- 1Institute of Health Policy Studies and Department of Surgery, University of California, San Francisco, San Francisco, CA, United States
- 2San Francisco Veterans Affairs Health Care System, San Francisco, CA, United States
- 3Department of Medicine, University of California, San Francisco, San Francisco, CA, United States
- 4Department of Medicine, University of Nevada, Reno, Reno, NV, United States
- 5Department of Neurology, University of California, San Francisco, San Francisco, CA, United States
- 6Department of Anesthesia, University of California, San Francisco, San Francisco, CA, United States
Veteran access to sleep medicine is of paramount importance to the Veterans Health Administration (VA). To increase access, VA has created community referral policies and programs, as well as telehealth programs. In 2017, the Office of Rural Health (ORH) funded a TeleSleep initiative focused on reaching rural Veterans with unmet sleep needs. ORH provided 3–6 years of funding to help 19 hubs support 98 spoke sites serving rural Veterans. As ORH funding concluded, each hub identified its path to sustainment. This case study follows one TeleSleep hub in VA's western geographic region as it transitioned from ORH funding sustainment as a regional Sleep Clinical Resource Hub. This case study describes the real-world process of adaptation in care delivery strategies. One key area of adaptation revolved around whether to deliver care via the patient's home facility or the provider's home facility. In early 2021, the TeleSleep team implemented an innovative provider transfer model, where temporary reinforcements from the TeleSleep hub increased the workforce capacity of spoke sites, similar to the concept of locum tenens. In this provider transfer model, TeleSleep clinicians scheduled, documented, and billed for each encounter at the Veteran's home facility. Positioning TeleSleep clinicians as local providers facilitated communication and referrals and promoted continuity and quality of care for Veterans in their home facility. This provider transfer model reduced the administrative burden of providers and schedulers and supported patient-side-only documentation of care. While this mirrors current locum tenens practice, transferring providers did not fit VA's financial model as implemented by the western region's Sleep Clinical Resource Hub. Therefore, in December 2021, VA aligned TeleSleep with VA's preferred practice of patient rather than provider transfers. In the patient transfer model, providers schedule and document in both the provider and patient electronic health records, and bill in the provider's facility. However, reflecting on this period of innovation, TeleSleep team members concluded that the provider transfer model could improve patient safety and care coordination while reducing the administrative burden of frontline clinicians. Further research and development are needed to align the provider transfer model with VA's financial model.
1 Introduction: description of the nature of the problem being addressed and rationale for the proposed innovation
Veterans suffer disturbed sleep due to conditions ranging from sleep apnea to post-traumatic stress disorder. In response to increasing Veteran demand for comprehensive sleep services, the Veterans Health Administration (VA) seeks to grow capacity by expanding facility-based services and telehealth infrastructure (Kaul et al., 2021; Sarmiento et al., 2019).
For telehealth delivery of sleep care, VA initially targeted rural regions, which are more likely to be designated as medically underserved. VA's Office of Rural Health (ORH) invested in a successful delivery model, the TeleSleep Enterprise-Wide Initiative, beginning in March 2017. This initiative provided initial funding for hub (usually urban medical centers) and spoke (rural or highly rural) sites to collaborate on virtual delivery of sleep care (Chun et al., 2023). In the ORH initiative, 19 rural-serving facilities with 98 spoke sites volunteered to be early adopters of TeleSleep, and the implementation was successful in reaching Veterans and increasing access to sleep care (Sarmiento et al., 2019).
In April 2020, the Sierra Pacific Veteran Integrated Service Network (VISN 21), consisting of seven VA healthcare systems with 50 spoke sites in the western region of the United States, concluded that virtual sleep medicine could benefit non-rural as well as rural Veterans. VISN 21 provided financial support for a San Francisco-based TeleSleep hub with the goal of providing services regionally. This implementation case study provides a detailed account of how TeleSleep adapted as it evolved from ORH funding to VISN 21 sustainment.
2 Context (setting and population) in which the innovation occurs
The setting for this case study was VISN 21, described by VA as follows: “The Network serves Veterans in northern and central California, Nevada, Hawaii, the Philippines and U.S. Territories in the Pacific Basin. VISN 21 provides a continuum of comprehensive health care services through seven VA Medical Centers, nine co-located Community Living Centers, and 41 Community-Based Outpatient Clinics (CBOCs).” (Veterans Health Administration, 2021).
VISN 21 serves over 400,000 Veterans, many of whom suffer from disordered sleep. In 2019, sleep medicine doctors in VISN 21 tested or treated 24,000 Veterans, mostly through in-person care pathways. The prevalence of diagnosed sleep-related breathing disorders among Veterans treated at the VA was 22% in 2018, with an actual estimated prevalence exceeding 60% when including undiagnosed Veterans (Folmer et al., 2020). Thus, we estimate the VISN's total addressable population for sleep medicine as in the range of 88,000 (22% of 400,000) to 240,000 Veterans (60% of 400,000).
3 Case study time frame
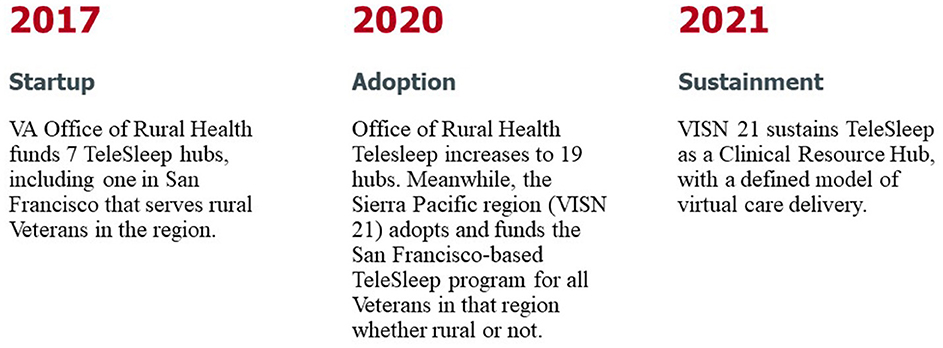
This case study reports on the initial TeleSleep ORH program launched in March 2017 and follows it through the third year of sustainment as a VISN 21 Sleep Clinical Resource Hub in September 2023 (Figure 1).
