- 1Arkansas Children's Hospital, Urology Division, Little Rock, AR, United States
- 2Urology Department, University of Arkansas for Medical Sciences, Little Rock, AR, United States
- 3University of Arkansas for Medical Sciences, School of Medicine, Little Rock, AR, United States
- 4Arkansas Children’s Research Institute (ACRI), Little Rock, AR, United States
Introduction: Minimal data exist on the accuracy of preoperative assessment with telemedicine compared to in-person preoperative evaluation. The study compared the efficacy of telemedicine in a clinic or home setting with an in-person approach for pediatric patients with urologic surgical problems.
Methods: Preoperative pediatric urologic telemedicine patients between 5 days and 7 years evaluated at our institution were reviewed between January 2011 and June 2020. Both traditional clinic telemedicine patients (TM) and home telemedicine patients (TMH) were included and compared with an in-person (IP) control cohort. Caregivers were invited to complete a National Research Council (NRC) satisfaction phone survey. Data on demographics, preoperative diagnosis/surgical plan, diagnosis at surgery, and surgical procedure were collected.
Results: Ninety-six patients with completed surveys were included in the study (34 TM, 24 TMH, and 38 IP). The median age was 10 months TM, 4 months TMH, and 6 months IP. Ethnicity was predominantly non-Hispanic white: 82.4% TM, 91.7% TMH, and 89.5% IP (p = 0.413). Preoperative assessment accuracy was equivalent in the three groups, with 29/34 (85.3%) TM patients, 22/24 (91.7%) TMH patients, and 35/38 (92.1%) IP patients having an accurate surgical plan (p = 0.69). Overall caregiver satisfaction was equivalent (p = 0.231).
Conclusion: Use of telemedicine for pediatric urological surgical planning may be as effective in accuracy and caregiver satisfaction as in-person evaluation.
Introduction
Telemedicine has been proven as an effective means of providing specialized medical care to rural patients around the world (1–3). With the COVID-19 pandemic, the availability of in-person consultations has become more restricted, especially in more elective surgical fields such as urology. However, the current pandemic has provided a unique opportunity to evaluate the efficacy of telemedicine for evaluations traditionally requiring in-person consultation while theoretically lowering the overall risk of potential exposure to the virus.
The vast population of Arkansas resides in a rural setting, with 62.9% living in an area with a population of less than 50,000. The state currently ranks 46 out of 50 for its high poverty level (4, 5). Our pediatric healthcare system employees are the only state board-certified, fellowship-trained pediatric urologists and are centrally located within a 150-mile circumference of the population. The distance required for in-person evaluation of pediatric urologic diseases can be economically and logistically challenging for patients and families. Consequently, our urology division implemented a telemedicine program almost 10 years ago and has reported the feasibility of telemedicine in multiple areas, such as postoperative evaluation, prenatal consultation, and follow-up management of enuresis (6–8).
The utilization of telemedicine for preoperative evaluation has been successfully implemented in the traditional clinic-to-clinic setting in recent years. However, with the onset of the COVID-19 pandemic, telemedicine evaluations were primarily performed with patients in their own homes rather than in a traditional clinic setting. The aims of the current study are to (1) compare the accuracy of preoperative telemedicine evaluations in the clinic and home settings to that of a traditional in-person appointment, (2) compare preoperative telemedicine evaluations in a traditional clinic setting to that of home telemedicine, and (3) compare parental satisfaction in each of these settings.
Materials and methods
Patients treated with initial preoperative evaluation using telemedicine at our institution between January 2011 and June 2020 were identified from the medical records and retrospectively reviewed after obtaining IRB approval (#261258). Within this cohort, both traditional clinic telemedicine patients (TM) and home telemedicine patients (TMH) were further subcategorized for the analysis. A control group of preoperative pediatric urologic patients (IP) matched by diagnosis and zip code was selected from the medical records for comparison. Patients in each subgroup were evaluated preoperatively by one of the three pediatric urologists at our institution. Exclusion criteria included patients less than 5 days or greater than 7 years of age, patients with non-English-speaking families, patients in Department of Human Services (DHS) custody, and preoperative telemedicine patients whose procedures had not been completed at the time of this study. Data on demographics, preoperative diagnosis and surgical plan, distance traveled for preoperative evaluation, diagnosis on the date of surgery, and surgical procedure conducted were obtained.
