- 1Surgical Team: Infants, Toddlers, Children (STITCh), Queensland Children’s Hospital, South Brisbane, QLD, Australia
- 2Mayne Academy of Paediatrics and Child Health, Faculty of Medicine, University of Queensland, St Lucia, QLD, Australia
Background: Cryptorchidism is the most common referral to our paediatric surgical telehealth service. There is a paucity of literature on this condition in a telehealth context. We wished to determine the accuracy of telehealth in the diagnosis of cryptorchidism, and to examine for any predictors that may increase diagnostic confidence.
Methods: Retrospective analysis of a consecutive cohort from November 2009 (start of service) to December 31st 2021. Data from telehealth were compared against eventual surgical outcomes.
Results: There were 387 consecutive patients seen, resulting in 335 bookings for orchidopexy. 69/327 patients presenting for operation did not have an orchidopexy performed. Operations did not proceed as booked for 37% of children. Referrals for bilateral cryptorchidism were more likely to be normal on face to face review. The average round-trip distance for families from home to hospital, and back, was 948km.
Conclusions: Telehealth is not an accurate method for assessing cryptorchidism. Operations were cancelled for 1 in 5 children, and altered for 3 in 8. Travel distances for families were significant. The inaccuracy of telehealth for assessing cryptorchidism must balance inconvenience for families against disruption to elective operating lists.
Introduction
Background and rationale
Queensland has 4.9 million people spread over 1.73 million km2, with a population density of less than one person per square kilometre over 93% of the state. It is more than 2500km from the Northern tip to our children’s hospital in the Southeast corner. There are only three paediatric surgical units servicing Queensland and northern New South Wales, so parents are often expected to travel long distances to see a paediatric surgeon. Given Queensland’s geography and population distribution, the provision of efficient and equitable paediatric surgical services remains a challenge. Telehealth addresses these challenges.
The use of telemedicine in the management of paediatric surgical conditions is well described in the literature (1–3). Queensland has reported on over 20,000 telemedicine consultations, and the Department of Paediatric Surgery at Queensland Children’s Hospital has reported a median distance saved per patient of 600km in telemedicine consultations for burns (4). We have demonstrated the benefits of a cost-effective service to both hospital and family for many paediatric conditions (4–6). In late 2009 our existing Telehealth service was expanded into general paediatric surgery, building on our unit’s telemedicine program for patients with burns. Burns, and their resulting scars, are relatively easy to see. For many conditions history, radiology and visualisation only are required. Some examinations are relatively simple to talk a clinician through. There are a number of conditions where examination expertise is more difficult to acquire, such as the examination of patients with apparent cryptorchidism.
The Canadian experience demonstrates telemedicine for paediatric surgical conditions is beneficial and has high concordance with face-to-face diagnoses (1, 3, 7). However, in three studies from Alberta, Manitoba and Saskatchewan only six patients with a referral diagnosis of undescended testes (UDT) are mentioned in the combined reports (1, 3, 7). We have previously reported our own experience with paediatric surgical telemedicine (8, 9). Questions regarding testicular descent represent the most common referral diagnosis to our outpatient clinics, representing 17% of all referrals. In our telemedicine cohort we noted good concordance generally with the eventual face-to-face diagnosis, but had some concerns regarding the diagnostic accuracy of telemedicine for cryptorchidism (9).
Objectives
This aim of this study is to review the outcomes of all patients referred with a presumptive disorder of testicular descent who were first seen via telehealth, and subsequently booked for an orchidopexy. Our hypothesis is that there would be a relatively poor concordance between telemedicine and subsequent face-to-face diagnosis. Our aims were to determine if there were any factors that may suggest higher (or lower) accuracy with the telehealth referral diagnosis. Such factors might include:
● referral source (eg General Practitioner, Paediatrician, etc),
● patient age,
● laterality of the UDT (unilateral vs bilateral),
● the results of any ultrasound scans (USS), and
● the experience of the originating site examiner.
Methods
Study design and setting
This is a retrospective chart review of a consecutive cohort of patients referred to an established paediatric telehealth service. We expanded our telehealth into general paediatric surgery in November 2009, giving us our start date. The end date for this cohort was 31st December 2021, in order to allow sufficient lead-time for face-to-face assessments and outcomes to be determined.
Participants
Only new referrals for anomalies of testicular descent (undescended testis/es, cryptorchidism, ?retractile/?undescended testes) were included. Post-operative visits were excluded. Patients not subsequently seen face-to-face were excluded. The unit of assessment was the patient (rather than the testis in cases of bilateral pathology).
Variables and data sources
Patients are referred by GPs, Paediatricians, or other providers (eg Neonatologists, Urologists). They are then seen via Telehealth, usually at a hospital with appropriate facilities nearest to the family home. Telehealth clinics are not routinely performed by doctors in training at our institution, thus patients were assessed by a Consultant Paediatric Surgeon from Brisbane. At the originating site there are a variety of clinicians in attendance; including nursing staff, junior medical staff, Paediatricians or General Practitioners. There was often no clinician present at the local site, reflecting work practices at those sites. Consultations are conducted via a dedicated and secure videolink, with the ability for the Brisbane site to manipulate the originating site camera (pan, tilt, and zoom) to be able to watch the examination.
