- 1The Johns Hopkins Hospital, Johns Hopkins Medicine, Baltimore, MD, United States
- 2West Virginia University Hospitals, Morgantown, WV, United States
Background: Telemedicine is now commonplace and an accepted modality for delivering health care due to the coronavirus pandemic. It has proven useful in increasing access to traditionally limited subspecialties and bridged the gap of local regional geographic restraints. We report a follow up of our experience building tele-consultation capacity for pediatric urology in a resource constrained area. Specifically, we hypothesize that hybrid tele-consultation is a safe modality for postoperative evaluation. A secondary goal of this study is to evaluate perceived barriers to implementing this practice from the perspective of advanced practice providers (APPs).
Methods: After obtaining IRB approval (IRB# 1910741113), patients were prospectively recruited for tele-consultation encounters with a tertiary academic center between August 2018 and March 2020 (pre-dating the coronavirus pandemic). Advanced practice providers received additional training in physical diagnosis and examination prior to returning to satellite clinics in their local communities and facilitating tele-consultation with an academic pediatric urologist. Postoperative outcomes were analyzed out to eight weeks and any peri- and postoperative complications were assessed using the Clavien-Dindo classification system. Finally, anonymous surveys were administered to the APPs at the conclusion of the recruitment period to assess their satisfaction with telemedicine clinics and perceived barriers to implementation.
Results: 92 telemedicine encounters took place between August 2018 and March 2020. The most common reasons for presentation were undescended testis (UDT) (n=15), urinary tract infection (n=13) and enuresis (n=13). The most common surgical case booked by the APPs in the satellite clinic was orchiopexy (n=10). Mean distance travel saved was 299.8 miles. In 23 patients who were schedule surgery, only two patients (8.7%) had an initial diagnosis that differed with their APP pre-operative diagnosis. Of the 22 patients who underwent surgery, all elected telemedicine visits for postoperative evaluation. No patient experienced complications. Initial consultations averaged 14 minutes (range 9 to 20 minutes), while mean duration of postoperative evaluations was 9 minutes (range 6 to 13 minutes). With regards to surveys, APPs reported an overall positive experience with tele-consultation (4.5/5, n=7) and all planned on incorporating it into their future practice (4.9/5, n =7).
Conclusion: A hybrid tele-consultation video conferencing clinic with heavy reliance on APPs is a safe, reliable and economical way to address pediatric subspecialty surgical needs in the rural setting. With proper training and exposure, APPs can safely perform preoperative assessments and correctly refer patients for surgical intervention, adding efficiency to the surgical subspecialty workflow.
Introduction/Background
Technology enabling telemedicine capabilities has existed in some form for nearly 50 years, however, it has only been utilized as a tool in pediatric surgical care for just over a decade (1, 2). Despite the early piloting of tele-urologic video-consultation for patient visits in the mid-1990s at a center in West Virginia (WV), urology remained one of the specialties with the lowest rates of telemedicine (3). The SARS-CoV-2 novel coronavirus, which lead to the coronavirus pandemic (COVID-19) beginning early 2020, forced widespread adoption out of necessity to ensure patient care (4). Much has been added to the collective telemedicine experience since then with nearly 7,371 PubMed mentions of “telemedicine” and “COVID-19 experience” as of January 2022.
We previously reported on our experience in building a teleconsultation practice within the space of telemedicine prior to the coronavirus pandemic in West Virginia (WV), a state with a limited pediatric urology presence historically. To fill the gap in care, we employed the help of advanced practice providers (APPs) who received additional clinical experience in pediatric urology with particular attention to physical examination and diagnosis who then returned locally to referring satellite clinics within the health system. Teleconsultation was then utilized at these satellites between the consulting APP and pediatric urologist at the academic medical center. Important findings included a mean roundtrip driving time of 4 hours 46 minutes saved, or 299.8 miles saved per patient. Most importantly, in our preliminary experience with 92 teleconsultation visits we found an overall concordance rate in diagnoses (teleconsultation vs in-person) of 91.3%. Additionally, our results were reproducible at two other sites, increasing the capacity within a rural state to 4 total sites (5).
In what follows, we provide a follow up to our experience with respect to postoperative care, complications, and barriers to building a tele-urology practice, all of which relied heavily on our APPs. Their partnership with the pediatric urologists ensured safety through the entire process, from preoperative diagnosis through (virtual) postoperative follow up.
