
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Oral. Health , 28 March 2024
Sec. Oral Epidemiology
Volume 5 - 2024 | https://doi.org/10.3389/froh.2024.1363982
This article is part of the Research Topic The Association Between Oral Health and Mental Health View all 6 articles
 Tasha Powell1*
Tasha Powell1* Heather Taylor2
Heather Taylor2
Objective: Very little is known about the association between poor mental health and poor oral health outcomes in the United Sates. This study investigated the prevalence of complete tooth loss among those with and without perceived poor mental health in a nationally representative sample of noninstitutionalized U.S. adults.
Methods: Using a cross-sectional study design, we analyzed the 2019 Medical Expenditures Panel Survey to determine the unweighted and weighted prevalence of complete tooth loss among adults. Chi-squared and multivariate logit regression with marginal effects were used to measure the association between complete tooth loss and perceived poor mental health, controlling for respondent characteristics.
Results: The prevalence of adults (ages 18 and older) experiencing complete tooth loss was 6% (95% CI: 5.6–6.4). Individuals who have perceived poor mental health were 1.90 percentage points (pps) more likely to report missing all their natural teeth (P = 0.006: 95% CI: 0.5–3.3). Other relevant predictors of complete tooth loss included current smoking status (5.9 pps; 95% CI: 4.5 to 7.2) and secondary education (−6.4 pps (95% CI: −7.0 to −4.8).
Conclusions: Overall, self-reported poor mental health was found to be associated with a greater likelihood of reporting complete tooth loss. Findings from this study underscore the need for greater integration of care delivery between behavioral health specialists and dental providers.
Mental illnesses (i.e., conditions that affect cognition, emotion, and behavior) (1) and poor oral health (i.e., conditions and outcomes of oral diseases that include dental caries, periodontal (gum) disease, tooth loss, and oral cancer) (2) are two seemingly distinct domains, but emerging evidence suggests an intricate association (3). Existing studies suggest that individuals who experience a mental illness have a higher risk of poor oral health than those in the general population (4, 5). This may, in part, be due to certain risk factors among those with mental illness. For example, individuals who experience mental illness are frequently prescribed psychotropic medications, which have numerous negative oral side effects, such as xerostomia (dry mouth) and mouth ulcers (6, 7). Those who experience mental illness may also struggle to manage typical daily functions, such as remembering to stick to a schedule and maintaining their personal hygiene, including oral hygiene (8). Furthermore, they are also more likely than the general population to (1) consume diets high in fermentable carbohydrates which contributes to the initiation and progression of dental caries (3), (2) have comorbidities such as alcohol and substance use which is associated with dental caries, oral pain, and tooth infection (9), and (3) smoke cigarettes which can lead to periodontal disease and tooth loss (10, 11).
Given the lifestyle habits and risk factors among those with mental illnesses, understanding oral health outcomes among this population becomes very important. If poor oral health remains unaddressed, those with mental illness may experience worsening levels of self-esteem and reduced quality of life, further perpetuating complications related to their mental illness (3). However, most of our current understanding of the association between mental illnesses and oral health has been conducted in countries such as the United Kingdom, Australia, and Taiwan (3, 6, 7, 11–15). Of the existing U.S. based scientific literature, studies have limited their analyses to a small subset of a broad array of existing mental illness diagnoses, such as severe mental illness or depression (16–22). Nevertheless, there are many other mental illnesses, such as anxiety, which are related to bruxism (excessive teeth grinding) and attrition (tooth wear) and can also contribute to worse oral health (23, 24). Thus, there is a need to broadly understand whether, and to what extent, mental illnesses (including those less severe) are related to oral health so that population-level interventions can be targeted appropriately to address co-occurring health needs.
The purpose of this cross-sectional study is to determine the prevalence of complete tooth loss, a measure of poor oral health, among those experiencing mental illness in the United States. Specifically, this study will examine the relationship between self-reported poor mental health and complete tooth loss among a nationally representative survey of U.S. civilian noninstitutionalized adults (25). Complete tooth loss reflects a lifetime of dental disease and a history of (or absence) of treatment (26). We hypothesize that adults with poor mental health are more likely to experience complete tooth loss when compared to the general population. Findings from this study may inform policy on vulnerable populations and will also be of interest to behavioral health specialists, caregivers, dental professionals, and social workers who care for individuals with mental illness and wish to improve their oral and overall health (3).
