
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Reprod. Health , 15 December 2023
Sec. Adolescent Reproductive Health and Well-being
Volume 5 - 2023 | https://doi.org/10.3389/frph.2023.1244540
 Wondu Belayneh1
Wondu Belayneh1 Zerai Kassaye2
Zerai Kassaye2 Temesgen Arusi3*
Temesgen Arusi3* Netsanet Abera4
Netsanet Abera4 Admassu Hantalo5
Admassu Hantalo5 Biruk Melkamu6
Biruk Melkamu6 Muluken Gutulo7
Muluken Gutulo7
Background: Dysmenorrhea is pain during menstrual flow and is the most common gynecologic complaint in reproductive-age girls. The severity of dysmenorrhea ranges from mild to severe pain during menstruation, which affects their academic activities.
Objective: To assess the prevalence and associated risk factors of dysmenorrhea and its effects on academic activities among Hawassa University students from April 1–30/2021.
Methods: A cross-sectional study was conducted and a systematic random sampling technique was used to select 348 study participants. Standardized self-administered questionnaires were used to obtain relevant data. The severity of pain was assessed using a verbal multidimensional scoring system and Numerical Pain Rating Scale (NPRS) methods. The collected data was entered into Epi info version 7 and exported to SPSS version 21 for analysis and then descriptive statistics and logistic regression analysis were performed.
Results: The prevalence of dysmenorrhea was 80% (277). Of those affected by dysmenorrhea, using the verbal multidimensional scoring system, 47.6% (132) were found to have mild pain, 39.7% (110) had moderate pain, and 12.6% (35) had severe pain. However, using the Numeric Pain Rating Scale (NPRS), 21.7% (60) were found to have mild pain, 33.2% (92) had moderate pain, 37.5% (104) had severe pain, and 7.6% (21) had very severe pain. It was found to have a negative effect on academic activity, such as loss of concentration in class (p = 0.00), disruption of study time (p = 0.00), sleep disturbances (p = 0.00), issues in personal relationships (p = 0.00), and absenteeism (p = 0.00). Associated factors included being sexually active, having a family history of dysmenorrhea, and the presence of depression.
Conclusion: Dysmenorrhea is prevalent in this study and has a significant impact on academic activities. Family history of dysmenorrhea, being sexually active, and the presence of depression are associated factors.
Dysmenorrhea is lower abdominal pain during menstrual flow. It can be classified as primary or secondary dysmenorrhea based on the pathology. Primary dysmenorrhea is pain during menstrual flow without an identified cause. Secondary dysmenorrhea is pain during menstrual flow with an identified cause. The pain starts during the first 24–36 h of menstruation and lasts 2–3 days post menses. Primary dysmenorrhea is usually encountered during the earlier years of menstrual flow. The pathophysiology of pain is associated with increased prostaglandin production (PGF2α and PGE2) and abnormal uterine sensitivity to prostaglandins, which is a widely accepted theory. Increased production of prostaglandin in the face of increased sensitivity of uterine muscle to prostaglandin results in myometrium contractility, which exposes the uterus to hypoxia and ischemia in the uterus, which ultimately results in pain (1–6).
Since the reporting of pain is influenced by different sociocultural factors, the prevalence has wide variation across the globe. According to recent systemic reviews and meta-analysis, the pooled prevalence of primary dysmenorrhea ranges between 60% and 73% (7–10). However, other published reports indicate that the prevalence ranges from 16.8% to 95% (1, 2, 11–13). The Ethiopian prevalence is 64.7%−85.4% (14–16). The severity of dysmenorrhea varies across different reproductive age groups and countries. This disparity is possible because dysmenorrhea varies according to the age of women included in the study samples (17).
There are multiple factors associated with dysmenorrhea. Factors like age, alcohol use, family history, low BMI, the extent of menstrual flow, anxiety, chronic pelvic pain, and duration of flow are associated with dysmenorrhea (7, 8, 10, 18–22).
Dysmenorrhea has a significant impact on quality of life, academic performance, and personal relationships. This impact depends on the extent of the pain experienced. The effects on academic performance were found to mainly include study time, concentration, participation in group activities, examination performance, and class attendance. Social withdrawal, poor personal activities, sleep disturbances, and limited daily activities are also among the effects (1, 14, 15, 21, 23).
In Ethiopia, despite the negative sociocultural belief in women's empowerment programs, there has been significant progress in their participation in organizational and political leadership, the economy, and enrollment in higher education since the adoption of their empowerment plan in the past two decades. Women have participated in a significant number of Ethiopian political and economic activities in recent years. For example, women made up 50% of the Ethiopian cabinet in 2021, the country's president is a woman, and 35.7% of university students are female. Thus, equal involvement in social, intellectual, cultural, political, and economic concerns will be difficult to attain if there are obstacles that negatively affect young women's academic performance in universities (23–25).
Considering the valueless role of women in the country, these young female university students are of productive age and will become leaders of society and represent hope for the country and the community. Any problem that affects this age group will have a tremendous economic and psychological burden on the community and country. Furthermore, there is limited evidence on the prevalence, associated factors, and effects of dysmenorrhea on academic activities among female university students; thus, this study aims to identify these factors.
