
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Urol., 06 June 2022
Sec. Pediatric, Adolescent and Developmental Urology
Volume 2 - 2022 | https://doi.org/10.3389/fruro.2022.895102
This article is part of the Research TopicWomen in Pediatric, Adolescent, and Developmental Urology: Volume IView all 11 articles
 Katerina Lembrikova1
Katerina Lembrikova1 George Aninwene II2
George Aninwene II2 Katherine L. Christensen3
Katherine L. Christensen3 Megha Tandel4
Megha Tandel4 Lorna Kwan2
Lorna Kwan2 Daniel Gonzalez-Padilla5
Daniel Gonzalez-Padilla5 Jeremy Teoh6
Jeremy Teoh6 Renea Sturm2*
Renea Sturm2*Introduction: Robotic adoption has rapidly increased within urology. Initial uptake in adult urology has outpaced that seen in pediatric procedures. The aim of this study was to determine adult and pediatric urologist satisfaction with specific procedural steps in lower urinary tract reconstruction (LUTR) using an open versus robotic approach and define drivers and barriers to robotics adoption to inform device development relevant to current needs.
Methods: A survey was distributed to practicing urologists. Questions assessed surgeon demographics, technology adoption, satisfaction with anastomotic steps in continent neobladder (CN) and augmentation cystoplasty (AC), and drivers/barriers influencing robotic use.
Results: Of 110 respondents, 49% practiced in academic institutions; 51% reported non-academic, private, or other. Specializations were pediatrics (36%), oncology/robotics (25%), or other (39%). Sixty-eight percent completed training in the past decade. In the past year, 55% completed only open CN or AC, 36% only robotic, and 9% both. Of those that performed robotic procedures, 5% used only an intra-corporeal approach, 85% used only extra-corporeal, and 10% used both. Surgeons who performed robotic LUTR alone expressed high satisfaction with all CN and AC procedural steps evaluated. Overall, of the anastomoses evaluated, urologists found urethrovesical anastomoses more satisfactory using a robotic versus open approach. Pediatric versus adult urologists were overall less satisfied with the robotic approach. In terms of robotic adoption, major drivers for CN were adoption by neighboring institutions, improved perioperative outcomes, and equivalent oncological outcomes; barriers were cost of robotic purchase and maintenance, surgeon support for robotics, and difficult learning curve. Major drivers for AC were adoption by neighboring institutions, decreased operative time, and equivalent oncological outcomes; barriers were increased operative time, cost, and minimal perceived benefit of extracorporeal procedures.
Conclusion: Urologic oncologists and surgeons performing robotic LUTR alone were highly satisfied with the robotic approach. Pediatric urologists reported lower overall satisfaction with robotic steps in LUTR, potentially corresponding with limitations of current robotic platforms for pediatric application and relative training exposure. Major drivers overall were competition and outcomes; major barriers were cost, operative time, and learning curve. Based on this select surgeon cohort recruited through targeted social media platforms, maximizing surgeon experience through training and innovations to reduce complication rates is anticipated to facilitate broader adoption of robotics in LUTR. Future studies that include a broad international distribution across the specialty may further pinpoint specified needs for adult versus pediatric specialists and drive targeted robotics platform development.
The introduction of the da Vinci® surgical system over 20 years ago was followed by rapid adoption in the field of urology, with demonstrated effectiveness for both oncological and benign conditions (1). Based on data from the National Cancer Database, the proportion of robotic-assisted radical cystectomies performed in the United States increased from 22% in 2010 to 40% by 2015, with rates exceeding 50% in recent multicenter series (2). In pediatrics, robotic application to lower urinary tract reconstruction (LUTR) has lagged behind this adoption trend, potentially reflecting a prioritization of platform development and testing for adult procedures by surgical and robotic device companies (2, 3). Furthermore, evidence remains inconclusive regarding the value proposition for application of the surgical robot to LUTR (4). A study across practice types and specialties within urology is needed to better understand the myriad factors that influence both adult and pediatric urologists in surgical approach selection for these cases.
While surgeon perspectives regarding preferred approach are based on multiple factors, several key themes can be observed in discussions with surgeons and the available data that may inform robotics use in LUTR (5). These include risk of perioperative complications, long-term outcomes (e.g., oncological, continence), surgical training and volume, patient–surgeon decision-making, device limitations, and market factors. Consistent with the relative surgical complexity and patient comorbidity profile of individuals undergoing a CN or AC, perioperative complications are common and costly (6). The role of robotics to decrease perioperative complication rates in LUTR has yet to be established and may differ between intracorporeal versus extracorporeal approaches (7). A randomized controlled multi-center trial (Randomized Open versus Robotic Cystectomy, RAZOR) has reported 2-year non-inferiority overall between open versus extracorporeal robotic procedures in the primary outcome of progression-free survival. In a review of related publications, the potential value of robotics must be further balanced against higher cost and longer operative time; the data regarding the effect of this on morbidity are conflicting (8, 9). Similarly, there are studies that report an advantage in terms of length of stay with RARC and robotic AC, while others indicate equivalent outcomes (8–10). Put together, available data regarding outcomes alone do not fully explain the gradual trend toward increased robotics use in LUTR.
