
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Urol. , 25 August 2022
Sec. Pediatric, Adolescent and Developmental Urology
Volume 2 - 2022 | https://doi.org/10.3389/fruro.2022.972708
This article is part of the Research Topic Applications of Telehealth in Pediatric Urology View all 8 articles
 Ryan F. Walton1
Ryan F. Walton1 Hans C. Arora1,2
Hans C. Arora1,2 Rachel J. Berkowitz1
Rachel J. Berkowitz1 Ilina Rosoklija1
Ilina Rosoklija1 Earl Y. Cheng1,3
Earl Y. Cheng1,3 Emilie K. Johnson1,3*
Emilie K. Johnson1,3*Research Objective: Telemedicine is now a critical healthcare delivery modality. Prior studies of telemedicine in pediatric urology are lacking parent/patient perspectives. This study aims to assess interest in and factors associated with willingness to participate in telemedicine, and to compare perceptions of telemedicine before and after pandemic-related implementation.
Study Design: This was a cross-sectional study of parents of pediatric urology patients that attended in-person clinic visits (Pre-Telemedicine cohort; January-March 2020) and telemedicine visits (Post-Telemedicine cohort; April-July 2020).
Principal Findings: The response rates were 83.4% (Pre-Telemedicine, N =205) and 32.5% (Post-Telemedicine, N =89). Overall, most parents had a college or graduate level degree (71.9%), private insurance (71.6%), and a plurality were 36-40 years old (30.7%). Their children were mostly white (68.9%), 23.7% were Hispanic/Latino, and the median patient age was 3.3 years (range: 0.1–32.1). There were no demographic differences between the Pre-and-Post-Telemedicine sub-groups.
Pre-Telemedicine: Most (84.3%) were willing to participate in a new, follow-up, or post-operative telemedicine visit. There were no associations between demographics and willingness. Comfort in video visits without a physical exam (3.23% Unwilling vs 38.2% Willing, = <0.001), comfort with technology (22.6% vs 71.6%, p = <0.001), belief that quality of care is similar between telemedicine and in-person visits (3.23% vs 24.0%, p = <0.001), and estimated costs from in-person visits (6.67% vs 30.3%, p = 0.004) were all positively associated with willingness.
Post-Telemedicine: Most indicated that telemedicine met their needs (88.6%), and that they were satisfied with the both the quality of technology used (83%) and the interaction with the urologist (89.9%) during the telemedicine visit.
Comparison of Pre-and-Post-Telemedicine: In reference to the Pre-Telemedicine respondents, Post-Telemedicine respondents more frequently strongly agreed that telemedicine is as private (51.5% vs 77.5%, p = <0.001), secure (49.5% vs 66.3%, p = 0.02), and complete (33.2% vs 51.1%, p = 0.02) as in-person visits.
Conclusions: Most parents had high willingness to participate and positive perceptions of telemedicine prior to the COVID-19 era. Factors associated with willingness were elucidated. Families that participated in telemedicine reduced direct costs and saved time. Lastly, these results suggest that confidence in telemedicine had increased after experience with telemedicine. These data support continued telemedicine access and coverage/reimbursement beyond the pandemic.
The technological advancement and expansion in computer (e.g., phones, tablets, laptops) and internet access has offered a wide variety of possibilities for telehealth, which includes “a collection of means or methods for enhancing the health care, public health, and health education delivery and support using telecommunications technologies,” such as text, audio, video, and audio-video communication between patients, providers, and consultants (1). Telemedicine is one telehealth modality which was initially proposed to address the scarcity of medical care available in rural areas, then expanded to include soldiers on battlefields. More recently, telemedicine has become a prevalent way to meet the elevated demands of densely populated urban and suburban areas (2).
Patients who need a pediatric urologist may benefit from telemedicine because experts within this small specialty are concentrated in urban areas among academic hospitals, which require families to travel long distances—increasing emissions of carbon dioxide and other atmospheric pollutants (3–5)—and incur larger direct costs (e.g., parking, transportation) and indirect costs (e.g., missed school or work) (6). Following the COVID-19 pandemic, telemedicine has also provided safety benefits by limiting opportunities for viral exposure for both patients and healthcare workers. Despite the benefits and dramatic increase in utilization of telemedicine for the past 15 years in primary care and behavioral health, telemedicine utilization in pediatric urology in the United States was uncommonly reported prior to the COVID-19 era (7–11). A variety of potential medical, reimbursement and regulatory, and ethical barriers have been proposed to contribute to this lack of utilization (2, 8, 12). But, in the United States, the driving force for the rapid and widespread utilization of telemedicine—almost overnight—seemed to be contingent on keeping practices financially viable, i.e., 1) the sudden inability to see patients in-person due to stay-at-home orders during the onset of the COVID-19 pandemic and 2) the subsequent financial incentives and relaxed regulations that were provided by the federal government (7, 9). Though there has been a gradual decline in telemedicine utilization among pediatric urologists in the United States since mid-2020 due to the lifting of stay-at-home restrictions and the re-opening of clinic capacities, utilization may still be greater than pre-pandemic levels, as is evidenced at one institution (7), and, if the financial and regulatory incentives for telemedicine remain intact, it is assumed telemedicine will remain a critical healthcare delivery modality in the United States.
