- 1Arnhold Institute for Global Health, Icahn School of Medicine at Mount Sinai, New York, NY, United States
- 2Center for Global Health, Indiana University School of Medicine - Lafayette, West Lafayette, IN, United States
- 3Department of Media Studies, School of Literature, Language and Media, University of the Witwatersrand, Johannesburg, South Africa
- 4Department of Mental Health and Behavioral Sciences, Moi University, Eldoret, Kenya
- 5School of Medicine, Institute of Human Virology, Baltimore, MD, United States
- 6Institute for Human Virology, Institute of Human Virology Nigeria, International Research Centre of Excellence (IRCE), Abuja, Nigeria
- 7School of Medical Sciences, University of Cape Coast, Cape-Coast, Ghana
- 8Department of Community Health & Social Medicine, The City University of New York, New York, NY, United States
- 9Center for Interdisciplinary Research on AIDS Yale University, New Haven, CT, United States
Objectives: This review seeks to critically analyze studies assessing gender differences in HIV-related knowledge among adolescents and young people in low- and middle-income countries.
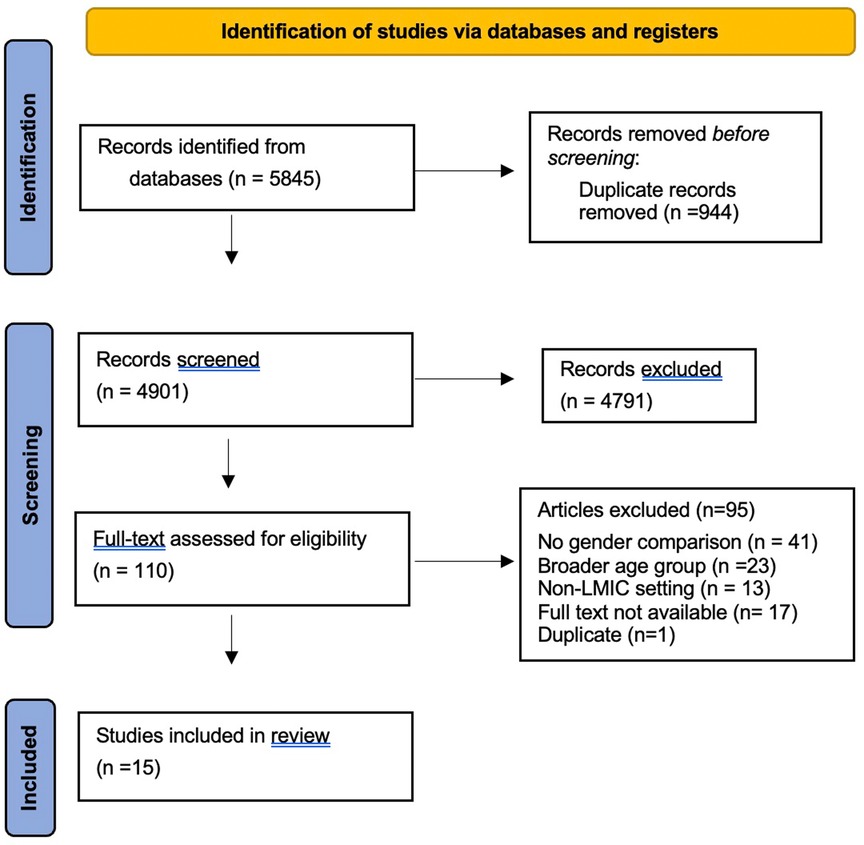
Methods: Using PRISMA guidelines and searching Pubmed and Scopus online databases, the search strategy combined search keywords with Boolean operators: (HIV OR AIDS) AND (knowledge) AND (gender) AND (adolescents). AC and EG conducted the search and independently reviewed all articles in Covidence software; conflicts were resolved by GC. Articles were included if they evaluated differences in HIV knowledge in at least two groups ages 10–24 and were implemented in a low or middle-income country.
Results: The search resulted in 4,901 articles, of which fifteen studies, implemented in 15 countries, met selection criteria. Twelve evaluated differences in HIV knowledge in school settings; three evaluated participants in clinic settings. Adolescent males consistently scored higher in composite knowledge scores, as well as knowledge of HIV transmission, prevention, attitudes and sexual decision-making.
Conclusion: We found gender-based discrepancies between knowledge, perception of risk and HIV prevalence among youth globally, with boys consistently scoring higher in HIV knowledge. However, there is significant evidence that social and cultural contexts render girls at high risk of HIV infection, and the gaps in girls' knowledge and boys' roles in HIV risk must be addressed urgently. Future research should consider interventions that facilitate discussion and HIV knowledge building across genders.
Introduction
Globally, there are 1.8 billion adolescents and young people aged 10–24 years, representing one quarter of the world's population, 86% of whom live in low and middle-income countries (LMIC) (1). Adolescence is a critical period of biological, psychological and socioemotional development (2, 3), with new transitions, increasing autonomy and sexual debut for many young adults (4). Sexual debut in adolescence presents new challenges and risks of sexually transmitted infections, and is associated with the highest HIV risk among all age groups (5). Thus, it is critical that HIV education, particularly as related to behavioral risks, sexual health decision-making and HIV prevention strategies are prioritized for this group.