Another factor cited by surgeons that influences decision-making regarding preferred surgical approach includes educational background and training in robotics. As robotics exposure has increased in training overall, graduating residents and fellows may select the procedural approach with which they have the most experience. However, robotic LUTR remains low volume at most sites, limiting the potential for the majority of trainees to complete the approximately 40 robotic cystectomies required before reaching an operative time plateau (11). Such factors will continue to impact robotics adoption in LUTR; however, as is noted in relation to outcomes data, educational factors and experience alone do not fully explain the gradual increase in robotics adoption in LUTR.
Other influences driving the adoption of the robotic approach may stem from non-clinical considerations. The decision regarding surgical approach includes the impact of joint decision-making between the patient and their surgeon. From a patient standpoint, the decision regarding operative approach and surgeon selection additionally may include factors such as financial constraints, insurance reimbursement, surgeon preference, and local availability of the surgical robot (12). Beyond LUTR in bladder cancer, robotic AC in pediatrics may be further limited as instrumentation, and devices designed for the adult patient can present unique challenges when applied to infants and small children (13). Put together, factors impacting approach to LUTR are broad and incompletely understood, extending beyond outcomes data to include surgeon training, patient, and network-based factors.
The aim of this study was to investigate the relative impact of a range of potential influences on surgeon adoption of robotics in LUTR, including both CN and AC. Specifically, this study evaluated the impact of specialized urologic practice areas and/or current robotics use in CN or AC on preferences for technology adoption, satisfaction with specific anastomoses performed during each procedure, and perceived benefits versus barriers to robotics adoption.
An international survey using Qualtrics XM (14) was distributed to practicing urologists through targeted social media channels, including Twitter, Facebook, LinkedIn, and Urologic List-Servs. Initial questions assessed practice location and setting, training, and targeted procedural volume. The remainder of the survey assessed general and surgical technology adoption, suitability of open versus robotic approaches for specific procedural steps in CN and AC (range, 0–10; 10 as best), and drivers/barriers reported to impact robotic use in these procedures. For technology adoption, respondents were asked to describe themselves as loving and being first to experiment with, liking and using before most, using when most people are, using as one of the last people, or skeptical of new technologies (15). For suitability of procedural steps, respondents were asked to rate the GI tract, bowel-to-bladder or bladder-to-bladder anastomoses/closures. They were also asked to rate the following based on procedure: ureteroenteric and urethrovesical anastomoses for CN versus appendix isolation and catheterizable channel implantation for AC. For drivers and barriers, respondents were asked to identify major barriers from a list of choices that were developed through a rigorous interview process of stakeholders in the urologic robotic industry via the National Science Foundation I-Corps program (5, 16). Respondents were excluded due to incompleteness if surveys lacked responses regarding urologic specialty, technology, or surgical device adoption.
Each survey section was analyzed by provider specialty and by use of surgical approaches in LUTR. Provider specialty was categorized into three groups: pediatrics, oncology plus robotic surgery, and other, which included andrology, endourology/stone disease, female pelvic medicine and reconstruction, general urology without subspecialty, laparoscopic surgery, male genitourinary reconstruction, renal transplantation, and others. Surgical approach was categorized into three groups: open only, robotic only, or both open and robotics utilization. Respondent characteristics, technology adoption, and drivers/barriers were presented as frequencies by group and suitability scores were presented with box-and-whisker plots comparing across groups by medians (IQR). All analyses were conducted using SAS 9.4 (SAS Institute Inc, Cary, NC) and were two-sided with an α level of 0.05 for statistical significance.
A total of 174 individuals initiated the survey. Of those, 64 were excluded due to incompleteness (20 missing specialty and adoption questions, 44 missing at least one adoption question); 110 were included in the analysis. Table 1 provides a summary of the survey respondent characteristics by provider specialty. Approximately half of the participants were employed by an academic medical center (49%) and completed their training after 2014 (50%). Approximately three of four urologists had access to a da Vinci robot within their institution of practice (76%). Those without access to a da Vinci robot resided in Africa (65%), South America (31%), and the United States (4%). Of those with access to a robot, 66 of 84 (79%) performed robotic LUTR procedures in the past year; 9 of 84 (11%) performed more than 100 robotic LUTR procedures annually. Most surgeons with access to a robot performed 1–30 robotic LUTR procedures annually (56%). CN and ileal conduit procedures were performed by urologists with a practice focus in oncology or robotic surgery (65% and 49%, respectively), while augmentation cystoplasties were more often performed by pediatric urologists (43%). Regardless of LUTR procedure (ileal conduit, CN, or AC), urologists across all specialties reported that an extracorporeal robotic approach to urinary diversion was most common (range, 82%–100%).
