- 1Department of Pediatric Urology, Nicklaus Children’s Hospital, Miami, FL, United States
- 2College of Medicine, University of Central Florida, Orlando, FL, United States
- 3College of Medicine, University of Florida, Jacksonville, FL, United States
Introduction: Open surgery is considered the standard of care for pediatric urological procedures. Nonetheless, Robotic Assisted Laparoscopic Surgeries (RALS) have become increasingly popular in pediatrics as they allow for quicker recovery times, lower narcotic use, better cosmesis, and better intraoperative visibility. However, there are concerns regarding the usefulness of RALS in the infant population, as operating on smaller patients limits mobility of the robotic arms and can result in arm collisions.
Objective: The aim of this study was to compare the clinical and postoperative outcomes of infants undergoing robotic vs open pyeloplasty or ureteroureterostomy.
Materials and Methods: Retrospective study conducted between 2012 to 2022, 114 infants who underwent pyeloplasty (81 open pyeloplasty and 33 robotic pyeloplasty) and 21 who underwent ureteroureterostomy (9 open ureteroureterostomy and 12 robotic ureteroureterostomy) were included.
Results: Mean age at surgery in the pyeloplasty cohort was 4.81 ± 3.1 months in the open group, and 6.24 ± 2.6 months in the robotic group (p=0.13), and in the ureteroureterostomy cohort was 7.67 ± 3.16 months in the open group and 7.58 ± 2.75 months in the robotic group (p=0.95). Operative time was found to be shorter in robotic pyeloplasty and robotic ureteroureterostomy, when compared to the open approaches. Postoperative complications, its severity, and the surgical success were comparable among the pyeloplasty and ureteroureterostomy groups. Only 1(3%) complication related to the robotic technique was reported in the pyeloplasty cohort. The length of hospital stay was found to be similar between the ureteroureterostomy groups, while in the pyeloplasty cohort the robotic group showed a significant shorter hospital stay than the open group. Overall, the mean follow-up was greater than 12 months.
Conclusion: Our results demonstrated that robotic pyeloplasty and ureteroureterostomy performed in infants are feasible, safe, and durable procedures, with an additional benefit of reducing duration of operative time and hospital stay.
1. Introduction
Open surgery is considered the standard of care for pediatric urological procedures due to its consistent, well-documented and durable success rates, affordable costs, and its lack of restriction on patient’s age or need for special equipment (1–3). Nonetheless, in the last two decades, Robotic Assisted Laparoscopic Surgeries (RALS) have become increasingly popular in pediatrics as they allow for quicker recovery times, lower narcotic use, better cosmesis, and better intraoperative visibility (4, 5). For instance, the use of RALS in pediatric urology has increased 8.1% per year with renal pelvis/ureter surgery being the most commonly performed (6).
However, the use of robotic surgery in infants is still controversial due to the potential technical difficulties inherent in the anatomy and physiology of small children (7). Furthermore, multiple reports have suggested RALS can increase overall surgical time (8–11). In infants this would not only lead to longer general anesthetic use, but a longer exposure to abdominal insufflation volumes and pressures, which can increase the risk of cardiovascular collapse (12). Moreover, longer operative times have been associated with an increased risk of surgical site infections (13).
In light of these concerns, there is a lack of consensus on whether RALS would be beneficial in the infant population since open techniques are known to provide excellent long-lasting results with low morbidity (1, 14). At our institution, RALS has recently been performed in select cases for children ≤12 months, most commonly for pyeloplasty or ureteroureterostomy. We aimed to report and evaluate our surgical and postoperative outcomes of these RALS and compare them to open surgery in patients ≤12 months of age. We hypothesized that robotic surgery would have comparable results to open surgery in infants.
2. Materials and methods
2.1. Study population and design
After obtaining IRB approval, an institutional database of patients who underwent pyeloplasty or ureteroureterostomy was retrospectively reviewed. This database included all patients evaluated at our tertiary children’s hospital from 2012 to 2022. Primary inclusion criteria were patients who underwent either open (control group) or robot-assisted (case group) pyeloplasty (PP) or ureteroureterostomy (UU), and patients ≤12 months. Patients were excluded if they were older than 12 months of age, had both PP and UU performed, or had incomplete medical records.
