
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Urol., 05 October 2022
Sec. Male Urology
Volume 2 - 2022 | https://doi.org/10.3389/fruro.2022.990560
This article is part of the Research TopicMinimally Invasive Techniques in Benign Prostatic Hyperplasia (BPH) SurgeryView all 6 articles
 Jamil Ghahhari1*
Jamil Ghahhari1* Petros Sountoulides1
Petros Sountoulides1 Davide Campobasso2
Davide Campobasso2 Alessio Faieta1
Alessio Faieta1 Francesco Sessa3,4
Francesco Sessa3,4 Lorenzo Viola3
Lorenzo Viola3 Giampaolo Siena5
Giampaolo Siena5 Filippo Cianci6
Filippo Cianci6 Luca Cindolo1,6
Luca Cindolo1,6Objective: In this study, we evaluate the short- and mid-term results of water vapor thermal therapy (WVTT) for LUTS (lower urinary tract symptoms) due to benign prostatic hyperplasia (BPH).
Methods: Patients with LUTS due to BPH who underwent WVTT from September 2019 to April 2022 were included in this prospective, single-center study. Data regarding functional and sexual outcomes were evaluated by validated questionnaires as well as uroflowmetry, urinalysis and cultures, digital rectal examination, serum prostate-specific antigen, and transrectal ultrasound. The patients were followed-up with 3, 6, 12, and 18 months after the procedure.
Results: Eighty-four men were treated. Mean ± SD prostate volume, operative time, and hospital stay were 76.9 ± 26.3 ml, 14 ± 18.5 min, and 0.9 ± 0.7 days, respectively. The catheter was removed after 7 ± 4.4 days. A significant (p < 0.05) improvement in Qmax, IPSS, QoL, OAB-q SF, ICIQ-SF, and IIEF- 5 from the baseline at the last follow-up (18 months) was recorded. Seventy-six (90%) patients reported a significant improvement in ejaculatory function (de novo dry ejaculation in 4 patients). Early (≤30 days) postoperative complications were reported in 70% of patients, all grade 1 according to Clavien–Dindo. No late (>30 days) Clavien–Dindo >1 procedure-related complications occurred. Three patients required reoperation (6–12 months after surgery).
Conclusion: WVTT is an effective and safe treatment for the management of LUTS due to BPH in the short- and mid-term follow-up, and it provides negligible sequelae with respect to ejaculation.
Lower urinary tract symptoms (LUTS), secondary to benign prostatic hyperplasia (BPH), and subsequent bladder outlet obstruction (BOO) have a significant negative impact on the quality of life of an increasing number of elderly male patients worldwide (1). Approximately 15 million patients in the USA suffer from obstructive LUTS, 80% of whom are over 70 years of age (1).
Although pharmacotherapy with either alpha 1-blockers, 5-ARIs (5-alpha-reductase inhibitors), or combination is usually the first line of therapy, there is a limit to what drugs can offer in terms of sustained relief of symptoms and avoidance of BPH progression. Surgical treatment is sought when drugs fail to provide the expected benefit or are not tolerated or complications arise due to BPH (2, 3).
However, according to the latest American and European guidelines to date, Transurethral resection of the prostate (TURP), anatomical endoscopic enucleation (AEEP), and open prostatectomy are the recommended surgical standards for a moderate-sized to large prostate (2, 4).
Although TURP and AEEP are highly effective in providing relief from symptoms, they come with side effects that are hardly negligible (ejaculatory dysfunction, stress urinary incontinence, prolonged dysuria, and a small risk of bleeding) (5).
To cover the treatment gap between pharmacotherapy and cavitating prostate surgery, a variety of minimally invasive surgical techniques (MISTs) have been introduced and endorsed in BPH surgery (6, 7).
