
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Reprod. Health , 14 July 2023
Sec. Reproductive Epidemiology
Volume 5 - 2023 | https://doi.org/10.3389/frph.2023.1165204
This article is part of the Research Topic Inequities and Disparities in Reproductive Health: Reproductive Epidemiology View all 10 articles
 Tegene Atamenta Kitaw*
Tegene Atamenta Kitaw* Ribka Nigatu Haile
Ribka Nigatu Haile
Background: Being a mother for the first time is the most significant event in a woman's life. “Age at first birth” refers to a mother's age in years when she gives birth to her first child. The age of first childbirth has physical, economic, and social implications. However, little is known about this issue in Ethiopia. Thus, this study sought to determine the time to first childbirth and its predictors at a national level.
Methods: Data were extracted from the 2019 Ethiopia Demographic and Health Survey using STATA version 17 software. A total of 8,885 weighted reproductive-age women (15–49 years) were included in this study. A Kaplan–Meier survivor curve was generated to estimate the time of first childbirth. A log-rank test was used to compare the difference in survival curves. Akaike information criteria and Bayesian information criteria were calculated to select the appropriate survival model for the data. The Weibull accelerated failure time model with no frailty distribution was used to identify significant predictors.
Results: The overall median survival time to first childbirth was 18 years. The significant predictors of time to first childbirth were the educational level of the mother [primary education (ϕ = 1.036, 95% CI: 1.011, 1.063), secondary and above education (ϕ = 1.154, 95% CI: 1.118, 1.191)], knowledge of any contraceptive method [know at least one (ϕ = 1.051, 95% CI: 1.006, 1.101)], and media exposure (ϕ = 1.048, 95% CI: 1.011, 1.086).
Conclusion: The median survival time to first childbirth was 18 years, which is lower than the optimal age for first childbirth (late 20 s and early 30 s). The timing of first childbirth in Ethiopia is mainly influenced by the educational level of women, knowledge of contraceptive methods, and exposure to media. Thus, exposing women to educational materials and other awareness-creation campaigns regarding the consequences of early first childbirth and strategies to improve women's knowledge of contraceptive methods is highly recommended.
Age at first birth refers to the woman's age in years when she gives birth to her first child (1). Childbirth is the most significant event in a woman's life. It is an intense event that is physically, psychologically, socially, and culturally significant (2). The impact could be positive, both in the short and long term; however, sometimes, it could result in negative and traumatizing events (3).
Globally, nearly 16 million girls aged between 15 and 19 give birth to their first child each year (4). In developing countries, approximately one-third of women begin having children at 19 or younger, and nearly half of the first births in adolescence are from girls aged 17 or younger. Half of the girls who give birth between the ages of 15 and 17 have a second birth in adolescence, and 11 percent of girls with two births have the third birth in adolescence (5). Early pregnancy and motherhood are common in east African countries, ranging from 18% in Kenya and 29% in Malawi (6).
The socioeconomic implications of youth pregnancy and early childbearing are significant in developing nations and are linked with maternal mortality, low birth weight, poor school achievement and productivity, and, subsequently, intergenerational poverty transmission (7, 8). As the age at first birth decreases, the likelihood of maternal mortality rises. Girls who give birth under 15 and between 15 and 19 years of age are five and two times more at risk of mortality related to pregnancy and childbirth consequences, respectively, than women aged 20–24 at first birth (9, 10). Additionally, pregnancy-related consequences, such as eclampsia, obstetric fistula, and systemic infection, are linked to early age at first birth (11). Later in women's lives, early age birth is also linked to an increased risk of diabetes mellitus, hypertension, lung disease, and poor physical performance (12). In addition to having an adverse effect on the mother's health, it also has negative repercussions on their education, work prospects, and opportunities. Moreover, it is related to societal consequences such as violence, rejection, and shame (13). Additionally, early age at first birth significantly affects a country's population growth, particularly in countries where modern contraception is underutilized (11, 14). Under 5 morbidity is also greater among children born to mothers under 20 years of age (15). Additionally, the risk of newborn mortality is considerably higher for infants whose mothers are under 16 years of age (16). However, bearing a first child at an advanced age is associated with a higher risk of miscarriage, multiple pregnancies, diabetes, chromosomal abnormities, and maternal mortality (10, 17).
The age at first birth varies across different regions. Among European Union (EU) countries the mean age of women at first childbirth ranges from 26.3 in Bulgaria to 31.3 in Italy (18). The median ages at first birth in East Asia and the Pacific (19), Bangladesh (20), Nigeria and Ghana (21, 22), Sub-Saharan Africa (23), and Uganda are 20.2, 16.34, 20, 19, and 19.2 years, respectively (24). In Ethiopia, 13% of women aged 15–19 have begun childbearing and 2% are pregnant with their first child. One in two women aged 25–49 give birth for the first time before age of 20 years (25).
Lower level educational status (26–28), rural residency (21), poor wealth index (29), unemployment (14), husband's education and occupation (30), early age at first sexual intercourse (28, 31), younger age at first marriage (32, 33), peer pressure (34), and smoking status (35) were identified as predictors for early age at first childbirth in several studies.