Materials and Methods
Overview
Initial data collection was performed after receiving IRB approval (IRB# 1910741113). Pediatric urology patients were prospectively recruited for telemedicine encounters at a tertiary academic center between August 2018 and March 2020. Recruitment was based on family preference, with telemedicine visits offered to all eligible patients. The accrual period ended immediately prior to pandemic-induced changes. Variables captured included reason for consult, total mileage, driving time, home zip code and operative intervention, if any, based on diagnosis and was previously reported.
Training and Workflow
APPs received dedicated didactic and clinical pediatric urology training alongside a fellowship-trained pediatric urologist for a period of two weeks at our academic center before returning to the satellite sites (Figure 1). Patient visits were conducted in-person at one of our rural, satellite facilities. The APP at each satellite facility was responsible for performing an initial intake, assessment, and physical examination for each patient. The final part of each patient visit included an APP-initiated video conference with a fellowship-trained urologist/APP to discuss the findings and appropriate next steps with the patient and their family. If appropriate, patients were consented and offered the opportunity to schedule a surgical visit at the primary academic center. The primary urologist met in-person with each patient in the preoperative holding area on the day of surgery to perform their own physical exam and confirm the diagnosis prior to proceeding with surgery. In the absence of signs or symptoms of concern, patients and their families were given the option of either a video or in-person visit with the primary surgeon or an APP for post-operative follow up visits.
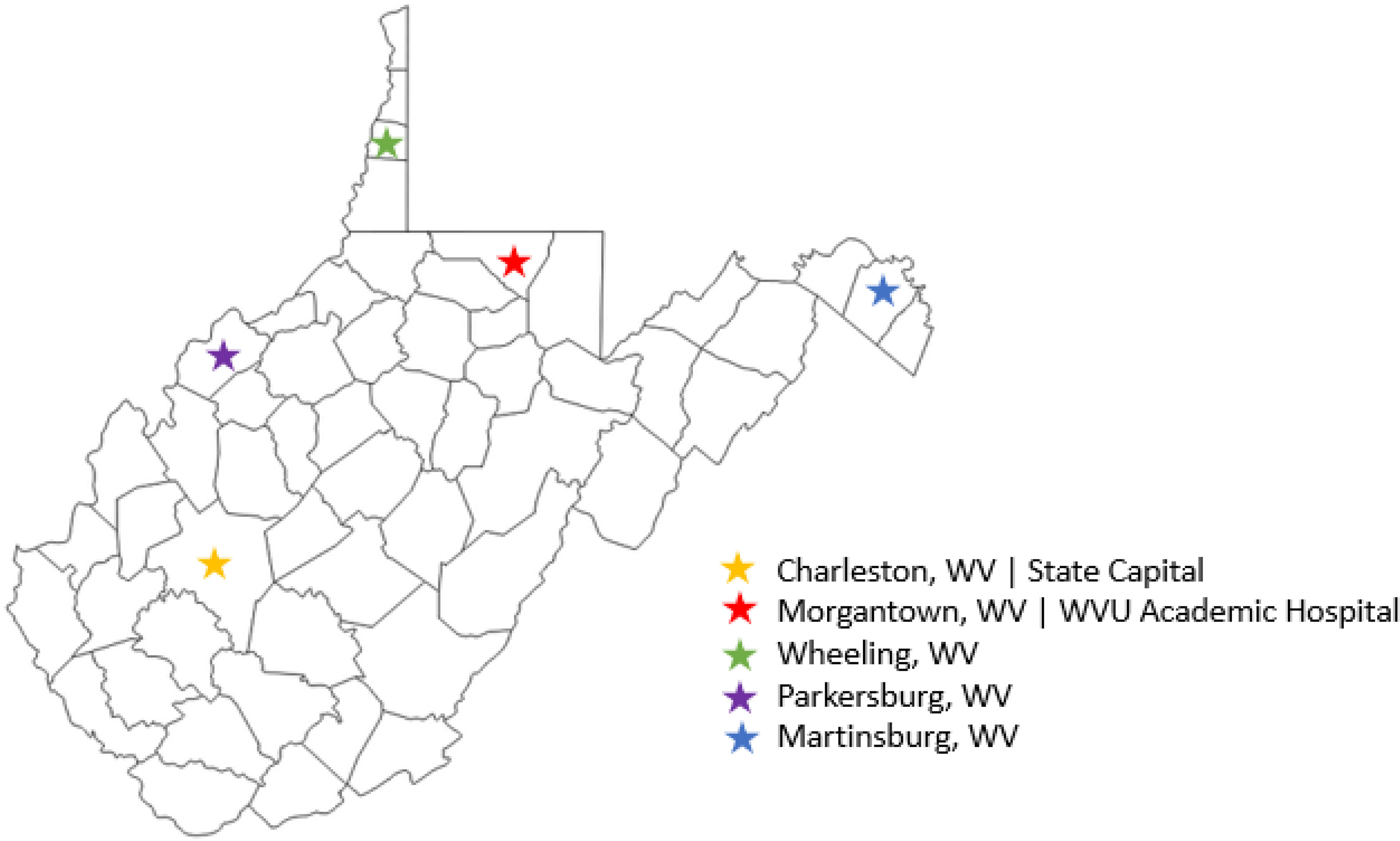
Figure 1 West Virginia state map depicting location of satellite sites (purple, blue and green stars) in relation to academic teaching hospital (red star).
