- 1Department of Nephrology, Nefrocenter Medica San Carlo, Rome, Italy
- 2Department of Surgical Sciences, San Giovanni Addolorata Hospital, Rome, Italy
- 3Department of Surgeries, ARNAS Ospedale Garibadli, Catania, Italy
Orthotopic neobladder represents the best option for bladder reconstruction in terms of body image preservation and postoperative QoL for patients submitted to radical cystectomy. This technique offers also good short-term and logn-term functional outcomes. Nowadays, ileal orthotopic neobladder is the the bladder reconstruction of choice for both sexes of because there is large evidence of its superiority respect to other techniques in terms of surgical and functional results. Complications may develop during the follow-up, therefore clinical and instrumental adequate assessment is mandatory to early recognize alterations of neobladder function thus to prevent damages to the reservoir itself and to the kidney function, which can affect patients’ quality of life. Literature has shown that urodynamics and videourodynamics have significantly contributed to assess the functional aspects of ileal neobladders since the beginning of their use in patients submitted radical cystectomy, helping surgeons to improve the technical aspects of the procedure. After the preliminary results, many groups have observed that urodynamics and videourodynamics are the best tools to evaluate morphology and function of ileal neobladders. These diagnostic methods help to correctly diagnose the cause of altered neobladder function simultaneously providing anatomical informations that can be related to clinical signs and symptoms. Recent studies have confirmed the usefullness of these instruments also in patients with ileal neobladder achieved by laparoscopic and robotic approach, confirming the higher diagnostic value also respect to modern imaging techniques, as three dimensional computed tomography and magnetic resonance.
Introduction
On the basis of the EAU Oncologic Guidelines, radical cystectomy (RC) is prescribed in patients suffering from T2–T4a, N0–Nx, or M0 disease (1). However, also patients experiencing recurrent high-risk non-muscle invasive urothelial carcinoma, not responsive to immunotherapy or intravesical chemotherapy, or subjects presenting tumors that cannot be managed by endoscopic surgery, are eligible for RC (2). In the pre-operative assessment, surgeons discuss with patients which type of urinary diversion (UD) should be adopted after RC, and ileal conduit or neobladder reconstruction has to be considered (1). The most important factors that should determine the choice between the two reconstructive techniques are the patient’s age, comorbidities, cognitive status, and patient’s desire, ensuring to have provided a well-informed decision, aiming to a successful treatment and preventing the risk of postoperative regret (3). Despite that complications of RC are uniformly reported in literature, most of these depend on type of UD (4). Therefore, it is important an adequate selection of the reconstructive technique after RC to avoid severe complications and to protect patient’s quality of life (QoL). Patients suitable for orthotopic neobladder are submitted, after RC, to surgical techniques allowing to replace the native bladder by bowel reconfigured segments in the pelvis (neobladder). This reservoir maintains urinary continence due to the preservation of the external urethral sphincter. As reported by the EAU Oncologic Guidelines, orthotopic bladder techniques are now used both in men and women, and there is large evidence of their safety and reliability during the time (1). For these reasons, most patients undergoing RC receive orthotopic bladder substitution (1, 5, 6). Performing orthotopic UD pertains to expert surgical teams, generally in high-volume centers, because it requires not only the correct selection of patients but also good surgical experience and preparation to train the patient in the management of the neobladder and, above all, the ability to early recognize and manage the possible functional complications related to it. In the following paragraphs, we will describe technical principles of a neobladder reconstruction and the main functional complications that can develop. Then, the contribution of urodynamics (UDM) and video UDM (VUDM) to the development of the most modern techniques of orthotopic neobladder reconstruction and the indication to use these tools for the diagnosis and management of complications associated with UD will be discussed. A specific research strategy on PubMed has been adopted using the following keywords: urodynamic/video urodynamic/neobladder/orthotopic urinary diversion/radical cystectomy. Moreover, the following documents have been examined regarding bladder cancer management and urodynamics techniques: “European Association of Urology Guidelines” and the “Good Urodynamic Practices”.
