- 1Department of Dentistry, Vita-Salute San Raffaele University, Milan, Italy
- 2Istituto Giuseppe Cozzani, La Spezia, Italy
- 3Department of Integrated Diagnostic and Surgical Sciences, University of Genoa, Genoa, Italy
Introduction: A condylion–gonion–menton (Co–Go–Me) angle threshold of 125.5° has been introduced as a predictive parameter of cephalometric mandibular response in the orthopedic treatment of growing Class II patients with functional appliances, despite some contradictions in the literature. Considering the lack of studies evaluating the role of skeletal anchorage, this study aims to reassess the threshold of 125.5° in the Co–Go–Me angle as a useful predictor in growing skeletal Class II patients treated with acrylic splint Herbst appliance and two mini-screws in the lower arch (STM2).
Methods: Thirty-five consecutively treated patients (20 males, 15 females; mean age, 11.37 years) with mandibular retrusion were classified into two groups according to their Co–Go–Me baseline values (Group 1, <125.5°; Group 2, >125.5°). The STM2 protocol involved the use of the MTH Herbst appliance with an acrylic splint in the lower arch and two interradicular mini-screws as anchorage reinforcement. Cephalometric analysis was performed by the same operator for each patient at baseline (T0) and at the end of the Herbst phase (T1). The effects of time and group on the variables were assessed by a repeated-measures analysis of variance. The primary research outcome was the difference between the groups in terms of mandibular responsiveness to treatment referred to as the relative difference (T1−T0) in Co_Gn.
Results: The mean duration of the treatment was 9.5 months. No statistically significant differences between groups were detected at baseline, except from the expected SN/GoMe° (p < 0.001) and Co–Go mm (p = 0.028). No statistically significant changes between groups, which were caused by the treatment, were found considering the mandibular sagittal and vertical skeletal parameters. Similarly, no statistically significant differences were found in the dental changes between the high-angle and low-angle patients, apart from the upper molar sagittal position (p = 0.013).
Discussion and conclusions: The 125.5° threshold in the Co–Go–Me value was not a reliable predictive parameter for the mandibular response in growing patients treated with the MTH Herbst appliance and lower skeletal anchorage. Due to its effective control in the sagittal and vertical planes, the STM2 technique might be an appropriate protocol to use in treating skeletal Class II patients, regardless of the growth pattern.
Introduction
Class II is one of the most frequent malocclusions affecting approximately one-third of the world's population (1). The origin of this condition is either dental, skeletal, or both, but mandibular retrusion is the most common cause, even though it can also be produced by maxillary protrusion or a combination of them (2, 3). In addition to dental features, patients generally present a convex profile, which negatively affects the aesthetic appearance of the face (4).
Apart from a proper diagnosis, the success of a Class II orthopedic treatment depends on several variables, including the type of appliance, patient growth, and timing of intervention (5).
Among different types of functional appliances, the Herbst appliance is one of the most efficient due to the reduced need for compliance. This fixed appliance promotes mandibular advancement and reduces maxillary sagittal growth (6–8). In addition, it acts on the dentition through distalization of the upper arch and mesialization of the lower one. While skeletal effects are favorable, the typical dental compensations (i.e., lingual tipping of the upper incisors and buccal flaring of the lower ones and distalization of the upper molars and mesialization of the lower ones) caused by anchorage loss (8, 9) could reduce the overjet needed for a proper mandibular advancement, partially compromising the final treatment outcome (4).
These side effects could be overcome with the introduction of skeletal anchorage (10). The combination of Herbst appliance with a lower acrylic splint and two buccal temporary anchored devices (TADs) in the lower arch (STM2: Skeletal Therapy Manni Telescopic Herbst with two TADs) has already demonstrated to be effective in encouraging a significant mandibular advancement, limiting the undesired proclination of lower incisors (8).
In addition to the type of appliance, another crucial element that influences the outcome of this orthopedic treatment might be the timing of intervention. Generally, the time window around the growth peak is considered the best one for increasing the skeletal effects (11, 12).
Despite these predictive factors, great variability in individual response is known depending on the type of protocol and appliance (13–15), even with the same workflow (2, 5). Therefore, it is of great clinical interest to better define other predictors to expect a good or poor response to treatment. Patient growth patterns can influence orthodontic treatment (16); therefore, several cephalometric methods have been proposed to examine mandibular development. Among various methods (17–19), an important value is the condylion–gonion–menton (Co–Go–Me) angle determined by the ratio of the condylar axis to the base of the mandible (20). This element provides important information about the patient's verticality and growth pattern. According to Franchi and Baccetti (5), patients with a Co–Go–Me angle of less than 125.5° would respond positively to Class II functional jaw orthopedic therapy when applied at the peak of growth. Similarly, the study conducted by Baccetti et al. (21) showed a favorable increase in the mandibular length associated with a pre-treatment Co–Go–Me angle of less than 123°. This is correlated with the improved soft tissue and chin projection when the patient is treated with bonded Herbst, followed by fixed appliances. On the contrary, in the study conducted by Fleming et al. (22), no correlation was found between the Co–Go–Me angle and the skeletal and dentoalveolar responses to treatment with a Twin-Block appliance.