4 Detail to understand key programmatic elements
4.1 Program planning framework
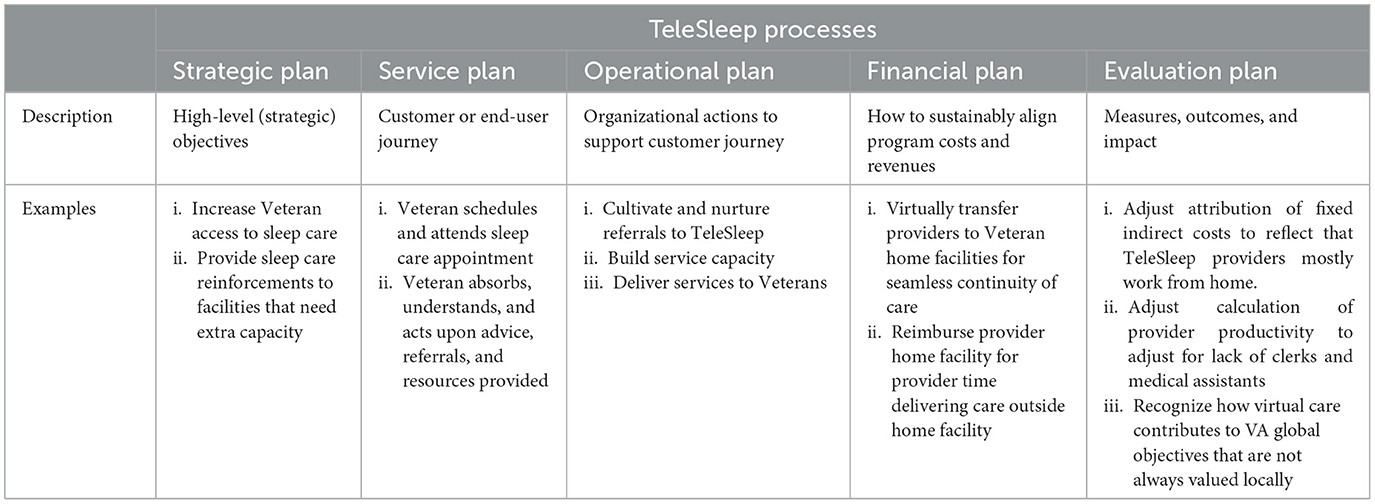
As we adapted TeleSleep, we relied on a five-step program planning framework (Collins, 1994; Rossi et al., 1999). This framework describes a program's internal processes (Belkora et al., 2023; Belkora, 2015). Following this framework, we continually refined TeleSleep's strategic; service; operational; financial; and evaluation plans (Table 1).
4.2 Strategic plan
In 2020, upon being adopted by the VISN 21 region, the San Francisco-based TeleSleep hub drafted a strategic plan. We first articulated a problem statement: “Sleep disorders and poor sleep quality affect the quality of life of millions of Veterans and contribute to serious illness, disability and even death.” In the face of these problems, we stated the TeleSleep vision: “Save lives and reduce suffering by creating a world in which Veterans sleep all night, every night.” Toward this vision, we asserted the TeleSleep purpose: “Deliver sleep care to Veterans wherever and whenever they need it—in a way that is financially sustainable for VA.” TeleSleep mobilized around a mission statement: “Reduce disparities in access to sleep care among Veterans.” We summarized our initial approach: “Provide sleep care reinforcements to facilities that need extra capacity.” Our tagline: “Better Sleep, Better Health.” Measurable goals and objectives for TeleSleep included: increase VISN 21′s capacity to provide sleep care to its Veterans; stabilize the workforce within VISN 21; provide gap coverage for providers on extended leave or upon staff turnover; improve care coordination for Veterans; reduce avoidable referrals to outsourced community care; and reduce overall costs of community care (Kaul et al., 2021; Donovan et al., 2019; Weaver et al., 2020).
In June 2021, VA faced the global safety recall of positive airway pressure devices used by more than 700,000 Veterans. This required TeleSleep leaders to adapt and address an additional set of sleep care needs for impacted Veterans (Belkora et al., 2023). The recall spurred innovation in delivering TeleSleep care with the goal of getting patients scheduled and seen as quickly as possible to support treatment decisions involving affected devices. To accomplish this goal, VA opened recall clinics each facility and assigned TeleSleep clinicians to staff these clinics. These providers scheduled, documented, and billed at the patient's home facility. Another strategic adaptation occurred in December 2021, when VISN 21 completed the integration of the TeleSleep program into VISN 21′s Clinical Resource Hub (CRH) model of virtual care delivery (Rubenstein et al., 2023; Gujral et al., 2024; Burnett et al., 2023).
4.3 Service plan
We characterized the baseline (in-person) sleep medicine service plan in a Veteran-centered narrative, illustrated by quotes from earlier qualitative research (Nicosia et al., 2021) (Table 2). This is consistent with the VA's strategic initiative to describe services in terms of Veteran life journey maps (US Department of Veterans Affairs, 2022).