Adolescents and young people living with HIV (AYPLWH) represent the fastest-growing subgroup of people living with HIV; this is due to the increased incidence of new HIV infections within this age group, and the growing number of perinatally-infected youth reaching adolescence and young adulthood (6). As adolescents mature into adulthood, the risk of HIV transmission to sexual partners or infants remains high, necessitating intensive prevention and educational interventions (7). Investigation of adolescent HIV literacy provides an opportunity to assess gaps in knowledge that may perpetuate risk-taking behavior and inform the development of interventions to combat transmission among this high-risk group. Increased HIV-related knowledge has the potential to mitigate risk-taking and other health behaviors that contribute to HIV infection.
Furthermore, investigating potential gender differences in HIV knowledge can provide insight into the need for gender-based interventions to mitigate HIV risk behaviors among adolescents. Harmful gender-based reproductive health norms adopted in adolescence influence long-term health, as they create health inequities for girls and young women, a population most at risk of new HIV infections in high-burden LMICs. The consequences of these harmful norms and inequities include sexual violence, loss of autonomy and agency, and higher rates of sexually transmitted infections including HIV. This warrants a gender-based investigation of factors-including HIV knowledge or lack thereof- associated with high rates of HIV transmission or of strategies and opportunities for prevention.
Investigating differences in HIV literacy across gender allows for better understanding of the relationship between gender and HIV knowledge-related determinants of HIV transmission, especially as it relates to sexual behavior. Better understanding of the relationships between gender, HIV knowledge and HIV transmission can inform the development of responsive interventions to address gender norms that negatively impact HIV knowledge acquisition. This review seeks to critically analyze studies assessing gender differences in HIV-related knowledge among adolescents in LMIC. It aims to identify specific HIV-related topics in which adolescents' knowledge and understanding may differ based on gender, to inform tailored education strategies for the prevention of HIV in this population. The studies included in this review compare outcomes between adolescents and young people assigned male and female at birth and will refer to them as girls and boys throughout; this review reflects sex assigned at birth and not necessarily gender identity.
Methods
Search strategy and selection criteria
We used the Preferred Reporting Items for Systematic Reviews (PRISMA) guidelines to conduct this review (8). We searched the PubMed and Scopus online databases for peer reviewed articles and searched the grey literature through the HIV/AIDS Clearing House, USAID Development Experience Clearinghouse, UNESCO HIV and AIDS Education Clearinghouse, and the WHO and UNAIDS websites. The search strategy was completed on 18 August 2021 and combined search keywords with Boolean operators: (HIV OR AIDS) AND (knowledge) AND (gender) AND (adolescents). The search was run again on 18 October 2022, which returned no additional articles meeting inclusion criteria.
To be included, articles must have met the following criteria: (1) quantitatively evaluated differences in HIV knowledge and perspectives of at least two groups with different sex assigned at birth; (2) included adolescents and young people between ages 10–24 years; (3) included at least one quantitative HIV knowledge outcome measure, and (4) implemented in a LMIC as defined by the World Bank Country Classification (9). There were no exclusion criteria related to study design, provided they met inclusion criteria and were peer-reviewed research. There were no time period limits for this search.
Data extraction and analysis
Two authors (AC and EG) conducted the search in Pubmed and Scopus online databases and exported articles into Covidence software for managing reviews (10). The search strings (HIV OR AIDS) AND (knowledge) AND (gender) AND (adolescents) were used in both databases, returning a total of 5,485 articles. Covidence software removed duplicates and AC and EG independently reviewed all article titles and abstracts to determine whether the studies met the inclusion criteria. Conflicts were resolved by a third reviewer (GC) to reach consensus. AC and EG reviewed the full text articles to determine if studies should be included, and GC provided secondary review of conflicts. References from included articles were reviewed and screened for additional publications. This process is represented in Figure 1. AC and EG extracted data from the included studies in Covidence for analysis. Article author, journal of publication, publication date, country location of study, region type, study aims and design, instrument(s) used to measure HIV knowledge and topics assessed, target population, sample size and sex distribution of sample, enrollment setting, and results were extracted. A sub-set of the extracted data can be found in Table 1.
Results
After conducting searches in all target databases, we identified 5,845 potentially relevant articles and reports (Figure 1). After removing duplicates, a total of 4,901 peer-reviewed articles and gray literature remained for title and abstract review. Full text review was completed for 110 articles, followed by review of references included in reviews and articles meeting inclusion criteria. Ninety-five articles were excluded after full text review because they did not include a gender-specific comparison of HIV knowledge (n = 41), did not take place in a LMIC (n = 13), included a broader age group (n = 23), or full text could not be located (n = 17). One duplicate identified through the references of an included article was removed at that stage (11). Data extraction was conducted for 15 peer-reviewed articles.