General and surgical technology adoption differed across reported use of open versus robotic surgical approaches but not by provider specialty (Figures 1A–D). Consistent with their adoption of robotics, providers who reported only use of the robotic approach in CN or AC scored higher on the innovation curve than providers who only used an open approach; this finding was observed for both general and surgical technology adoption (57% vs. 24%–25% and 43% vs. 11%–17%, respectively). However, regardless of surgical approach or specialty, participating urologists overall scored highly on measures of willingness to adopt new technologies and surgical devices (15).
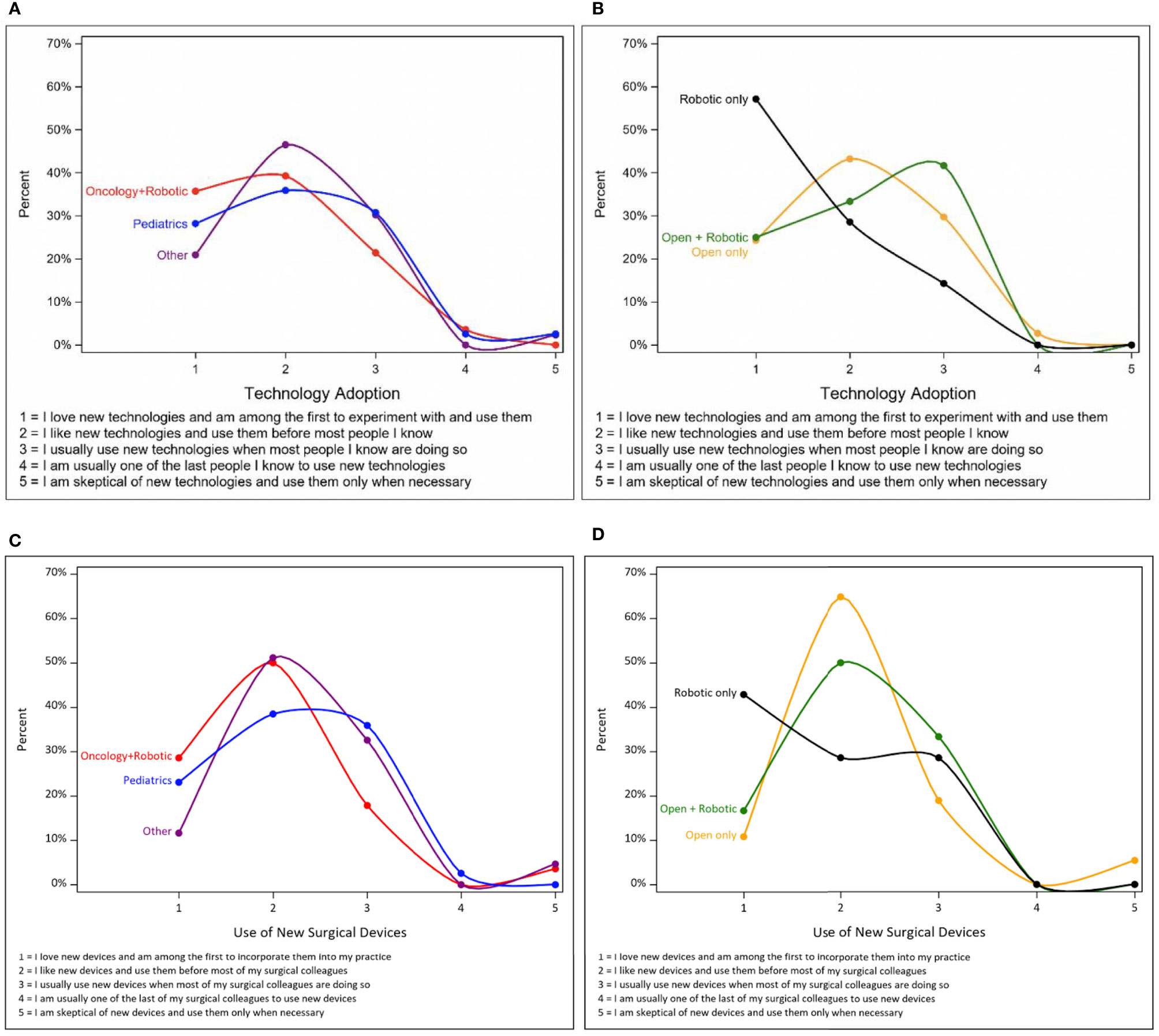
Figure 1 General technology and new medical device adoption by surgical approach and provider specialty. (A) Technology adoption by surgical approach. (B) Technology adoption by provider specialty. (C) Surgical device adoption by surgical approach. (D) Surgical device adoption by provider specialty.
The next set of questions evaluated urologist satisfaction with specific procedural steps, evaluating the impact of urologic specialty and robotic experience in LUTR (Figure 2A; Supplementary Table S1A). Median responses for pediatric urologist satisfaction with all assessed anastomotic steps in an open AC was 9.0; for a robotic AC satisfaction with anastomoses was lower, ranging from 3.0 to 7.5. The lowest scores across fields, indicating less satisfaction with the procedural step, were assigned to the ureteroenteric and urethrovesical anastomoses regardless of approach. Urologist satisfaction with these same procedural steps was also assessed based on reported robotic and open LUTR experience (Figure 2B; Supplementary Table S1B). Urologists using both open and robotic approaches to CN or AC reported an overall lower median satisfaction with anastomoses using a robotic approach versus their respective satisfaction with the open approach for each procedure. Among urologists using only an open approach, a similar trend was observed with lower overall median satisfaction provided for anastomoses using a robotic versus open approach. On the contrary, those who only completed robotic LUTR in the past year reported higher satisfaction with the robotic approach for varied anastomotic steps. Of note, however, there were only three providers (two with the open and robotic approach and one with only robotic approach) that performed robotic AC, therefore limiting analysis within this cohort.