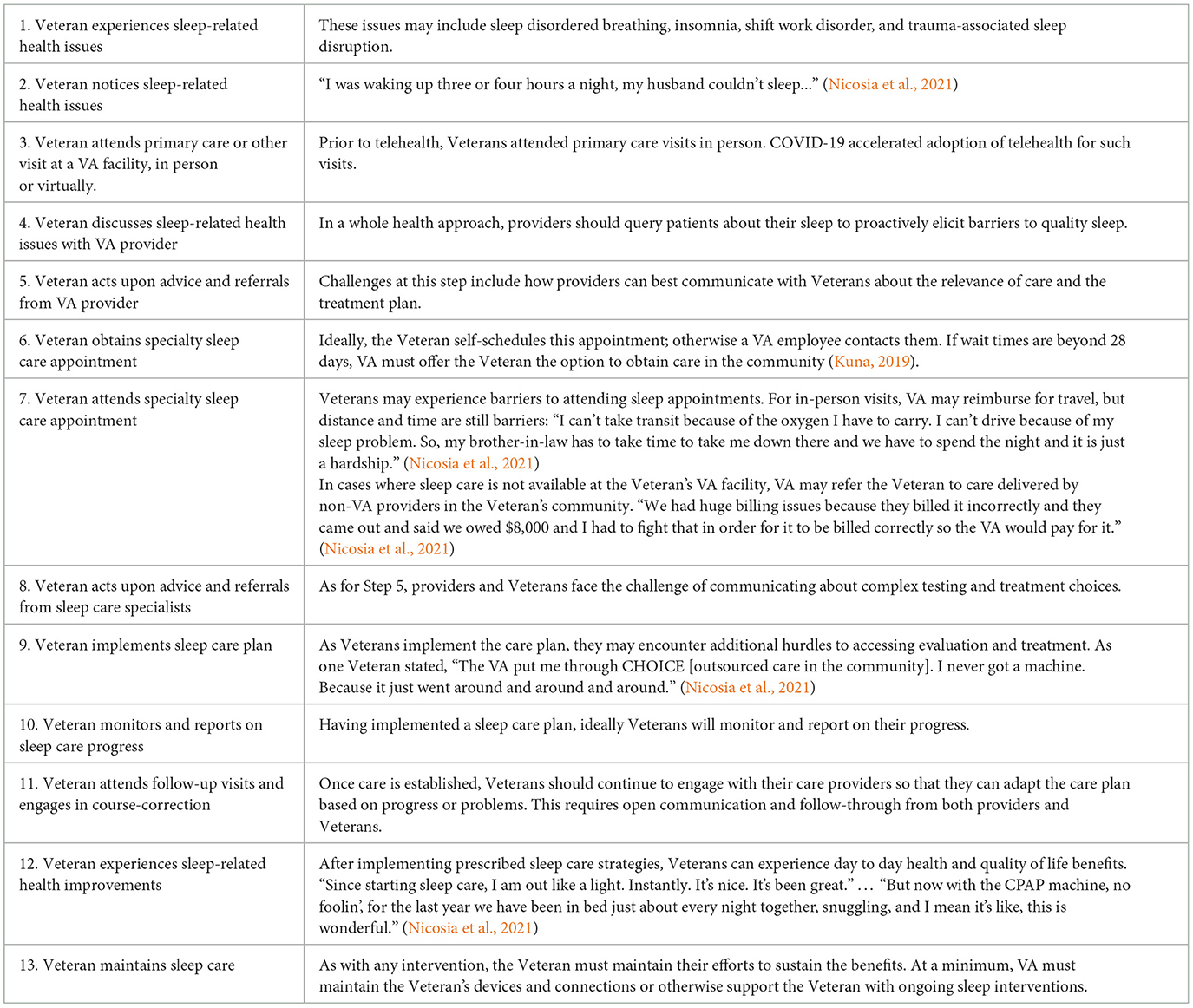
Table 2. Veteran journey through diagnosis and treatment for sleep disturbances—steps and description.
The initial ORH TeleSleep program aimed to improve the journey for rural Veterans by tapping into the telehealth capacity of sleep providers at various VA facilities. Specifically, TeleSleep introduced an optional virtual referral to specialist sleep care at steps 5 and 7 in the Veteran's journey (Table 2). In step 7, sleep technologists, respiratory therapists, or telehealth clinical technologists taught Veterans to use specialized sleep recorders at their domicile. TeleSleep physicians and nurse practitioners then interpreted the test results and prescribed therapies as needed.
For steps 8–10 of the Veteran journey, TeleSleep referred Veterans to various services such as surgery, dental, behavioral sleep medicine, and weight management programs, or prescriptions for prosthetic devices or medications. Where possible, TeleSleep delivered care via telehealth.
From the Veteran's perspective, the TeleSleep journey remained similar for the implementations in 2017 by Office of Rural Health and in 2020 by the Sierra Pacific Region (VISN 21). Veterans could always decline TeleSleep in favor of in-person care. For some Veterans, the journey became more complicated in June 2021 with the global safety recall of positive airway pressure devices. For those Veterans, we described changes to the Veteran journey in a published case study (Belkora et al., 2023).
4.4 Operational plan
The San Francisco-based TeleSleep hub articulated the following operational plan for its VISN 21 implementation in 2020.
4.4.1 Scan the environment and define the plan
TeleSleep leaders identified stakeholders; took an inventory of readily available sleep resources at every facility within VISN 21; evaluated cost and volume of services referred to “community care” outside of VA; and defined project roles, responsibilities, and an organizational chart. Weekly meetings with facility sleep leads provided insight into the needs of each facility at the local level and established communications to begin standardization and dissemination of information.
4.4.2 Coordinate personnel
TeleSleep coordinated its personnel through synchronous (e.g., chat, online meetings) and asynchronous communication (e.g., email). Through these mechanisms, TeleSleep onboarded and trained personnel in its procedures. Occasional in-person meetings also helped strengthen relationships and collaboration among team members.
TeleSleep also designed and implemented a provider coverage schedule across multiple clinic time zones (Pacific, Hawaii, Mountain, Samoa, Chamorro Time Zones), and allowed employees to live throughout these time zones as well as in Central and Eastern time. This geographic expansion increased the pool of qualified providers and facilitated recruitment. Being virtual, providers could also more easily cover for each other during absences.
4.4.3 Cultivate and nurture referrals to TeleSleep
TeleSleep signed formal referral agreements with VISN 21 facilities. These agreements included Service Level Agreements and Telehealth Service Agreements, which cover credentialing and privileging, scopes of services, and guidance on referral and discharge criteria and how to request coverage by the VISN 21 TeleSleep team. TeleSleep leadership presented an overview of services to multiple stakeholder audiences including facility-based sleep staff, VISN 21 community of practice, and Community Care staff (who could offer virtual care by VISN 21′s TeleSleep team as an alternative to community care). TeleSleep programmed a VA informatics application (known as Light Electronic Access Framework) as a portal to solicit, receive, route, and track requests for telehealth services.
4.4.4 Build service capacity
In order to provide comprehensive virtual sleep care across VISN 21, TeleSleep established several realms including behavioral, dental, medical, and surgical sleep subspecialty services. Within these services, TeleSleep hired clinical and administrative personnel. The clinical personnel included physicians, nurses, respiratory therapists, medical instrument technicians, dentist, and dental assistant. Administrative personnel initially included a program manager, business manager, and advanced medical support assistants. VISN 21 subsequently reassigned these administrative personnel outside of TeleSleep in 2021. Hiring and onboarding took longer than expected due to the following issues. First, both TeleSleep leadership and VISN 21 human resources personnel faced capacity constraints. Second, for VA's central human resources function, bringing new personnel into a VISN based structure was novel, and VA had to develop and gain experience with new procedures for doing so. Third, the VISN 21 Clinical Resource Hub could provide only very limited administrative support to TeleSleep during 2020–21.