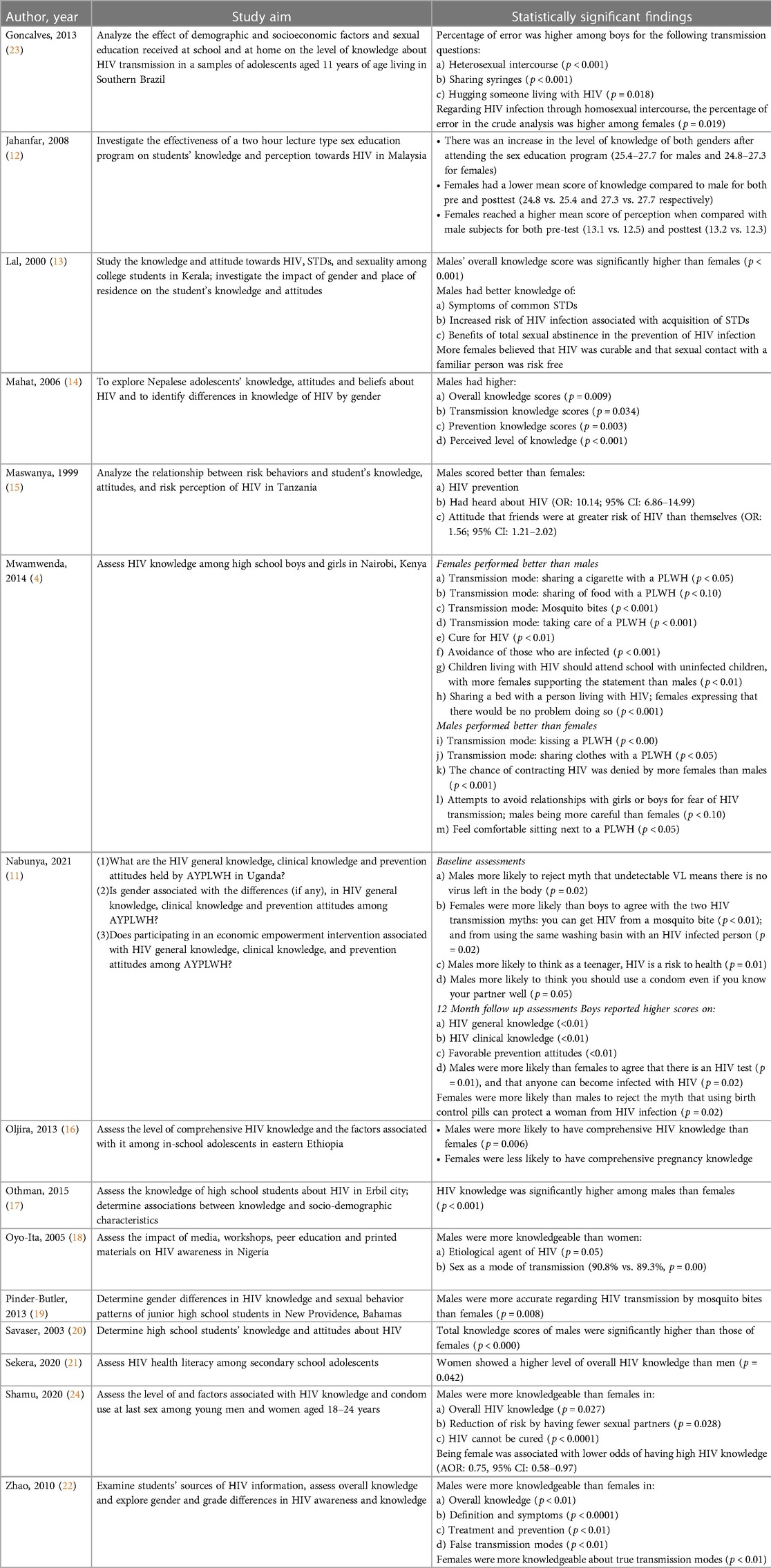
The 15 studies that met selection criteria varied by study design, enrollment location and outcome measures (Table 1). In total, the included studies enrolled 17,043 adolescents between age 10 and 24 years, comprising 8,947 (52%) males and 8,096 (48%) females. The studies covered four different study designs: randomized control trials, cross-sectional one-time survey assessments, cross-sectional pre-posttest assessments, and prospective cohort studies, and only two studies were interventional (11, 12). Most of the included studies (N = 12) evaluated differences in HIV knowledge in the school setting (12–22), particularly among secondary school- and college-aged students; three studies evaluated these differences in the clinic setting (11, 23, 24). Furthermore, most included studies (N = 12) utilized study-developed HIV knowledge outcome measures (4, 11, 12, 13, 14, 17–23), while three studies used adapted UNAIDS or WHO tools to evaluate HIV knowledge (15, 16, 24). The selected studies reported a range of outcomes that are presented in Table 2.