Given the lack of utilization of telemedicine among pediatric urologist in the United States prior to the pandemic, there is also relatively little research available on telemedicine within pediatric urology in the United States. In 2018 (pre-COVID), Finkelstein et al. found that that the literature was sparse (13). As of 2022, there are still less than 20 pediatric urology publications (14). Available reviews in pediatric surgery (8), urology (15), and pediatric urology (14) indicate that telemedicine is practical, safe, offers high patient and provider satisfaction, and shows similar clinical outcomes compared with in-person visits. Though prior studies report telemedicine utilization and satisfaction in pediatric urology, parent/patient perspectives have not been comprehensively explored. Thus, this study aimed to: (1) assess parent interest in and factors associated with willingness to participate in telemedicine, and (2) to compare perceptions of telemedicine before and after rapid pandemic-related implementation of this care modality for pediatric urology patients.
This was a two-phase cross-sectional survey study of parents/caregivers (“parents”) of pediatric urology patients. The study was reviewed and considered exempt by the Ann & Robert H. Lurie Children’s Hospital of Chicago Institutional Review Board. Study data were collected and managed using REDCap electronic data capture tools hosted at Northwestern University (16, 17).
The Pre-Telemedicine cohort consisted of parents of pediatric urology patients who attended in-person clinic visits from January 2020 to March 2020 at a freestanding children’s hospital in an urban setting, as well as those that attended ancillary/satellite clinics in suburban settings. Pre-Telemedicine surveys were collected during an in-person clinic visit and were administered by a trained research coordinator.
Following the rapid implementation of telemedicine—in response to the COVID-19 pandemic restrictions on in-person visits—a similar Post-Telemedicine online survey was distributed. During the time period of the Post-Telemedicine group survey, selection criteria for patients to undergo a telemedicine visit was determined by the pediatric urologist, i.e., the default at this time was to offer telemedicine to any visit the pediatric urologist thought was possible to be completed via telemedicine. During the telemedicine visit, physical examinations were performed—unless the visit was audio only. The quality of the exam varied depending on patient age and cooperation of the patient during the visit. Further, a physical examination was not critical for some visits (e.g., follow up for review of imaging results and next steps). The survey was sent to parents via email with an attached REDCap survey link after completing a pediatric urology telemedicine visit from April 2020 to July 2020. Respondents were sent one reminder email with a REDCap survey link attached if they did not complete the survey within 14 days. Participants who did not complete their survey after this reminder email were subsequently called on the telephone and, if interested in taking the online survey, were sent another survey link to the provided email address on file. Only English-speaking families were included.
A multi-page survey was administered to parents: Pre-Telemedicine in-person survey (Appendix 1) and Post-Telemedicine online survey (Appendix 2). For the Pre-Telemedicine sub-group, the dependent variable of interest was willingness to participate in a hypothetical telemedicine appointment (i.e., willing versus unwilling).
Independent variables included demographics (i.e., child age, parent age, race, ethnicity, insurance status, highest educational attainment, self-reported household income), whether the child was a new patient, and location of the clinic visit (Main Campus/Hospital, Satellite Clinic). Prior experience with technology and telemedicine were also assessed, including previous parental participation in a video conference call, possession of a video-enabled device, access to broadband/high-speed internet at home, and whether the parent previously participated in telemedicine for themselves or their child. Appointment burden was assessed by whether the parent missed work for an in-person appointment, whether the child missed school, time and distance traveled to the in-person visit, estimated direct cost related to attending the in-person visit, and total days lost from regular schedule in order to attend an in-person visit. Parents were also asked to report the maximum amount they were willing to pay out-of-pocket for a telemedicine visit for their child.
The following independent variables about attitudes towards telemedicine were measured by level of agreement to a statement via five point Likert-type scale: confident that video visits with a provider can be as (1) private, (2) secure, and (3) complete as in-person visits, comfortable with provider observing a live physical exam via video while it is performed by another provider, comfortable with participating in a video visit without a direct physical exam being performed, comfortable enough with technology to participate in video visits with provider, prefer to see provider over video rather than have the total costs of an in-person visit, e.g., travel, missed work, etc., and belief that the quality of care with a video visit is the same as the quality of care of an in-person visit.
Responses were deidentified and descriptive statistics were performed. Respondent comments at the end of each survey (Pre-Telemedicine and Post-Telemedicine) were qualitatively analyzed via content analysis to determine common themes. Bivariate analysis of Pre-Telemedicine participant responses was performed to determine potential demographics and factors associated with willingness to participate in a hypothetical telemedicine appointment, which was defined based on responses to the following items: 1) Willingness to participate in Telemedicine for Surgical Follow-Up, 2) Willingness to participate in Telemedicine for Return Follow-Up (non-surgical) and 3) Willingness to participate in Telemedicine for New Patient Visit. If any of these (1, 2 or 3) had a response of Very Willing or Somewhat Willing, then the participant was considered “willing.” If none of these variables had a response of Very Willing or Somewhat Willing, then the participant was considered “unwilling.” Attitudes towards telemedicine were also compared between Pre-Telemedicine and Post-Telemedicine sub-groups. Comparisons were completed with bivariate statistics, i.e., Chi-squared test and Student’s t-test or Fisher’s exact test and Mann-Whitney U test when necessary. Statistical analyses were performed using R v3.6.3 (Vienna, Austria).