Data Analysis
Postoperative outcomes were analyzed out to eight weeks and any peri- and postoperative complications were assessed using the Clavien-Dindo classification system. Financial analysis was performed using data on duration of telemedicine visits and calculating cost per minute based on established billing procedures at our institution. Finally, anonymous surveys were administered to the APPs at the conclusion of the recruitment period to assess their satisfaction with telemedicine clinics and perceived barriers to implementation. In our model we had three APPs at the main academic center (Morgantown, WV) and one at each satellite campus (Wheeling, Parkersburg, and Martinsburg, WV) as seen in Figure 1. Descriptive statistical analysis was performed using the Analysis ToolPak within Microsoft Excel. Five-point Likert scales for eight items were averaged with outcomes plotted using Tableau Software (Seattle, WA) (Figure 2). Per question percent agreement was calculated based on the proportion of responders responding with “Strongly agree” and “Agree”.

Figure 2 Opinions with telemedicine amongst Advance Practice Providers within Pediatric Urology. Percent agreement follows each item. Bar graph indicates breakdown of provider agreement level as a percent of overall respondents with average response within circle.
Results
92 telemedicine encounters took place between August 2018 and March 2020. The most common reason for presentation was undescended testis (UDT) (n=15), followed by recurrent UTI (n=13) and enuresis (n=13). The most common surgical case booked by the APP in the satellite clinic was orchiopexy (n=10). In 23 patients who were schedule surgery, only two patients (8.7%) had an initial diagnosis that differed with their APP pre-operative diagnosis. The two cases were noted when the patient presented for surgery. One case was cancelled after bilateral descended testes were noted on physical exam, although the original diagnosis was unilateral undescended testis. The other patient was pre-operatively diagnosed with hypospadias but found to have an orthotopic meatus, however, he did have ventral chordee and underwent correction with circumcision at the parents’ request. Pre-operative examination is the standard in our practice, so no patients received general anesthesia unnecessarily.
Of the 22 patients who underwent surgery, all elected telemedicine visits for postoperative evaluation. The mean time to follow up was 8 weeks (range 6-9), which is the preferred length of follow up for our institution. No postoperative complications were encountered in this group. Finally, durations of videoconference visits were tabulated. Initial consultations averaged 14 minutes (range 9 to 20 minutes), while mean duration of postoperative evaluations was 9 minutes (range 6 to 13 minutes).
Anonymous surveys were reviewed to assess APP attitudes toward telemedicine and perceived barriers to implementation. The distribution of the five-point Likert scales responses from 7 responders are included in Figure 2. Subjective additional commentary was also consolidated for review (Figure 3). Overall, APPs reported a positive experience with telemedicine (4.4/5), with all planning on continued use of telemedicine in the future (4.9/5). Generally, APPs felt they were able to provide a comparable level care in IPVs and VVs (3.9/5).