Children treated with TM were evaluated in an originating site clinic setting with the patient being triaged by the staff there and assisted through the telemedicine appointment by the nursing staff at the remote clinic. During the telemedicine appointment, a nurse obtained vital signs, oriented each patient to the teleconsultation, and then prepared them for the physical examination. During the examination, the physician at the distant site used a camera in the room at the originating site to obtain close-up views of the surgical area. When the clarity of the video image was poor, the nurse at the originating site would send a digital image via encrypted email to the physician. The videoconferences employed Internet Protocol transmission and commercial videoconferencing equipment (Edge 95 MXP, Cisco). A high-definition camera allowed a ×7 zoom and could be used to take snapshots of a conference. At the distant site at our institution, the display used was a high-definition screen located in a private conference room in the urology office. To adjust the necessary precautions related to the COVID-19 pandemic, patients were treated with TMH rather than TM. These patients and their caregivers completed an e-checkin and were triaged by nurses at a distant site in our clinic. High-resolution still images also were forwarded through the patient portal for most patients for review by a pediatric urologist to aid in decision-making. A standardized instruction guide for caregiver image acquisition was forwarded to the families with the e-checkin process. A telemedicine consultation room was used for both the TM and TMH evaluations with a low-tier device such as a smartphone or a tablet device used for TMH while connected through the hospital network or cellular connection.
For the IP cohort, a standard in-person evaluation was performed using surgical counseling by the pediatric urologist. Except in cases with scheduling conflicts, the patient is subsequently scheduled with the pediatric urologist who originally evaluated the patient preoperatively.
For all cohorts, the primary caregiver of each patient present at the preoperative visit was contacted by a research nurse and invited to participate in a follow-up questionnaire using a standard National Research Corporation (NRC) satisfaction phone survey. The NRC is a standard validated questionnaire designed for traditional in-person evaluation (Appendix A). Both telemedicine groups were queried with the validated telemedicine NRC questionnaire (Appendix B). Responses to the NRC questionnaire were documented on a Likert scale (Strongly Disagree 1–Strongly Agree 5). Greater scores indicate more satisfaction.
The primary end point, the accuracy of preoperative surgical planning, was compared across groups using a chi-square test. All other variables measured on a categorical scale were compared with either chi-square or Fisher’s exact tests, and the results are displayed as frequencies and percentages. Outcome variables measured on a continuum were evaluated for normality and equal variances. These variables were highly skewed; therefore, Wilcoxon’s rank-order test was conducted to compare groups. The median and inquartile range (IQR) were used to display the results of nonnormally distributed variables. All analyses were conducted in SAS software, version 9.4 (SAS Institute, Cary, NC, USA). P-values less than 0.05 were considered statistically significant.
Results
Charts from 116 patients (43 TM, 31 TMH, and 42 IP) were identified. Of these patients, 96 met eligibility criteria for satisfaction surveys, with the remainder excluded due to: the age of >7 (n = 12) at the time of the survey, DHS custody (n = 5), initial pre-op evaluation performed by an advanced practice nurse practitioner (n = 1), and non-English-speaking caregivers (n = 2).
