- 1Department of Psychiatry, Psychotherapy, Psychosomatics and Medical Psychology, Center for Advanced Psychology in Plastic and Transplant Surgery, Medical University of Innsbruck, Innsbruck, Austria
- 2Division of Plastic Surgery, Brigham and Women’s Hospital, Boston, MA, United States
- 3Department of Visceral, Transplant and Thoracic Surgery, Center of Operative Medicine, Medical University of Innsbruck, Innsbruck, Austria
- 4Department of Plastic and Reconstructive Surgery, Vascularized Composite Allotransplantation (VCA) Laboratory, Johns Hopkins University School of Medicine, Baltimore, MD, United States
Vascularized Composite Allotransplantation (VCA) offers a unique option to restore form and function after limb loss or facial trauma that cannot be satisfactorily accomplished through traditional prosthetics or reconstructions. Establishing a successful Upper Extremity Transplantation (UET) program requires strong leadership and a structured surgical team, and extensive interdisciplinary collaboration. We conducted a qualitative study among 12 health care professionals and patients. Informed consent was obtained per protocol, and semi-structured interviews were conducted online and recorded. Participants reported their perceptions of factors that either favored or hindered a successful outcome, including functional status before and after surgery, preparation for transplant, shared decision-making, rehabilitation, and psychosocial support. Thematic analysis revealed that it is essential to establish a team comprising various disciplines well before performing VCA procedures. Defining a common goal and choosing a defined leader is a key factor in procedural success and requires open collaboration beyond what is typical. Primary described categories are interdisciplinary collaboration and skills of the VCA team, building and leading a VCA team, pre-transplant procedures, post-transplant course, and factors to consider when establishing a program. The basic roles of team science play an outsized role in establishing a VCA program. Transplantation medicine involves various overlapping scientific and medical categories requiring health professionals to consciously work together to establish complex vertical and horizontal communication webs between teams to obtain positive outcomes. In addition to medical considerations, patient-specific factors such as transparent communication, therapy plan establishment, plan adherence, and continual follow-up are significant factors to overall success.
Introduction
Vascularized Composite Allotransplantation (VCA) has emerged as a promising reconstructive technique to restore form and function among patients suffering from devastating limb and facial injuries. Given the complexities intrinsic to composite grafts, implementation of an upper extremity (UE) VCA program requires meticulous planning, robust infrastructure, and multidisciplinary collaboration. In this manuscript, we will explore these crucial elements, ranging from surgical expertise and immunosuppression protocols to ethical considerations and long-term sustainability. By illuminating the often-unseen intricate tapestry that forms the foundation of a thriving VCA initiative, we hope to highlight overlooked criteria that will help guide medical institutions and practitioners toward establishing and fostering successful VCA programs, ultimately benefiting patients worldwide.
VCA involves melding multiple intricate microsurgical techniques, requiring the expertise of microvascular, orthopedic, and plastic surgeons working together to repair various tissue types, while concurrently efficiently communicating to reduce ischemic time (1–3). Meanwhile, effective donor procurement is integral to procedural success and necessitates a strong relationship with local organ procurement organizations (OPOs). This may be achieved via frequent meetings with OPOs and practice procurements (4–6). The procurement process must optimize donor identification as well as donor-recipient matching for immunological compatibility to minimize the substantial risk of rejection. This in turn requires expertise in transplant immunology to establish immunosuppression protocols determining appropriate patient-specific regimens to prevent rejection while mitigating side effects and complication risks. Overarching the above considerations is the perioperative period, which requires a complex balance of physical and psychological support (7–12). UE transplantation is both physically and psychologically taxing, limiting its suitability to a subset of the patient population who are both motivated and prepared for the inevitable challenges and setbacks during recovery. This is best accomplished via rigorous patient selection criteria and comprehensive evaluation of potential recipients including medical/physical, psychological, and social support factors to ensure they can cope with the procedure, and adhere to the post-transplant care plan (7, 13). An interdisciplinary team of psychologists, physical therapists, and occupational therapists should be involved in the pre- and post-transplant rehabilitation process as recipients prepare for surgery, then work to regain functional use of the transplanted limb (14). For instance, psychiatric teams should assess patients’ ability to accept the new graft as part of their body, as well as coping mechanisms they possesses that will help them navigate media attention, ongoing intensive medical care, and intimate reliance on caregivers (12). Specifically, psychiatric providers must screen for underlying psychiatric conditions, perceptions of body image, overall quality of life, and ability to adhere to follow-up care (8). Concurrently, other team members must establish the complicated rehabilitation protocols required for successful VCA, which include elements such as preoperative functional assessments, initial postoperative evaluation, intermediate therapy, and late maximization of function (15). Thus, a successful VCA program requires not only exceptional surgical skill, but open and detailed collaboration among various medical groups, including transplant medicine, immunology, rehabilitation, psychiatry, and social work.
Outside of the procedure itself, there are multiple domains to consider. For instance, VCA raises a host of other issues, such as informed consent, donor source, and allocation policies (16, 17). Ensuring compliance with these ethical, legal, and regulatory requirements is essential to the establishment and functioning of a VCA program. At the same time, VCA is a costly procedure, and securing adequate financial support and resources for the program's sustainability is crucial. This includes funding for surgeries, immunosuppressant medication, follow-up care, and research. In particular, a commitment to ongoing research and innovation is essential to improve outcomes, reduce complications, optimizing the procedure's cost/benefit ratio, and thereby improve future odds for long-term success. Similarly, raising public awareness about VCA can help foster support for the program both financially and by increasing the number of potential donors.