Given these apparent contradictions and the lack of studies considering the role of skeletal anchorage, this study aims to better evaluate whether or not the Co–Go–Me angle can also be considered an effective predictor in the orthopedic treatment of skeletal Class II patients treated with fixed functional appliance and mini-screws. In particular, the null hypothesis of this investigation is that the 125.5° threshold in the Co–Go–Me angle is not a predictive parameter for mandibular response in growing patients treated with MTH Herbst and two lower TADs (STM2).
Materials and methods
Study design and recruitment
This retrospective study was performed on a sample of 35 skeletal Class II patients (20 males, 15 females; mean age, 11.37 ± 1.82 years) with a convex profile, who were consecutively treated with the STM2 technique. The inclusion criteria for this investigation were as follows: bilateral angle Class II Division 1 malocclusion (≥1/2 cusp width), skeletal Class II (ANB ≥ 4°), overjet ≥4 mm, permanent or late mixed dentition, aesthetic improvement of the profile simulating a mandibular advancement, and signed informed consent. The exclusion criteria were as follows: the presence of a systemic disease, bone pathology, tooth agenesis or premature loss of permanent teeth, previous orthodontic treatments, and incomplete available records. All patients were evaluated and consecutively treated by the same operator with the main goal of maximizing the skeletal effects and limiting the protrusion of the lower incisors.
Treatment protocol
A palatal expansion with a rapid palatal expander (RPE, A0620-13 Leone expansion screw, Sesto Florentino, Italy) was performed before the Herbst insertion in all patients because a transversal discrepancy was observed when simulating mandibular advancement. The activation protocol for the palatal expansion was one turn per day (0.2 mm for each activation) until the correction was completed.
The following STM2 protocol was then used: an MTH Herbst appliance with an acrylic splint (American Orthodontics, Sheboygan, WI, USA) was applied and initially activated with a mandibular advancement of 4 mm. At the same time, two TADs (length, 8.0 mm, diameter, 1.4 mm; Osstem Implant Co, Ltd., Seoul, South Korea) were placed in the lower arch only to act as anchorage reinforcement during the Herbst treatment (Figure 1). Based on bone availability, the insertion sites were between the first molar and the second premolar or between the two premolars (8) on the mucogingival line or in the attached gingiva. The TAD inclination was either perpendicular or tilted at 45° with respect to the alveolar bone depending on the clinical and anatomical conditions. The pre- and post-insertion radiographs of the interradicular implant sites were taken to check the distance of the TAD from the dental roots. All TADs were manually inserted without predrilling. The bilateral elastic chains (Memory Chain; American Orthodontics, Sheboygan, WI, USA) were stretched with a force of approximately 150 g from the head of the mini-screws to the direct buttons bonded on the buccal surface of lower canines as anchorage reinforcement. The elastic chains were changed at every appointment, supposing an average reduction of approximately 40% of the force after 1 month (23).

Figure 1. STM2 protocol: Herbst appliance with mini-screws in the lower arch used as anchorage reinforcement. The force applied to the screws is an elastic chain from the head of the mini-screws to a direct button applied on the canines.
The mandible was advanced by gradual increments (2 mm every 2 months) until the full correction of Class II (molar and canine Class I relationship) was reached, but the appliance was never removed before 9 months.
Cephalometric evaluation
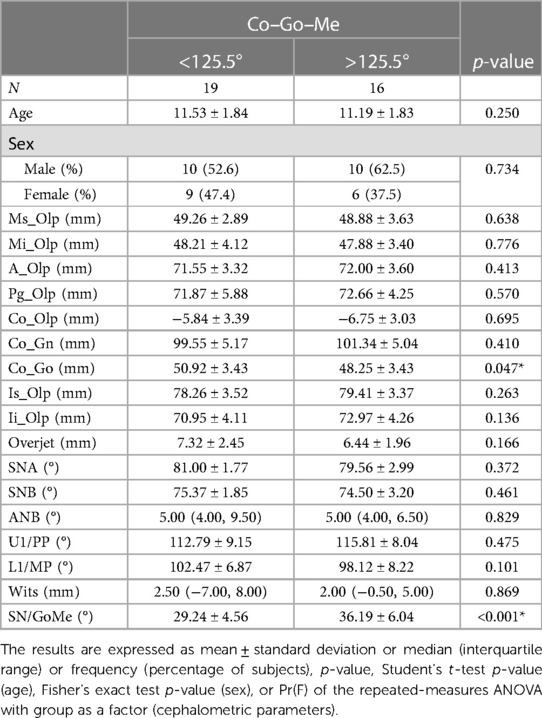
Three dropouts were registered and excluded from the analysis. All the other patients completed the treatment. Lateral cephalograms were collected at baseline (T0) and at the time of Herbst appliance removal (T1). A modified cephalometric Pancherz analysis (24) was performed for each patient at T0 and T1. The considered parameters are shown in Table 1.