WVTT delivered via the Rezūm system is one of the most studied options among this new family of MISTs (7, 8). WVTT can be delivered even in the outpatient setting under sedation. WVTT works by delivering stored thermal energy (540 calories/ml H2O) in the form of vapor to the prostatic glandular tissue. The adenoma collagenous pseudocapsule acts as a natural barrier to the convective flow of steam, and this is what allows us to limit the treatment area to the obstructive hyperplastic prostate tissue located in the transition zone (9). As a result, no thermal effects occur outside the transitional zone boundaries. The 5-year data from the multicenter randomized sham-controlled trial confirmed the relief of significant and durable symptoms, flow rate improvement, and low surgical retreatment rates without impacting sexual function (8).
This prospective study aimed to evaluate the short-term results of WVTT via the Rezūm system in a single-center cohort of patients.
From September 2019 to April 2022, data were prospectively gathered from a consecutive series of patients undergoing WVTT (Rezūm system, Boston Scientific, Marlborough, MA, USA) for obstructive and symptomatic LUTS/BPH. Preoperative evaluation included patients’ medical history, evaluation of the degree of symptoms, bother (IPSS) urine cultures, digital rectal examination (DRE), serum prostate-specific antigen (PSA), transrectal prostate ultrasound (TRUS), uroflowmetry (UFM), and post-void residual (PVR).
To assess urinary incontinence, we used the overactive bladder quality-of-life short-form questionnaire (OAB-q SF) (10) and International Consultation on Incontinence Questionnaire-Urinary Incontinence Short Form (ICIQ-UI SF) (11). Sexual function was assessed using the International Index of Erectile Function – Erectile Function (IIEF-EF) (12). The rate of preoperative and postoperative antegrade ejaculation, defined as the emission of semen after orgasm, was subjectively recorded at baseline and during follow-up.
Postoperative Patient Global Impression of Improvement (PGI-I) was assessed according to the PGI-I scale (13). The present study was conducted in accordance with the Standards of Good Clinical Practice and the Declaration of Helsinki, and all patients signed a written informed consent form. Regular follow-up visits were conducted at 3, 6, 12, and 18 months for each patient.
Preoperative and postoperative parameters were compared and statistically analyzed at the 5% level of significance. Data normality was tested using the Shapiro-Wilk test. The paired t-test was used for normally distributed data, and the Wilcoxon paired test was used for the others (PVR, PSA).
Results were evaluated using IBM® SPSS® Statistics Version 27.
All procedures were performed by the same surgeon (LC). Patients were under sedation throughout the procedure. The procedure started with a rigid cystoscopy and evaluation of the size and contour of the prostate. The Rezūm device was inserted transurethrally, and the prostate was treated with WVTT energy delivered through injections at specific sites on the prostate. Each injection of water vapor lasted for 9 sec. The number of treatments varied depending on the size of the gland and the presence of a median lobe. At the end of the procedure, an 18-20 Ch Foley bladder catheter was placed. The removal of the catheter was usually fixed seven days from its placement. In four patients a temporary prostatic stent (Exime®, Rocamed 9, Avenue Albert II MC 98000 Monaco, France). was placed instead of a bladder catheter (14). Alpha-blocker medication was maintained for another 3 weeks after catheter removal.
Eighty-four patients were included in the study. In total, eight (9.5%) patients were on retention at the time of the procedure. All patients were under medical treatment for LUTS caused by BPH—alpha-blocker (48%), 5ARI (7%), or a combination of these (45%). The characteristics of the study population are reported in Table 1.
The mean operative time was 14.7 ± 7.9 minutes. Two patients required concomitant urethrotomy for urethral stricture to accommodate the device, one patient underwent endoscopic resection of an incidental bladder tumor, and another underwent removal of a bladder stone. The procedure was performed in the outpatient setting and all patients were discharged on the same day, but in eight cases the hospital stay was prolonged due to concomitant surgical procedures or for administrative reasons. Fifty-three (63%) patients presented with a median lobe. The bladder catheter was removed after 7 ± 4.4 days Compared with the baseline, Qmax showed a significant increase at 3, 6, 12, and 18 months after surgery (p < 0.001; Table 2A; Figure 1). IPSS and QoL also improved significantly from baseline at 3, 6, 12, and 18 months (p < 0.001; Table 2A; Figure 1).
