- 1Biobehavioral Pediatric Pain Lab, Department of Psychiatry and Behavioral Sciences, Boston Children's Hospital, Boston, MA, United States
- 2Pain & Affective Neuroscience Center, Department of Anesthesiology, Critical Care, and Pain Medicine, Boston Children's Hospital, Boston, MA, United States
- 3Nuffield Department of Women's and Reproductive Health, Medical Sciences Division, University of Oxford, Oxford, United Kingdom
- 4Division of Adolescent/Young Adult Medicine, Boston Children's Hospital, Boston, MA, United States
- 5Harvard Medical School, Boston, MA, United States
- 6Department of Psychiatry, Harvard Medical School, Boston, MA, United States
Awareness and visibility of transgender individuals have grown exponentially. However, conceptualizing sexual and reproductive health (SRH) as “women's” or “men's” health services further marginalizes transgender and gender-expansive (TGE) youth. Multiple reviews and commentaries have been published on the topic of SRH care for adults under the umbrella term of sexual and gender minorities, all with a call to action for more inclusive care and the need for more clinical research involving TGE individuals, and notably, TGE youth. Results from adult TGE studies are often translated to describe adolescent models. However, models specific to adolescent TGE populations are needed to understand their unique SRH needs. This review will describe the current literature relating to SRH needs of TGE youth and adults, highlighting key areas with significant disparities in need of further research. This comprehensive summary will also provide recommendations for clinicians and researchers with the goal of improving SRH care and obtaining wider representation in both clinical settings and research directed toward TGE youth.
Case Study
In May 2019, the New England Journal of Medicine published a case study describing the power and limits of classifying sex and gender within medicine (1). Sam, 32 years old, presented to an emergency department with severe and intermittent abdominal pain. Despite disclosing his transgender identity, the electronic medical system indicated his affirmed gender, and therefore, medical staff evaluated him as a man with a non-urgent condition. Several hours later, Sam delivered a stillborn baby. This tragic case begs the following questions: What are the healthcare experiences of transgender and gender-expansive (TGE) individuals with sexual and reproductive health (SRH) needs? What is the empirical evidence supporting the needs of this population? What is the frequency of cases like Sam's? Most importantly, what do clinicians and researchers need to learn from this case to prevent SRH injustices from reoccurring? Selected studies were compared and summarized by the authors, leading to our suggestions and recommendations for treating TGE youth, which may then prevent adults, such as Sam, from experiencing poor medical care.
Introduction
SRH healthcare is often conceptualized as “women's” or “men's” health services, which may be excluding many people from seeking care. Using the inclusive umbrella term will allow health care professionals to use an organ inventory as opposed to the currently used, often binary, options (2). Health care professionals should be sensitive and understand how gender, as opposed to sex assigned at birth, can directly affect clinical practice. Those who identify as transgender have a gender identity that differs from the sex that was assigned at birth; those who identify as non-binary may have a more complex, fluid, multifaceted, or otherwise less clearly defined gender than a transgender person (3). Those who identify as transgender can be further divided into two groups: transgender women (assigned male at birth) and transgender men (assigned female at birth). Although often incorporated into the same broad “sexual and gender minority” category, TGE individuals have healthcare needs that are distinct from those who identify as lesbian, gay, and bisexual (LGB). LGB issues are often interpersonal, related to their relationships with others, while gender issues are intrapersonal, with an emphasis on an individual's identity and self-expression. This distinction is rarely emphasized in the literature (4). Furthermore, TGE individuals have unique SRH health needs, but are often excluded from gynecological and reproductive practices, as current guidelines and recommendations exist within a gender binary, heteronormative system, catering care to those who identify as heterosexual and cisgender (5). Awareness and visibility of transgender individuals have exponentially increased over recent years. Multiple reviews and commentaries have been published on the topic of SRH care under the umbrella term of “sexual and gender minorities”, (6–16) and include a call to action for more inclusive care and clinical research involving TGE individuals. However, TGE youth face unique barriers in receiving care and this subset population remains vastly under-researched. This review will discuss barriers to care for TGE adolescents and young adults, emphasizing the unique SRH care needs of this population and ultimately providing recommendations for U.S. clinicians and researchers with the goal of improving SRH care for TGE youth.
The prevalence of TGE individuals, particularly adolescents, remains relatively undefined and existing data are likely underestimated (17, 18). The American College of Obstetrics and Gynecology Committee Opinion published in March 2021 estimated 150,000 youth and 1.4 million adults living in the U.S. identify as transgender (19). Previous estimates include data from: (1) The 2011 National Transgender Discrimination Survey (20) which included 6,450 participants ages 18 to 89 and found that 33% of respondents did not identify as exclusively male or female, and 14% identified as gender-nonconforming; and (2) The 2015 U.S. Transgender Survey (18) which included 27,715 participants over 18 years old with 31% identifying as non-binary. As social stigma decreases and education surrounding sex and gender increases, (21) the prevalence of adolescents identifying as a gender other than cisgender has been increasing (3% in 2018) (22). However, according to the Harris Poll, (23) 2019 societal acceptance decreased and was accompanied by an increase in LGBTQ discrimination because of sexual orientation or gender identity (24). This is thought to be a product of a lack of non-discrimination laws for the LGBTQ community and the political and cultural divide brought on by the election year of 2016. Transgender, and specifically non-binary adolescent populations, are underrepresented in clinical and biomedical research and as a result, vast knowledge gaps exist.
The Problem: Barriers to Care
TGE youth encounter significant interpersonal and structural barriers to receipt of high-quality healthcare, including discrimination, lack of clinician knowledge and health systems obstacles. TGE youth often experience social stigma, harassment, and rejection, and unlike adults, TGE youth are embedded in families and schools which may make such stigma difficult to escape (25). Health care settings are often sites of mistreatment, where discriminatory practices range from refusal of care to verbal, physical or sexual abuse (26). A secondary analysis from the 2015 U.S. Transgender Survey (N = 19,157) found that almost one-quarter of transgender adults avoided healthcare due to anticipated discrimination, with the highest prevalence among transgender men (27). The intimate nature of SRH makes this issue particularly acute: 33% of transgender people and 48% of transgender men have delayed healthcare or avoided preventive measures (e.g., pelvic exams or STI screening) out of fear of discrimination or disrespect (28). Compared to cisgender, LGB-identifying individuals, transgender adults are more likely to delay care and report negative effects of disclosure to their clinician (29). Racial disparities also exist, as transgender people of color experience significantly higher levels of transphobic discrimination compared to their White counterparts in accessing health services (30). Barriers to care are even more pronounced and complex for transgender youth who are reliant on parental support and insurance coverage for care. A 2016 study aimed at understanding perceived barriers to care among transgender youth (ages 14–22 years) and their caregivers identified six themes (31): (1) few accessible pediatric providers are trained in gender-affirming health care; (2) lack of consistently applied protocols; (3) inconsistent use of chosen name/pronoun; (4) uncoordinated care and gatekeeping; (5) limited/delayed access to pubertal blockers and cross-sex hormones; and (6) insurance exclusions.