Delaying pregnancy and childbearing in adolescent women may result in higher academic achievement, ensuring women's economic independence and a better life. Even though promising progress has been made so far regarding age at first birth, early childbearing remains a great challenge in Ethiopia. In 2021, Ethiopia launched a new national adolescent and youth health strategy (2021–2025) with the aim of reducing early age at first pregnancy from 13% to 7% and increasing the median age at first marriage from 17 to 18, thereby reducing early age at first birth (36). Understanding the current nationwide status of age at first birth will play an enormous role in achieving the above-stated goal.
A few related studies have been undertaken so far in Ethiopia. Most studies focused on only teenage and/or adolescent childbearing (37, 38). Furthermore, studies were limited to specific districts/areas (39). Survival analysis of time to first birth among reproductive-age women will have a paramount role in subduing those limitations and further estimating the significant impact of predictor variables at a national level. The age at which childbearing first commences will have a crucial role in estimating the overall fertility level at the country level. Furthermore, this study uses recent Ethiopia Demographic and Health Survey (EDHS, 2019) data, which is crucial in providing up-to-date information on national improvements regarding early childbearing.
Based on the latest census figures and projections from trading economics, the total population in Ethiopia was estimated at 115.0 million people in 2020 (40). The final report of the EDHS 2019 contained detailed information at a national level from the nine regional states and two city administrations of Ethiopia. The administration levels went from regions to zones and through woreda. A survival analysis was conducted among reproductive-age group (15–49) women in Ethiopia using the EDHS data. The EDHS was implemented by the Ethiopian Public Health Institute (EPHI) in collaboration with the Central Statistical Agency (CSA) and the Federal Ministry of Health (FMoH). The target populations were women aged 15–49 and men aged 15–59 in selected households across Ethiopia. The EDHS contains information on the background characteristics of the respondents, maternal health care, fertility, marriage and sexual activity, child feeding practices, nutritional status of women and children, and adult and childhood mortality. Data collection was carried out from March to June 2019 (41).
We received a letter permitting us to acquire the EDHS 2019 data from the DHS program after making a reasonable request. Data extraction was carried out to select reproductive-age women. For this study, a weighted sample of 8,885 reproductive-age women was drawn. The data extraction period was from October 1, 2022 to October 15, 2022. All reproductive-age women (15–49 years) in Ethiopia were the source population, whereas all reproductive-age women (15–49 years) in Ethiopia in the selected enumeration area were the study population.
The 2019 EDHS sample was stratified and selected in two stages. Each region was stratified into urban and rural areas, yielding 21 sampling strata. In the first stage, 305 enumeration areas (EAs) (93 in urban areas and 212 in rural areas) were selected with a probability proportional to EA size. In the second stage, a fixed number of 30 households per cluster were selected with an equal probability systematic selection from the newly created household listing. Sample allocation was carried out to ensure that survey precision was comparable among regions. A total of 25 EAs were selected from eight regions (including two city administrations), and 35 EAs were selected from the three largest regions: Amhara, Oromia, and the Southern Nations, Nationalities, and Peoples' Region (SNNPR). The detailed sampling procedure is accessible in the EDHS 2019 report (41). In this study, a total of 8,885 weighted reproductive-age women (15–49 years) were included. The highlighted sampling procedure for this study is indicated in the figure below (Figure 1).
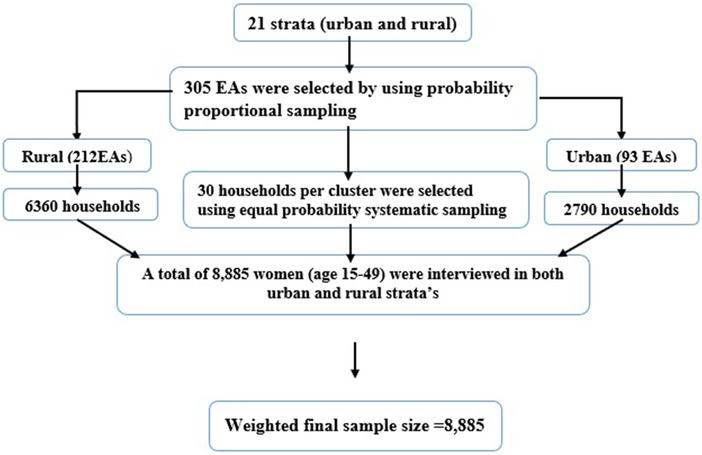
Figure 1. Schematic representation of the sampling procedures in the study of time to first childbirth and its predictors among reproductive age women in Ethiopia (EDHS, 2019). EAs; enumeration areas.
All reproductive-age women (15–49 years) in the selected enumeration area were included in the study, whereas women declared infecund were excluded.
The dependent variable is the time (in years) at first childbirth. This study considered different explanatory variables to determine predictors of time to first childbirth (Table 1).
Event: mothers who first gave birth until the 2019 EDHS data collection end date. Censored: women who did not first give birth until the 2019 EDHS data collection date. Time to first birth: age of the mother in years when she first gave birth (42).