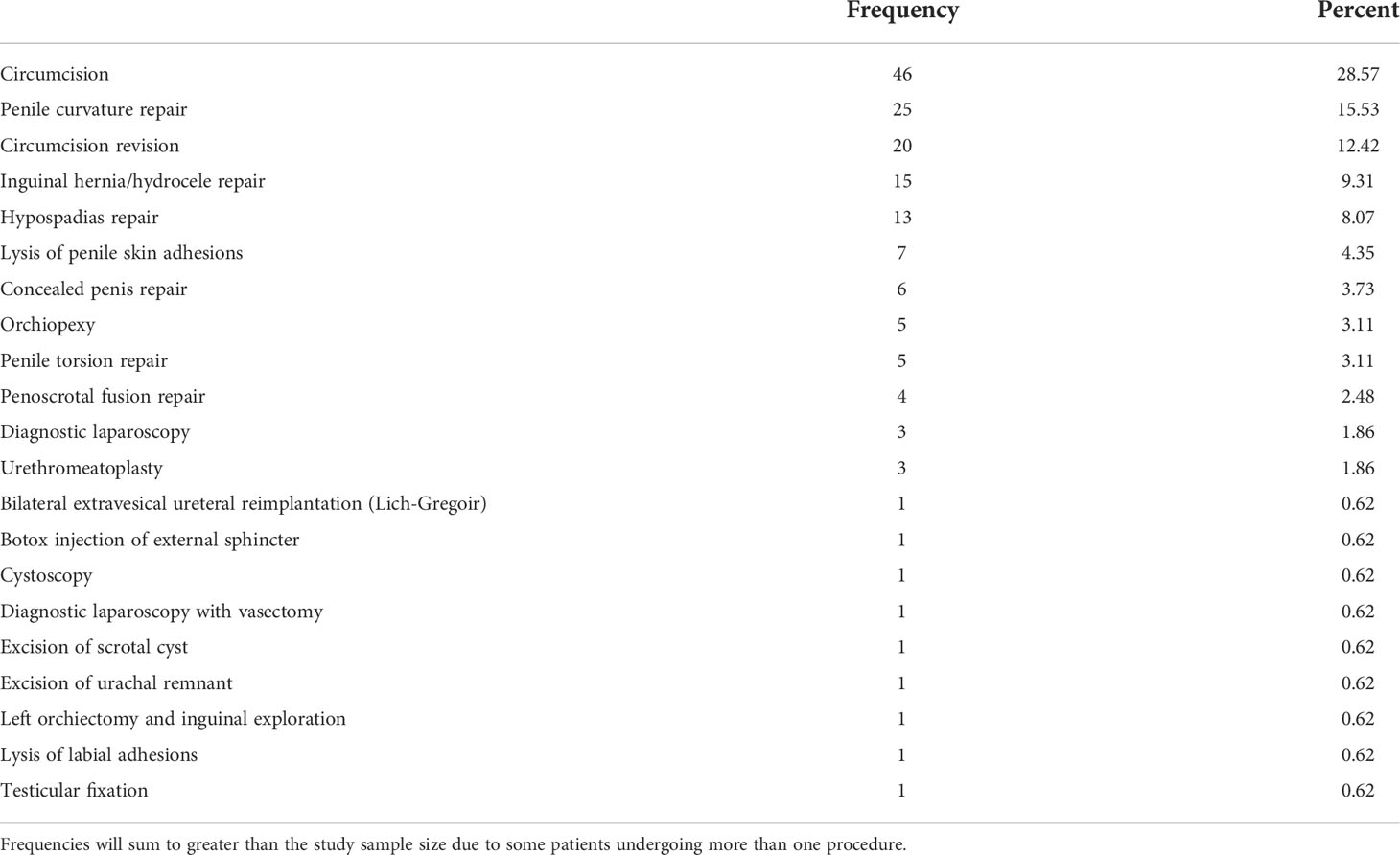
The 96 patients and caregivers included in the study yielded 58 preoperative telemedicine patients (34 TM and 24 TMH) and 38 traditional IP patients (Table 1). For TM, TMH, and IP patients, the median age was 10 months (IQR: 5–23), 4 months (IQR: 2–8), and 6 months (IQR: 2–12), respectively. A significant difference in the median age (p = 0.022) was noted between the TM and TMH subgroups. The distribution of ethnicity was predominantly non-Hispanic white for each group (p = 0.413).
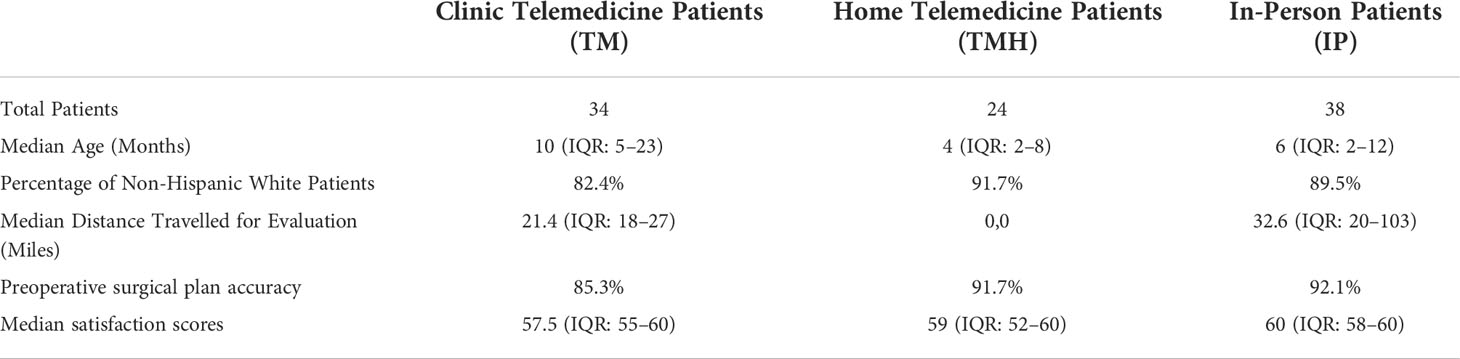
Table 1 Patient demographics, accuracy of reported preoperative diagnosis, and patients’ guardian satisfaction.