Pre-Telemedicine in-person surveys were offered to 247 parents and completed by 206 (83.4% response rate). Post-Telemedicine online surveys were successfully sent via email to 274 parents and completed by 89 (32.5% response rate). For the entire cohort (N=295), a plurality of parents were 36-40 years old (30.7%), and most respondents had a college or graduate level degree (71.9%) and had private insurance (71.6%). Their children were mostly White (68.9%), 23.7% were Hispanic/Latino, and the median child age was 3.3 years (range: 0.1-32.1). Across the entire cohort, survey respondents regularly attended 10 different clinic locations, with one location accounting for more than half (54.9%) of completed surveys (Figure 1). Table 1 shows demographics grouped by Pre-Telemedicine and Post-Telemedicine respondents, with no statistically significant differences between sub-groups.
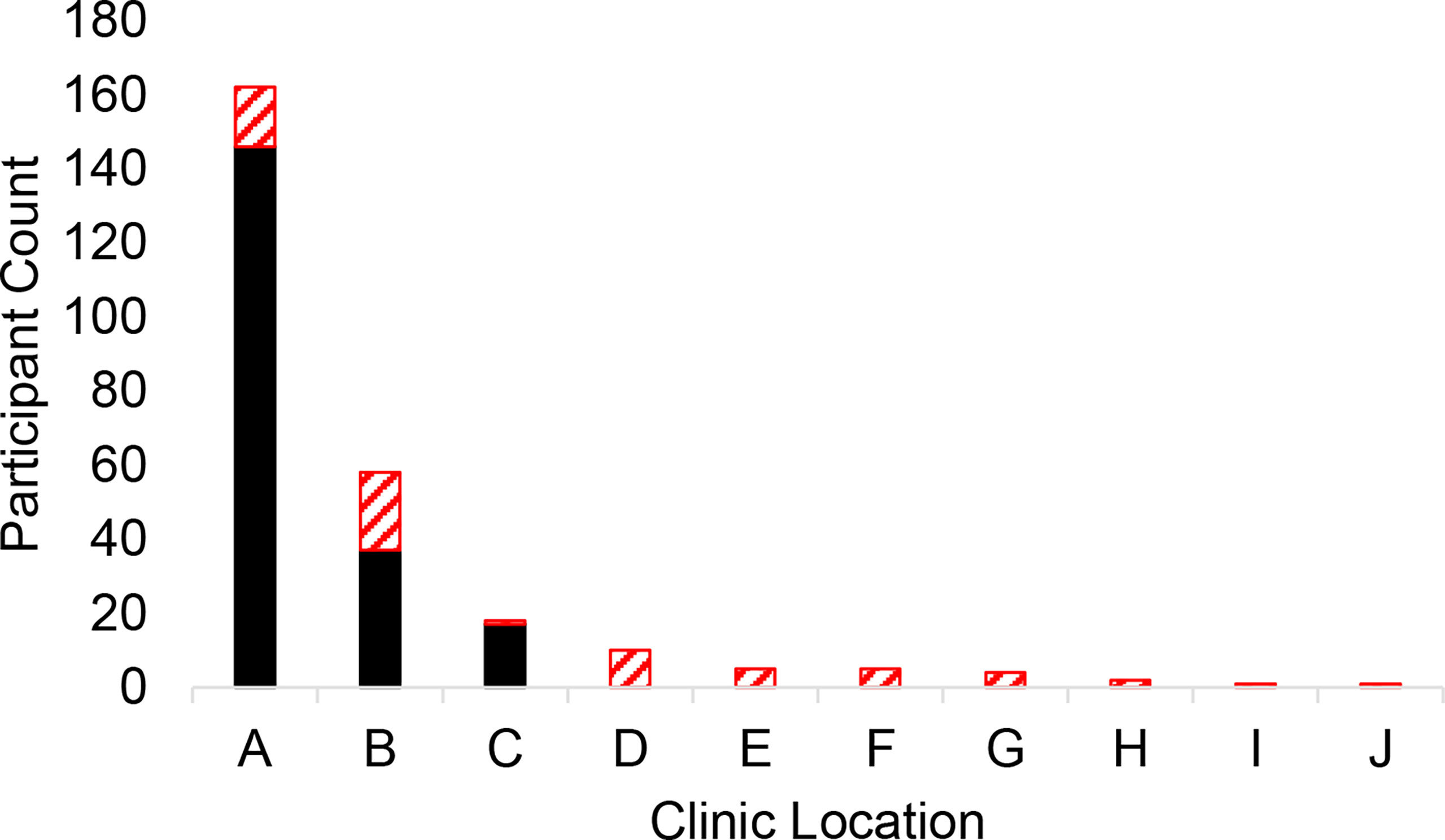
Figure 1 Clinic locations where Pre-Telemedicine Visit participants completed in-person surveys (black) and Post-Telemedicine Visit participants reported as the typical location they attend for in-person visits (red stripes).