Despite its virtual nature, the program still had to arrange dedicated space to house and teach health professions trainees, and to store, distribute and process sleep equipment. Trainees included sleep medicine fellows and internal medicine and neurology residents, who collectively further increased TeleSleep capacity. Clinical equipment included home sleep apnea testing (HSAT) and positive airway pressure (PAP) devices used in testing and treating sleep disordered breathing.
Delivering care began with building of clinic schedules for surgical, medical, and sleep testing appointments. Each facility in VA has its own instance of the electronic health record system; there are 170 instances in total and 8 instances in VISN 21. Prior to TeleSleep, these instances had no standardized interfaces (e.g., menus) or care pathways for sleep medicine. TeleSleep also had to configure systems for scheduling patients in remote facilities; for conducting telephone or video visits; for viewing and editing patient medical records; for viewing raw data or interpreting results from diagnostic or therapeutic interventions; and for prescribing treatments and ordering prosthetic or other devices.
4.4.5 Deliver services to Veterans
In order to identify referrals, a TeleSleep consult manager queried a centralized consult tracker fed by each facility's health record system for electronic consults placed by referring providers. In following up on each referral, TeleSleep providers conducted comprehensive reviews of VA, Department of Defense, and non-VA community records in order to triage patients to the next step of care with appropriate context. They communicated the results of this triage to TeleSleep schedulers, with instructions regarding which scheduling grid was appropriate. These grids reflect the practitioner type (e.g., physician, nurse practitioner, respiratory therapist, etc.), availability of open appointments, modality of how the visit would occur (e.g., video chat vs. telephone), and reminder communication method (e.g., Short Messaging Service text, postcard, letter).
Schedulers booked TeleSleep appointments following two different scenarios, corresponding to the two major epochs in the program's evolution. Between March 2017 and December 2021, TeleSleep pioneered a new service delivery model. Before TeleSleep, when patients sought care remotely in person, the patient traveled to the remote facility, registered as new patients at that facility, and experienced care as if that facility were their home facility. When developing TeleSleep as an ORH program, program leaders introduced a patient-centered variation. For some participating sites, the ORH instead arranged to bring the remote providers into the Veteran's home facility as if that facility were the provider's home facility. For those sites, between March 2017 and December 2021, schedulers entered one appointment in the health record system of the Veteran's home facility. After 2021, when TeleSleep was fully integrated into VA's Clinical Resource Hub model, TeleSleep reverted to the Clinical Resource Hub practice of transferring Veterans to the provider home facility. Therefore, after 2021, schedulers needed to enter two mirrored appointments: one in the Veteran's home facility and one in the provider's home facility.
Once scheduled, TeleSleep providers delivered services to Veterans online, by telephone, by video chat, and by mail. For example, TeleSleep mailed sleep testing devices to Veterans; educated the Veterans by phone or video chat about sleep apnea and trained them on how to complete the test at their domicile; downloaded, scored, and processed returned devices; interpreted data to establish a diagnosis; notified patients of test results and the care plan; entered orders or consults for follow up care consistent with the care plan established or service agreement with the spoke facility. If the Veteran required a Positive Airway Pressure device, the TeleSleep provider prescribed it; ordered the device and supplies from a centralized warehouse; and educated the Veteran on use of the device and remotely monitored treatment to follow.
When documenting encounters and coding them for billing purposes, TeleSleep providers followed two different scenarios, corresponding once again to two different epochs in the program's evolution. Between March 2017 and December 2021, the provider created a single progress note in the electronic health record system of the Veteran's home facility. In addition to documenting the encounter, the remote sleep provider could add a return to clinic order. This alerted local schedulers to schedule a follow up appointment with the referring provider in order to assure continuity of care. The remote sleep provider also used the electronic health record at the Veteran's home facility to refer the Veteran to any required local services such as sleep testing. The remote provider documented all this in the electronic health record of the Veteran's home facility in order to maximize local visibility into the entire remote episode of care. Prior to December 2021, this Veteran-side documentation also included billing information for the episode of care.
After 2021, providers entered a progress note in the provider's home facility system that included billing information. To maintain full visibility in the Veteran's home facility system, the provider additionally documented in the Veteran's home facility record a full note with detailed clinical information as well as referrals and return to clinic orders. This Veteran-side documentation did not include billing information.
4.4.6 Return veterans to facilities
When a Veteran completed an episode of testing and treatment, TeleSleep providers returned the Veteran to the referring providers in the Veteran's home facility. TeleSleep providers accomplished this by discussing a follow up care plan with the Veteran; writing a transition-of-care note that they asked a provider from the Veteran's home facility to additionally sign; and placing a “return to clinic” request for local facility schedulers to schedule the Veteran with the referring provider for follow-up care. That follow-up care often leveraged VA employees at the Veteran's home facility who were able to implement the care prescribed by the TeleSleep specialty care providers. Such employees extending the sleep care included sleep technologists, respiratory therapists, and registered nurses. These facility-based employees were able to support patients through sleep testing, treatment (e.g., Positive Airway Pressure devices), care coordination, and education.
4.5 Financial plan
While innovating in telehealth, TeleSleep had to navigate financial structures within VA designed for in-person, facility-based care. One constraint was that facilities pay salaries from budget allocations generated by provider workload, and VA providers can only be paid by a single facility, i.e., the provider's home facility. Meanwhile, VA assigns each Veteran to a home facility where Veterans ideally obtain as much of their care as possible to assure continuity and quality of care.
In conventional VA care delivery programs, when providers at a Veteran's home facility cannot deliver the care required by a Veteran, they can transfer the patient to a facility where care is available. This is known as an interfacility patient transfer. Veterans can also seek care in community settings, but for this report we are focusing on how VA can best provide care inside the system.
