- 1Department of Urology, Columbia University Irving Medical Center, New York, NY, United States
- 2Post-Research Completion Affiliation: Department of Urology, Boston Children’s Hospital, Boston, MA, United States
Introduction and Objectives: The standardization of fetal sonography has enabled early detection of genitourinary anomalies and referral for prenatal counseling with pediatric urologists. Prenatal urologic consultation can determine the need for antenatal and postnatal intervention, assuage parental anxiety, and establish continuity of care. The COVID-19 pandemic led to a significant increase in virtual visits (VVs). Our aim was to characterize a cohort of patients who underwent prenatal VVs with pediatric urologists and to assess adherence to prenatal recommendations for neonatal urologic care.
Materials and Methods: Data were collected through retrospective chart review of all patients receiving prenatal virtual consultation for genitourinary anomalies at our institution from July 1, 2020 to September 30, 2021. Data collected include maternal and gestational age at the time of prenatal imaging and VV, diagnosis of the fetus and neonate, and adherence to pediatric urological recommendations.
Results: During the study period, there were 70 prenatal VVs for 69 singleton and 1 twin gestation. 84 prenatal genitourinary diagnoses were made in these 71 cases. Of the 56/71 children known to have been born by the time of analysis, there are 63 postnatal genitourinary diagnoses. Postnatal diagnoses were consistent (38/56, 68%) or partially consistent (16/56, 29%) with prenatal diagnoses in 54/56 neonates (96%). There was 100% adherence to the postnatal imaging and antibiotic recommendations. One patient failed to attend the postnatal visit and one patient is due for repeat postnatal imaging to determine the necessity of follow-up.
Conclusions: Prenatal VVs promoted effective counseling of genitourinary anomalies and were associated with impressive postnatal adherence to prenatal recommendations. This is, to our knowledge, the first study to assess the impact of prenatal virtual pediatric urological consultation on postnatal adherence to prenatal recommendations. Future study will benefit from survey of the patient VV experience and evaluation of the relative merits of virtual versus in-person prenatal visits in a prospective, randomized fashion.
Introduction
Screening with fetal sonography has become standard in obstetric care throughout the United States, enabling early detection of anatomic abnormalities. Urologic anomalies are common among these, with renal malformations detected in up to 2% of all pregnancies, accounting for 20-30% of all prenatally detected congenital anomalies (1, 2). In large retrospective screening studies, the sensitivity of prenatal ultrasound for detecting renal malformations is as high is as 88.5% (1, 3). The clinical implications of these prenatal findings vary widely. While a majority will be managed expectantly, a minority require urgent intervention (4). Furthermore, when a definitive diagnosis cannot be made prenatally, prompt postnatal imaging with repeat ultrasound or a voiding cystourethrogram (VCUG) is often necessary to determine appropriate care. Time is of the essence in these decisions, and failure to act appropriately can lead to unnecessary tests and treatment, if not long-term disability or death.
Considering their complexity and potential severity, prenatal diagnoses of urologic anomalies are often followed by a referral to a pediatric urologist for counseling to assuage parental anxiety and to establish continuity of care. While this is widely accepted as an appropriate subspecialty referral, the actual effect of prenatal counseling for genitourinary anomalies – on the health of the fetus and infant, the cost of care, and the burden to parents – is not well described. Moreover, the factors that make these visits impactful are not well known. Is there an optimal time during pregnancy for counseling? Are in-person visits necessary, or can these consultations be conducted virtually to reduce travel costs, time away from work, and unnecessary exposure to a hospital setting?
The advent of the COVD-19 pandemic and attendant efforts to minimize unnecessary hospital exposures has led to a significant increase in the use of virtual visits (VVs) across fields, including pediatrics (5–7). Examination of this period in healthcare permits investigators to ask whether or not VVs will be an acceptable alternative to in-person visits for various purposes in the post-pandemic era. Given that prenatal consultations with pediatric subspecialists like urologists require no concurrent physical exam, this would seem to be an ideal opportunity to leverage telemedicine.