The lack of adequate clinician training is one of the most often cited barriers to quality care for TGE populations (32). The 2011 National Transgender Discrimination Survey found that 50% of respondents reported having to teach their clinicians about their own healthcare needs that may be specific to TGE individuals, such as hormone usage, reproductive conditions and menstruation suppression (20). Researchers have responded by surveying clinicians about their knowledge and attitudes towards caring for TGE individuals. (33, 34) A 2015 survey of 141 obstetrician-gynecologists across nine academic hospitals found that 80% did not receive training in residency regarding the care of transgender patients; only 35% and 29% felt comfortable caring for male-to-female and female-to-male transgender patients, respectively (33). The findings from another recent study are equally discouraging (35); of the 169 board-certified obstetrician-gynecologists surveyed in 2018, less than half (43%) reported training specific to the healthcare needs of LGB or TGE individuals. Moreover, this study found previous clinician training was not associated with increased comfort in taking care of TGE patients. Mounting research suggests that increasing hours of TGE health education is not sufficient; rather, future training should address personal biases and internalized transphobia (36).
Structural inequities imbedded within the healthcare system can limit access to healthcare for transgender people. Many transgender individuals lack health insurance, which may be partially due to the higher prevalence of unemployment and poverty faced by these individuals relative to the general US population (37). TGE adolescents and young adults are at a further disadvantage, as they are reliant on their parents for not only insurance coverage (31, 38) but also support of their gender identity, which they often do not have (39). As a result, transgender individuals, particularly youth, are disproportionately represented in the homeless population (40). Even for those individuals and families who are insured, barriers persist, as private insurers have historically excluded coverage for medical interventions related to gender affirmation and transition (41). A study examining barriers to gender transition-related healthcare in Massachusetts found that mental health coverage emerged as one of the factors most strongly associated with an inability to access care (42). Previously, a diagnosis of gender dysphoria by a mental health professional was required before approval was granted to cover gender affirming therapy or surgery (43). With new informed consent models, patients are able to access gender-affirming hormones through their primary care clinician without a diagnosis of gender dysphoria, (44) which is the feeling of discomfort or distress that might occur in people whose gender identity differs from their sex assigned at birth or sex-related physical characteristics. However, not all clinics use informed consent models, and most insurers still require a diagnosis for those seeking gender affirming surgery. Similarly, electronic health records (EHRs) may pose as a structural barrier if gender identity is not included as an important variable to care. For example, birth sex auto-populates medical recommendations for clinicians that may be needed for a person assigned female or male at birth during specific ages (e.g., menstruation preparation, prostate exam). Including both sex and gender as important clinical variables in EHRs could aid in decreasing both structural and interpersonal barriers for TGE youth and young adults when receiving SRH care (45). Advocacy work is needed to eliminate roadblocks to accessing medically necessary transition-related care for TGE youth across the U.S (46).
These barriers to healthcare result in increased health risk and an increased likelihood of negative health outcomes for an already vulnerable population. The consequences of inadequate care are staggering. According to one retrospective cohort study, 56% of youth who identified as transgender reported previous suicidal ideation, and 31% reported a previous suicide attempt, compared with 20% and 11% among matched youth who identified as cisgender, respectively (12). The social and economic marginalization and abuse experienced by TGE individuals has been shown to increase these health risks (47). It is imperative that clinicians, researchers and public health officials collaborate to mitigate these barriers and improve both access and quality of care for this population.
The Role of the Obstetrician-Gynecologist
Current Expectations
As highlighted above, lack of adequate provider training often poses a significant barrier to TGE individuals obtaining sensitive SRH care. Thus, gynecologists striving to provide inclusive SRH care should be informed on the reproductive health needs and considerations of all genders, not only those who are cisgender. In 2011, the American College of Obstetricians and Gynecologists assembled a committee to assist gender-diverse individuals in obtaining routine treatment and screening, as well as gender-affirming care needs (48). Transgender males who have internal and external female anatomy will need standard SRH care such as contraception counseling, reproductive health education, breast, and gynecologic cancer screenings, STI testing, and menstrual management. However, it is important for obstetrician-gynecologists to understand the various options for hormonal and surgical gender affirmation, as these interventions impact the SRH needs and considerations of TGE individuals. The following section first defines medical options to affirm gender and thereafter explores implications across key SRH domains.
Medical Options to Affirm Gender
Delaying pubertal changes through administration of gonadotropin-release hormone (GnRH) agonists, may decrease discomfort and improve quality of life while creating time and space for gender identity exploration (7). New evidence suggests that affirming interventions during adolescence improve psychosocial outcomes, such as decreasing suicidality and increasing attainment of higher education, employment, and reliable housing (49). Pubertal suppression may also reduce the need for later surgery because physical changes that are otherwise irreversible (protrusion of the Adam's apple, male pattern baldness, voice change, breast growth, etc.) are prevented (50). Gender affirming hormones (GAH), (i.e., testosterone and estrogen), enable TGE individuals to gain characteristics that match their gender identity. The most recent Endocrine Society guidelines indicate that medications can be started in patients younger than 16 years old (51). A wide range of gender-affirming surgeries (previously referred to as gender reassignment surgeries) are also available to TGE individuals such as feminizing vaginoplasty, masculinizing phalloplasty, metoidioplasty (clitoral enlargement), as well as face and voice procedures (52).
Sexual Desire and Function
TGE youth who may or may not be receiving medications for transition are often exploring their sexual identity and sexual pleasure. TGE receiving GAH, such as pubertal suppression and cross-sex hormones, may experience side effects from these medications that impact their sexual health. For example, a multicenter one-year prospective clinical trial of 53 trans men and 53 trans women receiving GAH showed a significant increase in sexual desire and clitoral pain in trans men receiving testosterone (53). Trans women in this study reported decreased sexual desire as a side effect of decreased testosterone concentrations. TGE youth taking pubertal suppression medication may also experience decreased libido as a side effect (54). Gender affirming surgeries also impact sexual functioning. A study examining the outcomes of vaginoplasty, the procedure that restructures the head of the penis into a clitoris and creates a vaginal cavity, found that 90% of trans females who had the surgery reported that they were still able to have an orgasm with 75% reporting that their orgasms were either the same or more intense than before (55). Research on procedures for trans men (e.g., phalloplasty and metoidioplasty), have shown generally positive outcomes; however, for some decreased phallic sensation and the inability to penetrate negatively impacted sexual wellbeing (56). Those using puberty blockers or testosterone/estrogens may be navigating changes to libido. When counseling trans men, clinicians should discuss how patients might develop pleasurable sex and how erogenous stimulation may have to be rediscovered. Youth, particularly TGE youth, show variable amounts of comfort with discussing physical intimacy and sexual intercourse with peers, partners, and providers and may not even know what questions to ask (57).
Menstruation
Menstruation may lead to dysphoria for TGE youth with female anatomy (58). A recent survey of TGE adults with masculine identities showed mixed attitudes toward menstruation, with most reporting feeling unsafe and uncomfortable using men's restrooms during times of menstruation (59). Medications that lead to cessation of menses can be an important first step in gender-affirming care and may be used on their own or with GAH. This may be helpful for TGE youth who do not have access to GAH therapy, as there are no documented adverse outcomes, and only benefits reported with respect to an individual's quality of life (60–63).
