- 1Department of Surgery, Division of Urology, Duke University Health System, Durham, NC, United States
- 2Department of Urology, Oregon Urology Institute, Springfield, OR, United States
Introduction and review of history
Over the course of urological history, there have been many different surgical techniques to treat urethral stricture disease. The basis of treatment has focused on procedures that offered a durable outcome, limited morbidity, and limited sexual side effects. Early management of urethral stricture disease revolved around the use of local flaps of penile and scrotal skin, with rates of failure around 20%–30% (1). A need for more durable outcomes resulted in an exploration of free graft substitution. Iterations included meshed split-thickness skin grafts (STSGs), with success rates of 80%, which require multiple stages and have morbidity associated with harvest (2). There is also bladder mucosa, with rates of failure around 12% at 28 months and morbidity associated with harvesting the graft with open surgery (3). The first described use of buccal mucosal grafts (BMGs) for urethral reconstruction was in the early 19th century by Sapezhko, and the buccal mucosa was characterized as the ideal graft tissue because of its robust epithelium, resistance to infection, and ease of transfer (1, 4). Interestingly, the use of free oral grafts for urethral stricture disease predated the use of STSGs and bladder mucosa but fell out of favor. The use of free oral grafts dates back to the early 1890s (4). It was not revived until 1941 when Humby first used BMGs for urethral reconstructions (5). Fast forward to 1996, and Morey and McAninch described a two-team approach and the use of BMGs for urethroplasty using a ventral onlay approach (6). In 1998, Barbagli et al. popularized a dorsal onlay approach using BMGs for bulbar urethral strictures, and in 2009 Kulkarni et al. described a unilateral dorsal onlay using BMGs (7, 8). At this present time, the use of buccal mucosa is the standard graft for substitution urethroplasty (9).
Advantages of BMG
One fundamental technique in reconstructive urology is tissue transfer. To have an effective graft tissue there needs to be a wide availability of tissue and minimum harvest site morbidity, the graft must take to a vascular bed, and there needs to be ease of replication and harvest. A BMG is an ideal graft as the epithelium is thick with high elastic fiber content, the lamina propria is thin, and there is a wide availability with ease of harvest and minimal morbidity (10, 11).
Buccal mucosa is a non-keratinizing stratified squamous epithelium phenotypically similar to the penile and glandular urethra (12). It is exposed to a moist environment with natural immunity factors that protect the tissue from infection (13). The vascular characteristics of a BMG, which allow it to be an optimal graft for urethroplasty, are secondary to a panlaminar plexus, where the vascular supply penetrates from the submucosa to lamina propria (10, 14). This promotes angiogenesis and revascularization at the graft bed during graft take (10). Furthermore, when the lamina propria is harvested with epithelium, the graft can be thinned without altering its vascular or physical characteristics (14).
When compared with other substitution grafts for urethroplasty (lingual and lower lip), BMGs have fewer donor site complications (9, 11, 15–18). However, there are no reported differences in success rates of urethroplasty between BMGs and lingual grafts (11, 16, 17). Recently, both the American Urological Association (AUA) and the European Urological Association (EUA) guidelines promoted the preferential use of BMGs for urethral reconstruction over penile skin flaps (19, 20).
Technical considerations during the harvest of BMGs
The buccal mucosa is innervated by the long buccal nerve of cranial nerve III and the superior alveolar nerves of cranial nerve II (12). The vascular supply stems from the buccal artery, which branches from the maxillary artery (12). The borders of the buccal mucosa include the vermilion border anteriorly, the retromolar trigone posteriorly, and the mandibular and maxillary mucolabial folds superiorly and inferiorly. Just lateral to the buccal mucosal and lamina propria is the buccinator muscle, which should be left intact to limit postoperative pain and speech and mastication difficulty. The most important anatomical landmark recognized at time of harvest is the parotid or Stensen’s duct. This is identified as a small raised nodule located on the mucosa adjacent to the maxillary second molar (12).
At our institution, patients undergoing BMG urethroplasty undergo a standard harvest technique. A separate sterile instrument table is used. Harvest can be completed with a standard endotracheal tube or laryngeal mask airway secured to the contralateral side of harvest. Patients do not receive any oral preparation or antibiotic cleanses preoperatively or intraoperatively. The patient is draped in quartered-off sterile surgical towels. A surgical retractor, such as a Sluder–Jansen mouth retractor, with a tongue blade can be used. Our preference is to simplify the process and use a dry X-ray-detectable gauze sponge and pack the tongue in the contralateral mouth space. This, combined with three robust stay sutures placed 1–2 cm inside the inner vermilion border at the oral commissure and separated at 3–4 cm, is a more than sufficient retraction. Stensen’s duct is marked, and the expected graft length is marked circumferentially in an ellipsoid fashion with the desired width. There should be at least a 3- to 5-mm distance between the graft harvest site and Stensen’s duct. The distal aspect of the graft should be about 1–2 cm from the vermilion border, and the oral commissure retraction stitch can be incorporated into the distal graft apex to allow for further retraction during harvest (Figure 1). Using a spinal needle, normal saline is used to hydrodissect the mucosa. The previously marked graft site is incised with a 15 blade and the remainder of the graft is separated from the buccal fat pad and buccinator muscle with sharp scissor dissection. Bovie electrocautery can be used for hemostasis at the graft bed. Our preference is to close the graft site using a running-locking absorbable suture (Figure 2). The mouth is then packed with X-ray-detectable gauze sponges soaked in 1% lidocaine with 1:100,000 epinephrine and left until the end of the case. The graft is then de-fatted with scissor dissection down to the white lamina propria, perforated with a 15 blade, and placed in saline.
