
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Reprod. Health , 17 July 2023
Sec. Reproductive Epidemiology
Volume 5 - 2023 | https://doi.org/10.3389/frph.2023.1113926
This article is part of the Research Topic Inequities and Disparities in Reproductive Health: Reproductive Epidemiology View all 10 articles
Background: Unintended pregnancy is one of the most serious health issues in low and Middle-Income Countries (LMICs), posing significant health, economic, and psychosocial costs to individuals and communities. However, there is limited evidence on the prevalence of unintended pregnancies and their determinants in LMICs. Hence, this study aimed to assess the prevalence of unintended pregnancy and its associated factors among childbearing-age women in LMICs.
Method: Data for the study were drawn from a recent 61 Demographic and Health Surveys (DHS) conducted in LMICs. A total sample of 187,347 mothers who gave birth in the five years preceding the survey was included. STATA version 16 was used to clean and analyze the data. Multilevel multivariable logistic regression was employed to identify individual and community-level factors of unintended pregnancy in LMICs. In the multivariable analysis, an adjusted odds ratio with a 95% confidence level was reported to indicate statistical association.
Results: The pooled magnitude of unintended pregnancy in LMICs was 26.46%% (95% CI: 25.30%, 27.62%), ranging from 19.25%% in Egypt to 61.71% in Bolivia. Working status (AOR = 1.03; 95% CI: 1.01, 1.06), having a husband with no education (AOR = 1.07; 95% CI: 1.00, 1.15), and primary education (AOR = 1.05; 95% CI: 1.01, 1.11), women from male-headed households (AOR = 1.04; 95% CI: 1.00, 1.08), media exposure (AOR = 1.05; 95% CI: 1.02, 1.08), unmet need for contraception (AOR = 1.05; 95% CI: 1.02, 1.08), distance from a health facility (AOR = 1.03; 95% CI: 1.00, 1.06) were significantly associated with unintended pregnancy.
Conclusion: Unintended pregnancy rates remain high in LMICs. Women whose husband has no education and primary education, women with media exposure, working status, women who live in a household headed by male, women with unmet need for contraception, and women with a big problem of distance to health facilities were variables that were significant predictors of unintended pregnancy. When attempting to minimize unintended pregnancy in LMICs, these factors need to be considered. Furthermore, most of these attempts should be driven by government entities in low and middle-income countries.
Unintended pregnancies are pregnancies that are unwanted and/or mistimed at the time of conception (1, 2). Because of the consequences associated with both the mother's and child's social and health outcomes, unintended pregnancy is a major public health concern in both high-income countries and Middle-Income countries (LMICs) (3–5). It is estimated that 208 million pregnancies occur worldwide each year, with 46% of them becoming unintended (6). Annually, more than 14 million unintended pregnancies were reported in Sub-Saharan Africa (7). Although the global trend of unintended pregnancy has decreased over time, it remains high with significant regional variations (6, 8–11).
Although it is a problem in both high-income countries and LMICs, unintended pregnancy has decreased in high-income countries compared to LMICs (7). In some areas, unintended pregnancy accounts for more than half of all pregnancies (12). In low-income countries, the rate of unintended pregnancy varies between 7.2 and 59.6 per 100 person-years of follow-up (11).
Maternal and neonatal mortality remain unresolved public health problems (12–15). Unintended pregnancy causes maternal morbidity and mortality as a result of the complications of unsafe abortion, miscarriage, and unplanned births (16–18). Unintended pregnancy has serious consequences for women's and children's health and well-being (19). Abortions occur in more than half of unintended pregnancies (12, 20). Unintended pregnancies can lower the use of maternal (21–24), and neonatal (25) health services utilization, and worsen maternal health outcomes (2, 26–28). Moreover, unintended pregnancy is associated with malnutrition, mental illness, and vertical transmission of the Human immunodeficiency virus (HIV) to children (29, 30).
Maternal health issues are the first key research area in sexual and reproductive health till 2030 (31). Unintended pregnancy is one of the most serious public health problems that impose major health, economic, and psychosocial costs on individuals and communities, as well as significant emotional damage to women, families, and society (32–34). Besides, unintended pregnancy is associated with preeclampsia, obstetric bleeding, stigma, and socioeconomic inequalities (2, 27, 35, 36).
Different variables such as maternal age (37–39), marital status (37, 39, 40), wealth status (7, 38, 41), having an occupation (42), educational status of women (1, 19, 41–43), media exposure (37, 44), parity (37, 38, 45), family size (37, 45), contraceptive use (38, 42), being victims of sexual violence (46–48) were found predictors of unintended pregnancy.
Tackling unintended pregnancy is one way to reduce the high rates of maternal and neonatal mortality (20, 24–26, 49, 50). To the best of our knowledge, no studies have been conducted to investigate the magnitude of unintended pregnancy in LMICs. Because the majority of unintended pregnancies occur in low- and middle-income countries, there is a critical need to explore the underlying causes of unintended pregnancies among women in these countries. Hence, the primary goals of this study were to determine the prevalence of unintended pregnancy and to assess the effects of potential underlying factors on unintended pregnancy among women aged 15–49 in LMICs.
This study used the Demographic Health Survey (DHS) data from 61 low and middle-income countries collected between 2008 and 2020. By measuring key indicators deemed important, a DHS survey allows countries to generate data that can be used to inform policy and practice. Each country's survey includes a variety of datasets such as men, women, children, birth, and household datasets. For this study, we used individual record (IR) data. To select study participants, the DHS employs a two-stage stratified sampling technique.
This study only included women between the ages of 15 and 49 who had given birth within the previous five years of the survey. As a result, the total sample size was 187,347, with respondents from each country ranging from 607 in Guyana to 9,534 in Nigeria. A detailed description of the survey year, sample size, and sample characteristics is presented in Table 1.