Contraception
All transgender people who have gonads and engage in sexual activity that could result in pregnancy should be counseled on the need for contraception (64). GAH should not be used as a form of contraception. Particularly, testosterone, a known teratogen, may lead to abnormalities of physiological development of the embryo if a patient becomes pregnant (65). Unintended pregnancies have occurred in transgender men receiving testosterone. Therefore, contraceptive needs should be addressed, especially in patients who have maintained their uterus (66). Moreover, some TGE individuals may be at risk for engaging in high-risk sexual behavior. Specifically, TGE youth are at high risk for sexual abuse and engaging in commercial or survival sex, (67) increasing the need for appropriate contraceptive counseling and sexually transmitted infection protection. The interpersonal and structural barriers to high-quality healthcare outlined above have led to contraception access issues, including the inability to afford services, lack of clinicians with expertise in gender-affirming therapy, difficulty in securing health insurance, and misconceptions about unintended pregnancy (68). Health care professionals, and those who care for adolescents, need to be aware of who may require and should receive advice about pregnancy prevention and contraception. Rather than assuming a patient's sexual orientation, clinicians should take a thorough sexual history based on the patient's identity and anatomy, with the understanding that gender identity does not determine sexuality (69). Additionally, clinicians and researchers should be aware and sensitive to issues that may affect gender and sexual health, notably gender affirming-hormone therapies that may affect fertility and libido.
Pregnancy
Numerous studies have documented increased pregnancy rates in adolescent sexual and gender minorities compared with their heterosexual counterparts, with an estimated increased risk of adolescent pregnancy rate between 2 and 10 times (56, 70–72). This finding may be explained by a broad spectrum of sexual health risks experienced by TGE individuals, including an earlier age of first sexual intercourse, exposure to sexual abuse, and a higher number of sexual partners (73). TGE youth face conflict with their gender identity and potentially their sexual orientation. It is likely that their experience is similar to cisgender LGB adolescents as it pertains to reproductive health considerations. As outlined, the principles of obstetrical practice regarding pregnancy in a transgender male are not complex once a clinician has received appropriate training. However, the barriers to care and societal discrimination may cause pregnancy-related psychological distress. Two studies highlight both psychological issues experienced by transgender men contemplating pregnancy or bearing a child, as well as the unique medical implications for both the parent and fetus (66, 74). Similar to pregnancy research in TGE youth, few data exist on abortions in this population. Abortion-providing clinicians and advocates have long recognized the need for high-quality, gender-affirming care for their patients, although little is known about these services at facilities that provide abortions (75). Current abortion care should be adapted to include and affirm the experiences of this underserved population (76).
Fertility Options and Attitudes
TGE individuals, similar to cisgender people, may want to become pregnant and reproductive desire has found to be high among transgender individuals. A recent Australian study surveyed 409 transgender and non-binary adults and found that, of participants who were not already parents, 33% hoped to have children in the future (77). A 2016 survey (n = 156) showed 71% of transgender and non-binary people surveyed were interested in adoption and 35.9% in biological parenthood (63). More gender nonconforming youth (44%) than transgender youth (26%) expressed interest in biological fertility. Medical interventions, such as GAH and surgeries, pose significant risk to reproductive potential and fertility outcomes. Specifically, the long-term effects of GAH on reproductive function are unknown (78). The World Professional Association of Transgender Health, the American Society for Reproductive Medicine, and the Endocrine Society recommend that all transgender patients be counseled on options for fertility preservation prior to initiating gender-affirming surgeries or hormonal transition (78–80). There are relatively limited data specific to fertility preservation for transgender individuals and current approaches are extrapolated from options for fertility preservation after oncologic diagnoses (80).
Options for individuals assigned female at birth vary by pubertal status and include embryo and oocyte cryopreservation, both of which are established in practice (81). Notably, both oocyte and embryo cryopreservation require controlled ovarian stimulation with repeated assessment by transvaginal ultrasound, which may be uncomfortable or emotionally distressing for these patients (80). Transgender men who have already initiated GAH therapy (testosterone) may still pursue oocyte or embryo cryopreservation (80). Recent findings have shown ovarian tissue cryopreservation to be a promising option. In 2019, the American Society of Reproductive Medicine opinion report on fertility preservation stated: “ovarian tissue cryopreservation is no longer considered experimental should be considered an established medical procedure” (82). A recent study showed that ovarian tissue does not seem to be morphologically affected by prolonged testosterone treatment; (83) however, there are conflicting data in the literature (84) and more research is needed in this area. Despite potential interventions, the use of reproductive options is surprisingly low (85). Some transgender adolescents have expressed discomfort with the idea of using their own body parts for reproduction (63) and oocyte cryopreservation has been shown to be associated with worsening gender dysphoria (86). Youth in these studies also identified cost, desire not to delay medical transition, and future plans to adopt children or no desire to have children as reasons for declining fertility preservation.
Endometriosis
The SRH community has become increasingly aware of how TGE youth are experiencing complications of gynecologic organs. For example, transgender male adolescents have a uterus and ovaries leaving them susceptible to developing painful gynecological medical conditions such as endometriosis. This common gynecological disease, leads to chronic pelvic pain, decreased quality of life, (87) and has the proclivity to adversely affect choices surrounding fertility options. In addition, endometriosis negatively impacts social/romantic relationships and sexual intimacy (88). Endometriosis in adolescence, the typical period of symptom onset, (87) is an even more challenging problem as the disease may present with several clinical and pathological differences that are not observed in adult women (89). This disease affects at least 10% of cisgender women of reproductive age, although endometriosis also affects TGE people. To date, only one study has examined the prevalence, presentation, and impact of endometriosis in non-binary youth (90) with the conclusion that evaluation for endometriosis is underutilized when transgender youth present with pelvic pain and dysmenorrhea. Even for those with a known diagnosis, GAH therapy may not remedy endometriosis-associated pain. The impact of endometriosis must be considered for TGE youth in the context of the interpersonal and structural barriers to accessing SRH care, as outlined above. Further research is warranted regarding endometriosis and other gynecologic conditions in TGE individuals, particularly adolescents, to improve quality of care for this population.
Recommendations for Providing Gender-Affirming SRH Care to TGE Adolescents
Adolescent medicine clinicians and researchers can lead the way in providing affirming and empowering care at a time when individuals are becoming aware of and developing their gender identities and sexual orientations. The gender-affirmative care model supports gender diversity as a normal part of human development, compared the others that may treat gender diversity as a disorder (6). The model uses strengths-based terminology, which emphasize an individual's self-determination and autonomy (Table 1). All clinical office staff also play a role in affirming a patient's gender identity. Frontline staff such as receptionists and clinical assistants can be involved in creating an affirming environment. Clinicians and staff should make direct and non-judgmental inquiries about a patient's experience and feelings before applying any labels. Thereafter, a patient-asserted name and pronouns should be used by staff and are ideally reflected in the electronic medical record without creating duplicate charts. In the clinical environment, making flyers available or displaying posters related to LGBTQ health issues, including information for children who identify as TGE and families, reveals inclusivity and awareness (50).