Data for this cross-sectional study were derived from the 2019 Medical Expenditure Panel Survey (MEPS) data (27). We followed the STROBE guidelines for the reporting of this cross-sectional observational study (28). MEPS is a nationally representative annual survey of noninstitutionalized persons across the United States. This survey utilizes a subsample of participants from the previous year's National Health Interview Survey, conducted by the National Center for Health Statistics (29, 30). Thus, data collection for this analysis occurred between January and December of 2018 (30, 31). We used data from the MEPS household component (MEPS-HC), which collects participant information via interviews on demographic characteristics, health conditions (including dental services), insurance status, and quality of life data (29). Previous studies have reported on the validity of measures used in MEPS, including those used in the household component (32, 33).
In 2019, 28,512 persons were included in MEPS-HC (27). Because we were only interested in adults for our analysis, we excluded anyone who was under the age of 18 (n = 6,558). Since MEPS-HC data are publicly available and deidentified, this study was deemed exempt from IRB approval.
Our dependent variable, complete tooth loss, was constructed as a binary indicator based on whether or not an individual reported they “lost all upper and lower teeth” in the MEPS-HC interview. Respondents who reported “Yes” to having lost all upper and lower teeth were coded as “1” and labeled as having “complete tooth loss”. All individuals who reported “No” to having “lost all upper and lower teeth” were coded as “0”. Individuals who were “unable” or “refused” to answer this question were recoded as having a missing value for this variable (n = 517) but these observations remained in the sample.
Our main explanatory variable was whether an adult perceived their mental health to be poor. Respondents of the MEPS-HC interview were asked: “In general, would you say your mental health is excellent, very good, good, fair, or poor?” Respondents who reported “poor” or “fair” mental health were coded as “1”, while individuals who reported “good”, “very good”, and “excellent” mental health were coded as “0”. For individuals that were “unable” or “refused” to respond to this question, we recoded their responses to missing values (n = 388) but these observations remained in the sample.
Other independent factors served as controls in our analysis given their known relationship to healthcare utilization according to Andersen's Behavioral Model of Health Services Use (34). These control variables included gender (male, female), relationship status (married, widowed, divorced, separated, never married), income as percentage of the federal poverty line (FPL) [poor/negative (at FPL or below), near poor (FPL to less than 125% of the FPL), low income (125% to less than 200% FPL), middle income (200% to less than 400% FPL), high income (400% or greater FPL)], unemployed (yes, no), and health insurance coverage (private, public only, uninsured). We considered the following variables as confounding factors that are likely related to both our dependent and main explanatory variable: age (18–24; 25–34; 35–44; 45–54; 55–64; 65–74; 75+), race/ethnicity (Hispanic, non-Hispanic white, non-Hispanic black, non-Hispanic Asian, non-Hispanic other races or multiple races), education [no degree, high school/General Equivalency Diploma (GED)some college], private dental insurance (yes, no), general health status (excellent, very good, good, fair, poor,) current smoker status (yes, no), and whether they “cannot afford dental care” (yes, no). In most cases, we kept variables as they were defined, measured, and recorded within the MEPS datasets. For a few variables, data was reconstructed for the purposes of this analysis based on the distribution of responses per category and ease of interpretation (age, education, poor mental health).
First, we tabulated unweighted and weighted descriptive statistics for each variable of interest included in our study, as well as the prevalence of complete tooth loss. Next, using Chi-Square tests, we examined the bivariate relationships between complete tooth loss and perceived mental health and respondent characteristics. To address potential sources of bias, we considered measures of collinearity and used a stepwise approach while building our adjusted regression model. The mean variable inflation factor (VIF) for included variables was 1.31 (A VIF above 5 is considered to indicate variables to be highly correlated and problematic to estimating unbiased regression coefficients). Because odds ratios cannot be compared across different population samples or interpreted as absolute effects, we chose to estimate marginal effects (35). Thus, we estimated the marginal effects of perceived mental health and each respondent characteristic included in the multivariate logit regression model. Marginal effects can be interpreted as the absolute risk difference of each independent variable when holding all other covariates at their mean value. Corresponding 95% confidence intervals were calculated for all regression estimates, and findings were considered statistically significant if p-values were below 0.05. For all analyses, MEPS survey weights were applied to obtain accurate weighted estimates and standard errors, using Stata 17 statistical software (36). MEPS survey weights adjust for survey nonresponse and disproportionate sampling of certain populations (37).
