- Department of Health Sciences, University of York, York, England
Background: The relationship between SRH and mental health among men is not well documented, especially in the 10–24 age group. This scoping review aimed to investigate what is known about the association between SRH and mental health among young men (10–24) in LMICs.
Methods: Embase, APA PsycInfo, MEDLINE(R) ALL, ASSIA and the Cochrane Library of Database of Systematic Reviews were searched from the year of establishment up to August 2022. The review was reported using the PRISMA-ScR checklist.
Results: A total of (n = 2636) studies were identified from the five databases. After the completion of screening, only ten studies (n = 8 cross-sectional, n = 1 mixed methods and n = 1 qualitative) met the eligibility criteria and were included in the review. The findings suggest that there is a reciprocal relationship between mental health and SRH. Sperm concentration and total sperm count were found to be lower in depressed men. Poor mental health was associated with early sexual debut, higher rates of sexual activity and an increased number of sexual partners. Poor mental health was also found among men who had sex with men (MSM). In addition, we found a relationship between sexual abuse, sexual coercion and poor mental health.
Conclusion: The findings of this unique study indicate that poor mental health is associated with poor SRH outcomes and vice versa among young men (10–24) living in LMICs. However, further research will be needed to establish the temporal relationship between SRH and mental health outcomes.
1. Introduction
Sexual and reproductive health (SRH) needs of adolescent boys and young men (aged 10–24) often remain unmet due to issues such as limited use of SRH services, reluctance to seek help as well as poor access to services (1). Sexual and reproductive health rights (SRHR) for all are enshrined in 2030 Sustainable Development Goals agenda in SDGs (3.7, 4.7 and 5.6) (2). However, the majority of SRH research has focused upon health outcomes for girls and women (3) and males have not always been prioritised (4).
The limited research on the sexual and reproductive health of young men (3) largely focusses on HIV and sexually transmitted diseases. Globally, 16.8 million men are known to be living with HIV (5) and the age-standardized incidence rates of syphilis, chlamydia, gonorrhoea, and trichomoniasis are higher in males compared to females (6).
Depression and anxiety were reported to be among the top ten leading causes of the global disease burden in the 10–24 year age group (7). Although anxiety and depression rates are reported to be lower in males (13%) compared to females (20%), suicide rates in males are much higher (8). The age-standardized suicide rate for males in 2019 was 12.6 per 100,000 when compared to 5.4 per 100,000 for females (9). Approximately 77% of these deaths occurred in low-and-middle-income countries (LMICs) (9). The actual burden of mental ill health and the suicide rates in LMICs may differ due to the scarcity of empirical evidence and misclassification of deaths (9, 10). Seeking help for mental health conditions is often stigmatized in men and adolescent males (11) and may impact reporting. In addition, the majority of research on adolescents originates from high-income countries (12). Considering that around half of the population of the world is aged younger than 25 and that 90% of 10–24 year olds live in LMICs (13), this is a significant public health problem.
Although a relationship has been shown between poor mental health and sexual behaviour, such as men self-medicating using alcohol or other substances during emotional distress leading to risky sexual behaviours (5, 8, 14, 15), to the best of our knowledge no previous review has explored the association between sexual and reproductive health and mental health among young men in LMICs. Furthermore, evidence indicates that adolescents growing up in regions with higher levels of income inequality have a wide spectrum of poor health outcomes (16) which suggests that adolescent males growing up in LMICs with high levels of income inequality are at risk of experiencing poor sexual and reproductive health and mental health outcomes. Therefore, engaging males should be an important component in all programmes as it has the potential to improve the SRH and mental health of all young people (17).
Thus, considering that there is a paucity of literature on the SRH of young men and that there is potentially underreporting of mental health issues in LMICs, the interaction between these two key issues is unclear, particularly in the 10–24-year age group. To understand the potential association between SRH and mental health for young men, a scoping review (18) was conducted.
