
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Reprod. Health, 03 May 2023
Sec. HIV and STIs
Volume 5 - 2023 | https://doi.org/10.3389/frph.2023.1072700
This article is part of the Research TopicImpact of COVID-19 on HIV/STI Screening, Prevention, and TreatmentView all 5 articles
Introduction: While the U.S. has seen a sustained rise in STI cases over the past decade, the impact of the COVID-19 on STIs and HIV is unclear.
Methods: To examine the short- and medium-term impacts of COVID-19 and HIV and STI testing and diagnosis, we compared pre-pandemic trends to three periods of the pandemic: early- pandemic, March-May 2020; mid-pandemic June 2020-May 2021; and late-pandemic, June 2021-May 2022. We compared average number of monthly tests and diagnoses, overall and by gender, as well as the monthly change (slope) in testing and diagnoses.
Results: We find that after decreases in average monthly STI and HIV testing and diagnoses during the early- and mid-pandemic, cases were largely back to pre-pandemic levels by the late-pandemic, with some variation by gender.
Conclusion: Changes in testing and diagnoses varied by phase of the pandemic. Some key populations may require additional outreach efforts to attain pre-pandemic testing levels.
The U.S continues to see rising cases of many STIs each year. The COVID-19 impacted access to testing as well as led to changes in sexual behaviors that could reduce transmission. The 2020 STD surveillance report shows that chlamydia, gonorrhea, and syphilis have all been increasing over the last decade; however, there were declines in the diagnosis of all three during the early months of the pandemic, leading to “uncertainty and difficulty in interpreting” the surveillance data from the pandemic (1). Preliminary data from 2021 suggest increasing cases for all three bacterial infections (2). Similar trends have been seen in Chicago, IL; chlamydia and syphilis cases have had an upward trend since at least 2003, while gonorrhea cases started increasing in 2015 (3).
Furthermore, the impacts of COVID-19 were not consistent but have been evolving since March 2020. Key changes during the early pandemic included changes in access to testing, shifts in public health and clinical staff to COVID-19 related projects, and changes in sexual behavior due to the emphasis on social distancing (4, 5). In addition, throughout the first year of the pandemic, there were also shortages of STI testing materials (6). However, access to testing, staffing, and sexual behaviors have not remained at the extreme lows seen in the early months of the pandemic. Interestingly, modeling suggests that duration of reduced sexual behavior compared to the duration of decreased testing access could lead to overall increases or decreases in HIV and STI cases, depending on the balance between the two (7). Based on the pandemic experience in Illinois, we defined pandemic time periods as: pre-pandemic, Jan 2017-Feb 2020; early-pandemic, March-May 2020, marked by the closing of schools and non-essential business, along with a shift to tele-medicine; mid-pandemic, June 2020-May 2021, described as gradually reopening, with intermittent restrictions re-imposed; and late-pandemic, June 2021-May 2022, noted for large scale vaccinations & masking restrictions removed (8).
In this paper, we seek to describe the short and medium-term changes in STI and HIV testing & diagnosis throughout multiple phases of the COVID-19 pandemic, specifically from March 2020 through May 2022, in order to better meet the current needs of STI & HIV testing.
Data was extracted from electronic medical records (EMR) of patient visits (ages 18–90) with an HIV or bacterial STI (chlamydia, gonorrhea, or syphilis) test at a large sexual and gender minority focused federally qualified health center (FQHC) in Chicago, Illinois from January 2017 through May 2022. Bacterial infection screenings could be performed at any anatomical site (i.e., penile, vaginal, oropharyngeal, anal/rectal).
We examined four main outcomes: bacterial STI tests, bacterial STI diagnoses, HIV tests, and HIV diagnoses. HIV outcomes were restricted to those who were documented as HIV-negative at the time of testing. We first compared monthly averages for each outcome by pandemic phase, using t-tests (assuming unequal variance) and the pre-pandemic period as the reference; we repeated the comparisons of means, stratifying by self-reported gender (including cis men, cis women, trans men, transwomen, nonbinary, or other/unknown), our a priori primary predictor. To assess if the month to month changes for each outcome differed by pandemic phase, we then modeled the total monthly number of tests or diagnoses using linear regressions with time (month), pandemic period (as dummy variables), and time-pandemic period interactions, using an interrupted time-series approach (9). The slopes for each period were compared to the pre-pandemic period. We also graphed these changes over time, both overall and by gender; however due to small numbers we did not use gender in the interrupted time-series models. In the graphs, we also included the “counterfactual” of each model, which is the pre-pandemic slope continued over all time periods.