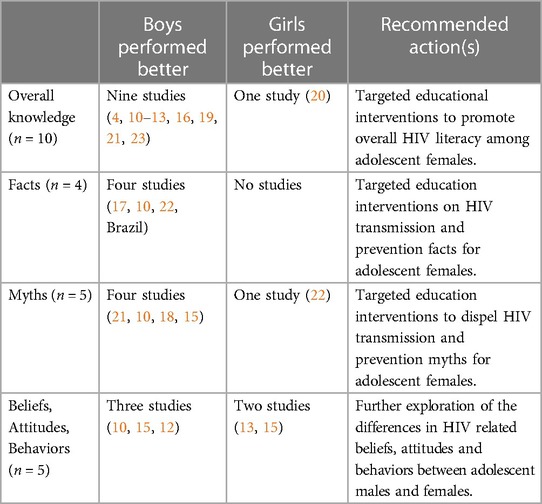
Overall HIV knowledge
Eleven of the 15 included studies reported overall HIV knowledge scores. The majority of these 11 studies (N = 9) reported significantly higher knowledge among males as compared to females (11–14, 16, 17, 20, 22, 24). These findings were true across several countries; males demonstrated higher overall knowledge assessments in studies conducted in Malaysia, India, Nepal, Uganda, Ethiopia, Iraq, Turkey, South Africa, and China. Six of these nine studies were conducted in secondary schools (12, 14, 16, 17, 20, 22) while the other three were conducted in college (13) and clinic settings (11, 24).
A minority (N = 2) of studies reported more varied findings regarding overall HIV knowledge (19, 21). In the Czech Republic, secondary school girls showed a significantly higher level of overall HIV knowledge than boys (p = 0.042) (21). Pinder-Butler and colleagues reported no differences in overall HIV knowledge between secondary school boys and girls in the Bahamas (19). Additionally, among secondary school adolescents in Nepal, Mahat and colleagues found that boys scored significantly higher than girls on self-perception of their level of HIV knowledge (p < 0.001) (14). Lastly, Nabunya and colleagues reported no gender differences in knowledge among adolescent clinic patients in Uganda regarding a cure for HIV (11).
HIV knowledge by gender before and/or after an intervention
Nabunya et al, Uganda
In Uganda, Nabunya and colleagues investigated HIV clinical knowledge among 702 adolescents (306 males vs. 396 females) before and one year after an economic empowerment intervention to improve ART adherence (11). At baseline, males were more likely to reject the myth that undetectable viral load meant that there is no virus left in the body (p = 0.02). At follow up, males were more likely to agree that: (1) there is an HIV test (p = 0.01) and (2) that anyone can become infected with HIV (p = 0.02). Males were also more likely to know that: (1) CD4 count measures how many “soldier” cells are in the body to fight HIV (p < 0.01); (2) low CD4 count means fewer “soldier” cells to fight infections (p < 0.01); (3) viral load tests measure how much HIV is in the blood (p < 0.01); (4) resistant virus means that medicine no longer works to lower or slow down the virus (p < 0.01); and (5) the virus can be resistant if medication doses are missed (p < 0.01) In addition, males were more likely to reject the following myths: (1) it's ok for a person to stop taking their medication if their CD4 count is high or if they feel healthy (p < 0.01) and; (2) undetectable viral load means there is no virus left in the body (p = 0.01). Nabunya and colleagues hypothesized that the observed differences may be rooted in gender and cultural norms in which girls and women have more restricted opportunities for education and are expected to know less about sex, boys and men have decision-making power around safe sex, and open discussions around sex among adolescents is considered taboo (11).
Jahanfar et al, Malaysia
In Malaysia, Jahanfar and colleagues investigated HIV knowledge among 182 adolescents (73 males vs. 109 females) before and immediately after a two-hour talk on sexual education (12). The authors reported an increase in HIV knowledge among both males and females after the sex education program; mean scored increased from 25.4 to 27.7 for males and from 24.8 to 27.3 for females. As compared to their male counterparts, females had a lower mean score of knowledge for both pre and posttest assessments (pre-test scores: 24.8 female vs. 25.4 male and posttest scores: 27.3 female vs. 27.7 male).
HIV transmission and prevention: facts vs. myths
Eight included studies assessed knowledge by asking participants to identify facts vs. myths of HIV transmission modes (4, 11, 14, 18–20, 22, 23). In Nepal, Mahat and colleagues reported that males were more knowledgeable than females and had higher overall transmission knowledge scores (p = 0.034), particularly in HIV prevention (p = 0.003) (14). In Nigeria, Oyo-Ita and colleagues reported no gender differences in overall knowledge regarding modes of HIV transmission (18). In Turkey, Savaser reported no gender differences in knowledge about risk categories for individuals or key groups (20).
Myths
In China, Zhao et al. included questions regarding both true and false transmission modes; males were more knowledgeable in identifying false transmission modes (p < 0.01); females were more knowledgeable about true transmission modes (p < 0.01) (22). Lal and colleagues reported that both males and females were equally misinformed about the risk of getting HIV by donating blood to a blood bank (13). There were no gender differences in the identification of the following myths as modes of HIV transmission: use of a common toilet seat, and shaking hands with a PLWH (4). The belief that HIV is punishment for engaging in sex out of wedlock was rejected equally by both sexes (4).