2. Methods
A preliminary search via Ovid on AMED, Embase, Ovid MEDLINE, APA PsycInfo and Google Scholar with the search terms “scoping review”, “systematic review”, “sexual health”, “reproductive health” and “mental health” was conducted to search for existing scoping or systematic reviews on the topic. There were no reviews examining the association between SRH and mental health other than one focused on women (19).
The Arksey and O’Malley framework for scoping was employed (18). The framework has five stages: (i) identifying the research question; (ii) identifying relevant studies; (iii) study selection; (iv) charting the data; and (v) collating, summarizing and reporting the results. To further strengthen the methodological rigour, the review was reported using the PRISMA-ScR checklist (20) (Supplementary Table 1). The research question was developed using the (21) framework which specified the concept, the population, and important outcomes of interest in this review. In addition, eligibility criteria were developed around the research question.
Case studies, commentaries, letters, conference abstracts and studies that were not in English were excluded. Studies were also excluded if the female population was more than 50% and if there was no association reported between SRH and mental health so that the focus of the review was maintained. To ensure that the search strategy captured a wider geographical landscape, EPOC LMIC filters were utilised to search for articles (22). However, considering that the EPOC LMIC filter list has not been recently updated, all high-income countries as per World Bank 2023 fiscal year classification (23) were removed from the list before running the search strategy. A modified two-step search strategy was then used to search for relevant articles (24). Initially, a circumscribed search was conducted on Embase and CINAHL Complete and terms contained in the titles and abstracts from the search results were analysed and used in the second step of the search strategy.
Using the initial search terms, a comprehensive search was performed on Embase, APA PsycInfo, MEDLINE(R) ALL, ASSIA and the Cochrane Library Database of Systematic Reviews up to 8 August 2022. The search results were imported into Covidence where the titles and abstracts were screened by one reviewer with a 10% random selection independently screened by two further reviewers. The following search terms were used in different combinations and adapted for each database.
• (“Reproductive health”) (“Sexual health”) OR (sexual reproductive health) OR (reproductive NEAR/2 service*) OR (reproductive health care)
• (“Mental health”) OR (mental health) OR (psychological health) OR (psychological well-being) OR (psychiatric health) OR (mental disorders) OR (mental disease)
• Juvenile OR (“Adolescents”) OR adolesce* OR teen* (“Young adults”) OR (young adulthood) OR (young pe*)
• Men OR boy* OR male* OR (male pe*)
• (LMIC) OR (low NEAR/3 countr*) OR (insert modified EPOC LMIC FILTER LIST)
• (“Reproductive health”) (“Sexual health”) OR (sexual reproductive health) OR (reproductive NEAR/2 service*) OR (reproductive health care) AND (“Mental health”) OR (mental health) OR (psychological health) OR (psychological well-being) OR (psychiatric health) OR (mental disorders) OR (mental disease) AND juvenile OR (“Adolescents”) OR adolesce* OR teen* (“Young adults”) OR (young adulthood) OR (young pe*) AND men OR boy* OR male* OR (male pe*) AND (LMIC) OR (low NEAR/3 countr*) OR (insert modified EPOC LMIC filter list)
Key information was charted in a Microsoft Word document which included the following headings: author(s), year of publication, type of publication, country/region, aims/purpose, population, outcomes, methods of measurement and key findings that related to the scoping review question. Analysis of the results utilised a three step process: (i) analysing the data; (ii) reporting the results; and (iii) applying meaning to the results (25). The findings were presented with respect to the research question and the objectives of the scoping review using graphs, figures, and tables where applicable.
3. Results
3.1. Study selection
A total of (n = 2,632) studies were identified from five databases. Altogether, (n = 1,154) studies were removed as duplicates whilst (n = 1,482) were progressed for screening. A further (n = 1,404) titles and abstracts were excluded, and (n = 78) studies were sought for retrieval. Only (n = 73) studies were assessed for full text eligibility and of these, (n = 63) were excluded following full text screening according to our eligibility criteria (Supplementary Table 2). Ten studies (26–35) met the inclusion criteria and were included in the review (see Figure 1).