Most Pre-Telemedicine survey respondents reported being willing to participate in a hypothetical telemedicine appointment (83.5%), as well as discuss: lab results (93.2%), imaging results (93.2%) and new symptoms (78.2%) via telemedicine. Respondents commonly reported missing work (61.2%) or their child missing school (46.9%) for their day-of in-person visit. Nearly all Pre-Telemedicine respondents had access to high-speed/broadband internet at home (93.7%) and owned a video-enabled device (98.1%). The majority had previous experience with video chat technology (73.8%) and were comfortable enough with technology to participate in telemedicine (87.4%). However, many respondents had reported they did not themselves, or on behalf of their children, have prior experience with telemedicine (90.7% and 94.6%, respectively). Many preferred telemedicine compared to in-person visits to avoid total costs accrued with in-person visits (60.2%), but less than half (49.0%) believed the quality of care with a telemedicine visit was the same as an in-person visit. Respondents commonly reported incurring an estimated direct cost of $10 to $50 from their in-person visit (42.7%), but there were some individuals that reported an estimated direct cost greater than $1000 (2.4%). A plurality reported the estimated travel time to an in-person visit to be 15 to 45 minutes (39.3%).
There were no statistically significant associations found between demographics (including income, insurance, education, and parent age) and willingness to participate in telemedicine (Table 2). Table 3 shows associations between survey responses and willingness to participate in a hypothetical telemedicine visit. Comfort with participating in a video visit without a direct physical exam being performed (3.23% Unwilling vs 38.2% Willing, p=<0.001), comfort with technology (22.6% vs 71.6%, p=<0.001), belief that quality of care is similar between telemedicine and in-person visits (3.23% vs 24.0%, p=<0.001), and estimated direct costs from the in-person visit at time of survey completion (6.67% vs 30.3%, p=0.004) were all positively associated with willingness. Past participation in telemedicine—either for the parent or on behalf of the parent’s child—was not statistically significantly associated with willingness. Missed work or school, access to broadband/high-speed internet access at home, distance traveled to in-person visit, and travel time to the visit were also not associated with willingness.
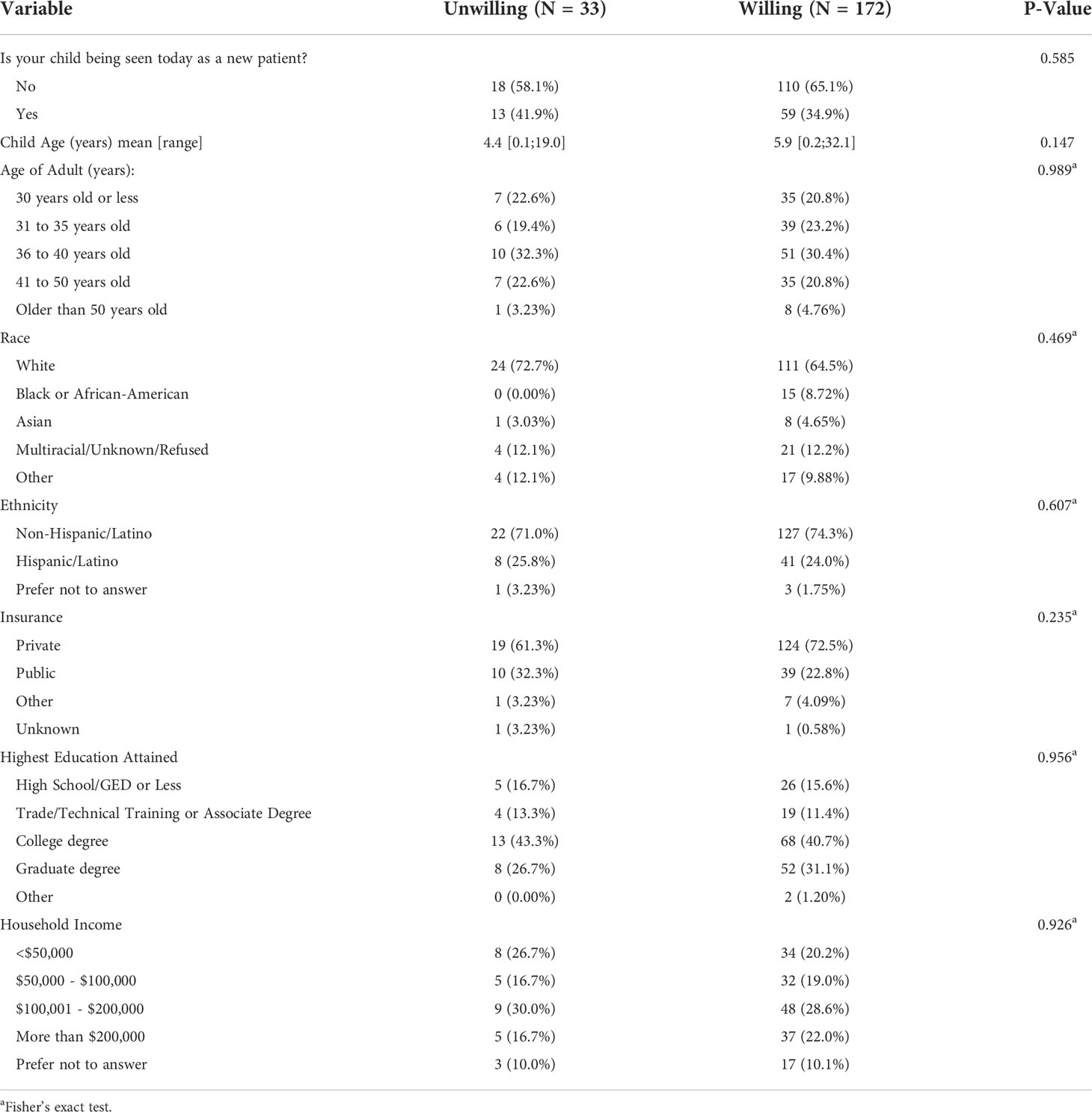
Table 2 Demographics Associated with Willingness to Participate in Telemedicine among Pre-Telemedicine Cohort.