An institution-based cross-sectional study was conducted at Hawassa University College of Medicine and Health Sciences (HUCMHS) from April 1–30/2021. All randomly selected undergraduate female students at the HUCMHS Campus were the study population.
The single population proportion formula was used to determine the sample size required to conduct this study from the prevalence of dysmenorrhea occurrence among female students at Mekelle University College of Medicine and Health Science 71.8% (15), at 95% certainty and 5% margin of error to achieve a total sample size of 348 female students after adding 10% of the non-response rate. Out of 720 female students currently studying at CMHS Campus, 348 students were selected by systematic random sampling technique. The departments were listed alphabetically from the Department of Anesthesia to Radiotechnology; then, female students in each department were listed. After obtaining the female student list from the college registrar, it was arranged alphabetically, from anesthesia to radiotechnology; this final list of students was used as the sampling frame. After choosing the first student randomly, it was decided to take every other student with a K-value of 2. If there was any absence from class or dropping out, the next student was taken as a sample. Before distributing the questionnaire, any students who were found to be amenorrhoeic, pregnant, within six months post-partum, or currently lactating after being asked were excluded from the study, and the next student was then selected.
The data collection tool used in the study was adapted from the literature review and was prepared in English but translated to the local language (Amharic) by two professionals and then again translated back into English by two professionals. Before the questionnaire came into effect, it had been checked for inconsistency. The data collection tools had three parts: sociodemographic characteristics, menstruation characteristics, severity, and the impact of dysmenorrhea on academic activities. The study participants were screened for depression using patient health question nine (PHQ-9) depression screening tools (26, 27). The pain score was made with a numeric pain rating (NPR) and verbal multidimensional pain score system (VMPS) (28). The data collection instrument was pretested on 20 students who were not included in the final analysis, and relevant modifications were instituted before the commencement of actual data collection. Parallelly, data collectors were trained for three days before starting the collecting process. The data was collected by those three trained collectors [trained year two and year three residents (medical doctors on obstetrics and gynecology specialty study)] through a standardized self-administered questionnaire after explaining the questions to those who were unable to understand. The training was given to data collectors by supervisors, including the principal investigator, regarding confidentiality and freedom of the participants to terminate filling out the questionnaire. Supervisors contacted data collectors on a daily basis in case of any problems or difficulties. The completeness of the data was checked by the principal investigator.
Responses for PHQ-9 were summarized based on the mean section total score (by assigning 1 for yes response and 0 for no, or 0–3 for PHQ-9). It was then reported as no depression (0–4), mild depression (5–9), moderate depression (10–14), moderately severe depression (15–19), and severe depression (20–27). Moreover, the presence of anxiety was analyzed using the GAD-7 scale and summarized based on the mean total score (seven questions with a 0–3 rating, and no (0–4), mild (5–9), moderate (10–14), and severe anxiety (15–21)). The severity of pain was assessed using two methods. The first was the NPRS segmented numeric version of the visual analog scale (VAS), where the respondents scored their pain from 0 to 10. The second was the VMPS method, grading the pain severity with analgesia, having systemic symptoms, and affecting daily activities: painful menses requiring analgesics but seldom inhibiting activity (grade I, mild pain); daily activity affected, requiring analgesics, which give sufficient relief (grade II, moderate pain); and daily activity inhibited by dysmenorrhea, with insufficient relief from painkillers (grade III, severe pain). The collected data were checked, cleaned, and entered into Epi data version 7 and exported to SPSS version 21 for further data cleaning and analysis. The information is described in tables, graphs, means, and frequency, including the effect of dysmenorrhea on daily academic activities. The presence of an association between independent and outcome variables was checked by the Pearson chi-square test. Additionally, each independent variable was fitted separately into bivariate logistic analysis to evaluate the degree of association with the outcome variable. Thus, multivariate logistic regression analysis was done on variables with p-values less than 0.05. The significance level was obtained at an odds ratio of 95% CI and p-value < 0.05.
Ethical clearance for written informed consent was obtained from the Institutional Review Board (IRB) of the College of Medicine and Health Sciences, Hawassa University, Ethiopia, with clearance letter no. RPGe/76/2021. The IRB gave ethical clearance. After attaining approval from the institutional review board of Hawassa University, informed consent was taken from the study participants after informing them of the aim of the study. They were informed that confidentiality would be maintained and that they could leave the study at any time if they felt that way inclined. All methods were performed according to the relevant guidelines and regulations.
In total, 99.4% of the respondents were involved in the study. The ages of respondents ranged from 18 to 36 years, with a median of 21 years. The majority, 89.6% (N = 310), came from urban areas, whereas 10.4% (N = 36) were from rural areas (Table 1).
Out of the total 346 respondents, 31 (9%) had a past medical illness, 17 (4.9%) had a past surgical illness, 8 (2.3%) had past abdominopelvic surgery, 16 (4.6%) had a past pelvic infection, and 9 (2.6%) had an ovarian cyst. The history of contraceptive use was reported in 49 (14.2%) participants and pregnancy was reported in 18 (5.2%) participants. The age range for menarche was reported between 9 and 18 years. More than three-quarters of the respondents (77.4%) reported menarche between 12 and 14 years. A large proportion of the study participants reported regular menses (78.3%) (Table 1).