In this study, we sought to characterize a cohort of parents who underwent virtual prenatal counseling with a pediatric urologist. Our specific aim was to assess the adherence to prenatal recommendations by neonatal providers and subsequent postnatal urologic follow-up. We hypothesized that adherence rates and follow-up would be high across a range of diagnoses, indicating that VVs are an acceptable and safe alternative to in-person visits for prenatal consultations for genitourinary anomalies.
Materials and methods
Following institutional review board approval, we retrospectively reviewed the charts of all patients who underwent prenatal video consultations for genitourinary anomalies by one of three pediatric urologists at our institution from July 1, 2020 to September 30, 2021. These visits were captured using the ICD-10 codes O35.8XX0 and Z71.89 and eliminating all non-virtual visits. As this was a descriptive study of a carefully selected group of patients, there were no additional exclusion criteria. Data collected included maternal and gestational age at the time of prenatal imaging and VV, diagnosis of the fetus and neonate, and adherence to recommendations made during the VV. Patients in whom one or more, but not all, of the prenatal and postnatal diagnoses were the same were considered “partially consistent.” For example, if a fetus was diagnosed prenatally with unilateral hydronephrosis and found in life to have bilateral hydronephrosis, this was considered partially consistent.
If there was prenatal concern that a postnatal intervention and/or a higher level of neonatal care would be necessary, it was recommended that delivery occur at the primary hospital (an urban tertiary care children’s hospital). Patients born outside of the primary hospital at one of two affiliate community hospitals also providing obstetrical services were included in our analysis of postnatal diagnoses, adherence, and follow-up. All three hospitals are located within ten miles of one another and share an electronic medical record system. Pediatric urological consultation is available at the primary hospital and one of the affiliated community hospitals. At the other affiliated community hospital, telephonic pediatric urological consultation is available, but in-person evaluation occurs postnatally in the outpatient setting. Patients born at other hospitals were excluded from postnatal analysis due to lack of access to necessary data.
Results
During the study period, there were 70 prenatal VVs for 71 fetuses (69 singleton and 1 twin gestation). All parents were seen for just one prenatal visit at a median gestational age of 31.3 weeks (IQR 23.6 – 36.0). Median maternal age at the time of the VV was 32 years (IQR 29-36). An interpreter was used in 12/70 (17%) of these visits.