3.2. Study characteristics
The included studies were from four LMIC regions (Sub-Saharan Africa, South Asia, East Asia Pacific and Latin America and the Caribbean). Four studies were from Uganda (26–29), one study was from India (34), one study was from China (35), one study was from Mexico (33), one study was from Nigeria (30), one study was from Eswatini (32) and one study was from Ivory Coast (31) (Supplementary Figure 1). Eight of the ten studies were cross-sectional studies, one utilised mixed method approaches (a cross-sectional study combined with a qualitative study), and one was a qualitative study.
3.3. Collating, summarizing and reporting the results
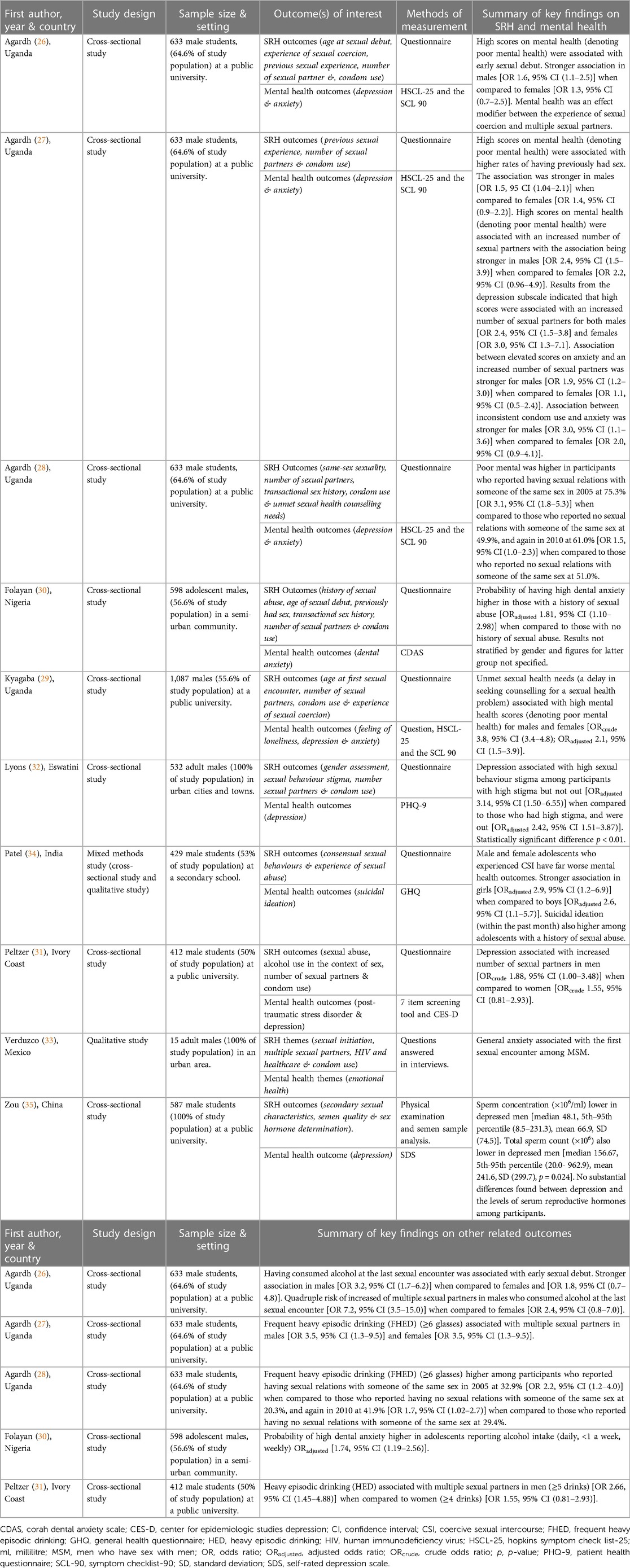
All studies included adolescents and young adults with 4,293 who defined themselves as male. Two studies included younger adolescent men (30, 34), one study focussed on college age students (35), and the remaining studies focussed on those aged 18–24. The phenomenon of interest in all the studies was the association between SRH (age at sexual debut, sexual coercion, previous sexual experience, number of sexual partners, condom use, transactional sex history, unmet sexual health counselling needs, gender assessment, sexual behaviour stigma, alcohol use in the context of sex, sexual initiation, HIV and healthcare, secondary sexual characteristics, sex hormone determination and same-sex sexuality) and mental health (anxiety, depression, post-traumatic stress disorder, suicidal ideation, emotional health) (Supplementary Figure 2). There were differences in the type of SRH and mental health outcomes included as well as in the method of measurements used to assess these outcomes. In addition, some studies reported on more than one of the SRH and mental health outcomes.