All analyses were conducted in SAS 9.4. The institution's IRB reviewed and deemed this study protocol exempt.
Data were contributed by 72,443 unique patients across 257,412 visits, most of which occurred in the pre-pandemic phase (Table 1). This is a visit-level analysis, with most visits from young adults (45%), cis (cisgender) men (74%), and gay patients (of any gender) (50%); 41% identified as White, 27% as Black, and 22% as Hispanic/Latinx. People living with HIV prior to their study visit made up 21% of visits. There were few changes in demographics between the different pandemic phases; however, data collection did change with race/ethnicity and sexual orientation information being unreported for a larger proportion of patients starting in the early-pandemic.
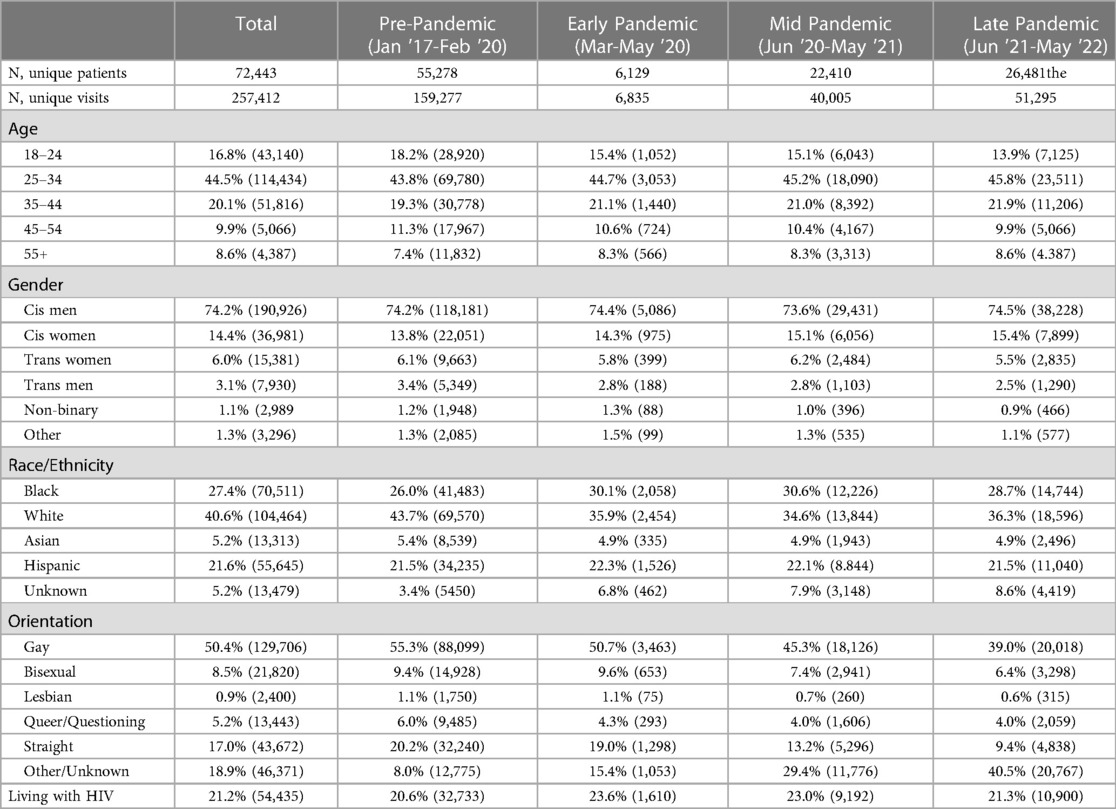
Table 1. Demographics & testing across all visits with bacterial STI or HIV testing, by pandemic phase.