STATA version 17 software was used to extract data from the EDHS 2019 individual (women) record folder. The data were coded, cleaned, and edited. Listing and sorting were carried out to find any missing values. Descriptive statistics were analyzed and presented in terms of frequency and percentage. Age at first birth is calculated as the age difference between the mother and her oldest child. A Kaplan–Meier survivor curve was used to determine the time (years) of first childbirth. A log-rank test was computed to compare the difference in survival curves between categories of variables. A Shenfield residual was fitted and computed to test the assumption of the Cox proportional hazard. Akaike information criteria (AIC) and Bayesian information criteria (BIC) were calculated to select the appropriate survival model for the data. Multicollinearity was checked before running the selected survival model. A VIF above 4 or tolerance below 0.25 indicated that multicollinearity might exist (43). In this study, the maximum VIF was 2.30 with a mean VIF of 1.54 and the minimum tolerance value was 0.43. Thus, there was no multicollinearity between covariates. Variables with a p ≤ 0.25 in the bivariate analysis were fitted and included in the multivariable Weibull accelerated failure time (AFT) model. In the multivariable analysis, variables with a p ≤ 0.05 were considered statically significant.
Survival analysis is a statistical method for analyzing data in which the outcome variable of interest is the time until an event occurs. The outcome of interest in this study was the time to first childbirth, which is time to event data and do not merely depend on whether the event occurred or not but also the time at which the event occurred. Thus, it is best suited to use a survival analysis model. Furthermore, the outcome of interest contained both an event and a time. Thus, linear and logistic regressions were not appropriate. Additionally, those regression models are not well enough equipped to handle censoring events.
A total of 8,885 weighted reproductive-age women were included for the examination on the time to first childbirth in Ethiopia; 5,855 (65.9%) of women gave birth to at least one child (event). Weighted frequency analysis showed that 6,024 (67.8%) of the respondents resided in rural areas. Regarding educational status, 3, 589 (40.4%) of the respondents had no formal education. A total of 3,052 (34.4%) reproductive age women were in the poor household wealth index category. Concerning knowledge of any contraceptive method, 424 (4.8%) of the women did not know of any contraceptive method (Table 2).
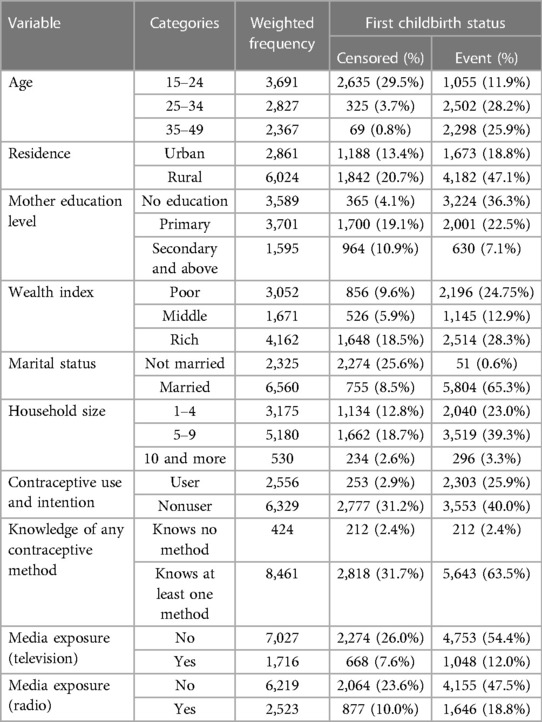
Table 2. Socio-demographic and reproductive health-related characteristics of women in Ethiopia (EDHS, 2019).
The overall median survival time to first childbirth was 18 years. The total follow-up time contributed by all study participants was 107,124 person years. The survival probability of time to first childbirth beyond 14, 16, 18, and 20 years was 87.8%, 72.6%, 53.5%, and 34.4%, respectively (Figure 2).
The median survival time differed among the participant characteristics. The median survival time was 19 years for women who resided in an urban area and 17 years for women from a rural area. By educational status, the median survival time was 17 years for women with no formal education and 20 years for those with secondary and above education. Regarding the wealth index, the median survival times for poor, middle, and rich were 17, 18, and 19 years, respectively.
A Kaplan–Meier survival curve and log-rank test were computed to compare and estimate the survivor function among different characteristics of the respondent. In the Kaplan–Meier survival curve, one survivorship function curve located under another implies that the lower curve group has a lower survival status than the upper curve group. Furthermore, the difference is explained statistically by the log-rank test.
Generally, the Kaplan–Meier survival curve shows that women who reside in a rural area, have no formal education, and have lower wealth index categories had their first child earlier than the reverse group. Furthermore, the log-rank test p-value showed that there was a significant difference in survival experience among covariates of residence (p < 0.001) (Figure 3), women's educational level (p < 0.001) (Figure 4), and wealth index categories (p < 0.001) (Figure 5).
The rho statistic p-value of all covariates and the global test p-value in the Schoenfeld residual was below 0.05. Therefore, the proportional hazard assumption was not fulfilled. Thus, the accelerated failure time model was considered.