The intraclass correlation coefficients (ICC) were calculated for the linear and angular measurements for 15 randomly selected cephalograms. Traces were performed by the same operator at one time after a 4-week interval. For angular measurements, the mean ICC value was greater than 0.98. For linear variables, the value was greater than 0.99.
The patients were classified into two groups according to their Co–Go–Me baseline value (<125.5° for Group 1 and >125.5° for Group 2). The observation periods for both group samples were all matched (39.00 weeks for Group 1, SD = 5.17, and 36.75 weeks for Group 2, SD = 5.00). No statistically significant difference was found.
The primary outcome of the research was the difference between the groups in terms of mandibular responsiveness to the treatment referred to as the relative difference (RD T1−T0) in Co_Gn.
Sample size
The sample size estimation showed that 15 patients for each group achieved 80% power to detect the mean difference in Co–Gn of 2.00 mm, yielding a 2.50 estimated standard deviation of differences and a 0.05 significance level (alpha) using a t-test. The 2.0 mm threshold was chosen as a clinically significant difference (4). The standard deviation was estimated according to a previous test over the sample.
Statistical analysis
The continuous variables are given as means ± standard deviations (SD) and medians with interquartile range (IR), whereas the categorical variables are given as number and/or percentage of subjects.
The baseline differences among ages were tested using the Student's t-test adjusted by using the Bonferroni method, while those between the sex compositions of the groups were tested by using the exact Fisher's test.
A repeated-measures analysis of variance (ANOVA) with group and time as factors was performed to assess the effects of time and group and any relative interaction in the cephalometric parameters. The differences with a p-value < 0.05 were selected as significant. The data acquired were analyzed in an R v3.4.4 software environment (25).
Results
The mean duration of the treatment was 9.5 months (SD = 1.29). The baseline (T0) cephalometric values, mean age, and sex classification of both groups are shown in Table 1. No significant differences were found between the groups at the beginning of treatment, aside from SN/GoMe° (29.24 ± 4.56 Group 1 vs. 36.19 ± 6.04 Group 2; p < 0.001), which was significantly higher in patients with the Co–Go–Me angle of >125.5° and Co–Go (50.92 mm ± 3.43 mm Group 1 vs. 48.25 mm ± 3.43 mm Group 2; p = 0.047), which was statistically higher in patients with Co–Go–Me angle of <125.5°.
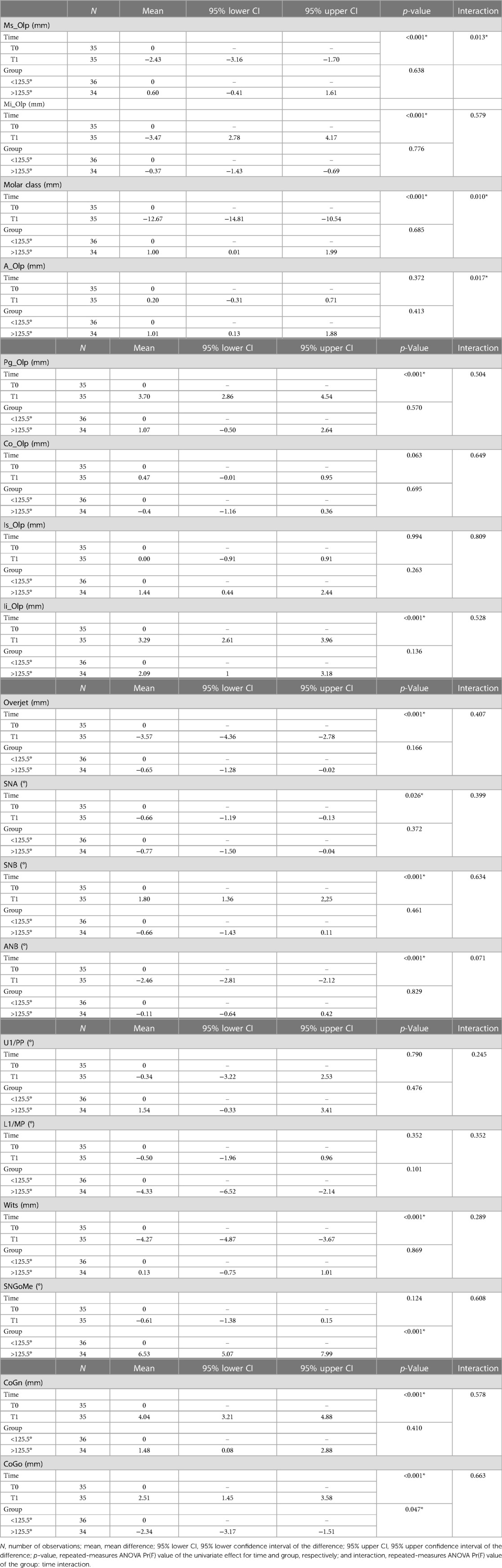
The results of the repeated-measures ANOVA with time and group as factors are shown in Table 2.