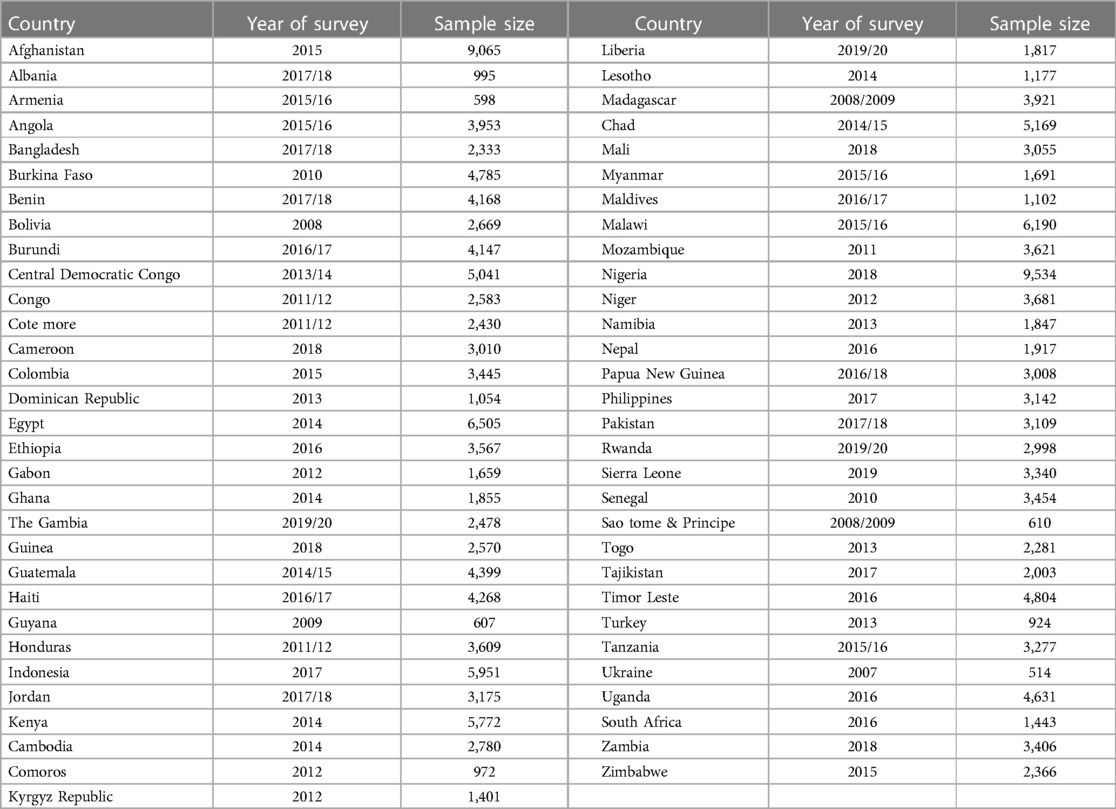
Table 1. Sample size determination in the study of the magnitude of unintended pregnancy among pregnant women, LMICS, DHS, 2008–2020.
The outcome variable was unintended pregnancy, which is composed of both pregnancies that are wanted no more or wanted later (mistimed). It was a binary variable, women with mistimed pregnancies or unwanted pregnancies were recorded as “unintended pregnancies”, while those who needed pregnancy then were recorded as ‘intended pregnancy’ (13). The study included individual-level independent variables such as the age of women (15–19, 20–24, 25–29, 30–34, 35–39, 40–44, and 45–49 years), educational status of women (no education, primary, secondary, and higher), educational status of the husband (no education, primary, secondary, and higher), media exposure (yes or no), working status (working or not working), terminated pregnancy (yes or no), household wealth status (poorest, poorer, middle, richer, or richest), household members (≤5, 6–10 or >10), and sex of household head (male or female), intention to use contraceptive (yes or no), and unmet need for contraceptive (yes or no). Community-level factors such as place of residence (rural or urban) and distance to health facilities (big problem and not a big problem) were also included.
Media exposure was created by asking women about the frequency of radio, television, and newspapers. It is classified as “yes” if women had at least one type of media exposure, such as radio, newspaper, or television, and “no” otherwise.
We appended the data from 61 LMICs after extracting the variables based on existing literature. Before any statistical analysis, the data were weighted using sampling weight to restore the survey's representativeness. The data was cleaned and statistical analyses were carried out using STATA version 16. Frequencies and percentages were used to describe the background characteristics of the study participants. We conducted a multilevel logistic regression analysis, assuming that each community has a different intercept and fixed coefficient, with a random effect applied at the cluster level. Factors with a p-value ≤0.2 in crude odds ratio (COR) were selected as candidates for the adjusted model, finally, the adjusted odds Ratio (AOR) with 95% CI was reported, and variables with p-values less than 0.05 were declared to be significant predictors of unintended pregnancy in the multivariable analysis.
The fixed effects method was utilized to estimate the relationship between unintended pregnancy and independent variables, which was expressed as an odds ratio with a 95% confidence interval and a p-value of 0.05.The random effects, which are measures of variation of unintended pregnancy across communities or clusters, were expressed in terms of the Intra-Class Correlation (ICC), the median odds ratio (MOR), and the proportional change in variance (PCV). The ICC shows the differences between clusters in unintended pregnancy among reproductive-aged women. The ICC is calculated as , Where; VA represents the area-level variance (51–53). The MOR indicates the central value of the odd ratio between the highest and the lowest risk regions when two clusters are chosen at random. The MOR is calculated as , where VA donates the area level variance (54, 55).
The PCV measures the proportion of total observed individual variation that can be attributed to differences between clusters. The PCV is calculated as; , whereas; Vnull represents the variance of the initial model, while VA represents the variance of the model with more terms (54, 55).