Four studies used the Hopkins Symptom Check List-25 (HSCL-25) developed by (36) and the Symptom Checklist-90 (SCL-90) developed by (37) to measure mental health outcomes (anxiety and depression) (26–29). One study used the Corah Dental Anxiety Scale to measure dental anxiety (30), whilst the others used the Patient Health Questionnaire (PHQ-9) to measure depression (32), the General Health Questionnaire (GHQ) to assess mental health (34), the Center for Epidemiologic Studies Depression scale (CES-D) to measure depression (31) and the Self-rated Depression Scale (SDS) to measure depressive symptoms (35). One study included outcomes on post-traumatic stress disorder (PTSD) and measured the outcome using a 7-item screening tool (31). Eight studies used a self-reported questionnaire to measure SRH and mental health outcomes (26–32, 34). One study conducted qualitative interviews with the participants (33) whilst another study incorporated focus group discussions as part of a mixed methods study (34). Additionally, one study used a physical examination (to assess secondary sexual characteristics) and a diagnostic test (to assess semen quality) as a method of measurement (35).
Characteristics of the included studies outlining the key findings are shown in Table 1.
4. Discussion
4.1. Key findings
The scoping review aimed to investigate what is known about the association between SRH and mental health of young men aged 10–24 in LMICs. Findings suggest there is a reciprocal interaction between mental health and SRH. In particular, sperm concentration and total sperm count was lower in depressed men (35). Poor mental health was associated with early sexual debut (26), higher rates of having previously had sex and an increased number of sexual partners (27). Depression and anxiety specifically, were also associated with an increased number of sexual partners (27, 31), and anxiety was also associated with inconsistent condom use (27).
The interaction between mental health and sexual abuse was also highlighted. Dental anxiety was associated with a history of sexual abuse (30) and adolescent males who experienced coercive sexual intercourse experienced poor mental health. Furthermore, suicidal ideation increased among those male adolescents with a history of sexual abuse (34). Findings further suggest that a delay in seeking counselling for a sexual health problem was associated with poor mental health (29). Our results also indicate that alcohol use at the last sexual encounter was associated with multiple sexual partners (26, 27, 31).
4.2. Comparison to current literature
The association between semen quality and poor mental health was consistent with findings from (38, 39). These studies found that sperm concentration and sperm count were lower in males who were experiencing depression and anxiety. Although the findings from the review suggest that there were no differences between depression and the levels of serum reproductive hormones, this was contradicted by the (38) study which found that testosterone levels were lower in men who experience anxiety and depression.
The relationship between poor mental health, early sexual debut and the experience of having previously had sex was consistent with findings from previous studies (40, 41). Kastbom (41) found that adolescent boys who reported symptoms of depression and anxiety had a higher likelihood of experiencing early sexual debut [OR 2.63, 95% CI (1.64–4.29)] when compared to adolescent boys who reported no symptoms of depression and anxiety. Similarly, Meier (40) found that adolescents who had early sexual debut and split up with their partner had a higher likelihood of experiencing depressive symptoms.
The correlation between poor mental health and increased number of sexual partners among males was consistent with findings from (42). The study found that adolescents with psychiatric problems particularly those who were in the “mania” category had a higher probability of reporting two or more sexual partners [OR 3.2, 95% CI (1.1–9.5)]. Although the results in this study were not stratified by gender.