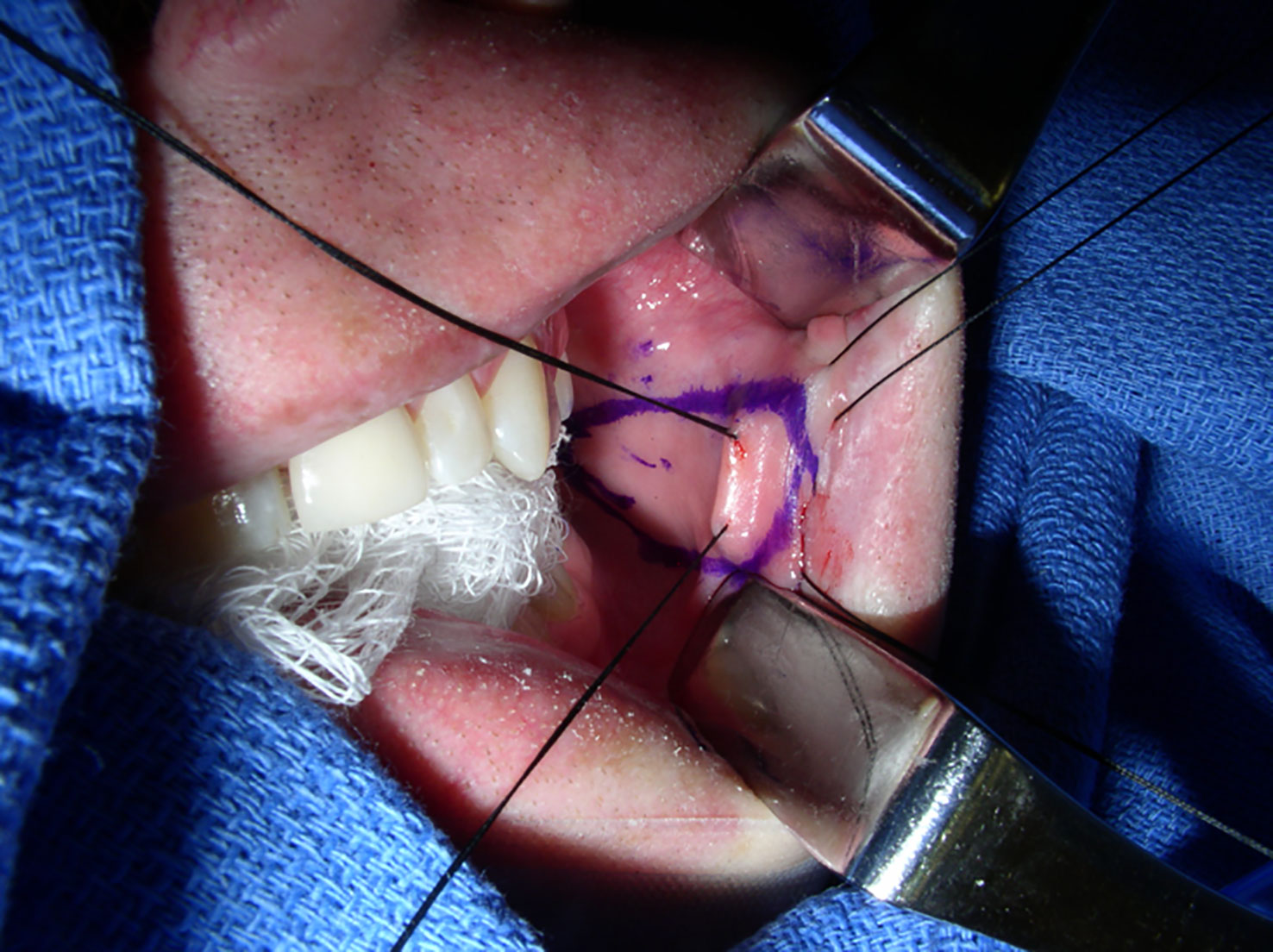
Figure 1 Typical setup for BMG harvest. The dry X-ray-detectable gauze sponge is packed to the contralateral oral space, and three retraction sutures are used with the middle incorporated into the distal apex of the graft. The Army–Navy retractors were used only for photographic exposure of the harvest site and are not typically needed during harvest. The image was obtained intraoperatively at Duke University Medical Center, with the operation completed under routine care. BMG, buccal mucosal graft.

Figure 2 The BMG donor harvest site closed with an absorbable running suture. The blue dot indicates the Stensen’s duct. The image was obtained intraoperatively at Duke University Medical Center, with the operation completed under routine care. BMG, buccal mucosal graft.
Care of the BMG harvest site
Although donor site complications are rare in both historic and contemporary series, oral care pathways and oral antiseptics remain commonly employed. The use of oral antiseptics for BMG urethroplasty is a relatively new development in the urologic literature. In their seminal report in 1992, Dessanti et al. described BMG harvesting as a “septic procedure” with no mention of oral antiseptic use (21). In the first reported adult series utilizing BMGs for urethroplasty the following year, El-Kasaby et al. (1993) reported no mention of oral care regimens or local antiseptic treatments (22). In their report on a two-team technique for buccal harvest in 1996, Morey and McAninch used penicillin G to prevent oral flora infection and made no use of oral antiseptics (6). The use of a povidone-iodine mouth rinse can be first found as a suggestion in the discussion by Burger et al. (1992) for comfort reasons (23), but the practice of using any preoperative oral antiseptics in the urology literature was not described until 2003 (24). Chlorhexidine was probably adopted from infection prevention efforts in other disciplines (24, 25), and was not specifically mentioned in the urologic literature until 2005, by MacDonald and Santucci (26).