Four models were fitted to select the best-fit model for the data using deviance: the null model (model without independent variables), model I (model with individual-level variables), model II (models including community-level variables), and model III (model with both individual and community-level variables). Deviance information criteria (DIC) (−2 × log-likelihood value) were used to assess the goodness of fit. The Variance Inflation Factor (VIF) was used to test for multicollinearity among the selected independent variables.
The data set was obtained from the DHS website after a formal request and permission from the major DHS. All methods were performed following the Demographic and Health Surveys (DHS) program's relevant guidelines and regulations. The dataset was not allowed to be shared with other organizations and has remained confidential.
Majority of the participants are in the age group of 25–29 [49,946(26.66%)]. Single women had a greater proportion of unintended pregnancies (27.75%), while the least proportion was recorded among married women (25.90%). Women who are from urban areas had a greater proportion of unintended pregnancies (26.57%) than women from rural areas (25.80%). Women who are from the poorest households have a higher proportion of unintended pregnancies (26.65%) compared to women from the richest household (25.80%) (Table 2).
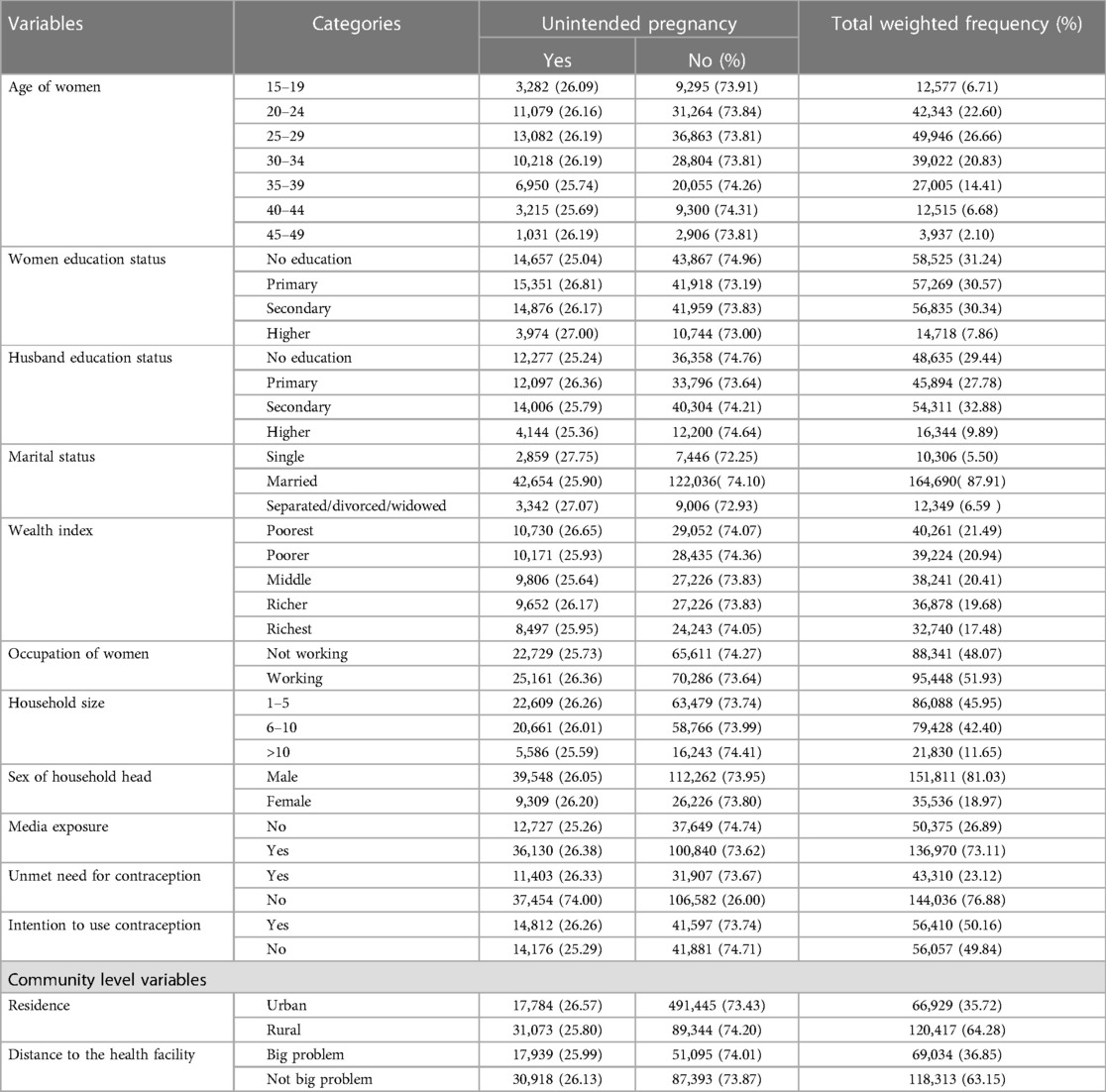
Table 2. Relationship between individual and community level variables and unintended pregnancy among pregnant women, LMICS, DHS, 2008–2020.
The overall prevalence rate of unintended pregnancy in LMICs was 26.08% (95% CI: 26.00%, 26.41%). The highest prevalence of unintended pregnancy was reported in Bolivia at 61.71% (95% CI: 61.69%, 61.73%), and the lowest proportion of unintended pregnancy was recorded in Egypt at 19.25% (95% CI: 19.24%, 19.26%) (Figure 1).
Based on the final model (Model III, which includes both individual and community-level variables), occupation, husband's education, unmet need for contraceptive, and media exposure, and distance to health facilities were variables statistically associated with unintended pregnancy.