Out of a total of 346 respondents, 135 (39%) had a variable frequency of sporting activity, 2 (0.6%) smoked cigarettes, 131 (37.9%) had a variable frequency of alcohol consumption, and 66 (19.1%) were sexually active (Table 2).
Among the students, in general, the most common symptoms associated with menses were back pain (67%); dizziness, weakness, fatigue (65.3%); bloating (55.5%); breast pain (52.9%); and irritability and mood swings (59.8%) (Supplementary Table S1).
Of all students, 72% reported anxiety and 73% had positive screening for depression. Moreover, 74% of students who reported anxiety (Figure 1) and 76% of those with positive screening for depression (Figure 2) had complained of dysmenorrhea.
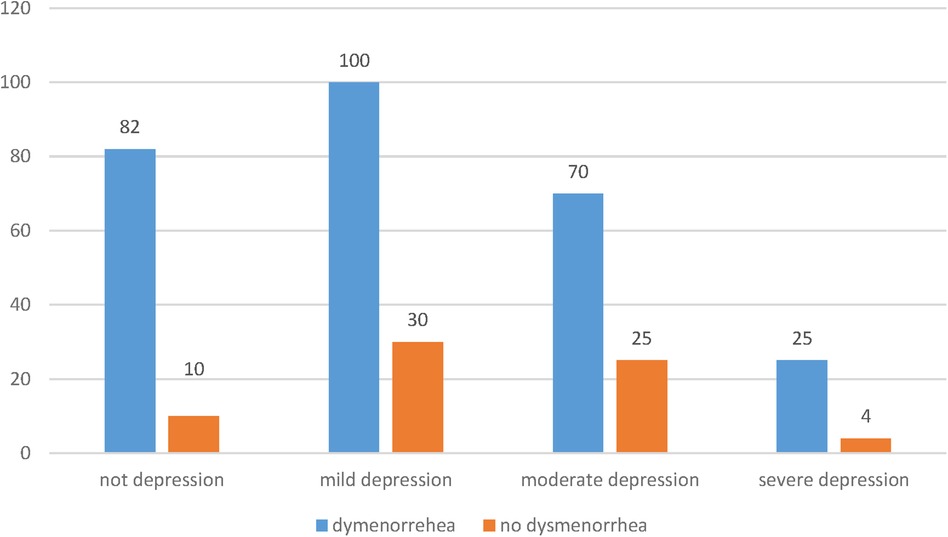
Figure 2. Result of positive screening of depression (PHQ-9) assessment of students in HU, CMHS in 2021.
The prevalence of dysmenorrhea was found to be 80.1% (Table 3). Using the Numeric Pain Rating Scale, out of 277 students with dysmenorrhea, 21.7% (60), 33.2% (92), 37.5% (104), and 7.6% (21) of the respondents reported mild, moderate, severe, and very severe intensity of pain, respectively. According to the verbal multidimensional scoring system, out of 277 students, 47.6% (132) of students' menstruation was painful but seldom inhibited normal activity, seldom requiring analgesics (mild pain). In total, 39.7% (110) of students' daily activity was affected; analgesics were required and gave sufficient relief so that absence from school was unusual (moderate pain). In 12.6% (35) of students, daily activity was inhibited by dysmenorrhea, with analgesics giving insufficient pain relief (severe pain).
Among the students with dysmenorrhea, the most common symptoms associated were back pain (71.8%); dizziness, weakness, and fatigue (75.1%); bloating (62.8%); and breast pain (58.1%). Of the respondents with dysmenorrhea, 83% (194) reported that the disorder interfered with their academic performance; of these, 48% were mildly affected, 25.6% were moderately affected, and 9% were severely affected. Dysmenorrhea interfered with the concentration of 86.6% (N = 240) of participants; of these, 46.2% were mildly affected, 26.7% were moderately affected, and 13.7% were severely affected (Table 4).