A total of 21,954 non-institutionalized adults, representing 253,548,355 people, were included in this 2019 cross-sectional analysis. Descriptive statistics of the sample's characteristics are presented in Table 1. The prevalence of adults reporting poor mental health was 8.3% (95% CI: 7.8–8.8). The prevalence of complete tooth loss among all adults was 6.0% (95% CI: 5.6–6.4).
Table 2 displays the bivariate relationship between complete tooth loss and individual-level factors, including self-reported poor mental health. The relationship between poor mental health and complete tooth loss was found to be statistically significant (β = 0.131; p-value < 0.001). Statistically significant relationships were also found between complete tooth loss and income (p < 0.001), education (p < 0.001), private dental insurance (p < 0.001), and smoking status (p < 0.001).
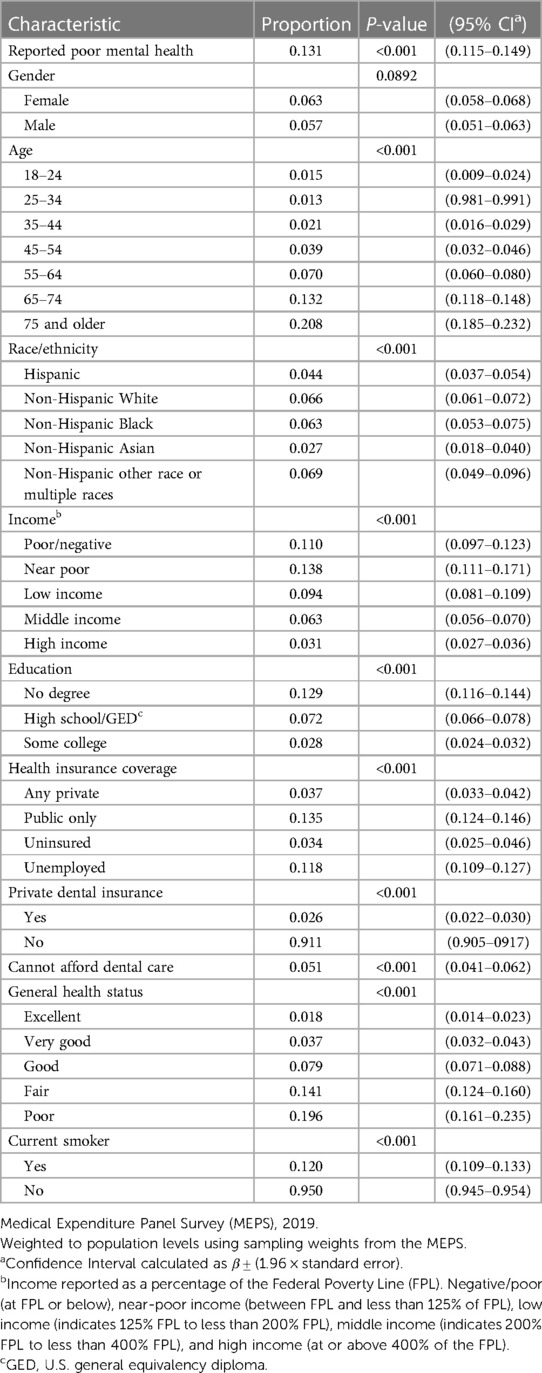
Table 2. Bivariate relationship between complete tooth loss and individual level factors (N = 21,954).
To examine the magnitude of effect of each independent variable and our main explanatory variable (perceived poor mental health) we present marginal effects from our multivariate regression model in Table 3. Adults who self-reported poor mental health were 1.9 percentage points (pps) (95% CI: 0.5–3.3) more likely to have complete tooth loss than those self-reporting good mental health. One of the largest predictors (by effect magnitude) of complete tooth loss was current smoking status [5.9 (pps); 95% CI: 4.5–7.2]. Another relevant predictor (by effect magnitude) was having a secondary education, which was negatively associated with complete tooth loss [−6.4 pps (95% CI: −7.0 to −4.8)] as compared to individuals with no degree/diploma. Adults reporting fair general health status (3.8 pps; 95% CI: 2.4–5.2) or poor general health status (4.4 pps; 95% CI: 2.4–6.4) were more likely to report complete tooth loss compared to those reporting excellent general health status. Finally, higher age was positively associated with complete tooth loss, as adults above age 45 were 2.6 pps (95% CI: 1.3–3.8) more likely to report complete tooth loss compared to adults below age 25.