Women whose husbands have no education and primary education were 1.07 (AOR = 1.07; 95% CI: 1.00, 1.15), and 1.09 (AOR = 1.09; 95% CI: 1.02, 1.17) times higher odds of experiencing unintended pregnancies respectively than women who have higher education. The odds of unintended pregnancy in those who are currently working are 1.03 (AOR = 1.03; 95% CI: 1.00, 1.06) times higher than that of women who are not working. The risk of unintended pregnancy among women who live in a household with a male head was 1.04 (AOR = 1.04; 95% CI: 1.00, 1.08) times higher as compared to women who live in a household with a female head. Women who are exposed to media have 1.05 (AOR = 1.05; 95% CI: 1.02, 1.08) times higher odds of having an unintended pregnancy than those women who have not been exposed to media. The odds of experiencing unintended pregnancy among those women who had an unmet need for contraception were 1.05 (AOR = 1.05; 95% CI: 1.02, 1.08) times higher compared to those without an unmet need for contraception. Mothers who perceive distance from the health facility as a big problem had 1.03 (AOR = 1.03; 95% CI: 1.00, 1.06) times higher odds of having an unintended pregnancy compared to their counterparts (Table 3).
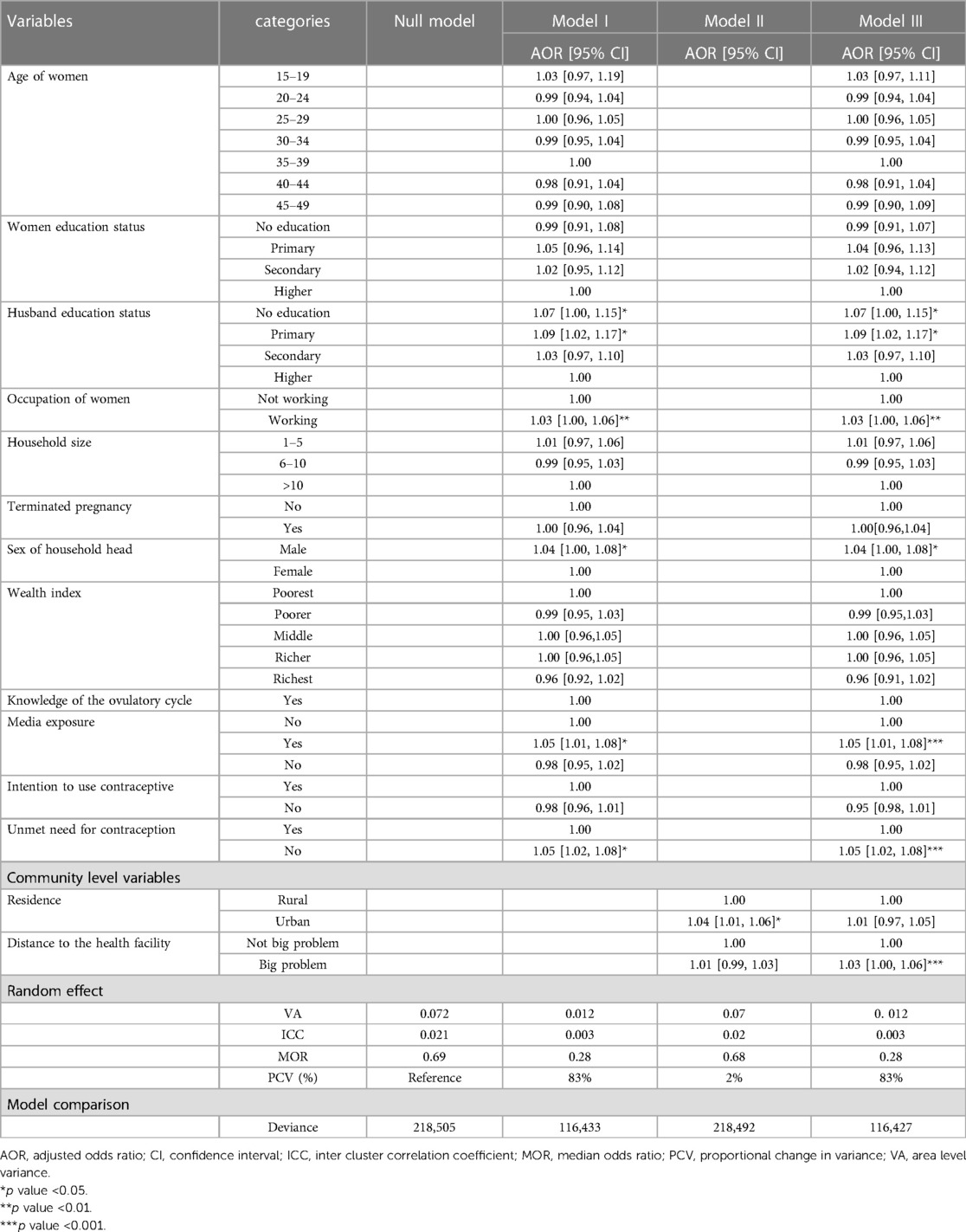
Table 3. Multilevel multivariable analysis of factors associated with unintended pregnancy among women in LMICs, DHS 2008–2020.
The random effects results are shown in Table 3. It was found that in the empty model (Model 0), there are substantial variations in unintended pregnancies among LMICs. The ICC in the null model showed that about 2.1% (0.021) of the total variance was attributable to the community where the women live. Model III, which includes both individual and community-level variables, was chosen due to its low deviance (116,427). Therefore, Model III, the complete model with both the selected individual and household/community factors, was the best.
The pooled magnitude of unintended pregnancy in LMICs was 26.46%% (95% CI: 25.30%, 27.62%). The finding is higher than a study done in Six Asian countries (19.1%) (56) and lower than a study done in SSA (29.0%) (13). It is critical to recognize that, while unintended pregnancies are common in LMICS, some variations still exist across countries. The possible reason for this variation might be the difference in the health system of each country. According to our findings, unintended pregnancy rates in low- and middle-income countries range from 19.25% in Egypt to 61.71% in Bolivia.
