- 1University of Colorado School of Medicine, Aurora, CO, United States
- 2Department of Pediatric Urology, Children’s Hospital Colorado, Aurora, CO, United States
- 3Division of Urology, Department of Surgery, University of utah School of Medicine, Salt Lake City, UT, United States
Introduction: Telemedicine has had a slow integration into surgical subspecialties like urology. Little data exists on its effect on urologic patient-provider rapport nor long term clinical outcomes. The purpose of this study was to assess the feasibility and parent-reported experience with telemedicine visits in a tertiary pediatric urology practice during the COVID-19 pandemic.
Methods: Parents/guardians of pediatric urology patients who were seen via telemedicine between March 12th - October 30th, 2020, at Children’s Hospital Colorado main campus or a satellite campus were contacted within 1 week of their child’s visit and invited to take a telephone survey. A total of 4 yes/no questions and an open-ended question was asked to explore domains of the drawbacks and benefits to telemedicine. Categorical responses and associations between parent demographics and telehealth satisfaction were analyzed with descriptive statistics. Open-ended questions were analyzed using a team-based content analysis approach.
Results: Response rate was 76.7% (376/490). Median patient age was 4 years. 60.9% (229/376) patients were male, and 39.1% (147/376) patients female. 96.5% of parents felt that all their questions were answered by the end of their appointment. 97.8% of parents felt comfortable using telemedicine for future appointments. Patient sex, age, provider type, insurance type, clinic site, distance from clinic site, and visit diagnosis had no significant impact on survey response. Based on open-ended responses, five general themes emerged: issues with accessing technology, time saving logistics, challenging clinical interactions, a positive overall experience, and parents having about a 50/50 split in preference for telemedicine or in person visits. Multiple parents expressed discomfort with a genital exam via telemedicine.
Conclusions: Overall, parents found telemedicine to be an acceptable alternative to in-person visits and demonstrated a willingness to continue to use it in the future. Patient diagnosis and insurance type had no effect on parent response. Parents noted that pediatric urology offers unique challenges due to its personal and sensitive treatment, including the need to evaluate the genitalia. As the role of telemedicine continues to expand, consideration of these challenges is needed to ensure that pediatric urology patients and their parents are comfortable with this approach.
Introduction
Telemedicine, formally defined as the remote diagnosis and treatment of patients by means of telecommunications technology, has been practiced since the beginning of the 20th century (1). Despite its long tenure, telemedicine has had a slow integration and adaptation into modern medicine, especially into surgical subspecialties like Urology (2). Little data exist on telemedicine’s effect on urologic patient-provider rapport and long term clinical outcomes of urological telemedicine. However, prior studies suggest that telemedicine can be successfully implemented for several common urologic diagnoses (3, 4). Pediatric urology patients in particular struggle with access to care, with pediatric urologists accounting for only 8.3% of all practicing urologists in the United States (5). In an effort to increase access to urologic care, pediatric urology has taken significant strides towards the implementation of telemedicine, showing similar satisfaction to in person visits, with the additional benefits of eliminating costs associated with travel and time away from work and school (2). However, prior studies were conducted in situations where patients largely had the option to participate in either in-person or telemedicine visits.
The advent of the COVID-19 pandemic provided a unique opportunity to assess the feasibility and acceptance of Pediatric Urology telemedicine more broadly, with millions across the nation having little choice in the modality of healthcare accessible to them, regardless of location, socioeconomic status, or access to specialty care. Telemedicine was the only option for many patients in our practice due to the risk of infection that precluded in-person visits. To gauge the feasibility and parent-reported satisfaction with this change in care, we administered a telemedicine satisfaction survey to parents/guardians of pediatric urology patients during a national lockdown due to COVID-19. We hypothesized that telemedicine would be an acceptable alternative for patients compared to in-person care.
Methods
Study Location
After local IRB approval was obtained (COMIRB Protocol 20-2855), pediatric urology patients and their parent/guardian seen via telemedicine between March 12th – October 30th, 2020, at Children’s Hospital Colorado main campus (a large tertiary referral center) or at one of two satellite campus sites, Colorado Springs (COS) and South Campus, were included in this study. During this time, telemedicine was the only option for pediatric urological care available to patients through our health care system.