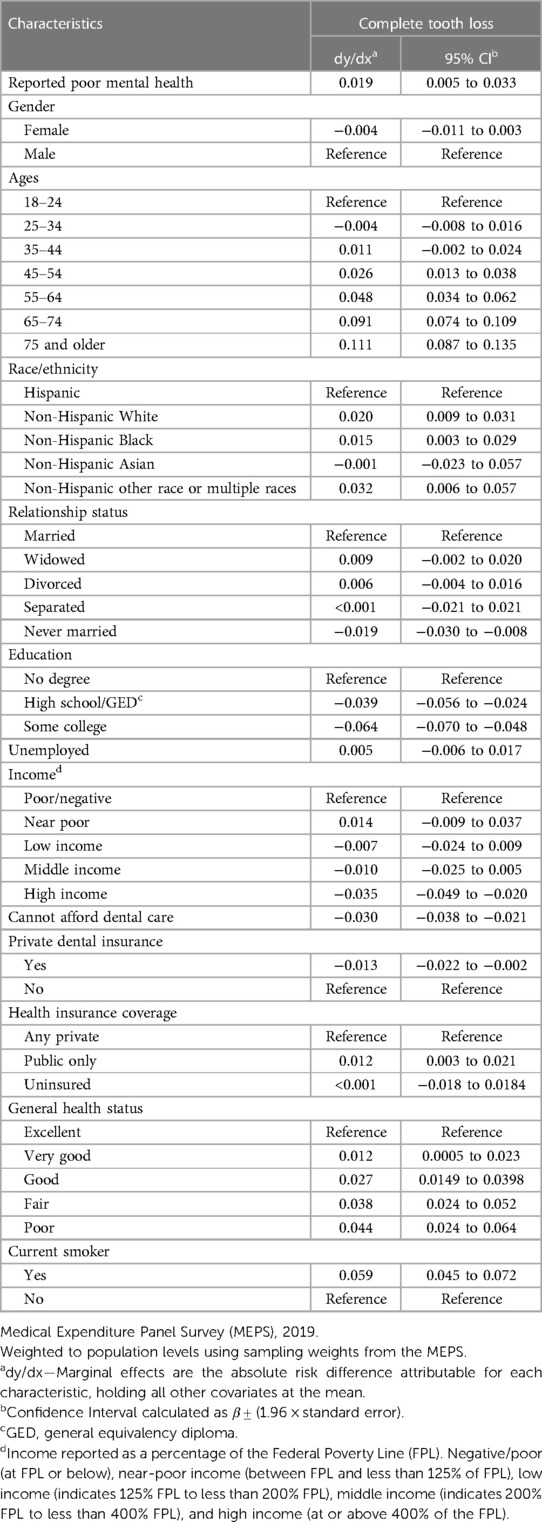
Table 3. Marginal effect of factors associated with complete tooth loss among U.S. adults 2019 (N = 16,906).
This study sought to determine the prevalence of complete tooth loss and examine its relationship with perceived poor mental health among adults within the United States. Overall, we found the prevalence of complete tooth loss among a nationally representative sample of adults was 6.0%. Furthermore, as hypothesized, we found that complete tooth loss was positively associated with self-reported poor mental health, even when controlling of other respondent characteristics.
Several studies have examined the prevalence of complete tooth loss and reported higher rates in the United States. One study assessed 2017 MEPS data and reported the prevalence of complete tooth loss to be 11.4% while another study assessed MEPS data over time (2015–2018) and measured the prevalence at 12.9% (38, 39). While these studies report a prevalence rate higher than what we found in this current study, these previous studies were restricted to a subset of the population, those over the age of 50. This current study examined the prevalence of complete tooth loss among all adults over the age of 18, hence why our prevalence rate is nearly half of what has been reported in past MEPS analyses.