The relationship between alcohol and sexual behaviours has been documented before and that men are more likely to self-medicate using alcohol or other substances when experiencing mental health problems (8). Furthermore (43), found that participants who abused alcohol were more likely to report higher levels of depressive or additional psychiatric symptoms. Previous studies have documented the link between SRH and alcohol (44, 45). Further research would be required to establish the causal relationship between alcohol abuse, SRH and poor mental health.
SRH legislation and policies also impact on mental health. For instance, there are 67 United Nations member states that criminalise private consensual same-sex acts among adults (31 in Africa, 9 in Latin America and the Caribbean, 22 in Asia and 6 in Oceania) (46). The concern is that the SRH needs of MSM remain unmet which will potentially lead poor mental health outcomes. According to (47), the health needs of men who have sex with men (MSM) are often disregarded in regions where homosexuality is forbidden. In addition, the criminalisation of same-sex acts has been found to be associated with higher levels of perceived sexual stigma (48). Our findings suggest that poor mental health was higher in MSM and that depression was significantly higher in males who experienced sexual behaviour stigma (28, 32). In addition, the first sexual encounter among MSM was linked to anxiety (33). This could partially explain why we found that frequent heavy episodic drinking was higher among MSM (28).
4.3. Strengths and limitations
The review was conducted with rigour and was reported using the PRISMA-ScR checklist. Developing comprehensive search strategies and using two additional reviewers to pilot the rigorous eligibility criteria enhanced the credibility of the results. To our knowledge, this is the first review to map out the association between SRH and mental health among young men in LMICs. Considering that the included studies are from four LMIC regions, this enabled a study of a relatively heterogenous population.
Although the results point to the fact that poor mental health is associated with poor SRH outcomes and vice versa, it was difficult to separate temporality. This was due to the study designs of the included studies. Causality cannot be inferred because of the absence of temporal elements particularly in cross-sectional study designs (49). Therefore, we cannot ascertain the direction of the association between SRH and mental health which is limitation of this study. Additionally, the exclusion of grey literature and studies not in English implies that some studies meeting the eligibility criteria may have been missed. Finally, the different mental health measurement tools made it difficult to make comparisons between studies and could have led to an overestimation or underestimation of the reported mental health symptoms. Thus, these findings need to be interpreted with caution.
4.4. Implications for research and practice
The findings confirm a paucity of studies investigating the link between SRH and mental health in men. This hinders the understanding of the dynamic interaction between these important issues. Consequently, there is a need for well-designed studies that will map the temporal association between SRH and mental health among young men.
Most young adults in LMICs have limited or no access to SRH education and services (50). In addition, evidence suggests that adolescent males are less aware of mental health services (51). Lack of access to information about SRH and mental health may potentially act as a barrier and hamper adolescent males’ ability to acknowledge their need to access SRH and mental health services. Therefore, there is a need for more research on intervention strategies that can be employed to mitigate this challenge.
Although there was heterogeneity in the location of the studies, 70% occurred in an education setting with students. These study populations may not be a true representation of the population of young men in LMICs considering that those not enrolled in educational institutions will be excluded. Therefore, there is a compelling need to conduct further research in different contexts and with diverse populations. Future studies should ensure that data on SRH and mental health is collected at national levels across LMICs. This research could be key in informing national SRH and mental health policy.
5. Conclusion
The findings of our review suggest that poor mental health is associated with poor SRH outcomes and that poor SRH outcomes are associated with poor mental health among young men (10–24) living in LMICs. Further research is needed to establish any causal relationship between the different SRH and mental health outcomes and should include a wide range of participants.
Author contributions
AMJ designed and supervised the study and contributed to writing and editing the draft. SM conducted the study and wrote the first draft. KF co-supervised the study and contributed to the draft. All authors agree to be accountable for the content of the work. All authors contributed to the article and approved the submitted version.
Funding
AMJ and KF are funded by the University of York.