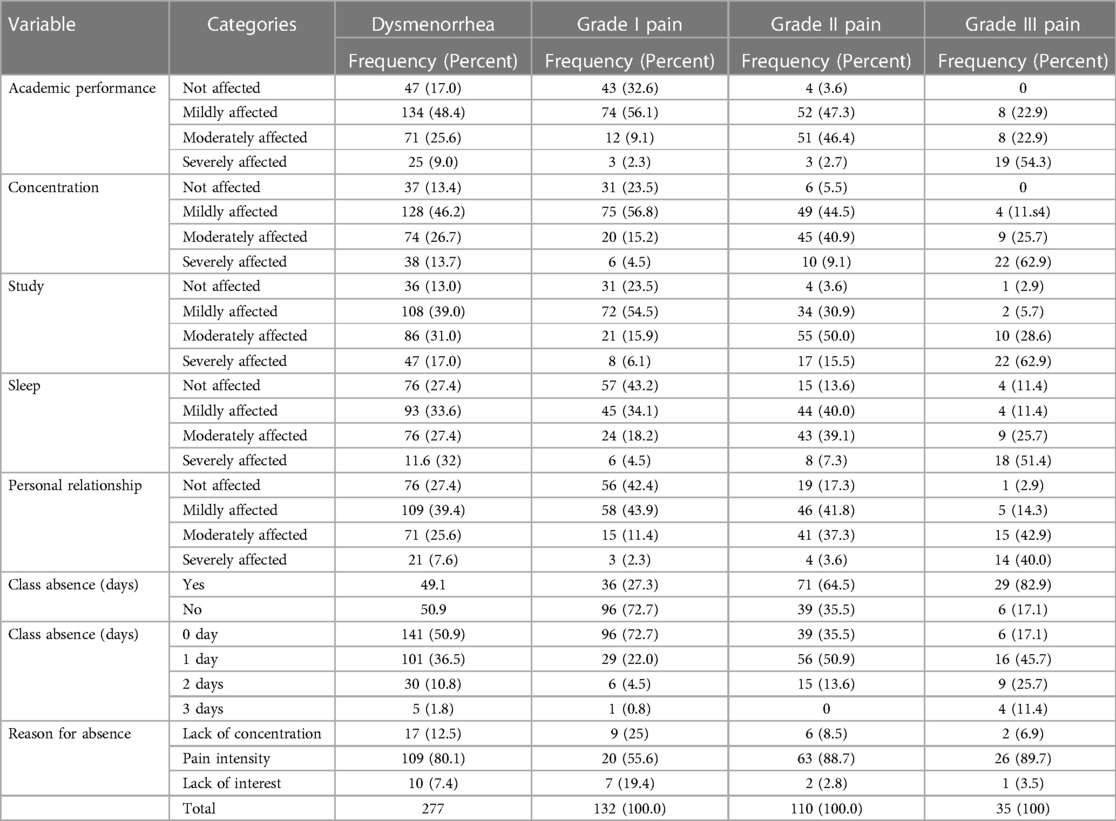
Table 4. Effects of dysmenorrhea on academic activities among dysmenorrhea and based on the grade of pain severity, at HU, COMHS, 2021.
The potential impact of dysmenorrhea on academic activities was sought through chi-square analysis, and it was found to have a negative impact on academic performance (p = 0.00), concentration (p = 0.00), study time (p = 0.00), relationships (p = 0.00), and sleeping time (p = 0.00) (Table 5). Furthermore, in bivariate logistic analysis, the following factors were identified as significantly associated with dysmenorrhea: marital status, use of contraception, pregnancy, sexual activity, maternal dysmenorrhea, sister with a history of dysmenorrhea, and clot in menses. However, multivariate logistic regression analysis identified the following factors as being significantly associated with dysmenorrhea: being sexually active, maternal history of dysmenorrhea, sister with a history of dysmenorrhea, and presence of depression.
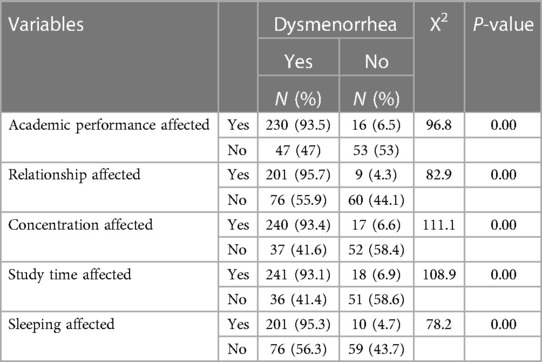
Table 5. The association of academic performance with dysmenorrhea using Chi-square, students at HU, COMHS 2021.
Being sexually active was the determinant factor of dysmenorrhea. Sexually active female students were more than three times more likely to develop dysmenorrhea compared to those who were not sexually active [AOR = 3.260 (1.00–10.647)]. Family history is a strong risk factor for dysmenorrhea: for those with a mother and sister with dysmenorrhea, the risk was AOR = 8.481 (95% CI, 3.608–19.934) and AOR = 4.012 (95% CI, 1.929–8.346) times higher than those without a family history of dysmenorrhea, respectively. Students who had a history of positive screening for depression had a 5.7 times higher risk compared to those who had no history of depression (AOR = 5.683, (95% CI, 1.762–18.329) (Table 6; Supplementary Table S2).
