149.2013.00433.x
Gadsby, S. (2017). Distorted body representations in anorexia nervosa. Conscious. Cogn. 51, 17–33. doi: 10.1016/j.concog.2017.02.015
Giummarra, M. J., Bradshaw, J. L., Nicholls, M. E., Hilti, L. M., and Brugger, P. (2011). Body integrity identity disorder: deranged body processing, right fronto-parietal dysfunction, and phenomenological experience of body incongruity. Neuropsychol. Rev. 21, 320–333. doi: 10.1007/s11065-011-9184-8
Hasler, B. S., Spanlang, B., and Slater, M. (2017). Virtual race transformation reverses racial in-group bias. PLoS ONE 12:e0174965. doi: 10.1371/journal.pone.0174965
Kaplan, R. A., Rossell, S. L., Enticott, P. G., and Castle, D. J. (2013). Own-body perception in body dysmorphic disorder. Cogn. Neuropsychiatry 18, 594–614. doi: 10.1080/13546805.2012.758878
Keizer, A., van Elburg, A., Helms, R., and Dijkerman, H. C. (2016). A virtual reality full body illusion improves body image disturbance in anorexia nervosa. PLoS ONE 11:e0163921. doi: 10.1371/journal.pone.0163921
Kokkinara, E., and Slater, M. (2014). Measuring the effects through time of the influence of visuomotor and visuotactile synchronous stimulation on a virtual body ownership illusion. Perception 43, 43–58. doi: 10.1068/p7545
Lee, H., McAuley, J. H., Hübscher, M., Kamper, S. J., Traeger, A. C., and Moseley, G. L. (2016). Does changing pain-related knowledge reduce pain and improve function through changes in catastrophizing? Pain 157, 922–930. doi: 10.1097/j.pain.0000000000000472
Levenig, C., Hasenbring, M., Kleinert, J., and Kellmann, M. (2016). Body image and low back pain. Schmerz 30, 437–443. doi: 10.1007/s00482-016-0122-9
Levenig, C. G., Kellmann, M., Kleinert, J., Belz, J., Hesselmann, T., and Hasenbring, M. I. (2019). Body image is more negative in patients with chronic low back pain than in patients with subacute low back pain and healthy controls. Scand. J. Pain 19, 147–156. doi: 10.1515/sjpain-2018-0104
Lozano, L. M., García-Cueto, E., and Muñiz, J. (2008). Effect of the number of response categories on the reliability and validity of rating scales. Methodology 4, 73–79 doi: 10.1027/1614-2241.4.2.73
Matamala-Gomez, M., Donegan, T., Bottiroli, S., Sandrini, G., Sanchez-Vives, M. V., and Tassorelli, C. (2019a). Immersive virtual reality and virtual embodiment for pain relief. Front. Hum. Neurosci. 13:279. doi: 10.3389/fnhum.2019.00279
Matamala-Gomez, M., Gonzalez, A. M. D., Slater, M., and Sanchez-Vives, M. V. (2019b). Decreasing pain ratings in chronic arm pain through changing a virtual body: different strategies for different pain types. J. Pain 20, 685–697. doi: 10.1016/j.jpain.2018.12.001
Moseley, G. (2003). A pain neuromatrix approach to patients with chronic pain. Man. Ther. 8, 130–140. doi: 10.1016/S1356-689X(03)00051-1
Moseley, G. L. (2004). Evidence for a direct relationship between cognitive and physical change during an education intervention in people with chronic low back pain. Eur. J. Pain 8, 39–45. doi: 10.1016/S1090-3801(03)00063-6
Moseley, G. L., and Flor, H. (2012). Targeting cortical representations in the treatment of chronic pain a review. Neurorehabil. Neural Repair 26, 646–652. doi: 10.1177/1545968311433209
Moseley, G. L., Gallace, A., and Spence, C. (2012). Bodily illusions in health and disease: physiological and clinical perspectives and the concept of a cortical ‘body matrix’. Neurosci. Biobehav. Rev. 36, 34–46. doi: 10.1016/j.neubiorev.2011.03.013
Nicholas, M. K., McGuire, B. E., and Asghari, A. (2015). A 2-item short form of the pain self-efficacy questionnaire: development and psychometric evaluation of PSEQ-2. J. Pain 16, 153–163. doi: 10.1016/j.jpain.2014.11.002
Nishigami, T., Wand, B. M., Newport, R., Ratcliffe, N., Themelis, K., Moen, D., et al. (2019). Embodying the illusion of a strong, fit back in people with chronic low back pain. A pilot proof-of-concept study. Musculosk. Sci. Pract. 39, 178–183. doi: 10.1016/j.msksp.2018.07.002
Riva, G., Wiederhold, B. K., and Gaggioli, A. (2017). A healthy mind in a healthy virtual body: the future of virtual reality in health care. Ann. Rev. Cyberther. Telemed. 15, 3–7.