In a multivariable multilevel logistic regression analysis, paternal education, working status, median exposure, household wealth index, residence, and distance to health facilities were significantly associated with unintended pregnancy in low and middle-income countries.
Women whose husbands have no education and primary education have higher odds of unintended pregnancy compared to women whose husbands have higher education (57, 58). Partners who have no formal education or a lower level of education are less likely to encourage their wives to use modern contraceptives and a woman's pregnancy intentions and parenting decisions are influenced by her partner's attitude (59). Improving the male partner's educational status is critical because the male partner has a strong influence on most household decisions, including the timing of pregnancy and the number of children desired (58).
Women who have media exposure have higher odds of unintended pregnancy compared to women who have no media exposure. This finding is contradictory to a study done in Ethiopia (44, 60), Nepal (61), and Pakistan (62). The possible justification might be even though media exposure creates awareness, that women having exposure to media may have an increased chance of social networks that may expose them to unintended pregnancy.
Women who are currently working have higher odds of unintended pregnancy compared to women who are not currently working. This finding is consistent with a study done in Ethiopia (63, 64) This finding is contradictory to a study done in Ethiopia (65) and Cambodia (66). The possible reason might be women with occupations may have a high level of social interaction and the nature of their work, which may lead to casual sex followed by unwanted pregnancy (63).
The likelihood of unintended pregnancy was higher among women who lived in a household with a male head than among women who lived in a household with a female head. The finding is similar to previous findings (67). Women living in male-headed households may not have the opportunity to actively participate in family planning decisions, resulting in an unmet need for family planning and unintended pregnancy (68).
Women with unmet family planning needs were more likely to experience unintended pregnancy than those with met needs. The finding is consistent with previous studies (69–73). The possible justification for this could be that the unmet need for contraception has exposed women to the risks of unplanned pregnancy. Addressing the challenges and unmet need for contraception should be a priority for reducing unintended pregnancies in low- and middle-income countries.
Women with a big problem with distance to health facilities have higher odds of having unintended pregnancies than women who do have not a big problem. The finding is consistent with a study done in Ethiopia (74–76). The possible reason might be that women facing a big problem of distance to health facilities may have a problem accessing health care such as contraception (77).
The use of weighted, nationally representative large datasets of low and middle-income countries, with advanced statistical analysis techniques that account for the nature of DHS data for better parameter estimation was a strength of this study. However, due to the cross-sectional type of data, uncovering the causality between dependent and independent variables is challenging. The data was obtained through self-reports from women five years before the survey, which could be a cause of recall bias. Moreover, because it depends on the factors available in the DHS data set, the most significant explanatory factors such as medical-related factors, and the quality of maternal health services may be missed.
Unintended pregnancy rates remain high in LMICs. Women whose husband has no education and primary education, women with media exposure, working status, women who live in a household headed by a male, women with unmet need for contraception, and women with a big problem of distance to health facilities were variables that were significant predictors of unintended pregnancy. When attempting to minimize unintended pregnancy in LMICs, these factors need to be considered. Furthermore, most of these attempts should be driven by government entities in low and middle-income countries.
Publicly available datasets were analyzed in this study. This data can be found here: www.dhsprogram.com.
The data set was obtained from the DHS website after a formal request and permission from the major DHS. All methods were performed following the Demographic and Health Surveys (DHS) program's relevant guidelines and regulations. The dataset was not allowed to be shared with other organizations and has remained confidential. The patients/participants provided their written informed consent to participate in this study.
FMA originates the research concept. FMA, AZA, RET, TA, and BAT wrote the main manuscript text. All authors contributed to the article and approved the submitted version.
We would like to thank the measure DHS program for providing the data set.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
AOR, adjusted odds ratio; CI, confidence interval; DHS, demographic and health survey; ICC, intra-class correlation coefficient; LMICs, low and middle-income countries; PCV, proportional change in variance.
1. Goshu YA, Yitayew AE. Prevalence and determinant factors of unintended pregnancy among pregnant women attending antenatal clinics of Addis Zemen hospital. PLoS One. (2019) 14(1):e0210206. doi: 10.1371/journal.pone.0210206
2. Dehingia N, et al. Unintended pregnancy and maternal health complications: cross-sectional analysis of data from rural Uttar Pradesh, India. BMC Pregnancy Childbirth. (2020) 20(1):188. doi: 10.1186/s12884-020-2848-8
3. Khajehpour M, Simbar M, Jannesari S, Ramezani-Tehrani F, Majd HA. Health status of women with intended and unintended pregnancies. Public Health. (2013) 127(1):58–64. doi: 10.1016/j.puhe.2012.08.011
4. Jalaly P, Ghodsi Z, Hojjatoleslami S. Health behavior’s deference in intended and unintended pregnancies. Procedia Soc Behav Sci. (2015) 185:156–9. doi: 10.1016/j.sbspro.2015.03.420
5. Petersen R, Moos MK. Defining and measuring unintended pregnancy: issues and concerns. Women's Health Issues. (1997) 7(4):234–40. doi: 10.1016/S1049-3867(97)00009-1
6. Bearak J, Popinchalk A, Alkema L, Sedgh G. Global, regional, and subregional trends in unintended pregnancy and its outcomes from 1990 to 2014: estimates from a Bayesian hierarchical model. The LANCET Global Health. (2018) 6(4):e380–9. doi: 10.1016/S2214-109X(18)30029-9
7. Ameyaw EK, Budu E, Sambah F, Baatiema L, Appiah F, Seidu AA, et al. Prevalence and determinants of unintended pregnancy in Sub-Saharan Africa: a multi-country analysis of demographic and health surveys. PLoS One. (2019) 14(8):e0220970. doi: 10.1371/journal.pone.0220970
8. Dutta M, Shekhar C, Prashad L. Level, trend and correlates of mistimed and unwanted pregnancies among currently pregnant ever married women in India. PLoS One. (2015) 10(12):e0144400. doi: 10.1371/journal.pone.0144400
9. Finer LB, Zolna MR. Declines in unintended pregnancy in the United States, 2008–2011. N Engl J Med. (2016) 374(9):843–52. doi: 10.1056/NEJMsa1506575
10. Branum AM, Ahrens KA. Trends in timing of pregnancy awareness among US women. Matern Child Health J. (2017) 21(4):715–26. doi: 10.1007/s10995-016-2155-1
11. Ampt FH, Willenberg L, Agius PA, Chersich M, Luchters S, Lim MS. Incidence of unintended pregnancy among female sex workers in low-income and middle-income countries: a systematic review and meta-analysis. BMJ Open. (2018) 8(9):e021779. doi: 10.1136/bmjopen-2018-021779
12. World Health Organization. Every newborn every women: an action plan to end preventable deaths (2014). Available at: www.who.int/about/licensing/copyright_form/en/index.html
13. World Health Organization & Ethiopia. Ministry of Health. Success factors for women’s and children’s health: Ethiopia (2015).