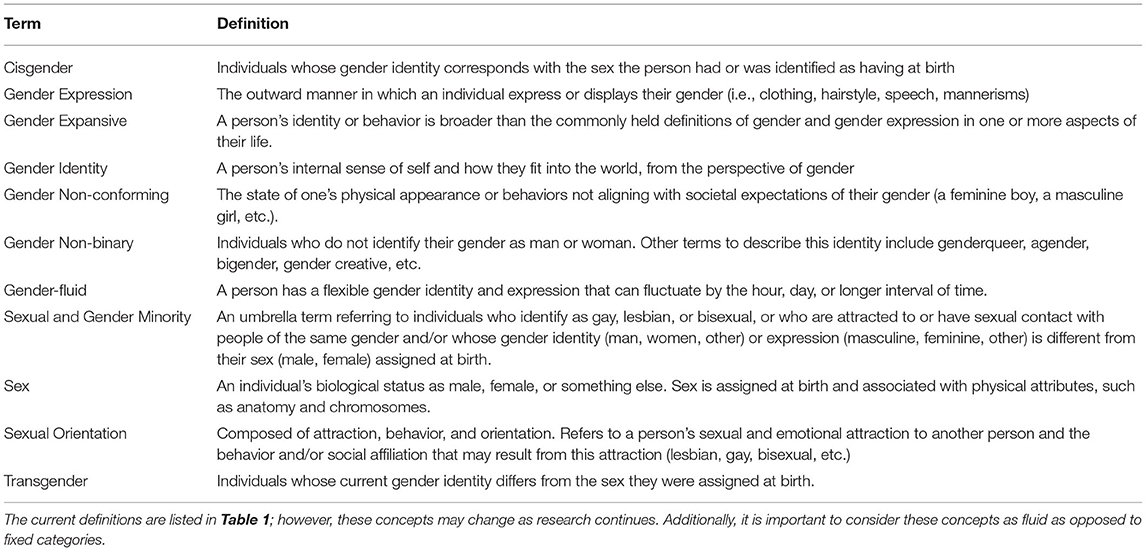
Table 1. Relevant terms and definitions defined by the World Health Organization's glossary for terms and tools for providing gender-affirmative care.
Support from a multidisciplinary and collaborative health care team would greatly improve health outcomes for TGE youth (91). Since 2007, when the first multidisciplinary gender clinic was established within a pediatric institution, (92) the number of such pediatric subspecialty programs has grown significantly (93). Despite the growing number of clinics, these valuable, affirming spaces remain inaccessible to some. Moreover, existing clinics often have high patient volumes leading to long waiting periods to be seen by a clinician. Gender affirming care may not always lead to gynecology referral as most care falls under the umbrella of primary care (69, 94). A 2016 study aimed at understanding perceived barriers to care among transgender youth (ages 14–22 years) and their caregivers also identified the following recommendations: (1) development of protocols for the care of young transgender patients, as well as roadmaps for families; (2) increased number of multidisciplinary gender clinics; (3) providing cross-sex hormones at an age that permits peer-congruent development; and (4) designating a navigator for transgender patients in clinics (31). An assessment of patient/caregiver satisfaction at a pediatric multidisciplinary gender clinic in Seattle, WA found that families were highly satisfied with multidisciplinary, coordinated health care with respondents endorsing the presence of a Care Navigator as integral to providing support to families during a process often fraught with barriers and emotional stress (95).
Re-conceptualizing outdated terminology may also serve to create an affirming environment. For example, endometriosis researchers have suggested relabeling the condition with the term “gendered disability”, as this is a more accurate depiction of the science and lived experiences of those with endometriosis (96). Additionally, researchers call for shifting the language used to describe endometriosis (96–98): (1) Discuss uteruses/ovaries/penises and other body parts without assigning them a gender; (2) Use phrases like “internal/external reproductive organs”; (3) Use language such as “people who menstruate/are pregnant/ produce sperm;” and (4) Use “cisgender” rather than “biologically female/male”; (5) Use people with endometriosis instead of women or patients; (6) Refer to endometriosis family/siblings/friends, instead of ladies/sisters/cysters; and (7) Discuss endometriosis as a system-wide, gendered disability that impacts the organs, nervous system, cognitive abilities, mood, respiration, circulation, and digestive functions as well as the reproductive system.
Sexual and gender minority people, including members of the lesbian, gay, bisexual, transgender, and queer communities, are understudied and underrepresented in research. Recent studies have shed light on the LGBTQ community's perspective on how SGMs are addressed in current studies (99). Findings from focus groups and qualitative studies have revealed: (1) sexual and gender questions did not allow for identity fluidity and complexity, reducing inclusion and representation; and (2) question stems and answer choices were often not clear as to whether gender identity or sexual orientation were being assessed (100). Measurement error from imprecise survey questions impose biases. A recent study aimed at the development of an affirming and customizable electronic survey of SRH experiences found that: (1) TGE community input from initial conceptualization to final implantation is essential; (2) investigators need to be mindful of gender-diversity and differences in sexual orientation when defining study eligibility criteria to directly reduce selection bias; and (3) the ability to use individualized, affirming, customized language for sexual and reproductive body parts and processes may avoid gender dysphoria evoked for some by medical terms (101). Lessons learned from these findings may inspire other researchers to innovate and think more inclusively, thereby creating affirming research for marginalized groups, such as TGE youth and adults. See Table 2 for a synthesized summary of published recommendations for clinicians and researchers with the benefit of the patient described.
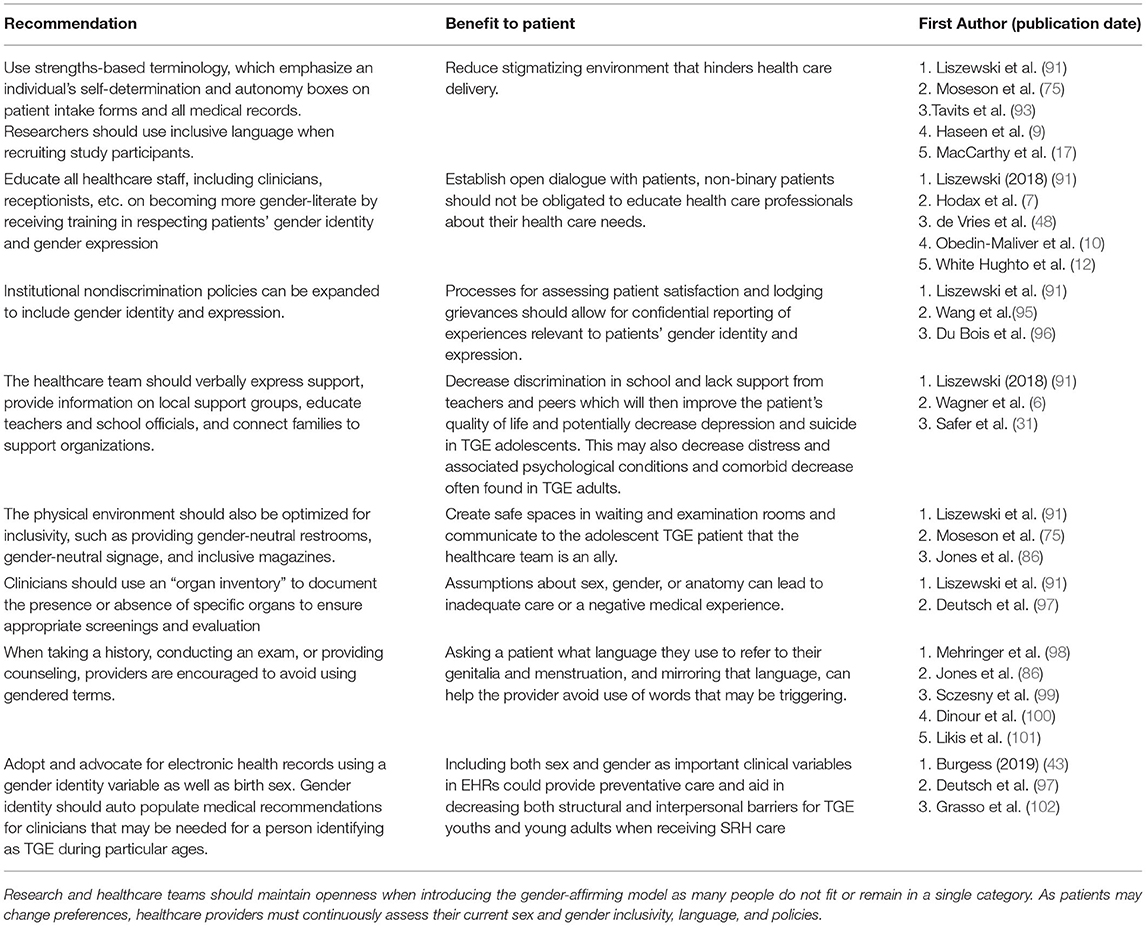
Table 2. Suggestions for clinicians and researchers for providing care using the gender-affirming care model with the described patient benefit and source of recommendation.