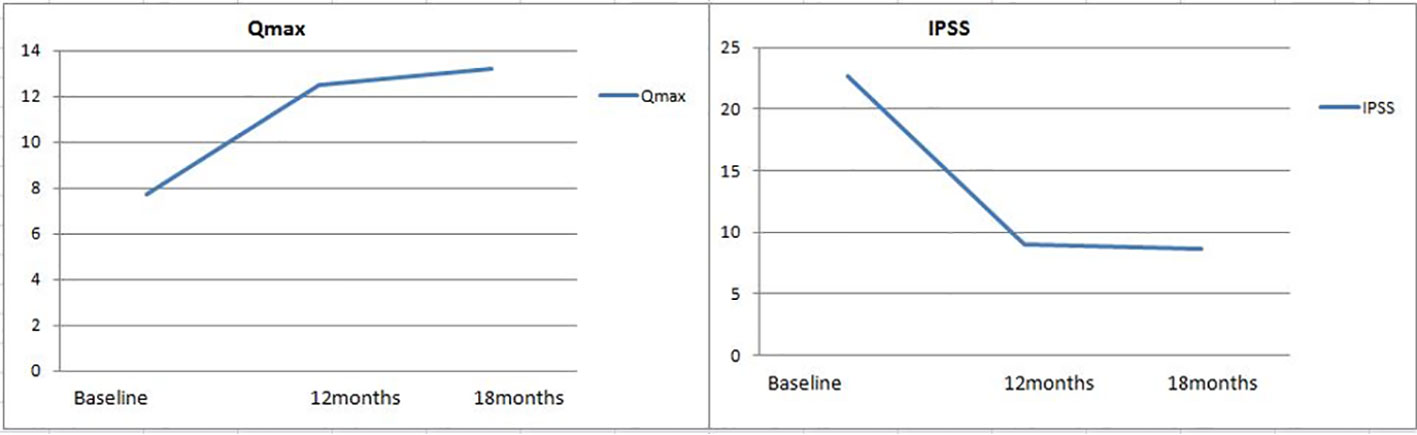
Figure 1 Variation over time of functional outcomes after Rezūm. Qmax, maximum flow rate; IPSS, International Prostate Symptom Score.
For the OAB-q SF and ICIQ-UI SF, substantial reductions emerged at the 12- and 18-month follow-ups that were statistically significant for the OAB-q SF (p < 0.001) but not for ICIQ (Table 2B). An improving trend was also highlighted in the early postoperative period and at 12-18 months after treatment (Table 2B). De novo dry ejaculation was noted in four (4.7%) patients after treatment. No intraoperative complications were reported.
Early postoperative complications were reported in 59 patients (70%), with the vast majority being grade 1 according to the Clavien–Dindo classification—mostly dysuria, nocturia, hematuria, urgency, and burning sensation on urination. Eight patients (9.5%) suffered from acute urinary retention (AUR) following a trial without catheter (TWOC) with the need for bladder drainage for some additional days. At the next TWOC, six patients achieved spontaneous urination while for the remaining two patients, it was necessary to wait additional three weeks until spontaneous urination occurred. Four patients (4.7%) had a UTI (urinary tract infection) treated with antibiotics. One patient had a late episode of gross hematuria with clot retention requiring hospitalization 28 days after the procedure. No late (>30 days from surgery) Clavien >1 complications occurred. In 14% of the cases, the following adverse events occurred: persistent mild to severe dysuria, occasional hematuria, hematospermia, decrease in ejaculatory volume, weak flow, or nocturia. One subject had a bladder stone in a diverticulum 6 months after the procedure.