Orthotopic neobladders: surgical technique, functional aspects, and complications
Orthotopic neobladder is the preferred procedure for bladder substitution, allowing body image preservation and good QoL after surgery (7). There is large evidence in literature that orthotopic neobladders provide good functional outcomes, especially when ileum is adopted for the reconstruction. In 1987, Hautmann was the first to report the surgical steps and clinical results of this kind of procedure (8). Since this experience, the advantages of the use of ileum for bladder reconstruction were clearly shown: good capacity, compliance, and low incidence of both ureteral reflux and urinary incontinence (UI). Different shapes of ileal neobladders have been proposed and reported in literature. However, the most important principles that make these reservoirs feasible to reproduce the anatomy and function of a native bladder are the use of a detubularized segment of ileum, the creation of a reservoir as similar as possible to the shape of the native bladder, and an uretero-neo vesical anastomosis with anti-reflux technique. The spherical shape helps to minimize the absorptive surface, whereas detubularization along the anti-mesenteric border reduces pressure peaks caused by coordinated bowel contractions (9). Indeed, a spherical shape of the reconstructed bladder achieves four times the capacity and a quarter of the pressure respect to those of a cylinder-shaped made with the same bowel extension. Even if some papers report somewhat advantages of sigmoid neobladders in terms of spontaneous voiding, large part of literature shows better functional results in patients with ileal ones in terms of bigger capacity, lower intra-neobladder pressures, daytime and nighttime UI, and risk to develop reflux (10). Following Hautmann’s normative work, many authors have proposed different surgical techniques for bladder reconstruction using the ileum. Among the most used techniques, there are the Studer neobladder (11), the Padua neobladder (12), the Camey neobladder (13), and the U-shaped neobladder (14). All these techniques have substantially overlapped results, with some differences depending on the number of cases and the follow-up period. Ileal neobladders are all characterized by postoperative short-term and long-term complications (15). Short-term complications occur within 30 days from surgery and can be sub-divided in minor (fever, wound dehiscence, pneumonia, anemia needing blood transfusion, or ileus) and major (sepsis and the need of surgical re-treatment). Long-term complications are considered those developing after 90 days from surgery, and the most reported are urinary tract infections, vesicourethral anastomosis stricture, ureterolithiasis, and neobladder stones. Functional complications of orthotopic ileal neobladders according to the Clavien Dindo classification were reported by Cicione et al. (9). In this paper, the authors describe functional complications as reported by review manuscripts. First of all, they resumed data about incidence of UI, reported as a rate varying from 15% to 50% of patients suffering from nighttime incontinence (16). The UI mechanism in orthotopic neobladder setting is multifactorial, attributable to absence of guarding reflex, persistence of bowel peristaltic activity, low compliance of the pouch, or sphincteric deficiency. The higher rate of nocturnal UI has been explained also as due to overnight greater urine output after neobladder than before RC. The nocturnal secretion of vasopressin makes hyperosmolar urine and leads intestinal neo-bladder wall to secret water to reduce urine osmolarity (17). Another functional complication reported in these case series is urinary retention. Patients submitted to orthotopic neobladder usually learn to urinate spontaneously by the relaxation of the pelvic floor using abdominal pressure. Most authors suppose that urinary retention is due to a kink in the urethral-neobladder anastomosis as the reservoir falls posteriorly during Valsalva maneuver. However, autonomic denervation of the urethra with inability to relax the sphincter has been also suggested (17). Long-term follow-up of ileal orthotopic neobladders shows the occurrence of other possible urinary functional complications: neobladder-ureteral reflux, uretero-renal hydronephrosis, and stones formation in the urinary tract. The incidence of complications is variable among the different case series. However, these complications are responsible for symptoms and clinical signs and can decrease renal function and reduce QoL. This is the main reason why the management of patients with orthotopic UD must be entrusted to expert teams and, above all, using of evaluation tools suitable for a precise morpho-functional assessment.