Discussion
Women's health and men's health should be described as sexual and reproductive health. TGE individuals have been largely excluded from clinical care and clinical research leading to large gaps in knowledge regarding their experiences, options, and needs in both settings. Extrapolating data from other populations (e.g., solely transgender data, solely adult data) may not lead to accurate conclusions. Thus, research catering to TGE adolescents, young adults, and non-binary individuals, would be beneficial to the field of SRH. Obstetrician-gynecologists and other clinicians who specialize in gynecological care should assume their role in the care of TGE adolescents and young adults while maintaining awareness of the consequences of inadequate care, and the many existing interpersonal and structural barriers to receiving high quality SRH care. Adolescent clinicians and researchers can lead the way in providing affirming and empowering care at a time when individuals are becoming aware of and developing their gender identities and sexual orientations.
Inclusive clinical care and research that addresses the relationship between sex assigned at birth, gender identity and social determinants of health are crucial to achieving health equity (102). Commonly used or validated measures of sexual and reproductive health experiences typically use heteronormative and cis-normative assumptions and language, such as the types of sex people are having; (4, 103) the gender, sex assigned at birth, and current organs of people's partners; and their capacity for pregnancy (98). Clinical care and research are interconnected, as questions that arise in clinical care motivate and drive research, and research subsequently informs the standard of care and new healthcare policies. TGE youth greatly need wider representation in both settings.
Author Contributions
CL and RS conducted the literature review and wrote the first draft of the manuscript. CG and CS contributed to manuscript preparation. All authors made a significant contribution to the work reported, whether that is in the conception, and took part in drafting, revising or critically reviewing the article gave final approval of the version to be published have agreed on the journal to which the article has been submitted and agree to be accountable for all aspects of the work. All authors contributed to the article and approved the submitted version.
Funding
Support was provided by awards to CG – MCHP T71MC00009 LEAH training grant (HRSA/HHS) and R01 from the Eunice Kennedy Shriver NICHD (R01 HD101421); and CS – K23 Career Development (GM123372) & Supplement (GM123372-04S1) Awards from NIH, a Peer Review Medical Research Program Investigator-Initiated Research Award from the United States Department of Defense (W81XWH19105060); and support from the Boston Center for Endometriosis/Marriott Family Foundation.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Stroumsa D, Roberts EFS, Kinnear H, Harris LH. The power and limits of classification — A 32-year-old man with abdominal pain. New Engl J Med. (2019) 380:1885–8. doi: 10.1056/NEJMp1811491
2. Rosendale N, Goldman S, Ortiz GM. Harber, LA. Acute clinical care for transgender patients: a review. JAMA Internal Med. (2018) 178:1535–43. doi: 10.1001/jamainternmed.2018.4179
3. Terminology and definitions | Transgender Care. Available online at: https://transcare.ucsf.edu/guidelines/terminology. (accessed January 23, 2021)
4. Meyer IH. Why lesbian, gay, bisexual, and transgender public health? Am J Public Health. (2001) 91:856–9. doi: 10.2105/AJPH.91.6.856
5. Sbragia JD, Vottero B. Experiences of transgender men in seeking gynecological and reproductive health care: a qualitative systematic review protocol. JBI Database Systemat Rev Implement Rep. (2019) 17:1582–8. doi: 10.11124/JBISRIR-2017-004029
6. Wagner J, Sackett-Taylor AC, Hodax JK, Forcier M, Rafferty J. Psychosocial overview of gender-affirmative care. J Pediatr Adolesc Gynecol. (2019) 32:567–73. doi: 10.1016/j.jpag.2019.05.004
7. Hodax JK, Wagner J, Sackett-Taylor AC, Rafferty J, Forcier M. Medical options for care of gender diverse and transgender youth. J Pediatr Adolesc Gynecol. (2020) 33:3–9. doi: 10.1016/j.jpag.2019.05.010
8. Committee Opinion No. 685: Care for transgender adolescents. Obstetrics Gynecol. (2017) 129:e11–6.
9. Haseen B, Kahn A, Belton A, Bayer CR. Health care for transgender men: what is missing in OB/GYN Care? J Low Genit Tract Dis. (2020) 24:232–3. doi: 10.1097/LGT.0000000000000507
10. Obedin-Maliver J. Time for OBGYNs to care for people of all genders. J Women's Health. (2015) 24:109–11. doi: 10.1089/jwh.2015.1518
11. Leonardi M, Frecker H, Scheim AI, Kives S. Reproductive health considerations in sexual and/or gender minority adolescents. J Pediatr Adolesc Gynecol. (2019) 32:15–20. doi: 10.1016/j.jpag.2018.09.010
12. White Hughto JM, Reisner SL, Pachankis JE. Transgender stigma and health: A critical review of stigma determinants, mechanisms, and interventions. Soc Sci Med. (2015) 147:222–31. doi: 10.1016/j.socscimed.2015.11.010
13. Jarin J. The Ob/Gyn and the transgender patient. Curr Opin Obstetrics Gynecol. (2019) 31:298–302. doi: 10.1097/GCO.0000000000000562
14. Kanj RV, Conard LAE, Trotman GE. Menstrual suppression and contraceptive choices in a transgender adolescent and young adult population. J Pediatr Adolesc Gynecol. (2016) 29:201–2. doi: 10.1016/j.jpag.2016.01.100
15. Dutton L, Koenig K, Fennie K. Gynecologic care of the female-to-male transgender man. J Midwifery Women's Health. (2008) 53:331–7. doi: 10.1016/j.jmwh.2008.02.003
16. Light A, Wang LF, Zeymo A, Gomez-Lobo V. Family planning and contraception use in transgender men. Contraception. (2018) 98:266–9. doi: 10.1016/j.contraception.2018.06.006
17. MacCarthy S, Reisner SL, Nunn A, Perez-Brumer A, Operario D. The time is now: attention increases to transgender health in the United States but scientific knowledge gaps remain. LGBT Health. (2015) 2:287–91. doi: 10.1089/lgbt.2014.0073
18. Meerwijk EL, Sevelius JM. Transgender population size in the United States: a meta-regression of population-based probability samples. Am J Public Health. (2017) 107:e1–8. doi: 10.2105/AJPH.2016.303578
19. Bonnington A, Dianat S, Kerns J, Hastings J, Hawkins M, De Haan G, et al. Society of Family Planning clinical recommendations: Contraceptive counseling for transgender and gender diverse people who were female sex assigned at birth. Contraception. (2020) 102:70–82. doi: 10.1016/j.contraception.2020.04.001
20. Grant JM, Mottet LA, Tanis J, Harrison J, Herman J, Keisling M. Injustice at every turn a report of the national transgender discrimination survey. Accelerating Acceptance. (2017).