Survey Development
The survey was developed for quality improvement purposes, with the aim of improving technological issues and clinical interactions that may have arisen using telemedicine. Parents/Guardians were contacted within 1 week of their telemedicine visit and invited to take a brief telephone survey about their experience. The survey included 4 yes/no questions and 1 open-ended question (Table 1). Yes/No questions were developed by clinic staff in order to assess if parents/guardians felt competent in operating the online chart system and video software, as well as their experience during the virtual visit. For the purposes of this analysis, the questions were divided into the “feasibility” category if it addressed the logistics of accessing the appointment software or the “experience” category if it addressed the content of the telemedicine visit. For the “MyChart-E-Check-in”, parents were contacted by the clinic medical assistant one day prior to their scheduled appointment to aid parents in downloading the “MyChart App” and video software, signing consent forms, and verification of patient demographics (question 1). For the “Technical Call”, parents were contacted 30 minutes prior to their scheduled appointment by the clinic medical assistant to ensure that the correct software was downloaded and operational (question 2). Three clinic nurses administered the survey. The questions were read aloud to the parent/guardian over the phone and verbal responses were recorded electronically in a password-protected excel document. Parents were called once and, if not available, a voicemail was left requesting a callback if the parent/guardian wanted to participate.
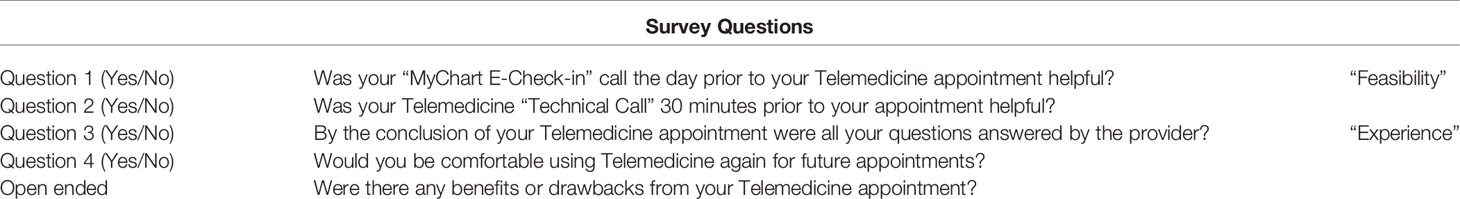
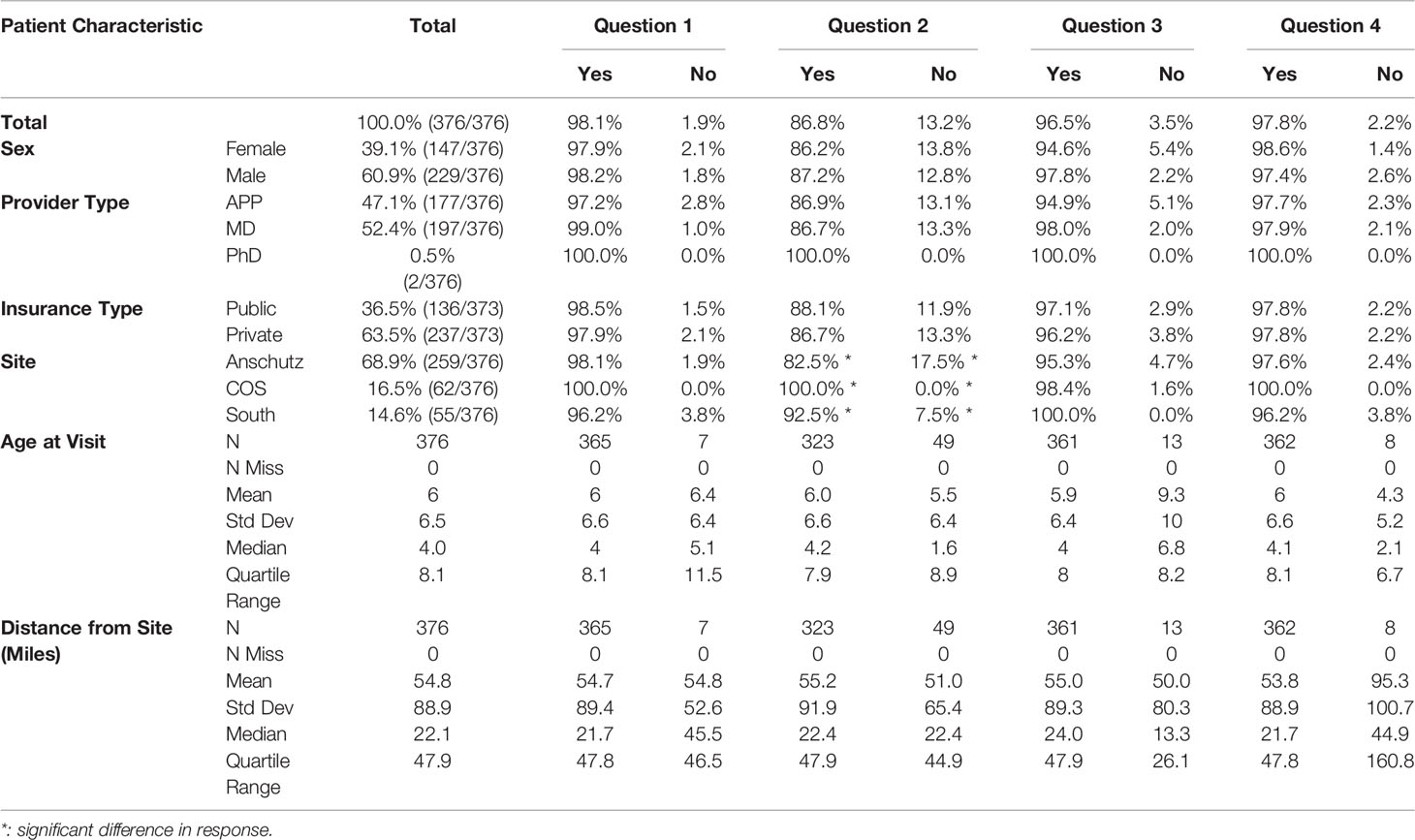
Table 1 Survey questions administered to parents/guardians whose child was seen via telemedicine for their appointment.