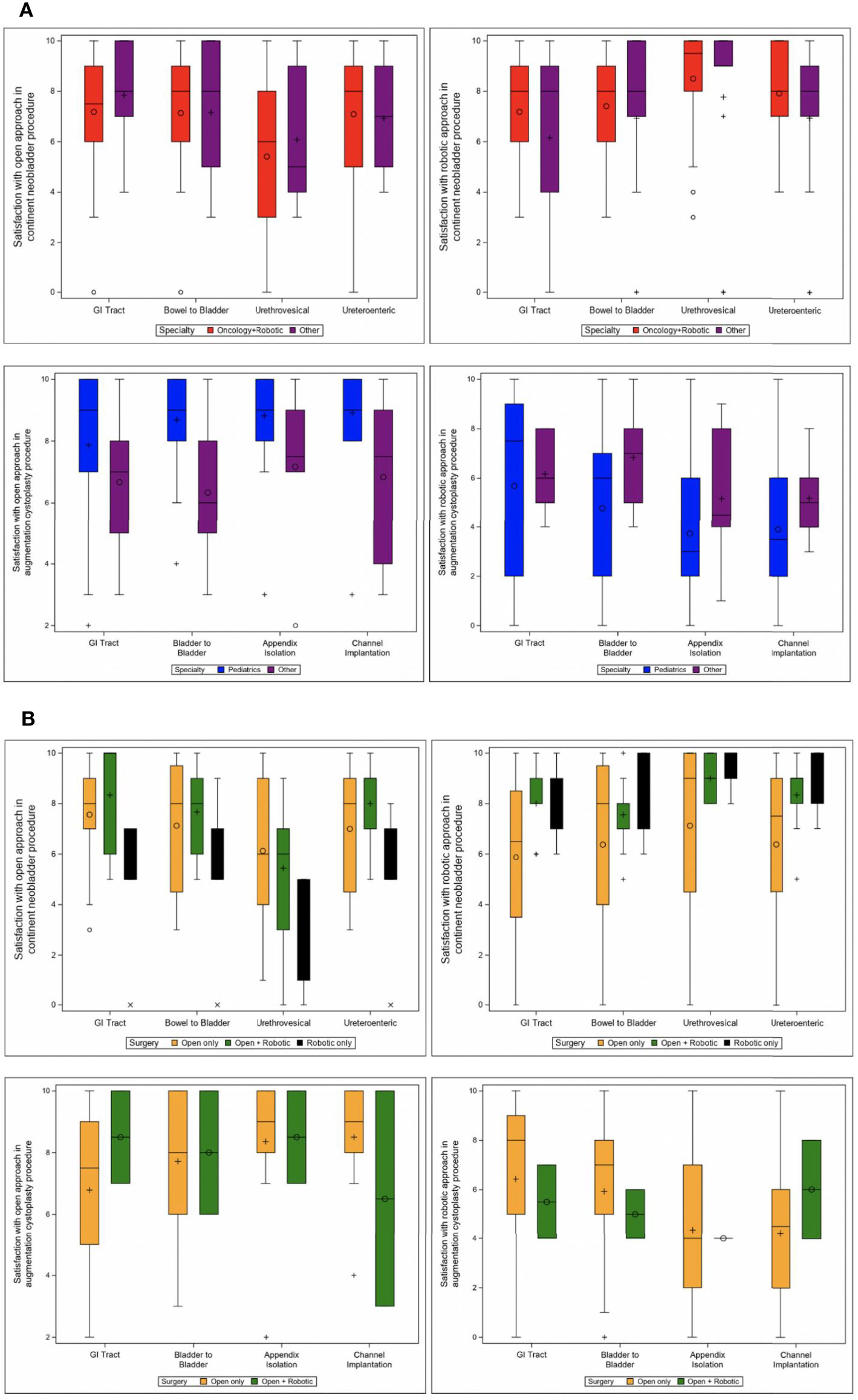
Figure 2 Rating of satisfaction of procedural steps for continent neobladder and augmentation cystoplasty. (A) Satisfaction by specialty. (B) Satisfaction by surgery type. Other includes: andrology, endourology/stone disease, female pelvic medicine and reconstruction, general urology without subspecialty, laparoscopic surgery, male genitourinary reconstruction, renal transplantation, and other.