In this current study, we found a significant bivariate relationship between those self-reporting poor mental health and complete tooth loss in the U.S. This relationship remained significant even after controlling for other factors in our multivariate regression models, as evident by the higher likelihood of complete tooth loss among those with perceived poor mental health. This finding is similar to studies which have examined the relationship between mental illness and tooth loss in other countries (3, 18). People with varying forms of mental illness often grapple with a myriad of challenges that can lead to poor oral outcomes such as complete tooth loss. These challenges may include side effects from commonly prescribed psychotropic drugs that often cause xerostomia (dry mouth), stigma and barriers to receiving dental care, a diet high in fermentable carbohydrates, and poor daily oral hygiene (40, 41).
One recent U.S. based survey study by Tiwari et al. (2022) similarly found that self-reported poor oral health was significantly related to self-reported poor mental health (2). Authors of this study reported that those with self-reported poor mental health were also statistically more likely to report unmet dental needs compared to their counterparts (2). Findings from this current study go a step further beyond unmet dental need and demonstrate that self-reported poor mental health is also positively related to the likelihood of experiencing measurable poor oral health outcomes (complete tooth loss). Tiwari et al. (2022) found that the majority of individuals who reported poor mental health did nothing about their oral health symptoms (2). These oral health symptoms, if not addressed appropriately, can lead to an increase in debilitating dental diseases, and eventual tooth loss (3, 40). For instance, one study revealed that over a third (−35%) of adults with mental illness require dental extractions due to delayed dental care brought on by unaddressed dental caries or infection (42). As more extractions are needed, individuals may eventually experience full edentulism (missing all natural teeth) and may subsequently need to consider dentures. Because dentures cannot perfectly stimulate true tooth function and form, these prostheses may perpetuate poor mental health by exacerbating low self-esteem and social withdrawal (3). Thus, the relationship between poor mental health and poor oral health is likely cyclical and pervasive in nature.
Beyond self-reported poor mental health, we also found smoking status to be the largest positive predictor (in magnitude) of complete tooth loss. Nearly forty percent of non-institutionalized persons with mental illnesses smoke (43). Furthermore, the smoking rate is twice as high among individuals with depression than the general population (44, 45). As mentioned, individuals who struggle with mental illness often have poor oral hygiene which can be exacerbated by social risks factors such as smoking. Smoking has a significant negative effect on oral health and can lead to periodontal disease, infection, and higher rates of dental extractions (3, 42, 46). Given the strong correlation between smoking and oral and mental health, medical and dental providers should seek ways to coordinate care for mutual patients who suffer from mental illnesses and engage in risky behaviors, such as smoking. By better addressing these habits and providing tobacco cessation help, providers may be able to make improvements in individual- and population-level mental and oral health.
Finally, some evidence suggests that those with mental illness face significant barriers to accessing dental care. For instance, some healthcare providers stigmatize patients who have mental illnesses, leading to excessively delayed treatment, if not denying care due to unconscious bias or inadequate behavioral health training that would allow providers to effectively manage patients and provide optimal care (47). Also, persons with mental illness often have an altered cognitive state and present with poor communication skills creating other barriers to dental care (16). These barriers may exacerbate or worsen their individual oral health among those with mental illness (48). Future research should continue to analyze these relationships, particularly within vulnerable communities who experience significant health disparities. It is important for policymakers, behavioral health specialists, caregivers, dental professionals, and social workers who manage or care for individuals with mental illness to understand whether, and to what extent, mental illness is related to oral health so that interventions can be targeted appropriately and needs can be better addressed.
While our study was the first to examine the association between perceived poor mental health and complete tooth loss in the U.S., there are several study limitations to note. First, our cross-sectional study design inhibits internal validity and therefore the ability to determine causality (49). Second, we used self-reported survey data which lends itself to recall and social desirability biases. Third, “mental health” is a broad term that includes many factors as well as the absence of a broad arrange of conditions and disorders (50). Nevertheless, research suggests that self-reported mental health measures are good proxy variables for clinically definitions of mental health (51). Fourth, given MEPS sampling design of non-institutionalized individuals, we know very little about the prevalence or extent of complete tooth loss among institutionalized adults, who are statistically more likely to have mental illnesses (52, 53). Thus, while our data are nationally representative, our findings cannot be generalized to the institutionalized U.S. adult population. Given this limitation, we likely underestimated the association between perceived poor mental health and complete tooth loss (52, 53). Fifth, our findings may also be explained by reverse causality, this is, that complete tooth loss drives perceived poor mental health. Additional prospective research that studies these relationships overtime is needed to tease out the true mechanisms of action within this observed relationship. And finally, survey data can be subject to nonresponse bias. However, we applied appropriate MEPS sampling weights to account for this potential bias in nonresponse.