Patients were identified from prospectively gathered telehealth referral records. Telehealth records, patient clinical charts, and operation reports were used to gather data. Data were gathered on demographics, referral diagnosis, use of sonography, telehealth consultation and diagnosis, face-to-face review and diagnosis, operative data, and follow-up consultations. Human Research Ethics Committee (HREC) approval for this study was obtained prior to commencement (HREC/17/QRCH/143).
Outcomes
Outcomes of interest were the accuracy of telehealth diagnosis, as evidenced by the numbers of patients booked for orchidopexy who subsequently underwent an operation. If there was a significant false positive rate (cancellation following face-to-face review) then we wished to see if there were any predictors that may be used to increase confidence regarding the telemedicine diagnosis. Possible predictors a priori were the job role of the originating site examiner, USS findings (if performed), and age of the patient. We wondered if ‘bilateral UDT’ sonographically may reflect normal testes retracting in response to anxiety (or cold sonography gel) at the time of the USS. We were also interested to examine the potential impacts on travel distances saved for families.
Statistical methods
Statistical analyses were performed using SPSS version 28 (IBM Corporation, Armonk, NY, USA). Data were not expected to be normally distributed, so medians and interquartile ranges (IQR) were used for continuous data. Non-parametric two-tailed tests were used throughout, with a p-value of 0.05 deemed significant.
Results
Participants and descriptive data
There were 387 children referred with a disorder of testicular descent, seen via Telehealth between commencement of the service on 1st November 2009 and the end of December 2021 (Figure 1). Some children (21) were seen more than once via Telehealth prior to a decision being made (discharge or orchidopexy). Most of these reviews occurred early in our experience, and were done when we thought the examination was normal but could not be entirely sure. On a few occasions children were brought back as they were under three months old and were therefore re-reviewed to allow time for spontaneous descent post-delivery.
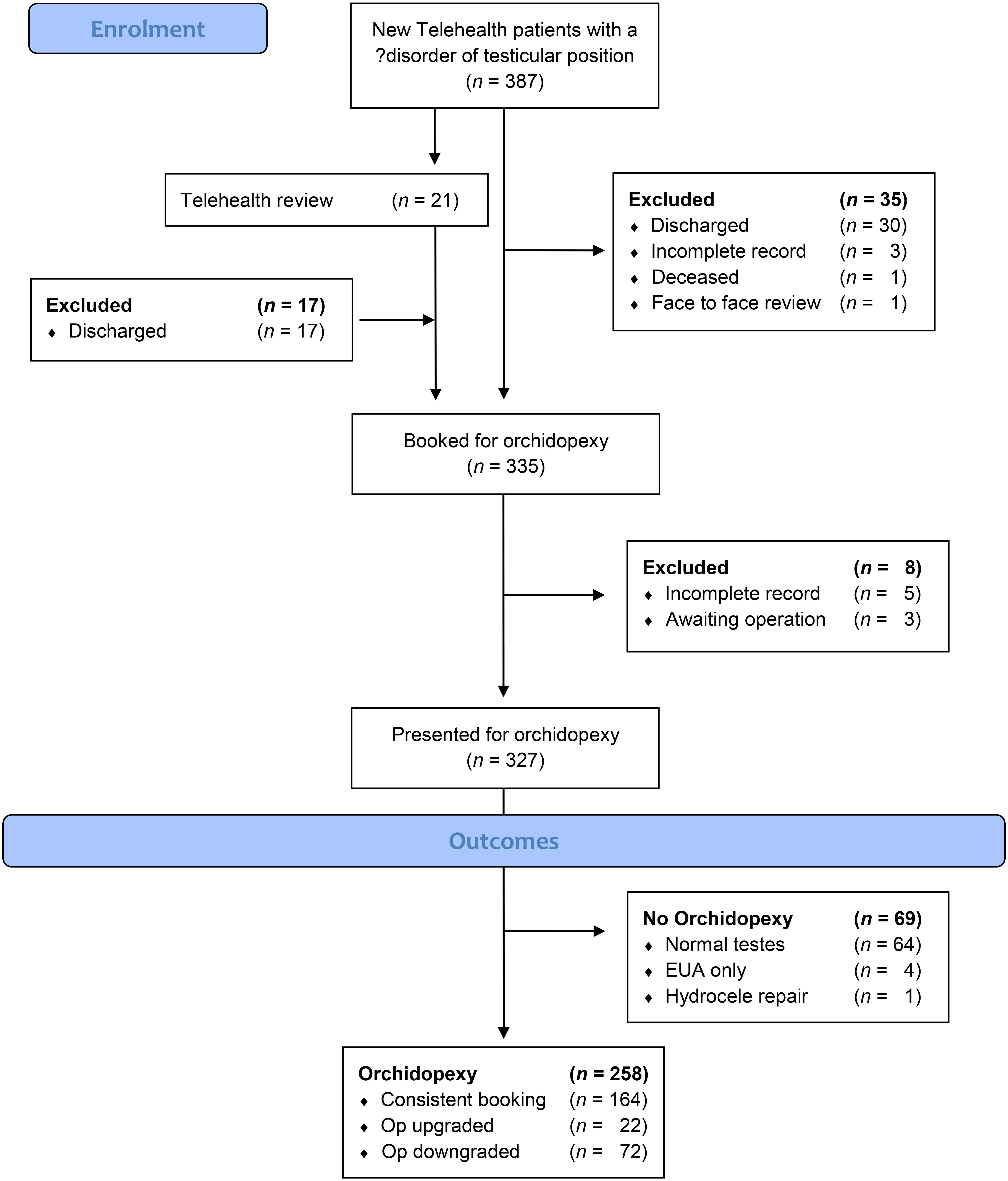
Figure 1 CONSORT diagram of consecutive referrals for cryptorchidism, seen in paediatric surgical telehealth.