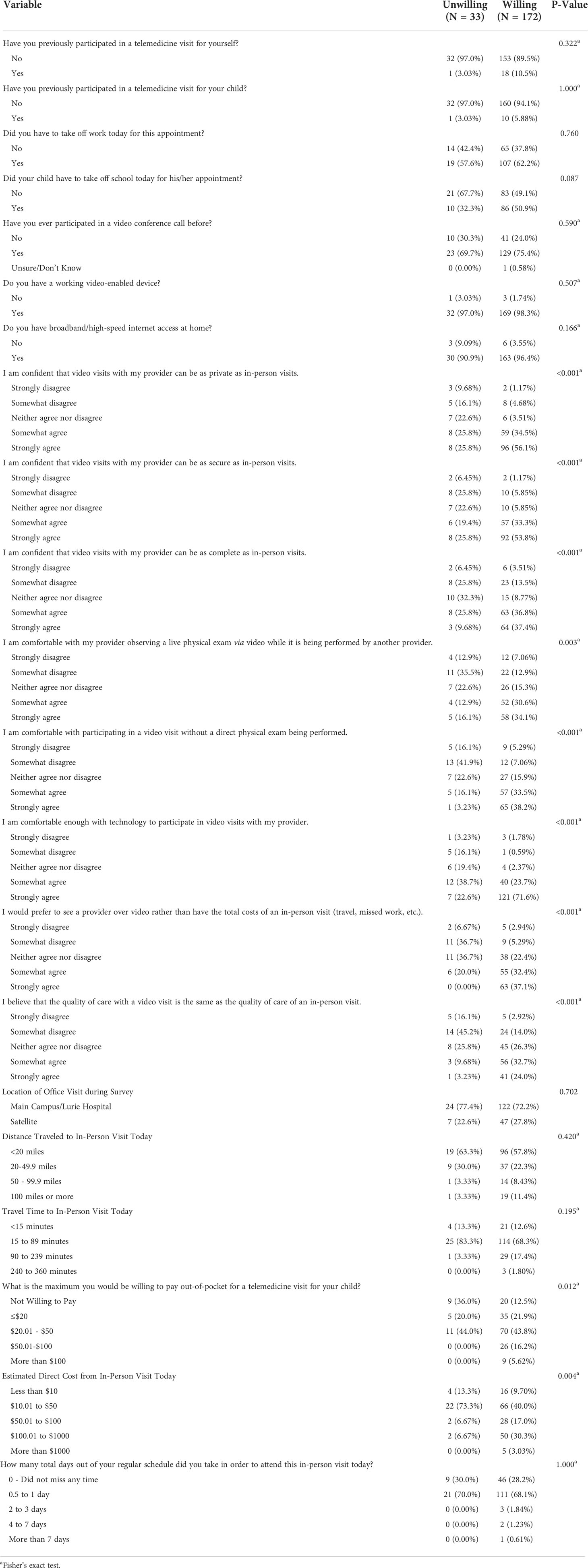
Table 3 Factors Associated with Willingness to Participate in Telemedicine among Pre-Telemedicine Cohort.
Despite the majority reporting that they would feel comfortable participating in telemedicine without a direct physical exam being performed (62.1%) or with a provider observing a live physical exam being performed by another provider (57.8%), there were many who disagreed that their day-of in-person visit could have been performed via telemedicine (56.4%) or that they would have preferred for their in-person visit to have been performed via telemedicine (64.4%). This was a common theme found among qualitative comments as well (18 out of 55; 32.7%), which highlighted the expressed interest in participating in telemedicine if a physical examination was not thought to be necessary.
The majority of patients completed their telemedicine visit via video visit (91%). Of the eight patients (9%) that underwent a telephone visit, three were offered a video visit, but did not complete the video visit due to technological difficulties. Under one quarter of parents had previously participated in telemedicine for themselves (23.6%) or their child (22.5%). Most Post-Telemedicine respondents indicated that telemedicine met their needs (88.6%), and that they were satisfied with both the quality of technology used (83%) and the interaction with the urologist (89.9%) during the telemedicine visit. Additionally, most reported that, compared to an in-person visit, the quality of interaction with the urologist via telemedicine was similar or better (78.8%). A plurality reported time saved from participation in a telemedicine visit to be 45 to 90 minutes (25.8%), with a reported $10-to-$50 saved (43.2%). Lastly, most reported that they would typically need to miss a half-day to one-day from their regular schedule in order to attend an in-person visit (67.4%).