Urodynamic assessment of orthotopic ileal neobladders
UDM and VUDM represent the best method to assess bladder-sphincteric function and to evaluate its morpho-functional characteristics. According to the “Good Urodynamic Practice”, the aim of clinical UDM “is to reproduce symptoms while making precise measurements in order to identify the underlying causes for the symptoms and to quantify the related pathophysiological processes” (18). As above reported, orthotopic ileal neobladders may be affected by functional alterations that can determine urinary symptoms, especially in the long-term follow-up. However, independently from symptoms evidence, a proper evaluation of neobladder function should be mandatory to prevent damages to the reservoir itself and to the upper urinary tract. UDM and VUDM have been used to evaluate neobladders since many years. Preliminary studies on UD have been done on Kock ileal reservoirs since 1995 (19) and 1996 (20), showing that these techniques could achieve good results in terms of UI, voiding function, and patient’s QoL. These studies highlighted that pressure inside the reservoir was low due to detubularization, reducing the risk of UI and ureteral reflux (21). A significant report on UDM evaluation of ileal neobladder has been described by the group of Alcini in 1997 (22). These authors reported the results of a survey including 60 men submitted to ileocaeco-urethrostomy with multiple transverse taeniamyotomies. On the basis of UDM outcomes, they concluded that taeniamyotomies could provide similar outcomes than a detubularized bowel, with a low tension on the intestinal wall and consequent low internal pressure, a near-spherical shape, allowing at the same time a good basal tone thus to guarantee optimal emptying and avoiding deterioration of the reservoir. Similar experiences have been reported by numerous groups on the following, different, neobladder techniques: Studer neobladder (23), Hautmann neobladder (24, 25), ileal-W neobladder (26), vesica ileale padovana (VIP) (27), ileal S-pouch (28), Roaxel Coadou reservoir (29), U-shaped neobladder (30), Camey neobladder (31), and the Perugia neobladder (32). A very large experience on UDM performed in urinary diverted patients is reported by Muto. This Italian group collected data from 606 patients operated from 1992 to 2012, with a very long mean follow-up (81 months) (33). This paper clearly described how UDM contributes to show and support the functional results of ileal neobladders reconstructed using staplers, and the authors suggest this surgical technique also for laparoscopic and robotic approaches. In all the procedures reported by the manuscripts abovementioned, ileal reservoirs were obtained by ileal detubularization and using anti-reflux ureteral-neobladder anastomosis. Some years after these studies, a long-term analysis of functional outcomes of ileo-caeco urethrostomies was performed by Carbone et al. using VUMD and a simultaneous pelvic floor electromyography (34). This experience revealed the better contribution provided by the VUDM technique due to the following reasons Table 1:
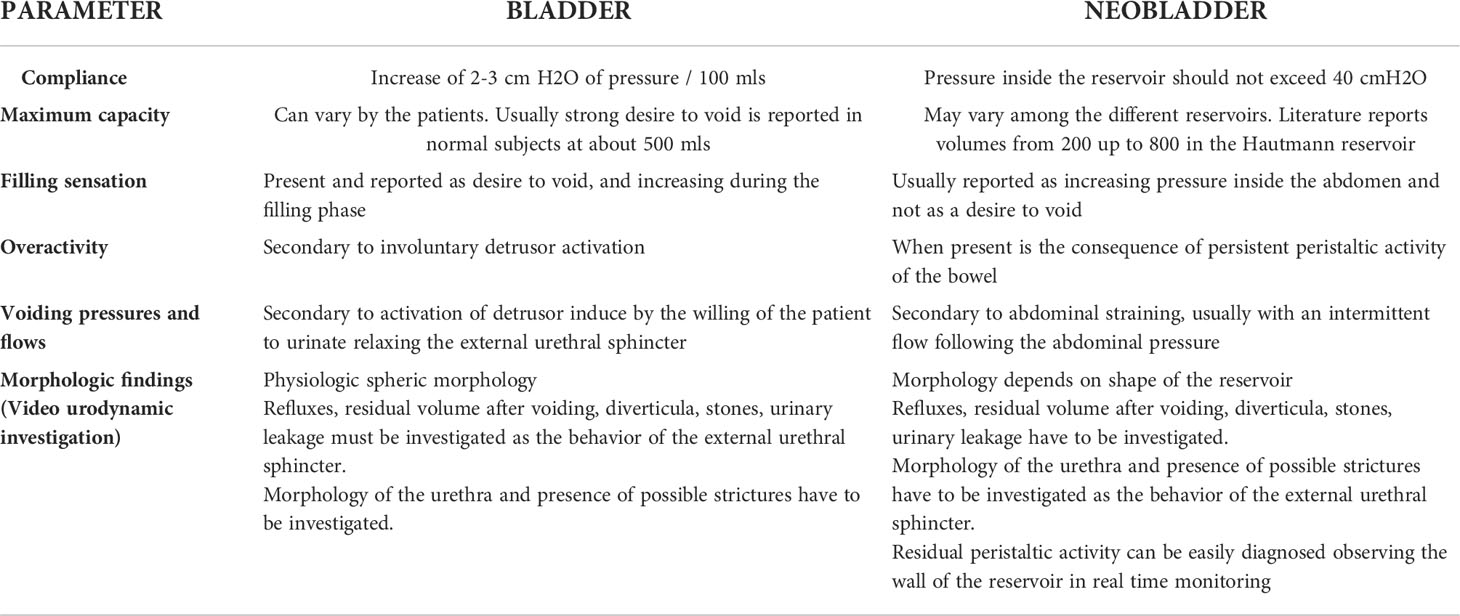
Table 1 Urodynamic and Video urodynamic outcomes: comparison between bladder and neobladder findings.
- it allows an evaluation of neobladder morphology, assessing if the anatomical result corresponds to that required by the reconstructive technique;
- it contributes to identify residual peristaltic activity;
- it allows to document ureteral refluxes;
- it contributes to diagnose type and severity of UI, allowing more precision in the definition of the leak point pressure by combining the instrumental pressure recording with the simultaneous observation of the contrast in the urethra;
- it allows to observe the morphologic characteristics of the urethra and to record pressures in the abdomen during straining, pressures inside the reservoir, and the micturition flow;
- when performed, perineal electromyography allows to verify the normal muscle reflexes during stress tests and to evaluate if patient can adequately relax or not the perineal floor during abdominal straining exerted to void the neobladder.
Even if not all the authors report the methodology, usually UDM and VUDM are performed with patients in lying or standing position, using a 6-Fr bladder catheter to fill the neobladder and a rectal balloon to register abdominal pressures. Filling is performed usually at low speed (20–30 ml/min). In the VUDM test, contrast medium instead of saline solution at room temperature is used. Only few authors add perineal superficial electromyography to record the pelvic muscle activity.