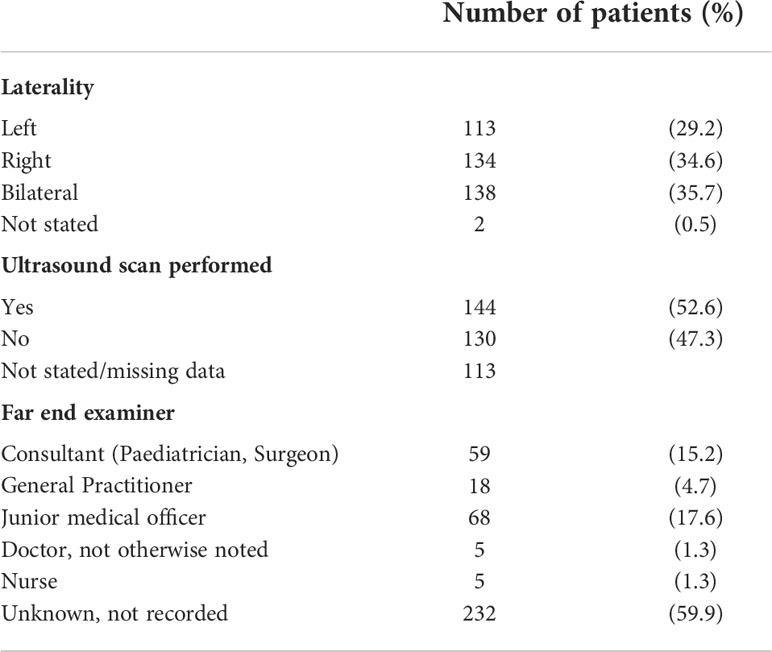
The median age at first Telehealth consultation was 20 months (IQR 11-52 months; range 0-173). Referrals were evenly distributed between left, right, and bilateral UDT (Table 1). Ultrasound had been performed in 52.7% of all referrals. Our records detailing the presence of an originating site examiner, and their job role, were scant. In approximately 60% of cases there was no documentation in the clinical record of an originating site examiner (either their presence/absence, or their role). Children were seen in Telehealth by one of eight paediatric surgeons in Brisbane. The median wait from Telehealth decision to operation date was 14 weeks (IQR 9.14-22.96 weeks). There was a significant reduction in the median wait when comparing 2009-2014, with 2016 and beyond (independent samples median test, p = 0.010). 2015 was a transition year, for reasons outlined below in the discussion. Operations were performed at a median of 23 months (IQR 14-58.5).
Telehealth consultations were made to 42 different towns or sites (Table 2). Six sites (Rockhampton, Bundaberg, Gladstone, Hervey Bay, Toowoomba, Emerald) accounted for 79.8% of all consultations. All other sites were ‘single-digit’ visits only, with 18 sites visited once only and a further 10 twice only. For the most part, consultations were to the local hospital or GP practice. During the COVID lockdowns, consultations were to people’s homes. The median round-trip distance for families to Brisbane was 948km (IQR 580-1238km, maximum 4272km).
Outcome data and main results
In 335 boys a booking for orchidopexy was made, and 327 of those children (97.6%) subsequently presented for their operation. Operations were cancelled on the day for 64/327 (19.6%) children as their testes were normally descended on preoperative review by a member of the paediatric surgical team. Four further children had an examination under anaesthetic only, without operation, as their testes were normally descended. A fifth child had a herniotomy performed for a unilateral hydrocele, also with normally descended testes. In total, 69/327 (21.1%) children did not have an orchidopexy performed.
Operations were upgraded (from unilateral to bilateral, and/or from open to laparoscopic) for 22/258, and downgraded for 72/258 after face-to-face review pre-operatively. A total of 94/258 (36.4%) orchidopexies did not proceed as booked.
Age of the patient; at referral, Telehealth appointment, or subsequent face-to-face pre-operative review was not predictive of whether an operation was subsequently performed or not.
The contemporaneous records did not often record clinical personnel present at the originating site, so data were insufficient to determine if examiner status there was predictive of operation with any degree of statistical confidence. Patients referred following a Paediatric Clinic review were more likely to proceed to operation than patients referred by General Practitioners (83.0% vs 76.8%, Pearson X2 p = 0.007).