One challenge with interfacility patient transfers is that they result in episodes of care away from the Veteran's home facility. Veterans register as new patients in the remote facility, where providers document, bill, and refer Veterans onward in the same way they treat Veterans for whom this is the home facility. Once the remote episode of care is complete, Veterans usually resume care for other conditions in their original home facility. Providers in the Veteran home facility can in theory look up the remote episodes of care by either (1) navigating to the consults section of the medical record, locating the interfacility consult, and expanding it to reveal associated documentation; or (2) launching another online portal to review medical records and using search terms for domains of care of interest (e.g., “sleep”, “echocardiography”, “pulmonary function test”). In practice only primary care providers, who order most interfacility care, consistently look up remote episodes, which under current conditions is very time consuming. Often the specialty care providers in the Veteran's home facility resume care without awareness of the care provided in remote facilities. This can result in problems with continuity, safety, and quality of care.
From March 2017 to December 2021, to address these challenges, TeleSleep implemented interfacility provider (rather than patient) transfers. TeleSleep providers joined the Veteran's home facility as if they were locum tenens, or visiting providers, and documented care inside the Veteran's usual and ongoing electronic health record. During the period March 2017 to April 2020, the ORH reimbursed the provider facilities for work done at Veteran home facilities. For TeleSleep's implementation in VISN 21, starting in April 2020, TeleSleep providers were not eligible for this funding from the ORH. Instead, TeleSleep proposed that VISN 21 facilities receiving TeleSleep care transfer funds to purchase this care from the provider's facility. However, VISN 21 never implemented the funds transfer model. Rather, VISN 21 required TeleSleep to align itself with the Clinical Resource Hub model. This model uses interfacility patient transfers and all billing is done at the provider facility. In order to address the quality, documentation, and coordination of care concerns resulting from interfacility patient transfers, the Clinical Resource Hub implemented double documentation. Providers billed and documented episodes of care in the electronic health record system of the provider's home facility; and then re-documented in the electronic health record system of the patient's home facility.
4.6 Evaluation plan
VA generally evaluates its care delivery using measures of volume of care delivered (outputs); labor and other costs of care delivered (inputs); and quality (outcomes). When accounting for costs, VA attributes fixed and variable costs to production units such as sleep programs using methodologies developed for physical facilities.
However, virtual programs such as TeleSleep may incur very different fixed and variable costs than facility-based sleep programs. VA has not yet adjusted its attribution of fixed and variable costs to reflect the differences. For example, VA currently attributes high fixed indirect costs to virtual programs such as TeleSleep, even though TeleSleep employees actually bear many of these costs themselves (e.g., home office, internet, and electricity).
Likewise, when measuring volume of care delivered, VA uses methodologies developed for delivery of in-person care at provider home facilities (which may not be the Veteran's home facility, as described above). In physical facilities, VA focuses on the length and number of visits as measures of production for providers. It's worth noting that, in physical facilities, staff are available to streamline patient visits, which increases provider productivity. For example, in physical facilities, clerks and medical assistants take vital signs, room patients, administer questionnaires, and complete mandatory health screenings. Furthermore, in person visits, rooming time is not included in the calculation of how long the visit lasts. Providers see a queue of Veterans in the order that they are roomed, and the visit time starts when the provider enters an exam room where a Veteran is waiting.
Conversely, virtual providers often conduct online visits without staff assistance. Providers often wait while Veterans navigate unfamiliar technology to enter the online appointment. This extra time corresponds to the in-person “rooming time” normally undertaken by medical assistants. In contrast to in person visits, here the Veteran's “rooming time” prolongs the appointment and VA evaluates this as reduced provider productivity. Providers also have to use visit time to administer questionnaires and screens and perform other tasks that are conducted by staff when visits are in person. Then providers still have to take history and guide patients in medical decision making. As a result, due to tasks being shifted from staff to providers, virtual providers take longer and see fewer patients.
VA's current view of virtual visits therefore is that they have similar costs to in-person visits (due to VA attributing similar fixed costs); while virtual providers complete a lower volume (due to providers waiting for Veterans to room themselves and providers using visit time to perform staff functions such as administering questionnaires and screens). Therefore, VA often perceives virtual care as costing more per unit of care delivered.
5 Discussion
As we trace the evolution of TeleSleep through this case study, we see variation in our five program dimensions: strategic plan, service plan, operational plan, financial plan, and evaluation plan. We can locate the variation on a spectrum ranging from VA's standard model of in-person, facility-based care to what we believe will be VA's future model of virtual provider transfers. We summarize the variation we observed in Table 3 and elaborate below.
5.1 Strategic plan
Each column of Table 3 represents a different strategy for assuring VA can provide care to all Veterans. Figure 2 presents a graphical illustration of key elements in Table 3.