On qualitative comments, feedback regarding the telemedicine platform was found to be a common theme, including issues related to audio (5/38, 13%) and video (2,38, 5.2%), as well as the recommendation for drawing capabilities for educational purposes (1/38, 2.6%). Also, preference for an in-person physical examination was common (8/38, 21.1%).
Post-Telemedicine respondents were more likely to be return patients (128/205, 64.0% Pre-Telemedicine vs 70/89, 78.7% Post-Telemedicine, p=0.02). Parents among the Post-Telemedicine sub-group, relative to the Pre-Telemedicine sub-group, more frequently reported having prior experience with telemedicine themselves (9.3% vs 23.6%, p=0.002) or on behalf of their child (5.4% vs 22.5%, p=<0.001). Post-Telemedicine respondents, compared with Pre-Telemedicine respondents, more frequently strongly agreed that telemedicine is as private, secure, and complete as in-person visits (Table 4).
In our study, parents of pediatric urology patients attending in-person visits prior to the COVID-19 pandemic had high willingness to participate in and positive perceptions of telemedicine. Parents participating in telemedicine during the beginning of the COVID-19 pandemic had high satisfaction with their visits and reported that their interaction with the provider was the same or similar to an in-person visit. Additionally, most parents participating in telemedicine visits reported savings in time and direct costs compared with conducting a similar visit in-person. When comparing perceptions between Pre-and-Post-Telemedicine sub-groups, confidence in telemedicine appears to have increased after experience with telemedicine.
This is the first study (to our knowledge) to focus specifically on parents of pediatric urology patients and their perceptions of and willingness to utilize telemedicine in pediatric urology. One study—conducted in pediatric urology and general surgery outpatient clinics—found that willingness to participate in a hypothetical telemedicine visit was positively associated with higher perceived costs from an in-person visit and distance traveled (18). While the cost-related finding is consistent with our results, parents of our patients with longer travel distances did not report higher willingness. The discrepancy in this latter finding may be due to the difference in the percent distribution of travel distances among patients between the two study cohorts, i.e., most of our patients lived within <20 miles of their clinic location and this was not the case in the other study.
Among the Pre-Telemedicine sub-group, there was no difference in willingness between new patients versus established patients, which is supported by existing literature (18). Comfort with participating in a video visit without a direct physical exam being performed was also found to be positively associated with willingness. In the literature, the lack of physical examination via telemedicine is reported by patients as disadvantageous (9, 19). While much of pediatric urological care can be delivered without an in-person physical examination, many conditions (e.g., undescended testes), require an in person physical exam (14). As our focus was different than prior investigations, the present study did not delineate patients based on diagnosis or medical complexity, but there have been several studies that have explored this in pediatric urology (9, 20, 21). Also, while we did not find similar comments in our qualitative data among survey respondents, some negative aspects of telemedicine might be relatively unique to urology, e.g., one participant in another study reported that “while the visit was fine, it was very unnerving to have my child expose himself on the camera” (9).
Among the Post-Telemedicine sub-group, we found high levels of satisfaction with telemedicine, which is supported by and within the range found in existing pediatric urology literature (89-100%) (14). Similarly, most reported that their medical needs were met, also in line with existing literature (9). It is difficult to generalize the quantity of time and costs saved for families from participation in telemedicine due to the variability in appointment burden placed on families across different hospital locations, but it was found in our study—as is the case in other studies—that parents reported some kind of savings when comparing their telemedicine visit with an in-person visit (9, 22).
Regarding the comparison between Pre-and-Post-Telemedicine sub-groups, the context in which this study developed is important. During the initial phases of this study (prior to the COVID-19 pandemic) our group was interested in exploring telemedicine as a medium of care, resulting in the survey administered to the Pre-Telemedicine sub-group. During the onset of COVID-19 our group began to offer pediatric urology care via telemedicine, so we developed a complementary survey for the Post-Telemedicine sub-group of parents who participated in telemedicine visits. Of note, nearly all parents of urology patients in the Pre-Telemedicine cohort had no experience with telemedicine. When stay-at-home orders were put into place, most visits were converted to telemedicine unless the clinician determined an in-person visit to be compulsory. While those among the Post-Telemedicine sub-group had more prior experience with telemedicine than the Pre-Telemedicine sub-group, they still had fewer than 1 in 4 with past experience with telemedicine. Given this, our results indicated that parents of pediatric urology patients who are relatively telemedicine-naïve have improved confidence in telemedicine after experience with the modality.