Three patients (3.5%) underwent surgical retreatment within the first year due to persistent or deteriorating symptoms. One patient was treated by the same surgeon with a transurethral incision of the prostate. Two patients underwent robot-assisted simple prostatectomy (RASP) and TURP elsewhere, with preoperative prostate volumes of 90 and 140 ml, respectively.
Patient Global Impression of Improvement (PGI-I) at the last control (18 months) showed 76 patients confirming a slight to significant improvement after treatment (90.5%), whereas 8 patients (9.5%) reported their condition as unmodified or worsened.
At the 18-month follow-up, prostate size showed a clear reduction of 30% (from 76.9 ± 26 to 54.5 ± 23.1 ml, p < 0.001). A similar trend of reduction was also observed for PSA at the last follow-up (a reduction from 3.5 ± 2.1 to 2 ± 2.2 ng/ml, p < 0.001).
Newer MISTs for the treatment of BPH-related LUTS are effective, safe, and attractive, in terms of maintaining ejaculation (12, 13). Temporary implantable nitinol device (iTIND), prostatic urethral lift (PUL), and convective water vapor energy ablation system (Rezūm system) are non-excisional, alternative ablative minimally invasive procedures with many studies published in the last decade (15–17).
The Rezūm system is a nonobstructive technique that achieves its purpose through the delivery of thermal energy in the form of water vapor injections onto the prostatic adenoma leading to cell necrosis while preserving sexual function and ejaculation, in an outpatient setting (8, 14, 18). This last point should not be underestimated in the COVID-19 era (19, 20).
The European Association of Urology (EAU) guidelines consider the Rezūm system an alternative ablative technique under investigation while acknowledging the controversial findings of two recent systematic reviews and the absence of randomized controlled trials (RCTs) versus a standard reference technique (2). On the other hand, the American Urological Association (AUA) guidelines recommend the Rezūm system for patients with LUTS attributed to BPH and a prostate volume <80 g (moderate recommendation; LE Grade C) who desire preservation of erectile and ejaculatory function (conditional recommendation; LE Grade C) (5).
Our study evaluated the early and mid-term functional outcomes of patients treated with the Rezūm system in a single center in real-life conditions. In accordance with the latest published data in the literature, Rezūm provided a significant improvement in uroflowmetry parameters and IPSS scores at the last follow-up (19–22). Furthermore, a significant improvement was noted in storage symptoms (a greater reduction in OAB-SF scores and a mild reduction in ICIQ-UI SF scores at the 18-month follow-up). Finally, a trend for improvement was also shown in sexual and ejaculatory function, mirrored in the IIEF-5 questionnaire, at the end of the follow-up.
The first Italian multicentric study released early results of 135 patients treated with the Rezūm system at 5 different institutions (19). The authors reported significant improvement in IPSS scores at 1, 3, and 6 months after the procedure, with a net gain of 17 points from the baseline. Furthermore, a mild to significant reduction of storage symptoms was seen, and significant improvement was also noted in sexual function with a substantial increase of IIEF-5 scores 6 months after intervention. Our data showed a progressive reduction in IPSS scores, with a stable 14-point improvement at the last follow-up (from 22.7 ± 6.2 to 8.7 ± 4.5 points at 18 months, p < 0.001). A significant improvement was noted in storage symptoms as well, which is mirrored in both the OAB-q SF and the ICIQ-UI SF scores (from 57.7 ± 17.1 to 18 ± 6, p < 0.001, and 2.7 ± 3.9 to 1.6 ± 0.5, p < 0.045, respectively). In the evaluation of sexual function, we observed an improvement in IIEF-5 scores (from 17.6 ± 7.1 at baseline to 22 ± 3.5 points at the 18-month follow-up) with only 3 (3.5%) patients complaining of de novo dry ejaculation after Rezūm treatment. Those results are in line with this multicentric analysis and also confirm those of the McVary studies (8, 23).