Overall, successful development of a VCA program for upper extremities requires a dedicated and multidisciplinary approach that considers medical, ethical, financial, and logistical aspects to provide the best possible outcomes for patients.
Materials and methods
Participants
All participants in the study were either patients that underwent UE VCA, recipients’ relatives, or health care professionals in the interdisciplinary VCA team at the Medical University Hospital Innsbruck. Participants received an introductory email requesting participation in an online interview and provided written informed consent. All study activities were approved by the Ethics Committee of the Medical University Hospital, Innsbruck (vote-nr. 1036/2023).
Interviews
Interviews were conducted between 04/2021 and 08/2021. We conducted a total of 12 interviews: four with UE VCA transplanted patients, one with a patient's relative, and seven with UE VCA health care professionals. A trained interviewer conducted the interviews using a semi-structured guide. The interview guide consisted of open-ended questions that asked participants about their perceptions of factors that either favored or hindered a successful transplant outcome. Topics included functional status before surgery, experience with the preparation for transplant, decision process and information transfer, rehabilitation and functional outcome after surgery, and family and social support. Interviews were conducted online and recorded with the interviewees’ consent. Subsequently, a qualitative analysis of the interview transcripts was performed.
Thematic analysis
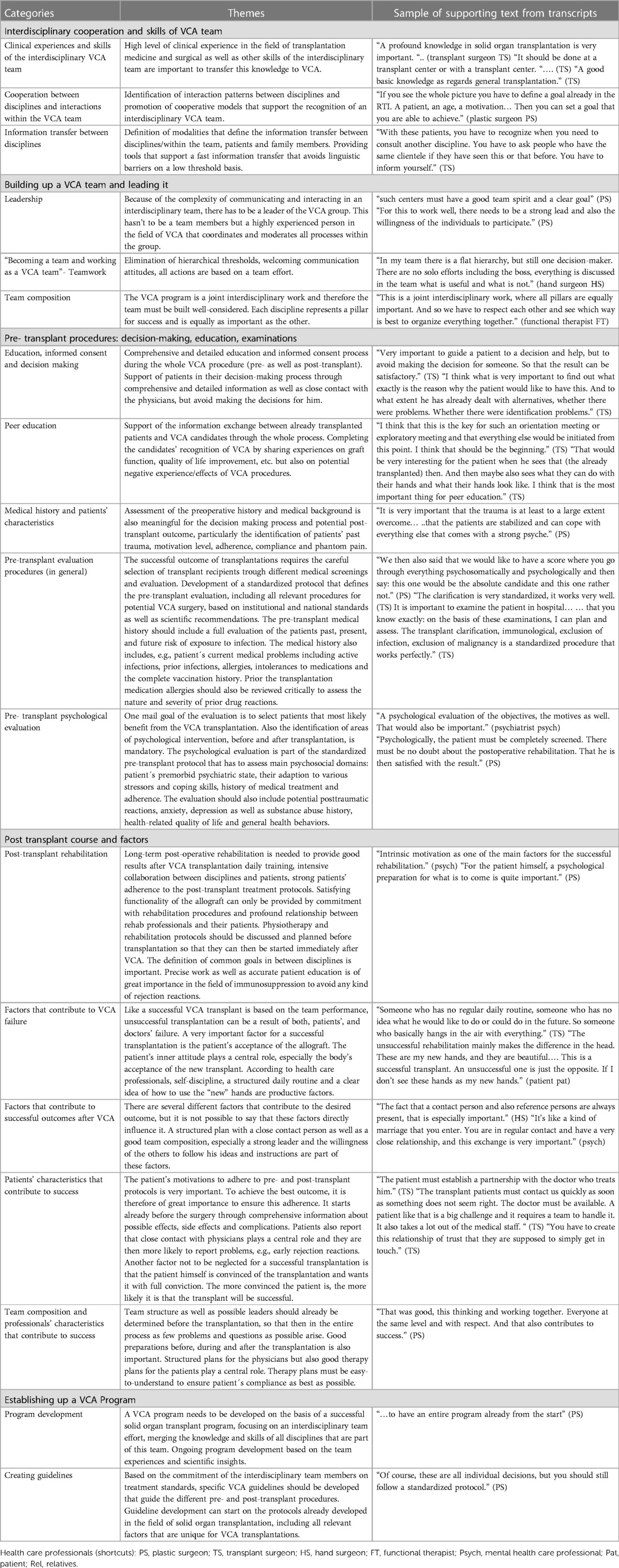
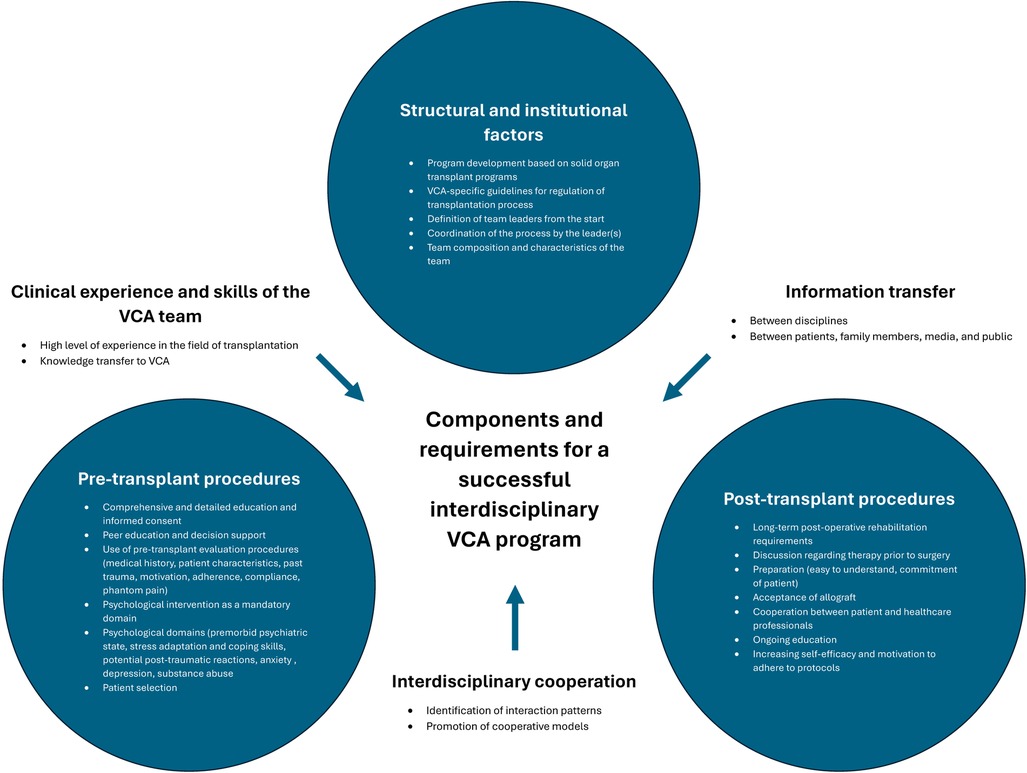
Thematic analysis was performed utilizing a standard qualitative methods. Salient words or phrases pertaining to factors influencing UE VCA success were coded into 51 codes and 10 subcodes which were applied to all transcript data. Codes were then categorized into themes, ensuring appropriate internal homogeneity shared within groups but with sufficient external heterogeneity to be distinct from other themes. We used qualitative analysis software (Atlas.ti, https://atlasti.com/) to extract citations supporting the themes. The interview recordings were reviewed to identify themes, using the qualitative analysis software to index their digital location in the recordings. All investigators agreed upon a thematic map showing relationships between the individual themes and the guiding questions of the study (see Table 1 and Figure 1).
Results
Patients, their relatives, and healthcare workers identified five critical components of a successful VCA program: interdisciplinary collaboration and VCA team skills, building and leading a VCA team, pre-transplant procedures, post-transplant course and factors, and establishing a VCA program. There is a dynamic interplay between these factors; for instance, efficient interdisciplinary collaboration and the development of team skills influences the ability of the team to build and lead, which in turn influences the implementation of thorough pre-transplant procedures and the understanding of the post-transplant course. It is the interaction of these components both among themselves (i.e., horizontally) and between one another (i.e., vertically) that underlines the holistic nature of building and sustaining a successful VCA program.
Interdisciplinary cooperation and skills of VCA team