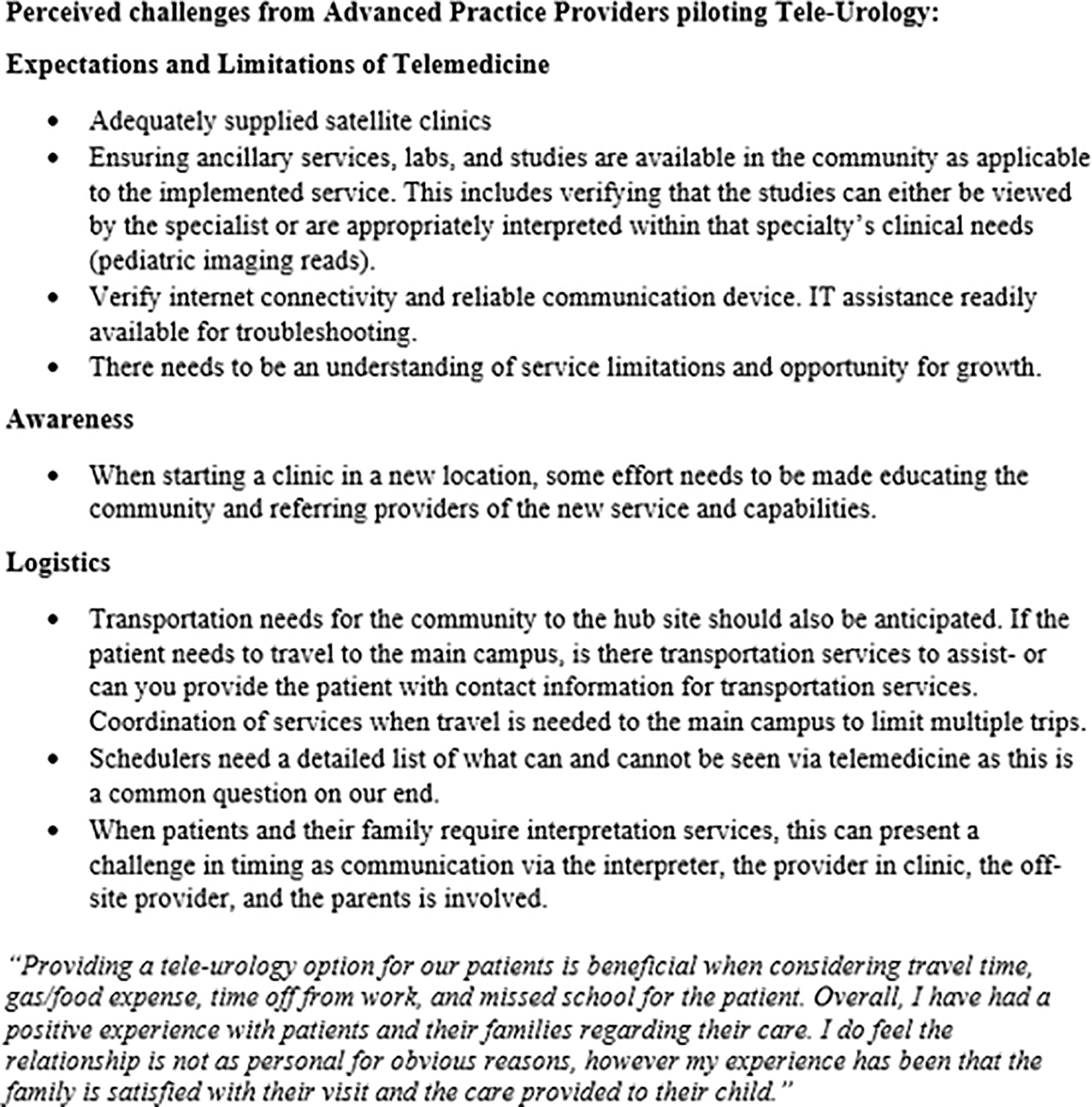
Figure 3 Perceived barriers to implementing a Pediatric Urology telemedicine clinic amongst Advanced Practice Providers.
Discussion
Telemedicine technology has existed within pediatric surgical subspecialty care for just over a decade, however, its implementation was only rapidly accelerated as a result of the COVID-19 pandemic, with a six-fold increase in the percentage of urologists using telemedicine programs in 2020 alone compared to 2019 (6). It has proven a useful tool in increasing access of surgical subspecialty care and a particular benefit in rural settings (5, 7).
Finkelstein et al. demonstrated the numerous benefits in implementing telemedicine in pediatric urology. In their cohort, travel and waiting for care accounted for 98.4% of the total time for an in-person visit, which carries implications with respect to time missed from work and school. Additionally, associated costs varied significantly, with VVs proving much cheaper compared to IPVs. In addition to being efficient and economical, most importantly, telemedicine was safe for postoperative evaluation with high levels of satisfaction. Interestingly, median recorded face time spent with the physician was greater in the VV experience compared to IPV, 33.3% vs 1.6%, respectively (8).