Statistical Analysis
Respondent/patient and visit characteristics were analyzed descriptively for differences in response to the satisfaction questions. Associations were tested using Pearson’s chi-square test for categorical characteristics (parent sex, insurance type, provider type, site). Fisher’s exact test was employed if more than 25% of cells in each contingency table contained expected counts less than 5. Continuous variables were analyzed using the non-parametric Kruskal-Wallis test (patient age at visit, distance from the residence to the site). All analyses were conducted using SAS v 9.4 (Cary, NC).
Qualitative Analysis
A content analysis was used to categorize responses to the open-ended question that concluded the brief survey. Two individuals independently reviewed each open-ended response (E.O., C.L.) and identified common themes. The reviewers independently categorized responses into the identified themes. When responses demonstrated more than one theme, such responses were broken into segments and segments were assigned to the appropriate theme. Responses and response segments were then identified as negative, positive, or neutral comment within each theme. When lack of certainty between the two reviewers arose regarding categorization, reviewers brought the response to the study team’s standing meetings and team consensus was used to categorize such response or response segments.
Results
Parent/guardians of 490 unique patients seen for a telemedicine appointment from March 12th – October 30th, 2020 were contacted to participate in the survey. 76.7% (376/490) agreed to participate. Patient demographic information was summarized to describe patients whose parent/guardian completed the survey. Demographic information was not accessible for patients whose parent/guardian did not complete the survey.
