- 1Department of Industrial and Systems Engineering, Virginia Polytechnic Institute and State University, Falls Church, VA, United States
- 2Private Practice of Pediatric Dentistry in Easley and Anderson, Easley, SC, United States
- 3Department of Geography, The State University of New York at Buffalo, Buffalo, NY, United States
Dental caries is a prevalent chronic disease among adolescents. Caries activity increases significantly during adolescence due to an increase in susceptible tooth surfaces, immature permanent tooth enamel, independence in pursuing self-care, and a tendency toward poor diet and oral hygiene. Dental caries in permanent teeth is more prevalent among adolescents in low-income families and racial/ethnic minority groups, and these disparities in adolescent dental caries experience have persisted for decades. Several conceptual and data-driven models have proposed unidirectional mechanisms that contribute to the extant disparities in adolescent dental caries experience. Our objective, using a literature review, is to provide an overview of risk factors contributing to adolescent dental caries. Specifically, we map the interactive relationships of multilevel factors that influence dental caries among adolescents. Such interactive multilevel relationships more closely reflect the complex nature of dental caries experience among the adolescent population. The methods that we use are two-fold: (1) a literature review using PubMed and Cochrane databases to find contributing factors; and (2) the system dynamics approach for mapping feedback mechanisms underlying adolescent dental caries through causal loop diagramming. The results of this study, based on the review of 138 articles, identified individual, family and community-level factors and their interactions contributing to dental caries experience in adolescents. Our results also provide hypotheses about the mechanisms underlying persistence of dental caries among adolescents.
Conclusions: Our findings may contribute to a deeper understanding of the multilevel and interconnected factors that shape the persistence of dental caries experience among adolescents.
1 Introduction
Dental caries is a complex, costly, and prevalent chronic disease. It is affected by multi-level factors ranging from individual's salivary characteristics (1), fluoride exposure (2) and dental anxiety (3), to family's health literacy (4), socioeconomic status (5) and community's geographical context and water fluoridation status (6). Rather than acting separately, these multilevel factors often interact with each other. According to the World Health Organization, dental caries is the 4th most expensive disease to treat (7). In the United States, 58% of adolescents aged 12–19 years have experienced dental caries from 2011 through 2014. The prevalence of dental caries is even higher (i.e., 66%) for adolescents in families whose income is less than 100% of the Federal Poverty Level (FPL) (8). The disparity in dental caries of adolescents’ experience has been persistent, as evidenced by lack of improvement relative to younger age cohorts This issue is not exclusive to the United States; a similar trend is observable globally (9). For instance, the National Australian Child Dental Survey conducted in 2003–2004 reported that 40%–57% of adolescents aged 12–15 had experienced dental caries (10), which highlights the widespread nature of this complex disease.
Fisher-Owens et al. (11) conducted a comprehensive study of factors, using the ecological approach, to depict a conceptual model of multilevel factors influencing children's oral health, including genetic and biological factors, the social environment, the physical environment, health behaviors, and dental and medical care. Although the authors acknowledged the presence of causal relationships and feedback loops, to the best of our knowledge, no study has hypothesized and mapped the causal reciprocal relationships among multilevel factors that influence dental caries among adolescents.
Multi-level factors that influence adolescents’ dental caries are not isolated and often interact, which makes reducing disparities in dental caries a challenging task. Systems science complements other analytic techniques by accounting for interactions among factors, delays in the system, and feedback mechanisms (12). In this study, we conduct a literature review of adolescents’ dental caries experience to identify the reciprocity of multi-level factors contributing to this chronic disease. We further categorize these contributing factors and present their frequency to provide an overview of the literature and highlight areas of opportunities for future interventions to reduce disparities in adolescents’ dental caries experience. We also apply a qualitative system dynamics approach (13) to hypothesize and map the reciprocal relationships of the identified factors. The strength of empirical support for each causal mechanism was assessed and prioritized for those that had been validated through the literature.
2 Methods
2.1 Search strategy
We conducted a literature review to identify journal publications related to adolescents’ dental caries experience. We conducted our search using two databases, PubMed and Cochrane library, between 1979 and 2021. The following keywords were searched in the title and abstract of both databases: dental caries and adolescent (PubMed: (dental caries [Title/Abstract]) AND (adolescent [Title/Abstract]), Cochrane library: (dental caries [Title/Abstract]) AND (adolescent [Title/Abstract]) with Oral Health, Child Health in Cochrane groups).
2.2 Inclusion and exclusion criteria
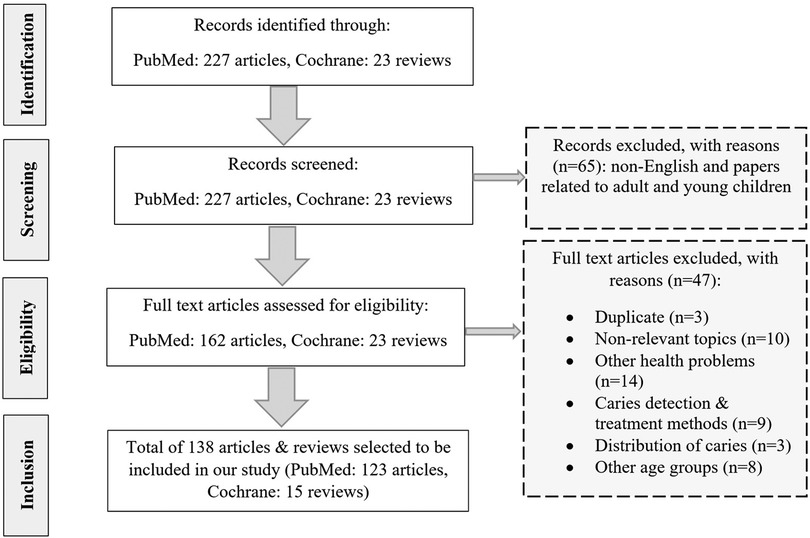
After an initial screening of the papers found in PubMed, we excluded articles not written in the English language and articles related to adults and young children. Also, after consulting with specialists in the field of oral health, we decided to only include Cochrane reviews and exclude Cochrane protocols and trials from the search results found in the Cochrane library. Then we combined all the articles found from the two databases and excluded the duplicates. After reading the abstracts of our combined list of papers, we excluded articles that focused on non-relevant topics, other health problems, comparison of caries detection & treatment methods, the distribution of caries among various teeth, and other age groups (Figure 1).
2.3 Study selection
After screening the abstract of the papers found in PubMed and Cochrane library, we selected 138 papers to be included in our study. From reviewing the selected papers, we identified factors affecting dental caries in adolescents that were studied in these papers and categorized the papers according to these identified factors. Then we mapped the feedback mechanisms that were revealed from this review of the literature using the Vensim software (https://vensim.com/software/). Key steps and results of this process are summarized below, with additional details provided in the Supplementary Material.
3 Results
3.1 Identification of factors
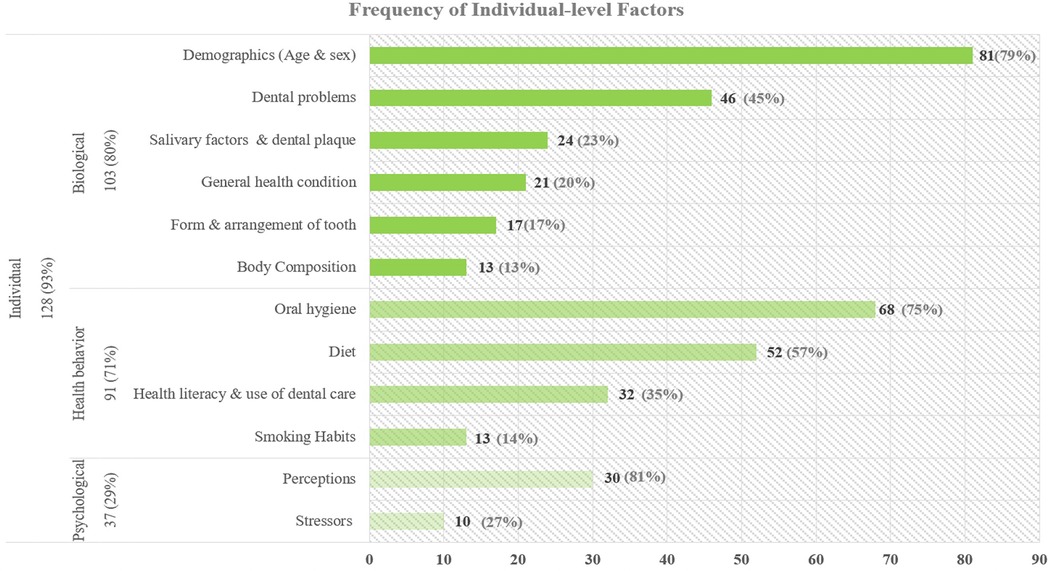
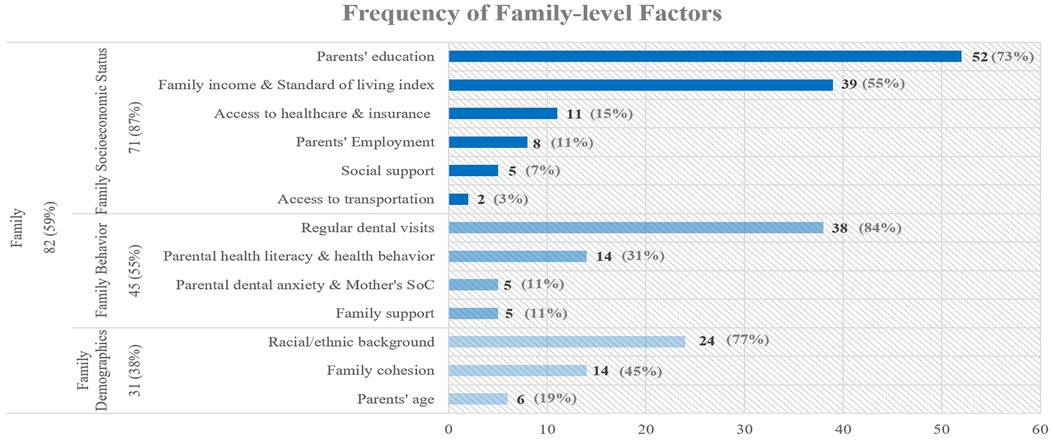
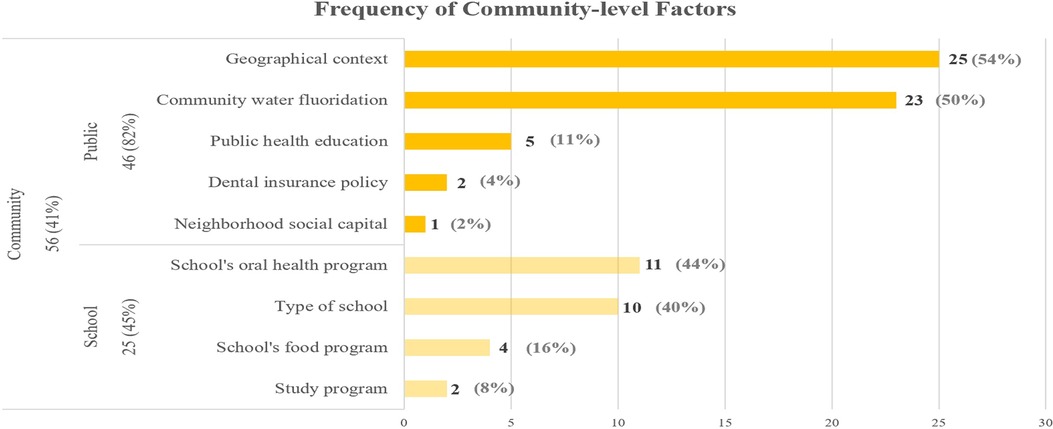
After reviewing the 138 articles selected by our search strategy, we identified 8 factors at 3 levels: individual level (n = 128), family level (n = 82), and community level (n = 56). Figure 2 demonstrates the categorization of articles by level along with the number of articles for each factor. Individual-level studies focused on three types of factors: biological (n = 103), health behavior (n = 91) and psychological (n = 37). Family-level articles focused on three types of factors: family socioeconomic status (n = 71), family behavior (n = 45) and family demographics (n = 31) factors. Community-level articles focused on two factors: public (n = 46) and school (n = 25). In the following sections, we further subcategorize each of these factors and summarize the related articles.