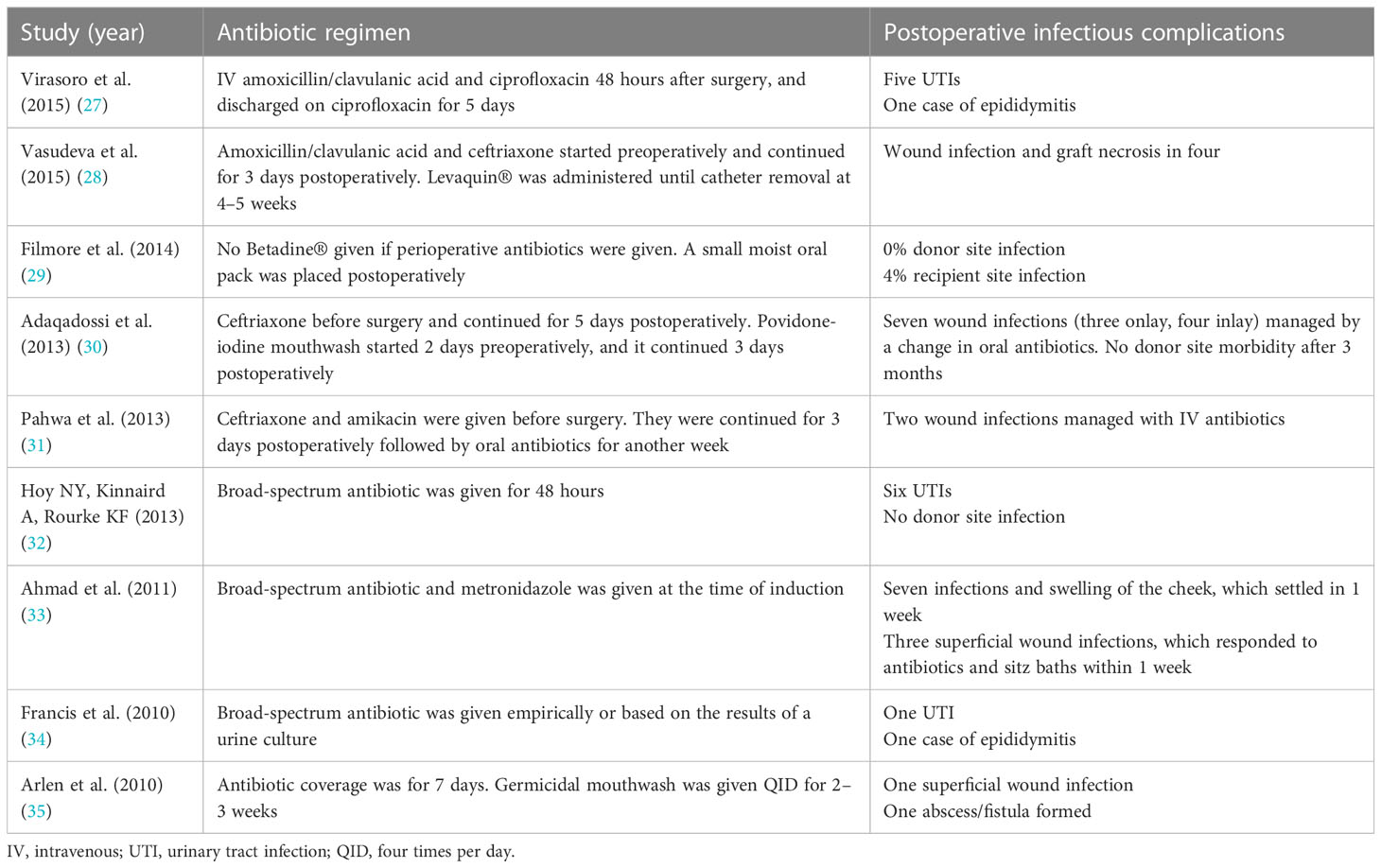
Early studies acknowledged that there was no evidence to support the use of aggressive sterilization measures and oral cleanses. Despite this, the use of antibiotics and germicidal mouthwashes in BMG studies was perpetuated with increasing duration and intensity to reduce the potential for infection (Table 1).
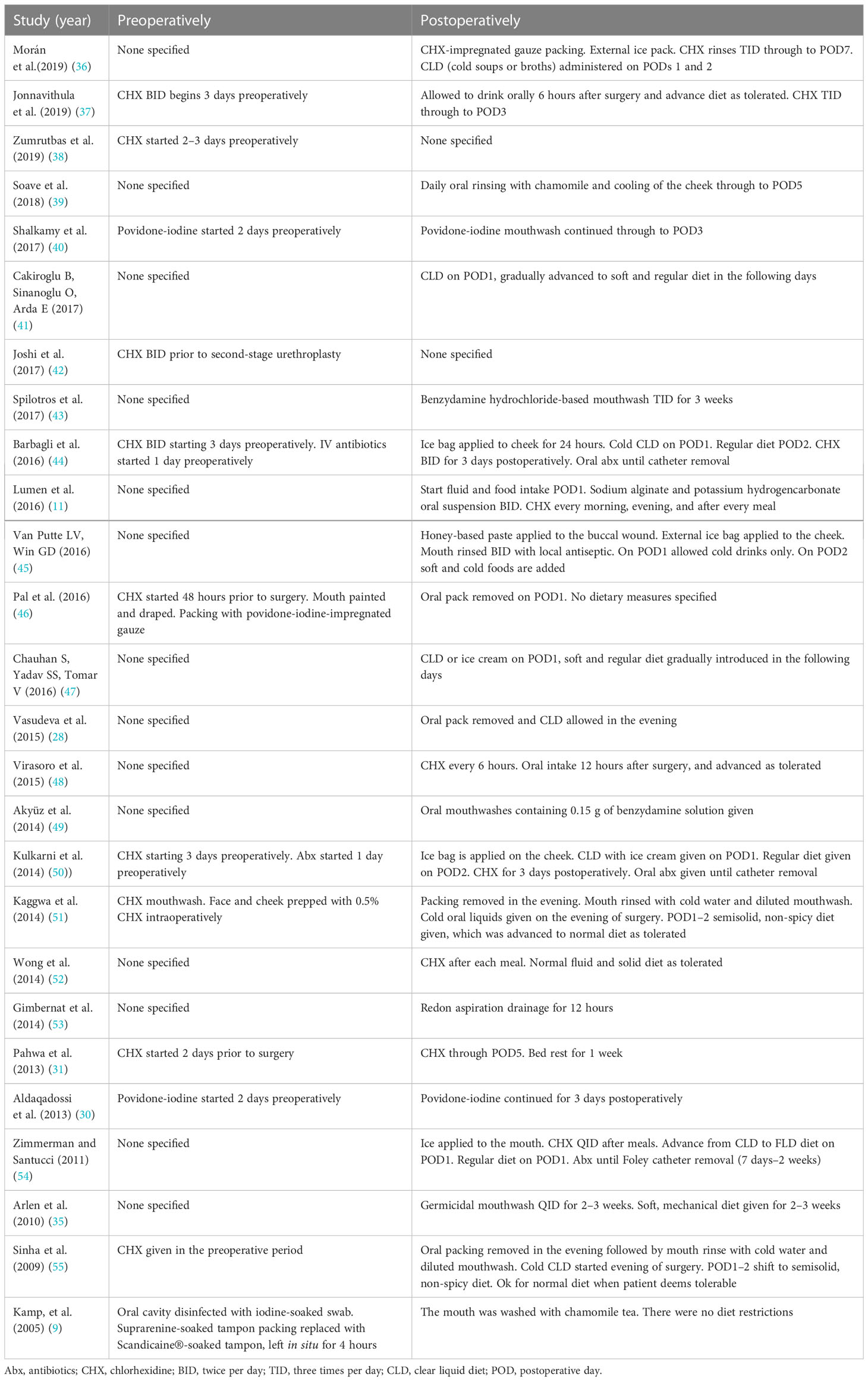
Today, oral care regimens and mouthwashes remain commonly employed and a review of the literature demonstrates significant heterogeneity between centers (Table 2).