This study represents an institutional, retrospective, case-control analysis. Data collected included demographics (gender, circumcision status, age at surgery), preoperative variables (Society of Fetal Urology hydronephrosis grade, vesicoureteral reflux, laterality of hydronephrosis, MAG3 split, presence of urinary tract infections), operative variables (operative time, crossing vessels, stent placement), and postoperative variables (hospitalization stay, complications, length of time of inserted stent, stent removal location, last postoperative Society of Fetal Urology grade, surgical improvement indicated, postoperative follow-up length).
Operative time was obtained from the electronic medical record as reported by the operating room personnel. Time was measured in minutes from “Surgery start” to “Surgery finish” and included the retrograde pyelogram/cystoscopy and stent placement. Surgical improvement was defined as decrease in ≥1 hydronephrosis grades according to the Society of Fetal Urology (SFU) classification, and a reduction or absence of ureteral dilation for those who underwent UU.
Data were managed using password-protected Excel files. Imaging data were taken directly from the radiologist’s report.
2.2. Technical surgical considerations
In the open procedures, a retroperitoneal approach was performed using a flank incision and Pfannenstiel incision in PP and UU, respectively. The intra-abdominal approach was used in both the robotic pyeloplasty (rPP) and the robotic ureteroureterostomy (rUU). Three robotic ports without any assistant or other ports and the Intuitive Surgery (Sunnyvale, California) Da Vinci Robotic platform were used in all cases.
From 2012 to 2016 (8 patients undergoing rPP and 1 undergoing rUU) the Si system was used in which 5mm ports were available. For most cases, since 2016, the Xi system with 8mm ports were implemented. Trocar access was gained with a periumbilical robotic port, which was used for the robotic camera, to start each case. In rPP, two more robotic ports were placed in the midline superior and inferior to the robotic port with at least 5cm between them. In rUU, lower quadrant abdominal ports were placed just lateral to the epigastric vessels. Incisions that matched the size of the port were routinely used to avoid port dislodgement, and if the ports were repeatedly coming out, a tegaderm dressing was applied to create a seal between the skin and the port.
Mean insufflation pressure was 10 mmHg and recirculation/filtration systems were not used. In both approaches a monopolar curved scissor and a micro-bipolar forceps were used for the dissection, and the micro-bipolar forceps with a needle driver was used for reconstruction with a poliglecaprone 25 (Monocryl) either a 5-0 or 6-0 in a running fashion for both the renal pelvis and to create the ureteroureterostomy. The Anderson–Hynes technique was used in all pyeloplasty cases, and an end to end UU with wide spatulation was used in all UU cases. If a ureterocele was present, the rUU was performed using the HIdeES techniques with removal of the distal upper ureter and the ureterocele was drained with a catheter and left open. A laparoscopic needle driver was used through one of the robotic ports to pass suture. If suction was required, either a robotic or laparoscopic suction irrigator system was used.
The decision to perform RALS or open surgery was at the discretion of the operating surgeon. Most patients underwent a cystoscopy with retrograde pyelogram and stent placement immediately prior to the robotic or open part of the procedure. Ureteral stents were either left with or without a string and the timing in which they were removed post-operatively was determined by the surgeon and not standardized.
2.3. Study objectives
The objectives of this study were to describe and compare the clinical outcomes of both robotic and open PP and UU surgical courses in the ≤12 months population.
2.4. Statistical analysis
Data were analyzed using IBM SPSS 28.0, and a p-value <0.05 was considered statistically significant. Continuous variables including age at surgery, MAG3 split, operative time, hospitalization stay in days, length of ureteral stent placement in days, and post-operative follow in days were analyzed using independent t-tests with surgical modality (open vs robotic) as the grouping variable. All categorical variables were assessed using either Chi-Squared analysis or Fischer-exact depending on the assumptions met.