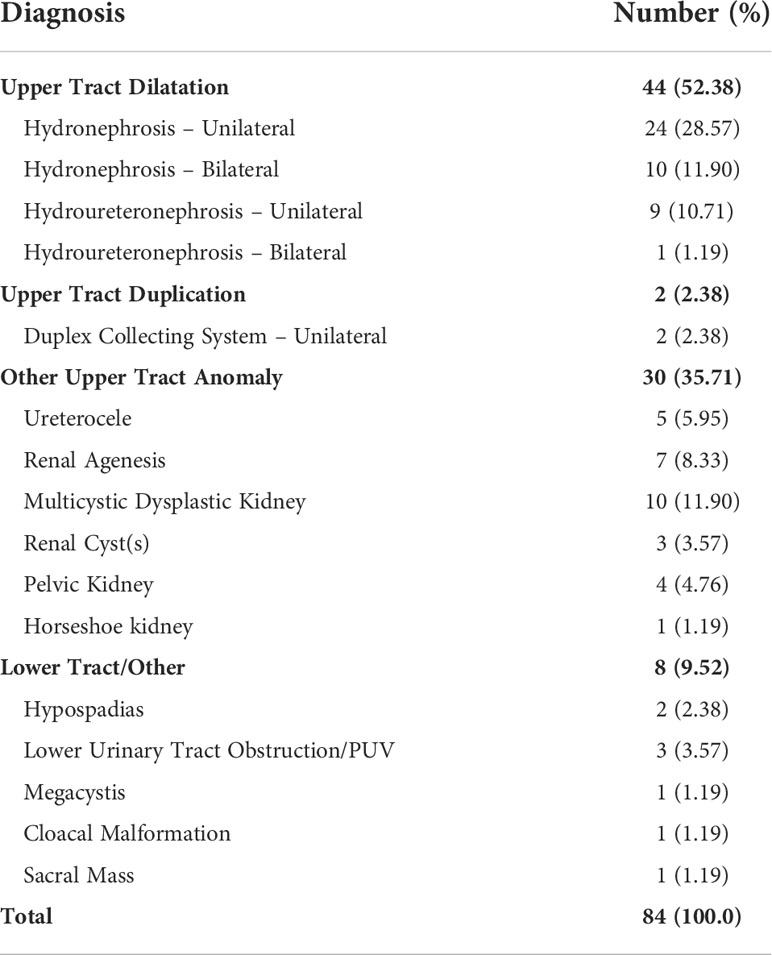
Figure 1 displays the patient participation in each stage of analysis. Eighty-four prenatal genitourinary diagnoses were made for the 71 fetuses (Table 1). Upper urinary tract dilatation was the most common category of prenatal anomaly diagnosed (44/84, 52%). Prenatal recommendations are delineated in Table 2. The need for a renal-bladder ultrasound (RBUS) in early infancy (prior to or at 4 weeks of life) was discussed for 83% (59/71) of cases. The need or possible need for a voiding cystourethrogram (VCUG) was noted for 23% (16/71). Antibiotic prophylaxis was discussed for 20% (14/71) of fetuses, all for whom a VCUG was either recommended or deemed necessary pending the results of a postnatal RBUS. In two cases, the likely need for a VCUG was recorded but a discussion about antibiotics was not documented.
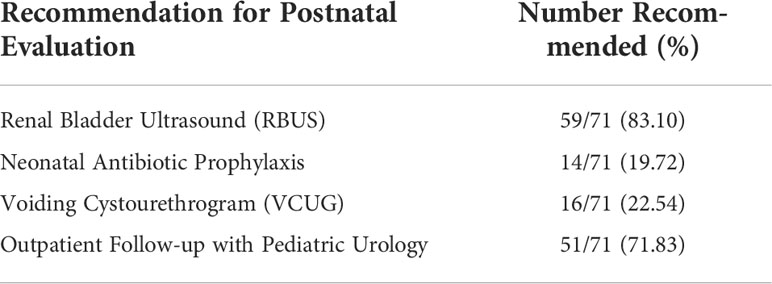
Table 2 Prenatal recommendations made for the postnatal urologic evaluation of the 71 cases seen virtually.
A specific age for recommended postnatal pediatric urological outpatient evaluation was documented for 72% (51/71) of cases. Follow-up was recommended between 2 and 6 weeks of life (median 3 weeks; IQR 3-4 weeks). One patient with prenatally diagnosed unilateral renal agenesis was recommended to have follow-up with nephrology only. Two mothers were advised to follow up once more in the prenatal period but did not, so final recommendations for life were not documented. In both cases, prenatally diagnosed malformations were severe (lower urinary tract obstruction (LUTO) and bilateral renal agenesis, respectively) necessitating prenatal consultations with multiple specialists. Both cases suffered neonatal demise within the first two days of life. A specific post-discharge follow-up plan was not documented in the remaining 17 fetuses (17/71, 24%), 15 for whom neonatal imaging prior to discharge was recommended and the other two of whom underwent elective termination.
At the time of this study, 62 neonates had been born. Ninety percent (56/62) were born within our hospital system, while six (6/62, 10%) were born outside of our hospital (i.e. without available data) and were excluded from postnatal analysis (Figure 1). The other 9/71 prenatally evaluated cases were excluded from postnatal analysis: 6 are pending delivery and 3 were electively terminated.
Seventy-seven percent (43/56) of deliveries within our hospital system occurred at full-term. Of the 13 patients born pre-term, one was delivered early due to a genitourinary diagnosis (oligohydramnios in a patient with prenatally diagnosed LUTO). The other 12 patients were born early due to a variety of non-urologic reasons. Of the 52/56 (93%) patients born where inpatient pediatric urology consultation was available, a neonatal consult was requested for 19/52 (37%).