The median distance traveled (miles) was significantly greater for the IP group (median = 32.6; IQR: 20–103) compared to the TM group (median = 21.4; IQR: 18–27) (p = .004). Additionally, miles traveled for both IP and TM groups was significantly greater than the TMH group, which did not require travel for the evaluation (p <.001).
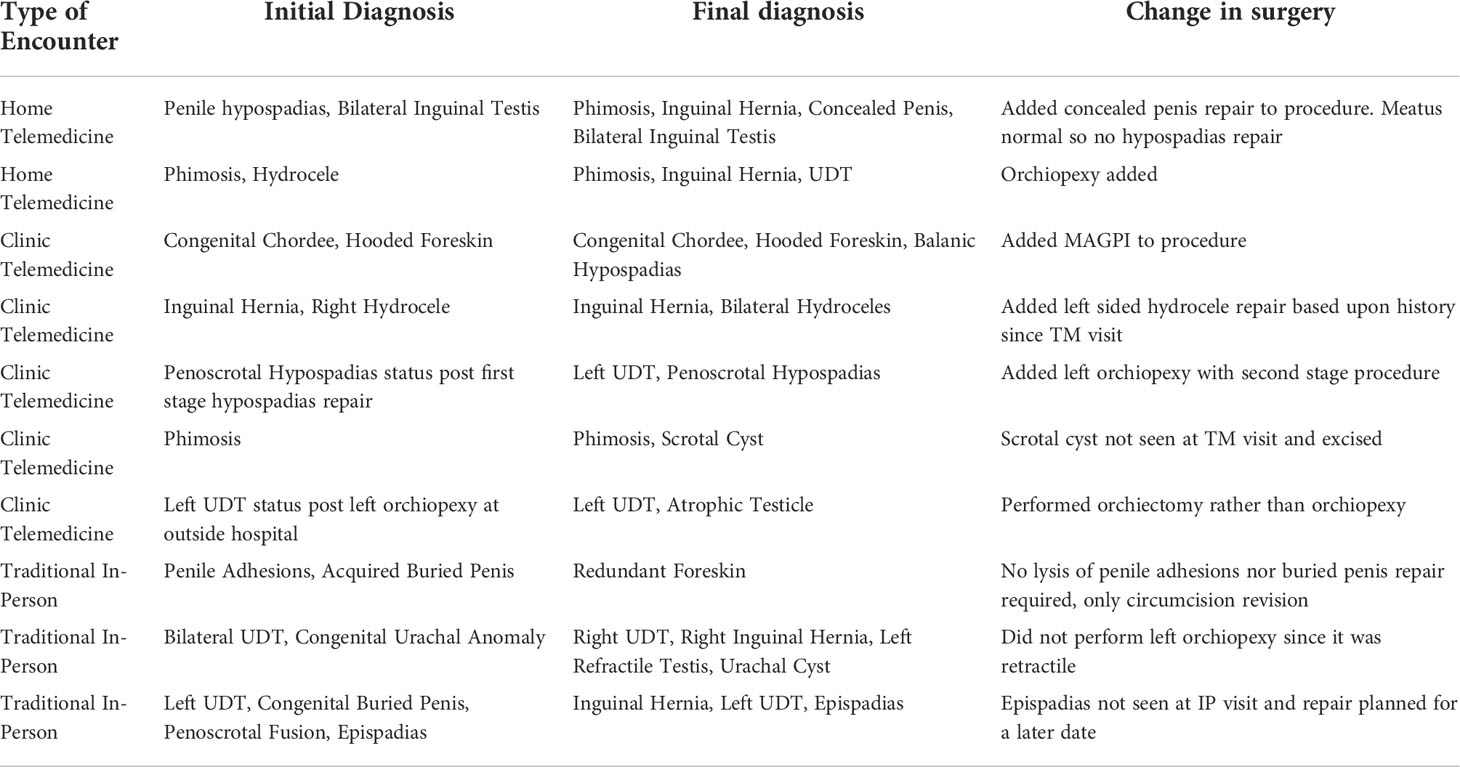
Various pediatric urologic procedures were performed for the three cohorts (Table 2). Preoperative assessment accuracy was equivalent in the three groups, with 29/34 (85.3%) TM patients, 22/24 (91.7%) TMH patients, and 35/38 (92.1%) IP patients having an accurate preoperative diagnosis and surgical plan (p = 0.69). The 10 patients who had a change in diagnosis and adjustment of the surgical planning on the date of the procedure are listed in Table 3. Various etiologies for the change in plan were noted, with the most common related to the presence, absence, or nature of undescended testes, with 4/10 patients requiring a change in plan on the date of surgery. An unexpected abnormality in the urethral meatus or lack thereof caused a change in diagnosis in 3/10 patients (presence/absence of hypospadias (2), epispadias (1)). Two of 10 patients had a change in plan for the management of buried or concealed penis.
Caregiver satisfaction was equivalent between the groups (p = 0.231) (Table 1), and satisfaction with telemedicine was equivalent between the TM and TMH cohorts (p = 0.913).
Discussion
Telemedicine has been used sparingly in the United States for the management of pediatric urologic patients post-surgery and for follow-up of medical conditions like enuresis. No evidence exists in the literature in this country examining its potential utility in the preoperative setting in urology (6–9). In addition to reports of management of medical diseases and postoperative follow-up, prior studies in Canada and Australia have demonstrated utilization of telemedicine in preoperative care in a standard clinic-to-clinic telehealth model. The initial study performed in 2002 in Saskatchewan demonstrated evidence of telehealth as an effective and acceptable means for delivering care. Thirty-three patients were scheduled for surgery, with 21 