3. Results
3.1. Robotic-assisted vs open pyeloplasty
Between 2012 and 2021, 81 patients underwent open pyeloplasty (oPP) and 33 who underwent robotic pyeloplasty (rPP) were included in the study. The indication for pyeloplasty in all patients was ureteropelvic junction obstruction (UPJO). Mean age at surgery in oPP was 4.81 ± 3.1 months (range=0-12 months) and in rPP was 6.24 ± 2.6 months (range=1-11 months) (p=0.13). Mean postoperative follow-up was significantly shorter in the rPP than in the oPP (13.7 months versus 26.4 months, p<0.001). Gender, circumcision status, preoperative grade of hydronephrosis and preoperative MAG3% split renal function were similar between groups (Table 1).
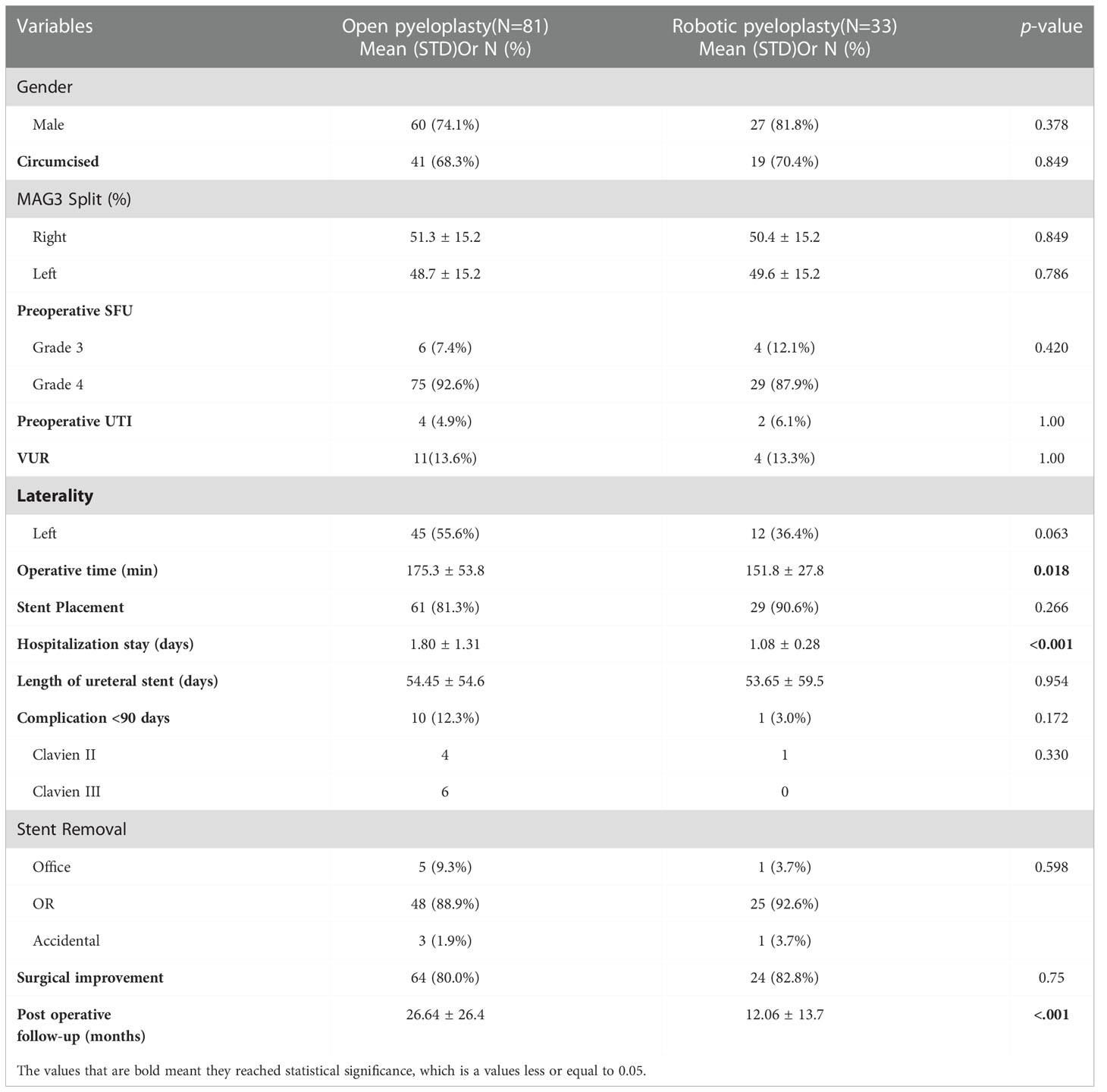
Table 1 Comparison of demographic, clinical, surgical, and postoperative variables between infants undergoing open vs robotic pyeloplasty.