There were 63 postnatal genitourinary diagnoses in the 56 neonates born within our hospital system (i.e. with available data, Table 3). Upper urinary tract dilatation persisted as the most common category for postnatal genitourinary pathology (35/63, 56%). In 54/56 neonates (96%), postnatal diagnoses were consistent (38/56, 68%) or partially consistent (16/56, 29%) with prenatal diagnoses. One patient was prenatally diagnosed with a unilateral duplicated collecting system and found in life to instead have unilateral hydronephrosis. In the final patient, the prenatally diagnosed anomaly, a renal cyst, was found to have resolved on subsequent prenatal imaging and no postnatal imaging was obtained.
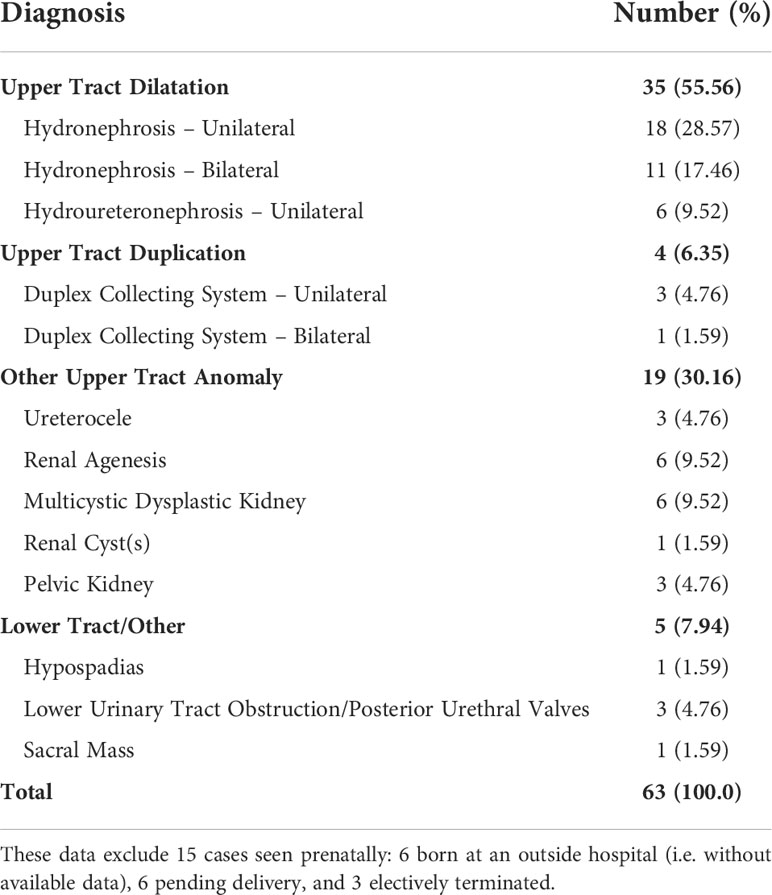
Table 3 Genitourinary diagnoses made in life in the 56 patients born within our hospital system to date.
The frequency of prenatal recommendations and the rate of postnatal adherence to these recommendations in patients born within our hospital system are displayed in Table 4. Across all three hospitals within our hospital system, there was 100% adherence by neonatal providers to imaging and antibiotic recommendations. In just one case, in a patient with posterior urethral valves (PUV), inpatient consultation was requested before prenatal antibiotics and imaging recommendations were pursued. Of the 33 patients born at our center who were directed to have an in-person postnatal visit, 82% (27/33) have been seen; 12% (4/33) are scheduled for their first follow-up in the future; and 6% (2/33) have no postnatal urologic follow-up scheduled. Both of these patients were diagnosed prenatally and confirmed on postnatal RBUS to have unilateral hydronephrosis. One has not returned to our hospital system since birth and the other patient is scheduled for a repeat RBUS as directed by his pediatrician. Two patients born at our center underwent surgery within the first month of life for their prenatally diagnosed malformations; one neonate had an unsuccessful attempt at PUV ablation that was converted to a vesicostomy, and another had transurethral incision of an obstructing ureterocele.