Patients referred with bilateral UDT were less likely to subsequently have an orchidopexy than those referred with unilateral UDT (Pearson X2 p < 0.001). Ultrasound scanning (whether performed or not) was not predictive of orchidopexy (p = 0.968).
Discussion
Key results
Published studies on telemedicine for paediatric surgery contain few or no patients with cryptorchidism. Our earlier work suggested telehealth assessment of cryptorchidism was potentially a problematic area (9). This study of our entire cohort to date confirms our suspicion telehealth assessment cannot be entirely relied upon. A significant number of patients booked for orchidopexy did not receive an operation (69/327, 21.1%). Of those who proceeded to operation, 22/258 (8.5%) had their operations upgraded, and 72/258 (27.9%) downgraded (from laparoscopic to open, from bilateral to unilateral, from inguinal to scrotal). These data have implications for the discussions we now have with families during telemedicine consultations for cryptorchidism. They also demonstrate how flexible the theatre team needs to be in gathering resources for these cases, and in the way such a list is planned. A good team huddle prior to the list commencing, to update the team of any changes, is essential.
Two of every three patients referred (258/387) proceeded to orchidopexy. This figure is in keeping with other cohorts referred to a specialist paediatric surgeon or paediatric urologist (10). Nearly a third of all patients were referred with bilateral UDT. This is approximately double population estimates from other studies and may reflect an incorrect diagnosis of retractile testes as undescended (11, 12). There was a statistically significant difference in the outcomes of these patients when compared to their unilateral peers, indicating ‘bilateral UDT’ could be used as an a priori indication of an increased likelihood of normal testes. This finding informs the discussion only; it is not strong enough to discharge a patient, as 67/138 patients referred with bilateral UDT eventually proceeded to orchidopexy on one or both sides.
The American Urological Association, British Association of Paediatric Surgery, Canadian Urological Association, European Association of Urology, European Society for Paediatric Urology, and the Nordic Consensus have all produced evidence-based guidelines on the assessment and management of cryptorchidism. None recommend the use of imaging in routine pre-operative evaluation (13–20). Despite these guidelines, it is clear ultrasound scanning is commonly utilised in the community assessment of testicular descent (>50% of this cohort) (21, 22). We did not find it helpful.
Ultrasound for non-palpable testis has a sensitivity of 45% and a specificity of 78% in identifying an intra-abdominal testis. It is not reliable enough to lead to alterations in planning (23). When assessing the palpable testis, sonography will report it as abnormal up to 84% of the time, and in a further 10% the contralateral (normal, unreferred) side will be reported as abnormal – presumably due to the cremasteric reflex (24). It’s not clear to us ultrasound scanning leads to any alteration in referral or pre-operative planning, but it can precipitate caregiver concerns regarding fertility and cancer risk. We found numerous occasions when families fixated on the (falsely positive) ultrasound scan over the clinical demonstration of a normally descended testis.
Age at referral was higher than ideal in our cohort, and did not significantly decrease over the years. This is a common finding in the literature, with a number of studies demonstrating a minority of children are referred by six months of age (thus allowing enough lead-time for an orchidopexy prior to one year of age) (25–29). Education campaigns and guidelines appear to have variable impact (22, 27, 28, 30). It’s possible parents may be a resource to initiate referral, and there are surveys of parental opinions that may be used to produce education packages (31). Secondary testicular ascent (acquired undescended testis) is a real phenomenon that may partially explain the older age at referral. It is difficult to determine its relative contribution to the commonly observed bimodal distribution of orchidopexies, and thus we have no way of knowing what proportion of these older children previously had scrotal testes (32, 33).
We observed a significant decrease in median wait times for orchidopexy in our cohort (Figure 2). Prior to 2015 the median wait time for each year was approximately 25-27 weeks. From 2016 onwards it significantly decreased to 10-14 weeks. 2015 appeared to be a transition year (median wait 19 weeks). At the end of 2014 two existing smaller children’s hospitals in Brisbane (the Royal Children’s Hospital and Mater Children’s Hospital) amalgamated into a new single hospital, the Queensland Children’s Hospital. Although all paediatric surgeons worked at both hospitals, only the Royal Children’s Hospital was providing Telehealth services and all patients booked from Telehealth were booked into this single facility. The decrease in waiting times correlates with the move to a single facility (though with no increase in paediatric surgeons) so it appears an economy of scale effect is visible here. The COVID-19 pandemic does not appear to have had an appreciable effect on waiting times, perhaps because Queensland Children’s Hospital, and Queensland more generally, were not subject to the same lockdowns and decrease in services seen in other states or countries.