Before pyeloplasty, incidence of urinary tract infection (UTI) was 6.1% in the rPP and 4.9% in the oPP (p=1). The presence of concomitant vesicoureteral reflux (VUR) between the two groups was similar (p=1). Operative time was significantly shorter in the rPP (151.1 ± 27.8 minutes) when compared to the oPP (175.3 ± 53.8) (p=0.018). None of the robotic-assisted pyeloplasties were converted to open procedures. Similarly, hospitalization stay was significantly shorter in the rPP than the in oPP (1.08 ± 0.28 versus 1.80 ± 1.31 days, p<0.001). The time with indwelling ureteral stent and the place of its removal (office, OR, or accidental) was similar between groups (p=0.95 and p=0.60, respectively). The rate of complications during the first 90-days after pyeloplasty and its severity according to the Clavien-Dindo classification were not significantly different between the groups (p=0.174 and p=0.455, respectively). There were no post-operative surgical site infections in either group. Improvement of ≥1 SFU grade of hydronephrosis after surgery was observed in 80% of the patients in the oPP and 82.8% of the patients in rPP (p=0.75).
3.2. Robotic-assisted vs open ureteroureterostomy
Between 2012 and 2022, 9 patients with a primary diagnosis duplex collecting systems who underwent open ureteroureterostomy (oUU) and 12 patients with a primary diagnosis duplex collecting systems who underwent robotic ureteroureterostomy (rUU) were included in the study. Concomitant ureterocele was present in 7 (77.8%) of oUU and 2 (16.7%) of rUU (p=0.009). Moreover, 56% of patients in oUU and 8% in the rUU had concomitant VUR (p=0.048). Mean age at surgery in oUU was 7.67 ± 3.16 months (range=3-12 months) and in rUU was 7.58 ± 2.75 months (range=5-12 months) (p=0.95). Although the oUU group had a longer mean follow-up than the rUU group, the difference was not significant (22 ± 19.37 vs 13.73 ± 13.20 months, respectively, with p=0.295). Gender, MAG3% split renal function, and the initial SFU grade of hydronephrosis of the upper pole moiety were similar among groups (Table 2).