The final survey section assessed perceived barriers and drivers to the adoption of robotic surgery for each of the specific procedures, CN and AC (Table 2). Overall, the top 3 perceived drivers for robotic adoption of CN were adoption by neighboring institutions, improved perioperative outcomes, and equivalent oncological outcomes, while the top 3 barriers were the cost of robotic purchase and maintenance, surgeon support for robotics, and difficult learning curve. The top 3 perceived drivers for robotic adoption of AC were adoption by neighboring institutions, decreased operative time, and equivalent outcomes, while the top 3 barriers were increased operative time, cost, and minimal perceived benefit of extracorporeal procedures.
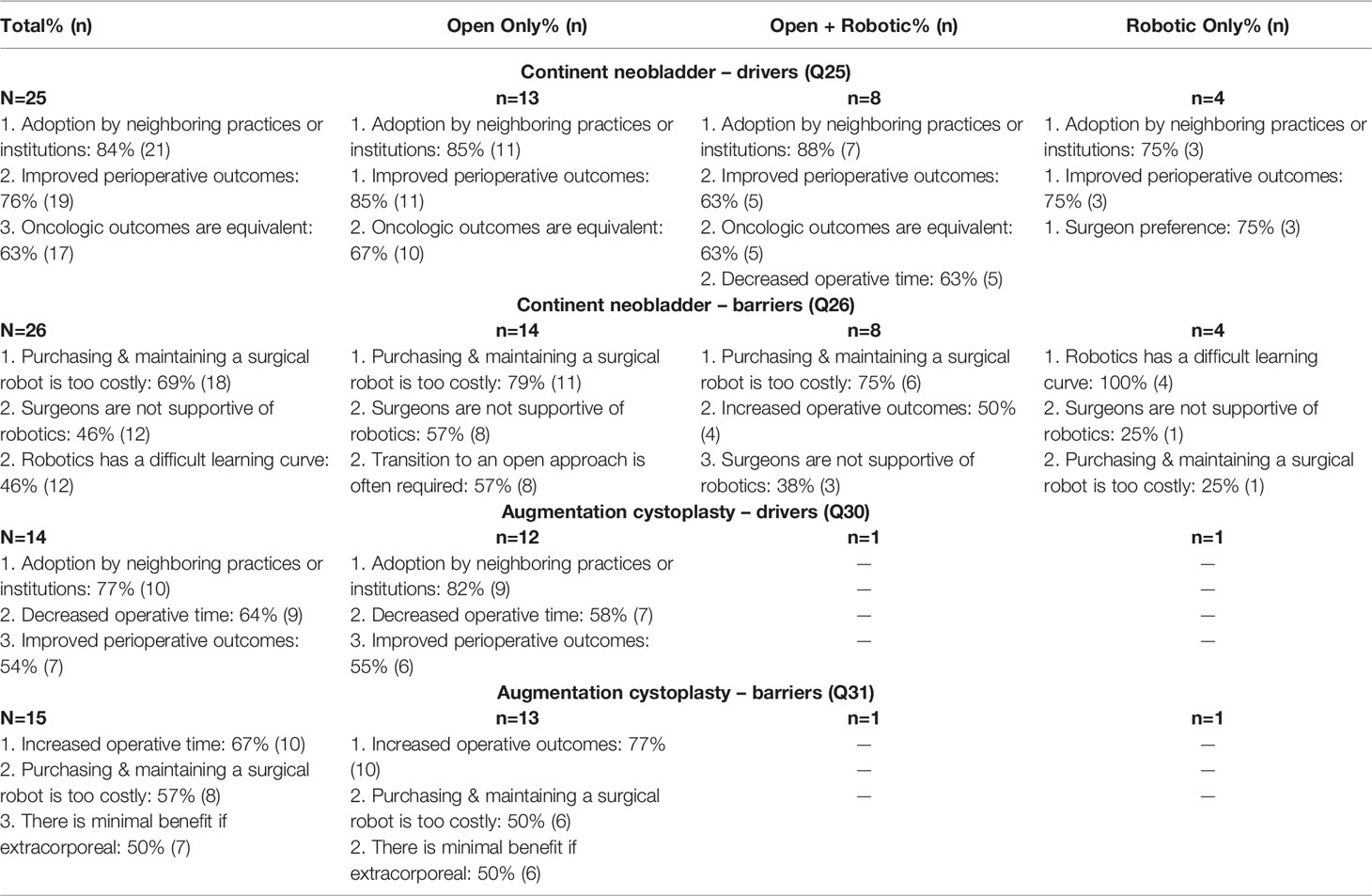
Table 2B Top drivers/barriers for continent neobladder and augmentation cystoplasty by surgical approach.
Specific to their experience with each surgical approach, urologists that currently perform only robotic CN cited the difficult learning curve as the top barrier, while those that performed open CN perceived cost as the greatest barrier. The only responses that were received for AC came from surgeons who performed open procedures, who reported that the greatest barrier to robotics use was a lack of evident improvement in operative outcomes. All respondents agreed that adoption by neighboring practices or institutions remained the greatest driver for both CN and AC, demonstrating the importance of factors beyond the surgeon, patient, or hospital system in isolation. Responses by specialty likewise demonstrated that urologists specializing in oncology and robotics found the greatest barrier for robotic adoption for CN to be cost. Other non-pediatric providers found the learning curve to be the greatest barrier. When looking at AC, pediatric urologists and other non-urologic or robotic providers perceived increased operative time to be the greatest barrier.