Patient Characteristics
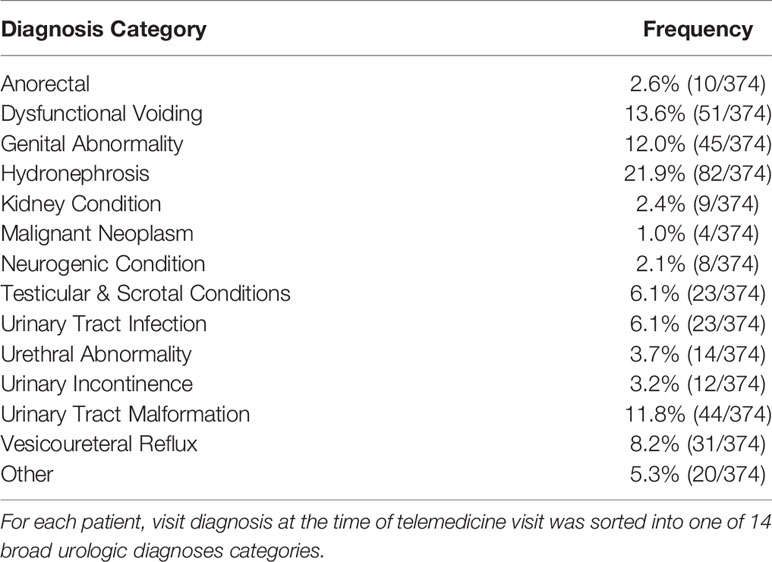
Median patient age at visit was 4.0 years. 60.9% (229/376) patients were male. 39.1% (147/376) were female. 52.4% (197/376) of patients were seen by a physician for their visit, 67.3% of patients had a visit for one of five diagnoses: dysfunctional voiding, genital abnormality, hydronephrosis, urinary tract malformation or vesicoureteral reflux (Table 3).
Survey Outcomes
98.1% of parents/guardians found the “MyChart E-Check-in” call the day prior to their telemedicine appointment helpful (question 1). 86.8% of parents/guardians found the Telemedicine “Technical Call” 30 minutes prior to their appointment helpful (question 2). 96.5% of parents/guardians had their questions answered by the provider by the conclusion of their telemedicine appointment (question 3). 97.8% of parents/guardians would be comfortable using Telemedicine again for future appointments (question 4). There was little evidence of difference in responses by co-variate values except clinic site of the telemedicine visit, where there was a significant difference in participant response to question 2 about the technical set up before the appointment by site (p < 0.001, Table 2).
Patient diagnosis at the time of visit had no significant impact on parent/guardian response to any survey question (Table 3).
Qualitative Themes
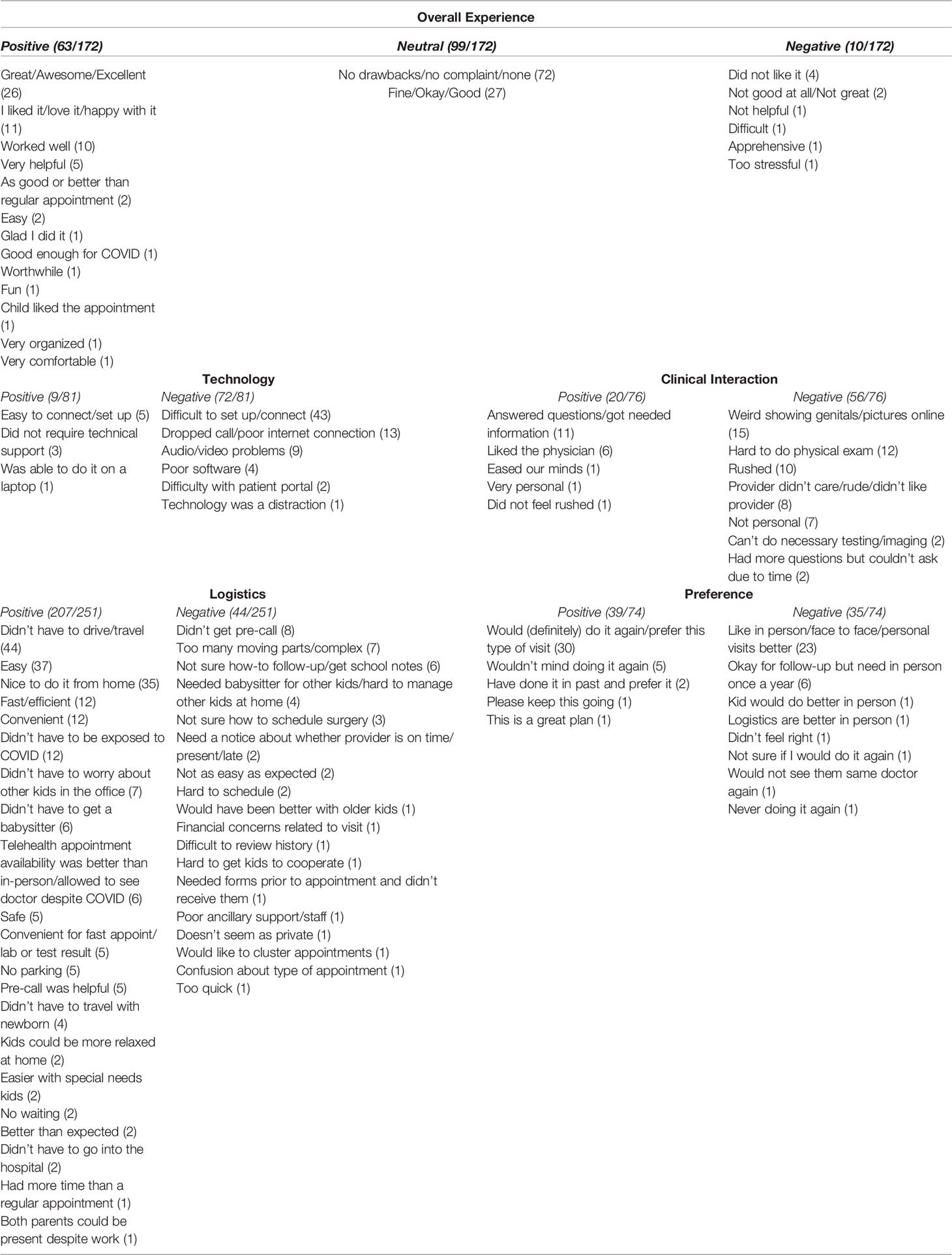
Five broad themes emerged from responses to the open-ended question: 1) Overall Experience, 2) Technology, 3) Clinical Interaction, 4) Logistics, and 5) Visit Preference (Table 4). There was a total of 380 open ended responses and 654 response segments that were categorized. No comments were excluded.
Overall Experience
There were 172 open ended responses that spoke to parents/guardian’s overall experience using telemedicine, which were largely positive or neutral responses. When commenting on their overall experience, most parents/guardians stated they had no complaints or did not experience any drawbacks to using telemedicine for their appointment, with statements such as “It was okay.” and “It doesn’t matter to us, we are at the hospital all the time, but this is fine too.” (99/172). Those