3.1.1 Individual-level factors
The most common factors studied in dental caries research are at the individual level. Figure 3 depicts the frequency of each factor and related subcategories in individual-level articles.
3.1.1.1 Biological
Biological factors are among the most common influences being studied in the research related to adolescent dental caries. Most studies controlled for demographics of subjects such as age and sex, and some found that adolescent girls have a higher chance of developing caries (14–17). Among dental problems, gingival conditions such as gingival bleeding and periodontal gum disease are examined in some caries research, as they both often result from poor oral hygiene that also leads to dental caries (18–20). Traumatic dental injuries and tooth pain, resulting from dental caries (21), have a negative impact on the oral health status of adolescents (22, 23). Studies show a positive association among caries index and visible plaque or dental biofilm (24), high levels of S. mutans and lactobacilli (25), salivary flow rate, reduced pH and low buffering capacity (26–28). In addition, genetic disorders such as Down syndrome (29), cleft syndrome (30), and family history of dental caries (31) were investigated. Multiple studies in the literature have analyzed the relationships between dental caries and several health conditions such as diabetes and poor metabolic control (15, 19, 32), obesity (33–35), juvenile idiopathic arthritis (36), and asthma (37, 38). Malocclusion is one of the conditions in form and arrangement of tooth, which is an identified risk factor in dental caries research as alignment and spacing of early permanent dentition is an important factor in developing caries (39–43). In addition, enamel defects in low birth weight adolescents (which are detectable once the tooth has emerged into the oral cavity) (44), body mass index (BMI), and waist circumference from body composition factors are significantly associated with dental caries (45).
3.1.1.2 Health behavior
Multiple components of adolescent health behavior including oral hygiene, dietary habits, and use of dental care have been studied widely. Oral hygiene (43, 46), specifically toothbrushing twice a day (43, 47, 48) using a fluoridated toothpaste, is consistently found to reduce dental caries (49–52). In addition, use of dental floss (53) and topical fluoride exposure (54, 55), such as fluoride mouth rinse (56), fluoride gels (57) and fluoride varnishes (58) are also recommended as their benefits for oral health are well established throughout the literature. The other health behavior frequently mentioned in studies of dental caries is diet (59). Several studies have shown that sugar consumption (33, 60–63), specifically sugar before bedtime (64), frequent snacking (46, 65, 66), irregular main meals, and skipping breakfast (65, 67) increase the risk of developing caries among adolescents. Health literacy and use of dental care affect dental caries (48, 68). Health literacy is positively associated with use of dental care (48, 69), communication with a dentist (48) and healthy diet (70), which enhance oral health quality of life (18). In addition, use of pit and fissure sealants prevents dental caries in adolescents (24, 54, 71–73). On the other hand, dental caries and oral health status of adolescents may affect school performance (74), school absenteeism (21), and future employment outcome (75), and consequently health literacy and use of dental care. Finally, other habits, such as smoking (35, 60, 65, 66) and use of snuff or smokeless tobacco (60), are also risk factors, as tobacco exposure (76) is associated with dental caries among adolescents. This association might work in both directions, as one study suggests that having dental caries in adolescence could be an indicator of becoming a smoker in adulthood (77). Alcohol intake has also been evaluated as a risk factor in some dental caries research (35, 60, 78, 79).
3.1.1.3 Psychological
Increasing evidence also highlights the impact of self-perception on adolescents’ dental caries experience and oral health status. Having healthy teeth is socially more desirable and increases adolescent's happiness (42), while untreated dental caries can negatively impact adolescents’ self-esteem and oral health quality of life (68, 80, 81). Adolescents are susceptible to peer influence which affects their health behavior and diet (81). Self-efficacy seems to play an important role in improving oral health practices through diet modification, reduction of sugar consumption, frequent toothbrushing and dental flossing (53, 81–84). High sense of coherence is usually associated with good health behaviors and studies indicate that adolescents with lower sense of coherence (85) are more likely to develop dental caries. On the other hand, another study has shown a positive association between higher internal locus of control (those who believe internal factors are responsible for their health) and dental caries risk (86). Avoidance behavior and unmet dental care needs of adolescents can be due to some common stressors such as fear of pain and dental anxiety (87), which may result from traumatic events and repeated painful experiences (88). Multiple studies have shown that dental caries prevalence is higher among adolescents who have higher levels of dental anxiety (18, 53, 89, 90).
3.1.2 Family-level factors
The second most common factors in literature were identified at the family level. Figure 4 presents the frequency of family level subfactors discussed in the articles.
3.1.2.1 Family socioeconomic
Several socioeconomic factors can contribute to untreated dental caries among adolescents, such as parents’ education, especially the mother's as the usual active caregiver, which can influence family and adolescents’ health literacy (16, 48, 84, 91, 92), family income, which can impact the household's access to dental care and ability to maintain a healthy diet (27, 92–95), access to healthcare and health insurance (14, 59, 96, 97), parents’ employment, especially the father's, which is usually how their children get dental insurance and can affect adolescents’ health behavior (84), access to social support and social benefits such as unemployment insurance (79, 81, 94, 98) and lack of access to transportation (43, 54).
3.1.2.2 Family behavior
Regular dental visits protect against adolescent dental caries, but their occurrence depends on parental commitment (47, 48, 66, 68, 69, 91, 99). Parental health literacy, especially mother's oral health knowledge (48, 54, 91) is negatively associated with adolescent's dental caries experience. Also, health values, beliefs, lifestyle (27, 43, 54, 96) and health behavior of parents (4, 81, 100) are major risk factors for adolescent dental caries prevalence. According to multiple studies, mothers’ sense of coherence (SoC) has a protective effect against adolescents’ dental caries (85, 101, 102). Also, parental dental anxiety, in terms of experiencing stress and painful dental treatment seems to impact their attitude toward seeking dental care for their children (96), which can consequently increase adolescent's chance of developing caries (91). Family support meaning having parents who promote and supervise good oral health, positively impacts oral health status of adolescents (43, 81, 85), while parental punishment is associated with high levels of caries among adolescents (103).
3.1.2.3 Family demographics
In addition, racial/ethnic background such as belonging to a non-white ethnicity or minority groups (5, 14, 48, 62, 69, 96) and being a recent immigrant (27) increase odds of dental caries. Also, higher level of family cohesion has a positive impact on the oral health literacy and dental visits of adolescents, which will consequently reduce their chances of developing caries (48, 69). Having separated parents and higher number of residents in the household are positively associated with untreated dental caries (94). Studies have included variables related to parental age (4, 15, 44, 48, 69, 91) such as young parents with less education in their analysis as a possible risk factor for adolescents’ dental caries.
3.1.3 Community-level factors
The third most common factors in this literature review were identified at the community level. Figure 5 shows the frequency of community level subfactors among articles.
3.1.3.1 Public
Most studies that examine the effect of geographical context on adolescents’ chance of developing caries, have found that living in a rural or remote area is associated with higher rates of dental caries (10, 17, 103, 104), while one study in Sweden showed that adolescents living in urban areas had a higher prevalence of dental caries, possibly due to higher access to cariogenic diet (105). Community water fluoridation is one of the most important community level factors, with its anti-caries benefit being well established in the literature (6, 10, 14, 47, 106–109). Previous studies have emphasized the importance of public health education in the form of educating the community about oral health (43), promotion of oral hygiene at maternal and child healthcare centers (97), preventive dental programs (110), dental health education (111) and interventions for reducing sugar consumption (112). Dental insurance policies such as low reimbursement by Medicaid (43) and coverage expansion of dental care (93) affect adolescents’ dental health. One study had included neighborhood social capital (which measures the trust and norms of reciprocity in the society) for analyzing inequalities in dental caries among adolescents but didn’t find any significant association between the two (79).