The model with the smallest AIC and BIC values was considered to be the best survival model for the given data. The Weibull accelerated failure time (AFT) model with no frailty was found to have the smallest AIC and BIC values (299.23 and 225.82). Thus, the Weibull accelerated failure time (AFT) model with no frailty was the best model for the data to describe the status of women towards time to first childbirth and its predictors (Table 3).
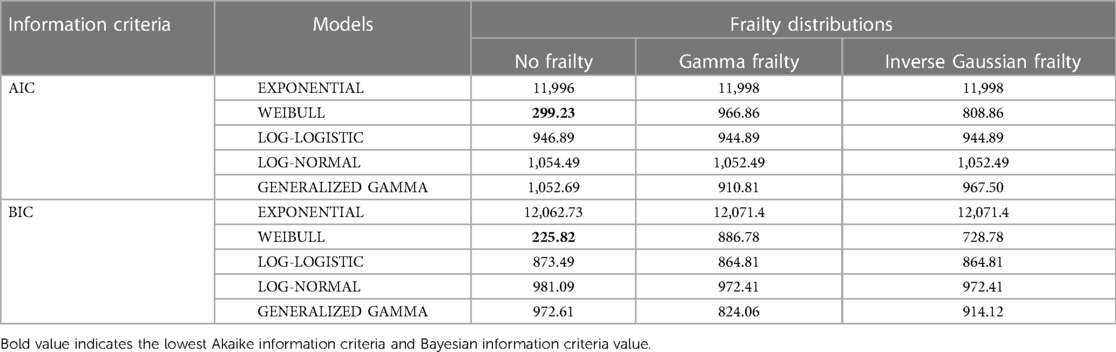
Table 3. Comparison of akaike information criteria and Bayesian information criteria among different accelerated failure time model and frailty distributions.
In the bivariable Weibull AFT model, age, residence, mother education level, wealth index, sex of household head, knowledge of any contraceptive method, media exposure (television), and media exposure (radio) were found to be significant, with a p ≤ 0.25. Additionally, in this model, mother educational level, knowledge of any contraceptive method, and media exposure (television) were predictors of time to first childbirth.
The acceleration factor for time to first childbirth among mothers who had secondary and above education level was 1.154 (ϕ = 1.154, 95% CI: 1.118, 1.191) compared with an uneducated mother. Additionally, the acceleration factor for time to first childbirth in mothers with only primary education was 1.036 (ϕ = 1.036. 95% CI: 1.011, 1.063) compared with the reference group (no education). This shows that uneducated women gave birth to their first child earlier than educated mothers.
Regarding knowledge towards contraceptive methods, the acceleration factor of time to first birth for women who know of at least one contraceptive method was 1.051 (ϕ = 1.051, 95% CI: 1.006, 1.101). This implies that women with knowledge of at least one contraceptive method have a delayed age at first birth compared to women without knowledge of contraceptive methods. In another way, women without knowledge of any contraceptive methods had their first child earlier than their counterparts. Women with media exposure (television) have a 1.048 times acceleration factor for time to first childbirth compared with the reverse group. (ϕ = 1.048, 95% CI: 1.011, 1.086) (Table 4).
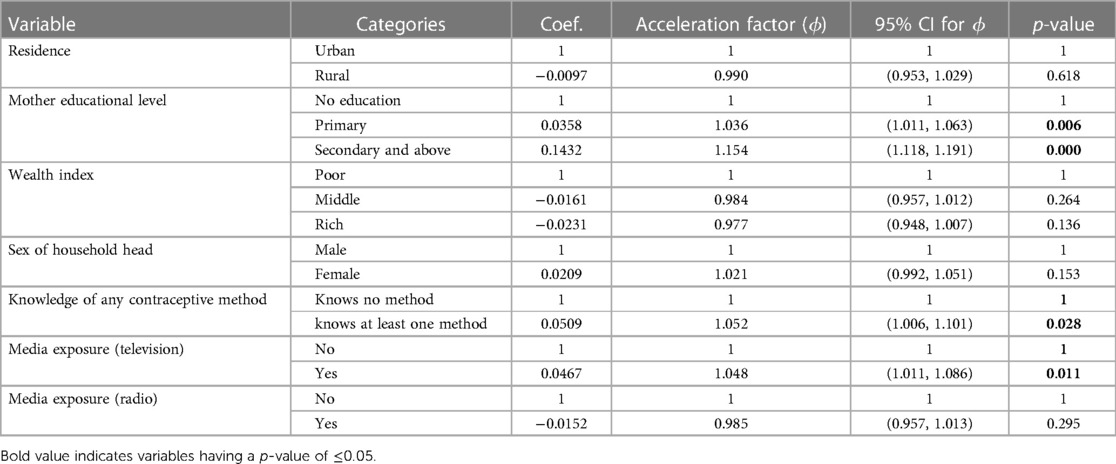
Table 4. Bivariable and multivariable weibull accelerated failure time (AFT) model analysis for predictors of time to first childbirth in Ethiopia [EDHS 2019 (n = 8,885)].
Time to first childbirth and its predictors were determined by using data from the recent 2019 Ethiopian Demographic Health Survey. Mother education level, knowledge of any contraceptive method, and media exposure (television) were found to be predictors of time to first childbirth.