having completed their surgery at the time of the study and no errors in diagnosis or change in surgical management were reported (10). A subsequent study in 2005 consisted of a telemedicine cohort of non-Winnipeg patients to control groups of patients seen in person for non-Winnipeg and Winnipeg patients (11). A total of 443 patients were included with 272 day surgery patients of which 59 (21.7%) were preceded by a telehealth consultation. No difference was identified in cancellation rates or delay in diagnosis although there was a significantly higher rate of complications in the telehealth cohort. Further evidence of the utilization and benefits of telemedicine for preoperative consultation was shown in Brisbane, Australia (12). The initial study reviewed the usage of telemedicine in 3,880 patients seen by a pediatric surgeon over a 13-year period from 2000 to 2012. During a single year near the conclusion of the study period (July 2011–June 2012), 224 patients were treated by a general pediatric surgeon for disease processes often treated by pediatric urologists in other countries, such as phimosis, hydrocele, inguinal hernia, hypospadias, and others. The Brisbane group later published a follow-up study in 2018 (13). A total of 183 children had 224 videoconferences, resulting in 74 surgical bookings, with the majority of patients seen via telehealth not scheduled for surgery (109/183, 60%). A high diagnostic concordance was noted with 67 of 71 patients undergoing the planned procedure. The majority of patients with a change in plan were diagnosed with undescended testis. The current study represents the first preoperative telemedicine analysis from the United States in pediatric urology. The effectiveness of telemedicine in surgical planning was comparable in both the clinic-to-clinic telemedicine and the home telemedicine settings as compared to traditional in-person evaluation, with significantly less distance traveled for patient families in both telemedicine cohorts. A high concordance rate for accurate surgical planning was noted across cohorts. This provides evidence of the ability of home telemedicine to enable adequate preoperative planning for a variety of diagnoses with 91.7% accuracy.