3.1.3.2 School
Prevalence of dental caries among adolescents seems to be dependent on several school related factors including school based oral health programs that may include dental screenings, oral health education and supervised fluoride mouth rinse programs (56, 97, 113–116), type of school (for example, higher prevalence of dental caries reported in public schools than private schools) (27, 68, 86, 92, 104), school's food program such as availability of healthy meals, drinking water and fruits instead of vending machines full of sugary drinks and snacks (43, 54, 112, 117), and finally adolescents’ study program (general, sports, vocational), which entails a particular social context that leads them to choose that program (for example, lower prevalence of dental caries for those enrolled in general studies and sports vs. the vocational program) (66, 78).
Results of this literature review demonstrate that among 138 selected articles, about 34% (n = 47) of the papers have only focused on one level, while about 40% (n = 54) papers have focused on two levels and only about 26% (n = 37) of the papers have focused on all three levels. This result shows that few studies have examined diverse factors in adolescents’ dental research (lack of detail complexity). In addition, dynamic complexity of adolescents’ dental caries, which arises from interactions among multiple factors, have not been explored in the literature. In the following section, we present the first map of reciprocal influences which is built upon our literature review.
3.2 Mapping feedback mechanisms
System dynamics is an approach for understanding the structure of complex systems and analyzing their behaviors (118–120). Dynamic complexities arise from interactions between elements of a system expressed as feedback mechanisms and accumulations of people, materials or information. A feedback loop is a series of variables and causal links that create a closed loop of causal influences (Figure 6). An arrow with a positive sign means that a change in the first variable produces a change in the second variable in the same direction, keeping all else constant. For example, the arrow relating two variables in Figure 6, “brushing with fluoride toothpaste” and “topical fluoride exposure” is positive, which means that increase in the former leads to an increase in the latter. An arrow with a negative sign means that a change in the first variable produces a change in the second variable in the opposite direction, keeping all else constant. For example, as shown in Figure 6, an increase in adolescent dental caries lowers self-esteem.
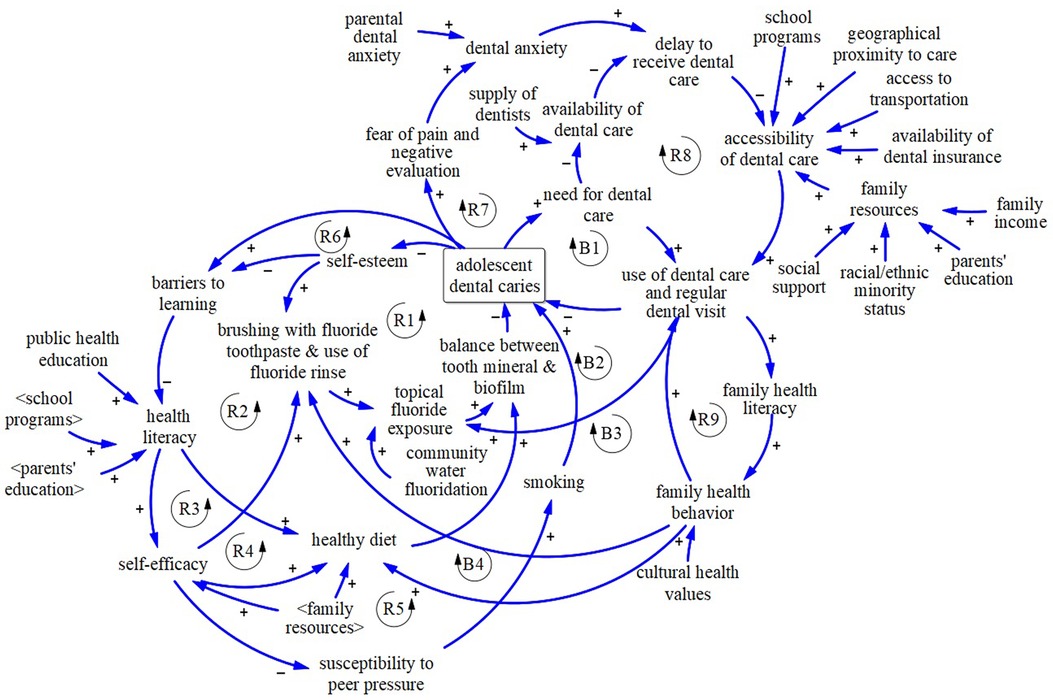
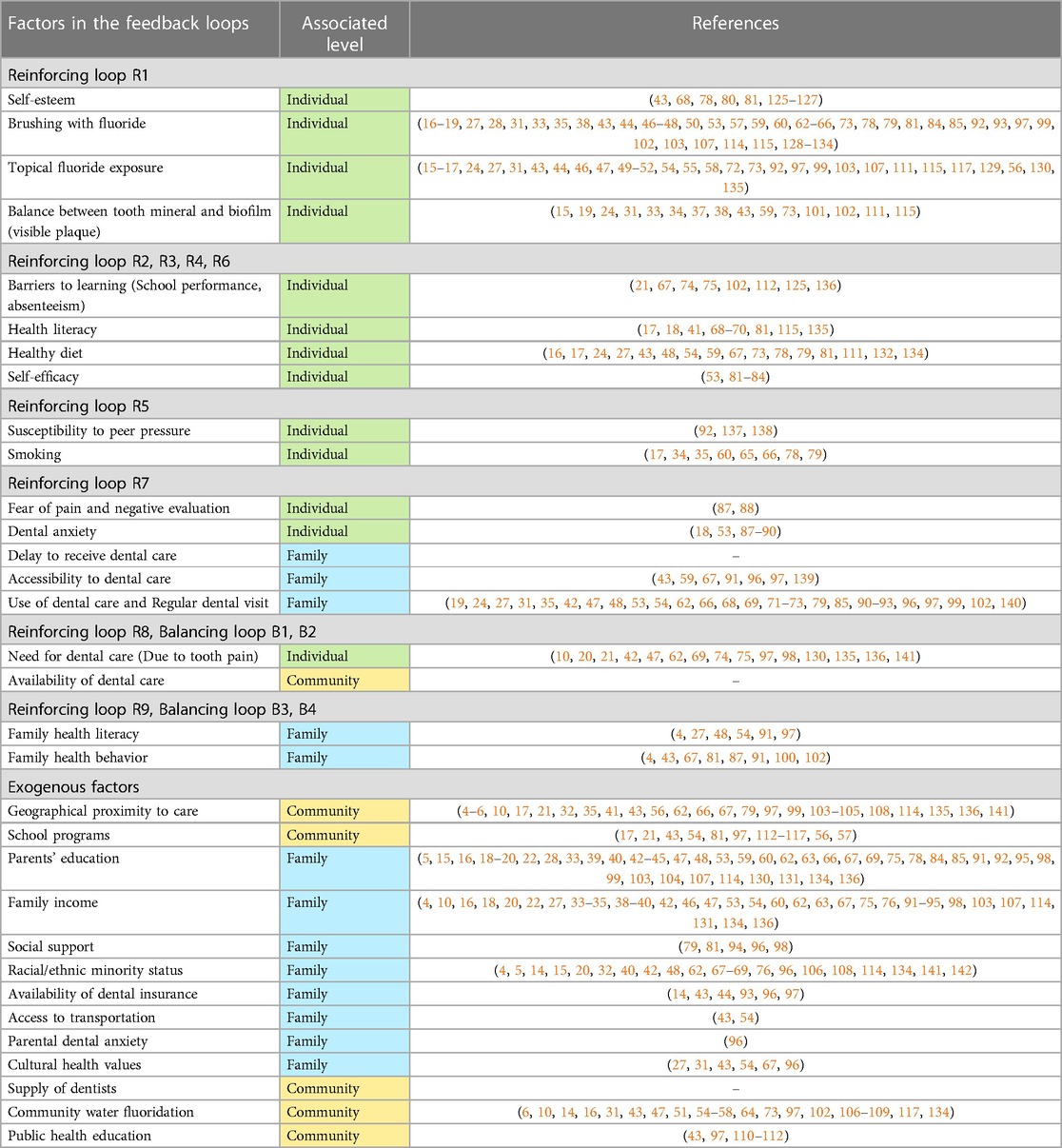
Figure 6. Causal loop diagram of feedback mechanisms affecting adolescents’ dental caries.  : Reinforcing Loop. R1: Dental caries & Deterioration in Self-esteem. R2: Learning Barriers, Health Literacy & Diet. R3: Health Literacy & Self-efficacy. R4: Self-efficacy & Diet. R5: Self-efficacy & Peer Pressure. R6: Dental caries & Barriers (School Performance). R7: Fear of Pain & Dental Anxiety. R8: Overburdened Dental clinics & Treatment Delay. R9: Family Health Behavior & Regular Dental Visits.
: Reinforcing Loop. R1: Dental caries & Deterioration in Self-esteem. R2: Learning Barriers, Health Literacy & Diet. R3: Health Literacy & Self-efficacy. R4: Self-efficacy & Diet. R5: Self-efficacy & Peer Pressure. R6: Dental caries & Barriers (School Performance). R7: Fear of Pain & Dental Anxiety. R8: Overburdened Dental clinics & Treatment Delay. R9: Family Health Behavior & Regular Dental Visits.  : Balancing Loop. B1: Need-Based Dental Visit. B2: Dental Visit & Fluoride Exposure. B3: Dental Visit & Family Health Behavior. B4: Family Health Behavior & Healthy Diet.
: Balancing Loop. B1: Need-Based Dental Visit. B2: Dental Visit & Fluoride Exposure. B3: Dental Visit & Family Health Behavior. B4: Family Health Behavior & Healthy Diet.