parents/guardians who had positive comments reported their experience being excellent and were happy with how the visit went, for example, parents commented “Best appointment ever.” and “This was so awesome, after spending all day at the hospital yesterday it was nice to just meet online and get all our questions answered.” (63/172). Few parents/guardians reported an overall negative experience. Those that did (10/172), reported not liking telemedicine and having difficulties with this type of patient visit, with comments such as “Didn’t like it. Will not schedule again – it felt rushed.” and “Too quick, too stressful.” (Table 4).
Technology
Of the 81 comments referencing technology, most were negative, with statements such as “Awful to connect and get connected. On hold with the help desk for over 15 minutes, then still had problems with connection. Visit was ok once it all got sorted out.” and “Didn’t get connected very easily but once we did, everything was pretty easy.” (72/81). The most common negative comment regarding technology was difficulty in setting up the connection for the visit (43/81). Parents/guardians also reported issues with dropped calls, poor internet connection, and audio/video problems (Table 4).
Clinical Interaction
There were 76 responses that referenced the parent/guardian’s clinical interaction using telemedicine. The majority of comments were negative (56/76). Several parents/guardians reported that the visit was rushed and the provider they saw did not care or was rude, with parent statements such as “Felt rushed, like he had somewhere he needed to be which I don’t feel in person” and “Felt like the provider was distracted and in a hurry. Don’t know if this is because of virtual visits or just how it is.” Most notably, several parents/guardians commented on feeling uncomfortable with showing their child’s genitalia online (15/76), for example, “Thought it was a little weird showing pictures over the video – not sure if I’m ok with that” and “Awkward showing my child’s privates.”. Additionally, parents/guardians commented on the difficulty of doing physical exams via telemedicine and lack of access to do necessary imaging/testing (Table 4).