21. Polaris Teen Center. More Teens Identify as Transgender in the U.S. - Polaris Teen Center. Published (2019). Available online at: https://polaristeen.com/articles/transgender-teens-america/. (accessed February 19, 2021)
22. Ellis SK. Accelerating Acceptance 2019. Published (2019). Available online at: https://www.glaad.org/sites/default/files/Accelerating Acceptance 2019.pdf. (accessed February 19, 2021)
23. Gruberg S, Mahowald L, Halpin J. The State of the LGBTQ Community in 2020 - Center for American Progress. Published October 6, (2020). Available online at: https://www.americanprogress.org/issues/lgbtq-rights/reports/2020/10/06/491052/state-lgbtq-community-2020/ (accessed February 19, 2021)
24. Simons L, Voss R. Advocating for transgender and gender expansive youth in the emergency setting. Clin Pediatr Emerg Med. (2020) 21:100780. doi: 10.1016/j.cpem.2020.100780
25. James SE, Herman JL, Rankin S, Keisling M, Mottet L, Anafi M. About the National Center for Transgender Equality. (2016)
26. Kcomt L, Gorey KM, Barrett BJ, McCabe SE. Healthcare avoidance due to anticipated discrimination among transgender people: a call to create trans-affirmative environments. SSM - Population Health. (2020) 11:100608. doi: 10.1016/j.ssmph.2020.100608
27. Rachlin K, Green J, Lombardi E. Utilization of health care among female-to-male transgender individuals in the United States. J Homosex. (2008) 54:243–58. doi: 10.1080/00918360801982124
28. MacApagal K, Bhatia R, Greene GJ. Differences in healthcare access, use, and experiences within a community sample of racially diverse lesbian, gay, bisexual, transgender, and questioning emerging adults. LGBT Health. (2016) 3:434–42. doi: 10.1089/lgbt.2015.0124
29. Kattari SK, Walls NE, Whitfield DL, Langenderfer-Magruder L. Racial and ethnic differences in experiences of discrimination in accessing health services among transgender people in the United States. Int J Transgenderism. (2015) 16:68–79. doi: 10.1080/15532739.2015.1064336
30. Gridley SJ, Crouch JM, Evans Y, Eng W, Antoon E, Lyapustina M, et al. Youth and caregiver perspectives on barriers to gender-affirming health care for transgender youth. J Adolesc Health. (2016) 59:254–61. doi: 10.1016/j.jadohealth.2016.03.017
31. Safer JD, Coleman E, Feldman J, Garofalo R, Hembree W, Radix A, et al. Barriers to healthcare for transgender individuals. Curr Opin Endocrinol Diabetes Obes. (2016) 23:168–71. doi: 10.1097/MED.0000000000000227
32. Unger CA. Care of the transgender patient: a survey of gynecologists' current knowledge and practice. J Women's Health. (2015) 24:114–8. doi: 10.1089/jwh.2014.4918
33. Kitts RL. Barriers to optimal care between physicians and lesbian, gay, bisexual, transgender, and questioning adolescent patients. J Homosex. (2010) 57:730–47. doi: 10.1080/00918369.2010.485872
34. Mehta PK, Easter SR, Potter J, Castleberry N, Schulkin J, Robinson JN. Lesbian, gay, bisexual, and transgender health: Obstetrician-gynecologists' training, attitudes, knowledge, and practice. J Women's Health. (2018) 27:1459–65. doi: 10.1089/jwh.2017.6912
35. Stroumsa D, Shires DA, Richardson CR, Jaffee KD, Woodford MR. Transphobia rather than education predicts provider knowledge of transgender health care. Med Educ. (2019) 53:398–407. doi: 10.1111/medu.13796
36. Dickey LM, Katz-Wise SL, Budge SL, Garza MV. Health disparities in the transgender community: Exploring differences in insurance coverage. Psychol Sex Orientat Gender Diversity. (2016) 3:275–82. doi: 10.1037/sgd0000169
37. Dowshen NL, Christensen J, Gruschow S. Health insurance coverage of recommended gender-affirming health care services for transgender youth: shopping online for coverage information. Transgender Health. (2019) 4:131–5. doi: 10.1089/trgh.2018.0055
38. Katz-Wise SL, Rosario M, Tsappis M. Lesbian, gay, bisexual, and transgender youth and family acceptance. Pediatr Clin North Am. (2016) 63:1011–25. doi: 10.1016/j.pcl.2016.07.005
39. Fraser B, Pierse N, Chisholm E, Cook H. LGBTIQ+ homelessness: a review of the literature. Int J Environ Res Public Health. (2019) 16:2677. doi: 10.3390/ijerph16152677
40. Bakko M, Kattari SK. Transgender-related insurance denials as barriers to transgender healthcare: differences in experience by insurance type. J Gen Intern Med. (2020) 35:1693–700. doi: 10.1007/s11606-020-05724-2
41. White Hughto JM, Rose AJ, Pachankis JE, Reisner SL. Barriers to gender transition-related healthcare: identifying underserved transgender adults in massachusetts. Transgender Health. (2017) 2:107–18. doi: 10.1089/trgh.2017.0014
42. Meyer W, Bockting WO, Cohen-Kettenis P, Coleman E, Diceglie D, Devor H, et al. The harry benjamin international gender dysphoria association's standards of care for gender identity disorders, sixth version. J Psychol Human Sex. (2002) 13:1–30. doi: 10.1300/J056v13n01_01
43. Deutsch MB. Use of the informed consent model in the provision of cross-sex hormone therapy: a survey of the practices of selected clinics. Int J Transgenderism. (2012) 13:140–6. doi: 10.1080/15532739.2011.675233
44. Burgess C, Kauth MR, Klemt C, Shanawani H, Shipherd JC. Evolving sex and gender in electronic health records. Federal Practitioner. (2019) 36:271–7.