We previously recommended soft food for 48 hours followed by a high-fiber diet, no alcohol for 24 hours, no nuts until the incision was completely healed, and the use of salt water rinses as needed for comfort. Mouthwash regimens were also used, such as Magic Mouthwash (lidocaine, aluminum hydroxide, and magnesium hydroxide), Mouthwash BLM (lidocaine, diphenhydramine, aluminum hydroxide, magnesium hydroxide, and simethicone) or 2% viscous lidocaine solution. Finding no significant benefit, however, we gradually relaxed these measures, and, commensurate with maxillofacial surgical standards, we have never utilized preoperative or intraoperative oral antibiotics. Our current postoperative care pathway includes unrestricted access to food and water, and patients are encouraged to advance their diet as tolerated. We have not found that reducing these measures and simplifying the postoperative pathway results in any deleterious impact on the patient experience.
Closure of the BMG donor site
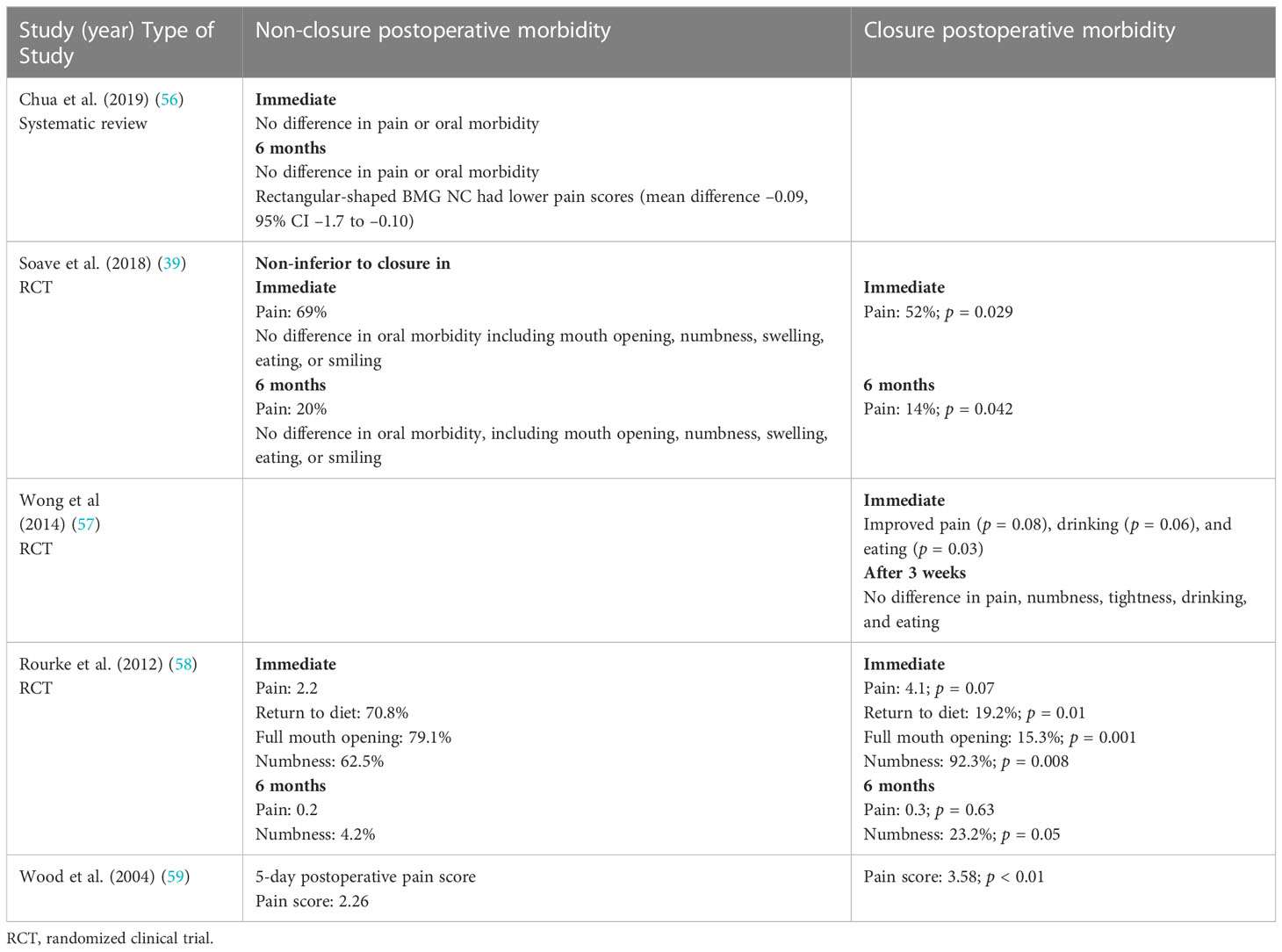
There have been several randomized clinical trials (RCTs) and studies evaluating the postoperative complications and morbidity associated with non-closure (NC) compared with closure (C) (Table 3).