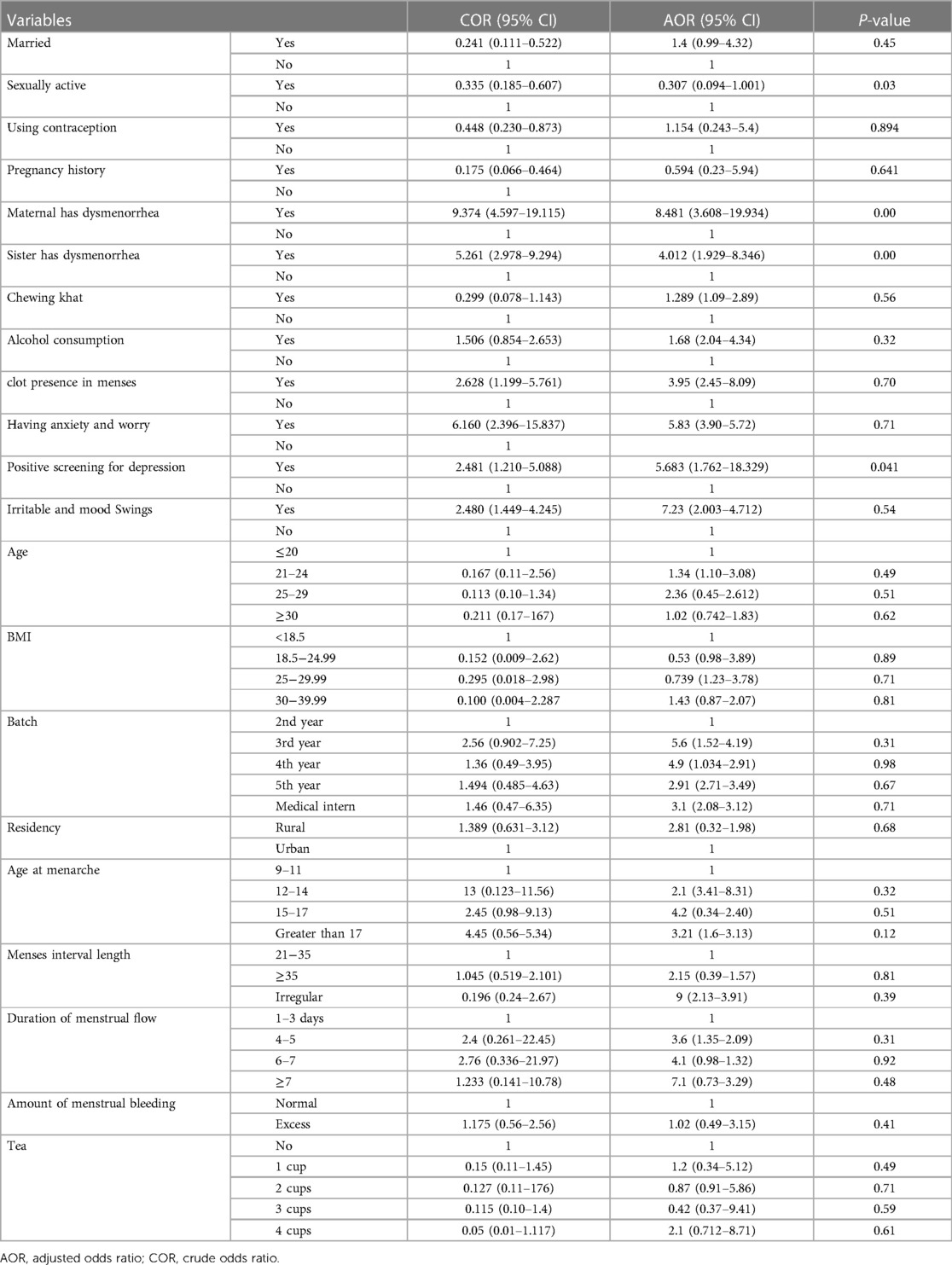
Table 6. Shows the results of the multivariate analysis using significant bivariate variables, of students at HU, COMHS 2021.
This study shows a prevalence of dysmenorrhea of 80.1%, which is comparable to studies done in northern Ethiopia, Nigeria, and Morocco (2, 12, 16) and other systemic reviews and meta-analysis (7–10), whereas the prevalence found in this study is higher than those of the study done in eastern Ethiopia, 69.3% (29); Mekelle University, 71.8% (15); and Kenya, 68.1% (23). The prevalence found in this study is lower than that found in Kuwait University (30), Lithuania Vilnius University (19), and Turkey (1). The variation is due to the assessment tool, method of data collection, sociocultural, ethnic, and lifestyle factors among females, as well as the absence of a universally accepted definition. Moreover, menstruation is considered a private issue in many cultures, so its associated complaints might be kept silent by most females. Above all, pain tolerance and reporting have been influenced by the cultural, religious, and traditional practices from one geographical area to the other. There are different coping mechanisms for pain across cultures and geography. Furthermore, the study population was comprised of university students who were away from their families, so there was no one to take care of them during painful menses, which made the threshold for pain low in this study population (30).
In this study, the prevalence of dysmenorrhea was found to be 80.1% (277) using the Numeric Pain Rating Scale; of those affected by dysmenorrhea, 21.7% (60), 33.2% (92), 37.5% (104), and 7.6% (26) reported mild, moderate, severe, and very severe pain intensity, respectively. This is similar to the findings of one study where 47.4% of unmarried women reported severe and very severe pain (31). According to the verbal multidimensional scoring system, 132 (38.1%) students had grade I mild pain, and 110 (32.1%) females had grade II moderate pain. Additionally, in 10.1% (35) of students, daily activity was inhibited by dysmenorrhea, and the effect of analgesics on the pain was insignificant (grade III, severe pain). This matches the findings of a study in Ethiopia and an Indian study where 55.26% of unmarried women were found to use pain relief on the second day of their menses) (16, 31). It is slightly higher than the systemic reviews done in 2022, wherein 31.1%, 25.7%, and 8.3% of girls were found to have mild, moderate, and severe pain, respectively (10). So, irrespective of the pain scoring methods, almost half of the female students suffered severe pain during menstruation, which shows how profound and complicated the problem is.