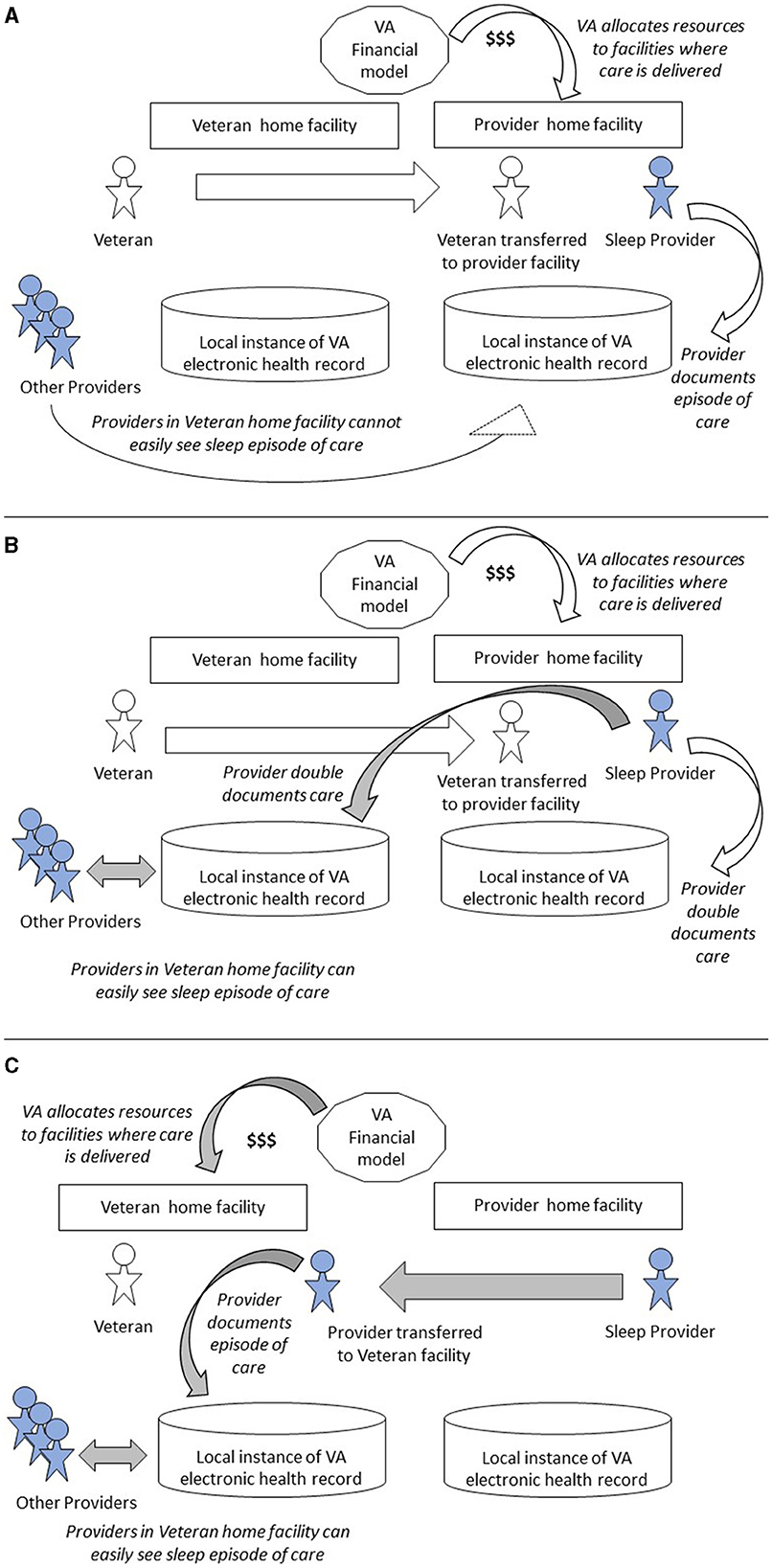
Figure 2. Variation in program processes when transferring patients vs. providers. (A) Patient transfer for in-person or Telehealth care. (B) Patient transfer to virtual Clinical Resource Hub. (C) Provider transfer to Veteran's home facility. Shaded arrows denote process changes, shaded people denote providers.
5.1.1 In-person care with option for interfacility patient transfer
Column 1 of Table 3 represents in-person care by sleep medicine providers. This is the traditional, legacy model of care in VA. If a Veteran's home facility lacks capacity to deliver timely access to care for the Veteran, the facility can transfer the patient to another facility for in-person care there. Figure 2A depicts this patient transfer scenario. VA pays to reimburse the Veteran for travel costs.
5.1.2 Interfacility patient transfer for virtual care from facility-based provider
Column 2 represents the situation where facility-based providers occasionally deliver care via telehealth rather than in person, in order to help another facility meet overflowing Veteran needs. Figure 2A also captures this scenario, except that the care is delivered via telehealth rather than in person.
5.1.3 Patient transfer to virtual Clinical Resource Hub
Column 3 represents a recent VA innovation, where a region creates a virtual Clinical Resource Hub. A Veteran's home facility can transfer the Veteran to this Clinical Resource Hub for care from a virtual team organized to deliver comprehensive sleep medicine as a regionally shared service. Figure 2B depicts this patient transfer scenario, in which providers document in the electronic health record systems of both provider and Veteran home facilities.
5.1.4 Virtual provider transfer to Veteran's home facility
Column 4 represents a proposed future state where VA deploys locum tenens providers as a shared service and transfers providers, not patients, between facilities. The locum tenens providers attend to Veterans in the Veteran home facility via telehealth. Figure 2C depicts this provider transfer scenario.
5.2 Service plan
While each column of Table 3 represents a distinct strategy, the recent virtual care strategies all share a common service plan.
5.2.1 Column 1, in person care with option for interfacility patient transfer
In this model, if the Veteran's home facility cannot provide timely access to sleep care for the Veteran, the Veteran must travel to a community site, or to another VA facility to obtain care. This is the legacy model that pre-dates telehealth.
5.2.2 Columns 2–4, representing variations in care delivered virtually
In all variations of virtual care at VA, Veterans can make use of VA's robust telehealth infrastructure. This includes the possibility of using telehealth technology from the Veteran's home facility if the Veteran needs assistance, or logging in from their domicile if the Veteran has internet access and the requisite technology skills.
5.3 Operational plan
Each care strategy in Table 3 has a corresponding operational plan.
5.3.1 Column 1, in person care with option for interfacility patient transfer
From an operational point of view, VA's legacy model faces challenges related to capacity planning. More Veterans require sleep care each year, but planners cannot predict exactly how many Veterans will seek such care from a facility in any given year. Planners must also contend with shortages in the supply of specialized labor; and competition to recruit and retain sleep medicine providers. The uncertainty and fluctuations in demand, combined with overall labor shortages, mean that facilities cannot always meet the regulatory standard for providing their Veterans with timely access to sleep care. The legacy VA model is to send the patient traveling in person to a community care site, or to another VA site with the capability to provide timely care. Transferring the patient to another facility allows VA as a system to in-source or out-source the provision of overflow care on an ad-hoc, unplanned basis.
5.3.2 Column 2, interfacility patient transfer for virtual care from facility-based provider
With the advent of telehealth at VA, if a provider at the other facility is able to provide virtual care, they will do so. Virtual care avoids the costs and inconvenience of Veteran travel. However, whether providing care in person (above) or virtually, the remote provider documents in the provider's home system. This means that these remote episodes of care are not easily visible to providers in the electronic health record of the Veteran's home facility. This results in a potential loss of safety, quality, and continuity of care.
5.3.3 Column 3, patient transfer to virtual Clinical Resource Hub
A virtual Clinical Resource Hub represents VA's planned/anticipated response to in-sourcing of overflow care. Ideally, the Clinical Resource Hub assembles a multidisciplinary team of providers who can deliver care wherever it is needed in the region. Providers in Clinical Resource Hubs deliver and document care in their home facilities, not the Veteran's home facility. However, they also document in the Veteran's home facility so that their episodes of care are easily visible to other providers in that facility. This double documentation is costly and wasteful in terms of provider time and morale, which also affect VA's challenges with retention and recruitment.