All dynamics are created from the interaction of two types of feedback mechanisms, expressed in reinforcing loops and balancing loops. Reinforcing (positive) feedback loops amplify the direction of original movement of any variable in the loop. For instance, reinforcing loop R1 in Figure 6, depicts that higher self-esteem improves oral hygiene behaviors such as brushing with fluoride toothpaste (121, 122) and use of fluoride rinse (123), which increases topical fluoride exposure. Higher topical fluoride exposure improves balance between mineral and biofilm, which lowers dental caries experience and leads to even higher self-esteem (124). Balancing (negative) feedback loops counteract the direction of the original change of a variable in the loop. For example, after experiencing dental caries, one may perceive the need for dental care and then may use it, which would reduce dental caries experience (balancing loop B1 in Figure 6). A causal loop diagram, which consists of reinforcing and balancing feedback loops, is used to show the reciprocal relationships among variables of a system (Figure 6).
3.3 Causal loop diagram
After identifying factors influencing adolescent dental caries in the literature, we mapped their reciprocal relationships using the system dynamics approach (Figure 6). Table 1 presents references for the factors included in the causal loop diagram that are extracted from the literature. A brief description of the causal loop diagram follows.
Grounded in the attribution and social learning theories, studies showed that psychological factors such as self-esteem can reduce dental caries experience both through improving brushing with fluoride toothpaste and use of fluoride rinse (143, 144) (Reinforcing loop R1 in Figure 6) and reducing school absence and barriers to learning (Reinforcing loop R2). Self-esteem and oral health quality of life affects school performance and absenteeism and health literacy (145). Higher health literacy increases the chance of eating a healthy diet, which improves the balance between tooth mineral and biofilm and reduces dental caries experiences (54) (Reinforcing loop R2 in Figure 6). Higher health literacy also raises self-efficacy, which increases brushing with fluoride toothpaste and use of fluoride rinse and reduces adolescent dental caries (Reinforcing loop R3). Reinforcing loop R4 captures the impact of self-efficacy on consuming a healthy diet and experiencing lower dental caries. Moreover, adolescents with lower self-efficacy are more likely to be influenced by peer pressure and develop bad habits such as smoking which will subsequently increase their chance of dental caries (Reinforcing loop R5 in Figure 6) (81, 146, 147). Note that reinforcing loops can act as a virtuous or vicious cycle. For example, when reinforcing loop R6 acts as a vicious cycle, it exacerbates dental caries through dental caries-related morbidity, which leads to school absence (21, 137, 148) and over time, it may influence health literacy and lead to a poorer diet and oral hygiene, and more dental caries experience (Reinforcing loop R6 in Figure 6) (138).
As shown in Figure 6, based on Berggren's model of dental fear and anxiety (149, 150), experiencing symptoms of dental caries could lead to fear of negative evaluation, which creates anxiety and avoidance or delay of dental care, leading to further deterioration of dental status (Reinforcing loop R7). Use of dental care depends on accessibility of dental care. Family resources, dental insurance, community characteristics, and school programs affect adolescent access to dental care (151–153). Disadvantaged adolescents tend to rely on overwhelmed safety net dental clinics and may therefore experience delays in obtaining care. This leads to progression of caries that could have been avoided or resolved with less invasive and expensive approaches, and further overloads the dental safety net (154) thus leading to lower accessibility of dental care for disadvantaged individuals (Reinforcing loop R8 in Figure 6). Thus, higher dental caries might overburden safety net clinics and lead to delay and higher dental caries experience of disadvantaged adolescents. Adolescents are twice as likely to forego using dental care if their parents had no dental visit in a year (155) (Reinforcing loop R9).
Balancing loops B1–B4 depict counteracting mechanisms that influence dental caries. After experiencing dental caries, a patient may seek preventive dental care including fluoride treatment that improves the balance between tooth mineral and biofilm and reduces the risk of new dental caries (Balancing loop B1 and B2). Use of dental care may also improve family health behavior and lead to more brushing with fluoride toothpaste and use of fluoride rinse (Balancing loop B3), as well as a healthy diet (Balancing loop B4), which will reduce the risk of adolescent dental caries experience (156, 157).
The map includes both endogenous variables (i.e., dynamic individual and environmental characteristics that arise from within the model boundary) and exogenous factors (i.e., characteristics from outside the model boundary). Characteristics such as racial/ethnic minority status, community water fluoridation, parental education are included as exogenous (non-modifiable) factors to the causal loop diagram. Genetic factors (e.g., quality of saliva and developmental defects of enamel and/or dentin) are also included as exogenous influences (Figure 6).
4 Discussion
Our study identifies and depicts the reciprocal interactions among multi-level factors and their contribution to adolescents’ dental caries experience using the system dynamics approach. Previous research has extensively examined individual, family, and community level influences on adolescents’ dental caries experience. Fisher-Owens and colleagues applied the ecological approach and provided a comprehensive list of multi-level factors that affect children's oral health, but underscored the difficulty of capturing causality due to the complex interplay of the factors involved (158). Our study takes a first step to hypothesize these reciprocal relationships and provide a systems perspective to enhance understanding about adolescent dental caries and the persistence of dental caries among adolescents. We identified the feedback mechanisms contributing to dental caries in adolescents based on a review of the literature with nine reinforcing and four balancing loops. These feedback loops encompass individual, family and community level factors.
We categorized factors studied in the literature and their reciprocal interactions at the include individual, family, and community level influences. The majority of the 138 articles, 93% (n = 128), examined individual level factors, while 59% (n = 82) and 41% (n = 56) of the studies included the family and community level factors, respectively. The top three influences frequently examined in the individual-level studies besides demographic factors such as age and sex (14–17), are oral hygiene (43, 46), diet (59), and dental problems (18–20). In articles that included family factors, the most frequently studied sub-factors are parents’ education (16, 48, 84, 91, 92), parental health literacy (48, 54, 91), dental visit (47, 48, 66, 68, 69, 91, 99), and family income (27, 92–95). Lastly, in the community-level studies, geographical context (10, 17, 103, 104), community water fluoridation (6, 10, 14, 47, 106–109), and schools’ oral health programs (56, 97, 113–116) are most frequently studied.
The causal loop diagram mapped in Figure 6 provides multiple insights. First, Reinforcing Loop R1 and R3 hypothesize the downward spiral of deterioration in self-esteem, self-efficacy, and dental health. Evidence-based school programs can work as a leverage by increasing health literacy to turn these vicious cycles into virtuous cycles and improve dental health. Second, reinforcing loop R8 hypothesizes the mechanisms underlying the persistence of dental caries among adolescents, particularly for lower socioeconomic groups. Disadvantaged adolescents are likely to receive dental care in overburdened dental safety net clinics and may therefore have to delay treatment, which exacerbates dental caries and requires more intensive and time-consuming treatments, further straining the system. State and local governments can increase use of dental care by expanding dental insurance, school programs, and improving community characteristics. In addition, the federal government can enact policies to increase the supply of dentists and increase access through improved reimbursement for dental care and expansion of the dental safety net. Third, as specified in reinforcing loop R9, family health behavior and adolescents’ use of dental care reinforce each other. Providing dental insurance for adults through Medicaid expansion has spillover or “welcome mat” effects on children's enrollment (159), meaning that children whose parents become eligible for Medicaid expansion are more likely to gain coverage. Thus, it is likely that targeting parents or children can enhance the dental health of the other group. Fourth, the causal loop diagram depicts multiple mechanisms through which dental caries can be affected and can explain heterogeneity in trajectories of adolescent dental caries. In other words, this map can be used to explain why some adolescents with similar demographic and socioeconomic characteristics may experience different trajectories of dental caries.
Our study's findings offer more than insights – they provide a pathway to actionable strategies, notably in the realm of oral health education. Building on the provided insights, we envision an intervention strategy inspired by motivational interviewing, which harmonizes well with our system dynamics approach. This strategy involves presenting individuals with a personalized menu of solutions to address dental caries at different levels. For instance, individuals might commit to regular brushing, families could reduce soda consumption, and communities could advocate for healthier vending machine policies in schools. What sets our approach apart is its ability to embrace the complexity of real-life feedback loops, making interventions more practical and attuned to people's daily realities. The framework developed in this study also provides a rich foundation for future simulation research and contributes a powerful tool for identifying prevention practices and policies to reduce adolescent dental caries.
This study has some limitations that should be acknowledged. First, the literature search was conducted using two platforms, PubMed, and Cochrane, which may exclude relevant studies from other sources. Although these two platforms serve as comprehensive databases for health studies, a productive extension of this work would be to conduct a systematic literature review with additional databases to minimize the likelihood of omitting studies related to adolescent dental caries. Second, the determination of which studies to include was based on scope rather than quality. Extensions of this work may usefully assess the quality of such studies in addition to their scope. Third, our map draws from existing literature, primarily comprised of cross-sectional studies, which can offer association between variables but cannot establish causality. As such, the causal loop diagram developed in this study is considered a hypothesis suitable for further development and testing using a quantitative simulation approach. Implementation of this causal hypothesis in a simulation model for policy analysis is a logical extension of this study in keeping with the system dynamics approach. Such analysis would reveal which feedback mechanisms are most salient under different circumstances and suggest which interventions to reduce dental caries would provide the greatest leverage.
To sum up, previous research on dental caries among adolescents has identified risk factors without accounting for reciprocal relationships among multilevel factors. To address this gap, this study applies the system dynamics method to develop a novel causal loop diagram, or causal map, of dental caries among adolescents. The literature-based causal loop diagram that we develop in this study identifies several reciprocal mechanisms underlying dental caries among adolescents, encompassing individual-, family-, and community-level factors. We use the map of reciprocal mechanisms to consider complex feedback mechanisms affecting adolescent dental caries that arise from these multilevel factors.To conclude, our findings may contribute to a deeper understanding of the multilevel and interconnected factors that shape the persistence of dental caries experience among adolescents and designing comprehensive interventions to reduce them.