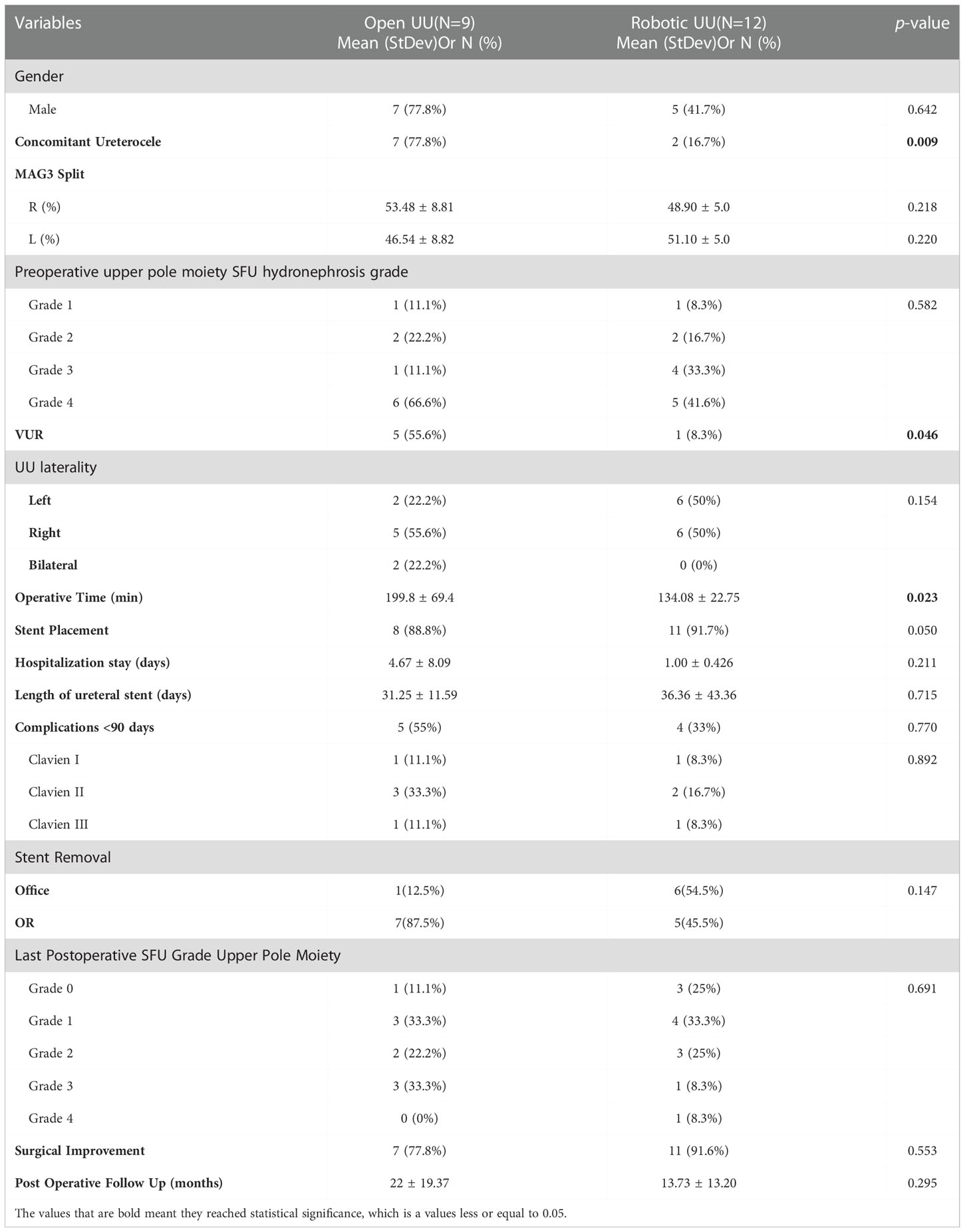
Table 2 Comparison of demographic, clinical, surgical, and postoperative variables between infants undergoing open vs robotic ureteroureterostomy.
Operative time was significantly shorter in the rUU (134.08 ± 22.75 minutes) when compared to the oUU (199.8 ± 69.4 minutes) (p=0.023). Hospitalization stay in the oUU (4.67 ± 8.09 days) and in the rUU (1.00 ± 0.426) was similar (p=0.211). There was no significant difference among length with indwelling stent and place of its removal (office or operative room) between groups (p=0.715 and p=0.147). The rate of complications during the first 90-days after UU and its severity according to the Clavien-Dindo classification were similar between groups (p=0.770 and p=0.892, respectively). There were no post-operative surgical site infections in either group. Only 1 complication unique to the robotic approach was reported in the rUU, an incisional port-site hernia. Improvement of ≥1 SFU grade of hydronephrosis after surgery was observed in 91.6% of the patients in the rUU and 77.8% of the patients in oUU (p=0.553).
4. Discussion
During the last decade, pediatric robotic urologic surgery has gained wide-spread adoption (15). Its instrument articulation with full range of motion, three-dimensional imaging, 10-fold camera magnification, tremor filtering, and limiting of surgeon fatigue, have made it the preferred surgical approach in the repair of many common pediatric urological conditions (9, 16). For instance, from 2005 to 2013, in the pediatric population the annual number of open pyeloplasty decreased by 10% while robotic pyeloplasty increased by 29% (17). Nonetheless, the use of robotic technology in infants remains controversial due to technical limitations such as small working space, large trocars, potential robotic malfunction, increased operative times, and high costs (4).