5.3.4 Column 4, virtual provider transfer to Veteran's home facility
Transferring providers to the Veteran's home facility could be implemented as part of a VA movement toward a nationally distributed workforce. One advantage of this model is that providers deliver and document care only in the Veteran's home facility, and this episode of care is easily visible to other providers in the Veteran's home facility.
5.4 Financial plan
The first three strategies in Table 3 share a common financial plan, while the last requires financial innovation at VA.
5.4.1 Columns 1–3, representing patient transfer models
When VA transfers Veterans internally, whether for in person or telehealth care, the provider accounts for the episode of care inside the provider's home facility, which is where VA deems the Veteran to be receiving care because the Veteran registers at that site to be seen by that provider. By the rules of VA's internal resource allocation system, known as the Veterans Equitable Resource Allocation or VERA, VA funnels resources to VISNs. VISNs in turn apply an allocation model to distribute funds to facilities in proportion to the population they serve and the care they have provided recently. Since VA rules also state that providers can only be paid by one facility, this system ensures that resources flow to where they are needed to pay providers. Note that VA designed and implemented VERA in an era of in-person care, i.e., before the advent of telehealth.
A consequence of this model, which is predicated on a capitated payment system, is that facilities that cannot deliver sleep medicine will cede budget to other facilities when referring Veterans to those facilities. This further erodes the capacity of the referring facilities. Yet VA also wants to maintain the capacity of facilities closest to the Veteran so that Veterans can obtain care near their domiciles. The dynamics of the current system will inexorably lead to concentration of resources at the largest urban facilities.
5.4.2 Column 4, virtual provider transfer to Veteran's home facility
In our proposed future-state model, transferring the provider rather than the patient would allow the provider to deliver, document, and bill for care in the Veteran's home facility. Under existing VA accounting rules, the Veteran's home facility would get credit for such episodes of care. One implementation of this model could involve modifying VA rules so that providers could be paid by multiple facilities. All the facilities where a provider delivered care would contribute a pro-rata share of the provider wages. Alternatively, VA could allow the home facility to invoice other facilities for services delivered virtually by their providers. Regardless of the tactical details, the desired outcome would be to concentrate resources according to the location of the Veteran receiving care rather than the location of the provider delivering care.
5.5 Evaluation plan
We propose that VA should adapt its evaluation of care efficiency and effectiveness, as its current methods distort the actual costs of virtual care.
VA financial models arose before the advent of telehealth and allocate costs as if all care is delivered in person at physical facilities. As a result, VA still attributes high indirect costs to sleep care delivered virtually, even though purely virtual providers working at home pay for their own office space, internet and electricity. In addition, virtual care may be associated with cost savings to VA as a system, for example because of avoided community care costs or avoided travel costs for Veterans. By adjusting its calculations, VA might discover that virtual care incurs a lower unit cost than in-person care.
As for quality of care, VA may need to more explicitly value and recognize how virtual care contributes to VA strategic objectives including: increasing care coordination and quality for Veterans who stay in VA; reaching rural and highly rural Veterans who may be living in care deserts; retaining Veterans and providers in VA longitudinally; and avoiding costs of community care. Taking into account these considerations, virtual programs may be reducing overall cost and adding currently underrecognized value to VA as a system.
5.6 Limitations
As an implementation case study, our account relies on details relating to a specific context: a region in the Veterans Health Administration. The insights from our case study may not generalize to other health delivery systems. While we provided many implementation details related to telehealth delivery of sleep medicine, the scope of our report did not include how remote providers prescribe medications, including controlled substances often used in sleep medicine. Another issue that we deemed out of scope for this report was VA's implementation of a new electronic health record system. This system, when eventually implemented, may alleviate some of the concerns we raised about the visibility of remote episodes of care to providers in the Veteran's home facility. Meanwhile, the scope of our report included a detailed account of our proposal to transfer providers rather than patients. We recognize that this model has not been fully tested, and should ideally be piloted before broader implementation. One empirical question is how funding hub provider time at remote or spoke patient facilities would affect activities outside of patient care, such as training and research. Funds accruing to spoke facilities should increase their capacity for delivering care under VA's financial model, but in so doing would divert funds from the hub facilities where providers are based. A question arises as to whether this would erode the development of centers of excellence in hub facilities.
6 Conclusion
This organizational case study follows TeleSleep through multiple adaptations as a VA region adopted, implemented, and sustained the program. The latest implementation of TeleSleep has increased Veteran access to sleep care. In order to further improve quality of care, we recommend that VA transfer providers, not patients, between facilities so that providers can deliver virtual care as if they were in the patient's home facility. Transferring providers may require VA to adapt its financial management practices so that a provider's home facility gets reimbursed for any provider time spent delivering care to patients at another facility. VA could even consider creating a single administrative entity acting as a national hub for all TeleSleep services. Such a national TeleSleep hub, which does not currently exist, would support more agile care delivery across the enterprise; maximize sharing of resources; facilitate implementation of standardization in sleep care nationally; and advance the country's vision for “One VA.”
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
JB: Conceptualization, Investigation, Methodology, Writing – original draft, Writing – review & editing, Data curation, Formal analysis, Validation. JR: Conceptualization, Project administration, Writing – review & editing. KW: Conceptualization, Data curation, Project administration, Writing – review & editing. MW: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Validation, Writing – review & editing. TR: Conceptualization, Investigation, Project administration, Writing – review & editing. SS: Conceptualization, Investigation, Project administration, Writing – review & editing. PC: Conceptualization, Investigation, Writing – review & editing. ES: Conceptualization, Investigation, Writing – review & editing. AM: Conceptualization, Investigation, Writing – review & editing. AG: Conceptualization, Investigation, Writing – review & editing. PK: Conceptualization, Investigation, Writing – review & editing. LA: Conceptualization, Investigation, Writing – review & editing. JT: Conceptualization, Investigation, Writing – review & editing. KS: Conceptualization, Project administration, Writing – review & editing, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Resources, Supervision, Validation, Writing – original draft.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The San Francisco Measurement Science Quality Enhancement Research Initiative (project number 1I50HX003266-01) and the VA Office of Rural Health TeleSleep Enterprise-Wide Initiative (PROG-0000018) contributed funding for this case study evaluation.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer SK declared a shared affiliation with the authors to the handling editor at the time of review.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Belkora, J. (2015). DEAL! Discovery, Engagement, and Leverage for Professionals. San Francisco, CA: Guidesmith, 238.