Author contributions
FS: Formal Analysis, Methodology, Software, Visualization, Writing – original draft, Writing – review & editing, Conceptualization, Data curation. NH: Conceptualization, Supervision, Writing – review & editing, Formal Analysis, Methodology. BP: Writing – review & editing, Conceptualization, Validation. SM: Writing – review & editing, Conceptualization, Formal Analysis.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
Virginia Tech's Open Access Subvention Fund supported publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/froh.2023.1285347/full#supplementary-material
References
1. Cunha-Cruz J, Scott J, Rothen M, Mancl L, Lawhorn T, Brossel K, et al. Salivary characteristics and dental caries: evidence from general dental practices. J Am Dent Assoc. (2013) 144(5):e31–40. doi: 10.14219/jada.archive.2013.0159
2. Cheng LL. Limited evidence suggests fluoride mouthrinse may reduce dental caries in children and adolescents. J Am Dent Assoc. (2017) 148(4):263–6. doi: 10.1016/j.adaj.2017.02.002
3. Schreiber EH, Scales JL. Anxiety and dental health in institutionalized delinquent adolescents. J Am Dent Assoc. (1971) 82(3):600–2. doi: 10.14219/jada.archive.1971.0097
4. Lundeen EA, Park S, Onufrak S, Cunningham S, Blanck HM. Adolescent sugar-sweetened beverage intake is associated with parent intake, not knowledge of health risks. Am J Health Promot. (2018) 32(8):1661–70. doi: 10.1177/0890117118763008
5. Polk DE, Kim S, Manz M, Weyant RJ. Is there an Appalachian disparity in dental caries in Pennsylvania schoolchildren? Community Dent Oral Epidemiol. (2015) 43(1):24–32. doi: 10.1111/cdoe.12135
6. Englander HR, DePaola PF. Enhanced anticaries action from drinking water containing 5 ppm fluoride. J Am Dent Assoc. (1979) 98(1):35–9. doi: 10.14219/jada.archive.1979.0030
7. Petersen PE. World health organization global policy for improvement of oral health - world health assembly 2007. Int Dent J. (2008) 58(3):115–21. doi: 10.1111/j.1875-595X.2008.tb00185.x
8. Dye BA, Mitnik GL, Iafolla TJ, Vargas CM. Trends in dental caries in children and adolescents according to poverty status in the United States from 1999 through 2004 and from 2011 through 2014. J Am Dent Assoc. (2017) 148(8):550–65.e7. doi: 10.1016/j.adaj.2017.04.013
9. Available online at: https://capp.mau.se/country-areas/.
10. Skinner J, Johnson G, Phelan C, Blinkhorn A. Dental caries in 14- and 15-year-olds in New South Wales, Australia. BMC Public Health. (2013) 13:1060. doi: 10.1186/1471-2458-13-1060
11. Fisher-Owens SA, Gansky SA, Platt LJ, Weintraub JA, Soobader M-J, Bramlett MD, et al. Influences on children’s oral health: a conceptual model. Pediatrics. (2007) 120(3):e510–20. doi: 10.1542/peds.2006-3084
12. Mabry PL, Olster DH, Morgan GD, Abrams DB. Interdisciplinarity and systems science to improve population health: a view from the NIH office of behavioral and social sciences research. Am J Prev Med. (2008) 35(2 Suppl):S211–24. doi: 10.1016/j.amepre.2008.05.018
13. Kim H, Andersen DF. Building confidence in causal maps generated from purposive text data: mapping transcripts of the federal reserve. Syst Dyn Rev. (2012) 28(4):311–28. doi: 10.1002/sdr.1480
14. Ditmyer M, Dounis G, Mobley C, Schwarz E. Inequalities of caries experience in nevada youth expressed by DMFT index vs. significant caries index (SiC) over time. BMC Oral Health. (2011) 11:12. doi: 10.1186/1472-6831-11-12
15. Hicks MJ, Flaitz CM. Epidemiology of dental caries in the pediatric and adolescent population: a review of past and current trends. J Clin Pediatr Dent. (1993) 18(1):43–9. PMID: 8110613
16. Warren JJ, Van Buren JM, Levy SM, Marshall TA, Cavanaugh JE, Curtis AM, et al. Dental caries clusters among adolescents. Community Dent Oral Epidemiol. (2017) 45(6):538–44. doi: 10.1111/cdoe.12317
17. Zeng L, Peng Y, Xu T, Wen J, Wan L, Ou X, et al. Dental caries and associated factors among adolescents aged 12–15 in Jiangxi Province, China. J Public Health Dent. (2020) 80(3):217–26. doi: 10.1111/jphd.12371
18. Xiang B, Wong HM, Perfecto AP, McGrath CPJ. The association of socio-economic status, dental anxiety, and behavioral and clinical variables with adolescents’ oral health-related quality of life. Qual Life Res. (2020) 29(9):2455–64. doi: 10.1007/s11136-020-02504-7
19. Elheeny AAH. Oral health status and impact on the oral health-related quality of life of Egyptian children and early adolescents with type-1 diabetes: a case-control study. Clin Oral Investig. (2020) 24(11):4033–42. doi: 10.1007/s00784-020-03273-w
20. Peres KG, Peres MA, Araujo CL, Menezes AM, Hallal PC. Social and dental status along the life course and oral health impacts in adolescents: a population-based birth cohort. Health Qual Life Outcomes. (2009) 7:95. doi: 10.1186/1477-7525-7-95
21. Krisdapong S, Prasertsom P, Rattanarangsima K, Sheiham A. School absence due to toothache associated with sociodemographic factors, dental caries status, and oral health-related quality of life in 12- and 15-year-old thai children. J Public Health Dent. (2013) 73(4):321–8. doi: 10.1111/jphd.12030
22. Feldens CA, Senna RA, Vargas-Ferreira F, Braga VS, Feldens EG, Kramer PF. The effect of enamel fractures on oral health-related quality of life in adolescents. Dent Traumatol. (2020) 36(3):247–52. doi: 10.1111/edt.12526
23. Kramer PF, Pereira LM, Ilha MC, Borges TS, Freitas MPM, Feldens CA. Exploring the impact of malocclusion and dentofacial anomalies on the occurrence of traumatic dental injuries in adolescents. Angle Orthod. (2017) 87(6):816–23. doi: 10.2319/041417-258.1
24. Wright JT. The burden and management of dental caries in older children. Pediatr Clin North Am. (2018) 65(5):955–63. doi: 10.1016/j.pcl.2018.05.005
25. Kingman A, Little W, Gomez I, Heifetz SB, Driscoll WS, Sheats R, et al. Salivary levels of Streptococcus mutans and lactobacilli and dental caries experiences in a US adolescent population. Community Dent Oral Epidemiol. (1988) 16(2):98–103. doi: 10.1111/j.1600-0528.1988.tb01852.x
26. Llena-Puy MC, Montañana-Llorens C, Forner-Navarro L. Cariogenic oral flora and its relation to dental caries. ASDC J Dent Child. (2000) 67(1):42–6. PMID: 10736657
27. Reddy P, Krithikadatta J, Srinivasan V, Raghu S, Velumurugan N. Dental caries profile and associated risk factors among adolescent school children in an Urban South-Indian city. Oral Health Prev Dent. (2020) 18(1):379–86. doi: 10.3290/j.ohpd.a43368
28. González-Aragón Pineda AE, García Pérez A, García-Godoy F. Salivary parameters and oral health status amongst adolescents in Mexico. BMC Oral Health. (2020) 20(1):190. doi: 10.1186/s12903-020-01182-8
29. González-Aragón Pineda AE, García Pérez A, García-Godoy F. Caries experience in children and adolescents with down syndrome: a systematic review and meta-analysis. Arch Oral Biol. (2020) 115:104715. doi: 10.1016/j.archoralbio.2020.104715
30. Pisek A, Pitiphat W, Chowchuen B, Pradubwong S. Oral health status and oral impacts on quality of life in early adolescent cleft patients. J Med Assoc Thai. (2014) 97(Suppl 10):S7–16. PMID: 25816532
31. Anderson M. Risk assessment and epidemiology of dental caries: review of the literature. Pediatr Dent. (2002) 24(5):377–85. PMID: 12412952
32. Wang Y, Xing L, Yu H, Zhao L. Prevalence of dental caries in children and adolescents with type 1 diabetes: a systematic review and meta-analysis. BMC Oral Health. (2019) 19(1):213. doi: 10.1186/s12903-019-0903-5
33. Carmo CDS, Ribeiro MRC, Teixeira JXP, Alves CMC, Franco MM, França AKTC, et al. Added sugar consumption and chronic oral disease burden among adolescents in Brazil. J Dent Res. (2018) 97(5):508–14. doi: 10.1177/0022034517745326
34. Moreira ARO, Batista RFL, Ladeira LLC, Thomaz EBAF, Alves CMC, Saraiva MC, et al. Higher sugar intake is associated with periodontal disease in adolescents. Clin Oral Investig. (2021) 25(3):983–91. doi: 10.1007/s00784-020-03387-1
35. Kim JA, Choi HM, Seo Y, Kang DR. Relations among obesity, family socioeconomic status, oral health behaviors, and dental caries in adolescents: the 2010–2012 Korea national health and nutrition examination survey. BMC Oral Health. (2018) 18(1):114. doi: 10.1186/s12903-018-0576-5
36. Skeie MS, Gil EG, Cetrelli L, Rosén A, Fischer J, Åstrøm AN, et al. Oral health in children and adolescents with juvenile idiopathic arthritis - a systematic review and meta-analysis. BMC Oral Health. (2019) 19(1):285. doi: 10.1186/s12903-019-0965-4
37. Stensson M, Wendt L-K, Koch G, Oldaeus G, Lingström P, Birkhed D. Caries prevalence, caries-related factors and plaque pH in adolescents with long-term asthma. Caries Res. (2010) 44(6):540–6. doi: 10.1159/000321566
38. Sodré CS, de Carvalho Ferreira D, Vieira MS, Cavalcante FS, Braga BS, Saintive S, et al. Clinical oral profile of pediatric patients with atopic dermatitis: a cross-sectional study. Oral Dis. (2021) 27(7):1834–46. doi: 10.1111/odi.13721