15. World Health Organization. Newborns: reducing mortality, key facts (2019). Available at: https://www.who.int/news-room/fact-sheets/detail/newborns-reducing-mortality
16. Singh A, Singh A, Thapa S. Adverse consequences of unintended pregnancy for maternal and child health in Nepal. (2015) 27(2):NP1481–91. doi: 10.1177/1010539513498769
17. Kabir SM. Causes and consequences of unwanted pregnancy from Asian women’s perspectives. (1989) 30:9–14. doi: 10.1016/0020-7292(89)90097-0
18. Mumah J, Kabiru CW, Mukiira C, Brinton J, Mutua M, Izugbara CO Unintended pregnancies in Kenya: a country profile (2014).
19. Alene M, Yismaw L, Berelie Y, Kassie B, Yeshambel R, Assemie MA. Prevalence and determinants of unintended pregnancy in Ethiopia: a systematic review and meta-analysis of observational studies. (2020) 15(4):e0231012. doi: 10.1371/journal.pone.0231012
20. Aztlan EA, Foster DG, Upadhyay U. Subsequent unintended pregnancy among US women who receive or are denied a wanted abortion. J Midwifery Womens Health. (2018) 63(1):45–52. doi: 10.1111/jmwh.12723
21. Nance N, Ralph L, Padian N, Cowan F, Buzdugan R, Mushavi A, et al. Unintended pregnancy and subsequent postpartum long-acting reversible contraceptive use in Zimbabwe. BMC Womens Health. (2018) 18(1):193. doi: 10.1186/s12905-018-0668-z
22. Abame DE, Abera M, Tesfay A, Yohannes Y, Ermias D, Markos T, et al. Relationship between unintended pregnancy and antenatal care use during pregnancy in Hadiya Zone, Southern Ethiopia. J Reprod Infertil. (2019) 20(1):42–51.30859081
23. Brittain K, Phillips TK, Zerbe A, Abrams EJ, Landon MY. Long-term effects of unintended pregnancy on antiretroviral therapy outcomes among South African women living with HIV. Aids. (2019) 33(5):885–93. doi: 10.1097/QAD.0000000000002139
24. Khan MN, Harris ML, Shifti DM, Laar AS, Loxton D. Effects of unintended pregnancy on maternal healthcare services utilization in low- and lower-middle-income countries: systematic review and meta-analysis. Int J Public Health. (2019) 64(5):743–54. doi: 10.1007/s00038-019-01238-9
25. Echaiz J, Blas M, Kancherla V. Unintended pregnancy and its impact on childhood rotavirus immunization in Peru. Rev Panam Salud Publica. (2018) 42:e96. doi: 10.26633/RPSP.2018.96
26. Judge-Golden CP, Borrero S, Zhao X, Mor MK, Callegari LS. The association between mental health disorders and history of unintended pregnancy among women veterans. J Gen Intern Med. (2018) 33(12):2092–9. doi: 10.1007/s11606-018-4647-8
27. Omani-Samani R, Amini Rarani M, Sepidarkish M, Khedmati Morasae E, Maroufizadeh S, Almasi-Hashiani A. Socioeconomic inequality of unintended pregnancy in the Iranian population: a decomposition approach. BMC Public Health. (2018) 18(1):607. doi: 10.1186/s12889-018-5515-5
28. Gharaee M, Baradaran HR. Consequences of unintended pregnancy on mother and fetus and newborn in North-East of Iran. J Matern Fetal Neonatal Med. (2020) 33(5):876–9. doi: 10.1080/14767058.2018.1500538
29. Baschieri A, Machiyama K, Floyd S, Dube A, Molesworth A, Chihana M, et al. Unintended childbearing and child growth in Northern Malawi. Matern Child Health J. (2017) 21(3):467–74.27491527
30. Claridge AM, Chaviano CL. Consideration of abortion in pregnancy: demographic characteristics, mental health, and protective factors. Women & Health. (2013) 53(8):777–94. doi: 10.1080/03630242.2013.831018
31. Hindin MJ, Christiansen CS, Ferguson BJ. Setting research priorities for adolescent sexual and reproductive health in low- and middle-income countries. Bull World Health Organ. (2013) 91(1):10–8. doi: 10.2471/BLT.12.107565
32. Mulatu T, Cherie A, Negesa L. Prevalence of unwanted pregnancy and associated factors among women in reproductive age groups at selected health facilities in Addis Ababa, Ethiopia. Journal of Women's Health Care. (2017) 6(392):2167–420. doi: 10.4172/2167-0420.1000392
33. Mamboleo N. Unwanted pregnancy and induced abortion among female youths: A case study of temeke district. Dar es Salaam, Tanzania: Muhimbili University of Health and Allied Sciences (2012).
34. Hernandez ND. An exploration of the meaning and consequences of unintended pregnancy among Latina cultural subgroups: Social, cultural, structural, historical and political influences. Tampa, Florida: University of South Florida (2013).