Of the respondents with dysmenorrhea, 83% reported that the disorder interfered with their academic performance, which was in line with the findings in northern Ethiopia and slightly lower than the study in Debre Brehan (15, 16) but higher than findings in Ghana and Turkey (1, 22). This may be due to socio-cultural differences, differences in pain tolerance between the populations, and methodological differences. Additionally, this might be due to the questionnaire design used to identify the effect on academic activities: ours included options (not affected, mildly affected, moderately affected, and severely affected), whereas the previously mentioned Turkey and Ghana studies used Yes/No options, whereby the students with mild negative effects might have chosen No in the Yes/No options.
In our study, 38% of all women reported interfering with their regular daily activities. Our finding was higher than studies done in Dutch which is one of the largest studies done so far to look into the impact of dysmenorrhea. The discrepancy may be due to the difference in the source population that is a community study (12). It interfered with the concentration of 86.6% of students, which was higher than the findings in Debre Brehan, Ghana, and Australia (16, 23, 32). More than two-thirds reported dysmenorrhea had interfered with their relationship (mild in 39.4% and moderate to severe in 33.2%), which was higher than in Debre Brehan, Mekelle, Ghana, and Australia (15, 16, 23, 32). It was lower than in Turkey, where 92% reported personal relationships were negatively affected by dysmenorrhea (1). This might be due to the questionnaire design used to identify effects on academic activities and differences in the study population. Additionally, there are different pain coping mechanisms across the regions and cultures. Therefore, due to dysmenorrhea, personal relationships and concentration are significantly affected.
Almost half of the students with dysmenorrhea, 49.1%, were found to have been absent from class during menses for 1–2 days. The most common reason for class absence was pain intensity, reported at 80.1%. This finding is higher than those of the studies in Mekelle, Ghana, and Australia (15, 23, 32) and lower than those of the studies in Debre Brehan and Gondar (14, 16). This may be due to differences in geography, culture, and pain tolerance. The study population was not similar across the studies: some included women in the community (33) and some included high school students (14), whereas our study used university students.
As indicated in this study, menstrual disturbances like dysmenorrhea and premenstrual syndrome have a significant negative impact on the quality of life of students. It affects the productivity of students through an increased rate of school absenteeism, poor academic performance, and poor social relationships with friends and families. Menstrual flow is controlled by the hypothalamus-pituitary gonadal/adrenal axis (HPG/A). The HPG axis regulates and controls it through different feedback mechanisms so that hormonal changes during menses are in strict hemostasis. It has been reported that different lifestyle factors, such as psychological, emotional, or physical stress, can negatively affect the HPG axis, thereby resulting in menstrual disturbances. Stressful conditions result in elevated levels of cortisol and energy demand, which can disrupt the normal hormonal changes during menses by affecting the HPG axis (9).
Being sexually active was the determinant factor of dysmenorrhea. Sexually active female students were found to be 70% less likely to develop dysmenorrhea than those who were not. This finding is similar to that of multiple studies across the scientific world (14, 15, 17, 24) and may be due to sexually active women being more likely to use contraceptive options, especially hormonal ones, which are protective against dysmenorrhea. Since the pathophysiology of dysmenorrhea is primarily hormonal disturbance around premenstrual time, hormonal contraceptives have a protective effect and are used as a treatment for dysmenorrhea.
Students whose mother and sister had a history of dysmenorrhea were found to be eight and four times more likely to experience dysmenorrhea, respectively, than students whose mother and sister had not experienced dysmenorrhea. Most studies revealed that females who had a positive family history of dysmenorrhea were more likely to develop the condition (14, 15, 22, 21). This study showed the presence of positive screening for depression was significantly associated with dysmenorrhea. Participants who had screened positive for depression had a 5.7 times higher risk of dysmenorrhea than those who had not. Mood disorders were associated with dysmenorrhea as this group has hypersensitivity to pain (17). Having depression was associated with a higher risk of dysmenorrhea (16). Furthermore, the strong effect of being depressed is associated with the risk of menstrual pain, with an odds ratio of 13.3 (33). There is no well-established mechanism for depression to increase the risk of dysmenorrhea; however, there is an overlapping neurohormonal and neurochemical mechanism in the pathophysiology of dysmenorrhea and depression. The progesterone metabolite will bind to the neuro-steroid binding site of the GABA (gamma-aminobutyric acid) receptor, rendering it resistant to activation; it will then decrease centrally GABA-mediated inhibition. Additionally, a lowering of serotonin levels is observed, and the serotonergic functioning pathway is estimated to be deficient in the brain by estimating its activity, so medications that augment serotonin are effective. However, the above mechanisms are associated with premenstrual syndromes, not merely dysmenorrhea (34).
Finally, it is recommended to provide counseling and health education to young female students regarding coping mechanisms for dysmenorrhea and pharmacologic management with nonsteroidal anti-inflammatory drugs and hormonal contraceptives, which are effective interventions (5, 6).
This study aimed to assess the factors and impacts of dysmenorrhea in young females. Moreover, it used two different scoring methods, especially numerical pain scoring, which has not been used widely in the literature.
Other possible causes of secondary dysmenorrhea, like endometriosis, PCOS (polycystic ovarian syndrome), and so on, were not excluded since they require investigation. The cross-sectional study lacks cause and effect association.