Patient and family perception of preoperative telemedicine utilization has been appraised in prior studies in Canada and Australia. In the 2002 Saskatchewan study, first-time users were asked to complete a satisfaction survey (10). The mean rating of the overall treatment experience at Telehealth was favorable, with 100% reporting that they would use Telehealth again and would recommend it to another person. It is important to note that patients were arbitrarily selected by the pediatric surgeon based upon residential address in relative proximity to a telehealth site and indication(s) for clinical evaluation though. In a 2011 study performed in Edmonton, Canada, 259 pediatric surgical telehealth encounters were performed by multiple pediatric surgical subspecialties, with pediatric surgery (103) and pediatric urology (63) accounting for the majority of the patient care volume (14). A telehealth user questionnaire was administered to both patients and providers after their telehealth session. Eighty-three patient questionnaires were completed, with 97% of patients reporting satisfaction with their telehealth session. However, the number of preoperative consultations within this series was not reported. In 2004, the Brisbane group published their findings on the management of pediatric burn patients with a telehealth evaluation in which patient satisfaction was assessed as well (15). Patient satisfaction was measured on 25 patients. Overall, patient parent feedback was very positive, with all families reporting that their medical condition was adequately managed via videoconference. However, 2/25 families reported concerns that their appointment was not confidential, and 44% of families either reported strongly or with some degree of uncertainty that the videoconference was not as good as a face-to-face evaluation. Neither of these studies utilized a validated questionnaire for querying patient or family satisfaction with telemedicine. In contrast, the current study assessed primary caregiver satisfaction with a validated NRC questionnaire for all cohorts and also a validated, telemedicine-specific questionnaire for the two telemedicine groups. The overall satisfaction with utilization of telemedicine in the traditional telemedicine and the home telemedicine groups was equivalent to that of a control group of patients evaluated in-person.
Changes associated with the COVID-19 pandemic to limit the spread of the virus have caused many countries to loosen restrictions on telemedicine use to deliver patient care. In the USA, for instance, the Centers for Medicaid and Medicare Services (CMS) expanded utilization of telemedicine on a temporary and emergent basis under the 1,135 waiver and the Coronavirus Preparedness and Response Supplemental Appropriations Act. With this effort, CMS waived HIPAA requirements on telemedicine and has reimbursed Medicare for real-time telemedicine interactive communication for physicians, nurse practitioners, physician assistants, and other specified members of the healthcare team (16). These visits are considered the same as in-person visits and are allowable for the originating site to be in the home of the patient. As a result of these changes, rapid adoption of telemedicine has occurred in this country over the past year, especially in the first part of the pandemic, with increased telemedicine volumes still observed in the latter part of 2020 (17). Beyond the typical benefits of reduced travel and associated costs, other benefits of telemedicine during the COVID pandemic include increased social distancing and a decreased risk of exposure to the virus. Analysis of the utilization and impact of telemedicine utilization in pediatric urology during the pandemic has been limited (18). Turcotte et al. (9) and the group from Quebec City, Canada, evaluated the perception of the physician of the success of utilization of telemedicine during the first four weeks of telemedicine during the first four weeks of confinement.confinement. Based upon 1,679 total telemedicine appointments for 18 pediatric and adult urologists, two-thirds of the cases were believed to have been managed effectively (9). However, neither the methodology employed for telemedicine nor the patient perception or satisfaction were reported in this study. Moving forward, it would be beneficial to better understand the volume and impact of telemedicine utilization in this field during the pandemic in order to potentially improve patient care post-pandemic with broader utilization of telemedicine.
One component impacted by the pandemic in the usage of telemedicine was that of the originating site, where the patient was located at the time of the telemedicine evaluation. Previously, the utilization of standard clinic-to-clinic telemedicine was most commonly employed, likely due to the reimbursement requirement of a healthcare facility for the originating site. With the loosened restrictions in the US for telemedicine usage by CMS, home telemedicine became reimbursable during the pandemic. Although our state had previously allowed for the home of the patient to serve as the originating site, reimbursement for patients insured by Medicaid was not mandated until the allowances made for the pandemic. It is not surprising that most of the data published on telemedicine usage in pediatric urology involves standard clinic-to-clinic telemedicine, yet Smith et al. (12) and the Brisbane group reported that 1% of the telemedicine encounters in this study were performed via Skype while the patient was in their home. Although this was not reported, it is likely that the telemedicine encounters analyzed in the study by Turcotte et al. (9) also involved home telemedicine since patients were sequestered in their homes at the time of the study. The current study is the first such analysis of the utilization of home telemedicine for preoperative evaluation of patients, with evidence demonstrated in one cohort that preparation for pediatric urologic surgery is as effective with this modality as with that of traditional in-person evaluation. In our experience, engaging families in home telemedicine appears more streamlined and potentially more effective. Patients and their families appear more comfortable with the interaction, and the triaging process is typically is more efficient.