35. Wado YD. Norms and stigma around unintended pregnancy in Alabama: associations with recent contraceptive use and dual method use among young women. Women Health. (2018) 58(10):1151–66. doi: 10.1080/03630242.2017.1414099
36. Bearak J, Popinchalk A, Ganatra B, Moller AB, Tunçalp Ö, Beavin C Unintended pregnancy and abortion by income, region, and the legal status of abortion: estimates from a comprehensive model for 1990–2019. Lancet Glob Health. (2020) 8(9):e1152–61. doi: 10.1016/S2214-109X(20)30315-6
37. Teshale AB, Tesema GA. Magnitude and associated factors of unintended pregnancy in Ethiopia: a multilevel analysis using 2016 EDHS data. BMC Pregnancy and Childbirth. (2020) 20(1):1–8. doi: 10.1186/s12884-020-03024-5
38. Aly Nor S, Amasha AR, Salah Salama N, Abdel-haleem AR. Prevalence of unintended pregnancy and associated factors in Port-Said city. Port Said Scientific Journal of Nursing. (2019) 6(1):101–20.
39. Nigussie K, et al. Magnitude of unintended pregnancy and associated factors among pregnant women in Debre Markos Town, East Gojjam Zone, Northwest Ethiopia: a cross-sectional study. Int J Womens Health. (2021) 13:129.33542661
40. Theme-Filha MM, et al. Factors associated with unintended pregnancy in Brazil: cross-sectional results from the birth in Brazil national survey, 2011/2012. Reprod Health. (2016) 13(Suppl 3):118. doi: 10.1186/s12978-016-0227-8
41. Haffejee F, et al. Factors associated with unintended pregnancy among women attending a public health facility in KwaZulu-Natal, South Africa. S Afr Fam Pract. (2018) 60(3):79–83.
42. Merga J, Wirtu D, Bekuma TT, Regasa MT. Unintended pregnancy and the factors among currently pregnant married youths in Western Oromia, Ethiopia: a mixed method. Plos One. (2021) 16(11):e0259262. doi: 10.1371/journal.pone.0259262
43. Gebremariam Weldearegawi G, Tekola KB, Fseha B. Teklehaymanot, magnitude and associated factors of unintended pregnancy among pregnant women at saesie tsaeda emba woreda eastern zone of Tigray, North Ethiopia, 2018. J Pregnancy. (2019) 2019:1694808. doi: 10.1155/2019/1694808
44. Admasu E, Mekonnen A, Setegn T, Abeje G. Level of unintended pregnancy among reproductive age women in Bahir Dar city administration, northwest Ethiopia. BMC Research Notes. (2018) 11(1):1–5. doi: 10.1186/s13104-018-4016-z
45. Bekele H, Dheressa M, Mengistie B, Sintayehu Y, Fekadu G. Unintended pregnancy and associated factors among pregnant women attending antenatal care at Bako Tibe district public health facility, Oromia region, Ethiopia. J Pregnancy. (2020) 2020:1–7. doi: 10.1155/2020/3179193
46. Acharya K, Paudel YR, Silwal P. Sexual violence as a predictor of unintended pregnancy among married young women: evidence from the 2016 Nepal demographic and health survey. BMC Pregnancy Childbirth. (2019) 19(1):196. doi: 10.1186/s12884-019-2342-3
47. Xiao X, Wu ZC, Chou KC. What has reproductive health decision-making capacity got to do with unintended pregnancy? Evidence from the 2014 Ghana demographic and health survey. PLoS One. (2019) 14(10):e0223389. doi: 10.1371/journal.pone.0223389
48. Fotso JC, Mukiira C. Contraceptive use and unintended pregnancy among young women and men in Accra, Ghana. PLoS One. (2018) 13(8):e0201663. doi: 10.1371/journal.pone.0201663
49. Guterman K. Unintended pregnancy as a predictor of child maltreatment. Child Abuse Negl. (2015) 48:160–9. doi: 10.1016/j.chiabu.2015.05.014
50. Engstrand S, Kopp Kallner H. Cost of unintended pregnancy in Sweden—a possibility to lower costs by increasing LARC usage. Contraception. (2018) 97(5):445–50. doi: 10.1016/j.contraception.2018.01.009
51. Austin PC, Merlo J. Intermediate and advanced topics in multilevel logistic regression analysis. Stat Med. (2017) 36(20):3257–77. doi: 10.1002/sim.7336
52. Sommet N, Morselli D. Keep calm and learn multilevel logistic modeling: a simplified three-step procedure using Stata, R, Mplus, and SPSS. Int Rev Soc Psychol. (2017) 30:203–18. doi: 10.5334/irsp.90
53. Weinmayr G, Dreyhaupt J, Jaensch A, Forastiere F, Strachan DP. Multilevel regression modelling to investigate variation in disease prevalence across locations. Int J Epidemiol. (2017) 46(1):336–47. doi: 10.1093/ije/dyw274
54. Merlo J, Chaix B, Yang M, Lynch J, Råstam L. A brief conceptual tutorial on multilevel analysis in social epidemiology: interpreting neighbourhood differences and the effect of neighbourhood characteristics on individual health. J Epidemiology Community Health. (2005) 59(12):1022–9.
55. Merlo J, Chaix B, Ohlsson H, Beckman A, Johnell K, Hjerpe P, et al. A brief conceptual tutorial of multilevel analysis in social epidemiology: using measures of clustering in multilevel logistic regression to investigate contextual phenomena. J Epidemiology Community Health. (2006) 60(4):290–7.