Our study found that in infants robotic pyeloplasty and ureteroureterostomy are feasible and safe procedures with success and postoperative complication rates similar to those seen in an open approach, and with potential additional benefits such as decreased operative time and hospital length of stay. In our series, the robotic pyeloplasty and UU groups presented significantly shorter operative times than the open pyeloplasty and UU groups, demonstrating that urologic robotic surgeries can be performed even quicker than open surgeries. Bansal et al. also reported significantly shorter operative times in robotic pyeloplasty when compared to open pyeloplasty (4). A quicker learning curve, in contrast to standard laparoscopy, and less dissection and suturing in an infant relative to older children, have been proposed as some of the explanations of why robotic surgeries have shown a decreased operative time in infants (4, 18).
We also found that there was not any significant difference in the number of complications and its severity (according to the Clavien-Dindo classification) during the first 90 postoperative days between the robotic and open approaches in the pyeloplasty and UU cohorts. Although the majority of studies reported similar results (10, 19, 20), some authors report that robotic pyeloplasty in infants has a higher number of complications than open pyeloplasty (4). In the case of UU in patients ≤12 months, there is a paucity of reported data reporting complication rates. Villanueva et al. reported 2 complications unrelated to the surgical technique in infants after undergoing robotic pyeloplasty; however, the study did not clearly state the number of complications that was observed in the open cohort (21). In older children undergoing UU, similar frequency of complication rates was observed between the robotic and open cohorts, with febrile urinary tract infection being the most common one in both groups (22).
Surprisingly, in our study the length of hospital stay was shorter in the robotic pyeloplasty group than in the open group. Lee et al. also found that robotic pyeloplasty patients presented a slightly shorter length of stay (1.6 days) than open pyeloplasty patients (2.1 days) (p=0.04) (22). One potential benefit about this result is decreasing health costs, as hospital length of stay has been reported as one of the most important determinants of health expenses (23). On the other hand, Kawal et al. and Dangle et al. have reported no significant difference in the length of hospital stay between infants undergoing either robotic or open pyeloplasty (10, 24). From the studies conducted in the pediatric population, rUU have shown comparable length of hospital stay to oUU, similar to what we report in our study (25).
Moreover, we found that the surgical success rate between open and robotic approaches in the pyeloplasty and UU cohorts was comparable. Similarly, a multi-institutional study of robotic pyeloplasty in infants reported a success rate of 91%, which has been described to be similar to pure laparoscopic and open approaches (26). Furthermore, in a study analyzing 79 rPP and 22 rUU a radiographic improvement was observed in 92% of infants (27). Even, studies analyzing age as a determinant of success in pediatric robotic surgeries, have found similar success rates independent of the age group (24).
This study is not without limitations. First, it was retrospective in nature and patients were not randomized or matched between the two study groups. Moreover, the number in the UU cohort was small and differed between the sub-groups. Given this small sample size, the study may have been underpowered to detect small differences in outcomes between the groups. In addition, we did not access for pain medication use after pyeloplasty or surgical costs, factors that could have potentially differed between the analyzed surgical approaches. Despite the limitations of this investigation, we believed that the paucity of extant data comparing robotic to open pyeloplasty and UU in infants makes the presented results useful for extending the application of robotic technology to infants, and in family counseling of expectations and future outcomes in postoperative period.