Logistics
Most of parents/guardian’s comments were about the logistics of using telemedicine. The comments regarding logistics were largely positive (207/251). Logistically, parents/guardians liked the fact that they didn’t have to leave their home for the visit, that it was easy & convenient, and noted that they were able to avoid exposure to COVID-19, with statements such as “I have to drive far every time I come for an appointment, so this was really a great way to get answers” and “I work from home, so this was great and easy – didn’t have to leave work for appointment.”. Other frequent comments touched on not having to hire a baby sitter, not worrying about parking, and their telemedicine visit being easier for children with special needs (Table 4).
Visit Preference
Responses regarding visit preference (in person vs. telemedicine) were split roughly evenly. 39/74 comments in this category preferred telemedicine visits with statements like “I actually prefer this to coming in to the hospital for a visit with my child” and “Definitely doing it again in the future. This was awesome and we got all our questions answered.”. Those who preferred in person visits (35/74) commented on preferring face to face and more personal interactions, for example, “I would rather be seen in person, this didn’t feel right.” and “I would have preferred an in-clinic visit. The connection wasn’t great.” (Table 4).
Discussion
This study conducted a descriptive analysis of parents/guardian’s experience using telemedicine in pediatric urology through a quality improvement survey during March – October 2020 of the COVID-19 pandemic. Our results confirm the data seen in the literature regarding telemedicine in pediatric urology – the vast majority of parents/guardians in this study found telemedicine in pediatric urology to be both feasible and a positive experience, with 98% of respondents indicating they would be willing to use telemedicine for future appointments. In addition, this study introduces the caregiver perspective on the benefits and drawbacks of telemedicine, specifically regarding the pediatric urology population and the nuisances that come with it.
Survey responses regarding feasibility and experience were not significantly impacted by patient sex, age, clinic site, provider type, insurance type, nor distance from clinic site, with the exception of survey question #2, where clinic site had a significant impact on survey response. Among the 3 clinic sites in this study, patients who were seen at the main campus, a large tertiary referral center, were more likely to find the “Technical Call” unhelpful. The call was intended to resolve any issues with accessing the software before the telemedicine visit. While there is no clear indication for this difference, the pediatric urology clinic at the main campus saw 70% of all patients included in this study. The volume of patients seen at the main campus may have impacted the overall quality of service provided to each individual patient, especially in the context of the massive shift from in person to telemedicine visits at the time. Our smaller clinic sites had more success in helping parents/guardians optimize the technical aspects of a telemedicine appointment.
Of note, insurance differences (private vs. public) had no bearing on respondent feasibility or satisfaction, which is important from an ethical and healthcare access standpoint, especially with the concern of the socioeconomic inequalities of urologic telemedicine (6). In contrast to our results, a recent study examining predictors of telemedicine video visit failures in pediatric urology during the COVID-19 pandemic found that public insurance (as opposed to private insurance or no insurance) was a significant predictor of video visit failure (7). Prior to the COVID-19 pandemic, coverage and reimbursement for telemedicine services were limited for those with public insurance (6). In Colorado, the state government issued a state of emergency for COVID-19, allowing telemedicine visits to qualify as billable encounters under Medicaid (8). It is unclear what degree of telemedicine coverage under public insurance will remain once public health emergency services expire. The sparse and contradictive evidence in the literature for telemedicine success using public insurance does not allow for definitive conclusion. Lack of continued coverage of publicly insured patients after the pandemic may negatively impact the socioeconomic inequalities of urologic telemedicine.