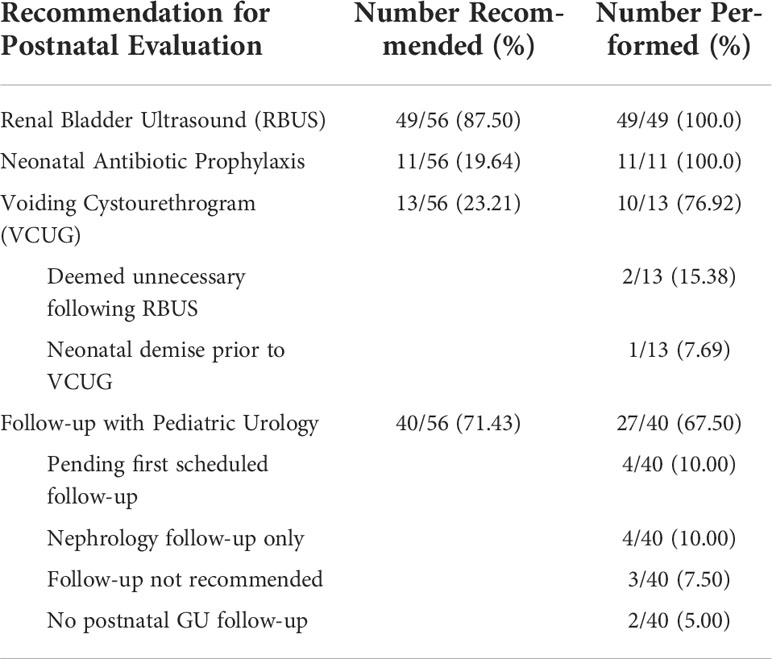
Table 4 Postnatal rates of adherence to prenatal recommendations made for the 56 patients born within our hospital system to date.
Discussion
For virtual medicine to become widely adopted in the post-COVID-19 era, it is critical that we ensure that VVs meet the clinical standards of in-person visits. This is already being evaluated in the world of pediatric urology, where recent contributions from Boston Children’s Hospital and Arkansas Children’s Hospital have demonstrated that the use of telemedicine for post-operative care leads to clinical outcomes similar to in-person visits (8, 9). These studies have also demonstrated important additional benefits of VVs, namely minimizing time spent traveling and waiting for in-person appointments and thereby limiting missed work and school.
However, there is limited literature addressing the effectiveness of VVs for prenatally diagnosed genitourinary anomalies. Prenatal urological consultations are a fitting application of virtual medicine for two reasons. First, these visits do not require a physical examination, eliminating the most significant limitation of VVs. Secondly, pediatric urology is a small field, and its providers are generally centralized to large tertiary medical centers, meaning that many patients must travel long distances for their care. This barrier is common across pediatric subspecialty care, but is significantly mitigated by the availability of telemedicine (10). Rabie et al, also from the University Arkansas, described a series of 25 VVs for prenatally diagnosed urologic anomalies conducted between 2009 and 2013 and reported that this was well tolerated by parents, with no negative feedback reported (11). Rabie and colleagues’ work is, to their knowledge and ours, the first and only previous publication to describe the use of telemedicine for prenatal urologic consultations. There are essential differences between this study and our own, however. Whereas a majority of the largely rural patient population in their study ultimately delivered at a local hospital, remote from the tertiary center where pediatric urologists were located, in our study, 90% of patients evaluated prenatally born to date were delivered within our hospital system (10% born elsewhere were excluded from post-natal analysis). Nonetheless, in both experiences, prenatal consultations in the form of VVs were shown to be a promising alternative to in-person care.
Patients in our study were evaluated for a wide range of genitourinary diagnoses. Prenatal ultrasound provided the appropriate diagnoses in most cases (69-96%), enabling appropriate perinatal recommendations. The rate of adherence to postnatal imaging and antibiotic recommendations made prenatally was 100 percent. Furthermore, while inpatient consultation from pediatric urology was available for most newborns (52/56, 93%), consultation was requested prior to initiating prenatal recommendations in only one case (1.9%). This means that, for a significant majority of patients, prenatal consultation, and the documentation thereof in the electronic medical record, was sufficient for appropriate postnatal urologic care. This may eliminate delays in postnatal diagnosis or treatment on the part of the urology service and minimize demand on a busy inpatient consultation service.