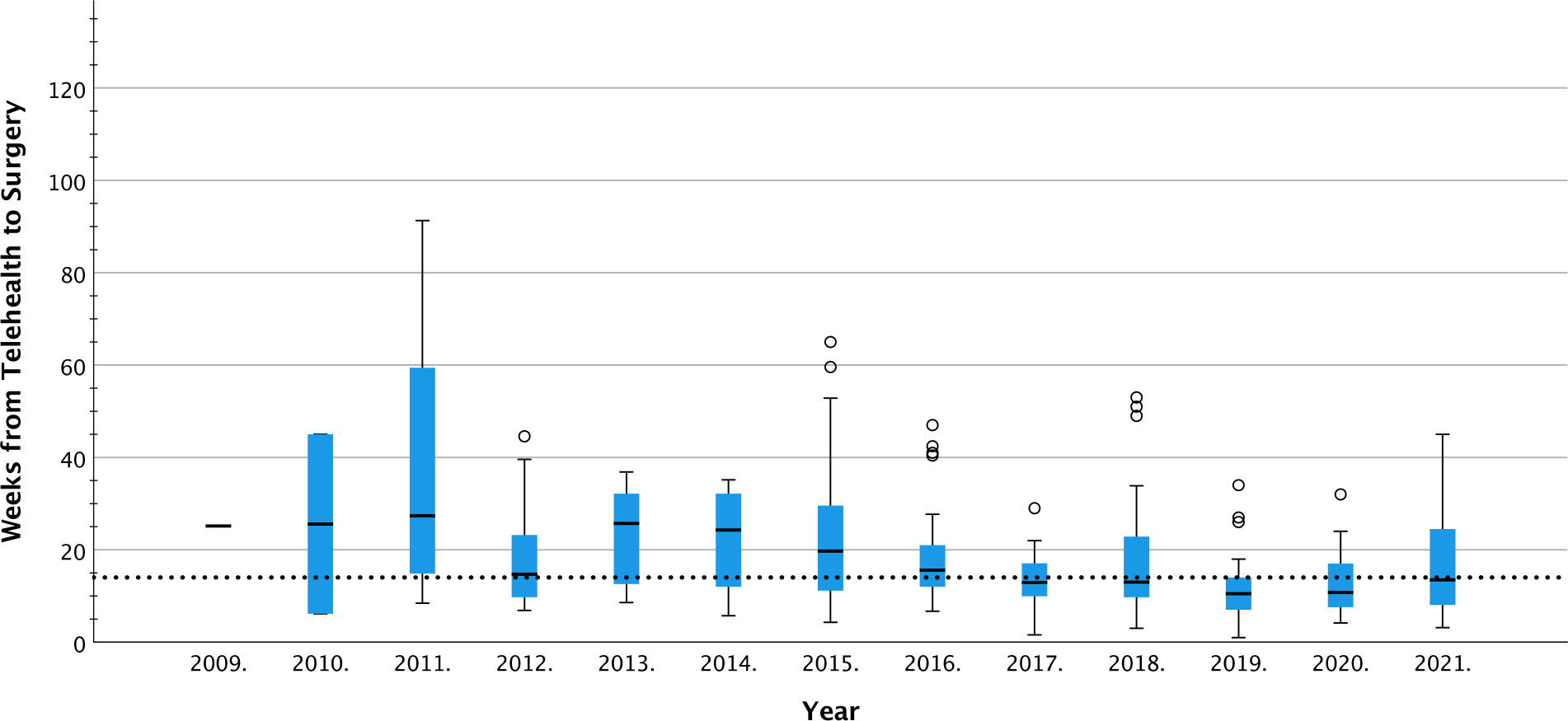
Figure 2 Tukey box plot of time delay (weeks) between Telehealth booking and surgery, by year of first Telehealth appointment. p = 0.01 (independent samples median test) Dotted line = cohort median.
In our cohort there was a ~20% chance an operation would be cancelled. This is not a high enough figure to deliberately overbook a list in expectation of cancellation. Those families cancelled on the day would otherwise have had to come to Brisbane for assessment if we did not have a Telehealth facility available, so there is no saving for them in terms of travel.
Travel distances for families were assessed as the single round-trip travel distance between Queensland Children’s Hospital and the Telehealth appointment site, (usually the nearest hospital or GP practice to the family home). For some families, travel of 100km or more is required even to attend a Telehealth appointment ‘close’ to home. These distances were not included in our calculations, but families still had a median round trip distance of nearly 1000km. Our intention is to save this travel time and cost as much as possible for distant families, by streamlining appointments to (ideally) one physical visit only. A preliminary Telehealth discussion enables the family to meet the surgical team, and for the team to discuss the importance of orchidopexy.
The facility the patients were seen at is not necessarily the referring facility, but is rather the closest appropriate facility to the family home. There was therefore no reason to expect any correlation between accuracy and facility. Despite the apparent wide discrepancy in accuracy at various originating sites (Supplementary Table 1), there was no statistically significant association between originating site and accuracy. This held true even after grouping sites by number of patients seen (1-3, 4-9, 10 or more) over the time of this study. A small number of patients were seen in their homes (seven) so no comments can be made in this regard. Patients referred by Paediatricians were more likely to proceed to operation than patients referred by GPs, suggesting it is the referrer rather than the facility that is a more important predictor. Numbers of other referrers (Neonatologist, Urologist, Emergency Physician) were too small to permit analysis regarding accuracy of referral.
There is a tension between disruption to lists, and disruption to families, that preliminary telehealth can only partially offset. While there are indicators, there is no constellation of findings convincing enough to be able to know a child will either definitely need an operation or can definitively be reassured. Preliminary assessment through a local paediatric clinic is more suggestive of a need for operation; ‘bilateral UDT’ is more suggestive of normal descent.