VUDM was introduced for the evaluation of ileal neobladders by Hautmann since 1987 (35) and 1988 (36). The authors designed a study properly dedicated to show functional outcomes of the ileal neobladder used for total bladder replacement. Following this experience, Aboseif and collaborators assessed ileal neobladder function and its continence mechanism in women 6 months after RC (37). The authors highlighted the contribution of the VUDM for diagnosing UI, showing intrinsic sphincteric deficiency with a low-mean abdominal leak point pressure of 48.3 cmH2O. During the following years, RC techniques have improved and mini-invasive approaches have been developed. Nowadays, high-volume centers perform RC and bladder ileal reconstruction by laparoscopic and robotic assisted procedures. Laparoscopic RC was firstly described in 1992, and after this, pioneering report described that laparoscopic and robotic RC combined with different UD techniques have been described as reproducible and characterized by low morbidity (38, 39). However, the affirmation of minimally invasive procedures for RC and intracorporeal bladder reconstruction has been supported by the observation of the favorable long-term functional results shown by UDM and VUDM. First report of VUDM combined with perineal electromyography performed on patients submitted to laparoscopic RC and totally intracorporeal ileal neobladder reconstruction dates to 2015 (40). The case series was comprehensive of 30 male patients evaluated after 6 months from surgery. Authors explored neobladder morphology, reservoir compliance, residual peristaltic activity, prevalence and type of UI, mean post-void residual volume, prevalence of ureteral reflux, and micturition pattern. On the basis of all these observations, the manuscript reported that the laparoscopic RC and intracorporeal neobladder reconstruction allowed to achieve not only good surgical outcomes but also satisfying functional results. This report defined the VUDM as the best tool to investigate neobladder function also after intracorporeal procedure because it offers an assessment of morphologic and functional details in a “real time” evaluation. In fact, VUDM overcomes the low sensitivity and inaccuracy of traditional cystography, or other imaging methods as computed tomography and magnetic resonance in the evaluation of functional complications of UD avoiding patients a second invasive diagnostic test. In this experience, the authors were capable to precisely associate clinical signs and symptoms to the VUDM findings: patients with high peristaltic activity were those suffering from neobladder-ureteral reflux; residual peristaltic activity was also associated with nocturnal urinary leakage; during VUDM, it was observed that patients with high Body Mass Index (BMI) had reduced neobladder expandability. Observations recorded during voiding phase showed that patients experiencing voiding dysfunction and higher post-void residual presented perineal-floor pseudo-dyssynergy. Stress UI was associated with high BMI and iatrogenic damage to the external sphincteric function. UDM and VUDM have been also adopted for the morpho-functional assessment of ileal neobladders achieved by totally intracorporeal robotic-assisted procedures. Minervini et al. reported their positive experience with a robotic intracorporeal neobladder configuration, showing good results by UDM findings in terms of neobladder capacity, compliance, and post-void residue (41). Satkunasivam et al. focused research on UDM outcomes and urinary function achieved in 28 men submitted to intracorporeal robotic ileal neobladder with a 9-month follow-up; the study showed very low post-void residual volume, good capacity, and compliance of the neobladder (42). UDM outcomes between robotic assisted intracorporeal versus extracorporeal neobladder have been compared in a prospective study on 40 men (43). UDM was performed 1 year after the surgical procedure. In this study, a precise report of UDM procedure is reported (7-Ch urethral catheter, 10-ml rectal balloon, filling cystometry with normal saline at room temperature, and 20–50 ml/min with maximum distension up to 700 ml). Good compliance and maximum capacity, normal pressures, and flow during micturition have been reported with no significant difference between the two techniques. These results confirmed those coming from other studies performed by Singh and Nayak (44, 45). Similar and favorable results have been described by the Italian group of Porpiglia in 45 patients submitted to Y-shaped totally intracorporeal neobladder reconstruction, followed by UDM at 12 months (46). The results of this investigation, which compared the robotic with the open approach, showed higher cystometric capacity with the open procedure, as higher maximum flow, and voiding volume during micturition, whereas continence outcomes resulted better in subjects submitted to robotic reconstruction. Favorable outcomes have been reported by UDM in patients submitted to robotic-assisted augmentation cystoplasty (47). Differently from oncologic case series above reported, these subjects suffered from neurogenic voiding dysfunction. The case series was represented by seven men and three women, and UDM results were described as excellent in terms of full continence, maximum cystometric capacity, maximum detrusor pressure, associated with no hydronephrosis, or de novo renal insufficiency. Some data are available from literature on UDM findings and urethral pressure profile results in patients with nocturnal enuresis after ileal bladder reconstruction. These studies revealed that men experiencing enuresis presented more severe residual peristaltic activity of the ileal neobladder if compared to continent individuals during filling cystometry (48). Moreover, it has been documented that patients suffering from enuresis had reduced urinary flow indexes than continent men and also a lower functional urethral length and lower values of closure urethral pressure. UDM findings were also useful to assess the favorable effects of drugs (oxybutynin, verapamil, and mebeverine) on controlling nocturnal enuresis in patients with ileal neobladders (49, 50), supporting the use of these treatments. Some authors focused their attention on voiding dysfunction in patients with ileal neobladder. Keszthely et al. designed a study to investigate etiology of UI and voiding alterations of men submitted to RC and modified ileal neobladder (Reddy) (51). Results were assessed by uroflowmetry, pressure/flow study, and urethral pressure profile. This study confirmed the voiding pattern of these subjects, who all voided the neobladder by the Valsalva maneuver; a significant maximum closure pressure of the external sphincter and maximal pressure values induce by voluntary control of the sphincter between patients partially or totally incontinent were described. The results of these investigations further support the evidence that the most important parameters of continence after RC with neobladder are represented by urethral pressures under resting conditions and during voluntary closure, a good capacity, and no significant residual bowel hyperactivity. Similar findings have been reported by Steers in a cohort of urinary diverted patients (men and women) with different surgical techniques of bladder reconstruction (52). On the basis of the outcomes of UDM, the authors underline the importance to know the pathogenetic mechanisms and risk factors of voiding dysfunction because the design of the neobladder, the operative technique, and accurate selection of patient are all crucial to achieve good outcomes. The use of neurophysiologic instruments combined to UDM and VUDM allows to better assess voiding dysfunction in patients with ileal neobladder. Perineal electromyography has been used in some studies to diagnose pseudo-dyssynergy during neobladder emptying (22, 34, 40). However, other neurophysiologic tests applied during UDM in urinary diverted patients provided interesting information about bladder neural control. As well known, bladder distension causes modification of somatic spinal motoneurons activity. Previous studies based on the soleus H reflex showed that this modulation develops at spinal level through propriospinal pathways (53). It has been observed that bladder afferent fiber activity reduces spinal motoneurons during bladder filling. This does not happen in ileal neobladders, as described in 2014 by Italian authors who reproduced this test in eight men who undergone RC with neobladder reconstruction. The results of this study, showing that neobladder distension does not inhibit the spinal motoneuron activity, induced to conclude that ileal afferent fibers do not act on modulation of spinal motoneuron’s activity as bladder afferent fibers do (54). This is one of the reasons that explain why urinary diverted patients with neobladder do not feel the same sensations during the neobladder distension as subjects with a native bladder do.