Riva, G., Wiederhold, B. K., and Mantovani, F. (2019). Neuroscience of virtual reality: from virtual exposure to embodied medicine. Cyberpsychol. Behav. Soc. Netw. 22, 82–96. doi: 10.1089/cyber.2017.29099.gri
Rosenberg, R. S., Baughman, S. L., and Bailenson, J. N. (2013). Virtual superheroes: Using superpowers in virtual reality to encourage prosocial behavior. PLoS ONE 8:e55003. doi: 10.1371/journal.pone.0055003
Samad, M., Chung, A. J., and Shams, L. (2015). Perception of body ownership is driven by Bayesian sensory inference. PLoS ONE 10:e0117178. doi: 10.1371/journal.pone.0117178
Schmitz, C. (2012). LimeSurvey: An Open Source Survey Tool. Hamburg: LimeSurvey Project. Retrieved from: http://www.limesurvey.org (accessed January 10, 2020).
Serino, S., Chirico, A., Pedroli, E., Polli, N., Cacciatore, C., and Riva, G. (2017). Two-phases innovative treatment for anorexia nervosa: the potential of virtual reality body-swap. Annu. Rev. Cyberther. Telemed. 15, 111–115. Available online at: https://www.scimagojr.com/journalsearch.php?q=19700174668&tip=sid&clean=0
Serino, S., Pedroli, E., Keizer, A., Triberti, S., Dakanalis, A., Pallavicini, F., et al. (2016). Virtual reality body swapping: a tool for modifying the allocentric memory of the body. Cyberpsychol. Behav. Soc. Netw. 19, 127–133. doi: 10.1089/cyber.2015.0229
Serino, S., Polli, N., and Riva, G. (2019). From avatars to body swapping: the use of virtual reality for assessing and treating body-size distortion in individuals with anorexia. J. Clin. Psychol. 75, 313–322. doi: 10.1002/jclp.22724
Slater, M. (2017). “Implicit learning through embodiment in immersive virtual reality,” in Virtual, Augmented, and Mixed Realities in Education (Singapore: Springer), 19–33. doi: 10.1007/978-981-10-5490-7_2
Slater, M., and Sanchez-Vives, M. V. (2014). Transcending the self in immersive virtual reality. Computer 47, 24–30. doi: 10.1109/MC.2014.198
Slater, M., Spanlang, B., Sanchez-Vives, M. V., and Blanke, O. (2010). First person experience of body transfer in virtual reality. PLoS ONE 5:e10564. doi: 10.1371/journal.pone.0010564
Sleijser-Koehorst, M. L., Bijker, L., Cuijpers, P., Scholten-Peeters, G. G., and Coppieters, M. W. (2019). Preferred self-administered questionnaires to assess fear of movement, coping, self-efficacy, and catastrophizing in patients with musculoskeletal pain—A modified Delphi study. Pain 160, 600–606. doi: 10.1097/j.pain.0000000000001441
Stanton, T. R., Moseley, G. L., Wong, A. Y., and Kawchuk, G. N. (2017). Feeling stiffness in the back: a protective perceptual inference in chronic back pain. Sci. Rep. 7:9681. doi: 10.1038/s41598-017-09429-1
Stratford, P. W., Binkley, J., Solomon, P., Finch, E., Gill, C., and Moreland, J. (1996). Defining the minimum level of detectable change for the Roland-Morris questionnaire. Phys. Ther. 76, 359–365. doi: 10.1093/ptj/76.4.359
Verhagen, A. P., Downie, A., Popal, N., Maher, C., and Koes, B. W. (2016). Red flags presented in current low back pain guidelines: a review. Eur. Spine J. 25, 2788–2802. doi: 10.1007/s00586-016-4684-0
Vlaeyen, J., Kole-Snijders, A. M., Boeren, R. G., and Van Eek, H. (1995). Fear of movement/(re) injury in chronic low back pain and its relation to behavioral performance. Pain 62, 363–372. doi: 10.1016/0304-3959(94)00279-N
Vlaeyen, J. W., Kole-Snijders, A. M., Rotteveel, A. M., Ruesink, R., and Heuts, P. H. (1995). The role of fear of movement/(re) injury in pain disability. J. Occup. Rehabil. 5, 235–252. doi: 10.1007/BF02109988
Wand, B. M., Catley, M. J., Rabey, M. I., O'Sullivan, P. B., O'connell, N. E., and Smith, A. J. (2016). Disrupted self-perception in people with chronic low back pain. Further evaluation of the fremantle back awareness questionnaire. J. Pain 17, 1001–1012. doi: 10.1016/j.jpain.2016.06.003
Keywords: virtual reality, low back pain, chronic pain, embodiment, body image, disability, rehabilitation, body illusions
Citation: Harvie DS, Rio E, Smith RT, Olthof N and Coppieters MW (2020) Virtual Reality Body Image Training for Chronic Low Back Pain: A Single Case Report. Front. Virtual Real. 1:13. doi: 10.3389/frvir.2020.00013
Received: 20 May 2020; Accepted: 04 August 2020;
Published: 14 September 2020.
Edited by:
Belinda Lange, Flinders University, AustraliaReviewed by:
Ali Fardinpour, Wise Realities Institute for Healthcare Emerging Technologies Research, AustraliaHadi Hosseini, Stanford University, United States
Copyright © 2020 Harvie, Rio, Smith, Olthof and Coppieters. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Daniel S. Harvie, ZC5oYXJ2aWVAZ3JpZmZpdGguZWR1LmF1
 Daniel S. Harvie
Daniel S. Harvie Ebonie Rio4
Ebonie Rio4 Ross T. Smith
Ross T. Smith Michel W. Coppieters
Michel W. Coppieters