Considering sagittal skeletal changes, no significant differences were observed between the groups in SNA° (−0.89 ± 1.27 Group 1 vs. −0.41 ± 1.98 Group 2; p = 0.399), SNB° (1.97 ± 1.37 Group 1 vs. 1.74 ± 1.55 Group 2; p = 0.634), ANB° (−2.86 ± 1.22 Group 1 vs. −2.15 ± 1.03 Group 2; p = 0.071), and Wits (−4.64 mm ± 1.82 mm Group 1 vs. −3.97 mm ± 1.85 mm Group 2; p = 0.289). The value representing the dimension of the mandibular body (Co_Gn) showed an increase in both groups (4.21 mm ± 2.72 mm in Group 1 and 4.03 mm ± 2.10 mm in Group 2; p = 0.578). Moreover, although not significant, the group with the Co–Go–Me angle of >125.5° showed a greater advancement of the pogonion (Pg_Olp) at the end of treatment in comparison with the group with the Co–Go–Me angle of <125.5° (3.34 mm ± 2.34 mm for Group 1 vs. 4.34 mm ± 2.41 mm for Group 2; p = 0.504). The maxillary bone base length (A-OLPmm) indeed slightly reduced in Group 1 (−0.39 mm ± 1.45 mm) and increased in Group 2 (0.82 mm ± 1.39 mm).
Considering the vertical skeletal changes, there was an increase in the mandibular ramus length (Co_Go) in both groups (2.71 mm ± 3.00 mm in Group 1 and 2.47 ± 3.45 in Group 2), but the difference was not statistically significant (p = 0.663). Similarly, there was a decrease in the mandibular plane angle (SN/GoMe°) in both groups (−0.39 ± 2.31 Group 1 vs. −0.81 ± 2.34 Group 2), but the difference was also not statistically significant (p = 0.608).
With regard to the dental parameters, there were no statistically significant changes between the groups in the upper incisor sagittal position (Is_Olp) (−0.11 mm ± 2.97 mm Group 1 vs. 0.12 mm ± 2.55 mm Group 2; p = 0.809) and inclination (U1/PP) (1.33 ± 9.36° Group 1 vs. −2.12 ± 7.77° Group 2; p = 0.245). Similarly, no statistically significant changes between the groups were registered in the lower incisor sagittal position (Ii-Olp) (3.50 mm ± 1.84 mm Group 1 vs. 3.06 mm ± 2.24 mm Group 2; p = 0.528) and inclination (L1/MP) (0.08 ± 4.43° Group 1 vs. −1.50 ± 4.46° Group 2; p = 0.352) and in the lower molar sagittal position (Mi_Olp) (3.67 mm ± 1.88 mm Group 1 vs. 3.26 mm ± 2.35 mm Group 2; p = 0.579). Conversely, the upper molar sagittal position (Ms_Olp) showed a statistically significant difference between the groups (−3.31 mm ± 2.38 mm Group 1 vs. −1.50 mm ± 1.62 mm Group 2; p = 0.013).
In this study, nine TADs failed and were immediately reinserted without significant consequences for the treatment. No significant issues were encountered during the treatment, except for some discomfort in the early stages of adaptation to the Herbst appliance. Three dropouts were registered: one related to medical issues independent of orthodontic treatment and two related to poor oral hygiene during treatment. These dropouts were excluded from the whole analysis.