To our knowledge, this is the first international survey evaluating the influence of urologic specialty and robotics experience on a myriad of factors influencing their use of surgical robotics for LUTR. We have found that urologist demographics, their perception of technology, satisfaction with procedural steps, and overarching barriers and drivers in the field all have an impact on this complex decision-making process. While multiple series in adult and pediatric urology have evaluated complication and readmission rates across these procedures in the short term, the consensus regarding the utility of robotics in LUTR among the urologic community is dissonant. Understanding the factors that drive the decision to utilize the surgical robot in LUTR more broadly is crucial to identify specific target areas for innovation and procedural enhancement. The distribution of an international survey to urologists of various backgrounds and specialty focus areas led to novel findings and provides an early vantage point to inform broader surveys and qualitative studies in this area.
This study is unique in the urology field in pairing drivers and barriers with an established measure of technology adoption commonly used in market evaluation. Our assessment was based on an iteration of the scientist Everett Rodger’s Diffusion of Innovations who proposed five defined sub-populations based on their enthusiasm and motivation to adopt innovative solutions: innovators, early adopters, early majority, late majority, and laggards (15). Overall, respondents in this study were categorized as highly to moderately innovative in terms of technology and surgical device adoption, representing the categories of innovators, early adopters, and early majority. That is, these are individuals who love, like, or use new technologies when other people are doing so, respectively. Although surgeons within the oncology and robotics fields were enthusiastic regarding their preferences for adoption of both general and surgical technology; there was no significant difference overall between pediatric and adult specialties. However, surgeons that only performed robotic procedures in the past year for LUTR were the most innovative on the adoption curves, representing an enthusiasm for new technologies that is reflected in their practice. The trend observed in our respondents demonstrates an affinity and trust toward novel surgical technology, an observation that can be leveraged when introducing new surgical equipment and may affect robotic adoption overall in this field.
When assessing urologist satisfaction with specific anastomotic steps in the CN and AC procedures, urologists overall reported that both approaches were satisfactory. However, there were trends observed between specialty and experience and satisfaction with an open versus robotic approach. For example, pediatric urologists had the lowest satisfaction scores for the robotic approach in AC and the highest for the open approach. However, it is noteworthy that within our sample of participants, most pediatric urologists performed surgeries exclusively via the open approach, while fellowship-trained urologic oncologists and robotic surgeons performed the greatest number of robotic LUTR procedures. These differences may be influenced by differences in robotic training by specialty and limitations in applying tools created for adult applications in pediatrics (17). Further studies are needed with a broader cohort of pediatric urologists to fully understand these drivers and barriers, including an expanded international component. Regardless, findings of the adoption curve across subspecialties in this survey are indicative of an innovative cohort that will be poised to adopt novel technologies and surgical advancements in the future.
Specific to the anastomotic step in the open CN, the urethrovesical and ureteroenteric anastomoses had the lowest satisfaction scores. Satisfaction with the robotic approach did not show the same variation. The study did not provide additional data regarding the specific reasons for satisfaction or dissatisfaction with these steps; this is an area for further evaluation. However, it is notable that participants who perform both open and robotic procedures reported less satisfaction with open anastomotic steps for the open approach versus those who perform only robotic procedures. Putting together the data regarding use of robotics and provider satisfaction with these procedural steps, it is possible that experience and perceived suitability of the robot for specific steps in the procedure are driving forces in robotics use, requiring further evaluation.
As hypothesized, multiple factors beyond cited patient outcomes affect technology adoption in this arena and will continue to drive the use of additional minimally invasive platforms as they enter this expanding market. The current study identified that adoption by neighboring institutions and improved perioperative outcomes were top drivers, and cost, operative time, and learning curve were top barriers. Of note, while much of the current literature surrounding this topic is focused on perioperative outcomes and readmissions, our survey responses showed that adoption by other institutions surpassed improved outcomes as a major driver. This parallels data regarding choice of technique for other procedures, such as management of vesicoureteral reflux in which it has been demonstrated that Deflux injection was selected based primarily on surgeon preference in exclusion of other factors including risk of failure and re-operation rates (18). Based on these findings, cost-effective interventions that achieve improved outcomes in complex procedures across multiple hospital settings and systems are needed to facilitate robotics adoption. Additional studies that quantify the necessary advances in learning curve and operative time required can further facilitate this trend.
A less anticipated finding was that the patient preference or demand for the surgical robot was not viewed as a major driver by either adult or pediatric urologists. Prior market analyses are conflicting in the relative effect of competition on hospital robotic adoption. A recent study looked at robotic acquisition data in a database of California hospitals to develop a model based on hospital characteristics and found that market competition did not significantly drive adoption of robotic surgical systems. Specifically, the authors found that hospitals in high volume markets were 12% more likely to purchase a surgical robot, while market competition increased that chance by only 2% (19). These findings from recent literature, combined with the findings from our survey, suggest that competition is multifactorial and that surgeon perspectives may differ from observed market trends.