In summary, our findings address relevant gaps in the literature related to mental illness and complete tooth loss among the U.S. adult population. The observed positive association between poor mental health and complete tooth loss underscores the importance of further exploring the interplay between mental illness and oral health.
Publicly available datasets were analyzed in this study. This data can be found here: MEPS HC-192 2016 Full Year Consolidated Data File. https://meps.ahrq.gov/data_stats/download_data/pufs/h192/h192doc.shtml.
Ethical approval was not required for the study involving humans in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and the institutional requirements.
TP: Conceptualization, Investigation, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing. HT: Conceptualization, Data curation, Formal Analysis, Methodology, Software, Supervision, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Ryff CD, Freeman EJ, McKinght-Eily LR, Dhingra S, Strine TW. Evolving definitions of mental illness and wellness. Prev Chronic Dis. (2010) 7:A19.20040234
2. Oral health. Available online at: https://www.who.int/health-topics/oral-health (Accessed January 20, 2024).
3. Kisely S. No mental health without oral health. Can J Psychiatry. (2016) 61:277–82. doi: 10.1177/0706743716632523
4. Tiwari T, Kelly A, Randall CL, Tranby E, Franstve-Hawley J. Association between mental health and oral health Status and care utilization. Front Oral Health. (2021) 2:732882. doi: 10.3389/froh.2021.732882
5. Hudson J. How mental health affects oral health. BDJ Student. (2021) 28:21–3. doi: 10.1038/s41406-021-0225-3
6. Page MM, Somerville-Brown LM. Psychotropic drugs and dentistry. Aust Prescr. (2007) 30:98–101. doi: 10.18773/austprescr.2007.059
7. Cockburn N, Pradhan A, Taing MW, Kisely S, Ford PJ. Oral health impacts of medications used to treat mental illness. J Affect Disord. (2017) 223:184–93. doi: 10.1016/j.jad.2017.07.037
8. Living Well with Serious Mental Illness (2023). Available online at: https://www.samhsa.gov/serious-mental-illness (Accessed September 24, 2022).
9. Hujoel PP, Lingström P. Nutrition, dental caries and periodontal disease: a narrative review. J Clin Periodontol. (2017) 44(Suppl 18):S79–84. doi: 10.1111/jcpe.12672
10. Waldron C, Nunn J, Phadraig CMG, Comiskey C, Guerin S, van Harten MT, et al. Oral hygiene interventions for people with intellectual disabilities. Cochrane Database Syst. Rev. (2019) 5:CD012628. doi: 10.1002/14651858.CD012628.pub2
11. Lawrence D, Mitrou F, Zubrick SR. Smoking and mental illness: results from population surveys in Australia and the United States. BMC Public Health. (2009) 9:285. doi: 10.1186/1471-2458-9-285
12. Macnamara A, Mishu MP, Faisal MR, Islam M, Peckham E. Improving oral health in people with severe mental illness (SMI): a systematic review. PLoS One. (2021) 16:e0260766. doi: 10.1371/journal.pone.0260766
13. Lewis S, Jagger RG, Treasure E. The oral health of psychiatric in-patients in south Wales. Spec Care Dentist. (2001) 21:182–6. doi: 10.1111/j.1754-4505.2001.tb00252.x
14. Kisely S, Lalloo R, Ford P. Oral disease contributes to illness burden and disparities. Med J Aust. (2018) 208:155–6. doi: 10.5694/mja17.00777
15. Matevosyan NR. Oral health of adults with serious mental illnesses: a review. Community Ment Health J. (2010) 46:553–62. doi: 10.1007/s10597-009-9280-x