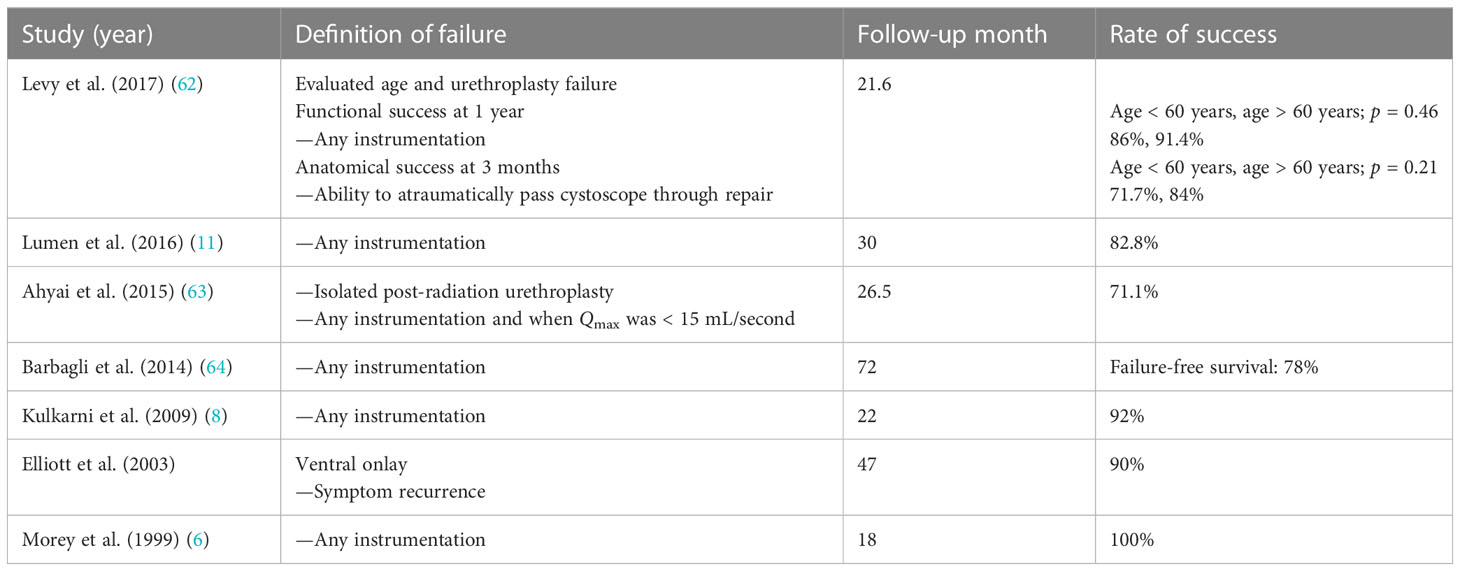
Urethroplasty success and outcomes
Recurrence rates are variable for BMG urethroplasty and differ based on urethral stricture location, length of stricture, and etiology. The success of urethroplasty is not universal and is difficult to define (60). A prospective study looking at five ways to define failure included: “1) stricture retreatment, 2) anatomical recurrence on cystoscopy [< 17 fr], 3) peak flow rate < 15 ml/second, 4) weak stream on questionnaire and 5) failure by any of these measures.” (60) The study found that success is highly variable and is inconsistent between definitions (60). This ultimately limits our ability to compare outcomes across studies. A systematic review of BMGs evaluating more than 2,000 urethroplasties noted no difference in dorsal vs. ventral onlay procedures (88.4% and 88.8% at 42.2 and 34.4 months, respectively), lateral onlay (83% at 77 months), the Asopa technique (86.7% at 28.9 months), and the Palminteri technique (90.1% at 21.9 months). (61) Table 4 includes several studies with definitions of failure and rates of success.
Reported complications of BMG substitution urethroplasty are rare or transient. Transient erectile dysfunction has been reported in 26% of patients with BMG substitution, compared with 50% in excision and primary anastomosis, with most recovering at 6 months and 90% of cases completely resolving (65). Even in complex urethral strictures of > 8 cm, the incidence of urethral pseudodiverticulum and penile chordee is reported to be around 3% (66).
BMG oral harvest complications
Lasting complications associated with BMG harvest are, overall, rare, with many reports noting early transient side effects. Several studies have reported low rates of long-term complications, including pain, oral tightness, numbness, and difficulty with mastication, mouth opening, and speech (18, 58, 59, 67). Pain at the donor site can be a transient side effect after surgery reported postoperatively in 50%–70% of patients in the first week (39). A multivariable analysis from a cohort of 553 patients undergoing BMG harvest reported that 53.2% of patients did not have postoperative pain, 32.4% had slight pain, and rare long-term difficulty with opening the mouth (95.5%), difficulty smiling (98.2%), and dry mouth (95.8%) (68). This study also found a 98.2% patient satisfaction with the procedure, with the only predictive variable for patient dissatisfaction being bilateral graft harvest (68).
Future directions
Tissue-engineered oral mucosa has been described with the intent to limit the morbidity in patients with long-length urethral strictures or those with recurrences and limited oral mucosa available, such as patients with lichen sclerosis (69, 70). This process involves autologously harvesting oral cells, which are then cultured on epithelial cell sheets, and after 2 weeks the sheets are then tubularized to form a two-layered graft (69). Bhargava et al. utilized tissue-engineered buccal mucosa in five patients with strictures secondary to lichen sclerosis. Buccal mucosal biopsies were taken and propagated using donor de-epithelialized dermis and used for both single- and two-stage procedures. At follow-up, two patients had limited graft take and all patients required further endoscopic treatment (71). Clearly, this is a promising avenue to explore, but further studies are needed before its widespread use.
Conclusion
BMG remains the gold standard for substitution graft urethroplasty. This review highlights the history of the use and widespread adoption of BMGs, the physiological characteristics of BMG that makes it an ideal graft material, the nuances of harvest and perioperative/preoperative variability in practices, associated complications, and future directions.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any identifiable images or data included in this article.
Author contributions
JF, AP, and KK contributed to the conception and design of the review; drafting and reviewing of the manuscript; revisions/edits; and a review of references. All authors contributed to the article and approved the submitted version.