56. Sarder A, Islam SM, Maniruzzaman , Talukder A, Ahammed B. Prevalence of unintended pregnancy and its associated factors: evidence from six south Asian countries. PLoS One. (2021) 16(2):e0245923. doi: 10.1371/journal.pone.0245923
57. Seifu CN, Fahey PP, Hailemariam TG, Atlantis E. Association of husbands’ education status with unintended pregnancy in their wives in southern Ethiopia: a cross-sectional study. PLoS One. (2020) 15(7):e0235675. doi: 10.1371/journal.pone.0235675
58. Beyene GA. Prevalence of unintended pregnancy and associated factors among pregnant mothers in Jimma town, southwest Ethiopia: a cross sectional study. Contraception and Reproductive Medicine. (2019) 4(1):1–8. doi: 10.1186/s40834-019-0090-4
59. Santelli J, Rochat R, Hatfield-Timajchy K, Gilbert BC, Curtis K, Cabral R, et al. The measurement and meaning of unintended pregnancy. Perspectives on Sexual and Reproductive Health. (2003) 35:94–101.12729139
60. Geda NR, Lako TK. A population based study on unintended pregnancy among married women in a district in southern Ethiopia. J Geogr Reg Plan. (2011) 4(7):417–27.
61. Acharya P, Gautam R, Aro AR. Factors influencing mistimed and unwanted pregnancies among Nepali women. J Biosoc Sci. (2016) 48(2):249–66. doi: 10.1017/S0021932015000073
62. Razzaq S, Jessani S, Rizvi N, Saleem S. Unintended pregnancy and the associated factors among pregnant females: Sukh Survey-Karachi, Pakistan. Journal of the Pakistan Medical Association. (2021) 71(11 (Suppl 7)):S50.
63. Kassie T, Moges G, Ali A, Tefera W. Magnitude and factors associated with unintended pregnancy among pregnant women in Addis Ababa, Ethiopia. Global Journal of Medicine and Public Health. (2017) 6(4):15.
64. Mulat S, Fekadu M, Abera H, Bekele G, Bedaso A. Prevalence of unplanned pregnancy and associated factors among mothers attending antenatal care at Hawassa city public hospitals, Hawassa, SNNPR, Ethiopia. Ethiopia J Women's Health Care. (2017) 6(387):2167–0420. doi: 10.4172/2167-0420.1000387
65. Moges Y, Worku SA, Niguse A, Kelkay B. Factors associated with the unplanned pregnancy at suhul general hospital, Northern Ethiopia, 2018. J Pregnancy. (2020) 2020. doi: 10.1155/2020/2926097
66. Rizvi F, Williams J, Hoban E. Factors influencing unintended pregnancies amongst adolescent girls and young women in Cambodia. Int J Environ Health Res. (2019) 16(20):4006. doi: 10.3390/ijerph16204006
67. Ayalew HG, Liyew AM, Tessema ZT, Worku MG, Tesema GA, Alamneh TS, et al. Prevalence and factors associated with unintended pregnancy among adolescent girls and young women in Sub-Saharan Africa, a multilevel analysis. BMC Women's Health. (2022) 22(1):1–9. doi: 10.1186/s12905-022-02048-7
68. Kluckow H, et al. Socio-demographic predictors of unintended pregnancy and late antenatal booking in Honiara, Solomon Islands. Aust N Z J Obstet Gynaecol. (2018) 58(3):349–57. doi: 10.1111/ajo.12782
69. Bishwajit G, Tang S, Yaya S, Feng Z. Unmet need for contraception and its association with unintended pregnancy in Bangladesh. BMC Pregnancy and Childbirth. (2017) 17(1):1–9. doi: 10.1186/s12884-017-1379-4
70. Kamal M, Islam A. Prevalence and socioeconomic correlates of unintented pregnancy among women in rural Bangladesh. Salud Pública de México. (2011) 53(2):108–15.
71. Nyarko SH. Unintended pregnancy among pregnant women in Ghana: prevalence and predictors. J Pregnancy. (2019) 2019:2019. doi: 10.1155/2019/2920491
72. Wondie AG. The association between unmet need for contraception and unintended pregnancy among reproductive-age women in Ethiopia. Medicine Access@ Point of Care. (2021) 5:23992026211033436. doi: 10.1177/23992026211033436
73. Yaya S, Ghose B. Prevalence of unmet need for contraception and its association with unwanted pregnancy among married women in Angola. PloS One. (2018) 13(12):e0209801. doi: 10.1371/journal.pone.0209801
74. Getu Melese K, Gebrie MH, Berta Badi M, Fekadu Mersha W. Unintended pregnancy in Ethiopia: community based cross-sectional study. Obstetrics and Gynecology International. (2016) 2016:2016. doi: 10.1155/2016/4374791
75. Bekele YA, Fekadu GA. Childbirth, factors associated with unintended pregnancy in Ethiopia; further analysis of the 2016 Ethiopian demographic health survey data. BMC Pregnancy and Childbirth. (2021) 21(1):1–7. doi: 10.1186/s12884-021-03924-0
76. Kassa N, Berhane Y, Worku A. Predictors of unintended pregnancy in Kersa, Eastern Ethiopia, 2010. Reprod Health. (2012) 9(1):1–7. doi: 10.1186/1742-4755-9-1
Keywords: unintended pregnancy, multilevel analysis, low and middle-income countries, child bearing age, women
Citation: Aragaw FM, Amare T, Teklu RE, Tegegne BA and Alem AZ (2023) Magnitude of unintended pregnancy and its determinants among childbearing age women in low and middle-income countries: evidence from 61 low and middle income countries. Front. Reprod. Health 5:1113926. doi: 10.3389/frph.2023.1113926
Received: 1 December 2022; Accepted: 29 May 2023;
Published: 17 July 2023.
Edited by:
Singh Rajender, Central Drug Research Institute (CSIR), IndiaReviewed by:
Thomas Hormenu, National Institutes of Health (NIH), United States© 2023 Aragaw, Amare, Teklu, Tegegne and Alem. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fantu Mamo Aragaw ZmFudHVtYTNAZ21haWwuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.