Belkora, J. K., Fields, B., Shamim-Uzzaman, Q. A., Stratford, D., Alfandre, D., Hollingshaus, S., et al. (2023). Veterans Health Administration response to 2021 recall of Philips Respironics devices: a case study. Front. Sleep 2:1129415. doi: 10.3389/frsle.2023.1129415
Burnett, K., Stockdale, S. E., Yoon, J., Ragan, A., Rogers, M., Rubenstein, L. V., et al. (2023). The clinical resource hub initiative: first-year implementation of the Veterans Health Administration regional telehealth contingency staffing program. J. Ambul. Care Manage. 46, 228–239. doi: 10.1097/JAC.0000000000000468
Chun, V. S., Whooley, M. A., Williams, K., Zhang, N., Zeidler, M. R., Atwood, C. W., et al. (2023). Veterans Health Administration TeleSleep Enterprise-Wide Initiative 2017-2020: bringing sleep care to our nation's veterans. J. Clin. Sleep Med. 19, 913–923 doi: 10.5664/jcsm.10488
Donovan, L. M., Coggeshall, S. S., Spece, L. J., Griffith, M. F., Palen, B. N., Parsons, E. C., et al. (2019). Use of in-laboratory sleep studies in the Veterans Health Administration and community care. Am. J. Respir. Crit. Care Med. 200, 779–782. doi: 10.1164/rccm.201902-0313LE
Folmer, R. L., Smith, C. J., Boudreau, E. A., Hickok, A. W., Totten, A. M., Kaul, B., et al. (2020). Prevalence and management of sleep disorders in the Veterans Health Administration. Sleep Med. Rev. 54:101358. doi: 10.1016/j.smrv.2020.101358
Gujral, K., Scott, J. Y., Dismuke-Greer, C. E., Jiang, H., Wong, E., Yoon, J., et al. (2024). The clinical resource hub telehealth program and use of primary care, emergency, and inpatient care during the COVID-19 pandemic. J. Gen. Intern. Med. 39, 118–126. doi: 10.1007/s11606-023-08476-x
Kaul, B., Hynes, D. M., Hickok, A., Smith, C., Niederhausen, M., Totten, A. M., et al. (2021). Does community outsourcing improve timeliness of care for veterans with obstructive sleep apnea? Med. Care 59, 111–117. doi: 10.1097/MLR.0000000000001472
Kuna, S. T. (2019). The Mission Act: challenges to sleep medicine and other specialties in the veterans health administration. Am. J. Respir. Crit. Care Med. 200, 663–664. doi: 10.1164/rccm.201906-1278ED
Nicosia, F. M., Kaul, B., Totten, A. M., Silvestrini, M. C., Williams, K., Whooley, M. A., et al. (2021). Leveraging Telehealth to improve access to care: a qualitative evaluation of Veterans' experience with the VA TeleSleep program. BMC Health Serv. Res. 21, 1–9. doi: 10.1186/s12913-021-06080-5
Rossi, P. H., Freeman, H. E., and Lipsey, M. W. (1999). Evaluation - A Systematic Approach. 6th Edn. Thousand Oaks, CA: SAGE Publications.
Rubenstein, L. V., Curtis, I., Wheat, C. L., Grembowski, D. E., Stockdale, S. E., Kaboli, P. J., et al. (2023). Learning from national implementation of the Veterans Affairs Clinical Resource Hub (CRH) program for improving access to care: protocol for a six year evaluation. BMC Health Serv. Res. 23:790. doi: 10.1186/s12913-023-09799-5
Sarmiento, K. F., Folmer, R. L., Stepnowsky, C. J., Whooley, M. A., Boudreau, E. A., Kuna, S. T., et al. (2019). National expansion of sleep telemedicine for veterans: The TeleSleep Program. J. Clin. Sleep Med. 15, 1355–1364. doi: 10.5664/jcsm.7934
US Department of Veterans Affairs (2022). Department of Veterans Affairs FY 2022-2028 Strategic Plan. Available at: https://department.va.gov/wp-content/uploads/2022/09/va-strategic-plan-2022-2028.pdf (accessed August 31, 2024).
Veterans Health Administration (2021). About the VA Sierra Pacific Network (VISN 21). Available at: https://www.visn21.va.gov/about/index.asp (accessed July 5, 2021).
Keywords: sleep medicine, telehealth, implementation, adaptation, sustainment, program process theory, program planning, organizational case study
Citation: Belkora JK, Reichert J, Williams K, Whooley MA, Rezayat T, Sorensen S, Chilakamarri P, Sanders E, Maas A, Gomez A, Kurien P, Ashbrook L, Thomas J and Sarmiento KF (2024) Implementing TeleSleep at Veterans Healthcare Administration: an organizational case study of adaptation and sustainment. Front. Sleep 3:1444689. doi: 10.3389/frsle.2024.1444689
Received: 06 June 2024; Accepted: 26 August 2024;
Published: 11 September 2024.
Edited by:
Stuart F. Quan, Harvard Medical School, United StatesReviewed by:
Richard Berry, University of Florida, United StatesSamuel Kuna, Corporal Michael J. Crescenz VA Medical Center, United States Department of Veterans Affairs, United States
Copyright © 2024 Belkora, Reichert, Williams, Whooley, Rezayat, Sorensen, Chilakamarri, Sanders, Maas, Gomez, Kurien, Ashbrook, Thomas and Sarmiento. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kathleen F. Sarmiento, a2F0aGxlZW4uc2FybWllbnRvQHZhLmdvdg==
 Jeffrey K. Belkora
Jeffrey K. Belkora Jill Reichert
Jill Reichert Katherine Williams
Katherine Williams Mary A. Whooley
Mary A. Whooley Talayeh Rezayat2,4
Talayeh Rezayat2,4 Stacy Sorensen
Stacy Sorensen Elizabeth Sanders
Elizabeth Sanders Philip Kurien
Philip Kurien Kathleen F. Sarmiento
Kathleen F. Sarmiento