16. Teng P-R, Lin M-J, Yeh L-L. Utilization of dental care among patients with severe mental illness: a study of a national health insurance database. BMC Oral Health. (2016) 16:87. doi: 10.1186/s12903-016-0280-2
17. McKibbin CL, Kitchen-Andren KA, Lee AA, Wykes TL, Bourassa KA. Oral health in adults with serious mental illness: needs for and perspectives on care. Community Ment Health J. (2015) 51:222–8. doi: 10.1007/s10597-014-9758-z
18. Kisely S, Quek L, Pais J, Lalloo R, Johnson N, Lawrence D. Advanced dental disease in people with severe mental illness: systematic review and meta-analysis. Br J Psychiatry. (2011) 199:187–93. doi: 10.1192/bjp.bp.110.081695
19. Hall JP, LaPierre TA, Kurth NK. Oral health needs and experiences of medicaid enrollees with serious mental illness. Am J Prev Med. (2018) 55:470–9. doi: 10.1016/j.amepre.2018.05.013
20. Al-Zahrani MS, Alhassani AA, Melis M, Zawawi KH. Depression is related to edentulism and lack of functional dentition: an analysis of NHANES data, 2005–2016. J Public Health Dent. (2021) 81:206–13. doi: 10.1111/jphd.12433
21. Almohaimeed B, Dube SR, Luo R. Investigating oral health among individuals with depression: NHANES 2015–2016. Saudi Dent J. (2022) 34:249–58. doi: 10.1016/j.sdentj.2022.01.001
22. Cademartori MG, Gastal MT, Nascimento GG, Demarco FF, Corrêa MB. Is depression associated with oral health outcomes in adults and elders? A systematic review and meta-analysis. Clin Oral Investig. (2018) 22:2685–702. doi: 10.1007/s00784-018-2611-y
23. Choi J, Price J, Ryder S, Siskind D, Solmi M, Kisely S. Prevalence of dental disorders among people with mental illness: an umbrella review. Aust N Z J Psychiatry. (2022) 56:949–63. doi: 10.1177/00048674211042239
24. Matsuyama Y, Jürges H, Dewey M, Listl S. Causal effect of tooth loss on depression: evidence from a population-wide natural experiment in the USA. Epidemiol Psychiatr Sci. (2021) 30:e38. doi: 10.1017/S2045796021000287
25. MEPS-HC Panel Design and Data Collection Process. Available online at: https://meps.ahrq.gov/survey_comp/hc_data_collection.jsp (cited February 10, 2024)
26. Peres MA, Macpherson LMD, Weyant RJ, Daly B, Venturelli R, Mathur MR, et al. Oral diseases: a global public health challenge. Lancet. (2019) 394:249–60. doi: 10.1016/S0140-6736(19)31146-8
27. MEPS HC-216 2019 Full Year Consolidated Data File. Available online at: https://meps.ahrq.gov/data_stats/download_data/pufs/h216/h216doc.pdf (accessed January 5, 2023)
28. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Available online at: https://www.equator-network.org/reporting-guidelines/strobe/ (accessed February 9, 2024)
29. Agency for Healthcare Research & Quality. Medical Expenditure Panel Survey Background (2019). Available online at: https://meps.ahrq.gov/mepsweb/about_meps/survey_back.jsp (cited February 24, 2023)
30. Agency for Healthcare Research & Quality. Medical Expenditure Panel Survey Content Summary of the Household Interview. Available online at: https://meps.ahrq.gov/survey_comp/hc_data_collection.jsp (Accessed April 19, 2022).
31. National Health Interview Survey (NHIS). Available online at: https://www.cms.gov/About-CMS/Agency-Information/OMH/resource-center/hcps-and-researchers/data-tools/sgm-clearinghouse/nhis (Accessed September 24, 2022).