Participants emphasized the importance of clinical knowledge, stating “…a profound knowledge in solid organ transplant is very important.” A significant level of clinical expertise in transplantation medicine, coupled with reconstructive surgical proficiency and a diverse skill set within the interdisciplinary team, is crucial for effectively applying this knowledge to VCA.
This involves pinpointing interaction patterns between different disciplines and fostering collaborative models that enhance the cohesion of an interdisciplinary VCA team. One respondent stated, “With these patients, you have to recognize when you need to consult another discipline.” Challenges to collaboration during procedures may include unrecognized biases by doctors against crossing surgical subspecialty silos, lack of familiarity with OR and support staff protocols by team members who may not often collaborate given the relative rarity of VCA procedures, and unspoken assumptions regarding the responsibilities and skill sets of participants. It also involves establishing clear modalities for information exchange beyond surgeons to other team members, patients, and their families. Equipping the team with tools that facilitate swift information transfer, while minimizing language barriers on an accessible platform, is essential. In this domain, challenges range from time pressures on team members and coordination of responsibilities for disseminating complex information to the potential for misunderstandings by patients and their support groups due to lack of context and the volume of medical information to be digested. Thus, equipping teams with tools that facilitate swift information transfer while minimizing vocabulary and language barriers is essential.
Building a VCA team and leading it
As discussed above, VCA programs extend far beyond the OR. The comprehensive care team encompasses experts and their support staff in Plastic Surgery, Orthopedic Surgery, Transplant Surgery, Transplant Medicine, Radiology, Pathology, Dermatology, Occupational and Physical Therapy, Psychology, Social Work, and Ethics (4). Given the complexity of these teams and the specialized knowledge they possess, selection of an experienced leader with team management skills is imperative to ensure group cohesion. This is not always the most senior team member. While their gravitas may be an asset, more important is the ability to collaborate in ways that encourage speaking freely, and challenging experts in diverse fields to consider other team members’ opinions. Once established, the leader must take responsibility to actively mediate group deliberations and ensure expertise from each discipline is first collected horizontally from all levels within a team, and then properly evaluated and disseminated vertically between teams. This sentiment backed repeatedly in interview responses stating for example “(F)or this to work well, there needs to be a strong lead and also the willingness of the individuals to participate.” In this way, VCA participants emphasize the importance to them of group deliberation and the intentional inclusion of all team members by a leader capable of executing this difficult assignment. For example, one participant stated, “In my team there is a flat hierarchy, but still one decision-maker. There are no solo efforts including the boss, everything is discussed in the team what is useful and what is not.”