Three studies (in Kenya, Uganda and the Bahamas) reported that males more accurately identified HIV-related transmission and prevention myths. Nabunya and colleagues found that males were less likely to agree with the myth that HIV can be transmitted from a mosquito bite (p < 0.01), or from using the same washing basin as a PLWH (11). Pinder-Butler found that males had more accurate information regarding HIV transmission by mosquito bites than females (p = 0.008) (19). In Kenya, sharing clothes with a person living with HIV was rejected as a mode of transmission by more males than females (p < 0.05) (4).
Three included studies reported that females were able to correctly identify HIV-related transmission and prevention myths. Mwamenda and colleagues report that more Kenyan females rejected the myth that mosquito bites led to HIV transmission (p < 0.001); taking care of a PLWH (p < 0.001), sharing food (p < 0.10) and sharing a cigarette (p < 0.05) were also rejected as modes of transmission by more females than males (p < 0.001) (4). Sharing syringes was discussed in one study, where the percentage of error was also lower among females (p < 0.001) (23). Percentage of error was lower among females for hugging a PLWH as a transmission mode (p = 0.018) (23). Nabunya and colleagues investigated HIV prevention knowledge among adolescent males and females in Uganda; females were more likely than males to reject the myth that using birth control pills can protect a woman from HIV infection (p = 0.02) (11).
Facts
Several studies reported results for individual questions regarding sexual intercourse as a mode of transmission (4, 11). One study reported no differences in identifying sex with a PLWH as a mode of transmission (4). One study included questions regarding HIV transmission from mother-to-child and found no gender differences in knowledge (11). Four studies (in Nigeria, Uganda, Kenya and Brazil) found that males had more accurate knowledge of true transmission modes and prevention strategies. Oyo-Ita and colleagues reported that Nigerian males were more knowledgeable than females in identifying sex as a mode of transmission (p = 0.00) (18). In Uganda, males were more likely to report accurate prevention attitudes, for example, acknowledgement that HIV impacts health (p = 0.01), and that it is appropriate to use a condom even with a known partner (p = 0.05) (11). Goncalves et al. reported a lower percentage of error among Brazilian males in identifying homosexual intercourse as an HIV transmission mode (p = 0.019) (23). Only one study, from Brazil, reported higher scores among females related to accurate identification of HIV- transmission modes (23). Goncalves and colleagues reported a lower percentage of error among females in identifying heterosexual intercourse as a mode of HIV-transmission (p < 0.001) (23).
Behaviors, beliefs and attitudes
Outcomes related to participant beliefs and attitudes were included as an exploratory measure, as beliefs and attitudes related to HIV are influenced by overall knowledge. Five of the included studies evaluated participants' beliefs, behaviors and attitudes regarding HIV. Mwamwenda and colleagues reported that females surveyed in Kenya more commonly believed that (presumably unsafe) sexual relationships with PLWH should be avoided (p < 0.001), and believed themselves to have less of a chance of contracting HIV than males (p < 0.001) (4). However, males more commonly reported taking action to avoid relationships for fear of HIV transmission (p < 0.10) (4). More females supported the idea that children living with HIV should attend school with children without HIV (p < 0.01) (4). More females reported no problems sharing a bed with a PLWH (p < 0.001); interestingly, more males reported feeling comfortable sitting next to a PLWH (p < 0.05) (4).
Nabunya and colleagues found that Ugandan males were more likely to think one should use a condom even if you know your partner well (p = 0.05) (11). In contrast, Lal and colleagues reported that more Indian females believed that sexual contact with a familiar person was risk-free, and that banning commercial sex work could control the spread of HIV; however, no statistical tests were conducted to estimate this difference (13). Maswanya and colleagues reported that Tanzanian males more commonly believed that their friends were at greater risk of HIV than themselves (OR: 1.56; 95% CI: 1.21–2.02) (25).
Discussion
This review identified 15 articles on gender differences in HIV knowledge among adolescents and young people in LMIC. Articles included in this review discuss adolescent knowledge between the ages of 11 and 24, a large age range that represents significant growth and development. Importantly, HIV-related knowledge may evolve as the individual progresses through the adolescent and young adult lifespan. We reviewed findings with respect to overall knowledge, facts vs. myths, and beliefs, behaviors and attitudes. We found that males were consistently found to be more knowledgeable about HIV than females when evaluated through a composite overall score (Table 3). When topics were broken down by question or literacy topic, there was variation in the findings, making it challenging to draw topic-specific conclusions. These findings highlight a critical need for HIV education programs for adolescents to assess knowledge not only broadly but by specific key topics. These key topics include myths and facts about HIV transmission and prevention and sexual decision-making, in which males more commonly reported higher knowledge.