39. Sá-Pinto AC, Rego TM, Marques LS, Martins CC, Ramos-Jorge ML, Ramos-Jorge J. Association between malocclusion and dental caries in adolescents: a systematic review and meta-analysis. Eur Arch Paediatr Dent. (2018) 19(2):73–82. doi: 10.1007/s40368-018-0333-0
40. Feldens CA, dos Santos Dullius AI, Kramer PF, Scapini A, Busato ALS, Vargas-Ferreira F. Impact of malocclusion and dentofacial anomalies on the prevalence and severity of dental caries among adolescents. Angle Orthod. (2015) 85(6):1027–34. doi: 10.2319/100914-722.1
41. de Llano-Pérula MC, Ricse E, Fieuws S, Willems G, Orellana-Valvekens MF. Malocclusion, dental caries and oral health-related quality of life: a comparison between adolescent school children in urban and rural regions in Peru. Int J Environ Res Public Health. (2020) 17(6):2038. doi: 10.3390/ijerph17062038
42. Tuchtenhagen S, Ortiz FR, Ardenghi TM, Antunes JLF. Oral health and happiness in adolescents: a cohort study. Community Dent Oral Epidemiol. (2021) 49(2):176–85. doi: 10.1111/cdoe.12589
43. Guzmán-Armstrong S. Rampant caries. J Sch Nurs. (2005) 21(5):272–8. doi: 10.1177/10598405050210050501
44. Nelson S, Albert JM, Lombardi G, Wishnek S, Asaad G, Kirchner HL, et al. Dental caries and enamel defects in very low birth weight adolescents. Caries Res. (2010) 44(6):509–18. doi: 10.1159/000320160
45. Chakravathy PK, Chenna D, Chenna V. Association of anthropometric measures and dental caries among a group of adolescent cadets of Udupi district, South India. Eur Arch Paediatr Dent. (2012) 13(5):256–60. doi: 10.1007/BF03262881
46. ur Rehman MM, Mahmood N, ur Rehman B. The relationship of caries with oral hygiene status and extra-oral risk factors. J Ayub Med Coll Abbottabad. (2008) 20(1):103–8. PMID: 190242001
47. Skinner J, Johnson G, Blinkhorn A, Byun R. Factors associated with dental caries experience and oral health status among New South Wales adolescents. Aust N Z J Public Health. (2014) 38(5):485–9. doi: 10.1111/1753-6405.12245
48. Neves ÉTB, Dutra LdC, Gomes MC, Paiva SM, de Abreu MHNG, Ferreira FM, et al. The impact of oral health literacy and family cohesion on dental caries in early adolescence. Community Dent Oral Epidemiol. (2020) 48(3):232–9. doi: 10.1111/cdoe.12520
49. Marinho VC, Higgins JP, Sheiham A, Logan S. Combinations of topical fluoride (toothpastes, mouthrinses, gels, varnishes) versus single topical fluoride for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. (2004) 2004(1):CD002781. doi: 10.1002/14651858.CD002781.pub2
50. Marinho VC, Higgins JP, Sheiham A, Logan S. Fluoride toothpastes for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. (2003) 2003(1):CD002278. doi: 10.1002/14651858.CD002278
51. Walsh T, Worthington HV, Glenny A, Marinho VC, Jeroncic A. Fluoride toothpastes of different concentrations for preventing dental caries. Cochrane Database Syst Rev. (2019) 3(3):CD007868. doi: 10.1002/14651858.CD007868.pub3
52. Marinho VC, Higgins JP, Sheiham A, Logan S. One topical fluoride (toothpastes, or mouthrinses, or gels, or varnishes) versus another for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. (2004) 2004(1):CD002780. doi: 10.1002/14651858.CD002780.pub2
53. Xiang B, Wong HM, Perfecto AP, McGrath CPJ. Modelling health belief predictors of oral health and dental anxiety among adolescents based on the health belief model: a cross-sectional study. BMC Public Health. (2020) 20(1):1755. doi: 10.1186/s12889-020-09784-1
54. Riccelli AE, Kelly LS. Prevention strategies for dental caries in the adolescent. Dent Clin North Am. (2006) 50(1):33–49. doi: 10.1016/j.cden.2005.09.004
55. Marinho VCC, Higgins JPT, Logan S, Sheiham A. Topical fluoride (toothpastes, mouthrinses, gels or varnishes) for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. (2003) 2003(4):CD002782. doi: 10.1002/14651858.CD002782
56. Marinho VC, Chong L-Y, Worthington HV, Walsh T. Fluoride mouthrinses for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. (2016) 7(7):CD002284. doi: 10.1002/14651858.CD002284.pub2
57. Marinho VCC, Worthington HV, Walsh T, Chong L-Y. Fluoride gels for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. (2015) 2015(6):CD002280. doi: 10.1002/14651858.CD002280.pub2
58. Marinho VCC, Worthington HV, Walsh T, Clarkson JE. Fluoride varnishes for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. (2013) 2013(7):CD002279. doi: 10.1002/14651858.CD002279.pub2
59. Kateeb E, Hamdan M, Fisher J. Oral health status and associated factors in a stratified cluster sample of marginalized Palestinian schools: a cross-sectional study. Oral Health Prev Dent. (2021) 19(1):373–81. doi: 10.3290/j.ohpd.b1694115
60. Methuen M, Kauppinen S, Suominen AL, Eloranta A-M, Väistö J, Lakka T, et al. Dental caries among finnish teenagers participating in physical activity and diet intervention: association with anthropometrics and behavioural factors. BMC Oral Health. (2021) 21(1):333. doi: 10.1186/s12903-021-01690-1
61. Thippeswamy HM, Kumar N, Acharya S, Pentapati KC. Relationship between body mass index and dental caries among adolescent children in South India. West Indian Med J. (2011) 60(5):581–6. doi: 10.1111/idj.12259
62. Laurence B, Farmer-Dixon CM, Southwell A, Marshall T, Shara N, Taylor G, et al. Sugar-sweetened beverage consumption and caries prevalence in underserved black adolescents. Pediatr Dent. (2021) 43(5):363–70. PMID: 34654498
63. Skinner J, Byun R, Blinkhorn A, Johnson G. Sugary drink consumption and dental caries in New South Wales teenagers. Aust Dent J. (2015) 60(2):169–75. doi: 10.1111/adj.12310
64. Goodwin M, Patel DK, Vyas A, Khan AJ, McGrady MG, Boothman N, et al. Sugar before bed: a simple dietary risk factor for caries experience. Community Dent Health. (2017) 34(1):8–13. doi: 10.1922/CDH_3926Goodwin06
65. Bruno-Ambrosius K, Swanholm G, Twetman S. Eating habits, smoking and toothbrushing in relation to dental caries: a 3-year study in Swedish female teenagers. Int J Paediatr Dent. (2005) 15(3):190–6. doi: 10.1111/j.1365-263X.2005.00621.x
66. Jung SH, Kim MH, Ryu JI. Inequalities in oral health among adolescents in Gangneung, South Korea. BMC Oral Health. (2018) 18(1):68. doi: 10.1186/s12903-018-0533-3
67. Hooley M, Skouteris H, Boganin C, Satur J, Kilpatrick N. Body mass index and dental caries in children and adolescents: a systematic review of literature published 2004–2011. Syst Rev. (2012) 1:57. doi: 10.1186/2046-4053-1-57
68. Neves ÉTB, Granville-Garcia AF, da Costa Dutra L, Bendo CB, de Morais Ferreira F, Paiva SM, et al. Association of oral health literacy and school factors with untreated dental caries among 12-year-olds: a multilevel approach. Caries Res. (2021) 55(2):144–52. doi: 10.1159/000514501
69. Neves ÉTB, de Lima LCM, da Costa Dutra L, Gomes MC, Siqueira MBLD, Paiva SM, et al. Oral health literacy, sociodemographic, family, and clinical predictors of dental visits among Brazilian early adolescents. Int J Paediatr Dent. (2021) 31(2):204–11. doi: 10.1111/ipd.12660
70. Fairchild RM, Broughton D, Morgan MZ. Knowledge of and attitudes to sports drinks of adolescents living in South Wales, UK. Br Dent J. (2017) 222(12):931–5. doi: 10.1038/sj.bdj.2017.542
71. Ahovuo-Saloranta A, Forss H, Walsh T, Nordblad A, Mäkelä M, Worthington HV. Pit and fissure sealants for preventing dental decay in permanent teeth. Cochrane Database Syst Rev. (2017) 7(7):CD001830. doi: 10.1002/14651858.CD001830.pub5
72. Kashbour W, Gupta P, Worthington HV, Boyers D. Pit and fissure sealants versus fluoride varnishes for preventing dental decay in the permanent teeth of children and adolescents. Cochrane Database Syst Rev. (2020) 11(11):CD003067. doi: 10.1002/14651858.CD003067.pub5
73. Griffen AL, Goepferd SJ. Preventive oral health care for the infant, child, and adolescent. Pediatr Clin North Am. (1991) 38(5):1209–26. doi: 10.1016/S0031-3955(16)38195-0
74. Ribeiro APD, Almeida RF, Medonca JGA, Leal SC. Oral health and its effect on the academic performance of children and adolescents. Pediatr Dent. (2018) 40(1):12–7. PMID: 29482676
75. Ortiz FR, Ardenghi TM, Maroneze MC, Paiva SM, Pordeus IA. Structuring adolescent’s oral health effects on labour market entry in a cohort study. Int J Paediatr Dent. (2021) 31(2):262–9. doi: 10.1111/ipd.12729
76. Akinkugbe AA, Moreno O, Brickhouse TH. Serum cotinine, vitamin D exposure levels and dental caries experience in U.S. adolescents. Community Dent Oral Epidemiol. (2019) 47(2):185–92. doi: 10.1111/cdoe.12442
77. Saari AJ, Kentala J, Mattila KJ. Flawed oral health of a non-smoking adolescent suggests smoking in adulthood. Eur J Public Health. (2015) 25(3):491–4. doi: 10.1093/eurpub/cku201
78. Stangvaltaite-Mouhat L, Furberg A-S, Drachev SN, Trovik TA. Common social determinants for overweight and obesity, and dental caries among adolescents in northern Norway: a cross-sectional study from the Tromsø study fit futures cohort. BMC Oral Health. (2021) 21(1):53. doi: 10.1186/s12903-021-01406-5