The prevalence of dysmenorrhea is relatively high among the female students attending university included in this study. It has a significant negative impact on students' academic performance. This study showed that being sexually active is protective against dysmenorrhea. Maternal history of dysmenorrhea, having a sister with a history of dysmenorrhea, and the presence of depression were significantly associated with dysmenorrhea.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
The studies involving humans were approved by Hawassa University College of health science and medicine ethical review board. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was required from the participants or the participants' legal guardians/next of kin in accordance with the national legislation and institutional requirements. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
WB: proposal development, data collection, data analysis, manuscript preparation, ZK: proposal development, data collection, data analysis, manuscript preparation. NA: proposal development, data collection, data analysis, manuscript preparation. MG: proposal development, data collection, data analysis, manuscript preparation. AH: proposal development, data collection, data analysis, manuscript preparation. BM: proposal development, data collection, data analysis, manuscript preparation. TA: proposal development, data collection, data analysis, manuscript preparation, manuscript finalization. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frph.2023.1244540/full#supplementary-material
1. Bilir E, Yıldız Ş, Yakın K, Ata B. The impact of dysmenorrhea and premenstrual syndrome on academic performance of college students, and their willingness to seek help. Turk J Obstet Gynecol. (2020) 17(3):196. doi: 10.4274/tjod.galenos.2020.97266
2. Lghoul S, Loukid M, Hilali MK. Prevalence and predictors of dysmenorrhea among a population of adole schoolgirls (Morocco). Saudi J Biol Sci. (2020) 27(7):1737–42. doi: 10.1016/j.sjbs.2020.05.022
3. Barcikowska Z, Rajkowska-Labon E, Grzybowska ME, Hansdorfer-Korzon R, Zorena K. Inflammatory markers in dysmenorrhea and therapeutic options. Int J Environ Res Public Health. (2020) 17(4):1191. doi: 10.3390/ijerph17041191
4. Chen CX, Draucker CB, Carpenter JS. What women say about their dysmenorrhea: a qualitative thematic analysis. BMC Womens Health. (2018) 18(1):1–8. doi: 10.1186/s12905-017-0499-3
6. Ferries-Rowe E, Corey E, Archer JS. Primary dysmenorrhea: diagnosis and therapy. Obstet Gynecol. (2020) 136(5):1047–58. doi: 10.1097/AOG.0000000000004096
7. Mitsuhashi R, Sawai A, Kiyohara K, Shiraki H, Nakata Y. Factors associated with the prevalence and severity of menstrual-related symptoms: a systematic review and meta-analysis. Int J Environ Res Public Health. (2022) 20(1):569. doi: 10.3390/ijerph20010569
8. Molla A, Duko B, Girma B, Madoro D, Nigussie J, Belayneh Z, et al. Prevalence of dysmenorrhea and associated factors among students in Ethiopia: a systematic review and meta-analysis. Womens Health. (2022) 18:17455057221079443. doi: 10.1177/17455057221079443
9. Maity S, Wray J, Coffin T, Nath R, Nauhria S, Sah R, et al. Academic and social impact of menstrual disturbances in female medical students: a systematic review and meta-analysis. Front Med (Lausanne). (2022) 9:821908. doi: 10.3389/fmed.2022.821908
10. Wang L, Yan Y, Qiu H, Xu D, Zhu J, Liu J, et al. Prevalence and risk factors of primary dysmenorrhea in students: a meta-analysis. Value Health. (2022) 25(10):1678–84. doi: 10.1016/j.jval.2022.03.023
11. Latthe P, Latthe M, Say L, Gülmezoglu M, Khan KS. WHO systematic review of prevalence sent of chronic pelvic pain: neglected reproductive health morbidity. BMC Public Health. (2006) 6(1):1–7. doi: 10.1186/1471-2458-6-177
12. Schoep ME, Nieboer TE, van der Zanden M, Braat DD, Nap AW. The impact of menstrual symptoms on everyday life: a survey among 42,879 women. Am J Obstet Gynecol. (2019) 220(6):569.e1–.e7. doi: 10.1016/j.ajog.2019.02.048
13. Bello FA, Akinyotu OO, Odubamowo KH. Dysmenorrhea among female students at a teaching hospital in South-Western Nigeria. Trop J Obstet Gynaecol. (2017) 34(2):129–33. doi: 10.4103/TJOG.TJOG_10_17
14. Azagew AW, Kassie DG, Walle TA. Prevalence of primary dysmenorrhea, its intensity, impact and associated factors among female students’ at gondar town preparatory school, northwest Ethiopia. BMC Womens Health. (2020) 20(1):1–7. doi: 10.1186/s12905-019-0873-4