Telemedicine providers also report favorable experiences with telemedicine. Although, not always optimal, providers believe that telemedicine enables adequate management of 96.5% of their pediatric urology cases (9). Combine this with the time, and expense, saved with VVs and favorable family experiences, and telemedicine provides a method to increase system efficiency in providing a limited resource more broadly.
We provide our experience and utilization of telemedicine in pediatric urology within a rural setting with severely limited access to the specialty. To illustrate, our mean mileage saved was 299.8 miles compared to 54 miles in other reported studies (8). In terms of time saved, the cost associated with the difference in mileage saved with respect to gas would be equally expected. Postoperatively, none of our 22 patients experienced a complication and mean virtual postoperative visit was just 9 minutes. While our providers overall reported favorable experiences with telemedicine (4.4/5), our focus was specifically on the APP experience given their significant role within our telemedicine framework. APPs believed they were able to provide a comparable level of care with VVs (3.9/5), that telemedicine was feasible in a surgical subspecialty (4.4/5) and planned to continue to increase integration of telemedicine in their future practice (4.1/5) (Figure 2).
Specific barriers APPs cited centered on reasonable expectations of what can, and cannot, be accomplished with a telemedicine visit with emphasis on preclinical screening of chief complaints. Other barriers included inconsistent availability of equipment, such as bladder scanners, necessary for point-of-care clinical information and counseling. APPs in our experience also noted the importance of community involvement and educating the community and local providers of new services and capabilities. Also, while this may be a byproduct of the rural setting, transportation needs to the community site still require anticipation as public transportation is nonexistent in much of the state, let alone at satellite clinics (Figure 4).
We did not find any difference in billing practices, as differential billing practices were not instituted at the host institution. However, differential billing for IPVs compared to VVs accounted for significant cost discrepancies in other series (8, 10). Our telemedicine framework is novel in that APPs were crucial early and often. Our telemedicine approach allowed APPs to schedule surgeries without direct physician oversight, a practice that has not been previously described in the literature. While this may cause debate, we found that dedicated APPs had a high diagnostic concordance (91.3%), this practice was safe (with no complications noted) and was necessary to address the overwhelming need for pediatric urologic care within WV. We found that a deliberately designed telemedicine team, with additional dedicated pediatric urology training was efficacious, and has emerged as the preferred method by the pediatric urology team – with over two years of experience now, 30% of outpatient surgeries are scheduled by APPs with involvement of the pediatric urologist only at the time of pre-operative evaluation with satisfactory results.
Our study does have its limitations. Notably, a small cohort at a single institution. While our initial recruitment was for feasibility purposes only, it was a long enrollment duration and still yielded a small cohort. Additionally, reasons for why patient families still chose IPV over VV requires further evaluation. However, our recruitment period concluded prior to COVID-19, which caused a subsequent acceleration in telemedicine. This allowed us to schedule patients for telemedicine visits based on preference, rather than out of necessity. Also, as our study was intended as a feasibility study, certain patient factors were not captured prospectively (as confined by the IRB approval), so additional information gleaned from this study in the future will rely on retrospective review.
Another limitation is that we typically only offer a single postoperative visit at 8 weeks. For conditions such as ureteropelvic junction obstruction status-post pyeloplasty, visits are scheduled after interim imaging. However, for conditions such as orchiopexy, a single 8-week postoperative visit may be insufficient to ensure testicular atrophy or loss does not occur. Typically, if the patient is an infant, we will instruct the parents or guardians to periodically assess the testicles and communicate the need for yearly assessment with child’s primary care provider. If any concerns over discordant growth are noted, we then schedule an IPV.
COVID-19 forced the widespread adoption of telemedicine in all aspects of medicine, including pediatric urology. With any rapidly integrated service, special care must be taken to ensure practitioners utilizing telemedicine deliver high-quality care. This includes the use of end-to-end encrypted teleconferencing technology and not more ubiquitous applications such as Zoom, Skype or Facetime. In addition to ensuring proper information technology resources, remote clinics must also be adequately supplied with specialty-specific necessities. Finally, ‘webside’ manner requires deliberate and intentional focus to ensure patients and families feel heard and benefit from the technology. This includes ensuring a private, quiet space with adequate lighting in addition to self-awareness by practitioners regarding body position, eye contact and purposeful listening (10). By carefully implementing these nuanced pearls, telemedicine can continue to bridge the gap of surgical subspecialty care and access in an efficient, cost-effective, and pleasant manner.