Pre-transplant procedures: decision making, education, and examinations
Prior to initiating treatment, clinicians must engage in shared decision-making with VCA candidates. Patient-centered language should be used to discuss each aspect of the procedure including preoperative screening, pharmacological therapies, recovery and rehabilitation, potential complications, and alternative options. Interviewees highlight the careful balance clinicians must take, stating it is “… very important to guide a patient to a decision and help, but to avoid making the decision for someone, so that the result can be satisfactory.” Clinicians in all disciplines should be pressed to acknowledge and emphasize patient autonomy as the ultimate arbiter in choosing whether to proceed with treatment, something that can be downplayed by even the most well-meaning practitioners.
Although easy to overlook, VCA patients also emphasize the benefits of exchanging information with other recipients. In particular, witnessing grafts first-hand helps prepare patients viscerally for their own choice, while sharing experiences affords them a sense of community. Thus, early integration with other VCA patients should, if practicable, be considered a mandatory part of patient education. Additionally, the foundation of VCA patient support groups is very important, e.g., the recently initialized international group “VCA world” (url: www.worldofvca.com).
In addition, potential VCA recipients must undergo extensive preoperative evaluation. Initially, assessments of patients’ past medical histories can be used to evaluate potential candidates. Patients must then undergo extensive additional screening prior to be listed for allotransplantation including preoperative testing with transplant medicine, renal, infectious disease, critical care, and rehabilitation services. Other workup includes routine transplantation laboratory testing, electromyography/nerve conduction studies, and imaging of both upper extremities.
Meanwhile, a comprehensive psychological evaluation must be an integral component of the standardized pre-transplant protocol. Patients undergo a thorough psychiatric history including post-traumatic reactions, anxiety, depression, and substance use. Clinicians must also ascertain their coping mechanisms and ability to adapt to different stressors as well as their level of motivation and adherence to previous medical treatments and their present level of motivation. Assessing health-related quality of life and general health behaviors is also essential.
Post-transplant course and factors
Achieving optimal results after a hand transplantation requires extensive post-operative rehabilitation. Daily training, close collaboration between various disciplines and patients, and strict adherence to treatment plans are pivotal for success. Intrinsic motivation stands out as a key factor in driving successful rehabilitation, and by extension, transplantation. Patients must undergo psychological preparation to ready themselves for what lies ahead. The team must also find out what is driving a patient's desire for VCA, as stated, “I think what is very important to find out what exactly is the reason why would like to have this. And to what extent he has already dealt with alternatives, whether there were problems.”
Physiotherapy protocols should be thoroughly discussed in an interdisciplinary manner and planned well in advance of the transplantation to avoid any delays in initiating the rehabilitation process. Disciplines must work vertically in a cohesive and open manner to establish mutual objectives. Then, educating patients about their responsibilities in the success of the VCA in language they can internalize is of paramount importance, particularly regarding immunosuppression. As a life-long and largely self-administered immunosuppression plan is required to prevent rejection, safeguarding the success of the procedure and the recipient's well-being cannot be achieved without full patient participation.
Certain characteristic patterns contribute significantly to success. As mentioned, the patient's motivation and adherence are crucial. As stated below, “Intrinsic motivation as one of the main factors for the successful rehabilitation.” Patients need to trust those responsible for their care, which is built step-by-step from the initial conversation and then throughout the VCA process via techniques including transparent communication delivered without hyperbole. Caregivers should acknowledge the primacy of patients’ viewpoints by showing empathy toward their emotional and physical challenges, and by encouraging them to participate in decision-making about their care, providing agency and enhancing trust. Doctors should be prepared to answer queries repeatedly, and contact persons, including physicians, surgeons, and medical staff, should be as accessible as possible as a close relationship is imperative for reporting any issues. Dr. Kumnig uses the phrase, “It's like a kind of marriage you enter …”
The patient's inner attitude is closely linked to the success of the transplantation as acceptance of the new transplant is pivotal. Patients must integrate the new allograft as part of their own body. They need to feel it, see it, and use it. In the interviews, the patients themselves expressed that they perceived the new hand as an integral part of their own body, emphasizing they felt this perception was instrumental in achieving significant success.
In summary, the composition and attributes of the professional team hold significant importance in this context. Potential leaders should be identified prior to transplantation. The planning stages—before, during, and after the surgery—are essential and must be precisely executed. Collaboration should be rooted in respect, with disciplines functioning as one cohesive team. Therapy plans should be straightforward to ensure patient adherence to treatment plans.
Establishing a VCA program
To ensure the success of a transplant, it is imperative to have a comprehensive VCA program in place from the outset. These programs should be built on the foundation of established programs for solid organ transplant, with a primary emphasis on interdisciplinary teamwork. The program should draw from the collective experiences of the team and be guided by current scientific knowledge and insights.