The overall median survival time (age) to first childbirth was 18 years. This finding is in line with a study carried out in Gambia (18 years) (44). This result is lower than the that from a study undertaken in several regions, such as the USA (26.9 years) (45), Ghana (19.91 years) (22), Uganda (19.2 years) (24), Nigeria (20 years) (33), and Kenya (20.3 years) (46). The awareness of women about the consequence of having babies at an early age and contraceptive access and utilization plays a paramount role in delaying age at first childbirth in developed countries (47). In developing countries like Ethiopia, women's autonomy regarding reproductive health decisions is low. This might lead to poor reproductive health care seeking behaviors, such as low contraceptive utilization, thereby resulting in early first childbearing (48, 49). In addition, the variation could be attributed to different factors such as age at first marriage, age at first sexual experience, and contraceptive usage, which were listed as factors that shortened the survival time of onset of first childbirth in different studies (22, 28, 50). For instance, the median ages at first marriage in Ethiopia and Kenya were 17.2 years (51) and 19 years (52), respectively. In addition, contraceptive use is quite different; the prevalence of contraceptive use in Kenya is 39% (53), whereas as in Ethiopia it is 20.42% (54).
On the contrary, the finding of this study is higher than the study conducted in Bangladesh (17.92 years) (55). This variation could be attributed to differences in religious beliefs. In Bangladesh, most of the population has a Muslim affiliation. A Muslim religious affiliation is closely linked with the early age of the mother at first birth (14). In addition, in Bangladesh, many people are unaware of the consequences of early marriage and early pregnancy (56).
This study revealed that women's educational level is a predictor of time to first childbirth. Women who attend primary, secondary, and higher education delayed their first childbirth more than those who did not have any education. This finding is consistent with a study carried out in Kenya (57), which concluded that the probability of giving birth at an earlier age decreases as the educational level increases. Similarly, a study carried out in Ghana revealed that the higher the woman's educational level, the longer the waiting time for her first birth: 73% of postsecondary level women had yet to give birth before the age of 30 (22). Furthermore, a study conducted in Bangladesh also found pretty consistent findings that women with higher levels of education have a lower risk of having an early first birth (42).
The possible explanation might be that uneducated women might not know the optimal age at which giving childbirth has the minimum risk. Education level and contraceptive utilization is directly proportional. The higher the education level, the higher the use of contraception (58). Thus, the low contraceptive use of uneducated mothers leads to early first childbirth. Therefore, enrolling women in at least primary education will reduce the incidence of early first childbirth and the related consequences.
This finding indicates a positive interaction between women's knowledge of contraceptive methods and delaying the time of first childbirth. This finding is supported by a study carried out in East Asia and the Pacific (19) that found that there is a high incidence of early first childbirth among women without any knowledge of contraceptive methods. Likewise, a study conducted in Tanzania (59) also revealed that contraceptive knowledge is considerably high among women who delay their first childbirth.
This might be because the likelihood of contraceptive use was high among women who know about contraceptives (60). Women might delay early-age maternity as long as she uses contraceptive methods. Thus, policymakers should emphasize improving women's knowledge of different types of contraceptives by providing access to information about contraceptives through healthcare providers, online resources, and community organizations. Furthermore, it is recommended that open dialogue about contraception is encouraged between women and their partners, family members, and healthcare providers. Thus, increasing women's knowledge of contraceptive methods can delay early maternity, preventing unintended adolescent pregnancy and early pregnancy-related mortality and morbidity.
Media exposure has also been found to be a predictor of time to first birth. Women who have access to media are less likely to give birth to their first child at an early age than those who did not have access. This result is in agreement with a study carried out in Bangladesh (61) that indicated that women exposed to media on a regular basis were less likely to give birth to their first child at an early age than those who are not exposed (44.8% vs. 70.2%).
This finding points to the fact that women who do not have access to media might be unaware of the complications associated with early age at first childbirth. In addition, maternal healthcare utilization, including family planning services, is significantly higher among women exposed to mass media, which delays early maternity (62). Furthermore, those who were not exposed to media were more likely to get married earlier and have earlier sexual experiences, resulting in early first childbirth. Thus, advertisements and educational programs through mass media targeting the consequences of early first childbirth on maternal and child health are highly recommended.
The strength of this study is that it uses nationally representative data and can be generalizable to all Ethiopian reproductive-age women. Owing to the self-reported nature of the data, there might be recall bias. As the data source is secondary, it is difficult to quantify other potential predictors of time to first childbirth. A lack of trend analysis is also a limitation of this study.
In this study, the median survival time to first childbirth was 18 years, which is lower than the optimal age for first childbirth, between the late 20 s and 30 s (63, 64). This is the ideal age for education. In addition to having implications on her social, physical, and mental health, being a mother at this age may prevent the woman from attending school. The timing of first childbirth in Ethiopia is mainly influenced by women's level of educational, knowledge of contraceptive methods, and access to media. Interventions could involve raising women's educational levels by exposing them to educational materials and other awareness-creation efforts regarding the consequences of early first childbirth. In addition, expanding adolescent and youth-friendly services in the country might increase women's knowledge of contraceptive methods. Furthermore, including sexual and reproductive health education programs in the educational curriculum also contributes to reducing early marriage and sexual initiation, thereby decreasing early first childbirth. Furthermore, policymakers and other non-governmental organizations should continuously invest resources in transmitting messages through mass media (television), such as advertisements and other programs, regarding the impact of early childbirth. In conclusion, a prospective follow-up study that includes other potential predictors is recommended.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
TAK: conception, proposal development, data acquisition, analysis, data interpretation, and article drafting. RNH: Participated equally in design, data management, analyses, interpretation, and manuscript write up. All authors contributed to the article and approved the submitted version.