In addition to universal adherence to prenatal recommendations, patients seen in prenatal VVs had high rates of follow-up after delivery, with just one patient not being seen in recommended urologic follow-up. While only a minority of these patients were seen by urologic consultants as inpatients, all parents had established a relationship with a pediatric urologist prior to delivery, which likely contributed to the high adherence to postnatal follow-up. While prenatal surgical consultations may prompt changes in the timing, mode, and site of delivery and inform decisions pertaining to termination and in utero treatment (12), their effect on the timeliness and appropriateness of neonatal evaluations and interventions and subsequent outpatient follow-up is less well studied. The data reported herein suggest that patients undergoing prenatal consultation are set up for success in this regard, and that VVs are an effective method for delivering these consultations.
While the present study evaluates novel endpoints pertaining to adherence and follow-up after virtual prenatal consultations, it does not assess the experience of families and providers. This has been evaluated in related fields, however. The aforementioned study from Boston Children’s Hospital found that all families attending virtual post-operative pediatric urological visits were “satisfied” or “very satisfied” with their experiences, with 98% reporting that VVs were more convenient than in-person visits (8). High rates of family and provider satisfaction have also been demonstrated in other pediatric surgical fields for a range of virtual medicine types (13–16). In a recent survey study of 91 high-risk obstetrical patients undergoing VVs for high-risk prenatal care, diabetes mellitus education, genetic counseling, and maternal-fetal medicine (MFM) consultations during the COVID-19 pandemic, Jeganathan et al. found that 86.9% of patients reported being satisfied with the care they received, with 78.3% stating that they would recommend telemedicine visits to others (17). Their providers were also surveyed; 87.8% reported a positive experience using telemedicine and 90.9% believed that telemedicine improved their patients’ access to care. Furthermore, the rates of no-show and cancelled appointments for all visit types, other than MFM consultations, significantly decreased following the implementation of telemedicine. As virtual medicine has been rapidly adopted during the COVID-19 pandemic, similar satisfaction with prenatal consultations have been reported by patients and providers in neonatology (18), MFM (19, 20), and genetics (21, 22). Notably, despite the heightened sensitivity of matters discussed and the importance of patient privacy in prenatal genetic consultations, these VVs have been well tolerated, with patients reporting high levels of confidence in the visit’s privacy and satisfaction with their providers’ attention to their emotional needs (21, 22). These data are encouraging as we consider the likely similar experiences of patients undergoing prenatal urologic consultation, though future study in this setting would benefit from questionnaires to assess patient and clinician satisfaction. Furthermore, while the execution of prenatal recommendations is one measure of success, it does not capture a parent’s understanding of their child’s diagnosis or the consultant’s recommendations. This is an unquestionably important goal for prenatal counseling and an endpoint that should be evaluated in future prospective investigations.
While we believe that the experience described herein demonstrates the feasibility and efficacy of virtual prenatal counseling for congenital genitourinary anomalies, this study’s retrospective nature, modest cohort size, and lack of control group limits our ability to rigorously assess its non-inferiority to in-person prenatal care. Furthermore, the nature of the cohort studied should be considered when extrapolating from our experience. In particular, the high rate of adherence and follow-up that we report may be supported by the fact that a high proportion of those patients seen by our providers prenatally ultimately deliver within our institution. As previously described (9, 11), virtual consultations are of great value to patients who live long distances from large tertiary centers, while it is often the case that these patients deliver in local, less well-staffed hospitals. This makes a case for continued improvements in the interconnectivity between electronic medical records, so that recommendations made at prenatal VVs are accessible to providers in local hospitals. Finally, the present study did not assess some important endpoints, namely the patient and provider experience including consideration of patient privacy and emotional support; the role of patient demographics and access to care in the feasibility of VVs; and the savings in travel time and cost as well as preserved work time and income theoretically afforded by virtual medicine.