Discussion
The goal of orthopedic treatment in patients with skeletal Class II and mandibular retrusion is to increase the projection of the pogonion, thereby reducing the convexity and improving the aesthetics of the profile. When evaluating the mandibular response to functional treatment, it could be useful to assess the skeletal divergence. In fact, the vertical pattern may affect the condylar growth and chin projection (26). Generally, hyperdivergent patients exhibiting a clockwise rotation of the mandible might be more difficult to treat than hypodivergent patients who exhibit a counterclockwise rotation pattern. Therefore, Baccetti and Franchi (21, 5) considered the Co–Go–Me angle as a decisive parameter in predicting a good or poor mandibular response to orthopedic treatment. According to these authors, the presence of a reduced Co–Go–Me angle (i.e., Co–Go–Me angle of <125.5°) is associated with a greater mandibular length gain when using functional appliances. Although other studies confirmed the role of the Co–Go–Me angle as a useful predictor and reported the possible occurrence of a greater chin advancement with a smaller angle (27, 28), the threshold of 125.5° in the Co–Go–Me angle could not be confirmed in the present study as a valid response predictor when Class II patients were treated with acrylic splint Herbst appliance with two lower TADs as anchorage reinforcement. In fact, Groups 1 and 2 showed an increase in pogonion projection (Pg_Olp) (i.e., 3.34 mm ± 2.34 mm and 4.34 mm ± 2.41 mm, respectively. The difference was not statistically significant (p = 0.504). Similarly, Group 1 had an increased Co_Gn value of 4.21 mm ± 2.72 mm, while Group 2 had an increased Co_Gn value of 4.03 mm ± 2.10 mm. Thus, both groups showed an increase in the mandibular body length after treatment with the acrylic splint Herbst appliance and two lower TADs. The Co–Go–Me angle value was, however, not decisive as regards the statistically significant difference between the two groups (p = 0.578). In confirmation, both groups showed a reduction in the ANB angle (−2.86 ± 1.22 in Group 1 and −2.15 ± 1.03 in Group 2) and Wits (−4.64 mm ± 1.82 mm in Group 1 and −3.97 mm ± 1.85 mm In Group 2), but the difference was not statistically significant (p = 0.071 and p = 0.289, respectively). Finally, considering the mandibular ramus length (Co_Go), an increase was obtained in both groups (2.71 ± 3.00 for Group 1 and 2.47 ± 3.45 for Group 2), but the difference was also not statistically significant (p = 0.663).
Comparing these results with those of the meta-analysis conducted by Yang (29) on the effects of the Herbst appliance on the sagittal position of the mandibular base (Pg_OLp), a greater Pog advancement was observed in the present study [3.34 mm ± 2.34 mm (Group 1) and 4.34 mm ± 2.41 mm (Group 2)] vs. the average of 1.45 mm found by the author. This confirmed the conclusions of Al-Dboush (30), stating that the combination of the Herbst appliance with TADs might increase the effectiveness of the traditional orthopedic treatment, thereby leading to a better projection of the chin, regardless of the growth pattern. On one hand, this outcome could be explained by greater control in the sagittal position of the lower incisors with skeletal anchorage, preserving the overjet needed for mandibular advancement (31). On the other hand, good control of the vertical dimension was also observed probably due to the presence of the acrylic splint, which allowed a slight reduction in skeletal divergence not only in Group 1 (SN/GoMe°=−0.39 ± 2.31°) but also and especially in Group 2 (SN/GoMe°=−0.81 ± 2.34; the difference was not statistically significant, p = 0.608). Different from other Class II functional appliances, the presence of the splint, which limited the extrusion of the lower molars, probably prevented the clockwise rotation of the occlusal plane. The result led to an effective control of the skeletal divergence (32, 8) with a greater sagittal projection of the chin in hyperdivergent patients as well.
Considering the dental parameters, no statistically significant differences were observed among the groups in the maxillary incisor sagittal position (p = 0.809) and inclination (p = 0.245). A similar condition was observed for the lower incisor sagittal position (p = 0.528) and inclination (p = 0.352).
Moreover, no statistically significant differences were observed among groups in the mandibular sagittal position (p = 0.579), while the maxillary molars distalized more in Group 1 (Ms-Olp = −3.31 mm ± 2.38 mm) than in Group 2 (−1.50 mm ± 1.62 mm; p = 0.013).
This could be explained considering that forces related to the Herbst appliance normally tend to mesialize the lower arch and distalize the upper one. In the STM2 technique, however, due to the mandibular anchorage reinforcement, most of the forces are transferred to the upper molars. In low-angle patients, these applied forces might be generally higher because of the greater muscular component and more horizontal because of the orientation of the hinges relative to the occlusal plane. The result might be a slightly greater distalization of the upper arch, not only onto the anchorage unit (upper molars) but also at the level of the upper incisors (Is-OLP mm = −0.11 ± 2.97 Group 1; 0.12 ± 2.55 Group 2, even though the difference is not significant, p = 0.809) and of the A point (A-OLP mm = −0.39 ± 1.45 Group 1; 0.82 ± 1.39 Group 2; p = 0.017). Although this increased distalization may result in a statistically significant difference in the molar relationship between the two groups, the magnitude of this difference appears to be of little clinical significance.