Funding
The authors declare that this study received funding from Boston Scientific. The funder was not involved in the study design, collection, analysis, interpretation of data, the writing of the article, or the decision to submit it for publication.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Peterson AC, Webster GD. Management of urethral stricture disease: developing options for surgical intervention. BJU Int (2004) 94(7):971–6. doi: 10.1111/j.1464-410X.2004.05088.x
2. Carr LK, Macdiarmid SA, Webster GD. Treatment of complex anterior urethral stricture disease with mesh graft urethroplasty. J Urol (1997) 157(1):104–8. doi: 10.1016/S0022-5347(01)65298-4
3. Monfort G, Bretheau D, Di Benedetto V, Bankole R. Urethral stricture in children: treatment by urethroplasty with bladder mucosa graft. J Urol (1992) 148(5):1504–6. doi: 10.1016/S0022-5347(17)36950-1
4. Korneyev I, Ilyin D, Schultheiss D, Chapple C. The first oral mucosal graft urethroplasty was carried out in the 19th century: the pioneering experience of kirill sapezhko (1857-1928). Eur Urol (2012) 62(4):624–7. doi: 10.1016/j.eururo.2012.06.035
5. Humby G, Higgins TT. A one-stage operation for hypospadias. J Br Surg (1941) 29(113):84–92. doi: 10.1016/j.juro.2015.02.044
6. Morey AF, McAninch JW. Technique of harvesting buccal mucosa for urethral reconstruction. J Urol (1996) 155(5):1696–7. doi: 10.1016/S0022-5347(01)66167-6
7. Barbagli G, Palminteri E, Rizzo M. Dorsal onlay graft urethroplasty using penile skin or buccal mucosa in adult bulbourethral strictures. J Urol (1998) 160(4):1307–9. doi: 10.1016/S0022-5347(01)62522-9
8. Kulkarni S, Barbagli G, Sansalone S, Lazzeri M. One-sided anterior urethroplasty: a new dorsal onlay graft technique. BJU Int (2009) 104(8):1150–5. doi: 10.1111/j.1464-410X.2009.08590.x
9. Kamp S, Knoll T, Osman M, Hacker A, Michel MS, Alken P. Donor-site morbidity in buccal mucosa urethroplasty: lower lip or inner cheek? BJU Int (2005) 96(4):619–23. doi: 10.1111/j.1464-410X.2005.05695.x
10. Duckett JW, Coplen D, Ewalt D, Baskin LS. Buccal mucosal urethral replacement. J Urol (1995) 153(5):1660–3. doi: 10.1016/S0022-5347(01)67497-4
11. Lumen N, Vierstraete-Verlinde S, Oosterlinck W, Hoebeke P, Palminteri E, Goes C, et al. Buccal versus lingual mucosa graft in anterior urethroplasty: a prospective comparison of surgical outcome and donor site morbidity. J Urol (2016) 195(1):112–7. doi: 10.1016/j.juro.2015.07.098
12. Markiewicz MR, Margarone JE, Barbagli G, Scannapieco FA. Oral mucosa harvest: an overview of anatomic and biologic considerations. EAU-EBU Update Ser (2007) 5(5):179–87. doi: 10.1016/j.eeus.2007.05.002
13. Rudney JD, Chen R. The vital status of human buccal epithelial cells and the bacteria associated with them. Arch Oral Biol (2006) 51(4):291–8. doi: 10.1016/j.archoralbio.2005.09.003
14. Jordan GH. Principles of tissue transfer techniques in urethral reconstruction. Urologic Clinics North America (2002) 29(2):267–75. doi: 10.1016/S0094-0143(02)00034-4
15. Sharma AK, Chandrashekar R, Keshavamurthy R, Nelvigi GG, Kamath AJ, Sharma S, et al. Lingual versus buccal mucosa graft urethroplasty for anterior urethral stricture: a prospective comparative analysis. Int J Urol (2013) 20(12):1199–203. doi: 10.1111/iju.12158
16. Pal DK, Gupta DK, Ghosh B, Bera MK. A comparative study of lingual mucosal graft urethroplasty with buccal mucosal graft urethroplasty in urethral stricture disease: an institutional experience. Urol Ann (2016) 8(2):157–62. doi: 10.4103/0974-7796.172214
17. Wang A, Chua M, Talla V, Fernandez N, Ming J, Sarino EM, et al. Lingual versus buccal mucosal graft for augmentation urethroplasty: a meta-analysis of surgical outcomes and patient-reported donor site morbidity. Int Urol Nephrol (2021) 53(5):907–18. doi: 10.1007/s11255-020-02720-7
18. Jang TL, Erickson B, Medendorp A, Gonzalez CM. Comparison of donor site intraoral morbidity after mucosal graft harvesting for urethral reconstruction. Urology (2005) 66(4):716–20. doi: 10.1016/j.urology.2005.04.045
19. Lumen N, Campos-Juanatey F, Greenwell T, Martins FE, Osman NI, Riechardt S, et al. et al: European Association of urology guidelines on urethral stricture disease (Part 1): management of Male urethral stricture disease. Eur Urol (2021) 80(2):190–200. doi: 10.1016/j.eururo.2021.05.022
20. Wessells H, Angermeier KW, Elliott S, Gonzalez CM, Kodama R, Peterson AC, et al. et al: Male Urethral stricture: American urological association guideline. J Urol (2017) 197(1):182–90. doi: 10.1016/j.juro.2016.07.087
21. Dessanti A, Rigamonti W, Merulla V, Falchetti D, Caccia G. Autologous buccal mucosa graft for hypospadias repair: an initial report. J Urol (1992) 147(4):1081–3. doi: 10.1016/S0022-5347(17)37478-5
22. El-Kasaby A, Fath-Alla M, Noweir A, El-Halaby M, Zakaria W, El-Beialy M. The use of buccal mucosa patch graft in the management of anterior urethral strictures. J Urol (1993) 149(2):276–8. doi: 10.1016/S0022-5347(17)36054-8
23. Bürger RA, Müller SC, El-Damanhoury H, Tschakaloff A, Riedmiller H, Hohenfellner R. The buccal mucosal graft for urethral reconstruction: a preliminary report. J Urol (1992) 147(3):662–4. doi: 10.1016/S0022-5347(17)37340-8
24. Sahin C, Seyhan T. Use of buccal mucosal grafts in hypospadia-crippled adult patients. Ann Plast Surg (2003) 50(4):382–6. doi: 10.1097/01.SAP.0000037274.65665.FF
25. Zamany A, Safavi K, Spångberg LS. The effect of chlorhexidine as an endodontic disinfectant. Oral Surgery Oral Medicine Oral Pathology Oral Radiology Endodontology (2003) 96(5):578–81. doi: 10.1016/S1079-2104(03)00168-9
26. MacDonald MF, Santucci RA. Review and treatment algorithm of open surgical techniques for management of urethral strictures. Urology (2005) 65(1):9–15. doi: 10.1016/j.urology.2004.07.011
27. Virasoro R, Storme OA, Capiel L, Ghisini DA, Rovegno A. [Buccal mucosa graft augmented anastomotic urethroplasty for the treatment of bulbar urethral strictures]. Arch Esp Urol (2015) 68(10):730–7.