Limitations
The main limitation of this study relates to diagnosis. Examination by a senior member of the paediatric surgical team has been taken as the gold standard, for the purposes of this study. Orchidopexy rates greater than the expected incidence of UDT (~1%) have been previously reported, suggesting this gold standard may not always be accurate (34). Testicular descent is not an ‘all or nothing’ phenomenon – a mid-scrotal testis with a marginally tight cord may be acceptable to one surgeon but not to another. Similarly, we also acknowledge the possibility boys with normal or retractile testes received an operation. A fasted patient from far away, and an operating list with a booking on it, are a powerful incentive to proceed – particularly in light of family and local General Practitioner expectations. A number of our patients cancelled on the day were subsequently re-referred by the same or a different GP. In most cases the patient was again examined and reassured, but a small number had an orchidopexy performed. There is no way of knowing if this was for an ascending testis, a missed UDT at first examination, or a normal testis being pexed to alleviate anxiety. Families sometimes requested an operation anyway, given the disruption already caused. It’s beyond the scope of this project to question the appropriateness of acquiescing to this request, but it’s probable this occurred for a proportion of this cohort. Scrotal (Bianchi) orchidopexies were performed for 10.7% of this cohort, and 13 patients had bilateral scrotal orchidopexies. This figure is lower than series published from institutions where this approach is an accepted part of practice (35–37). There was no association shown between distance from the hospital, and likelihood of proceeding to orchidopexy. The fact numerous patients did not receive an operation indicates a willingness to not proceed among our surgical group. We do however acknowledge the probability some children with normally descended testes had an orchidopexy performed. We may be able to mitigate this risk by further separating the pre-operative examination from the operation itself. Given the distances our patients travel, many arrive in Brisbane the day prior to planned operation. We are now preferencing examination the day prior to planned operation. That way, an unnecessary fasting period is avoided for a child, and it potentially gives time for us to replace the cancelled operation with a local patient from our waiting list. It also enables the family to return home early the following day.
There are several groups not captured in this study. We have no way of knowing if GPs are using ultrasound scanning to augment uncertain examination findings, and subsequently not referring patients with normal scans. If that is the case, then it could be argued from a GP perspective ultrasound scanning has some utility.
We have assumed those patients discharged following Telehealth review had normal testes. It is tempting to assume bilateral palpable scrotal testes are normal, whoever may be examining them. However, our initial cohort included one patient initially identified as normal who subsequently went on to have bilateral two-stage laparoscopic orchidopexies for intra-abdominal testes (9). This single case made us less willing to discharge patients from Telehealth, unless they had been seen repeatedly and found to have normally descended testes. Discharges from Telehealth in the later years of the cohort are infrequent and now occur only after face-to-face review by a Paediatric Surgeon or Paediatrician.
Interpretation
Telehealth is not accurate for assessing descent of the testis. There are identified factors that increase the likelihood of an operation not proceeding, but they are not sufficiently powerful to be able to replace face-to-face examination. Ultrasound scanning offers no increased utility, and can lead to inappropriate parental distress. An initial Telehealth appointment introduces the family to the surgical team and offers counselling and consent for the procedure. It also provides an opportunity to explain the importance of a potentially disruptive trip to Brisbane for a day case procedure. Pre-operative face-to-face assessment is vital. Assessing patients the day prior to their operation may allow further efficiencies in terms of operating list bookings, while also minimising potential disruption to families and children.
Despite these challenges, Telehealth still has utility in assessing children with potential disorders of testicular descent. For four out of five families care will be streamlined with a single visit only to Brisbane rather than two. The fifth family will already have been alerted to the possibility of, and reasons underpinning, their cancellation. They will also have had a single trip to Brisbane, with the addition of a fasting period for their child.
Generalisability
The Australian paediatric population is distributed over vast areas, with significant distances to travel to see a paediatric surgeon outside of major metropolitan centres. In countries with more ready access to a paediatric surgeon, or a paediatrician, Telehealth may not afford any additional benefit in the assessment of UDT. Centres considering using telehealth for cryptorchidism need to balance probable list disruption against family disruption. Our ideal solution in Queensland is to have a paediatrician at the originating site examine the child, with a paediatric surgeon online at the same time. We are working currently to achieve this.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
This study, involving human participants, was reviewed and approved by the Children’s Health Queensland Human Research Ethics Committee (HREC/17/QRCH/143). Written informed consent from the participants’ legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author contributions
CM and BP are responsible for the concept, and for drafting the protocol. All authors contributed to data collection. CM was primarily responsible for statistical analysis. CM and BP drafted the manuscript. All authors have contributed to editing and approving the final manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fruro.2022.993528/full#supplementary-material
Supplementary Table 1 | Referral centres, and outcomes, for patients referred with cryptorchidism.