Urologic diagnosis had no significant role in parent/guardian response to feasibility and experience using telemedicine. As telemedicine finds its role in pediatric urology, it is important for providers to decipher which diagnosis can be appropriately managed through telemedicine and which should be managed in person. Several studies in the adult urologic population give strong evidence for success in treating various urologic issues using telemedicine, including prostate cancer, urinary incontinence, pelvic organ prolapse, uncomplicated urinary stones and uncomplicated urinary tract infections (UTIs) (3, 9). To our knowledge, there is no literature looking at long term outcomes with pediatric urology specific diagnoses, as pediatric urology issues differ greatly compared to issues seen in adult urology. Prior to the COVID-19 pandemic, studies did examine postoperative outcomes in pediatric urology using telemedicine, and reported no differences in postoperative surgical complications or readmissions when compared to in-person visits (10, 11). Although this survey provides information regarding a single visit, it suggests that telemedicine can be used for a wide variety of non-postoperative pediatric urologic diagnosis as well. Data on long term outcomes per diagnosis in telemedicine, especially for non-postoperative visits, is needed for providers to be able to triage the appropriate type of visit needed for their patients.
Analysis of open-ended responses to the benefits and drawbacks to telemedicine provide a more granular view of what parent/guardians navigate in order to have their child seen. Parents/guardians were overall happy with telemedicine. Most cited benefits included not having to travel and the ease of telemedicine visits – with a little over half of the comments in the visit preference category mentioning a willingness/preference to use telemedicine again. Reported drawbacks of telemedicine largely regarded technology & clinical interaction, including set up/connection challenges and telemedicine visits feeling impersonal. As telemedicine use continues to evolve, reliably establishing an internet connection for telemedicine visits is fundamental to improving the feasibility of using telemedicine for clinical visits.
Unsurprisingly, parents/guardians reported showing their child’s genitalia online as a drawback, a legitimate concern of the use of telemedicine in pediatric urology that has not been addressed in the literature. In light of healthcare suffering from the highest number of cyber-attacks and data breaches, providers should be mindful when offering telemedicine visits to their patients and counsel parents/guardians about the potential risks when examination of genitalia is needed (12). Despite its challenges, parents/guardians reported an overall positive experience using telemedicine.
There are several limitations to the interpretation of this data. The survey utilized to gauge parent/guardian feasibility and experience using telemedicine was initially created for quality improvement purposes, thereby limiting the scope of data obtained for review. Additionally, the survey given only captures a solitary clinical visit and surveys patients from a single region, thus limiting its generalizability. During this time period, parents/guardians were limited to telemedicine appointments only, which may have affected patient satisfaction as this was the only modality of clinical care available. Our institution does not have non-pandemic telemedicine satisfaction information to compare to the pandemic era. It is unclear if these results are applicable to non-pandemic times, although telemedicine in urology has a long-standing history of high patient satisfaction. Lastly, medical record numbers were only documented for a portion of the patients whose parent/guardians participated in the survey, limiting our ability to most accurately describe the characteristics of those who were seen using telemedicine during this time period.
Despite these limitations, our study contributes to the existing literature by elucidating the caregiver perspective on the benefits and drawbacks of telemedicine in pediatric urology, with responses showing an overall satisfaction with telemedicine despite technological issues, visits feeling impersonal, and discomfort with showing genitalia online. COVID-19 continues to remain highly infectious and is a large burden to our healthcare system. Our survey results indicate that parent/guardians of pediatric urology patients had an overall positive experience using telemedicine and are overwhelmingly willing to utilize telemedicine in the future, regardless of patient diagnosis, patient age, provider type seen, insurance type, or distance from clinic. Understanding the impact and nuisances of telemedicine in pediatric urology will allow the best care for urology patients as it continues to expand its role in modern healthcare.