Regarding attitudes and behaviors related to HIV, there were concerning findings among females (4, 11, 13, 25). Females were less likely to perceive themselves at risk of contracting HIV, were less careful in avoiding unsafe sex with PLWH, were more likely to believe that sexual contact with a familiar person was low risk (13) and had poorer prevention attitudes regarding condom use (15). For adolescent girls, these findings represent a discrepancy between risk perception and HIV prevalence, as women and girls are much often at higher risk of acquiring HIV than their male counterparts (26, 27). Besides the female physiological vulnerability to sexually transmitted infections (28, 29), higher HIV risk and exposure among women and girls are influenced by gender norms that place them at increased risk. These norms include less access to formal and informal education (including HIV education) (27, 30, 31), early marriage (32, 33) and transactional and intergenerational sex (34–38).
Furthermore, in places where the predominant and most accessible prevention tool is the male condom, girls have limited ability to protect their sexual health, particularly in communities in which males hold more decision-making power regarding condom use. Use and adherence to biomedical HIV prevention strategies, like pre-exposure prophylaxis (PrEP) remains low in LMIC, often because of cost, access, and HIV-related stigma (39). Our findings and those of prior studies support a feminist approach to HIV prevention and relevant education for female adolescents, given their gender-based social vulnerabilities to HIV infection.
Our review identified two interventional studies that reported improvements in general knowledge, clinical knowledge and prevention attitudes regarding HIV. Both studies reported less of an interventional impact among girls (11, 12). These data are important as previous studies have demonstrated that correct knowledge regarding HIV is a powerful mechanism in the promotion of positive attitudes and engagement in safe-sexual practices; programs have focused on transmission knowledge as a means of counteracting misconceptions that lead to risk-taking behavior (40–42).
Limitations
Our study had some limitations. First, this review was limited to findings from only 15 studies in LMICs, which limits its generalizability to all LMICs. However, it highlights gaps in the geographical scope of research on gender-based evaluation of HIV knowledge among young people in the most high-burden settings. Furthermore, it identifies the knowledge areas of most concern in HIV knowledge by gender, as reported from currently available research. Second, the studies included were quite heterogeneous in design, and did not allow for a more uniform means of analysis. However, we were able to categorize all study findings across three major cross-cutting domains (Overall Knowledge; Myths and Facts; and Beliefs, Behaviors, and Attitudes). Third, across included studies, there were no in-depth assessments of HIV knowledge that took into account the level of formal education for individuals or for male vs. female sub-groups. Fourth, none of the studies meeting inclusion criteria evaluated HIV-related knowledge among sexual and gender minority adolescent groups—who are also highly vulnerable to HIV infection, and experience intense stigma and discrimination. Finally, the studies discussed include adolescents from 11 to 24 years, a broad age range with significant variation in growth and development. Future analyses should consider the differences in HIV knowledge within shorter developmental periods.
Conclusion
This majority of studies included in this review found that males are generally more knowledgeable about HIV than females, particularly regarding transmission and prevention. There was significant variation in topic-specific findings, so further research is needed to better understand topic-specific nuances in HIV-related knowledge, and gender norms that perpetuate gender-based gaps in HIV knowledge and decision-making power. For HIV prevention to be successful, LMICs with a high burden of HIV should integrate comprehensive HIV education into schools, clinics and other settings in which adolescents spend a significant amount of time. While there is significant evidence on the social and cultural contexts that lead girls and young women to be at particularly high risk of HIV infection, there remains a gap in knowledge of the roles boys and young men play in this continuum. Future research should consider interventions that facilitate discussion between adolescent boys and girls and how to address these gender dynamics effectively.
Author contributions
AC and RV: designed the review. RV, JW, NS-A and KB: provided content expertise. AC and EG: conducted the search and served as primary reviewers while GC resolved conflicts. AC: drafted the manuscript and all authors reviewed and provided revisions to the draft. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. UNFPA. Motherhood in childhood: facing the challenge of adolescent pregnancy, state of the world population report (2013).
2. Casey BJ, Jones RM, Hare TA. The adolescent brain. Ann N Y Acad Sci. (2008) 1124:111–26. doi: 10.1196/annals.1440.010
3. Choudhury S, Blakemore S-J, Charman T. Social cognitive development during adolescence. Soc Cogn Affect Neurosci. (2006) 1(3):165–74. doi: 10.1093/scan/nsl024
4. Mwamwenda TS. HIV/AIDS knowledge and gender differences among high school students in Nairobi, Kenya. Mediterr J Soc Sci. (2014) 5(27):645–54. doi: 10.5901/mjss.2014.v5n27p645
5. Kamala BA. editor knowledge, attitudes and practices on HIV prevention among secondary school students in Bukoba Rural, Kagera Region-Tanzania (2010).
6. Slogrove AL, Sohn AH. The global epidemiology of adolescents living with HIV: time for more granular data to improve adolescent health outcomes. Curr Opin HIV AIDS. (2018) 13(3):170–8. doi: 10.1097/COH.0000000000000449
7. Mabaso M, Maseko G, Sewpaul R, Naidoo I, Jooste S, Takatshana S, et al. Trends and correlates of HIV prevalence among adolescents in South Africa: evidence from the 2008, 2012 and 2017 South African national HIV prevalence, incidence and behaviour surveys. AIDS Res Ther. (2021) 18(1):97. doi: 10.1186/s12981-021-00422-3
8. Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. (2015) 4(1):1. doi: 10.1186/2046-4053-4-1
9. Fantom NJ, Serajuddin U. The world bank’s classification of countries by income. World Bank Policy Res Work Pap. (2016) 7528.