Adherence to standardized protocols and guidelines is essential. Specific guidelines tailored for VCA must be established to provide a clear framework for professionals to navigate through pre- and post-transplant procedures. The development of these guidelines should start early on and draw from the field of solid organ transplantation, while also incorporating factors that are unique to VCA. On respondent stated, “Of course, these are all individual decisions, but you should still follow a standardized protocol Of course, these are all individual decisions, but you should still follow a standardized protocol.”
While individual decisions may be necessary for each VCA transplant, it is crucial to adhere to standardized protocols to ensure consistency and optimal outcomes.
Discussion
We have strived to illuminate patient, family, and healthcare worker perspectives, values, and expectations of VCA programs. Our data provides valuable insights into the areas where providers’ and patients’ opinions are in agreement, and where they differ. Notably, while providers frequently commented on the structural elements of VCA programs, patients, perhaps unsurprisingly, more often discussed the psychosocial impact of the procedure. Combining these at times disparate viewpoints yields a more robust understanding of the critical components of a VCA program. Through this lens, we identified central themes including interdisciplinary cooperation and skills of the VCA team, forming a VCA team and leading it, pre-transplant procedures including decision-making, education, examinations, post-transplant course and factors, and establishment of a viable VCA program.
These themes are of particular importance when establishing a UE program given the unique aspects of VCA compared to the more extensively studied solid organ transplantation (SOT). In particular, VCA is a non-lifesaving treatment requiring substantial ongoing medical, psychological, and social support. While SOT recipients typically rely on their transplanted organ for survival, making transplantation more urgent, VCA patients are generally medically stable. Thus, providers have the luxury to spend more time choosing appropriate candidates and conducting screening procedures while patients have the leeway to deliberate if the procedure and team are a good match for their goals. In addition, VCA is a very complex surgical procedure, and rehabilitation and clinical outcomes are highly dependent on patient participation, necessitating identification of motivated, psychologically stable candidates with ample psychosocial support systems. Limb transplantation itself leads to substantial patient stress related to lifestyle changes, media attention, and inevitable reliance on family and friends, further underscoring the importance of a robust support system. At the same time, patient and family support, education, and advocacy is critical in discussing immunosuppression, the experimental nature of some aspects of these operations, and plans for failure including explantation to ensure patients are making a fully informed decision when consenting to undergo this elective procedure. Finally, VCA involves complex teamwork and requires strong leadership, collaboration between specialties, and appropriate hospital infrastructure.
Ethical and legal considerations vary between both transplantation programs, as they are influenced by the nature of the transplanted tissues and their impact on identity and autonomy. These issues may diverge from those encountered in SOT. In comparison to functional outcomes and quality of life, VCA has the potential to restore complex functions such as motor control, sensation, facial expressions what then significantly improves the quality of life. It's imperative that these aspects are thoroughly discussed as part of informed consent procedures and carefully considered in treatment plans. SOT prolong life and improve health, it's important to note here that it not always restores the full range of organ function or address aesthetic concerns.
It's evident that there are differences between these two organ transplantation procedures, highlighting the necessity for specialists and tailored approaches in both. Additionally, it's crucial to emphasize that both types of transplantations require an interdisciplinary approach and collaboration with both medical and non-medical professionals.
VCA relies on a near-seamless integration of expertise from various specialists, whose scope of practice may not otherwise overlap, in order to effectively complete an infrequent and challenging procedure. In this domain, team science can help explain how to promote communication and collaboration to achieve the common goal of optimized patient outcomes. Griffith et al. investigated the role of team dynamics in VCA programs, finding that regular ongoing meetings such as potential recipient reviews and discussions of transplantation criteria—even in the absence of an active candidate—helped to foster team cohesion and the contribution of individual expertise. In addition, practice sessions to refine protocols, rehearse transplantation techniques, and review safety and transitions improved procedures and helped identify potential areas requiring additional planning and training (18, 19). In cases of unexpected complications or emergencies, a well-coordinated team is essential for making rapid decisions and providing the best possible care (18, 20–22).
VCA also requires substantial lifelong commitment from the recipient. In selecting VCA candidates, clinicians must help patients carefully weigh the benefits (i.e., return of function and potentially improved quality of life) with the substantial risks (i.e., graft rejection and overall decreased life expectancy) while concurrently emphasizing patient autonomy. Dumont et al. proposed strategies to facilitate informed decision-making including absence of urgency to decide, acceptance of uncertainty of outcomes, and space for reluctance as the patient grapples with the possibility of transplantation (23). Novel avenues to thoroughly communicate with patients regarding the VCA process have been proposed; notably an eLearning program has been designed to train donor professionals which yielded improved clinician confidence and may help improve provider-patient communication (24). Similarly, educational websites have been developed to provide patients with educational information and found to have high patient satisfaction (17).
Patients opting for allotransplantation must then undergo a substantial medical and psychological workup. Though no universal selection guidelines have been established, a systemic review analyzing shared criteria between various facial transplant programs determined that common factors include e. g. psychological stability, overall appropriate physical status, and medical adherence (25). Meanwhile, Laspro et al. found that eligibility criteria for hand transplantation were consistently centered around capacity to manage the allograft, including access to follow-up, insurance coverage, psychological stability, history of medical adherence, but noted that factors related to immunosuppression were less emphasized (26). From a patient perspective, the most important themes regarding UE VCA selection criteria are younger age, good physical health, mental stability, willingness to “put in the work,” presence of specific amputation characteristics, and sufficient social support (16). Understanding such perspectives aids clinicians in aligning with patient expectations of the allotransplantation experience, and leads to enhanced patient education regarding the process (24).