Acknowledgments
We would like to thank David Brown, Academic Liaison Librarian for Health Sciences, Psychology, SPSW, Lifelong Learning and CRD at the University of York for his assistance and expertise with peer reviewing our search strategies.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frph.2023.1119407/full#supplementary-material
References
1. Ippf U. Global sexual and reproductive health package for men and adolescent boys,. London: IPPF and New York: UNFPA (2017).
3. Saewyc EM. What about the boys? The importance of including boys and young men in sexual and reproductive health research. J Adolesc Health. (2012) 51:1–2. doi: 10.1016/j.jadohealth.2012.05.002
4. Varga CA. The forgotten fifty per cent: a review of sexual and reproductive health research and programs focused on boys and young men in Sub-Saharan Africa. Afr J Reprod Health. (2001) 5:175–95. doi: 10.2307/3583334
5. Jahagirdar D, Walters MK, Novotney A, Brewer ED, Frank TD, Carter A, et al. Global, regional, and national sex-specific burden and control of the HIV epidemic, 1990–2019, for 204 countries and territories: the global burden of diseases study 2019. The Lancet HIV. (2021) 8:633–51. doi: 10.1016/S2352-3018(21)00152-1
6. Du M, Yan W, Jing W, Qin C, Liu Q, Liu M, et al. Increasing incidence rates of sexually transmitted infections from 2010 to 2019: an analysis of temporal trends by geographical regions and age groups from the 2019 global burden of disease study. BMC Infect Dis. (2022) 22:1–16. doi: 10.1186/s12879-021-07004-8
7. Abbafati C, Abbas KM, Abbasi-Kangevari M, Abd-Allah F, Abdelalim A, Abdollahi MA, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet. (2020) 396:1204–22. doi: 10.1016/S0140-6736(20)30925-9
8. Gough B, Novikova I. Mental health, men and culture: How do sociocultural constructions of masculinities relate to men’s mental health help-seeking behaviour in the WHO European region? Geneva: World Health Organization (2020).
10. Rehm J, Shield KD. Global burden of disease and the impact of mental and addictive disorders. Curr Psychiatry Rep. (2019) 21:1–10. doi: 10.1007/s11920-019-0997-0
11. Swann C, Telenta J, Draper G, Liddle S, Fogarty A, Hurley D, et al. Youth sport as a context for supporting mental health: adolescent male perspectives. Psychol Sport Exerc. (2018) 35:55–64. doi: 10.1016/j.psychsport.2017.11.008
12. Blum R, Boyden J. Understand young people in low-income countries. Nature. (2018) 554:435–7. doi: 10.1038/d41586-018-02107-w
13. Morris JL, Rushwan H. Adolescent sexual and reproductive health: the global challenges. Int J Gynaecol Obstet. (2015) 131:40–2. doi: 10.1016/j.ijgo.2015.02.006
14. Ritchwood TD, Ford H, Decoster J, Lochman JE, Sutton M. Risky sexual behavior and substance use among adolescents: a meta-analysis. Child Youth Serv Rev. (2015) 52:74–88. doi: 10.1016/j.childyouth.2015.03.005
15. Allen J, Balfour R, Bell R, Marmot M. Social determinants of mental health. Int Rev Psychiatry. (2014) 26:392–407. doi: 10.3109/09540261.2014.928270
16. Odgers CL. Income inequality and the developing child: is it all relative? Am Psychol. (2015) 70:722–31. doi: 10.1037/a0039836
17. Desrosiers A, Betancourt T, Kergoat Y, Servilli C, Say L, Kobeissi L. A systematic review of sexual and reproductive health interventions for young people in humanitarian and lower-and-middle-income country settings. BMC Public Health. (2020) 20:1–21. doi: 10.1186/s12889-020-08818-y
18. Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. (2005) 8:19–32. doi: 10.1080/1364557032000119616
19. Montagnoli C, Zanconato G, Cinelli G, Tozzi AE, Bovo C, Bortolus R, et al. Maternal mental health and reproductive outcomes: a scoping review of the current literature. Arch Gynecol Obstet. (2020) 302:801–19. doi: 10.1007/s00404-020-05685-1
20. Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. (2018) 169:467–73. doi: 10.7326/M18-0850
21. Booth A, Noyes J, Flemming K, Gerhardus A, Wahlster P, Wilt GJVD, et al. Guidance on choosing qualitative evidence synthesis methods for use in health technology assessments of complex interventions. Bremen (DE): Integrate-HTA (2016).