Discussion
The reported data show that both UDM and VUDM have been widely used for the assessment of orthotopic ileal neobladder surgical technique and for the evaluation of symptoms secondary to the alterations in the function of this type of UD. These diagnostic methods have shown to be feasible either to evaluate neobladder filling phase and voiding function. Almost all the studied examined support the good capacity, compliance, and anatomic results of these reservoirs also regarding the voiding function. In addition, it is largely reported their usefulness for diagnosing morphological and functional alterations that can develop during the postoperative time. Despite the large use of these diagnostic procedures, there is still no evidence about a standard UDM assessment of the intestinal neobladder. The studies presented by our report present different methods, and the case series obviously differ for type of neobladder examined, population sex, mean age, race, and for extension of follow-up. Regarding the UDM procedures, it must be considered that the same principles and parameters applied to an intact native bladder have been used for the ileum. Moreover, UDM results are conditioned by the shape and part of the bowel used. We can therefore assume this consideration as one of the limits of our report. Another limit should be considered the fact that most of studies have been performed on male population, whereas mixed cohorts and studies performed only in women are the minority. Nowadays, no prospective, randomized, multi-center clinical trials are available on this topic. However, it must be considered that the positive conclusions of all reported studies overlap, and this fact supports the use of UDM and of VUDM in the assessment of orthotopic ileal neobladders. Specifically, the simultaneous morphological and functional evaluation provided by VUDM (when necessary, also combined with neurophysiological tests such as perineal/external sphincter electromyography) cannot be reproduced by other imaging techniques, including also three-dimensional CT that has been applied only in some preliminary experiences (55). The examination of the manuscripts reviewed in this report shows that the management of patients with orthotopic ileal neobladder must be carried out by expert teams belonging to centers with high surgical volume. This allows the achievement of good surgical and oncological results by the UD and to ensure proper follow-up for diagnosing and treating possible complications. In the postoperative work-up, expertise on pathophysiology of UD permits to limit the use of invasive or expensive diagnostic methods only to selected cases. In fact, an adequate clinical and surgical preparation and a good UDM culture allow to achieve correct diagnoses even using conservative approaches. According to the principles of the so-called “non-invasive urodynamics” and the use of standardized clinical evaluation, uroflowmetry, and ultrasound, it is possible in many cases to reach a diagnostic conclusion on the dysfunction of the orthotopic ileal bladder without necessarily resorting to second level exams. This approach requires significant clinical preparation and expertise.
Conclusion
This report clearly shows the significant contribution of UDM and VUDM for the morpho-functional assessment of ileal orthotopic neobladders. Literature still lacks standardization in assessing outcomes, as well as objective outcome in urinary diverted patients’ measurements with questionnaires or standardized UDM assessments. However, considering the outcomes until now provided by UDM and VUDM performed on patients submitted to ileal orthotopic neobladder, literature clearly describes good morphologic and UDM results also after a totally intracorporeal procedure. In the next years, data on very long-term outcomes will be reported comparing different techniques, and this will allow to better standardize surgical procedures based on morpho-functional assessment (56).
Author contributions
GP: corresponding author and researcher who is expert in urodynamics. MF is expert in bladder surgery and reported data of surgical technique. AC is expert in voiding dysfunction and resumed data from Literature. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Hautmann RE, Abol-Enein H, Hafez K, Haro I, Mansson W, Mills RD, et al. Urinary diversion. Urology (2007) 69:17. doi: 10.1016/j.urology.2006.05.058
2. Babjuk M, Burger M, Compérat E, Gontero P, Liedberg F, Masson-Lecomte A, et al. Guidelines on non-muscle-invasive bladder cancer (Ta, T1 and CIS). edn. presented at the 36th EAU congress Milan. Arnhem, The Netherlands: EAU Guidelines Office (2001).