45. Human Rights Campaign. Finding Insurance for Transgender-Related Healthcare - HRC. Available online at: https://www.hrc.org/resources/finding-insurance-for-transgender-related-healthcare. (accessed January 23, 2021)
46. Almeida J, Johnson RM, Corliss HL, Molnar BE, Azrael D. Emotional distress among lgbt youth: the influence of perceived discrimination based on sexual orientation. J Youth Adolesc. (2009) 38:1001–14. doi: 10.1007/s10964-009-9397-9
47. Stroumsa D. The state of transgender health care: policy, law, and medical frameworks. Am J Public Health. (2014) 104:e31. doi: 10.2105/AJPH.2013.301789
48. de Vries ALC, McGuire JK, Steensma TD, Wagenaar ECF, Doreleijers TAH, Cohen-Kettenis PT. Young adult psychological outcome after puberty suppression and gender reassignment. Pediatrics. (2014) 134:696–704. doi: 10.1542/peds.2013-2958
49. Rafferty J. Ensuring comprehensive care and support for transgender and gender-diverse children and adolescents. Pediatrics. (2018) 142:e20182162. doi: 10.1542/peds.2018-2162
50. Hembree WC, Cohen-Kettenis PT, Gooren L, Hannema SE, Meyer WJ, Murad MH, et al. Endocrine treatment of gender-dysphoric/gender-incongruent persons: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. (2017) 102:3869–903. doi: 10.1210/jc.2017-01658
51. Overview of gender-affirming treatments and procedures | Transgender Care. Available online at: https://transcare.ucsf.edu/guidelines/overview. (accessed February 1, 2021)
52. Wierckx K, Caenegem EV, Schreiner T, Haraldsen I, Fisher AD, Tove K, et al. Cross-sex hormone therapy in trans persons is safe and effective at short-time follow-up: results from the European network for the investigation of gender incongruence. J Sex Med. (2014) 11:1999–2011. doi: 10.1111/jsm.12571
53. Guss C, Shumer D, Katz-Wise SL. Transgender and gender nonconforming adolescent care: psychosocial and medical considerations. Curr Opin Pediatr. (2015) 26:421. doi: 10.1097/MOP.0000000000000240
54. Hess J, Henkel A, Bohr J, Rehme C, Panic A, Panic L, et al. Sexuality after male-to-female gender affirmation surgery. Biomed Res Int. (2018) 2018:9037979. doi: 10.1155/2018/9037979
55. Grift TC, van de Pigot GLS, Kreukels BPC, Bouman M-B, Mullender MG. Transmen's experienced sexuality and genital gender-affirming surgery: findings from a clinical follow-up study. J Sex Marital Therapy. (2019) 45:201–5. doi: 10.1080/0092623X.2018.1500405
56. Haley SG, Tordoff DM, Kantor AZ, Crouch JM, Ahrens KR. Sex education for transgender and non-binary youth: previous experiences and recommended content. J Sex Med. (2019) 16:1834–48. doi: 10.1016/j.jsxm.2019.08.009
57. Frank SE. Queering menstruation: trans and non-binary identity and body politics. Sociol Inq. (2020) 90:371–404. doi: 10.1111/soin.12355
58. Chrisler JC, Gorman JA, Manion J, Murgo M, Barney A, Adams-Clark A, et al. Queer periods: attitudes toward and experiences with menstruation in the masculine of centre and transgender community. Cult Health Sex. (2016) 18:1238–50. doi: 10.1080/13691058.2016.1182645
59. Defreyne J, Motmans J, T'sjoen G. Healthcare costs and quality of life outcomes following gender affirming surgery in trans men: a review. Expert Rev Pharmacoeconomics Outcomes Res. (2017) 17:543–56. doi: 10.1080/14737167.2017.1388164
60. Kimberly LL, Folkers KM, Friesen P, Sultan D, Quinn GP, Bateman-House A, et al. Ethical issues in gender-affirming care for youth. Pediatrics. (2018) 142:e20181537. doi: 10.1542/peds.2018-1537
61. Achille C, Taggart T, Eaton NR, Osipoff J, Tafuri K, Lane A, et al. Longitudinal impact of gender-affirming endocrine intervention on the mental health and well-being of transgender youths: preliminary results. Int J Pediatr Endocrinol. (2020) 2020:8. doi: 10.1186/s13633-020-00078-2
62. Kuper LE, Stewart S, Preston S, Lau M, Lopez X. Body dissatisfaction and mental health outcomes of youth on gender-affirming hormone therapy. Pediatrics. (2020) 145:e20193006. doi: 10.1542/peds.2019-3006
63. Coleman E, Bockting W, Botzer M, Cohen-Kettenis P, DeCuypere G, Feldman J, et al. Standards of care for the health of transsexual, transgender, and gender-nonconforming people. Int J Transgenderism. (2012) 13:165–232. doi: 10.1080/15532739.2011.700873
65. Light AD, Obedin-Maliver J, Sevelius JM, Kerns JL. Transgender men who experienced pregnancy after female-to-male gender transitioning. Obstet Gynecol. (2014) 124:1120–7. doi: 10.1097/AOG.0000000000000540
66. Herbst JH, Jacobs ED, Finlayson TJ, McKleroy VS, Neumann MS, Crepaz N. Estimating HIV prevalence and risk behaviors of transgender persons in the United States: a systematic review. AIDS Behav. (2008) 12:1–17. doi: 10.1007/s10461-007-9299-3
67. Fix L, Durden M, Obedin-Maliver J, Moseson H, Hastings J, Stoeffler A, et al. Stakeholder Perceptions and Experiences Regarding Access to Contraception and Abortion for Transgender, Non-Binary, and Gender-Expansive Individuals Assigned Female at Birth in the US. Arch Sex Behav. (2020) 49:2683–702. doi: 10.1007/s10508-020-01707-w
68. Sherer I, Hanks M. Affirming pediatric care for transgender and gender expansive youth. Pediatr Ann. (2021) 50:e65–71. doi: 10.3928/19382359-20210115-01
69. Flicker S, Guta A, Larkin J, Flynn S, Fridkin A, Travers R, et al. Survey design from the ground up: collaboratively creating the toronto teen survey. Health Promot Pract. (2010) 11:112–22. doi: 10.1177/1524839907309868
70. Clark TC, Lucassen MF, Bullen P, Denny SJ, Fleming TM, Robinson EM, et al. The health and well-being of transgender high school students: results from the New Zealand adolescent health survey (Youth'12). J Adolesc Health. (2014) 55:93–9. doi: 10.1016/j.jadohealth.2013.11.008
71. Lindley LL, Walsemann KM. Sexual orientation and risk of pregnancy among New York City high-school students. Am J Public Health. (2015) 105:1379–86. doi: 10.2105/AJPH.2015.302553
72. Veale J, Watson RJ, Adjei J, Saewyc E. Prevalence of pregnancy involvement among Canadian transgender youth and its relation to mental health, sexual health, and gender identity. Int J Transgenderism. (2016) 17:107–13. doi: 10.1080/15532739.2016.1216345
73. Ellis SA, Wojnar DM, Pettinato M. Conception, pregnancy, and birth experiences of male and gender variant gestational parents: it's how we could have a family. J Midwifery Women's Health. (2015) 60:62–9. doi: 10.1111/jmwh.12213
74. Jones RK, Witwer E, Jerman J. Transgender abortion patients and the provision of transgender-specific care at non-hospital facilities that provide abortions. Contraception: X. (2020) 2:100019. doi: 10.1016/j.conx.2020.100019
75. Moseson H, Fix L, Ragosta S, Forsberg H, Hastings J, Stoeffler A, et al. Abortion experiences and preferences of transgender, nonbinary, and gender-expansive people in the United States. Am J Obstet Gynecol. (2021) 224:376.e1–376.e11. doi: 10.1016/j.ajog.2020.09.035