The authors are grateful to the Demographic and Health Surveys Program for granting them access to the dataset.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frph.2023.1165204/full#supplementary-material.
1. Motsima T. The risk factors associated with early age at first birth amongst Angolan women: evidence from the 2015–2016 Angola demographic and health survey. Eur J Med Health Sci. (2020) 2(2):5–8. doi: 10.24018/ejmed.2020.2.2.198
2. Horsch A, Ayers S. Childbirth and Stress. Stress: Concepts, Cognition, Emotion, and Behavior. Lausanne, Switzerland: University Hospital Lausanne (2016). 325–30.
3. Aune I, Marit Torvik H, Selboe ST, Skogås AK, Persen J, Dahlberg U. Promoting a normal birth and a positive birth experience - Norwegian women’s perspectives. Midwifery. (2015) 31(7):721–7. doi: 10.1016/j.midw.2015.03.016
4. Blum RW, Gates WH. Girlhood, not motherhood: preventing adolescent pregnancy: United Nations Population Fund (UNFPA) (2015).
5. UNFPA. Motherhood in childhood: The untold story (2022). Available at: https://www.unfpa.org/publications/motherhood-childhood-untold-story.
6. Wado YD, Sully EA, Mumah JN. Pregnancy and early motherhood among adolescents in five east African countries: a multi-level analysis of risk and protective factors. BMC Pregnancy Childbirth. (2019) 19(1):59. doi: 10.1186/s12884-019-2204-z
7. Chandra-Mouli V, Camacho AV, Michaud P-A. WHO guidelines on preventing early pregnancy and poor reproductive outcomes among adolescents in developing countries. J Adolesc Health. (2013) 52(5):517–22. doi: 10.1016/j.jadohealth.2013.03.002
8. Lloyd CB, Mensch BS. Marriage and childbirth as factors in dropping out from school: an analysis of DHS data from sub-Saharan Africa. Popul Stud. (2008) 62(1):1–13. doi: 10.1080/00324720701810840
9. Ngowa JDK, Kasia JM, Pisoh WD, Ngassam A, Noa C. Obstetrical and perinatal outcomes of adolescent pregnancies in cameroon: a retrospective cohort study at the Yaoundé general hospital. Open J Obstet Gynecol. (2015) 5(02):88. doi: 10.4236/ojog.2015.52012
10. Sakai T, Sugawara Y, Watanabe I, Watanabe T, Tomata Y, Nakaya N, et al. Age at first birth and long-term mortality for mothers: the Ohsaki cohort study. Environ Health Prev Med. (2017) 22(1):1–14. doi: 10.1186/s12199-017-0631-x
11. Gibbs CM, Wendt A, Peters S, Hogue CJ. The impact of early age at first childbirth on maternal and infant health. Paediatr Perinat Epidemiol. (2012) 26(Suppl 1(01):259–84. doi: 10.1111/j.1365-3016.2012.01290.x
12. Pirkle CM, de Albuquerque Sousa AC, Alvarado B, Zunzunegui MV. Early maternal age at first birth is associated with chronic diseases and poor physical performance in older age: cross-sectional analysis from the international mobility in aging study. BMC Public Health. (2014) 14:293. doi: 10.1186/1471-2458-14-293
13. UNICEF D. Monitoring the situation of children and women (2021). Available at: https://data.unicef.org/topic/child-health/adolescent-health/.
14. Ali M, Alauddin S, Khatun M, Maniruzzaman M, Islam SMS. Determinants of early age of mother at first birth in Bangladesh: a statistical analysis using a two-level multiple logistic regression model. J Public Health (Bangkok). (2021) 29(5):1081–7. doi: 10.1007/s10389-020-01228-9
15. Ahinkorah BO. Maternal age at first childbirth and under-five morbidity in sub-Saharan Africa: analysis of cross-sectional data of 32 countries. Arch Public Health. (2021) 79(1):151. doi: 10.1186/s13690-021-00674-5
16. Neal S, Channon AA, Chintsanya J. The impact of young maternal age at birth on neonatal mortality: evidence from 45 low and middle income countries. PLoS One. (2018) 13(5):e0195731. doi: 10.1371/journal.pone.0195731
18. Eurostat. Women in the EU are having their first child later (2021). Available at: https://ec.europa.eu/eurostat/web/products-eurostat-news/-/ddn-20210224-1.