The retreatment rate was 2.2% at the 1-year follow-up, in the McVary and Siena studies (8, 19). In our series, we found a retreatment rate of 3.57% at 18 months. This percentage is slightly higher than that presented by McVary, perhaps in relation to the greater average prostate volume, and it probably mirrors the real-life setting where more and more patients consider Rezūm to tackle LUTS while preserving antegrade ejaculation.
In our hands, the Rezūm system showed a very safe and effective profile, already highlighted in the recent systematic review and meta-analysis (9, 15, 17, 23–25). All the revisions available in the literature demonstrated that adverse events associated with Rezūm were minor, and the sexual dysfunction was minimal. This may be due to the minimally invasive nature of Rezūm’s convective heat transfer (9, 15, 17, 23–25). In our experience, we observed a rate of 70% in early AEs, all of them Clavien–Dindo grade I, which resolved within 3-4 weeks with adequate conservative measures. No late (>30 days from surgery) Clavien–Dindo >1 complications occurred.
We have to acknowledge some limitations of the present study. First is the retrospective design of the study with the limited number of patients included in the analysis. The monocentric nature could be seen as a limitation; however, it reflects real-life practice. Another possible limitation is the reliability of the data concerning the preservation of ejaculation, as our results relied on subjective patient evaluations.
Although the Rezūm procedure continues to gain popularity and acceptance from patients and urologists alike, further studies with larger sample sizes, longer follow-ups, and a randomized design comparable to other techniques or treatments are needed. Moreover, a trend toward expanding the standard indications to other clinical scenarios (such as patients with prostates >80cc, urinary retention, stones, urethral stenosis) should also be addressed in future trials (26), in view of the fact that model-based economic evaluations have demonstrated that this technique is an effective and cost-saving procedure and may also be an appropriate first-line alternative to pharmacotherapy for moderate-to-severe LUTS/BPH patients (27).
Rezūm is a promising MIST ejaculation-sparing treatment that has demonstrated excellent tolerability, safety, and efficacy in the short and medium term with a negligible rate of major complications and an acceptable retreatment rate. Further studies of greater statistical power are needed to confirm these preliminary data and possibly expand current indications.
The raw data supporting the conclusions of this article will be made available by the authors without undue reservation.
Ethical review and approval were not required for this study on human participants in accordance with local legislation and institutional requirements. The patients/participants provided their written informed consent to participate in this study.
JG, PS, and LC contributed to the conception and design of the study. DC and LV organized the database. AF performed the statistical analysis. GS and LC wrote the first draft of the manuscript. FS, FC, LV, and DC wrote sections of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version
LC does surgical proctorship for Rezūm procedures.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Egan KB. The epidemiology of benign prostatic hyperplasia associated with lower urinary tract symptoms: Prevalence and incident rates. Urol Clin North Am (2016) 43:289. doi: 10.1016/j.ucl.2016.04.001
2. Gravas S, Cornu JN, Gacci M, Hashim H, Herrmann TRW, Malde S, et al. EAU guidelines on management of non-neurogenic Male lower urinary tract symptoms (LUTS), incl. benign prostatic obstruction (BPO). In: EAU guidelines. Arnhem: The Netherlands: EAU Guidelines Office (2021). p. 1–112.