3. Check DK, Leo MC, Banegas MP, Bulkley JE, Danforth KN, Gilbert SM, et al. Decision regret related to urinary diversion choice among patients treated with cystectomy. J Urol (2020) 203:159. doi: 10.1097/JU.0000000000000512
4. Hautmann RE, de Petriconi RC, Volkmeret BJ. Lessons learned from 1,000 neobladders: the 90-day complication rate. J Urol (2010) 184:990. doi: 10.1016/j.juro.2010.05.037
5. Stein JP, Skinner DJ. Radical cystectomy for invasive bladder cancer: long-term results of a standard procedure. World J Urol (2006) 24:296. doi: 10.1007/s00345-006-0061-7
6. Hautmann RE, Volmer BJ, Schumacher MC, Gschwend JE, Studer UE. Long-term results of standard procedures in urology: The ileal neobladder. World J Urol (2006) 24:305. doi: 10.1007/s00345-006-0105-z
7. Palleschi G, Pastore A, Ripoli A, Silvestri L, Petrozza Carbone A. Videourodynamic evaluation of intracorporeally reconstructed orthotopic U- shaped ileal neobladders. Urololgy (2015) 85(4):883–9. doi: 10.1016/j.urology.2014.09.067
8. Hautmann RE, Eggart G, Frohneberg D, Miller K. The ileal neobladder. J Urol (1988) 139(1):39–42. doi: 10.1016/S0022-5347(17)42283-X
9. Cicione A, De Nunzio C, Lombardo R, Trucchi A, Manno S, Lima E, et al. Complications and quality of life of ileal conduit, orthotopic neobladder, ureterocutaneostomy: Systematic review of reports using the clavien dindo classification. Minerva Urol e Nefrol (2020) 72(4):408–19. doi: 10.23736/S0393-2249.20.03641-3
10. Schrier BP, Laguna MP, van der Pal F, Isorna S, Witjes JA. Ileal versus sigmoid neobladder as bladder substitute after radical cystectomy for bladder cancer: A meta-analysis. Eur Urol (2005) 47(5):679–85. doi: 10.1016/j.eururo.2004.10.018
11. Studer UE, Varol C, Danuser H. Orthotopic ileal neobladder. BJU Int (2004) 93(1):183–93. doi: 10.1111/j.1464-410X.2004.04641.x
12. Pagano F, Artibani W, Aragona F, Bassi P, Ruffato A, Mulonia A. Vesica ileale padovana (VIP): Surgical technique, long-term functional evaluation, complications and management. Arch Esp Urol (1997) 50(7):785–93. doi: 10.1159/000464024
13. Rauscher J, Farber RD, Parra RO. Camey procedure. a continent urinary diversione technique. AORN J (1991) 54(1):34–41, 44. doi: 10.1016/S0001-2092(07)67002-1
14. Minervini R, Morelli G, Fontana N, Minervini A, Fiorentini L. Functional evaluation of different ileal neobladders and ureteral reimplntation techniques. Eur Urol (1998) 34(3):198–202. doi: 10.1159/000019712
15. Demaegd L, Albersen M, Muilwijk T, Milenkovic U, Moris L, Everaerts W, et al. Comparison of postoperative complications of ileal conduits versus orthotopic neobladders. Transl Androl Urol (2020) 9(6):2541–54. doi: 10.21037/tau-20-713
16. Lee RK, Abol-Enein H, Artibani W, Bochner B, Dalbagni G, Daneshmand S, et al. Urinary diversion after radical cystectomy for bladder cancer: options, patient selection, and outcomes. BJU Int (2014) 113:11–23. doi: 10.1111/bju.12121
17. Hautmann RE, Hautmann SH, Hautmann O. Complications associated with urinary diversion. Nat Rev Urol (2011) 8:667–77. doi: 10.1038/nrurol.2011.147
18. SchÌfer W, Abrams P, Liao L, Mattiasson A, Pesce F, Spangberg A, et al. Good urodynamic practices: Uro£owmetry, FillingCystometry, and pressure-flow studies. Neurourol Urodynamics (2002) 21:261 274. doi: 10.1002/nau.10066
19. Kurzrock EA, Tomasic NA, Razi SS, Skinner DG, Bennett CJ. Fluorodynamic and clinical evaluation in males following construction of a Koch ileal urethral reservoir. Urol (1995) 46(6):801–3. doi: 10.1016/S0090-4295(99)80347-1
20. Grossfeld GD, Stein JP, Bennett CJ, Ginsberg DA, Boyd SD, Lieskovsky G, Skinner DG, et al. Lower urinary tract reconstruction in the female using the kock ileal reservoir with bilateral ureteroileal urethrostomy: Update of continence results and fluorourodynamic findings. Urology (1996) 48(3):383–8. doi: 10.1016/S0090-4295(96)00165-3
21. Peyret C, Géraud M, Conquy S, Martinache PR, Flam T, Zerbib M, et al. Debré BLow pressure bladder replacement after total cysto-prostatectomy. Apropos of a series of 40 patients. J Urol (Paris) (1991) 97(1):37–42.