Conclusion
Based on survey response to questions regarding experience, feasibility, benefits, and drawbacks using telemedicine, telemedicine seems to be an adequate alternative to in person visits in pediatric urology, specifically in the context of the COVID-19 pandemic. Nearly all parents/guardians felt as though their questions and concerns were properly addressed by their provider and indicated a willingness to use telemedicine in the future. However, parents/guardians noted that pediatric urology offers unique challenges due to its personal and sensitive treatment, including the need to evaluate the genitalia. As the role of telemedicine continues to expand, consideration of these challenges is needed to ensure that pediatric urology patients and their parents are comfortable with this approach.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by Colorado Multiple Institutional Review Board (COMIB) Protocol # 20-2855. Written informed consent from the participants’ legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author Contributions
EO, BC, CL, JC, and VV contributed to the conception and design of the study. KM, MH, and AA administered the survey analyzed in this study. CS performed the statistical analysis. EO wrote the first draft of the manuscript. CL, CS, and VV wrote sections of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Nesbitt TS. The Evolution of Telehealth: Where Have We Been and Where are We Going? Inst Med Natl Acad (2012). The Role of Telehealth in an Evolving Health Care Environment: Workshop Summary. (Washington, DC: The National Academies Press). doi: 10.17226/13466
2. Ellimoottil C, Skolarus T, Gettman M, Boxer R, Kutikov A, Kee BR, et al. Telemedicine in Urology: State of the Art. Urology (2016) 94:10–6. doi: 10.1016/j.urology.2016.02.061
3. Novara G, Checcucci E, Crestani A, Abrate A, Esperto F, Pavan N, et al. Telehealth in Urology: A Systematic Review of the Literature. How Much Can Telemedicine Be Useful During and After the COVID-19 Pandemic? Eur Urol (2020) 78:786–811. doi: 10.1016/j.eururo.2020.06.025
4. Gadzinski AJ, Ellimoottil C. Telehealth in Urology After the COVID-19 Pandemic. Nat Rev: Urol (2020) 17:3637–364. doi: 10.1038/s41585-020-0336-6
5. Association, A.U. American Urological Association, The State of the Urology Workforce and Practice in the United States 2018. (2020) Maryland, U.S.A.
6. Kirshenbaum E, Rhee EY, Gettman M, Spitz A. Telemedicine in Urology: The Socioeconomic Impact. Urol Clinics North America (2021) 48:215–22. doi: 10.1016/j.ucl.2021.01.006
7. Winkelman AJ, Beller HL, Morgan KE, Corbett ST, Leroy SV, Noona SW, et al. Benefits and Barriers to Pediatric Tele-Urology During the COVID-19 Pandemic. J Pediatr Urol (2020) 6:840.e1–6. doi: 10.1016/j.jpurol.2020.09.028
8. COVID-19 State of Emergency Changes to Telemedicine Services. (2021). (Colorado :Department of Health Care Policy and Financing, State of Colorado), https://hcpf.colorado.gov/provider-telemedicine.
9. Turcotte B, Paquet S, Blais A-S, Blouin A-C, Buldoc S, Bureau M, et al. A Prospective, Multisite Study Analyzing the Percentage of Urological Cases That Can Be Completely Managed by Telemedicine. Can Urol Assoc J (2020) 10(14):319–21. doi: 10.5489/cuaj.6862
10. Finkelstein JB, Cahill D, Young K, Humphrey K, Campbell J, Schumann C, et al. Telemedicine for Pediatric Urological Postoperative Care Is Safe, Convenient and Economical. J Urol (2020) 204:144–8. doi: 10.1097/JU.0000000000000750
11. Canon S, Shera A, Patel A, Zamilpa I, Paddack J, Fisher PL, et al. A Pilot Study of Telemedicine for Post-Operative Urological Care in Children. J Telemed Telecare (2014) 8(20)427–430. doi: 10.1177/1357633X14555610
Keywords: telemedicine, telehealth, pediatric urology, COVID-19, experience, urology
Citation: Ogundipe EA, Caldwell B, Leavitt C, Monnet K, Hedlind M, Anderson A, Colby J, Sevick CJ and Vemulakonda VM (2022) Parent-Reported Experience With Pediatric Urology Telemedicine Visits During the COVID-19 Pandemic. Front. Urol. 2:877521. doi: 10.3389/fruro.2022.877521
Received: 16 February 2022; Accepted: 23 May 2022;
Published: 27 June 2022.
Edited by:
Stephen Canon, Arkansas Children’s Hospital, United StatesReviewed by:
Christopher Roth, Louisiana State University, United StatesKolsoum Deldar, Shahroud University of Medical Sciences, Iran
Copyright © 2022 Ogundipe, Caldwell, Leavitt, Monnet, Hedlind, Anderson, Colby, Sevick and Vemulakonda. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Eniola A. Ogundipe, RW5pb2xhLm9ndW5kaXBlQGN1YW5zY2h1dHouZWR1
 Eniola A. Ogundipe
Eniola A. Ogundipe Brian Caldwell2
Brian Caldwell2