28. Vasudeva P, Nanda B, Kumar A, Kumar N, Singh H, Kumar R. Dorsal versus ventral onlay buccal mucosal graft urethroplasty for long-segment bulbar urethral stricture: a prospective randomized study. Int J Urol (2015) 22(10):967–71. doi: 10.1111/iju.12859
29. Fillmore WJ, Rieck KL. Buccal mucosa grafting for male urethroplasty: long-term follow up of patients’ experience with a team approach and primary closure. J Oral Maxillofac Surgery Medicine Pathol (2014) 26(4):437–42. doi: 10.1016/j.ajoms.2013.04.013
30. Aldaqadossi H, El Gamal S, El-Nadey M, El Gamal O, Radwan M, Gaber M. Dorsal onlay (B arbagli technique) versus dorsal inlay (A sopa technique) buccal mucosal graft urethroplasty for anterior urethral stricture: a prospective randomized study. Int J Urol (2014) 21(2):185–8. doi: 10.1111/iju.12235
31. Pahwa M, Gupta S, Pahwa M, Jain BD, Gupta M. A comparative study of dorsal buccal mucosa graft substitution urethroplasty by dorsal urethrotomy approach versus ventral sagittal urethrotomy approach. Adv Urol (2013) 2013. doi: 10.1155/2013/124836
32. Hoy NY, Kinnaird A, Rourke KF. Expanded use of a dorsal onlay augmented anastomotic urethroplasty with buccal mucosa for long segment bulbar urethral strictures: analysis of outcomes and complications. Urology (2013) 81(6):1357–61. doi: 10.1016/j.urology.2013.02.012
33. Ahmad H, Mahmood A, Niaz WA, Akmal M, Murtaza B, Nadim A. Bulbar uretheral stricture repair with buccal mucosa graft urethroplasty. J Pak Med Assoc (2011) 61(5):440–2.
34. Fransis K, Vander Eeckt K, Van Poppel H, Joniau S. Results of buccal mucosa grafts for repairing long bulbar urethral strictures. BJU Int (2010) 105(8):1170–2. doi: 10.1111/j.1464-410X.2009.08848.x
35. Arlen AM, Powell CR, Hoffman HT, Kreder KJ. Buccal mucosal graft urethroplasty in the treatment of urethral strictures: experience using the two-surgeon technique. ScientificWorldJournal (2010) 10:74–9. doi: 10.1100/tsw.2010.16
36. Moran E, Bonillo MA, Fernandez-Estevan L, Martinez-Cuenca E, Arlandis S, Broseta E, et al. Oral quality of life after buccal mucosal graft harvest for substitution urethroplasty. more than a bite? World J Urol (2019) 37(2):385–9. doi: 10.1007/s00345-018-2381-9
37. Jonnavithula N, Bachu D, Sriramoju V, Devraj R, Gunta R, Pisapati MV. Effect of infraorbital nerve block on postoperative pain and 30-day morbidity at the donor site in buccal mucosal graft urethroplasty. J Anaesthesiology Clin Pharmacol (2019) 35(1):114. doi: 10.4103/joacp.JOACP_211_17
38. Zumrutbas AE, Ozlulerden Y, Celen S, Kucuker K, Aybek Z. The outcomes of kulkarni’s one-stage oral mucosa graft urethroplasty in patients with panurethral stricture: a single centre experience. World J Urol (2020) 38(1):175–81. doi: 10.1007/s00345-019-02758-y
39. Soave A, Dahlem R, Pinnschmidt HO, Rink M, Langetepe J, Engel O, et al. Substitution urethroplasty with closure versus nonclosure of the buccal mucosa graft harvest site: a randomized controlled trial with a detailed analysis of oral pain and morbidity. Eur Urol (2018) 73(6):910–22. doi: 10.1016/j.eururo.2017.11.014
40. Shalkamy O, Abdelrahim A, Elmikkawy S, Mourad M, Eleweedy S. Long-term outcomes of single stage dorsal onlay buccal mucosa urethroplasty for different anterior urethral strictures: a prospective study. Urol Nephrol Open Access J (2017) 5(5):00188. doi: 10.15406/unoaj.2017.05.00188
41. Cakiroglu B, Sinanoglu O, Arda E. Outcome of buccal mucosa urethroplasty in the management of urethral strictures. Archivio Italiano di Urologia e Andrologia (2017) 89(2):139–42. doi: 10.4081/aiua.2017.2.139
42. Joshi PM, Barbagli G, Batra V, Surana S, Hamouda A, Sansalone S, et al. A novel composite two-stage urethroplasty for complex penile strictures: a multicenter experience. Indian J Urology: IJU: J Urological Soc India (2017) 33(2):155. doi: 10.4103/0970-1591.203426
43. Spilotros M, Sihra N, Malde S, Pakzad MH, Hamid R, Ockrim JL, et al. Buccal mucosal graft urethroplasty in men–risk factors for recurrence and complications: a third referral centre experience in anterior urethroplasty using buccal mucosal graft. Trans andrology Urol (2017) 6(3):510. doi: 10.21037/tau.2017.03.69
44. Barbagli G, Balò S, Sansalone S, Lazzeri M. How to harvest buccal mucosa from the cheek. Afr J Urol (2016) 22(1):18–23. doi: 10.1016/j.afju.2015.09.001
45. Van Putte L, De Win G. Modified one-stage dorsal-inlay buccal mucosa graft technique for ventral penile urethral and penile skin erosion: a step-by-step guide. Arab J Urol (2016) 14(4):312–6. doi: 10.1016/j.aju.2016.08.003
46. Pal B, Modi P, Modi J, Nagarajan R, Kumar S, Patel K, et al. Buccal mucosal graft urethroplasty in patients awaiting renal transplantation. In: Transplantation proceedings. (Ahmedabad, Gujarat, India: Elsevier) (2016). 2016, 21–5.
47. Chauhan S, Yadav SS, Tomar V. Outcome of buccal mucosa and lingual mucosa graft urethroplasty in the management of urethral strictures: a comparative study. Urol Ann (2016) 8(1):36. doi: 10.4103/0974-7796.165715
48. Virasoro R, Storme OA, Capiel L, Ghisini DA, Rovegno A. Buccal mucosa graft augmented anastomotic urethroplasty for the treatment of bulbar urethral strictures. Arch Esp Urol (2015) 1(68):10.