Shortcomings to the utilization of telemedicine in the clinic and at home for pediatric urologic preoperative evaluations do exist. Both bandwidth and connection speed impact the ability to perform telemedicine as well as the clarity of the encounter. The device or equipment that the clinic or family utilizes for the encounter plays an important role (15). For certain diagnoses that require significant clarity and resolution in visualizing a component of the physical examination, the ability to review a higher resolution image to supplement the real-time video interaction is important for surgical planning. For instance, the presence or absence of varying degrees of hypospadias in a patient with dorsal hood deformity and chordee is important for surgical equipment planning and the time allocated for the procedure. Also, certain physical examination findings require palpation. In pedatric urology, distinguishing retractile testes from truly undescended testes requires a skilled examiner either in person or at the originating site to establish the diagnosis. The findings of Browlee et al. underscore this challenge, with less than half (7/15) of patients booked for an orchidopexy having undergone the operation planned with the original teleconsultation (13). In the current study, 40% of patients with a change in plan on the date of surgery were related to inaccurate surgical planning for undescended testes, thus adding additional concern to the overall accuracy of telemedicine in management of undescended testes. Also, three patients had a change in surgical procedure upon retraction of the prepuce (Table 3), with one patient who had an unrecognized balanic hypospadias, one that was thought to have hypospadias but did not, and one who had an unrecognized epispadias. In each of these cases, physical examination of the person likely would not have revealed the ultimate diagnosis unless the prepuce had been forcefully retracted in the clinic before the day of surgery. Furthermore, the other 11 patients with hypospadias (11/13) were treated according to their original surgical plan without deviation in the postoperative diagnosis. High resolution still images were forwarded for all patients when adequate detail was not provided by the live video transmission, and this subjectively improved our confidence in the assessment of the presenting problem. Lastly, as compared to clinic-to-clinic telemedicine, patients requiring vital sign assessment, biometric monitoring with the necessary home equipment, or radiologic studies cannot be completely assessed with home telemedicine alone.
Limitations exist in the current study as well. First, it was a primarily retrospective study with inherent bias and a relatively small patient cohort. Due to study exclusions and timing limitations, the TMH group was slightly smaller than the TM and IP cohorts, which lessened the robustness of the data presented. Furthermore, although the survey component of the study was prospective, it was performed at different points in time for each group relative to their usage of telemedicine or evaluation in person in a traditional setting. A prospective study evaluating the usage of telemedicine compared with a control group in real-time with larger cohorts and prospective patient satisfaction surveys would be beneficial. Without randomization, though, inherent biases for or against the usage of telemedicine will likely exist. This type of study would also aid in broadening the understanding of the utility of home telemedicine in preparation for various diagnoses treated by pediatric urologists with surgical intervention.
Conclusion
The utilization of telemedicine for pediatric urological surgical planning may be as effective in accuracy and caregiver satisfaction as that of in-person evaluation. Less travel is required for preoperative pediatric urologic telemedicine patients, especially for those treated with telemedicine in the home setting. Limitations in the usage of telemedicine for the management of undescended testes exist.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the University of Arkansas for Medical Sciences Institutional Review Board. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author contributions
SC, JW, AP, and IZ contributed to the conception and design of the study. SC, JW, and BS administered the survey analyzed in this study. BS performed the statistical analysis. SC wrote the first draft of the manuscript. JW wrote sections of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fruro.2022.951036/full#supplementary-material
References
1. Marcin JP, Shaikh U, Steinhorn RH. Addressing health disparities in rural communities using telehealth. Pediatr Res (2016) 79(1-2):169. doi: 10.1038/pr.2015.192
2. Marcin JP, Ellis J, Mawis R, Nagrampa E, Nesbitt TS, Dimand RJ. Using telemedicine to provide pediatric subspecialty care to children with special health care needs in an underserved rural community. Pediatrics (2004) 113(1 Pt 1):1–6. doi: 10.1542/peds.113.1.1
3. Heath B, Salerno R, Hopkins A, Hertzig J, Caputo M. Pediatric critical care telemedicine in rural underserved emergency departments. Pediatr Crit Care Med (2009) 10(5):588–91. doi: 10.1097/PCC.0b013e3181a63eac