3. Cindolo L, Pirozzi L, Fanizza C, Romero M, Tubaro A, Autorino R, et al. Drug adherence and clinical outcomes for patients under pharmacological therapy for lower urinary tract symptoms related to benign prostatic hyperplasia: population-based cohort study. Eur Urol (2015) 68(3):418–25. doi: 10.1016/j.eururo.2014.11.006
4. Parsons JK, Barry MJ, Dahm P, Köhler TS, Lerner LB, Wilt TJ, et al. Surgical management of lower urinary tract symptoms attributed to benign prostatic hyperplasia: AUA guideline amendment 2020. J Urol (2020) 204(4):799–804. doi: 10.1097/JU.0000000000001298
5. Cornu JN, Ahyai S, Bachmann A, de la Rosette J, Gilling P, Gratzke C, et al. A systematic review and meta-analysis of functional outcomes and complications following transurethral procedures for lower urinary tract symptoms resulting from benign prostatic obstruction: An update. Eur Urol (2015) 67(6):1066–1096. doi: 10.1016/j.eururo.2014.06.017
6. Symeonidis EN, Sountoulides P. Drugs or mechanical devices for obstructive LUTS? Curr Drug Targets (2020) 21(15):1537–49. doi: 10.2174/1389450121666200630111723
7. Mollengarden D, Goldberg K, Wong D, Roehrborn C. Convective radiofrequency water vapor thermal therapy for benign prostatic hyperplasia: A single office experience. Prostate Cancer Prostatic Dis (2018) 21(3):379–85. doi: 10.1038/s41391-017-0022-9
8. McVary KT, Gittelman MC, Goldberg K, Patel K, Shore ND, Levin RM. Final 5-year outcomes of the multicenter randomized sham-controlled trial of rezūm water vapor thermal therapy for treatment of moderate-to-Severe lower urinary tract symptoms secondary to benign prostatic hyperplasia. J Urol (2021) 206(3):715–24. doi: 10.1097/JU.0000000000001778
9. Manfredi C, Arcaniolo D, Spatafora P, Crocerossa F, Fusco F, Verze P, et al. Emerging minimally invasive transurethral treatments for benign prostatic hyperplasia: a systematic review with meta-analysis of functional outcomes and description of complications. Minerva Urol Nephrol (2021) 74(4):389–99. doi: 10.23736/S2724-6051.21.04530-4
10. Groenendijk IM, Scheepe JR, Noordhoff TC, Blok BFM. The validation of the Dutch OAB-q SF: An overactive bladder symptom bother and health-related quality of life short-form questionnaire. Neurourol Urodyn (2019) 38(6):1775–82. doi: 10.1002/nau.24074
11. Grøn Jensen LC, Boie S, Axelsen S. International consultation on incontinence questionnaire - urinary incontinence short form ICIQ-UI SF: Validation of its use in a Danish speaking population of municipal employees. PloS One (2022) 17(4):e0266479. doi: 10.1371/journal.pone.0266479
12. Xi Y, Colonnello E, Ma G, Limoncin E, Ciocca G, Zhang H, et al. Validity of erectile function assessment questionnaires in premature ejaculation patients: A comparative study between the abridged forms of the international index of erectile function and proposal for optimal cutoff redefinition. J Sex Med (2021) 18(3):440–7. doi: 10.1016/j.jsxm.2020.11.018
13. Hossack T, Woo H. Validation of a patient reported outcome questionnaire for assessing success of endoscopic prostatectomy. Prostate Int (2014) 2:182–7. doi: 10.12954/PI.14066
14. Cindolo L, Ferrari R, Rabito S, Siena G, Spatafora P, Ferrari G. Rezum procedure with exime® stent: a step forward to micro-invasiveness. Minerva Urol Nephrol (2021) 73(3):273–5. doi: 10.23736/S2724-6051.21.04316-2
15. Suarez-Ibarrola R, Miernik A, Gratzke C, Schoeb DS. Reasons for new MIS. let's be fair: iTIND, urolift and rezūm. World J Urol (2021) 39(7):2315–27. doi: 10.1007/s00345-020-03453-z