49. Akyüz M, Güneş M, Koca O, Sertkaya Z, Kanberoğlu H, Karaman M. Evaluation of intraoral complications of buccal mucosa graft in augmentation urethroplasty. Turk J Urol (2014) 40(3):156–60. doi: 10.5152/tud.2014.46343
50. Kulkarni SB, Barbagli G, Sansalone S, Joshi PM. Harvesting oral mucosa for one-stage anterior urethroplasty. Indian J Urology: IJU: J Urological Soc India (2014) 30(1):117. doi: 10.4103/0970-1591.124222
51. Kaggwa S, Galukande M, Dabanja H, Luweesi H. Outcomes of dorsal and ventral buccal graft urethroplasty at a tertiary hospital in Uganda. Int Scholarly Res Notices (2014) 2014. doi: 10.1155/2014/316819
52. Wong E, Fernando A, Alhasso A, Stewart L. Does closure of the buccal mucosal graft bed matter? results from a randomized controlled trial. Urology (2014) 84(5):1223–7. doi: 10.1016/j.urology.2014.06.041
53. Gimbernat H, Arance I, Redondo C, Meilán E, Andrés G, Angulo JC. Treatment for long bulbar urethral strictures with membranous involvement using urethroplasty with oral mucosa graft. Actas Urol Esp (2014) 38(8):544–51. doi: 10.1016/j.acuro.2014.04.001
54. Zimmerman W, Santucci R. Buccal mucosa urethroplasty for adult urethral strictures. Indian J Urol (2011) 27(3):364–70. doi: 10.4103/0970-1591.85441
55. Sinha RJ, Singh V, Sankhwar SN, Dalela D. Donor site morbidity in oral mucosa graft urethroplasty: implications of tobacco consumption. BMC Urol (2009) 9(1):15. doi: 10.1186/1471-2490-9-15
56. Chua ME, Silangcruz JMA, Ming JM, Sarino EM, DeLong J, Virasoro R, et al. Nonclosure versus closure of buccal mucosal graft harvest site: a systematic review and meta-analysis of patient-reported outcomes. Urology (2019) 125:213–21. doi: 10.1016/j.urology.2018.12.008
57. Wong E, Fernando A, Alhasso A, Stewart L. Does closure of the buccal mucosal graft bed matter? results from a randomized controlled trial. Urology (2014) 84(5):1223–7. doi: 10.1016/j.urology.2014.06.041
58. Rourke K, McKinny S, St Martin B. Effect of wound closure on buccal mucosal graft harvest site morbidity: results of a randomized prospective trial. Urology (2012) 79(2):443–7. doi: 10.1016/j.urology.2011.08.073
59. Wood DN, Allen SE, Andrich DE, Greenwell TJ, Mundy AR. The morbidity of buccal mucosal graft harvest for urethroplasty and the effect of nonclosure of the graft harvest site on postoperative pain. J Urol (2004) 172(2):580–3. doi: 10.1097/01.ju.0000132846.01144.9f
60. Anderson KT, Vanni AJ, Erickson BA, Myers JB, Voelzke B, Breyer BN, et al. 3rd et al: defining success after anterior urethroplasty: an argument for a universal definition and surveillance protocol. J Urol (2022) 208(1):135–43. doi: 10.1097/JU.0000000000002501
61. Mangera A, Patterson JM, Chapple CR. A systematic review of graft augmentation urethroplasty techniques for the treatment of anterior urethral strictures. Eur Urol (2011) 59(5):797–814. doi: 10.1016/j.eururo.2011.02.010
62. Levy M, Gor RA, Vanni AJ, Stensland K, Erickson BA, Myers JB, et al. The impact of age on urethroplasty success. Urology (2017) 107:232–8. doi: 10.1016/j.urology.2017.03.066
63. Ahyai SA, Schmid M, Kuhl M, Kluth LA, Soave A, Riechardt S, et al. Outcomes of ventral onlay buccal mucosa graft urethroplasty in patients after radiotherapy. J Urol (2015) 194(2):441–6. doi: 10.1016/j.juro.2015.03.116
64. Barbagli G, Kulkarni SB, Fossati N, Larcher A, Sansalone S, Guazzoni G, et al. Long-term followup and deterioration rate of anterior substitution urethroplasty. J Urol (2014) 192(3):808–13. doi: 10.1016/j.juro.2014.02.038
65. Erickson BA, Granieri MA, Meeks JJ, Cashy JP, Gonzalez CM. Prospective analysis of erectile dysfunction after anterior urethroplasty: incidence and recovery of function. J Urol (2010) 183(2):657–61. doi: 10.1016/j.juro.2009.10.017
66. Xu YM, Qiao Y, Sa YL, Wu DL, Zhang XR, Zhang J, et al. Substitution urethroplasty of complex and long-segment urethral strictures: a rationale for procedure selection. Eur Urol (2007) 51(4):1093–1098; discussion 1098-1099. doi: 10.1016/j.eururo.2006.11.039
67. Markiewicz MR, DeSantis JL, Margarone JE III, Pogrel MA, Chuang S-K. Morbidity associated with oral mucosa harvest for urological reconstruction: an overview. J Oral Maxillofac Surg (2008) 66(4):739–44. doi: 10.1016/j.joms.2007.11.023
68. Barbagli G, Fossati N, Sansalone S, Larcher A, Romano G, Dell'Acqua V, et al. Prediction of early and late complications after oral mucosal graft harvesting: multivariable analysis from a cohort of 553 consecutive patients. J Urol (2014) 191(3):688–93. doi: 10.1016/j.juro.2013.09.006
69. Mikami H, Kuwahara G, Nakamura N, Yamato M, Tanaka M, Kodama S. Two-layer tissue engineered urethra using oral epithelial and muscle derived cells. J Urol (2012) 187(5):1882–9. doi: 10.1016/j.juro.2011.12.059
70. Chapple C. Tissue engineering of the urethra: where are we in 2019? World J Urol (2020) 38(9):2101–5. doi: 10.1007/s00345-019-02826-3
Keywords: urethroplasty, buccal mucosa, graft, complications, history
Citation: Foreman J, Peterson A and Krughoff K (2023) Buccal mucosa for use in urethral reconstruction: evolution of use over the last 30 years. Front. Urol. 3:1138707. doi: 10.3389/fruro.2023.1138707
Received: 06 January 2023; Accepted: 12 April 2023;
Published: 02 May 2023.
Edited by:
Francisco E. Martins, University of Lisbon, PortugalReviewed by:
Simone Morselli, University of Florence, ItalyFang Chen, Shanghai Children’s Hospital, China
Vladimir Kojovic, University of Belgrade, Serbia
Copyright © 2023 Foreman, Peterson and Krughoff. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jordan Foreman, Sm9yZGFuUkZvcmVtYW5AZ21haWwuY29t
 Jordan Foreman
Jordan Foreman Andrew Peterson
Andrew Peterson Kevin Krughoff2
Kevin Krughoff2