Before the COVID-19 pandemic, the average number of monthly bacterial STI tests (chlamydia, gonorrhea, or syphilis) was 3,807 (SD 825; Table 2); this decreased in the early- and mid-pandemic phases, although it was only statistically significantly lower in the mid pandemic. Monthly tests returned to a similar average in the late-pandemic (4,103 [SD 254]). Positive bacterial STI tests followed a similar pattern, with 618 (SD 118) average monthly diagnoses in the pre-pandemic phase, decreased positive results in the early- and mid-pandemic, with the latter statistically significant (523 [SD 70]), and a non-significant increase to 622 (SD 55) in the late-pandemic phase. When stratified by gender, patterns were overall similar, though there were some differences in which timepoints met statistical significance. Of note, cis women had significantly higher monthly tests in the late-pandemic compared to pre-pandemic, while trans men and non-binary patients had significantly lower monthly tests. In terms of positive tests by gender, trans women had a significantly lower average monthly diagnoses in the early-pandemic compared to the pre-pandemic, and trans men and non-binary patients had significantly lower diagnoses in the late-pandemic.
As Figure 1 and Table 3 show, the slopes in both testing and positive tests differed visually by each pandemic phase. Pre-pandemic there was an increasing slope in testing and positive tests (69 and 10, respectively); this rapidly and significantly became a decreasing slope during the brief earl- pandemic phase (Table 3). Slopes began increasing again in the mid-pandemic phase, with a slight decline in the late-pandemic—although neither of these two timepoints were significantly different from the pre-pandemic phase. The percent of tests positive (positivity rate) was 16.3% in the pre-, 18.7% in the early-,16.4% in the mid-, and 15.2% in the late-pandemic periods.
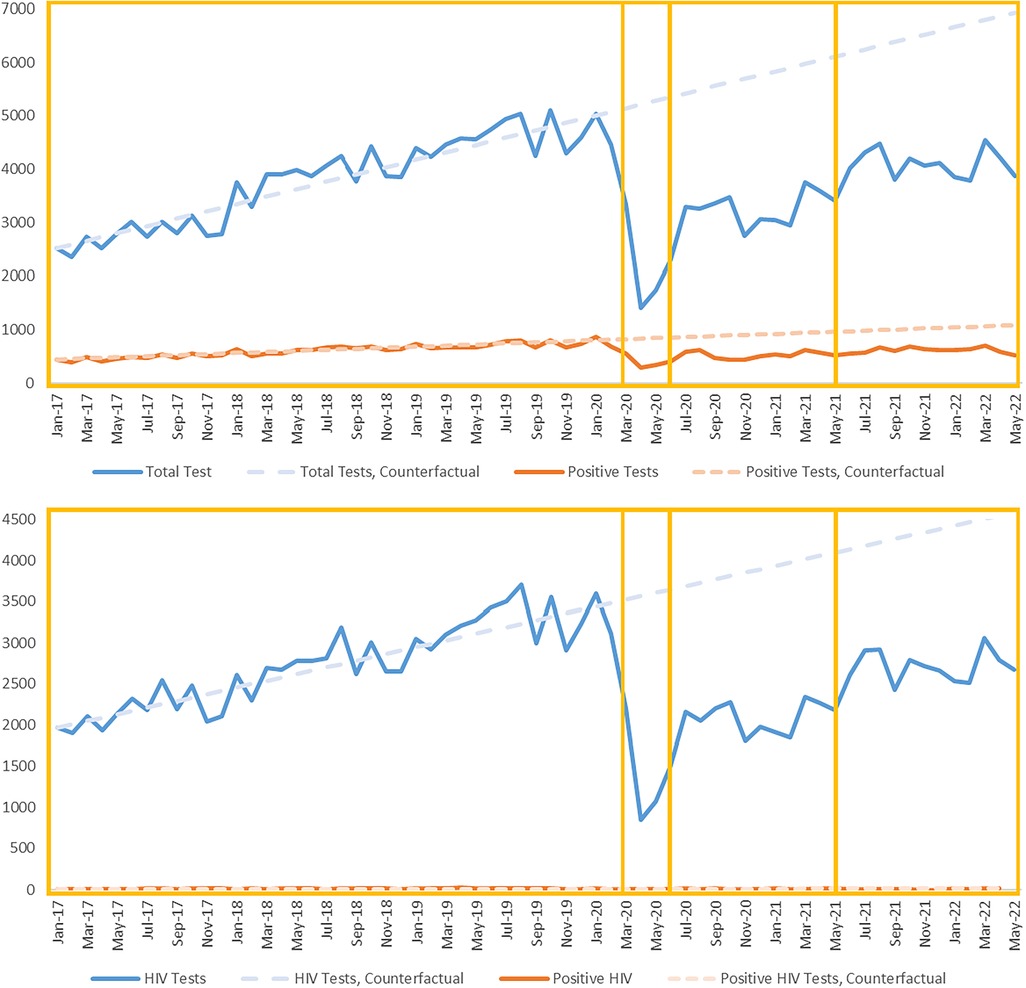
Figure 1. Total tests & positive tests over time, Any bacterial STI or HIV, by pandemic phase. The aggregate number of monthly tests (upper line) and positive tests (lower line) for any bacterial STI (upper pane) or HIV (lower pane) are shown as line graphs. The boxes delineate the Pre-, Early-, Mid-, and Late-Pandemic Phases. The dotted lines, marked counterfactual, are continuations of the pre-pandemic slope from each corresponding model.