The reason why the 125.5° threshold in the Co–Go–Me angle seems to be not decisive in assessing the mandibular response when the STM2 protocol is applied might be related to the applied therapy itself, which was different from the traditional one described in the article of Franchi and Baccetti (5). The STM2 technique involves the use of the telescopic Herbst associated with skeletal anchorage, elastic chains, and acrylic splint, with the main benefit of being represented by good control in both sagittal and vertical planes. A preliminary evaluation of the Co–Go–Me angle remains desirable in daily clinical practice in the treatment of skeletal Class II malocclusion. This parameter indeed makes it possible to predict the direction of the mandibular growth and preview the outcome of orthodontic therapy in cases where the STM2 technique is not adopted. Moreover, even when the orthodontist decides to use the Herbst appliance associated with skeletal anchorage, an evaluation of this parameter may be appropriate for the management of the occlusal plane during the second phase of treatment with multibracket therapy in order to achieve a proper occlusal result.
In the present study, nine TADs failed and were immediately reinserted without significant consequences for the treatment. This was in accordance with the mean failure rate reported in the current literature (33, 34). Generally, the acrylic splint Herbst appliance is associated with few emergencies, complications, and failures (35, 36). In this case, no significant issues were encountered during the treatment.
Despite the promising results, a larger sample size and more studies are necessary to confirm and better evaluate the success rate of such a protocol.
Moreover, a limitation of the study lies in the short-term evaluation of the treated patients, that is, only the Herbst phase was considered, even though the following one with multibracket appliances might affect the aesthetic outcome of the whole treatment. A long-term evaluation would also be necessary to assess the stability of the results. Finally, considering that the individual response could be influenced not only by the mean age at baseline but also by the skeletal maturation of the subjects, some maturity indicators could be considered in further evaluations.
Conclusion
This study on Class II skeletal malocclusion in growing patients treated with Manni telescopic Herbst appliance combined with lower mini-screws and elastic chains (STM2 technique) led to the following conclusions:
• The 125.5° threshold in the Co–Go–Me value is not a predictive parameter for the mandibular response in growing patients treated with an MTH Herbst appliance and two lower TADs (STM2).
• No statistically significant differences can be found in the mandibular sagittal and vertical skeletal changes between the high-angle and low-angle patients treated with the STM2 technique.
• No statistically significant differences can be found in the dental changes between the high-angle and low-angle patients treated with the STM2 technique, aside from the upper molar sagittal position.
• Due to its effective control in the sagittal and vertical planes, the STM2 technique might be an appropriate protocol in the treatment of skeletal Class II patients, regardless of the growth pattern.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by 2022/45 Comitato etico per la ricerca di Ateneo, University of Genoa. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
AM: Conceptualization, Investigation, Methodology, Writing – review & editing. MM: Data curation, Supervision, Writing – review & editing. AB: Conceptualization, Data curation, Writing – original draft. SD: Formal Analysis, Writing – original draft. EP: Writing – original draft. CC: Data curation, Writing – review & editing. GG: Supervision, Writing – review & editing. MC: Supervision, Writing – review & editing.