22. Sutton A, Campbell F. The ScHARR LMIC filter: adapting a low- and middle-income countries geographic search filter to identify studies on preterm birth prevention and management. Res Synth Methods. (2022) 13:447–56. doi: 10.1002/jrsm.1552
24. Peters M, Godfrey C, Mcinerney P, Munn Z, Trico A, Khalil H. Chapter 11: scoping reviews (2020 version). JBI (2020). https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups
25. Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci. (2010) 5:1–9. doi: 10.1186/1748-5908-5-69
26. Agardh A, Odberg-Pettersson K, Östergren PO. Experience of sexual coercion and risky sexual behavior among Ugandan university students. BMC Public Health. (2011) 11:1–12. doi: 10.1186/1471-2458-11-527
27. Agardh A, Cantor-Graae E, Östergren PO. Youth, sexual risk-taking behavior, and mental health: a study of university students in Uganda. Int J Behav Med. (2012) 19:208–16. doi: 10.1007/s12529-011-9159-4
28. Agardh A, Ross M, Östergren PO, Larsson M, Tumwine G, Månsson SA, et al. Health risks in same-sex attracted Ugandan university students: evidence from two cross-sectional studies. PLoS One. (2016) 11:1–10. doi: 10.1371/journal.pone.0150627
29. Kyagaba E, Asamoah BO, Emmelin M, Agardh A. Unmet medical care and sexual health counseling needs-a cross-sectional study among university students in Uganda. J Health Care Poor Underserved. (2014) 25:1034–51. doi: 10.1353/hpu.2014.0135
30. Folayan MO, El Tantawi M, Aly NM, Adeniyi AA, Oziegbe E, Arowolo O, et al. Associations between a history of sexual abuse and dental anxiety, caries experience and oral hygiene status among adolescents in sub-urban south west Nigeria. BMC Oral Health. (2021) 21:1–10. doi: 10.1186/s12903-020-01362-6
31. Peltzer K, Pengpid S, Tiembre I. Mental health, childhood abuse and HIV sexual risk behaviour among university students in Ivory Coast. Ann Gen Psychiatry. (2013) 12:1–8. doi: 10.1186/1744-859X-12-18
32. Lyons C, Stahlman S, Holland C, Ketende S, Van Lith L, Kochelani D, et al. Stigma and outness about sexual behaviors among cisgender men who have sex with men and transgender women in Eswatini: a latent class analysis. BMC Infect Dis. (2019) 19:1–10. doi: 10.1186/s12879-019-3711-2
33. Verduzco IL. Barriers to sexual expression and safe sex among Mexican gay men: a qualitative approach. American Journal of Men’s Health. (2016) 10:270–84. doi: 10.1177/1557988314561490
34. Patel V, Andrew G. Gender, sexual abuse and risk behaviours in adolescents: a cross-sectional survey in schools in goa. Natl Med J India. (2001) 14:263–7.11767217
35. Zou P, Wang X, Sun L, Chen Q, Yang H, Zhou N, et al. Semen quality in Chinese college students: associations with depression and physical activity in a cross-sectional study. Psychosom Med. (2018) 80:564–72. doi: 10.1097/PSY.0000000000000595
36. Parloff MB, Kelman HC, Frank JD. Comfort, effectiveness, and self-awareness as criteria of improvement in psychotherapy. Am J Psychiatry. (1954) 111:343–52. doi: 10.1176/ajp.111.5.343
37. Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The hopkins symptom checklist (HSCL): a self-report symptom inventory. Behav Sci. (1974) 19:1–15. doi: 10.1002/bs.3830190102
38. Bhongade MB, Prasad S, Jiloha RC, Ray PC, Mohapatra S, Koner BC. Effect of psychological stress on fertility hormones and seminal quality in male partners of infertile couples. Andrologia. (2015) 47:336–42. doi: 10.1111/and.12268