76. Riggs DW, Bartholomaeus C. Fertility preservation decision making amongst Australian transgender and non-binary adults. Reprod Health. (2018) 15:181. doi: 10.1186/s12978-018-0627-z
77. Chen D, Matson M, Macapagal K, Johnson EK, Rosoklija I, Finlayson C, et al. Attitudes toward fertility and reproductive health among transgender and gender-nonconforming adolescents. J Adolesc Health. (2018) 63:62–8. doi: 10.1016/j.jadohealth.2017.11.306
78. Ethics Committee of the American Society for Reproductive Medicine. Access to fertility services by transgender persons: an Ethics Committee opinion. Fertil Steril. (2015) 104:1111–5. doi: 10.1016/j.fertnstert.2015.08.021
79. Hembree WC, Cohen-Kettenis P, Delemarre-van de Waal HA, Gooren LJ, Meyer WJ 3rd, Spack NP, et al. Endocrine treatment of transsexual persons: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. (2009) 94:3132–54. doi: 10.1210/jc.2009-0345
80. Ainsworth AJ, Allyse M, Khan Z. Fertility preservation for transgender individuals: a review. In: Mayo Clinic Proceedings. (2020). doi: 10.1016/j.mayocp.2019.10.040
81. Practice Committee of the American Society for Reproductive Medicine. Electronic address: asrm@asrm.org. Fertility preservation in patients undergoing gonadotoxic therapy or gonadectomy: a committee opinion. Fertil Steril. (2019) 112:1022–33. doi: 10.1016/j.fertnstert.2019.09.013
82. Lierman S, Tilleman K, Braeckmans K, Peynshaert K, Weyers S. T'Sjoen G, De Sutter P. Fertility preservation for trans men: frozen-thawed in vitro matured oocytes collected at the time of ovarian tissue processing exhibit normal meiotic spindles. J Assist Reprod Genet. (2017) 34:1449–56. doi: 10.1007/s10815-017-0976-5
83. Loverro G, Resta L, Dellino M, Edoardo DN, Cascarano MA, Loverro M, et al. Uterine and ovarian changes during testosterone administration in young female-to-male transsexuals. Taiwan J Obstet Gynecol. (2016) 55:686–91. doi: 10.1016/j.tjog.2016.03.004
84. Chen D, Simons L, Johnson EK, Lockart BA, Finlayson C. Fertility preservation for transgender adolescents. J Adolescent Health. (2017) 61:120–3. doi: 10.1016/j.jadohealth.2017.01.022
85. Armuand G, Dhejne C, Olofsson JI, Rodriguez-Wallberg KA. Transgender men's experiences of fertility preservation: a qualitative study. Hum Reprod. (2017) 32:383–90. doi: 10.1093/humrep/dew323
86. Peiris AN, Chaljub E, Medlock D. Endometriosis. JAMA. (2018) 320:2608. doi: 10.1001/jama.2018.17953
87. Sieberg CB, Lunde CE, Borsook D. Endometriosis and pain in the adolescent- striking early to limit suffering: a narrative review. Neurosci Biobehav Rev. (2020) 108:866–76. doi: 10.1016/j.neubiorev.2019.12.004
88. Dowlut-McElroy T, Strickland JL. Endometriosis in adolescents. Curr Opin Obstet Gynecol. (2017) 29:306–9. doi: 10.1097/GCO.0000000000000402
89. Shim JY, Laufer MR, Grimstad FW. Dysmenorrhea and endometriosis in transgender adolescents. J Pediatr Adolesc Gynecol. (2020) 33:524–8. doi: 10.1016/j.jpag.2020.06.001
90. Katkin JP, Kressly SJ, Edwards AR, Perrin JA, Kraft CA, Richerson JE, et al. Guiding principles for team-based pediatric care. Pediatrics. (2017) 140:20171489. doi: 10.1542/peds.2017-1489
91. Spack NP, Edwards-Leeper L, Feldman HA, Leibowitz S, Mandel F, Diamond DA, et al. Children and adolescents with gender identity disorder referred to a pediatric medical center. Pediatrics. (2012) 129:418–25. doi: 10.1542/peds.2011-0907
92. Hsieh S, Leininger J. Resource list: clinical care programs for gender-nonconforming children and adolescents. Pediatr Ann. (2014) 43:238–44. doi: 10.3928/00904481-20140522-11
93. Guss CE, Woolverton GA, Borus J, Austin SB, Reisner SL, Katz-Wise SL. Transgender adolescents' experiences in primary care: a qualitative study. J Adolesc Health. (2019) 65:344–9. doi: 10.1016/j.jadohealth.2019.03.009
94. Inwards-Breland DJ, DiVall S, Salehi P, Crouch JM, Negaard M, Lu A, et al. Youth and parent experiences in a multidisciplinary gender clinic. Transgend Health. (2019) 4:100–6. doi: 10.1089/trgh.2018.0046
95. Jones CE. Queering gendered disabilities. J Lesbian Studies. (2020). doi: 10.1080/10894160.2020.1778852
96. Culley L, Law C, Hudson N, Denny E, Mitchell H, Baumgarten M, Raine-Fenning N. The social and psychological impact of endometriosis on women's lives: a critical narrative review. Hum Reprod Update. (2013) 19:625–39. doi: 10.1093/humupd/dmt027
97. Stroumsa D, Wu JP. Welcoming transgender and nonbinary patients: expanding the language of “women's health.” Am J Obstetrics Gynecol. (2018) 219:585.e1–585.e5. doi: 10.1016/j.ajog.2018.09.018
98. Obedin-Maliver J, Goldsmith ES, Stewart L, White W, Tran E, Brenman S, et al. Lesbian, gay, bisexual, and transgender-related content in undergraduate medical education. JAMA. (2011) 306:971–7. doi: 10.1001/jama.2011.1255
99. Suen LW, Lunn MR, Katuzny K, Finn S, Duncan L, Sevelius J, et al. What sexual and gender minority people want researchers to know about sexual orientation and gender identity questions: a qualitative study. Arch Sex Behav. (2020) 49:2301–18. doi: 10.1007/s10508-020-01810-y
100. Moseson H, Lunn MR, Katz A, Fix L, Durden M, Stoeffler A, et al. Development of an affirming and customizable electronic survey of sexual and reproductive health experiences for transgender and gender nonbinary people. PLoS ONE. (2020) 15:e0232154. doi: 10.1371/journal.pone.0232154
101. Winter S, Settle E, Wylie K, Reisner S, Cabral M, Knudson G, et al. Synergies in health and human rights: a call to action to improve transgender health. Lancet. (2016) 388:318–21. doi: 10.1016/S0140-6736(16)30653-5
102. Sevelius J. “There's No Pamphlet for the Kind of Sex I Have”: HIV-related risk factors and protective behaviors among transgender men who have sex with nontransgender men. J Assoc Nurses AIDS Care. (2009) 20:398–410. doi: 10.1016/j.jana.2009.06.001
Keywords: adolescent, sexual health, transgender, reproductive health, gender-affirming care, gender expansive
Citation: Lunde CE, Spigel R, Gordon CM and Sieberg CB (2021) Beyond the Binary: Sexual and Reproductive Health Considerations for Transgender and Gender Expansive Adolescents. Front. Reprod. Health 3:670919. doi: 10.3389/frph.2021.670919
Received: 22 February 2021; Accepted: 31 August 2021;
Published: 06 October 2021.
Edited by:
Fredrick Odhiambo Otieno, Nyanza Reproductive Health Society, KenyaReviewed by:
Tamaryn Crankshaw, University of KwaZulu Natal, South AfricaCherie Dhar, Ann & Robert H. Lurie Children's Hospital of Chicago, United States
Dewi Rokhmah, University of Jember, Indonesia
Copyright © 2021 Lunde, Spigel, Gordon and Sieberg. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Christine B. Sieberg, christine.sieberg@childrens.harvard.edu
†These authors have contributed equally to this work and share first authorship
 Claire E. Lunde
Claire E. Lunde Rebecca Spigel
Rebecca Spigel Catherine M. Gordon4,5
Catherine M. Gordon4,5 Christine B. Sieberg
Christine B. Sieberg