Prior to the COVID-19 pandemic, there were an average of 2,743 (SD 511) HIV tests and 17 (SD 4) HIV diagnoses each month. These both declined in the early-pandemic phase, with a significant drop in HIV diagnoses (9 [SD 2]). This decline continued in the mid-pandemic phase, with HIV tests significantly lower than the pre-pandemic period. While HIV tests have returned to levels similar to the pre-pandemic, HIV diagnoses remain slightly lower, at 12 (SD 6) per month. When examining these patterns by gender, cis men and cis women have the same overall pattern, but all other genders showed significantly lower HIV testing still in the late-pandemic compared to pre-pandemic. However, cis men were the only group to have significantly lower HIV diagnoses in the late-pandemic phase.
In terms of changes in slope (Figure 1; Table 3), HIV testing and diagnoses had been increasing month over month prior to the pandemic (slopes of 41 and 0.08 respectively; there was a large decline in testing during the early-pandemic that was significant (Table 3). Testing and diagnoses slopes began to increase again in the mid-pandemic and have slightly declined or stayed flat in the late-pandemic phase. Positivity rates were 0.60%, 0.63%, 0.72%, and 0.38% from early- to late-pandemic phases.
In this analysis, we found that the average monthly tests and diagnoses for bacterial STIs was lower but statistically significant during the early-pandemic. This decrease continued and was statistically significant (likely due to the larger sample size) through the mid-pandemic phase. However, by the late-pandemic, testing and diagnoses had returned to pre-pandemic levels or higher, with some variations by gender. There was a similar pattern for HIV, although HIV diagnoses were significantly lower in the early- and late-pandemic phases. For all testing and diagnoses, there was a sharp decline in the slope (that is, the month to month change) during the early-pandemic compared to pre-pandemic.
It is difficult to assess whether changes during the pandemic were due to behavior or access; in actuality the causes were likely multifactorial. The CDC found a decrease both in HIV testing and diagnosis from February through December 2020, compared to the year prior (10). Similar to our results, most of this difference occurred early in the pandemic, with testing returning but not quite research previous levels by the fall (10). Multiple studies found rapid decline in bacterial STI diagnoses and testing during early pandemic, with some interesting variations by race & ethnicity (11–13). Two other studies found lower testing and diagnoses for most STIs & HIV during the early-pandemic period, but a subsequent increase in diagnoses in the mid-pandemic (14, 15). A study in a pediatric primary care network found that the first 8 months of the pandemic (compared to the previous year) showed fewer STI tests but a similar number of cases (16). Finally, study in Washington state found a larger decrease in asymptomatic compared to symptomatic cases during the early pandemic, suggesting declines are due more to limited screening; however, this decline could have been related to either access or test-seeking behaviors (13).
In terms of behavior, U.S. survey of gay men at early (April-May 2020) and mid (November 2020-January 2021) pandemic timepoints found little evidence that number of sexual partners changed from pre-pandemic times (17). However 32% and 19% (respectively at early- and mid-timepoints) reported the pandemic made HIV testing difficult, while 29% and 18% reported the same for STI testing (17). Reported PrEP use was similar at both timepoints (27% & 25%) (17), indicating either that sexual activity was consistent or simply that PrEP users were comfortable with their PrEP routine even in the absence of sex. However, other studies have found changes in sexual practices, particularly in the early-pandemic period (18, 19).