This study has important limitations. We compared perceptions between two different groups, i.e., we did not perform a before and after comparison of the same patients. Further, the Pre-Telemedicine group was queried on a hypothetical telemedicine visit—and the vast majority of those within this group had no prior experience with telemedicine—while the Post-Telemedicine group had completed a telemedicine visit. This was a predominately privately insured, higher income, and highly educated, English-speaking population that nearly all had internet access and a video-enabled device, with >90% able to participate in video visits. Thus, these results may not be fully generalizable to other populations. Further, many patients across the US have access to the internet via cellular device only and we did not include in our survey such a question. While it has been shown that launching telemedicine in a predominately lower-socioeconomic area in the United States with limited internet access had similar satisfaction levels, most reported preference for phone visits (i.e., audio-only)—rather than video—due to technological limitations (23) and one study has shown that public insurance, relative to those with private insurance, was predictive of virtual visit failure, with virtual visit success defined as “satisfactory completion of the visit as assessed by the provider” (22). Moreover, those that are older in age, live in rural areas, lack adequate internet access, lower-socioeconomic status, or African American are more likely to utilize audio-only visits for urological care (24). Thus, neglecting to cover and reimburse audio-only visits will likely result in exacerbating health disparities among these groups. The Post-Telemedicine response rate was significantly lower than the Pre-Telemedicine response rate, which may bias results as it is possible that those who responded in the Post-Telemedicine group are different from the population that was sampled. Although, these two groups were samples from the same patient population that is seen at our urology service, i.e., two samples of the same whole. Further, we compared demographics between both groups and found no statistically significant differences. We did not collect data on patient diagnosis, and thus could not compare willingness to participate in telemedicine based on medical complexity or particular diagnoses, which may be most relevant with perceived need for a physical examination. Most studies in pediatric urology have focused on the parent perspective rather than child or patient perspectives, including ours, and a recent report has pointed out that this may be a shortcoming of telemedicine (25). The novelty of this study stems from its comparison of perceptions of telemedicine between an in-person visit group and a telemedicine visit group for the first time in pediatric urology. Also, this study, along with a few others, was performed during the unique period in which patients had less choice about whether to participate in a telemedicine visit, as in-person visits were severely limited during the beginning of the pandemic. Thus, perceptions of telemedicine among the Post-Telemedicine sub-group might be more revealing and resilient to sampling bias compared with patients who have continued to choose telemedicine now that in-person visits are more available.
Despite a lack of past participation in telemedicine among the Pre-Telemedicine cohort, most parents of pediatric urology patients had high willingness to participate and positive perceptions of telemedicine. Factors associated with willingness to participate in telemedicine were elucidated. Those that underwent a telemedicine visit reported high levels of satisfaction, as well as savings in time and direct costs from an in-person visit. Those that underwent a recent telemedicine visit also had a higher degree of positive perceptions of telemedicine, which suggests that confidence in telemedicine grew after experience with telemedicine. These data support continued telemedicine access and coverage and reimbursement beyond the pandemic.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Ann & Robert H. Lurie Children’s Hospital of Chicago. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
All authors were involved in study design. RW, HA, IR, and EJ were involved in drafting and revising the surveys. RW and HA were responsible for participant recruitment. RW, RB, IR, and EJ were responsible for data analysis and interpretation of the data. RW drafted the manuscript, and all other authors assisted with critical review and editing of the manuscript. All authors have approved of the final manuscript as submitted.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fruro.2022.972708/full#supplementary-material
Appendix 1 | – Pre-Telemedicine Survey.
Appendix 2 | – Post-Telemedicine Survey.
1. Center for connected health policy. What is telehealth? Available at: www.cchpca.org/about/about-telehealth.
2. Clark PA, Capuzzi K, Harrison J. Telemedicine: Medical, legal and ethical perspectives. Med Sci Monit (2010) 16(12):Ra261–72.
3. Connor MJ, Miah S, Edison MA, Brittain J, Smith MK, Hanna M, et al. Clinical, fiscal and environmental benefits of a specialist-led virtual ureteric colic clinic: A prospective study. BJU Int (2019) 124(6):1034–9. doi: 10.1111/bju.14847
4. Whetten J, Montoya J, Yonas H. ACCESS to better health and clear skies: Telemedicine and greenhouse gas reduction. Telemed J e-health Off J Am Telemed Assoc (2019) 25(10):960–5. doi: 10.1089/tmj.2018.0172