22. Alcini E, Racioppi M, D'Addessi A, Alcini A, Menchinelli P, Grassetti F, et al. The ileocaeco-urethrostomy with multiple transverse taeniamyotomies for bladder replacement: an alternative to detubularized neobladders. morphological, functional and metabolic results after 9 years' experience. Br J Urol (1997) 79(3):333–8. doi: 10.1046/j.1464-410x.1997.03265.x
23. XD Z, Yin H, Zhang N, Zhang Y, Yang Y. The long-term outcome of studer neobladder and associated complications. Zhonghua Wai Ke Za Zhi (2008) 46(20):1535–8.
24. Soulié M, Thoulouzan M, Seguin P, Mouly P, Vazzoler N, Pontonnier F, et al. Assessment of urinary incontinence in hautmann neobladder. Prog Urol (2000) 10(4):548–52. doi: 10.1016/s0090-4295(01)01354-1
25. Iantorno R, Nicolai M, Di Federico G, Menna C, Cipollone G, Tenaglia R. Orthotopic continent urinary diversion according to hautmann: 1989-1995. physiopathologic, morphologic and urodynamic, metabolic considerations and follow-up. G Chir (1997) 18(10):569–74.
26. Abol-Enein H, Ghoneim MA. Further clinical experience with the ileal-W neobladder and a serous-lined extramural tunnel for orthotopic substitution. Br J Urol (1995) 76(5):558–64. doi: 10.1111/j.1464-410X.1995.tb07778.x
27. Ferriero MC, Simone G, Rocchegiani A, Buscarini M, Papalia R, Alcini A, et al. Early and late urodynamic assessment of padua ileal bladder. Urology (2009) 73(6):1357–62. doi: 10.1016/j.urology.2009.01.053
28. Constantinides C, Manousakas T, Chrisofos M, Giannopoulos A. Orthotopic bladder substitution after radical cystectomy: 5 years of experience with a novel personal modification of ileal-s pouch. J Urol (2001) 166(2):532–7. doi: 10.1097/00005392-200108000-00027
29. Cortellini P, Larosa M, Ferretti S, Simonazzi M, Frattini A, Choua O. Rouxel coadou method of ileal neoladder: clinico-functional considerations. Acta Urol Belg (1995) 63(3):59–63.
30. Koie T, Hatakeyama S, Yoneyama T, Hashimoto Y, Kamimura N, Ohyama C. Uterus-, fallopian tube-, ovary-, and vagina-sparing cystectomy followed by U-shaped ileal neobladder construction for female bladder cancer patients: Oncological and functional outcomes. Urology (2010) 75(6):1499–503. doi: 10.1016/j.urology.2009.08.083
31. de Zong Z, et al. Functional outcome of a U-shaped ileocystoplasty (the camey I procedure) in cancer of the bladder. Apropos of 14 cases. Ann Urol (Paris) (1991) 25(1):3–9.
32. Porena M, Mearini L, Zucchi A, Zingaro MD, Mearini E, Giannantoni A. Perugia ileal neobladder: functional results and complications. World J Urol (2012) 30(6):747–52. doi: 10.1007/s00345-012-0985-z
33. Muto G, Collura D, Simone G, Muto GL, Rosso R, Giacobbe A, et al. Stapled orthotopic ileal neobladder after radical cystectomy for bladder cancer: Functional results and complications over a 20-year period. Eur J Surg Onc (2016) 42(3):412–8. doi: 10.1016/j.ejso.2015.11.010
34. Carbone A, Racioppi M, Trucchi A, Parascani R, Gezeroglu H, Delicato G, et al. Digital fluorographic video-urodynamics in the long-term morphofunctional evaluation of alcini's ileocecourethrostomy and ileal reservoir. Urol Int (2002) 69(3):184–9. doi: 10.1159/000063946
35. Hautmann RE, Egghart G, Frohneberg D, Miller K. The ileal neobladder. Urologe A (1987) 26(2):67–73. doi: 10.1016/S0022-5347(17)75266-4
36. de Petriconi R, Hautmann R, Egghart G, Frohneberg D. Low-pressure ileal neobladder formed by antimesentery section of circular smooth muscle fibers. J Urol (Paris) (1988) 94(1):9–14.
37. Aboseif SR, Borirakchanyavat S, Lue TF, Carroll PR. Continence mechanism of the ileal neobladder in women: A urodynamics study. World J Urol (1998) 16(6):400–4. doi: 10.1007/s003450050090
38. Huang J, Linn T, Xu K, Huang H, Jiang C, Han J, et al. Laparoscopic radical cystectomy with orthotopic ileal neobladder: a report of 85 cases. J Endourol (2008) 22:939–46. doi: 10.1089/end.2007.0298
39. Parra RO, Andrus CH, Jones JP, Boullier JA. Laproscopic custectomy: initial report on a new treatment for the retained bladder. J Urol (1992) 148:1140–4. doi: 10.1016/S0022-5347(17)36843-X
40. Palleschi G, Pastore AL, Ripoli A, Silvestri L, Petrozza V, Carbone A. Videourodynamic evaluation of intracorporeally reconstructed orthotopic U-shaped ileal neobladders. Urology (2015) 85(4):883–9. doi: 10.1016/j.urology.2014.09.067
41. Minervini A, Vanacore D, Vittori G, Milanesi M, Tuccio A, Siena G, et al. Florence Robotic intracorporeal neobladder (FloRIN): A new reconfiguration strategy developed following the IDEAL guidelines. BJU Int (2018) 121(2):313–7. doi: 10.1111/bju.14077
42. Satkunasivam R, Santomauro M, Chopra S, Plotner E, Cai J, Miranda G, et al. Gill IS.Robotic intracorporeal orthotopic neobladder: Urodynamic outcomes, urinary function, and health-related quality of life. Euro Urol (2016) 69(2):247. doi: 10.1016/j.eururo.2015.06.041
43. Khan A, et al. Functional outcome of robotic-assisted intracorporeal versus extracorporeal neobladder following radical cystectomy: Initial experience. Urol Ann (2021) 13(1):9–13.