32. Zuvekas SH, Olin GL. Validating household reports of health care use in the medical expenditure panel survey. Health Serv Res. (2009) 44:1679–700. doi: 10.1111/j.1475-6773.2009.00995.x
33. Olaisen RH, Flocke SA, Smyth KA, Schluchter MD, Koroukian SM, Stange KC. Validating the new primary care measure in the medical expenditure panel survey. Med Care. (2020) 58:52–8. doi: 10.1097/MLR.0000000000001220
34. Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. (1995) 36:1–10. doi: 10.2307/2137284
35. Norton EC, Dowd BE. Log odds and the interpretation of logit models. Health Serv Res. (2018) 53:859–78. doi: 10.1111/1475-6773.12712
37. Machlin S, Yu W, Zodet M. Computing Standard Errors for MEPS Estimates. Medical Expenditure Panel Survey (2005). Available online at: https://meps.ahrq.gov//survey_comp/standard_errors.jsp (cited March 8, 2023)
38. Sifuentes F, Castaneda-Avila AM, Lapane MA, L K. The relationship of aging, complete tooth loss, and having a dental visit in the last 12 months. Clin Exp Dent Res. (2020) 6:550–7. doi: 10.1002/cre2.309
39. Fleming E, Afful J, Griffin SO. Prevalence of tooth loss among older adults: united States, 2015–2018. NCHS Data Brief. (2020) 368:1–8.32600520
40. Lalloo R, Kisely S, Amarasinghe H, Perera R, Johnson N. Oral health of patients on psychotropic medications: a study of outpatients in Queensland. Australas Psychiatry. (2013) 21:338–42. doi: 10.1177/1039856213486308
41. Bardow A, Nyvad B, Nauntofte B. Relationships between medication intake, complaints of dry mouth, salivary flow rate and composition, and the rate of tooth demineralization in situ. Arch Oral Biol. (2001) 46:413–23. doi: 10.1016/S0003-9969(01)00003-6
42. Kisely S, Najman JM. A study of the association between psychiatric symptoms and oral health outcomes in a population-based birth cohort at 30-year-old follow-up. J Psychosom Res. (2022) 157:110784. doi: 10.1016/j.jpsychores.2022.110784
43. de Leon J, Diaz FJ. A meta-analysis of worldwide studies demonstrates an association between schizophrenia and tobacco smoking behaviors. Schizophr Res. (2005) 76:135–57. doi: 10.1016/j.schres.2005.02.010
44. Glassman AH, Helzer JE, Covey LS, Cottler LB, Stetner F, Tipp JE, et al. Smoking, smoking cessation, and major depression. JAMA. (1990) 264:1546–9. doi: 10.1001/jama.1990.03450120058029
45. Lasser K, Boyd JW, Woolhandler S, Himmelstein DU, McCormick D, Bor DH. Smoking and mental illness: a population-based prevalence study. JAMA. (2000) 284:2606–10. doi: 10.1001/jama.284.20.2606
46. Scannapieco FA. Systemic effects of periodontal diseases. Dent. Clin. North Am. (2005) 49:533–50. doi: 10.1016/j.cden.2005.03.002
47. Knaak S, Mantler E, Szeto A. Mental illness-related stigma in healthcare: barriers to access and care and evidence-based solutions. Healthc Manage Forum. (2017) 30:111–6. doi: 10.1177/0840470416679413
48. Ramon T, Grinshpoon A, Zusman SP, Weizman A. Oral health and treatment needs of institutionalized chronic psychiatric patients in Israel. Eur Psychiatry. (2003) 18:101–5. doi: 10.1016/S0924-9338(03)00023-3
49. Setia MS. Methodology series module 3: cross-sectional studies. Indian J Dermatol. (2016) 61:261–4. doi: 10.4103/0019-5154.182410
50. Taylor HL, Menachemi N, Gilbert A, Chaudhary J, Blackburn J. Economic burden associated with untreated mental illness in Indiana. JAMA Health Forum. (2023) 4:e233535–233535. doi: 10.1001/jamahealthforum.2023.3535
51. Nguyen MT, Chan WY, Keeler C. The association between self-rated mental health Status and total health care expenditure: a cross-sectional analysis of a nationally representative sample. Medicine (Baltimore). (2015) 94:e1410. doi: 10.1097/MD.0000000000001410
52. Bezerra CB, Saintrain MV, Nobre MA, Sandrin RL, Galera SC, Bruno ZV. Major depression and associated factors in institutionalized older adults. Psychol Health Med. (2020) 25:909–16. doi: 10.1080/13548506.2019.1710543
Keywords: mental disorders, oral health, dentistry, complete tooth loss, MEPS
Citation: Powell T and Taylor H (2024) The relationship between self-reported poor mental health and complete tooth loss among the US adult population in 2019. Front. Oral. Health 5:1363982. doi: 10.3389/froh.2024.1363982
Received: 31 December 2023; Accepted: 18 March 2024;
Published: 28 March 2024.
Edited by:
Jing Kang, King’s College London, United KingdomReviewed by:
Srinivas Pachava, SIBAR Institute of Dental Sciences, India© 2024 Powell and Taylor. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tasha Powell dG11cnJ5amVAaXUuZWR1
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.