19. Kennedy E, Gray N, Azzopardi P, Creati M. Adolescent fertility and family planning in east Asia and the pacific: a review of DHS reports. Reprod Health. (2011) 8(1):1–12. doi: 10.1186/1742-4755-8-11
20. Karim MA, Faruk MO. Patterns and differentials of age at first motherhood among married adolescents in Bangladesh. Biomed Sci. (2021) 7(3):86. doi: 10.11648/j.bs.20210703.15
21. Fagbamigbe AF, Idemudia ES. Survival analysis and prognostic factors of timing of first childbirth among women in Nigeria. BMC Pregnancy Childbirth. (2016) 16(1):1–12. doi: 10.1186/s12884-016-0895-y
22. Ida LA, Albert L. The statistical distribution and determinants of mother’s age at first birth. Am J Theor Appl Stat. (2015) 4(2):41–52. doi: 10.11648/j.ajtas.20150402.11
23. Negash WD, Asmamaw DB. Time to first birth and its predictors among reproductive age women in high fertility countries in sub-Saharan Africa: inverse weibull gamma shared frailty model. BMC Pregnancy Childbirth. (2022) 22(1):844. doi: 10.1186/s12884-022-05206-9
25. Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia demographic and health survey (2016). Addis Ababa, Ethiopia, and Rockville, Maryland, USA: CSA and ICF.
26. Yakubu I, Salisu WJ. Determinants of adolescent pregnancy in sub-Saharan Africa: a systematic review. Reprod Health. (2018) 15(1):15. doi: 10.1186/s12978-018-0460-4
27. Zare N, Nouri B, Moradi F, Parvareh M. The study of waiting time to first pregnancy in the south of Iran: a parametric frailty model approach. Int J Reprod Biomed. (2017) 15(1):11–6. doi: 10.29252/ijrm.15.1.11
28. Chowdhury A, Rumana A, Faisal A. Factors affecting age for first birth: an exploratory analysis on Bangladeshi women. Int J Res Stud Med Health Sci. (2017) 2(7):31–7. doi: 10.12691/ajphr-1-7-8
29. Khanal P. Determinant of age at first birth in Nepal: a study of adolescent and youth women in NDHS 2016. J Popul Dev. (2021) 2(1):130–40. doi: 10.3126/jpd.v2i1.43487
30. Thandar M, Moe HH, Htwe AA. Patterns and determinants of age at first birth of women in Myanmar. Asia-Pac Sustainable Dev J. (2021) 28(1):87–109. doi: 10.18356/26178419-28-1-4
31. Ndlovu S. Demographic and socio-economic determinants of age at first birth in Swaziland. PAA (2017). Annual Meeting; 2017: PAA.
32. Kassa GM, Arowojolu AO, Odukogbe AA, Yalew AW. Prevalence and determinants of adolescent pregnancy in Africa: a systematic review and meta-analysis. Reprod Health. (2018) 15(1):195. doi: 10.1186/s12978-018-0640-2
33. Kunnuji MON, Eshiet I, Nnorom CCP. A survival analysis of the timing of onset of childbearing among young females in Nigeria: are predictors the same across regions? Reprod Health. (2018) 15(1):173. doi: 10.1186/s12978-018-0623-3
34. Sarkar P. Determinants of age at first birth in Bangladesh. J Mod Math Stat. (2010) 4:1–6. doi: 10.3923/jmmstat.2010.1.6
35. Talukder A, Khan ZI, Khatun F, Tahmida S. Factors associated with age of mother at first birth in Albania: application of quantile regression model. Heliyon. (2021) 7(3):e06547. doi: 10.1016/j.heliyon.2021.e06547
36. Ethiopian Federal Ministry of Health. National adolescent and youth health strategy (2021-2025) (2021). Available at: https://ethiopia.unfpa.org/en/news/ethiopias-new-adolescent-and-youth-health-strategy-aims-halve-teenage-pregnancy
37. Mezmur H, Assefa N, Alemayehu T. Teenage pregnancy and its associated factors in eastern Ethiopia: a community-based study. Int J Womens Health. (2021) 13:267–78. doi: 10.2147/ijwh.S287715
38. Mathewos S, Mekuria A. Teenage pregnancy and its associated factors among school adolescents of arba minch town, southern Ethiopia. Ethiop J Health Sci. (2018) 28(3):287–98. doi: 10.4314/ejhs.v28i3.6
39. Ayele BGK, Gebregzabher TG, Hailu TT, Assefa BA. Determinants of teenage pregnancy in Degua Tembien district, Tigray, northern Ethiopia: a community-based case-control study. PloS One. (2018) 13(7):e0200898. doi: 10.1371/journal.pone.0200898
40. “Ethiopia Population - 2021 Data - 2022 Forecast - 1960–2020 Historical - Chart - News” (2022). Available at: https://tradingeconomics.com/ethiopia/population.
41. Ethiopian Public Health Institute (EPHI) and ICF. Ethiopia mini demographic and health survey (2019). Final report. Rockville, Maryland, USA: EPHI and ICF.
42. Rabbi AMF, Kabir M. Factors influencing age at first birth of Bangladeshi women-a multivariate approach. Am J Public Health Res. (2013) 1(7):191–5. doi: 10.12691/ajphr-1-7-8
44. Allal N, Sear R, Prentice AM, Mace R. An evolutionary model of stature, age at first birth and reproductive success in Gambian women. Proc Biol Sci. (2004) 271(1538):465–70. doi: 10.1098/rspb.2003.2623
45. Eickmeyer KJ, Payne KK, Brown SL, Manning WD. Crossover in the median age at first marriage and first birth: thirty-five years of change. Family Profiles. (2017):FP-17-22. doi: 10.25035/ncfmr/fp-17-22.