This study has certain limitations. Due to changes in data collection during the pandemic, we are not able to compare trends by race and/or ethnicity. We cannot account for changes in outreach or programming at different clinical sites that may have impacted testing among certain populations; we used all testing results, including STI walk-in services and primary care, which could have been differentially impacted. We did not collect data on behavior and therefore cannot separate out the effects of testing vs. sexual transmission. For multiple reasons, patients may not have chosen to report their actual gender, leading to possible misclassification. These data are from a sexual and gender minority focused health systems and the pandemic restrictions experienced in Chicago, IL likely differ from other areas of the nation; therefore these results are likely not generalizable to all settings.
In conclusion, we extend previous findings related to the early- and mid-pandemic phases. We find that HIV and STI testing and diagnoses had changed dramatically over different phases of the COVID-19 pandemic. However, by the late-pandemic phases—even including the Omicron wave—testing rates had largely returned to pre-pandemic levels, although they would likely have been higher in the pre-pandemic trajectories had continued uninterrupted. This pattern may help public health officials make decisions around resources during the acute phase of future public health emergencies. Testing and diagnoses appear to remain lower in some transgender and non-binary populations; in addition to improved outreach and communication with members of these communities, more research around both data collection and the impact of anti-trans stigma on disclosure of gender identity and sexual risk behaviors may be helpful to re-establish care and ensure latent infections are not being missed. Finally, using implementation science to understand how these clinics were able to restore high levels of testing would be a useful area of future research.
The data analyzed in this study is subject to the following licenses/restrictions: De-identified data are available by request. Requests to access these datasets should be directed to Maria Pyra, maria.pyra@northwestern.edu.
The studies involving human participants were reviewed and approved by Howard Brown Health IRB. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
MP developed the research question. TS and LR assisted with data collection and MP conducted the analysis; MH and AH contributed clinical considerations. MP drafted the manuscript. All authors contributed to the article and approved the submitted version.
We thank the staff of Howard Brown Health for their incredible work, particularly during the pandemic, and to the patients for contributing to this knowledge.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Sexually Transmitted Disease Surveillance, 2020. 2022 (cited 2022 Apr 12). Available at: https://www.cdc.gov/std/statistics/2020/default.htm
2. Preliminary 2021 STD Surveillance Data. 2022 (cited 2022 Sep 6). Available at: https://www.cdc.gov/std/statistics/2021/default.htm
3. CDPH. HIV/STI Surveillance Report, 2019. Chicago IL: Chicago Department of Public Health; 2020 Dec (cited 2021 Feb 16). Available at: https://www.chicago.gov/content/dam/city/depts/cdph/statistics_and_reports/CDPH-HIV-STI-REPORT-2020.pdf
4. Impact of COVID-19 on STDs. 2022 (cited 2022 Sep 7). Available at: https://www.cdc.gov/std/statistics/2020/impact.htm
5. Rogers B, Tao J, Murphy M, Chan PA. The COVID-19 pandemic and sexually transmitted infections: Where do we go from here? Sexually Transmitted Diseases. 2021 Apr 16 (cited 2022 Jan 5); Publish Ahead of Print. Available at: https://journals.lww.com/10.1097/OLQ.0000000000001445
6. Guidance and Resources During Disruption of STD Clinical Services. 2021 [cited 2022 Jan 5]. Available at: https://www.cdc.gov/std/prevention/disruptionGuidance.htm