10. Babineau J. Product review: covidence (systematic review software). J Can Health Libr Assoc. (2014) 35(2):68–71. doi: 10.5596/c14-016
11. Nabunya P, Byansi W, Muwanga J, Damulira C, Brathwaite R, Namuwonge F, et al. Gender, HIV knowledge and prevention attitudes among adolescents living with HIV participating in an economic empowerment intervention in Uganda. AIDS Care. (2021) 33(7):888–96. doi: 10.1080/09540121.2020.1844860
12. Jahanfar S, Lim AW, Loh MA, Yeoh AG, Charles A. Improvements of knowledge and perception towards HIV/AIDS among secondary school students after two hours talk. Med J Malaysia. (2008) 63(4):288–92.19385486
13. Lal SS, Vasan RS, Sarma PS, Thankappan KR. Knowledge and attitude of college students in Kerala towards HIV/AIDS, sexually transmitted diseases and sexuality. Natl Med J India. (2000) 13(5):231–6.11190050
14. Mahat G, Scoloveno MA. HIV/AIDS knowledge, attitudes and beliefs among Nepalese adolescents. J Adv Nurs. (2006) 53(5):583–90. doi: 10.1111/j.1365-2648.2006.03758.x
15. Maswanya ES, Moji K, Horiguchi I, Nagata K, Aoyagi K, Honda S, et al. Knowledge, risk perception of AIDS and reported sexual behaviour among students in secondary schools and colleges in Tanzania. Health Educ Res. (1999) 14(2):185–96. doi: 10.1093/her/14.2.185
16. Oljira L, Berhane Y, Worku A. Assessment of comprehensive HIV/AIDS knowledge level among in-school adolescents in eastern Ethiopia. J Int AIDS Soc. (2013) 16(1):17349. doi: 10.7448/IAS.16.1.17349
17. Othman SM. Knowledge about HIV/AIDS among high school students in Erbil city/Iraq. Glob J Health Sci. (2015) 7(1):16–23. doi: 10.5539/gjhs.v7n1p16
18. Oyo-Ita A, Ikpeme B, Etokidem A, Offor J, Okokon E, Etuk S. Knowledge of HIV/AIDS among secondary school adolescents in Calabar-Nigeria. Ann Afr Med. (2005) 4 (1):4.
19. Pinder-Butler S, Frankson MA, Hanna-Mahase C, Roberts R. HIV/AIDS knowledge and sexual behaviour among junior high school students in new providence, Bahamas. West Indian Med J. (2013) 62(4):318–22. doi: 10.7727/wimj.2013.169
20. Savaser S. Knowledge and attitudes of high school students about AIDS: a Turkish perspective. Public Health Nurs. (2003) 20(1):71–9. doi: 10.1046/j.1525-1446.2003.20110.x
21. Sekera JC, Preis J, Pazdiora P. Health literacy on HIV infection among adolescents in the Czech republic: a case study of two Czech cities plzeň and České budějovice. Epidemiol Mikrobiol Imunol. (2020) 69(4):182–8.33445942
22. Zhao Q, Li X, Stanton B, Mao R, Wang J, Zhong L, et al. HIV/AIDS awareness and knowledge among secondary school students in China. World Health Popul. (2010) 11(4):38–48. doi: 10.12927/whp.2010.21762
23. Gonçalves H, González-Chica DA, Menezes AM, Hallal PC, Araújo CL, Dumith SC. HIV/AIDS transmission knowledge among adolescents aged 11 years from southern Brazil. Rev Bras Epidemiol. (2013) 16(2):420–31. doi: 10.1590/S1415-790X2013000200017
24. Shamu S, Khupakonke S, Farirai T, Slabbert J, Chidarikire T, Guloba G, et al. Knowledge, attitudes and practices of young adults towards HIV prevention: an analysis of baseline data from a community-based HIV prevention intervention study in two high HIV burden districts, South Africa. BMC Public Health. (2020) 20(1):1249. doi: 10.1186/s12889-020-09356-3
25. Maswanya ES, Moji K, Aoyagi K, Takemoto T. Sexual behavior and condom use in female students in Dar-es-Salaam, Tanzania: differences by steady and casual partners. East Afr J Public Health. (2011) 8(2):69–76.22066289
27. Dellar RC, Dlamini S, Karim QA. Adolescent girls and young women: key populations for HIV epidemic control. J Int AIDS Soc. (2015) 18(2 Suppl 1):19408. doi: 10.7448/IAS.18.2.19408
28. El-Bassel N, Caldeira NA, Ruglass LM, Gilbert L. Addressing the unique needs of African American women in HIV prevention. Am J Public Health. (2009) 99(6):996–1001. doi: 10.2105/AJPH.2008.140541
29. Bond KT, Chandler R, Chapman-Lambert C, Jemmott LS, Lanier Y, Cao J, et al. Applying a nursing perspective to address the challenges experienced by cisgender women in the HIV status neutral care continuum: a review of the literature. J Assoc Nurses AIDS Care. (2021) 32(3):283–305. doi: 10.1097/JNC.0000000000000243