Limitations of the study include a small sample size (n=110) and a potential sampling bias due to the use of social media for recruitment of actively practicing urologists. Additionally, although the recruitment methods facilitated targeting individuals with an increased interest in robotic surgery and AC or CN in particular, the study had relatively high rates of missingness. One of our observations is that this often occurred at the point in the study when the focus became these relatively less commonly performed procedures and may further skew the responses received. Despite the fact that intracorporeal diversions overall have increased in use particularly in centralized study sites (20–22), based on the low number of respondents in this study that have completed intracorporeal procedures in the past year, our sample has not captured this trend. Providing that over half of the participants reside in the United States and Europe, regional differences in surgical choice may also not have been accurately captured due to the study geographic distribution. Our cohort overall was earlier in practice than the field as a whole; this age difference and/or the innovativeness observed may be reflective of their presence on and engagement with social media platforms. Increased exposure to pediatric urology and robotics earlier during residency may also affect scores and perceptions in a generational manner. Future studies with expanded number of participants and demographics to include residents and fellows, additional international participants to allow evaluation by location, and urologists through societies or other distribution methods not limited to social media may provide additional insights that were not captured by this study.
Put together, the factors for robotic adoption in LUTR are complex and extend beyond documented complication rates and patient outcomes. Rather, a more complete understanding of trends in robotics use will incorporate the role of competitors within the surgical market, improve perioperative outcomes, minimize cost, address learning curve and operative time regardless of practice volume, and acknowledge surgeon preferences. Furthermore, specific anastomotic steps and the unique challenges that they present in pediatric versus adult patients need to be addressed with focused learning and innovation to improve surgeon satisfaction. Each of these factors must be assessed and tackled by urologists and medical device companies alike if increased adoption is desired. Urology is an innovative field and is poised to tackle these unique challenges. A thoughtful consideration and further analysis of the wealth of experience and factors that influence robotics adoption is needed to ensure the ultimate aim of improved patient outcomes and minimized complications in complex procedures regardless of surgeon experience or hospital setting.
Current evidence exists for and against the use of the surgical robot in LUTR, with a focus on CN and AC. Pediatric urologists are overall less satisfied with the robotic approach for AC, as compared to urologic oncologists and surgeons who perform robotic LUTR alone who reported high levels of satisfaction with the robotic approach for varied sutured anastomoses. However, regardless of specialty focus and approach, ureteroenteric and urethrovesical anastomoses had the lowest satisfaction scores and are recommended areas for future targeted education and innovation. Major drivers for robotic use include competition across hospital systems and improved perioperative outcomes. Cost, operative time, and learning curve continue to be major barriers across subspecialties to robotics use in LUTR. Training modifications to maximize surgeon experience with targeted procedural steps, innovation to address high complication rates regardless of approach, and ensuring patient awareness of varied surgical offerings are anticipated to facilitate the ongoing trend toward increased robotics use in LUTR.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethical review and approval was not required for the study on human participants, in accordance with the local legislation and institutional requirements.
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The authors would like to acknowledge members of the following groups who participated in our survey, and their moderators for assistance with survey distribution: Facebook Robotic Urology Collaboration—RUC Group, Women Docs in Urology, #UroSoMe Twitter, and Pediatric Urology List-serv.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fruro.2022.895102/full#supplementary-material
1. Buffi NM, Lughezzani G, Hurle R, Lazzeri M, Taverna G, Bozzini G, et al. Robot-Assisted Surgery for Benign Ureteral Strictures: Experience and Outcomes From Four Tertiary Care Institutions. Eur Urol (2017) 71(6):945–51. doi: 10.1016/j.eururo.2016.07.022