7. Jenness SM, Le Guillou A, Chandra C, Mann LM, Sanchez T, Westreich D, et al. Projected HIV and bacterial sexually transmitted infection incidence following COVID-19–related sexual distancing and clinical service interruption. J Infect Dis. (2021) 223(6):1019–28. doi: 10.1093/infdis/jiab051
8. Documenting Illinois’ path to recovery from the coronavirus (COVID-19) pandemic, 2020–2021. Ballotpedia. (cited 2022 Jan 5). Available at: https://ballotpedia.org/Documenting_Illinois%27_path_to_recovery_from_the_coronavirus_(COVID-19)_pandemic,_2020-2021
9. Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. (2017) 46(1):348–55. doi: 10.1093/ije/dyw098
10. DiNenno EA. HIV Testing Before and During the COVID-19 Pandemic — United States, 2019–2020. MMWR Morb Mortal Wkly Rep. 2022 (cited 2022 Jun 23); 71. Available at: https://www.cdc.gov/mmwr/volumes/71/wr/mm7125a2.htm
11. Braunstein SL, Slutsker JS, Lazar R, Shah D, Hennessy RR, Chen S, et al. Epidemiology of reported HIV and other sexually transmitted infections during the COVID-19 pandemic, New York city. J Infect Dis. (2021) 224(5):jiab319. doi: 10.1093/ije/dyw098
12. Hill BJ, Anderson B, Lock L. COVID-19 Pandemic, Pre-exposure prophylaxis (PrEP) care, and HIV/STI testing among patients receiving care in three HIV epidemic priority states. AIDS Behav. (2021) 25(5):1361–5. doi: 10.1007/s10461-021-03195-y
13. Berzkalns A, Thibault CS, Barbee LA, Golden MR, Khosropour C, Kerani RP. Decreases in reported sexually transmitted infections during the time of COVID-19 in king county, WA: decreased transmission or screening? Sex Transm Dis. (2021) 48(8 Suppl):S44–9. doi: 10.1097/OLQ.0000000000001463
14. Menza TW, Zlot AI, Garai J, Humphrey S, Ferrer J. The impact of the SARS-CoV-2 pandemic on human immunodeficiency virus and bacterial sexually transmitted infection testing and diagnosis in Oregon. Sexual Trans Dis. (2021) 48(5):e59–63. doi: 10.1097/OLQ.0000000000001385
15. Pagaoa M, Grey J, Torrone E, Kreisel K, Stenger M, Weinstock H. Trends in nationally notifiable sexually transmitted disease case reports during the US COVID-19 pandemic, January to December 2020. Sex Transm Dis. (2021) 48(10):798–804. doi: 10.1097/OLQ.0000000000001506
16. Bonett S, Petsis D, Dowshen N, Bauermeister J, Wood SM. The impact of the COVID-19 pandemic on STI/HIV testing among adolescents in a large pediatric primary care network. Sex Transm Dis. (2021) 48(7):e91–e93. (cited 2021 Sep 13); Publish Ahead of Print. doi: 10.1097/OLQ.0000000000001427
17. Stephenson R, Sullivan SP, Pitter RA, Hunter AS, Chavanduka TMD. Are we still having sex? Results of round two of the love and sex in the time of COVID survey with gay, bisexual and other men who have sex with men. AIDS Behav. (2022) 26(7):2338–48. doi: 10.1007/s10461-022-03580-1
18. Pampati S, Emrick K, Siegler AJ, Jones J. Changes in sexual behavior, PrEP adherence, and access to sexual health services because of the COVID-19 pandemic among a cohort of PrEP-using MSM in the south. JAIDS J Acquir Immune Defic Syndr. (2021) 87(1):639–43. doi: 10.1097/QAI.0000000000002640
19. McKay T, Henne J, Gonzales G, Quarles R, Gavulic KA, Garcia Gallegos S. The COVID-19 pandemic and sexual behavior among gay and bisexual men in the United States. Sex Res Soc Policy: Rochester, NY; (2020) (cited 2023 Feb 24). Available at: https://papers.ssrn.com/abstract=3614113
Keywords: HIV testing, STI testing, COVID- 19, MSM (men having sex with men), transgender
Citation: Pyra M, Schafer T, Rusie L, Houlberg M, Thompson HM and Hazra A (2023) Temporary changes in STI & HIV testing & diagnoses across different phases of the COVID-19 pandemic, Chicago IL. Front. Reprod. Health 5:1072700. doi: 10.3389/frph.2023.1072700
Received: 17 October 2022; Accepted: 17 April 2023;
Published: 3 May 2023.
Edited by:
Kenneth K. Mugwanya, University of Washington, United StatesReviewed by:
Cyrus Ghaznavi, Keio University, Japan© 2023 Pyra, Schafer, Rusie, Houlberg, Thompson and Hazra. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Maria Pyra bWFyaWEucHlyYUBub3J0aHdlc3Rlcm4uZWR1
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.