30. Fasil N, Worku A, Oljira L, Tadesse AW, Berhane Y. Association between sexual and reproductive health education in peer group and comprehensive knowledge of HIV among adolescent girls in rural eastern Ethiopia: a community-based cross-sectional study. BMJ Open. (2022) 12(10):e063292. doi: 10.1136/bmjopen-2022-063292
31. Saul J, Bachman G, Allen S, Toiv NF, Cooney C, Beamon T. The DREAMS core package of interventions: a comprehensive approach to preventing HIV among adolescent girls and young women. PLoS One. (2018) 13(12):e0208167. doi: 10.1371/journal.pone.0208167
32. Raj A, Salazar M, Jackson EC, Wyss N, McClendon KA, Khanna A, et al. Students and brides: a qualitative analysis of the relationship between girls’ education and early marriage in Ethiopia and India. BMC Public Health. (2019) 19(1):19. doi: 10.1186/s12889-018-6340-6
33. Melesse DY, Cane RM, Mangombe A, Ijadunola MY, Manu A, Bamgboye E, et al. Inequalities in early marriage, childbearing and sexual debut among adolescents in sub-Saharan Africa. Reprod Health. (2021) 18(Suppl 1):117. doi: 10.1186/s12978-021-01125-8
34. Glynn JR, Caraël M, Auvert B, Kahindo M, Chege J, Musonda R, et al. Why do young women have a much higher prevalence of HIV than young men? A study in Kisumu, Kenya and Ndola, Zambia. AIDS. (2001) 15:s5–s60. doi: 10.1097/00002030-200108004-00006
35. Gregson S, Nyamukapa CA, Garnett GP, Mason PR, Zhuwau T, Caraël M, et al. Sexual mixing patterns and sex-differentials in teenage exposure to HIV infection in rural Zimbabwe. Lancet. (2002) 359(9321):1896–903. doi: 10.1016/S0140-6736(02)08780-9
36. Wamoyi J, Wight D, Plummer M, Mshana GH, Ross D. Transactional sex amongst young people in rural northern Tanzania: an ethnography of young women’s motivations and negotiation. Reprod Health. (2010) 7:2. doi: 10.1186/1742-4755-7-2
37. Dunkle KL, Jewkes RK, Brown HC, Gray GE, McIntryre JA, Harlow SD. Transactional sex among women in Soweto, South Africa: prevalence, risk factors and association with HIV infection. Soc Sci Med. (2004) 59(8):1581–92. doi: 10.1016/j.socscimed.2004.02.003
38. Comins CA, Rucinski KB, Baral S, Abebe SA, Mulu A, Schwartz SR. Vulnerability profiles and prevalence of HIV and other sexually transmitted infections among adolescent girls and young women in Ethiopia: a latent class analysis. PLoS One. (2020) 15(5):e0232598. doi: 10.1371/journal.pone.0232598
39. Cáceres CF, Borquez A, Klausner JD, Baggaley R, Beyrer C. Implementation of pre-exposure prophylaxis for human immunodeficiency virus infection: progress and emerging issues in research and policy. J Int AIDS Soc. (2016) 19(7(Suppl 6)):21108. doi: 10.7448/IAS.19.7.21108
40. Plautz A, Meekers D. Evaluation of the reach and impact of the 100% Jeune youth social marketing program in Cameroon: findings from three cross-sectional surveys. Reprod Health. (2007) 4(1). doi: 10.1186/1742-4755-4-1
41. Lydiè N, Robinson NJ, Ferry B, Akam E, De Loenzien M, Zekeng L, et al. Adolescent sexuality and the HIV epidemic in Yaoundé, Cameroon. J Biosoc Sci. (2004) 36(5):597–616. doi: 10.1017/S002193200300631X
Keywords: HIV, gender, knowledge, low and middle-income countries, adolescent
Citation: Chory A, Gillette E, Callen G, Wachira J, Sam-Agudu NA, Bond K and Vreeman R (2023) Gender differences in HIV knowledge among adolescents and young people in low-and middle-income countries: a systematic review. Front. Reprod. Health 5:1154395. doi: 10.3389/frph.2023.1154395
Received: 30 January 2023; Accepted: 12 June 2023;
Published: 26 June 2023.
Edited by:
Mudit Tyagi, Thomas Jefferson University, United StatesReviewed by:
Don Des Jarlais, New York University, United StatesMelkamu Merid Mengesha, Arba Minch University, Ethiopia
© 2023 Chory, Gillette, Callen, Wachira, Sam-Agudu, Bond and Vreeman. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ashley Chory YXNobGV5LmNob3J5QG1zc20uZWR1
 Ashley Chory
Ashley Chory Emma Gillette1
Emma Gillette1 Nadia A. Sam-Agudu
Nadia A. Sam-Agudu Rachel Vreeman
Rachel Vreeman