Funding
The authors declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Cozza P, Baccetti T, Franchi L, De Toffol L, McNamara JA. Mandibular changes produced by functional appliances in class II malocclusion: a systematic review. Am J Orthod Dentofac Orthop. (2006) 129(5):599.e1–12. doi: 10.1016/j.ajodo.2005.11.010
2. Chen JY, Will LA, Niederman R. Analysis of efficacy of functional appliances on mandibular growth. Am J Orthod Dentofac Orthop. (2002) 122(5):470–6. doi: 10.1067/mod.2002.126730
3. Perillo L, Padricelli G, Isola G, Femiano F, Chiodini P, Matarese G. Class II malocclusion Division 1: a new classification method by cephalometric analysis. Eur J Paediatr Dent. (2012) 13(3):192–6.22971255
4. Manni A, Mutinelli S, Cerruto C, Cozzani M. Influence of incisor position control on the mandibular response in growing patients with skeletal Class II malocclusion. Am J Orthod Dentofac Orthop. (2021) 159(5):594–603. doi: 10.1016/j.ajodo.2020.02.014
5. Franchi L, Baccetti T. Prediction of individual mandibular changes induced by functional jaw orthopedics followed by fixed appliances in Class II patients. Angle Orthod. (2006) 76(6):950–4. doi: 10.2319/110205-385
6. Valant JR, Sinclair PM. Treatment effects of the Herbst appliance. Am J Orthod Dentofac Orthop. (1989); 95(2):138–47. doi: 10.1016/0889-5406(89)90392-2
7. Flores-Mir C, Ayeh A, Goswani A, Charkhandeh S. Skeletal and dental changes in Class II Division 1 malocclusions treated with splint-type Herbst appliances: a systematic review. Angle Orthod. (2007) 77(2):376–81. doi: 10.2319/0003-3219(2007)077[0376:SADCIC]2.0.CO;2
8. Manni A, Mutinelli S, Pasini M, Mazzotta L, Cozzani M. Herbst appliance anchored to miniscrews with 2 types of ligation: effectiveness in skeletal Class II treatment. Am J Orthod Dentofac Orthop. (2016) 149(6):871–80. doi: 10.1016/j.ajodo.2015.11.029
9. Manni A, Cerruto C, Cozzani M. Herbst appliance supported by four miniscrews. J Clin Orthod. (2019) 53(12):737–44.32059226
10. Manni A, Pasini M, Mazzotta L, Mutinelli S, Nuzzo C, Grassi FR, et al. Comparison between an acrylic splint Herbst and an acrylic splint miniscrew-Herbst for mandibular incisors proclination control. Int J Dent. (2014) 2014:173187. doi: 10.1155/2014/173187
11. Malmgren O, Ömblus J, Hägg U, Pancherz H. Treatment with an orthopedic appliance system in relation to treatment intensity and growth periods a study of initial effects. Am J Orthod Dentofac Orthop. (1987) 91(2):143–51. doi: 10.1016/0889-5406(87)90472-0
12. Baccetti T, Franchi L, Toth R. Treatment timing for twin-block therapy. Am J Orthod Dentofac Orthop. (2000) 118:159–70. doi: 10.1067/mod.2000.105571
13. Patel HP, Moseley HC, Noar JH. Cephalometric determinants of successful functional appliance therapy. Angle Orthod. (2002) 72(5):410–7. doi: 10.1043/0003-3219(2002)072%3C0410:CDOSFA%3E2.0.CO;2.12401049
14. Tulloch JF, Proffit WR, Phillips C. Influences on the outcome of early treatment for Class II malocclusion. Am J Orthod Dentofacial Orthop. (1997) 111(5):533–42. doi: 10.1016/S0889-5406(97)70290-7
15. Staderini E, Ventura V, Meuli S, Maltagliati LÁ, Gallenzi P. Analysis of the changes in occlusal plane inclination in a Class II deep bite “teen” patient treated with clear aligners: a case report. Int J Environ Res Public Health. (2022) 19(2):651. doi: 10.3390/ijerph19020651
16. Valletta R, Rongo R, Pango Madariaga AC, Baiano R, Spagnuolo G, D’Antò V. Relationship between the condylion–gonion–menton angle and dentoalveolar heights. Int J Environ Res Public Health. (2020) 17(9):3309. doi: 10.3390/ijerph17093309
17. Bhullar M, Chachra S, Kochhar G, Kochhar A, Uppal A. Comparison of gonial angle determination from cephalograms and orthopantomogram. Indian J Dent. (2014) 5(3):123. doi: 10.4103/0975-962X.140820
18. Jiménez-Silva A, Carnevali-Arellano R, Vivanco-Coke S, Tobar-Reyes J, Araya-Díaz P, Palomino-Montenegro H. Craniofacial growth predictors for class II and III malocclusions: a systematic review. Clin Exp Dent Res. (2021) 7(2):242–62. doi: 10.1002/cre2.357
19. Perillo L, Isola G, Esercizio D, Iovane M, Triolo G, Matarese G. Differences in craniofacial characteristics in Southern Italian children from Naples: a retrospective study by cephalometric analysis. Eur J Paediatr Dent. (2013) 14(3):195–8.24295003
20. D’Antò V, Madariaga ACP, Rongo R, Bucci R, Simeon V, Franchi L, et al. Distribution of the condylion–gonion–menton (Co–Go–Me) angle in a population of patients from Southern Italy. Dent J. (2019) 7(4):1–10. doi: 10.3390/dj7040104
21. Baccetti T, Franchi L, Stahl F. Comparison of 2 comprehensive Class II treatment protocols including the bonded Herbst and headgear appliances: a double-blind study of consecutively treated patients at puberty. Am J Orthod Dentofac Orthop. (2009) 135(6):698.e1–10. doi: 10.1016/j.ajodo.2008.03.015
22. Fleming PS, Qureshi U, Pandis N, Dibiase AT. An investigation of cephalometric and morphological predictors of successful twin block therapy. Aust Orthod J. (2012) 28(2):190–6.23304967
23. Mirhashemi A, Saffarshahroudi A, Sodagar A, Atai M. Force-degradation pattern of six different orthodontic elastomeric chains. J Dent (Tehran). (2012) 9(4):204–15.23323182
24. Pancherz H, Hensen K. Occlusal changes during and after Herbst treatment: a cephalometric investigation. Eur J Orthod. (1986) 8(4):215–28. doi: 10.1093/ejo/8.4.215