79. Mathur MR, Tsakos G, Millett C, Arora M, Watt R. Socioeconomic inequalities in dental caries and their determinants in adolescents in New Delhi, India. BMJ Open. (2014) 4(12):e006391. doi: 10.1136/bmjopen-2014-006391
80. Brondani B, Emmanuelli B, Alves LS, Soares CJ, Ardenghi TM. The effect of dental treatment on oral health-related quality of life in adolescents. Clin Oral Investig. (2018) 22(6):2291–7. doi: 10.1007/s00784-017-2328-3
81. Hall-Scullin E, Goldthorpe J, Milsom K, Tickle M. A qualitative study of the views of adolescents on their caries risk and prevention behaviours. BMC Oral Health. (2015) 15:141. doi: 10.1186/s12903-015-0128-1
82. Gholami M, Knoll N, Schwarzer R. A brief self-regulatory intervention increases dental flossing in adolescent girls. Int J Behav Med. (2015) 22(5):645–51. doi: 10.1007/s12529-014-9459-6
83. Rachmawati YL, Maharani DA, Oho T. Cross-cultural adaptation and psychometric properties of the Indonesia version of the self-efficacy oral health questionnaire for adolescents. Int J Paediatr Dent. (2019) 29(3):345–51. doi: 10.1111/ipd.12472
84. Shirzaee N, Saied-Moallemi Z, Mohammadi M, Okati-Aliabad H. Toothbrushing and related factors among high school students in the southeast of Iran: a cross-sectional study. Int J Dent Hyg. (2021) 19(4):360–5. doi: 10.1111/idh.12534
85. Baxevanos K, Menexes G, Lazaridou A, Coolidge T, Topitsoglou V, Kalfas S. Dental caries and psychosocial factors: testing a conceptual model in adolescents. Community Dent Oral Epidemiol. (2021) 49(4):314–21. doi: 10.1111/cdoe.12653
86. Acharya S, Pentapati KC, Singh S. Influence of socioeconomic status on the relationship between locus of control and oral health. Oral Health Prev Dent. (2011) 9(1):9–16. https://api.semanticscholar.org/CorpusID:755827421594202
87. Anaise JZ, Mann J. Prevalence of dental caries and demands for services among Israeli kibbutz youth. Community Dent Oral Epidemiol. (1982) 10(3):161–2. doi: 10.1111/j.1600-0528.1982.tb01343.x
88. Nermo H, Willumsen T, Johnsen JK. Changes in dental anxiety among 15- to 21-year-olds. A 2-year longitudinal analysis based on the Tromsø study: fit futures. Community Dent Oral Epidemiol,. (2019) 47(2):127–33. doi: 10.1111/cdoe.12434
89. Kruger E, Murray Thomson W, Poulton R, Davies S, Harvey Brown R, Silva PA. Dental caries and changes in dental anxiety in late adolescence. Community Dent Oral Epidemiol. (1998) 26(5):355–9. doi: 10.1111/j.1600-0528.1998.tb01973.x
90. Thomson WM, Broadbent JM, Locker D, Poulton R. Trajectories of dental anxiety in a birth cohort. Community Dent Oral Epidemiol. (2009) 37(3):209–19. doi: 10.1111/j.1600-0528.2009.00473.x
91. Shin BM, Park DY. Association between the prevalence of dental caries in children and factors related to their mothers. Int J Dent Hyg. (2017) 15(4):e173–9. doi: 10.1111/idh.12261
92. Eid SA, Khattab NMA, Elheeny AAH. Untreated dental caries prevalence and impact on the quality of life among 11–14-year-old Egyptian schoolchildren: a cross-sectional study. BMC Oral Health. (2020) 20(1):83. doi: 10.1186/s12903-020-01077-8
93. Shin B-M, Jung S-H, Kim M-H, Ryu J-I. Did the extended coverage policy contribute to alleviating socioeconomic inequality in untreated dental caries of both children and adolescents in South Korea? BMC Oral Health. (2020) 20(1):124. doi: 10.1186/s12903-020-01112-8
94. de Sousa FS, Lopes BC, Costa EM, Alves CMC, de Sousa Queiroz RC, Tonello AS, et al. Do social inequalities persist in the distribution of dental caries in adolescents from Maranhão? Contributions of a population-based study. Cien Saude Colet. (2021) 26(7):2625–34. doi: 10.1590/1413-81232021267.08562021
95. Stona P, Kramer PF, Vargas-Ferreira F, de Amorim LM, Coelho EMdRB, Feldens CA. Socioeconomic and intraoral polarization of untreated caries and tooth loss among male adolescents. Braz Oral Res. (2021) 35:e031. doi: 10.1590/1807-3107bor-2021.vol35.0031
96. Javier JR, Huffman LC, Mendoza FS. Filipino child health in the United States: do health and health care disparities exist? Prev Chronic Dis. (2007) 4(2):A36. PMID: 17362627 PMCID: PMC1893134
97. Zhang Q, van Palenstein Helderman W, Yee R, Bian Z, Fan M, Holmgren C. Situational analysis of dental caries and existing oral health care of children and adolescents in Hubei province, people’s republic of China: implications for change. Oral Health Prev Dent. (2008) 6(1):13–21. PMID: 18399303
98. Vettore MV, Ahmad SFH, Machuca C, Fontanini H. Socio-economic status, social support, social network, dental status, and oral health reported outcomes in adolescents. Eur J Oral Sci. (2019) 127(2):139–46. doi: 10.1111/eos.12605
99. Tudoroniu C, Popa M, Iacob SM, Pop AL, Năsui BA. Correlation of caries prevalence, oral health behavior and sweets nutritional habits among 10–19-year-old cluj-napoca Romanian adolescents. Int J Environ Res Public Health. (2020) 17(18):6923. doi: 10.3390/ijerph17186923
100. Mattos MG, Fernandez CA, Masterson D, Maia LC, de Almeida Neves A. Is the caregivers’ oral health related to dental caries in children or adolescents? A systematic review. Clin Oral Investig. (2019) 23(10):3843–54. doi: 10.1007/s00784-019-02814-2
101. Lage CF, Fulgencio LB, Corrêa-Faria P, Serra-Negra JM, Paiva SM, Pordeus IA. Association between dental caries experience and sense of coherence among adolescents and mothers. Int J Paediatr Dent. (2017) 27(5):412–9. doi: 10.1111/ipd.12275
102. Freire M, Hardy R, Sheiham A. Mothers’ sense of coherence and their adolescent children’s oral health status and behaviours. Community Dent Health. (2002) 19(1):24–31. PMID: 11922408
103. Nicolau B, Marcenes W, Allison P, Sheiham A. The life course approach: explaining the association between height and dental caries in Brazilian adolescents. Community Dent Oral Epidemiol. (2005) 33(2):93–8. doi: 10.1111/j.1600-0528.2005.00213.x
104. Veerasamy A, Kirk R, Gage J. Epidemiology of dental caries among adolescents in Tamil Nadu, India. Int Dent J. (2016) 66(3):169–77. doi: 10.1111/idj.12216
105. Kramer A-CA, Hakeberg M, Petzold M, Östberg A-L. Demographic factors and dental health of Swedish children and adolescents. Acta Odontol Scand. (2016) 74(3):178–85. doi: 10.3109/00016357.2015.1063160
106. Whelton H, Crowley E, O'Mullane D, Donaldson M, Kelleher V, Cronin M. Dental caries and enamel fluorosis among the fluoridated and non-fluoridated populations in the Republic of Ireland in 2002. Community Dent Health. (2004) 21(1):37–44. PMID: 15074871
107. Broffitt B, Levy SM, Warren J, Cavanaugh JE. Factors associated with surface-level caries incidence in children aged 9–13: the Iowa fluoride study. J Public Health Dent. (2013) 73(4):304–10. doi: 10.1111/jphd.12028
108. Slade GD, Grider WB, Maas WR, Sanders AE. Water fluoridation and dental caries in U.S. children and adolescents. J Dent Res. (2018) 97(10):1122–8. doi: 10.1177/0022034518774331
109. Iheozor-Ejiofor Z, Worthington HV, Walsh T, O'Malley L, Clarkson JE, Macey R, et al. Water fluoridation for the prevention of dental caries. Cochrane Database Syst Rev. (2015) 2015(6):CD010856. doi: 10.1002/14651858.CD010856.pub2
110. Morgan MV, Campain AC, Adams GG, Crowley SJ, Wright FA. The efficacy and effectiveness of a primary preventive dental programme in non-fluoridated areas of Victoria, Australia. Community Dent Health. (1998) 15(4):263–71. PMID: 9973728
111. Leatherman GH. Oral hygiene for children: a look at what we must have and what we should do. Int Dent J. (1982) 32(3):252–8. PMID: 6958653
112. von Philipsborn P, Stratil JM, Burns J, Busert LK, Pfadenhauer LM, Polus S, et al. Environmental interventions to reduce the consumption of sugar-sweetened beverages and their effects on health. Cochrane Database Syst Rev. (2019) 6(6):CD012292. doi: 10.1002/14651858.CD012292.pub2
113. Nylander A, Kumlin I, Martinsson M, Twetman S. Effect of a school-based preventive program with salivary lactobacillus counts as sugar-motivating tool on caries increment in adolescents. Acta Odontol Scand. (2001) 59(2):88–92. doi: 10.1080/000163501750157216
114. Yang Q, Xi Y, Liu H, Luo J, Ouyang Y, Sun M, et al. Free sugars intake among Chinese adolescents and its association with dental caries: a cross-sectional study. Nutrients. (2021) 13(3):765. doi: 10.3390/nu13030765
115. Nguyen VTN, Zaitsu T, Oshiro A, Tran TT, Nguyen YHT, Kawaguchi Y, et al. Impact of school-based oral health education on Vietnamese adolescents: a 6-month study. Int J Environ Res Public Health. (2021) 18(5):2715. doi: 10.3390/ijerph18052715
116. Arora A, Kumbargere Nagraj S, Khattri S, Ismail NM, Eachempati P. School dental screening programmes for oral health. Cochrane Database Syst Rev. (2019) 7(7):CD012595. doi: 10.1002/14651858.CD012595.pub4
117. Wharton B, Wharton P. Nutrition in adolescence. Nutr Health. (1987) 4(4):195–203. doi: 10.1177/026010608700400403
118. Sterman J. Business Dynamics: Systems Thinking and Modeling for a Complex World. 1st ed. Boston: McGraw-Hill/Irwin (2000). p. 982.