39. Zorn B, Auger J, Velikonja V, Kolbezen M, Meden-Vrtovec H. Psychological factors in male partners of infertile couples: relationship with semen quality and early miscarriage. Int J Androl. (2008) 31:557–64. doi: 10.1111/j.1365-2605.2007.00806.x
40. Meier AM. Adolescent first sex and subsequent mental health. American Journal of Sociology. (2007) 112:1811–47. doi: 10.1086/512708
41. Kastbom ÅA, Sydsjö G, Bladh M, Priebe G, Svedin CG. Sexual debut before the age of 14 leads to poorer psychosocial health and risky behaviour in later life. Acta Paediatr. (2014) 104:91–100. doi: 10.1111/apa.12803
42. Brown LK, Hadley W, Stewart A, Lescano C, Whiteley L, Donenberg G, et al. Psychiatric disorders and sexual risk among adolescents in mental health treatment. J Consult Clin Psychol. (2010) 78:590–7. doi: 10.1037/a0019632
43. Miller BE, Miller MN, Verhegge R, Linville HH, Pumariega AJ. Alcohol misuse among college athletes: self-medication for psychiatric symptoms? J Drug Educ. (2002) 32:41–52. doi: 10.2190/JDFM-AVAK-G9FV-0MYY
44. Vasilenko SA, Lanza ST. Predictors of multiple sexual partners from adolescence through young adulthood. Journal of Adolescent Health. (2014) 55:491–7. doi: 10.1016/j.jadohealth.2013.12.025
45. Parnes JE, Rahm-Knigge RL, Conner BT. The curvilinear effects of sexual orientation on young adult substance use. Addict Behav. (2017) 66:108–13. doi: 10.1016/j.addbeh.2016.11.012
46. Mendos LR, Botha K, Lelis RC, López de la Peña E, Savalev I, & Tan D. State-sponsored homophobia: global legislation overview update. Switzerland: Geneva (2020).
47. Glasier A, Gülmezoglu AM, Schmid GP, Moreno CG, Van Look PFA. Sexual and reproductive health: a matter of life and death. Lancet. (2006) 368:1595–607. doi: 10.1016/S0140-6736(06)69478-6
48. Arreola S, Santos GM, Beck J, Sundararaj M, Wilson PA, Hebert P, et al. Sexual stigma, criminalization, investment, and access to HIV services among men who have sex with men worldwide. AIDS Behav. (2015) 19:227–34. doi: 10.1007/s10461-014-0869-x
49. Spector PE. Do not cross me: optimizing the use of cross-sectional designs. J Bus Psychol. (2019) 34:125–37. doi: 10.1007/s10869-018-09613-8
50. Feroz AS, Ali NA, Khoja A, Asad A, Saleem S. Using mobile phones to improve young people sexual and reproductive health in low and middle-income countries: a systematic review to identify barriers, facilitators, and range of mHealth solutions. Reprod Health. (2021) 18:1–13. doi: 10.1186/s12978-020-01059-7
Keywords: sexual and reproductive health, men’s health, mental health, adolescent, low and-middle-income countries, scoping review
Citation: Mhlongo S, Mason-Jones AJ and Ford K (2023) Sexual, reproductive and mental health among young men (10–24) in low-and-middle income countries: a scoping review. Front. Reprod. Health 5:1119407. doi: 10.3389/frph.2023.1119407
Received: 8 December 2022; Accepted: 6 November 2023;
Published: 4 December 2023.
Edited by:
Margaret Fitch, University of Toronto, CanadaReviewed by:
Subasri Narasimhan, Emory University, United States© 2023 Mhlongo, Mason-Jones and Ford. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Amanda J. Mason-Jones YW1hbmRhLm1hc29uLWpvbmVzQHlvcmsuYWMudWs=
 Siphiwe Mhlongo
Siphiwe Mhlongo Amanda J. Mason-Jones
Amanda J. Mason-Jones Keith Ford
Keith Ford