Conclusion
Telemedicine has not only proven a crucial tool in providing care to patients throughout the recent pandemic, but also in extending care to patients in resource constrained areas. The authors report their experience with a hybrid model, tele-consultation, which relies heavily on the APP-pediatric urologist partnership to deliver high-quality care. Our model is unique in that APPs schedule surgery with high diagnostic accuracy and provide a viable option in postoperative care through the use of tele-consultation.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by West Virginia University Hospital Institutional Review Board. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author Contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work, and approved it for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Pettit S, Young E, Jung I. Systematic Review of Telemedicine in Pediatric Urology. J Pediatr Urol (2021) 1:1–6.
2. Shivji S, Metcalfe P, Khan A, Bratu I. Pediatric Surgery Tele-Health: Patient and Clinician Satisfaction. Pediatr Surg Int (2011) 27:523–6. doi: 10.1007/s00383-010-2823-y
3. Hayes WS, Tohme W, Komo D, Dai H, Persad SG, Benavides A, et al. A Telemedicine Consultative Service for the Evaluation of Patients With Urolithiasis. J Urol (1998) 51(1):39–43. doi: 10.1016/S0090-4295(97)00486-X
4. Dubin JM, Wyant WA, Balaji NC, Ong WL, Kettache RH, Haffaf M, et al. Telemedicine Usage Among Urologists During the COVID-19 Pandemic: Cross-Sectional Study. J Med Internet Res (2020) 22:e21875. doi: 10.2196/21875
5. Ferari C, Mitchell K, Crigger C, Zupper S, Wildasin A, Ost M, et al. Bridging the Gap – Building Surgical Subspecialty Telemedicine Clinics in the Rural Setting. Urol Pract (2021). doi: 10.1097/UPJ.0000000000000284
6. Makarov D, Penson D2020 The State of the Urology Workforce and Practice in the United States. American Urological Association (2021).
7. Canon S, Zamilpa I, Patel A, Marquette M, Makarov D, Penson M. MP32-02 Telemedicine Utilization in Pediatric Urology and Beyond. J Urol (2017) 197:e408–9. doi: 10.1016/j.juro.2017.02.977
8. Finkelstein JB, Cahill D, Young K, Humphrey K, Campbell J, Schumann C, et al. Telemedicine for Pediatric Urological Postoperative Care Is Safe, Convenient and Economical. J Urol (2020) 204(1):144–8. doi: 10.1097/JU.0000000000000750
9. Turcotte B, Paquet S, Blais AS, Blouin AC, Bolduc S, Mureua M, et al. A Prospective, Multisite Study Analyzing the Percentage of Urological Cases That Can Be Completely Managed by Telemedicine. Can Urol Assoc J (2020) 14:319–21. doi: 10.5489/cuaj.6862
Keywords: telemedicine, pediatric urology, tele-urology, teleconsultation system, advanced practice clinicians
Citation: Crigger C, Sholklapper T, Mitchell K, Eckert K, Zupper S, Bartlett M, Ost MC and Al-Omar O (2022) From Start-to-Finish: A Partnership With Advanced Practice Providers in Tele-Consultation Within Pediatric Urology. Front. Urol. 2:876560. doi: 10.3389/fruro.2022.876560
Received: 15 February 2022; Accepted: 24 March 2022;
Published: 11 April 2022.
Edited by:
Christopher Long, Children’s Hospital of Philadelphia, United StatesReviewed by:
Julia Beth Finkelstein, Boston Children’s Hospital, United StatesEnrico Checcucci, IRCCS Candiolo Cancer Institute, Italy
Copyright © 2022 Crigger, Sholklapper, Mitchell, Eckert, Zupper, Bartlett, Ost and Al-Omar. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chad Crigger, Y2hhZC5iLmNyaWdnZXJAZ21haWwuY29t
 Chad Crigger
Chad Crigger Tamir Sholklapper
Tamir Sholklapper Katharina Mitchell2
Katharina Mitchell2 Osama Al-Omar
Osama Al-Omar