References
1. Shivji S, Metcalfe P, Khan A, Bratu I. Pediatric surgery telehealth: patient and clinician satisfaction. Pediatr Surg Int (2011) 27(5):523–6. doi: 10.1007/s00383-010-2823-y
2. Inumpudi A, Srinivas M, Gupta DK. Telemedicine in pediatric surgery. Pediatr Surg Int (2001) 17(5–6):436–41. doi: 10.1007/s003830000528
3. Miller GG, Levesque K. Telehealth provides effective pediatric surgery care to remote locations. J Pediatr Surg (2002) 37(5):752–4. doi: 10.1053/jpsu.2002.32270
4. Smith AC, Youngberry K, Mill J, Kimble R, Wootton R. A review of three years experience using email and videoconferencing for the delivery of post-acute burns care to children in Queensland. Burns (2004) 30(3):248–52. doi: 10.1016/j.burns.2003.11.003
5. Smith AC, Youngberry K, Christie F, Isles A, McCrossin R, Williams M, et al. The family costs of attending hospital outpatient appointments via videoconference and in person. J Telemed Telecare (2003) 9 Suppl 2(2_suppl):S58–61. doi: 10.1258/135763303322596282
6. Smith AC, Scuffham P, Wootton R. The costs and potential savings of a novel telepaediatric service in Queensland. BMC Health Serv Res (2007) 7(1):35. doi: 10.1186/1472-6963-7-35
7. Postuma R, Loewen L. Telepediatric surgery: capturing clinical outcomes. J Pediatr Surg (2005) 40(5):813–8. doi: 10.1016/j.jpedsurg.2005.01.049
8. Smith AC, Garner L, Caffery LJ, McBride CA. A review of paediatric telehealth for pre- and post-operative surgical patients. J Telemed Telecare (2014) 20(7):400–4. doi: 10.1177/1357633X14552373
9. Brownlee GL, Caffery LJ, McBride CA, Patel B, Smith AC. Telehealth in paediatric surgery: Accuracy of clinical decisions made by videoconference. J Paediatr Child Health (2017) 190:15. doi: 10.1111/jpc.13599
10. Snodgrass W, Bush N, Holzer M, Zhang S. Current referral patterns and means to improve accuracy in diagnosis of undescended testis. Pediatrics (2011) 127(2):e382–8. doi: 10.1542/peds.2010-1719
11. Moslemi MK. Evaluation of orchiopexy practice patterns in patients with cryptorchidism: a single-centre study. J Pediatr Urol (2014) 10(2):230–2. doi: 10.1016/j.jpurol.2013.08.009
12. de Vries AM, Hack WWM, Heij HA, Meijer RW. Perioperative surgical findings in congenital and acquired undescended testis. J Pediatr Surg (2010) 45(9):1874–81. doi: 10.1016/j.jpedsurg.2010.02.121
13. Braga LH, Lorenzo AJ, Romao RLP. Canadian Urological association-pediatric urologists of Canada (CUA-PUC) guideline for the diagnosis, management, and followup of cryptorchidism. Can Urol Assoc J (2017) 11(7):251–60. doi: 10.5489/cuaj.4585
14. Ritzén EM, Bergh A, Bjerknes R, Christiansen P, Cortes D, Haugen S, et al. Nordic Consensus on treatment of undescended testes. Acta Paediatr (2007) 96(5):638–43. doi: 10.1111/j.1651-2227.2006.00159.x
15. Kolon TF, Herndon CDA, Baker LA, Baskin LS, Baxter CG, Cheng EY, et al. Evaluation and treatment of cryptorchidism: AUA guideline. J Urol (2014) 192(2):337–45. doi: 10.1016/j.juro.2014.05.005
16. Niedzielski JK, Oszukowska E, Słowikowska-Hilczer J. Undescended testis – current trends and guidelines: a review of the literature. Arch Med Sci Ams (2016) 12(3):667–77. doi: 10.5114/aoms.2016.59940
17. British Association of Pediatric Surgeons (BAPS), British Association of Urologic Surgeons (BAUS), Royal College of Surgeons of England (RCS). Commissioning guide: paediatric orchidopexy for undescended testis. Lincoln's Inn Fields, London: British Association of Pediatric Surgeons (BAPS), British Association of Urologic Surgeons (BAUS), Royal College of Surgeons of England (RCS) (2015).