5. Vidal-Alaball J, Franch-Parella J, Lopez Seguí F, Garcia Cuyàs F, Mendioroz Peña J. Impact of a telemedicine program on the reduction in the emission of atmospheric pollutants and journeys by road. Int J Environ Res Public Health (2019) 16(22):4366. doi: 10.3390/ijerph16224366
6. Finkelstein JB, Cahill D, Young K, Humphrey K, Campbell J, Schumann C, et al. Telemedicine for pediatric urological postoperative care is safe, convenient and economical. J Urol (2020) 204(1):144–8. doi: 10.1097/JU.0000000000000750
7. Diaz-Miron J, Ogle S, Kaizer A, Acker SN, Rove KO, Inge TH. Surgeon, patient, and caregiver perspective of pediatric surgical telemedicine in the COVID-19 pandemic era. Pediatr Surg Int (2022) 38(2):241–8. doi: 10.1007/s00383-021-05016-8
8. Metzger G, Jatana K, Apfeld J, Deans KJ, Minneci PC, Halaweish I. State of telemedicine use in pediatric surgery in the USA–where we stand and what we can gain from the COVID-19 pandemic: A scoping review. World Journal of Pediatric Surgery (2021) 4(1). doi: 10.1136/wjps-2020-000257
9. Gan Z, Lee SY, Weiss DA, Van Batavia J, Siu S, Frazier J, et al. Single institution experience with telemedicine for pediatric urology outpatient visits: Adapting to COVID-19 restrictions, patient satisfaction, and future utilization. J Pediatr Urol (2021) 17(4):480.e1–.e7. doi: 10.1016/j.jpurol.2021.05.012
10. Rabie NZ, Canon S, Patel A, Zamilpa I, Magann EF, Higley J. Prenatal diagnosis and telemedicine consultation of fetal urologic disorders. J Telemed Telecare (2016) 22(4):234–7. doi: 10.1177/1357633X15595556
11. Canon S, Shera A, Patel A, Zamilpa I, Paddack J, Fisher PL, et al. A pilot study of telemedicine for post-operative urological care in children. J Telemed Telecare (2014) 20(8):427–30. doi: 10.1177/1357633X14555610
12. Contreras CM, Metzger GA, Beane JD, Dedhia PH, Ejaz A, Pawlik TM. Telemedicine: Patient-provider clinical engagement during the COVID-19 pandemic and beyond. J Gastrointest Surg Off J Soc Surg Aliment Tract (2020) 24(7):1692–7. doi: 10.1007/s11605-020-04623-5
13. Finkelstein JB, Cahill D, Kurtz MP, Campbell J, Schumann C, Varda BK, et al. The use of telemedicine for the postoperative urological care of children: Results of a pilot program. J Urol (2019) 202(1):159–63. doi: 10.1097/JU.0000000000000109
14. Pettit S, Young E, Jung I. Systematic review of telemedicine in pediatric urology. J Pediatr Urol (2022) 18(1):17–22. doi: 10.1016/j.jpurol.2021.09.024
15. Novara G, Checcucci E, Crestani A, Abrate A, Esperto F, Pavan N, et al. Telehealth in urology: A systematic review of the literature. How much can telemedicine be useful during and after the COVID-19 pandemic? Eur Urol (2020) 78(6):786–811. doi: 10.1016/j.eururo.2020.06.025
16. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform (2009) 42(2):377–81. doi: 10.1016/j.jbi.2008.08.010
17. Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O'Neal L, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform (2019) 95:103208. doi: 10.1016/j.jbi.2019.103208
18. Bator EX, Gleason JM, Lorenzo AJ, Kanaroglou N, Farhat WA, Bägli DJ, et al. The burden of attending a pediatric surgical clinic and family preferences toward telemedicine. J Pediatr Surg (2015) 50(10):1776–82. doi: 10.1016/j.jpedsurg.2015.06.005
19. Lakshin G, Banek S, Keese D, Rolle U, Schmedding A. Telemedicine in the pediatric surgery in Germany during the COVID-19 pandemic. Pediatr Surg Int (2021) 37(3):389–95. doi: 10.1007/s00383-020-04822-w
20. Holzman SA, Davis-Dao CA, Khoury AE, Fortier MA, N Kain Z. Telemedicine and patient satisfaction during the COVID-19 pandemic: A case-control study of outpatient pediatric urology patients. J Child Health Care Prof Working Children Hosp Community (2021) 13674935211058272. doi: 10.1177/13674935211058272
21. Charnell AM, Hoen L, Sforza S, Spinoit AF, Radford A. Remote consultations in paediatric urology-not just for pandemics? J Pediatr Urol (2021) 17(2):260–2. doi: 10.1016/j.jpurol.2021.01.001
22. Winkelman AJ, Beller HL, Morgan KE, Corbett ST, Leroy SV, Noona SW, et al. Benefits and barriers to pediatric tele-urology during the COVID-19 pandemic. J Pediatr Urol (2020) 16(6):840.e1–.e6. doi: 10.1016/j.jpurol.2020.09.028
23. Watts KL, Abraham N. "Virtually perfect" for some but perhaps not for all: Launching telemedicine in the Bronx during the COVID-19 pandemic. J Urol (2020) 204(5):903–4. doi: 10.1097/JU.0000000000001185
24. Odukoya EJ, Andino J, Ng S, Steppe E, Ellimoottil C. Predictors of video versus audio-only telehealth use among urological patients. Urol Practice (2022) 9(3):198–204. doi: 10.1097/UPJ.0000000000000301
Keywords: telemedicine, survey research, patient perspectives, pediatric urology, telehealth
Citation: Walton RF, Arora HC, Berkowitz RJ, Rosoklija I, Cheng EY and Johnson EK (2022) Parent perspectives about pediatric urology telemedicine visits before and after COVID-19-driven rapid implementation. Front. Urol. 2:972708. doi: 10.3389/fruro.2022.972708
Received: 18 June 2022; Accepted: 04 August 2022;
Published: 25 August 2022.
Edited by:
Julia Beth Finkelstein, Boston Children’s Hospital and Harvard Medical School, United StatesReviewed by:
Stephen Canon, Arkansas Children’s Hospital, United StatesCopyright © 2022 Walton, Arora, Berkowitz, Rosoklija, Cheng and Johnson. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Emilie K. Johnson, ZWtqb2huc29uQGx1cmllY2hpbGRyZW5zLm9yZw==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.