While future research should address the above parameters, we hope that our experience will be instructive to other pediatric urologists interested in providing prenatal virtual care for their patients. We found that virtual medicine allowed for effective parental counseling of fetal genitourinary anomalies and was associated with impressive postnatal adherence to prenatal recommendations.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Columbia University Institutional Review Board (Protocol #AAAT7053). Written informed consent from the participants’ legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author contributions
GM: conception of study aims and methods, patient chart review, statistical analysis, manuscript writing. DS: patient chart review, manuscript review and revision. MM: manuscript review and revision. JF: conception of study aims and methods, manuscript review and revision. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
VV, Virtual visit; RBUS, renal-bladder ultrasound; VCUG, voiding cystourethrogram; LUTO, lower urinary tract obstruction; MFM, maternal-fetal medicine
References
1. Wiesel A, Queisser-Luft A, Clementi M, Bianca S, Stoll C, Group ES. Prenatal detection of congenital renal malformations by fetal ultrasonographic examination: an analysis of 709,030 births in 12 European countries. Eur J Med Genet (2005) 48(2):131–44. doi: 10.1016/j.ejmg.2005.02.003
2. Queisser-Luft A, Stolz G, Wiesel A, Schlaefer K, Spranger J. Malformations in newborn: results based on 30,940 infants and fetuses from the mainz congenital birth defect monitoring system (1990-1998). Arch Gynecol Obstet (2002) 266(3):163–7. doi: 10.1007/s00404-001-0265-4
3. Grandjean H, Larroque D, Levi S. Sensitivity of routine ultrasound screening of pregnancies in the eurofetus database. the eurofetus team. Ann N Y Acad Sci (1998) 847:118–24. doi: 10.1111/j.1749-6632.1998.tb08932.x
4. Clayton DB, Brock JW 3rd. Prenatal ultrasound and urological anomalies. Pediatr Clin North Am (2012) 59(4):739–56. doi: 10.1016/j.pcl.2012.05.003
5. Howie F, Kreofsky BL, Ravi A, Lokken T, Hoff MD, Fang JL. Rapid rise of pediatric telehealth during COVID-19 in a Large multispecialty health system. Telemed J E Health (2022) 28(1):3–10. doi: 10.1089/tmj.2020.0562
6. Williams S, Hill K, Xie L, Mathew MS, Ofori A, Perry T, et al. Pediatric telehealth expansion in response to COVID-19. Front Pediatr (2021) 9:642089. doi: 10.3389/fped.2021.642089
7. Reingold SM, Hadjipanayis A, van Esso D, Del Torso S, Dornbusch HJ, de Guchtenaere A, et al. COVID-19 era effect on pandemic and post-pandemic pediatric telemedicine use: A survey of the European academy of pediatrics research in ambulatory settings network. Front Pediatr (2021) 9:713930. doi: 10.3389/fped.2021.713930
8. Finkelstein JB, Cahill D, Young K, Humphrey K, Campbell J, Schumann C, et al. Telemedicine for pediatric urological postoperative care is safe, convenient and economical. J Urol (2020) 204(1):144–8. doi: 10.1097/JU.0000000000000750
9. Canon S, Shera A, Patel A, Zamilpa I, Paddack J, Fisher PL, et al. A pilot study of telemedicine for post-operative urological care in children. J Telemed Telecare (2014) 20(8):427–30. doi: 10.1177/1357633X14555610
10. Hooshmand M, Foronda C. Comparison of telemedicine to traditional face-to-Face care for children with special needs: A quasiexperimental study. Telemed J E Health (2018) 24(6):433–41. doi: 10.1089/tmj.2017.0116