Indeed, identification of an enthusiastic, motivated, and psychologically stable candidate equipped to cope with unique physical and psychosocial challenges is paramount (9). Psychological assessment procedures including the diagnostic interview as well as instruments such as the Psychosocial Assessment of Candidates for Transplantation (27) and the Stanford Integrated Psychosocial Assessment for Transplantation (28) have been employed. In addition, it is important to assess patients’ psychiatric history, body image adaptation to trauma, cognitive preparedness, coping techniques, and motivation (10). Kumnig et al. determined that, among hand transplant candidates, psychological impairments commonly include social withdrawal, embarrassment, and poor quality of life; while motivation for transplant varied based on bi- versus unilateral impairment, native versus accidental hand loss, and degree of social integration (11). In addition, lower-risk candidates have been identified as those with realistic expectations and ability to actively participate in physical therapy (13). Of note, psychosocial factors have been demonstrated to be predictive of clinical outcomes among solid organ transplant recipients—a phenomenon which may extend to VCA patients (29). In particular, depression and impaired cognitive function, and posttransplant psychological factors are associated with increased clinical risk among SOT patients. Meanwhile, psychological flexibility and self-efficacy may be protective (29). In VCA UE recipients, rejection has been observed in 33% of patients with depression, 22% of those with posttraumatic stress disorder, and 17% of individuals with anxiety (7). These factors may contribute to patients’ motivation to adhere to the lifelong therapies required to sustain the allograft. Several studies have indicated a higher incidence of organ-related complications and an elevated risk of organ rejection in non-adherent patients. Unsurprisingly, the need for expert interdisciplinary collaboration permeates into the psychosocial domain as well. Hummel et al. conducted semi-structured interviews among UE staff, transplant patients, and relatives and determined that interdisciplinary teams with adequate resources for patient selection as well as ongoing close provider involvement contribute to transplantation success (30).
Similarly, social work departments play a vital role in ensuring that a robust social support system is in place as patients work to regain a sense of self, body image, and identity (9, 12, 30–32). In particular, patients and their caregivers have identified community and caregiver support as crucial factors in VCA success (33, 34). Regrettably, inclusion of social criteria in candidate selection introduces an inherent inequity; and as VCA becomes more mainstream it will be incumbent on researchers to determine the association between social support and patient outcomes, and how to attenuate social risk among marginalized individuals with fewer resources.
Achieving a successful transplant outcome requires the active involvement and dedication of the patient. Adherence to medical advice, open communication with the transplant team, and utilization of social support networks are pivotal elements in ensuring long-term transplant success.
Limitations
There are several limitations of this work including the small sample size of 12 participants. This reflects an intrinsic challenge of VCA research as the patient population worldwide is quite limited, and thus better suited for qualitative, rather than quantitative, analyses. Another limitation is that our data is skewed by the larger proportion of interview responses from healthcare providers than patients, making the sentiments of VCA team members more heavily represented. Thus, our results primarily focus on provider opinions with complementary insights from VCA recipients. In addition, we identified discrepancies in the content of responses between providers and patients. This is likely related to an additional question about the psychological impact of VCA which was included in the patient interview, prompting VCA recipients to focus on their individual experiences while providers discussed the more structural elements of the program. In a related fashion, patients, who are more intimately familiar with their own VCA journey are more likely to comment on this aspect of the process than providers. Another limitation is the absence of media-related aspects in the interview. There was no discussion about how the public media reacted to transplant recipients and how extensively information about allotransplantation is disseminated. Additionally, no intraoperative or surgical questions were asked; instead, the questions primarily focused on the psychosocial aspects of transplantation. Intraoperative issues, difficulties, and challenges were not mentioned, which would undoubtedly bring about new insights. Future interviews should include questions related to surgical technique, intraoperative complications, and the interplay between various specialties in the OR.
Other important points not addressed in the work are the abilities and skills of the patients. Considering these would certainly provide more insights and a better understanding of what to look for when selecting patients. A study focusing primarily on patients, their characteristics, abilities, and traits would undoubtedly significantly impact the field of VCA.
Furthermore, a detailed discussion of ethical and political aspects was also missing from the interview questions. Future studies should also place greater emphasis on surgical aspects such as intraoperative challenges, team dynamics, as well as pre-, intra-, and postoperative difficulties. Additionally, immersing the patients’ abilities and skills could provide valuable insights and enhance understanding of VCA outcomes Addressing these aspects can enhance both pre- and post-transplantation processes and treatment plans.
Conclusions
Team science plays a critical role in establishing and maintaining a VCA program. Complex vertical and horizontal communication webs between teams and important. Interdisciplinary cooperation, team-building, and shared decision-making are all important components to success.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics Committee of the Medical University of Innsbruck. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their informed consent to participate in this study.
Author contributions
MK: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. CK: Data curation, Formal Analysis, Investigation, Visualization, Writing – original draft, Writing – review & editing. AZ: Formal Analysis, Validation, Visualization, Writing – original draft, Writing – review & editing, Investigation. GB: Formal Analysis, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. ST: Formal Analysis, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
ST receives grant support from the Department of Defense (DoD) for research into hand transplantation: DoD Congressionally Directed Medical Research Programs: W81XWH-16-2-0067, W81XWH-17-1-0400, and W81XWH-19-RTRPQRA. Opinions, interpretations, conclusions, and recommendations are those of the authors and are not necessarily endorsed by the Department of Defense.