18. Radmayr C, Dogan HS, Hoebeke P, Kocvara R, Nijman R, Silay S, et al. Management of undescended testes: European association of Urology/European society for paediatric urology guidelines. J Pediatr Urol (2016) 12(6):335–43. doi: 10.1016/j.jpurol.2016.07.014
19. Selvarajah D, McDowell D, Jehangir S, Smith G. Unnecessary ultrasound imaging in the management of undescended testis. Med J Australia (2021) 215(11):528–8. doi: 10.5694/mja2.51324
20. Shin J, Jeon GW. Comparison of diagnostic and treatment guidelines for undescended testis. Clin Exp Pediatr (2020) 63(11):415–21. doi: 10.3345/cep.2019.01438
21. Milford K, Pokarowski M, Chua M, Lorenzo A, Koyle M. Unnecessary ultrasounds in children with undescended testes: An interrogation of the impact of the choosing wisely campaigns and clinical practice guidelines. Paediatr Child Health (2020) 26(5):299–304. doi: 10.1093/pch/pxaa099
22. Carpenter CP, Johnston D, Tourville E, Sharadin C, Alzubaidi AN, Giel DW. Inappropriate imaging for management of cryptorchidism: Has the choosing wisely® recommendation reduced occurrence? J Pediatr Urol (2020) 16(4):462.e1–6. doi: 10.1016/j.jpurol.2020.06.017
23. Tasian GE, Copp HL. Diagnostic performance of ultrasound in nonpalpable cryptorchidism: A systematic review and meta-analysis. Pediatrics (2011) 127(1):119–28. doi: 10.1542/peds.2010-1800
24. Wayne C, Guerra LA, Yao J, Keays MA, Leonard MP. Use of ultrasound for the palpable undescended testis: a wasteful practice. Fam Pract (2017) 35(4):452–4. doi: 10.1093/fampra/cmx128
25. Bearrick EN, Dixon C, Kaplan A, O’Brien S, Radosevich D, Tejpaul R, et al. Referral patterns for undescended testis: A 7 year comparative analysis of primary care providers. J Pediatr Urol (2021) 17(5):736.e1–6. doi: 10.1016/j.jpurol.2021.06.017
26. Point D, Morley C, Tourchi A, Reddy S, Sirisreetreerux P, Gearhart J, et al. Rural versus urban compliance in the management of cryptorchidism: is there a difference? Eur J Pediatr (2017) 176(8):1067–73. doi: 10.1007/s00431-017-2946-4
27. Trump T, Elbakry AA, Haffar A, McClelland D, Morley C, Al-Omar O. The impact of targeted education of American urological association cryptorchidism guidelines in a rural state: Improvement still needed. Res Rep Urol (2021) 13:437–43. doi: 10.2147/RRU.S316563
28. Boehme P, Geis B, Doerner J, Wirth S, Hensel KO. Shortcomings in the management of undescended testis: guideline intention vs reality and the underlying causes – insights from the biggest German cohort. Bju Int (2018) 122(4):644–53. doi: 10.1111/bju.14171
29. Jensen MS, Olsen LH, Thulstrup AM, Bonde JP, Olsen J, Henriksen TB. Age at cryptorchidism diagnosis and orchiopexy in Denmark: A population based study of 508,964 boys born from 1995 to 2009. J Urol (2011) 186(4):1595–600. doi: 10.1016/j.juro.2011.03.070
30. Cho A, Ball M, Read K, Tharmapoopathy P, Ross AR, Mathur A, et al. Educational survey of regional general practitioner’s management of paediatric patients with undescended testis. J Pediatr Urol (2016) 12(3):151.e1–7. doi: 10.1016/j.jpurol.2015.11.010
31. Chung JM, Lee CY, Shin DG, Kang DI, Kim JS, Cho WY, et al. Parental perception of optimal surgical age for correction of cryptorchidism: A multicenter surveillance study. Urology (2011) 78(5):1162–6. doi: 10.1016/j.urology.2011.04.075
32. Stec AA, Thomas JC, DeMarco RT, Pope JC, Brock JW, Adams MC. Incidence of testicular ascent in boys with retractile testes. J Urol (2007) 178(4):1722–5. doi: 10.1016/j.juro.2007.05.091
33. Keys C, Heloury Y. Retractile testes: A review of the current literature. J Pediatr Urol (2012) 8(1):2–6. doi: 10.1016/j.jpurol.2011.03.016
34. Capello SA, Giorgi LJ, Kogan BA. Orchiopexy practice patterns in new York state from 1984 to 2002. J Urol (2006) 176(3):1180–3. doi: 10.1016/j.juro.2006.04.052
35. Rajimwale A, Brant WO, Koyle MA. High scrotal (Bianchi) single-incision orchidopexy: a “tailored” approach to the palpable undescended testis. Pediatr Surg Int (2004) 20(8):618–22. doi: 10.1007/s00383-004-1243-2
36. Dayanç M, Kibar Y, Tahmaz L, Yildirim I, Peker AF. Scrotal incision orchiopexy for undescended testis. Urology (2004) 64(6):1216–8. doi: 10.1016/j.urology.2004.06.069
Keywords: telemedicine, cryptorchidism, paediatric, orchidopexy, undescended testis
Citation: McBride CA, Patel B, Xu E and Bairagi A (2022) Assessing for cryptorchidism via telehealth is not always accurate: A Paediatric cohort study. Front. Urol. 2:993528. doi: 10.3389/fruro.2022.993528
Received: 13 July 2022; Accepted: 12 August 2022;
Published: 31 August 2022.
Edited by:
Julia Beth Finkelstein, Boston Children’s Hospital and Harvard Medical School, United StatesReviewed by:
Stephen Canon, Arkansas Children’s Hospital, United StatesChristopher Long, Children’s Hospital of Philadelphia, United States
Copyright © 2022 McBride, Patel, Xu and Bairagi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Craig A. McBride, Y21jYnJpZGVAcGFlZHN1cmdlcnkuY29t
†These authors have contributed equally to this work and share first authorship
 Craig A. McBride
Craig A. McBride Bhaveshkumar Patel1,2†
Bhaveshkumar Patel1,2† Anjana Bairagi
Anjana Bairagi