11. Rabie NZ, Canon S, Patel A, Zamilpa I, Magann EF, Higley J. Prenatal diagnosis and telemedicine consultation of fetal urologic disorders. J Telemed Telecare (2016) 22(4):234–7. doi: 10.1177/1357633X15595556
12. Crombleholme TM, D'Alton M, Cendron M, Alman B, Goldberg MD, Klauber GT, et al. Prenatal diagnosis and the pediatric surgeon: the impact of prenatal consultation on perinatal management. J Pediatr Surg (1996) 31(1):156–62. doi: 10.1016/S0022-3468(96)90340-1
13. Metzger GA, Cooper J, Lutz C, Jatana KR, Nishimura L, Deans KJ, et al. The value of telemedicine for the pediatric surgery patient in the time of COVID-19 and beyond. J Pediatr Surg (2021) 56(8):1305–11. doi: 10.1016/j.jpedsurg.2021.02.018
14. DeAntonio JH, Kang HS, Cockrell HC, Rothstein W, Oiticica C, Lanning DA. Utilization of a handheld telemedicine device in postoperative pediatric surgical care. J Pediatr Surg (2019) 54(5):1005–8. doi: 10.1016/j.jpedsurg.2019.01.032
15. Kim EN, Tyrell R, Moss WD, Siddiqi FA. Implementation of telehealth in a pediatric plastic surgery clinic: A single center's response to COVID-19. Ann Plast Surg (2022) 88:589–93. doi: 10.1097/SAP.0000000000003092
16. Shivji S, Metcalfe P, Khan A, Bratu I. Pediatric surgery telehealth: patient and clinician satisfaction. Pediatr Surg Int (2011) 27(5):523–6. doi: 10.1007/s00383-010-2823-y
17. Jeganathan S, Prasannan L, Blitz MJ, Vohra N, Rochelson B, Meirowitz N. Adherence and acceptability of telehealth appointments for high-risk obstetrical patients during the coronavirus disease 2019 pandemic. Am J Obstet Gynecol MFM (2020) 2(4):100233. doi: 10.1016/j.ajogmf.2020.100233
18. Jackson LE, Bishop CE, Vats KR, Azzuqa AA. Meeting families where they are: institution, evaluation, and sustainability of telemedicine prenatal neonatology consultation in the COVID-19 pandemic health emergency. Semin Perinatol (2021) 45(5):151417. doi: 10.1016/j.semperi.2021.151417
19. Madden N, Emeruwa UN, Friedman AM, Aubey JJ, Aziz A, Baptiste CD, et al. Telehealth uptake into prenatal care and provider attitudes during the COVID-19 pandemic in new York city: A quantitative and qualitative analysis. Am J Perinatol (2020) 37(10):1005–14. doi: 10.1055/s-0040-1712939
20. Oelmeier K, Schmitz R, Mollers M, Braun J, Deharde D, Sourouni M, et al. Satisfaction with and feasibility of prenatal counseling via telemedicine: A prospective cohort study. Telemed J E Health (2021). doi: 10.1089/tmj.2021.0309
21. Danylchuk NR, Cook L, Shane-Carson KP, Cacioppo CN, Hardy MW, Nusbaum R, et al. Telehealth for genetic counseling: A systematic evidence review. J Genet Couns (2021) 30(5):1361–78. doi: 10.1002/jgc4.1481
Keywords: telemedicine, virtual visit, prenatal diagnosis, prenatal care, congenital abnormalities, pediatric urology
Citation: Moran GW, Schoenfeld D, Movassaghi M and Finkelstein JB (2022) Evaluating the efficacy of virtual prenatal counseling for genitourinary anomalies. Front. Urol. 2:951238. doi: 10.3389/fruro.2022.951238
Received: 23 May 2022; Accepted: 13 July 2022;
Published: 01 August 2022.
Edited by:
Kiarash Taghavi, Monash Children’s Hospital, AustraliaReviewed by:
Jaynaya Marlow, Wellington Hospital, New ZealandRamesh Mark Nataraja, Monash Children’s Hospital, Australia
Copyright © 2022 Moran, Schoenfeld, Movassaghi and Finkelstein. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Julia B. Finkelstein, SnVsaWEuZmlua2Vsc3RlaW5AY2hpbGRyZW5zLmhhcnZhcmQuZWR1
 George W. Moran
George W. Moran Daniel Schoenfeld
Daniel Schoenfeld Miyad Movassaghi
Miyad Movassaghi Julia B. Finkelstein
Julia B. Finkelstein