46. Kenya national bureau of statistics KMoH, National AIDS control council/Kenya, Kenya Medical research institute, national council for population, development/Kenya a. Kenya demographic and health survey: key indicators 2014 (2014).
47. Frederiksen BN, Ahrens KA, Moskosky S, Gavin L. Does contraceptive use in the United States meet global goals? Perspect Sex Reprod Health. (2017) 49(4):197–205. doi: 10.1363/psrh.12042
48. Edossa ZK, Debela TF, Mizana BA. Women’s decision on contraceptive use in Ethiopia: multinomial analysis of evidence from Ethiopian demographic and health survey. Health Serv Res Manag Epidemiol. (2020) 7:2333392820924565. doi: 10.1177/2333392820924565
49. Wado YD. Women’s autonomy and reproductive health-care-seeking behavior in Ethiopia. Women Health. (2018) 58(7):729–43. doi: 10.1080/03630242.2017.1353573
50. Pandey A, Nath DC. Frailty approach to age at first birth in Uttar Pradesh-India. GSTF J Math Statistics Oper Res. (2015) 3:1–6. doi: 10.5176/2251-3388_3.1.60
51. Makheti FM. Determinants of age at first marriage in Kenya: a comparative analysis between men and women (2008).
52. Gobena MG, Alemu YM. Analyzing factors associated with time to age at first marriage among women in Ethiopia: log logistic-gamma shared frailty model. BMC Womens Health. (2022) 22(1):191. doi: 10.1186/s12905-022-01775-1
53. Lunani LL, Abaasa A, Omosa-Manyonyi G. Prevalence and factors associated with contraceptive use among Kenyan women aged 15–49 years. AIDS Behav. (2018) 22(Suppl 1):125–30. doi: 10.1007/s10461-018-2203-5
54. Gebre MN, Edossa ZK. Modern contraceptive utilization and associated factors among reproductive-age women in Ethiopia: evidence from 2016 Ethiopia demographic and health survey. BMC Womens Health. (2020) 20(1):61. doi: 10.1186/s12905-020-00923-9
55. Nahar MZ, Zahangir MS. Patterns and determinants of age at first birth in Bangladesh. Turk J Popul Stud. (2013) 35:63–77. Available at: https://dergipark.org.tr/tr/pub/nufusbilim/issue/22954/245671
56. Ainul S, Amin S. Early marriage as a risk factor for mistimed pregnancy among married adolescents in Bangladesh. Asia-Pac Popul J. (2015) 30(1):8–28. doi: 10.18356/0392d441-en
57. Ferré C. Age at first child: does education delay fertility timing? The case of Kenya. The case of Kenya (February 1, 2009) World Bank Policy Research Working Paper. 2016(4833).
58. Babore GO, Heliso AZ. Contraceptive utilization and associated factors among youths in Hossana town administrative, Hadiya zone, Southern Ethiopia. PLoS One. (2022) 17(11):e0275124. doi: 10.1371/journal.pone.0275124
59. Sedekia Y, Nathan R, Church K, Temu S, Hanson C, Schellenberg J, et al. Delaying first birth: an analysis of household survey data from rural Southern Tanzania. BMC Public Health. (2017) 17(1):134. doi: 10.1186/s12889-017-4069-2
60. Ukoji VU, Anele PO, Imo CK. Assessing the relationship between knowledge and the actual use of contraceptives among childbearing women in south-south Nigeria: evidence from the 2018 Nigeria demographic and health survey. BMC Public Health. (2022) 22(1):2225. doi: 10.1186/s12889-022-14728-y
61. Islam A, Alauddin S, Barna SD. Socioeconomic and demographic predictors of women’s first birth at an early age: evidence from Bangladesh’s demographic and health survey, 2004–2014. J Int Womens Stud. (2021) 22(1):359–73. Available at: https://vc.bridgew.edu/jiws/vol22/iss1/21
62. Fatema K, Lariscy JT. Mass media exposure and maternal healthcare utilization in south Asia. SSM Popul Health. (2020) 11:100614. doi: 10.1016/j.ssmph.2020.100614
Keywords: childbirth, determinants, Ethiopia, reproductive age, survival analysis, time to first
Citation: Kitaw TA and Haile RN (2023) Time to first childbirth and its predictors among reproductive-age women in Ethiopia: survival analysis of recent evidence from the EDHS 2019. Front. Reprod. Health 5:1165204. doi: 10.3389/frph.2023.1165204
Received: 13 February 2023; Accepted: 17 April 2023;
Published: 14 July 2023.
Edited by:
Yi-Xin Wang, Harvard University, United StatesReviewed by:
Chen Yingjun, Southern Medical University, China© 2023 Kitaw and Haile. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tegene Atamenta Kitaw dGVnZW5lMjAxM0BnbWFpbC5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.