16. Sokolakis I, Pyrgidis N, Russo GI, Sountoulides P, Hatzichristodoulou G. Preserving ejaculation: A guide through the landscape of interventional and surgical options for benign prostatic obstruction. Eur Urol Focus (2022) 8(2):380–3. doi: 10.1016/j.euf.2022.03.008
17. Tanneru K, Jazayeri SB, Alam MU, Kumar J, Bazargani S, Kuntz G, et al. An indirect comparison of newer minimally invasive treatments for benign prostatic hyperplasia: A network meta-analysis model. J Endourol (2021) 35(4):409–16. doi: 10.1089/end.2020.0739
18. Couteau N, Duquesne I, Frédéric P, Thiounn N, Timsit MO, Mejean A, et al. Ejaculations and benign prostatic hyperplasia: An impossible compromise? A comprehensive review. J Clin Med (2021) 10(24):5788. doi: 10.3390/jcm10245788
19. Siena G, Cindolo L, Ferrari G, Maruzzi D, Fasolis G, Condorelli SV, et al. Water vapor therapy (Rezūm) for lower urinary tract symptoms related to benign prostatic hyperplasia: early results from the first Italian multicentric study. World J Urol (2021) 39(10):3875–80. doi: 10.1007/s00345-021-03642-4
20. Rocco B, Sighinolfi MC, Sandri M, Altieri V, Amenta M, Annino F, et al. The dramatic COVID 19 outbreak in Italy is responsible of a huge drop of urological surgical activity: a multicenter observational study. BJU Int (2021) 127(1):56–63. doi: 10.1111/bju.15149
21. Cantrill CH, Zorn KC, Elterman DS, Gonzalez RR. The rezūm system–a minimally invasive water vapor thermal therapy for obstructive benign prostatic hyperplasia. Can J Urol (2019) 26:9787–93.
22. Dixon CM, Cedano ER, Pacik D, Vit V, Varga G, Wagrell L, et al. Two-year results after convective radiofrequency water vapor thermal therapy of symptomatic benign prostatic hyperplasia. Res Rep Urol (2016) 8:207–16. doi: 10.2147/RRU.S119596
23. Cocci A, Bocchino AC, Cito G, Lisa A, Russo GI, Giudice AL, et al. Role of rezum in the treatment of benign prostate hyperplasia: A review of the literature. Turk J Urol (2021) 47(6):452–60. doi: 10.5152/tud.2021.21128
24. Babar M, Loloi J, Tang K, Syed U, Ciatto M. Emerging outcomes of water vapor thermal therapy (Rezum) in a broad range of patients with lower urinary tract symptoms secondary to benign prostatic hyperplasia: A systematic review. Low Urin Tract Symptoms (2022) 14(3):140–54. doi: 10.1111/luts.12435
25. Arezki A, Sadri I, Couture F, Schwartz R, Nguyen DD, Zakaria AS, et al. Reasons to go for rezūm steam therapy: an effective and durable outpatient minimally invasive procedure. World J Urol (2021) 39(7):2307–13. doi: 10.1007/s00345-020-03457-9
26. Cindolo L, Campobasso D, Ferrari G, Cicione A, De Nunzio C. Expanding indications for rezum procedure. Urol Video J (2022) 14. doi: 10.1016/j.urolvj.2022.100154
Keywords: benign prostatic hyperplasia, water vapor thermal therapy, Rezūm, minimally invasive surgical treatment, lower urinary tract symptoms
Citation: Ghahhari J, Sountoulides P, Campobasso D, Faieta A, Sessa F, Viola L, Siena G, Cianci F and Cindolo L (2022) Mid-term results of water vapor thermal therapy in patients with lower urinary tract symptoms related to benign prostatic hyperplasia. Front. Urol. 2:990560. doi: 10.3389/fruro.2022.990560
Received: 10 July 2022; Accepted: 12 September 2022;
Published: 05 October 2022.
Edited by:
Afonso Morgado, Centro Hospitalar Universitário de São João (CHUSJ), PortugalReviewed by:
André Silva, University of Porto, PortugalCopyright © 2022 Ghahhari, Sountoulides, Campobasso, Faieta, Sessa, Viola, Siena, Cianci and Cindolo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jamil Ghahhari, amFtaWwuZ2hhaGhhcmlAZ21haWwuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.