44. Singh V, Mandal S, Patil S, Sinha RJ, Gupta DK, Sankhwar SN. Urodynamic and continence assessment of orthotropic neobladder reconstruction following radical cystectomy in bladder cancer; a prospective, blinded north Indian tertiary care experience. South Asian J Cancer (2014) 3:223–6. doi: 10.4103/2278-330X.142984
45. Nayak AL, Cagiannos I, Lavallée LT, Morash C, Hickling D, Mallick R, et al. Urinary function following radical cystectomy and orthotopic neobladder urinary reconstruction. Can Urol Assoc J (2018) 12(6):181–6. doi: 10.5489/cuaj.4877
46. Checcucci E, Manfredi M, Sica M, Amparore D, De Cillis S, Volpi G, et al. Porpiglia F.Robot-assisted-radical-cystectomy with total intracorporeal y neobladder: Analysis of postoperative complications and functional outcomes with urodynamics findings. Eur Surg Onc (2021) S0748–7983(21):00980–X.
47. Grilo N, Chartier-Kastler E, Grande P, Crettenand F, Parra J, Phé V. Robot-assisted supratrigonal cystectomy and augmentation cystoplasty with totally intracorporeal reconstruction in neurourological patients: Technique description and preliminary results. Euro Urol (2021) 79(6):858–65. doi: 10.1016/j.eururo.2020.08.005
48. el-Bahnasawy MS, Osman Y, Gomha MA, Shaaban AA. Persistent and occasional nocturnal enuresis in orthotopic urinary diversion: Is there a urodynamic difference? BJU Int (2005) 96(9):1373–7. doi: 10.1111/j.1464-410X.2005.05852.x
49. El-Bahnasawy MS, Shaaban H, Gomha MA, Nabeeh A. Linical and urodynamic efficacy of oxybutynin and verapamil in the treatment of nocturnal enuresis after formation of orthotopic ileal neobladders. a prospective, randomized, crossover study. Scand J Urol Nephrol (2008) 42(4):344–51. doi: 10.1080/00365590701832726
50. Hashem A, Abdellutif MM, Laymon M, Abdullateef M, Abdelhamid A, Mosbah A, et al. Clinical efficacy of mebeverine for persistent nocturnal enuresis after orthotopic W-neobladder. BJU Int (2021). doi: 10.1111/bju.15555
51. Keszthelyi A, Majoros A, Nyirády P, Mayer P, Bach D, Romics I. Voiding symptoms and urodynamic findings in patients with modified ileal neobladder. Pathol Oncol Res (2009) 15:307–13. doi: 10.1007/s12253-008-9099-8
52. Steers WD. Voiding dysfunction in the orthotopic neobladder. World J Urol (2000) 18(5):330–7. doi: 10.1007/s003450000146
53. Carbone A, Palleschi G, Parascani R, Morello P, Conte A, Inghilleri M. Eur urol. modulation of viscero-somatic hreflex during bladder filling. A possible tool in the differential diagnosis of neurogenic voiding dysfunctions. Eur Urol (2002) 42(3):281–8.
54. Palleschi G, Conte A, Pastore AL, Salerno G, Morgia G, Giannantoni A, et al. Does the neobladder filling modulate soleus h reflex? Clin Neurphyisiol (2014) 125(2):425–7. doi: 10.1016/j.clinph.2013.06.027
55. Sassi C, Santilli L, Concetti S, Schiavina R, Amadori E, Severini E, et al. Three-dimensional coomputed tomography of the orthotopic ileal neobladder reconstruction: Normal and abnormal findings. Urol Int (2009) 82(3):301–5. doi: 10.1159/000209362
Keywords: ileal neobladder, urodynamics, videourodynamics, voiding dysfunction, radical cystectomy
Citation: Palleschi G, Cardi A and Falsaperla M (2022) Urodynamic assessment of orthotopic urinary diversions. Front. Urol. 2:885826. doi: 10.3389/fruro.2022.885826
Received: 28 February 2022; Accepted: 07 July 2022;
Published: 19 August 2022.
Edited by:
Harrina Erlianti Rahardjo, Cipto Mangunkusumo Hospital, IndonesiaReviewed by:
Prahara Yuri, Universitas Gadjah Mada, IndonesiaCopyright © 2022 Palleschi, Cardi and Falsaperla. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Giovanni Palleschi, Z2lvdmFubmkucGFsbGVzY2hpQHVuaXJvbWExLml0
 Giovanni Palleschi
Giovanni Palleschi Antonio Cardi
Antonio Cardi Mario Falsaperla3
Mario Falsaperla3