Acknowledgments
We would like to thank all patients and colleagues that over several years generously have shared their experience within the field with us.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
HRQOL, health related quality of life; QOL, quality of life; VCA, vascularized composite allotransplantation; UE, upper extremity.
References
1. Hartzell TL, Benhaim P, Imbriglia JE, Shores JT, Goitz RJ, Balk M, et al. Surgical and technical aspects of hand transplantation: is it just another replant? Hand Clin. (2011) 27(4):521–30. doi: 10.1016/j.hcl.2011.08.001
2. Shores JT, Brandacher G, Schneeberger S, Gorantla VS, Lee WPA. Composite tissue allotransplantation: hand transplantation and beyond. J Am Acad Orthop Surg. (2010) 18:127–31. doi: 10.5435/00124635-201003000-00001
3. Schneeberger S, Gorantla VS, Brandacher G, Zeevi A, Demetris AJ, Lunz LG, et al. Upper-extremity transplantation using a cell-based protocol to minimize immunosuppression. Ann Surg. (2013) 257(2):345–51. doi: 10.1097/SLA.0b013e31826d90bb
4. Mendenhall SD, Brown S, Ben-Amotz O, Neumeister MW, Levin LS. Building a hand and upper extremity transplantation program: lessons learned from the first 20 years of vascularized composite allotransplantation. Hand (N Y). (2020) 15(2):224–33. doi: 10.1177/1558944718790579
5. Shores JT. Recipient screening and selection: who is the right candidate for hand transplantation. Hand Clin. (2011) 27:539–43. doi: 10.1016/j.hcl.2011.07.009
6. Shores JT, Brandacher G, Lee WPA. Hand and upper extremity transplantation: an update of outcomes in the worldwide experience. Plast Reconstr Surg. (2015) 135(2):351e–60e. doi: 10.1097/PRS.0000000000000892
7. Kinsley SE, Song S, Petruzzo P, Sardu C, Losina E, Talbot SG. Psychosocial predictors of upper extremity transplantation outcomes: a review of the international registry 1998–2016. Plast Reconstr Surg Glob Open. (2020) 8(9):e3133. doi: 10.1097/GOX.0000000000003133
8. Kumnig M, Jarvholm S. Vascularized composite allotransplantation: emerging psychosocial issues in hand, face, and uterine transplant. Curr Opin Organ Transplant. (2022) 27(6):501–7. doi: 10.1097/MOT.0000000000001028
9. Kumnig M, Jowsey SG, DiMartini AF. Psychological aspects of hand transplantation. Curr Opin Organ Transplant. (2014) 19(2):188–95. doi: 10.1097/MOT.0000000000000047
10. Kumnig M, Jowsey SG, Moreno E, Brandacher G, Azari K, Rumpold G. An overview of psychosocial assessment procedures in reconstructive hand transplantation. Transpl Int. (2014) 27(5):417–27. doi: 10.1111/tri.12220
11. Kumnig M, Jowsey SG, Rumpold G, Weissenbacher A, Hautz T, Engelhardt TO, et al. The psychological assessment of candidates for reconstructive hand transplantation. Transpl Int. (2012) 25(5):573–85. doi: 10.1111/j.1432-2277.2012.01463.x
12. Kumnig M, Jowsey-Gregoire SG. Key psychosocial challenges in vascularized composite allotransplantation. World J Transplant. (2016) 6(1):91–102. doi: 10.5500/wjt.v6.i1.91
13. Kinsley SE, Song S, Losina E, Talbot SG. Psychosocial risk stratification in upper extremity transplantation candidates. Hand (N Y). (2023):15589447231184895. doi: 10.1177/15589447231184895
14. Kubiak CA, Etra JW, Brandacher G, Kemp SWP, Kung TA, Lee WPA. Prosthetic rehabilitation and vascularized composite allotransplantation following upper limb loss. Plast Reconstr Surg. (2019) 143(6):1688–701. doi: 10.1097/PRS.0000000000005638
15. Bueno E, Benjamin MJ, Sisk G, Sampson CE, Carty M, Pribaz JJ, et al. Rehabilitation following hand transplantation. Hand (N Y). (2014) 9(1):9–15. doi: 10.1007/s11552-013-9568-8
16. Vanterpool KB, Gacki-Smith J, Downey MC, Nordstrom M, Luken M, Riggleman T, et al. Patient preferences of patient selection criteria for upper extremity vascularized composite allotransplantation: a qualitative study. SAGE Open Med. (2023) 11:20503121231181236. doi: 10.1177/20503121231181236
17. Vanterpool KB, Gacki-Smith J, Kuramitsu B, Downey M, Nordstrom MJ, Luken M, et al. A patient-centered website (within reach) to foster informed decision-making about upper extremity vascularized composite allotransplantation: development and usability study. JMIR Form Res. (2023) 7:e44144. doi: 10.2196/44144
18. Griffin JM, Kennedy CC, Boehmer KR, Hargraves IG, Amer H, Jowsey-Gregoire SG. Using team science in vascularized composite allotransplantation to improve team and patient outcomes. Front Psychol. (2022) 13:935507. doi: 10.3389/fpsyg.2022.935507