4. Arkansas . Available at: https://www.ers.usda.gov/webdocs/DataFiles/53180/25558_AR.pdf?v=0.
5. Poverty in Arkansas . Available at: https://www.welfareinfo.org/poverty-rate/arkansas/.
6. Canon S, Shera A, Patel A, Zamilpa I, Paddack J, Fisher PL. A pilot study of telemedicine for post-operative urological care in children. J Telemed Telecare (2014) 20(8):427–30. doi: 10.1177/1357633X14555610
7. Rabie NZ, Canon S, Patel A, Zamilpa I, Magann EF, Higley J. Prenatal diagnosis and telemedicine consultation of fetal urologic disorders. J Telemed Telecare (2016) 22(4):234–7. doi: 10.1177/1357633X15595556
8. Smith E, Cline J, Patel A, Zamilpa I, Canon S. Telemedicine versus traditional for follow-up evaluation of enuresis. Telemed J E Health (2021) 27(2):213–17. doi: 10.1089/tmj.2019.0297
9. Turcotte B, Paquet S, Blais AS, Blouin AC, Bolduc S, Bureau M, et al. A prospective, multisite study analyzing the percentage of urological cases that can be completely managed by telemedicine. Can Urol Assoc J (2020) 14(10):319–21. doi: 10.5489/cuaj.6862
10. Miller GG, Levesque K. Telehealth provides effective pediatric surgery care to remote locations. J Pediatr Surg (2002) 37(5):752. doi: 10.1053/jpsu.2002.32270
11. Postuma R, Loewen L. Telepediatric surgery: capturing clinical outcomes. J Pediatr Surg (2005) 40(5):813. doi: 10.1016/j.jpedsurg.2005.01.049
12. Smith AC, Garner L, Caffery LJ, McBride CA. A review of paediatric telehealth for pre- and post-operative surgical patients. J Telemed Telecare (2014) 20(7):400–4. doi: 10.1177/1357633X14552373
13. Brownlee GL, Caffery LJ, McBride CA, Patel B, Smith AC. Telehealth in paediatric surgery: Accuracy of clinical decisions made by videoconference. J Paediatr Child Health (2017) 53(12):1220–25. doi: 10.1111/jpc.13599
14. Shivji S, Metcalfe P, Khan A, Bratu I. Pediatric surgery telehealth: patient and clinician satisfaction. Pediatr Surg Int (2011) 27(5):523–6. doi: 10.1007/s00383-010-2823-y
15. Smith AC, Kimble R, Mill J, Bailey D, O'Rourke P, Wootton R. Diagnostic accuracy of and patient satisfaction with telemedicine for the follow-up of paediatric burns patients. J Telemed Telecare (2004) 10(4):193. doi: 10.1258/1357633041424449
16. Medicare Telemedicine health care provider fact sheet . Available at: https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-act-sheet.
17. The impact of COVID-19 on outpatient visits in 2020: Visits remained stable, despite a late surge in cases (2021). Available at: https://www.commonwealthfund.org/publications/2021/feb/impact-covid-19outpatient-visits-2020-visits-stable-despite-late-surge.
Keywords: pediatric urology, preoperative evaluation, telehealth, telemedicine, pediatrics
Citation: Canon S, Whitt J, Spray B, Patel A and Zamilpa I (2022) Efficacy and satisfaction of preoperative telemedicine evaluation of pediatric urologic patients. Front. Urol. 2:951036. doi: 10.3389/fruro.2022.951036
Received: 23 May 2022; Accepted: 06 July 2022;
Published: 05 August 2022.
Edited by:
Jason Van Batavia, Children’s Hospital of Philadelphia, United StatesReviewed by:
Mohan S. Gundeti, The University of Chicago, United StatesMarie Carmela Lapitan, University of the Philippines Manila, Philippines
Copyright © 2022 Canon, Whitt, Spray, Patel and Zamilpa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Stephen Canon, Y2Fub25zakBhcmNoaWxkcmVucy5vcmc=
 Stephen Canon
Stephen Canon Jedidiah Whitt
Jedidiah Whitt Beverly Spray4
Beverly Spray4