15. Yesuf TA, Eshete NA, Sisay EA. Dysmenorrhea among university health science students, Northern Ethiopia: impact and associated factors. Int J Reprod Med. (2018) 2018:9730328. doi: 10.1155/2018/9730328
16. Hailemeskel S, Demissie A, Assefa N. Primary dysmenorrhea magnitude, associated risk factors, and its effect on academic performance: evidence from female university students in Ethiopia. Int J Womens Health. (2016) 8:489. doi: 10.2147/IJWH.S112768
17. Burnett MA, Antao V, Black A, Feldman K, Grenville A, Lea R, et al. Prevalence of primary dysmenorrhea in Canada. J Obstet Gynaecol Can. (2005) 27(8):765–70. doi: 10.1016/S1701-2163(16)30728-9
18. De Sanctis V, Soliman AT, Elsedfy H, Soliman NA, Elalaily R, El Kholy M. Dysmenorrhea in adolescents and young adults: a review in different countries. Acta Biomed. (2016) 87(3):233–46.28112688
19. Vilšinskaitė DS, Vaidokaitė G, Mačys Ž, Bumbulienė Ž. The risk factors of dysmenorrhea in young women czynniki ryzyka bolesnego miesiączkowania u młodych kobiet. Wiad Lek. (2019) 72(6):1170–7. doi: 10.36740/WLek201906102
20. Chauhan M, Kala J. Relation between dysmenorrhea and body mass index in adolescents with rural versus an urban variation. J Obstet Gynaecol India. (2012) 62(4):442–5. doi: 10.1007/s13224-012-0171-7
21. Kural M, Noor NN, Pandit D, Joshi T, Patil A. Menstrual characteristics and prevalence of dysmenorrhea in college-going girls. J Family Med Prim Care. (2015) 4(3):426. doi: 10.4103/2249-4863.161345
22. Ju H, Jones M, Mishra G. The prevalence and risk factors of dysmenorrhea. Epidemiol Rev. (2014) 36(1):104–13. doi: 10.1093/epirev/mxt009
23. Acheampong K, Baffour-Awuah D, Ganu D, Appiah S, Pan X, Kaminga A, et al. Prevalence and predictors of dysmenorrhea, its effect, and coping mechanisms among adolescents in Shai Osudoku district, Ghana. Obstet Gynecol Int. (2019) 2019:5834159. doi: 10.1155/2019/5834159
26. Arroll B, Goodyear-Smith F, Cringle S, Gunn J, Kerse N, Fishman T, et al. Validation of PHQ-2 and PHQ-9 to screen for major depression in the primary care population. Ann Fam Med. (2010) 8(4):348–53. doi: 10.1370/afm.1139
27. Wubshet TY, Geberemichael SG, Adilo TM, Arusi TT, Gutulo MG, Assefa DZ, et al. Prevalence and associated factors of poststroke depression among outpatient stroke patients who have a follow-up at the outpatient neurology clinic of Zewditu memorial hospital in Addis Ababa, Ethiopia. Depress Res Treat. (2022) 2022:9750035. doi: 10.1155/2022/9750035
28. Kahl C, Cleland JA. Visual analog scale, numeric pain rating scale, and the McGill pain questionnaire: an overview of psychometric properties. Phys Ther Rev. (2005) 10(2):123–8. doi: 10.1179/108331905X55776
29. Mohammed H, Hassen N, Musa A. Dysmenorrhea and associated factors among secondary school students in East Hararghe zone, Eastern Ethiopia.. East Afr Health Biomed Sci. (2019) 3(1):39–48.
30. Al-Matouq S, Al-Mutairi H, Al-Mutairi O, Abdulaziz F, Al-Basri D, Al-Enzi M, et al. Dysmenorrhea among high-school students and its associated factors in Kuwait. BMC Pediatr. (2019) 19(1):1–12. doi: 10.1186/s12887-019-1442-6
31. Kaur S, Sheoran P, Sarin J. Assessment and comparison of dysmenorrhea in terms of severity of pain and utilization of nonsteroid anti-inflammatory drugs among unmarried and married women. Int J Caring Sci. (2015) 8(3):737.
32. Armour M, Parry K, Manohar N, Holmes K, Ferfolja T, Curry C, et al. The prevalence and academic impact of dysmenorrhea in 21,573 young women: a systematic review and meta-analysis. J Womens Health. (2019) 28(8):1161–71. doi: 10.1089/jwh.2018.7615
33. Tavallaee M, Joffres MR, Corber SJ, Bayanzadeh M, Rad MM. The prevalence of menstrual pain and associated risk factors among Iranian women. J Obstet Gynaecol Res. (2011) 37(5):442–51. doi: 10.1111/j.1447-0756.2010.01362.x
Keywords: dysmenorrhea, academic activities, family history, Hawassa University, depression
Citation: Belayneh W, Kassaye Z, Arusi T, Abera N, Hantalo A, Melkamu B and Gutulo M (2023) Prevalence of dysmenorrhea and associated factors and its effect on daily academic activities among female undergraduate students of Hawassa University College of Medicine and Health Sciences, Hawassa, Ethiopia. Front. Reprod. Health 5:1244540. doi: 10.3389/frph.2023.1244540
Received: 22 June 2023; Accepted: 1 November 2023;
Published: 15 December 2023.
Edited by:
Pentti Nieminen, University of Oulu, FinlandReviewed by:
Akmal El-Mazny, Cairo University, Egypt© 2023 Belayneh, Kassaye, Arusi, Abera, Hantalo, Melkamu and Gutulo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Temesgen Arusi dGVtYXRhbnR1NDA1QGdtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.