19. Ruebner RL, Reese PP, Denburg MR, Abt PL, Furth SL. End-stage kidney disease after pediatric nonrenal solid organ transplantation. Pediatrics. (2013) 132(5):e1319–26. doi: 10.1542/peds.2013-0904
20. Kozlowski SW, Ilgen DR. Enhancing the effectiveness of work groups and teams. Psychol Sci Public Interest. (2006) 7(3):77–124. doi: 10.1111/j.1529-1006.2006.00030.x
21. Lee SS, Jabloner A. Institutional culture is the key to team science. Nat Biotechnol. (2017) 35(12):1212–4. doi: 10.1038/nbt.4026
22. Stokols D, Misra S, Moser RP, Hall KL, Taylor BK. The ecology of team science: understanding contextual influences on transdisciplinary collaboration. Am J Prev Med. (2008) 35(2 Suppl):S96–115. doi: 10.1016/j.amepre.2008.05.003
23. Dumont M, Sann L, Gazarian A. Bilateral hand transplantation: supporting the patient’s choice. J Plast Reconstr Aesthet Surg. (2017) 70(2):147–51. doi: 10.1016/j.bjps.2016.11.010
24. Siminoff LA, Alolod GP, Davis EE, McGregor HR, Litsas DC, Sarwer DB, et al. Evaluation of an eLearning system to train health professionals to communicate about vascularized composite allotransplantation with donor families. Prog Transplant. (2022) 32(3):233–40. doi: 10.1177/15269248221107040
25. Parker A, Chaya BF, Rodriguez-Colon R, Hao Y, Kurian K, Trilles J, et al. Recipient selection criteria for facial transplantation: a systematic review. Ann Plast Surg. (2022) 89(1):105–12. doi: 10.1097/SAP.0000000000003255
26. Laspro M, Onuh OC, Carrion K, Brydges HT, Tran DL, Chaya BF, et al. Vascularized composite allotransplantation of the hand: a systematic review of eligibility criteria. Ann Plast Surg. (2023) 91(6):771–8. doi: 10.1097/SAP.0000000000003659
27. Olbrisch ME, Levenson JL, Hamer R. The PACT: a rating scale for the study of clinical decision-making in psychosocial screening of organ transplant candidates. Clin Transplant. (1989) 3:164–92.
28. Maldonado JR, Dubois HC, David EE, Sher Y, Lolak S, Dyal J, et al. The stanford integrated psychosocial assessment for transplantation (SIPAT): a new tool for the psychosocial evaluation of pre-transplant candidates. Psychosomatics. (2012) 53(2):123–32. doi: 10.1016/j.psym.2011.12.012
29. Smith PJ, Cendales LC. Psychosocial dimensions of hand transplantation: lessons learned from solid organ transplantation. Curr Opin Organ Transplant. (2019) 24(6):705–13. doi: 10.1097/MOT.0000000000000712
30. Hummel NR, Zuo KJ, Talbot S, Zimmerman ZE, Katz JN, Kinsley SE, et al. Psychosocial predictors in upper-extremity vascularized composite allotransplantation: a qualitative study of multidimensional experiences including patients, healthcare professionals, and close relatives. Front Psychol. (2023) 14:1092725. doi: 10.3389/fpsyg.2023.1092725
31. Kimberly LL, Onuh OC, Thys E, Rodriguez ED. Social support criteria in vascularized composite allotransplantation versus solid organ transplantation: should the same ethical considerations apply? Front Psychol. (2022) 13:1055503. doi: 10.3389/fpsyg.2022.1055503
32. Jowsey-Gregoire SG, Kumnig M, Morelon E, Moreno E, Petruzzo P, Seulin C. The chauvet 2014 meeting report: psychiatric and psychosocial evaluation and outcomes of upper extremity grafted patients. Transplantation. (2016) 100(7):1453–9. doi: 10.1097/TP.0000000000001013
33. Kinsley SE, Lenhard NK, Lape EC, Shah SB, Edwards RR, Katz JN, et al. Perceived success in upper-extremity vascularized composite allotransplantation: a qualitative study. J Hand Surg Am. (2021) 46(8):711.e1–e35. doi: 10.1016/j.jhsa.2021.01.001
Keywords: vascularized composite allotransplantation, bioethical issues, program development, upper extremity transplantation, patient selection, rehabilitation, multidisciplinary collaboration, qualitative research
Citation: Kumnig M, Kobler C, Zaccardelli A, Brandacher G and Talbot SG (2024) Advancing vascularized composite allotransplantation: essential factors for upper extremity transplant program development. Front. Transplant. 3:1406626. doi: 10.3389/frtra.2024.1406626
Received: 25 March 2024; Accepted: 27 May 2024;
Published: 11 June 2024.
Edited by:
Rolf Barth, The University of Chicago, United StatesReviewed by:
Ali-Farid Safi, Craniologicum – Center for Craniomaxillofacial Surgery, SwitzerlandBruce Gelb, New York University, United States
© 2024 Kumnig, Kobler, Zaccardelli, Brandacher and Talbot. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Martin Kumnig, bWFydGluLmt1bW5pZ0BpLW1lZC5hYy5hdA==
 Martin Kumnig
Martin Kumnig Caroline Kobler
Caroline Kobler Alessandra Zaccardelli
Alessandra Zaccardelli Gerald Brandacher3,4
Gerald Brandacher3,4 Simon G. Talbot
Simon G. Talbot