Conclusion
In this retrospective review comparing the clinical outcomes in infants undergoing robotic pyeloplasty and UU to the standard of care open approach, we found that robotic surgery is feasible and a safe procedure in children ≤12 months. Postoperative complications and surgical success are comparable in open and robotic approaches, and in the case of robotic pyeloplasty a decreased in length of hospital stay after surgery can be observed. Further studies and a larger cohort should be considered in the UU group to obtain more generalizable results as well as the cost-effectiveness of performing robotic surgery in infants.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Human Research Protection Program and Institutional Review Board of Nicklaus Children’s Hospital. Written informed consent from the participants’ legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author contributions
MC had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: MC, AA, DN, MCSA. Acquisition, analysis, or interpretation of data: MCSA, YG, AR, SI. Drafting of the manuscript: MA, YG, AR, SI, DN. Critical revision of the manuscript for important intellectual content: MC, DN, AA. Statistical analysis: MCSA, YG. Supervision: MC. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Polok M, Borselle D, Toczewski K, Apoznański W, Jędrzejuk D, Patkowski D. Laparoscopic versus open pyeloplasty in children: experience of 226 cases at one centre. Arch Med Sci (2019) 16(4):858–62. doi: 10.5114/aoms.2019.84496
2. O’Reilly PH, Brooman PJC, Mak S, Jones M, Pickup C, Atkinson C, et al. The long-term results of Anderson–hynes pyeloplasty. BJU Int (2001) 87(4):287–9. doi: 10.1046/j.1464-410x.2001.00108.x
3. Troxel S, Das S, Helfer E, Nugyen M. Laparoscopy versus dorsal lumbotomy for ureteropelvic junction obstruction repair. J Urol. (2006) 176(3):1073–6. doi: 10.1016/j.juro.2006.04.072
4. Bansal D, Cost NG, DeFoor WR, Reddy PP, Minevich EA, Vanderbrink BA, et al. Infant robotic pyeloplasty: comparison with an open cohort. J Pediatr Urol. (2014) 10(2):380–5. doi: 10.1016/j.jpurol.2013.10.016
5. Bilgutay AN, Kirsch AJ. Robotic ureteral reconstruction in the pediatric population. Front Pediatr (2019) 7:85. 10.3389/fped.2019.00085
6. Richards HW, Kulaylat AN, Cooper JN, McLeod DJ, Diefenbach KA, Michalsky MP. Trends in robotic surgery utilization across tertiary children’s hospitals in the united states. Surg Endosc. (2021) 35(11):6066–72. doi: 10.1007/s00464-020-08098-y
7. Finkelstein JB, Levy AC, Silva MV, Murray L, Delaney C, Casale P. How to decide which infant can have robotic surgery? just do the math. J Pediatr Urol. (2015) 11(4):170.e1–4. doi: 10.1016/j.jpurol.2014.11.020
8. Andolfi C, Adamic B, Oommen J, Gundeti MS. Robot-assisted laparoscopic pyeloplasty in infants and children: Is it superior to conventional laparoscopy? World J Urol (2020) 38(8):1827–33. doi: 10.1007/s00345-019-02943-z
9. Kim C. Robotic urologic surgery in infants: Results and complications. Front Pediatr (2019) 7:187. doi: 10.3389/fped.2019.00187
10. Dangle PP, Kearns J, Anderson B, Gundeti MS. Outcomes of infants undergoing robot-assisted laparoscopic pyeloplasty compared to open repair. J Urol. (2013) 190(6):2221–6. doi: 10.1016/j.juro.2013.07.063
11. Li P, Zhou H, Cao H, Guo T, Zhu W, Zhao Y, et al. Early robotic-assisted laparoscopic pyeloplasty for infants under 3 months with severe ureteropelvic junction obstruction. Front Pediatr (2021) 9:590865. doi: 10.3389/fped.2021.590865
12. Bergholz R, Botden S, Verweij J, Tytgat S, Van Gemert W, Boettcher M, et al. Evaluation of a new robotic-assisted laparoscopic surgical system for procedures in small cavities. J Robot Surg (2020) 14(1):191–7. doi: 10.1007/s11701-019-00961-y
13. Bludevich BM, Danielson PD, Snyder CW, Nguyen ATH, Chandler NM. Does speed matter? a look at NSQIP-p outcomes based on operative time. J Pediatr Surg (2021) 56(6):1107–13. doi: 10.1016/j.jpedsurg.2021.02.033