2. Elshabrawy A, Wang H, Dursun F, Kaushik D, Liss M, Svatek RS, et al. Diffusion of Robot-Assisted Radical Cystectomy: Nationwide Trends, Predictors, and Association With Continent Urinary Diversion. Arab J Urol (2022), 1–9. doi: 10.1080/2090598X.2022.2032562
3. Fuchs ME, DaJusta DG. Robotics in Pediatric Urology. Int Braz J Urol (2020) 46(3):322–7. doi: 10.1590/s1677-5538.ibju.2020.99.03
4. Zhao CC, Shakir NA, Zhao LC. The Emerging Role of Robotics in Upper and Lower Urinary Tract Reconstruction. Curr Opin Urol (2021) 31(5):511–5. doi: 10.1097/MOU.0000000000000908
5. Lembrikova K, Aninwene G, Tebon P, Becker M, Siapno A, Yamashiro J, et al. A Qualitative Assessment of Drivers, Barriers, and Value in Robotic-Assisted Lower Urinary Tract Reconstruction. J Urol (2021) 206:e941. doi: 10.1097/JU.0000000000002083.08
6. Zhang JH, Ericson KJ, Thomas LJ, Knorr J, Khanna A, Crane A, et al. Large Single Institution Comparison of Perioperative Outcomes and Complications of Open Radical Cystectomy, Intracorporeal Robot-Assisted Radical Cystectomy and Robotic Extracorporeal Approach. J Urol (2020) 203(3):512–21. doi: 10.1097/JU.0000000000000570
7. Balzano FL, Chan KG. Review of Intracorporeal and Extracorporeal Continent Urinary Diversion - Where do We Stand in 2021? Mini-invasive Surg (2021) 5(41):1–8. doi: 10.20517/2574-1225.2021.49
8. Tyritzis SI, Wiklund NP. Is the Open Cystectomy Era Over? An Update on the Available Evidence. Int J Urol (2018) 25(3):187–95. doi: 10.1111/iju.13497
9. Cohen AJ, Brodie K, Murthy P, Wilcox DT, Gundeti MS. Comparative Outcomes and Perioperative Complications of Robotic Vs Open Cystoplasty and Complex Reconstructions. Urology (2016) 97:172–8. doi: 10.1016/j.urology.2016.06.053
10. Tyritzis SI, Gaya JM, Wallestedt-Lantz A, Pini G, Everaerts W, de Naeyer G, et al. Current Role of Robotic Bladder Cancer Surgery. Minerva Urol Nefrol (2019) 71(4):301–8. doi: 10.23736/S0393-2249.19.03435-0
11. Guru KA, Perlmutter AE, Butt ZM, Piacente P, Wilding GE, Tan W, et al. The Learning Curve for Robot-Assisted Radical Cystectomy. JSLS (2009) 13(4):509–14. doi: 10.4293/108680809X12589998404128
12. Gunaratnam C, Bernstein M. Factors Affecting Surgical Decision-Making-A Qualitative Study. Rambam Maimonides Med J (2018) 9(1):1–8. doi: 1RMMJ.10324/RMMJ.10324
13. Gundeti MS, Castellan MA. Editorial: Robotic Assisted Laparoscopic Surgery (RALS) in Pediatric Urology. Front Pediatr (2020) 8:85. doi: 10.3389/fped.2020.00085
14. Qualtrics Xm. Available at: https://www.qualtrics.com/.
15. Petkova H, Schanker B, Samaha D. Barriers to Innovation in the Field of Medical Devices. Netherlands: World Health Organization (2010).
16. National Science Foundation I-Corps. Available at: https://www.nsf.gov/news/special_reports/i-corps/.
17. Sheth KR, Koh CJ. The Future of Robotic Surgery in Pediatric Urology: Upcoming Technology and Evolution Within the Field. Front Pediatr (2019) 7:259. doi: 10.3389/fped.2019.00259
18. Esposito C, Yamataka A, Varlet F, Castagnetti M, Scalabre A, Fourcade L, et al. Current Trends in 2021 in Surgical Management of Vesico-Ureteral Reflux in Pediatric Patients: Results of a Multicenter International Survey on 552 Patients. Minerva Urol Nefrol (2021). doi: 10.23736/S2724-6051.21.04430-X
19. Shen C, Gu D, Klein R, Zhou S, Shih YT, Tracy T, et al. Factors Associated With Hospital Decisions to Purchase Robotic Surgical Systems. MDM Policy Pract (2020) 5(1):2381468320904364. doi: 10.1177/2381468320904364
20. Ahmed K, Khan SA, Hayn MH, Agarwal PK, Badani KK, Balbay MD, et al. Analysis of Intracorporeal Compared With Extracorporeal Urinary Diversion After Robot-Assisted Radical Cystectomy: Results From the International Robotic Cystectomy Consortium. Eur Urol (2014) 65(2):340–7. doi: 10.1016/j.eururo.2013.09.042
21. Martin AS, Corcoran AT. Contemporary Techniques and Outcomes of Robotic Assisted Radical Cystectomy With Intracorporeal Urinary Diversion. Transl Androl Urol (2021) 10(5):2216–32. doi: 10.21037/tau.2019.09.45
Keywords: augmentation cystoplasty (or bladder augmentation), lower urinary tract reconstruction, robotic surgery, surgical innovation, augmentation cystoplasty, continent neobladder, Da Vinci surgical system®, robotics
Citation: Lembrikova K, Aninwene G II, Christensen KL, Tandel M, Kwan L, Gonzalez-Padilla D, Teoh J and Sturm R (2022) Approach to Lower Urinary Tract Reconstruction: A Survey of Adult and Pediatric Urologist Perspectives and Experiences. Front. Urol. 2:895102. doi: 10.3389/fruro.2022.895102
Received: 13 March 2022; Accepted: 25 April 2022;
Published: 06 June 2022.
Edited by:
Emilie K. Johnson, Ann & Robert H. Lurie Children’s Hospital of Chicago, United StatesReviewed by:
Joshua Cohn, Fox Chase Cancer Center, United StatesCopyright © 2022 Lembrikova, Aninwene, Christensen, Tandel, Kwan, Gonzalez-Padilla, Teoh and Sturm. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Renea Sturm, cnN0dXJtQG1lZG5ldC51Y2xhLmVkdQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.