25. R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria (2013).
26. Bjork A. Variations in the growth pattern of the human mandible: longitudinal radiographic study by the implant method. J Dent Res. (1965) 42:400–11. doi: 10.1177/00220345630420014701
27. Lombardo EC, Franchi L, Gastaldi G, Giuntini V, Lione R, Cozza P, et al. Development of a prediction model for short-term success of functional treatment of Class II malocclusion. Int J Environ Res Public Health. (2020) 17(12):1–7. doi: 10.3390/ijerph17124473
28. Kim JE, Mah SJ, Kim TW, Kim SJ, Park KH, Kang YG. Predictors of favorable soft tissue profile outcomes following Class II twin-block treatment. Korean J Orthod. (2018) 48(1):11–22. doi: 10.4041/kjod.2018.48.1.11
29. Yang X, Zhu Y, Long H, Zhou Y, Jian F, Ye N, et al. The effectiveness of the Herbst appliance for patients with Class II malocclusion: a meta-analysis. Eur J Orthod. (2016) 38(3):324–33. doi: 10.1093/ejo/cjv057
30. Al-Dboush R, Soltan R, Rao J, El-Bialy T. Skeletal and dental effects of Herbst appliance anchored with temporary anchorage devices: a systematic review with meta-analysis. Orthod Craniofac Res. (2022) 25(1):31–48. doi: 10.1111/ocr.12510
31. Huang Y, Sun W, Xiong X, Zhang Z, Liu J, Wang J. Effects of fixed functional appliances with temporary anchorage devices on Class II malocclusion: a systematic review and meta-analysis. J World Fed Orthod. (2021) 10(2):59–69. doi: 10.1016/j.ejwf.2021.02.001
32. Giuca MR, Pasini M, Drago S, Del Corso L, Vanni A, Carli E, et al. Influence of vertical facial growth pattern on Herbst appliance effects in prepubertal patients: a retrospective controlled study. Int J Dent. (2020) 2020:1018793. doi: 10.1155/2020/1018793
33. Alharbi F, Almuzian M, Bearn D. Miniscrews failure rate in orthodontics: systematic review and meta-analysis. Eur J Orthod. (2018) 40(5):519–30. doi: 10.1093/ejo/cjx093
34. Papageorgiou SN, Zogakis IP, Papadopoulos MA. Failure rates and associated risk factors of orthodontic miniscrew implants: a meta-analysis. Am J Orthod Dentofacial Orthop. (2012) 142(5):577–95.e7. doi: 10.1016/j.ajodo.2012.05.016
35. Manni A, Cozzani M, Mazzotta L, Fiore VP, Mutinelli S. Acrylic splint Herbst and Hanks telescoping Herbst: a retrospective study of emergencies, retreatments, treatment times and failures. Int Orthod. (2014) 12(1):100–10. doi: 10.1016/j.ortho.2013.12.015
Keywords: Class II, Herbst appliance, skeletal anchorage, gonial angle, TADs
Citation: Manni A, Migliorati M, Boggio A, Drago S, Paggi E, Calzolari C, Gastaldi G and Cozzani M (2024) Evaluation of the Co–Go–Me angle as a predictor in Class II patients treated with Herbst appliance and skeletal anchorage: a retrospective cohort study. Front. Oral. Health 5:1389628. doi: 10.3389/froh.2024.1389628
Received: 21 February 2024; Accepted: 16 April 2024;
Published: 30 April 2024.
Edited by:
Jan Christian Danz, University of Bern, SwitzerlandReviewed by:
Krzysztof Dowgierd, Regional Children's Hospital Craniofacial Center & Head Neck Surgery Department, PolandMaja Ovsenik, University of Ljubljana, Slovenia
© 2024 Manni, Migliorati, Boggio, Drago, Paggi, Calzolari, Gastaldi and Cozzani. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Andrea Boggio YW5kcmVhYm9nZ2lvOTBAZ21haWwuY29t
†These authors have contributed equally to this work and share first authorship
 Antonio Manni1,2,†
Antonio Manni1,2,† Andrea Boggio
Andrea Boggio Sara Drago
Sara Drago Giorgio Gastaldi
Giorgio Gastaldi