14. Trevisani LFM, Nguyen HT. Current controversies in pediatric urologic robotic surgery. Curr Opin Urology. (2013) 23(1):72–7. doi: 10.1097/MOU.0b013e32835b0ad2
15. Stern N, Wang P, Dave S. Instituting robotic pediatric urologic surgery in the Canadian healthcare system: Evaluating the feasibility and outcomes of robot-assisted pyeloplasty and ureteric reimplantation. Can Urol Assoc J (2021) 15(4):E215–20. doi: 10.5489/cuaj.6604
16. Cundy TP, Shetty K, Clark J, Chang TP, Sriskandarajah K, Gattas NE, et al. The first decade of robotic surgery in children. J Pediatr Surg (2013) 48(4):858–65. doi: 10.1016/j.jpedsurg.2013.01.031
17. Varda BK, Johnson EK, Clark C, Chung B, Nelson CP, Chang S. National trends of perioperative outcomes and cost for open, laparoscopic and robotic pediatric pyeloplasty. J Urol. (2014) 191(4):1090–5. doi: 10.1016/j.juro.2013.10.077
18. Samadi D, Levinson A, Hakimi A, Shabsigh R, Benson MC. From proficiency to expert, when does the learning curve for robotic-assisted prostatectomies plateau? The Columbia university experience. World J Urol. (2007) 25(1):105–10. doi: 10.1007/s00345-006-0137-4
19. Lee RS, Retik AB, Borer JG, Peters CA. Pediatric robot assisted laparoscopic dismembered pyeloplasty: comparison with a cohort of open surgery. J Urol. (2006) 175(2):683–7; discussion 687. doi: 10.1016/S0022-5347(05)00183-7
20. Srougi V, Yorioka M, Sanchez DCJ, Onal B, Houck CS, Nguyen HT. The feasibility of robotic urologic surgery in infants and toddlers. J Pediatr Urol. (2013) 9(6 Pt B):1198–203. doi: 10.1016/j.jpurol.2013.05.011
21. Villanueva CA. Open vs robotic infant ureteroureterostomy. J Pediatr Urol. (2019) 15(4):390.e1–4. doi: 10.1016/j.jpurol.2019.05.003
22. Lee NG, Corbett ST, Cobb K, Bailey GC, Burns AS, Peters CA. Bi-institutional comparison of robot-assisted laparoscopic versus open ureteroureterostomy in the pediatric population. J Endourol. (2015) 29(11):1237–41. doi: 10.1089/end.2015.0223
23. Brian E. Foundation for medical care control of hospital utilization: CHAP — a PSRO prototype. New Engl J Med (1973) 288(17):878–82. 4571246. doi: 10.1056/NEJM197304262881704
24. Kawal T, Srinivasan AK, Shrivastava D, Chu DI, Van Batavia J, Weiss D, et al. Pediatric robotic-assisted laparoscopic pyeloplasty: Does age matter? J Pediatr Urol (2018) 14(6):540.e1–6. doi: 10.1016/j.jpurol.2018.04.023
25. Ellison JS, Lendvay TS. Robot-assisted ureteroureterostomy in pediatric patients: current perspectives. Robot Surg (2017) 4:45–55. doi: 10.2147/RSRR.S99536
26. Avery DI, Herbst KW, Lendvay TS, Noh PH, Dangle P, Gundeti MS, et al. Robot-assisted laparoscopic pyeloplasty: Multi-institutional experience in infants. J Pediatr Urol. (2015) 11:590865(3). doi: 10.3389/fped.2021.590865
Keywords: robotic pyeloplasty, robotic ureteroureterostomy, robotic surgery, infant, open pyeloplasty, open ureteroureterostomy, pediatric urology
Citation: Suarez Arbelaez MC, Ghattas Y, Raymo A, Isern S, Alam A, Nassau DE and Castellan M (2022) Safety and feasibility of performing robotic ureteroureterostomy and robotic pyeloplasty in infants. Front. Urol. 2:1001054. doi: 10.3389/fruro.2022.1001054
Received: 22 July 2022; Accepted: 30 November 2022;
Published: 19 December 2022.
Edited by:
Christina Ho, Children’s National Hospital, United StatesReviewed by:
Mohan S Gundeti, The University of Chicago, United StatesMahesh R Desai, Muljibhai Patel Urological Hospital, India
Copyright © 2022 Suarez Arbelaez, Ghattas, Raymo, Isern, Alam, Nassau and Castellan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Miguel Castellan, bWlndWVsLmNhc3RlbGxAZ21haWwuY29t
 Maria Camila Suarez Arbelaez
Maria Camila Suarez Arbelaez Yasmine Ghattas
Yasmine Ghattas Adele Raymo
Adele Raymo Samantha Isern
Samantha Isern Alireza Alam
Alireza Alam Daniel E. Nassau
Daniel E. Nassau Miguel Castellan
Miguel Castellan