120. Richardson GP. Feedback Thought in Social Science and Systems Theory. Waltham, MA: Pegasus Communications (1999).
121. Honkala S, Honkala E, Al-Sahli N. Do life- or school-satisfaction and self-esteem indicators explain the oral hygiene habits of schoolchildren? Community Dent Oral Epidemiol. (2007) 35(5):337–47. doi: 10.1111/j.1600-0528.2006.00326.x
122. Pazos CTC, Austregésilo SC, Goes PSAd. Autoestima e comportamentos de saúde bucal em adolescentes. J Ciência & Saúde Coletiva. (2019) 24:4083–92. doi: 10.1590/1413-812320182411.02492018
123. Dumitrescu AL, Dogaru BC, Dogaru CD. Self-control and self-confidence: their relationship to self-rated oral health status and behaviours. Oral Health Prev Dent. (2009) 7(2):155–62. PMID: 19583041
124. Kaur P, Singh S, Mathur A, Makkar DK, Aggarwal VP, Batra M, et al. Impact of dental disorders and its influence on self esteem levels among adolescents. J Clin Diagnostic Res. (2017) 11(4):ZC05. doi: 10.7860/JCDR/2017/23362.9515
125. Prasertsom P, Kaewkamnerdpong I, Krisdapong S. Condition-specific oral health impacts in Thai children and adolescents: findings from the national oral health-related quality of life survey. Asia Pac J Public Health. (2020) 32(1):49–56. doi: 10.1177/1010539519899774
126. Peres KG, Barros AJD, Anselmi L, Peres MA, Barros FC. Does malocclusion influence the adolescent’s satisfaction with appearance? A cross-sectional study nested in a Brazilian birth cohort. Community Dent Oral Epidemiol. (2008) 36(2):137–43. doi: 10.1111/j.1600-0528.2007.00382.x
127. Sharma A, Mathur A, Batra M, Makkar DK, Aggarwal VP, Goyal N, et al. Objective and subjective evaluation of adolescent’s orthodontic treatment needs and their impact on self-esteem. Rev Paul Pediatr. (2017) 35(1):86–91. doi: 10.1590/1984-0462/;2017;35;1;00003
128. Yu M, Jiang Q-Z, Sun Z-Y, Kong Y-Y, Chen Z. Association between single nucleotide polymorphisms in vitamin D receptor gene polymorphisms and permanent tooth caries susceptibility to permanent tooth caries in Chinese adolescent. Biomed Res Int. (2017) 2017:4096316. doi: 10.1155/2017/4096316
129. Marshall TA, Curtis AM, Cavanaugh JE, Warren JJ, Levy SM. Beverage intakes and toothbrushing during childhood are associated with caries at age 17 years. J Acad Nutr Diet. (2021) 121(2):253–60. doi: 10.1016/j.jand.2020.08.087
130. Gil EG, Åstrøm AN, Lie SA, Rygg M, Fischer J, Rosén A, et al. Dental caries in children and adolescents with juvenile idiopathic arthritis and controls: a multilevel analysis. BMC Oral Health. (2021) 21(1):417. doi: 10.1186/s12903-021-01758-y
131. Roque TV, Magnani IQ, Paiva SM, Abreu LG. Impact of oral conditions on the quality of life of adolescents in a rural area of Brazil. Acta Odontol Latinoam. (2021) 34(1):81–7. doi: 10.54589/aol.34/1/081
132. Harris R, Gamboa A, Dailey Y, Ashcroft A. One-to-one dietary interventions undertaken in a dental setting to change dietary behaviour. Cochrane Database Syst Rev. (2012) 2012(3):CD006540. doi: 10.1002/14651858.CD006540.pub2
133. Kaur M, Himadi E, Chi DL. Prevalence of xerostomia in an adolescent inpatient psychiatric clinic: a preliminary study. Spec Care Dentist. (2016) 36(2):60–5. doi: 10.1111/scd.12154
134. Campain AC, Morgan MV, Evans RW, Ugoni A, Adams GG, Conn JA, et al. Sugar-starch combinations in food and the relationship to dental caries in low-risk adolescents. Eur J Oral Sci. (2003) 111(4):316–25. doi: 10.1034/j.1600-0722.2003.00056.x
135. Gupta T, Sequeira P, Acharya S. Oral health knowledge, attitude and practices of a 15-year-old adolescent population in Southern India and their social determinants. Oral Health Prev Dent. (2012) 10(4):345–54. PMID: 23301235
136. Baiju RMP, Peter E, Varghese NO, Varughese JM, Sivaram R, Narayan V. Development and initial validation of an oral health-related quality of life scale for older adolescents. Indian J Dent Res. (2019) 30(6):826–33. PMID: 31939355
137. Maharani DA, Adiatman M, Rahardjo A, Burnside G, Pine C. An assessment of the impacts of child oral health in Indonesia and associations with self-esteem, school performance and perceived employability. BMC Oral Health. (2017) 17(1):65. doi: 10.1186/s12903-017-0358-5
138. Källestål C, Dahlgren L, Stenlund H. Oral health behaviour and self-esteem in Swedish children. Soc Sci Med. (2000) 51(12):1841–9. doi: 10.1016/S0277-9536(00)00115-5
139. Deery C, et al. The dental caries status of Scottish adolescents reported to be regular attenders. Initial results from a primary dental care based research network. Br Dent J. (1999) 187(2):95–100.10464989
140. Fee PA, Riley P, Worthington HV, Clarkson JE, Boyers D, Beirne PV. Recall intervals for oral health in primary care patients. Cochrane Database Syst Rev. (2020) 10(10):CD004346. doi: 10.1002/14651858.CD004346.pub5
141. Bastos RS, Carvalho ÉS, Xavier A, Caldana ML, Bastos JRM, Lauris JRP. Dental caries related to quality of life in two Brazilian adolescent groups: a cross-sectional randomised study. Int Dent J. (2012) 62(3):137–43. doi: 10.1111/j.1875-595X.2011.00105.x
142. Hall-Scullin EP, Whitehead H, Rushton H, Milsom K, Tickle M. A longitudinal study of the relationship between dental caries and obesity in late childhood and adolescence. J Public Health Dent. (2018) 78(2):100–8. doi: 10.1111/jphd.12244
143. Litt MD, Reisine S, Tinanoff N. Multidimensional causal model of dental caries development in low-income preschool children. Public Health Rep. (1995) 110(5):607–17. PMID: 7480616 PMCID: PMC1381639
144. McCaul KD, Glasgow RE, Gustafson C. Predicting levels of preventive dental behaviors. J Am Dent Assoc. (1985) 111(4):601–5. doi: 10.14219/jada.archive.1985.0169
145. Kristjánsson AL, Sigfúsdóttir ID, Allegrante JP. Health behavior and academic achievement among adolescents: the relative contribution of dietary habits, physical activity, body mass index, and self-esteem. Health Educ Behav. (2010) 37(1):51–64. doi: 10.1177/1090198107313481
146. Kiran-Esen B. Analyzing peer pressure and self-efficacy expectations among adolescents. Soc Behav Pers. (2012) 40. doi: 10.2224/sbp.2012.40.8.1301
147. Golestan S, Abdullah H. Self-efficacy as a moderator in the relationship between peer pressure and family smoking, and adolescent cigarette smoking behavior. Asian Soc Sci. (2015) 11:84. doi: 10.5539/ass.v11n28p84
148. Gilchrist F, Marshman Z, Deery C, Rodd HD. The impact of dental caries on children and young people: what they have to say? Int J Paediatr Dent. (2015) 25(5):327–38. doi: 10.1111/ipd.12186
149. Berggren U, Meynert G. Dental fear and avoidance: causes, symptoms, and consequences. J Am Dent Assoc. (1984) 109(2):247–51. doi: 10.14219/jada.archive.1984.0328
150. De Jongh A, Schutjes M, Aartman IH. A test of Berggren’s model of dental fear and anxiety. Eur J Oral Sci. (2011) 119(5):361–5. doi: 10.1111/j.1600-0722.2011.00843.x
151. Fisher-Owens SA, Isong IA, Soobader MJ, Gansky SA, Weintraub JA, Platt LJ, et al. An examination of racial/ethnic disparities in children’s oral health in the United States. J Public Health Dent. (2013) 73(2):166–74. doi: 10.1111/j.1752-7325.2012.00367.x
152. Northridge ME, Kumar A, Kaur R. Disparities in access to oral health care. Annu Rev Public Health. (2020) 41:513–35. doi: 10.1146/annurev-publhealth-040119-094318
153. Ortiz AS, Tomazoni F, Knorst JK, Ardenghi TM. Influence of socioeconomic inequalities on levels of dental caries in adolescents: a cohort study. Int J Paediatr Dent. (2020) 30(1):42–9. doi: 10.1111/ipd.12572
154. Campagnaro R, de Oliveira Collet G, de Andrade MP, da Silva Lopes Salles JP, de Lourdes Calvo Fracasso M, Scheffel DLS, et al. COVID-19 pandemic and pediatric dentistry: fear, eating habits and parent’s oral health perceptions. Child Youth Serv Rev. (2020) 118:105469. doi: 10.1016/j.childyouth.2020.105469
155. Edelstein BL, Rubin MS, Clouston SAP, Reusch C. Children’s dental service use reflects their parents’ dental service experience and insurance. J Am Dent Assoc. (2020) 151(12):935–43. doi: 10.1016/j.adaj.2020.08.018
156. Arredondo EM, Elder JP, Ayala GX, Campbell N, Baquero B, Duerksen S. Is parenting style related to children’s healthy eating and physical activity in latino families? Health Educ Res. (2006) 21(6):862–71. doi: 10.1093/her/cyl110
157. Park H, Walton-Moss B. Parenting style, parenting stress, and children’s health-related behaviors. J Dev Behav Pediatr. (2012) 33(6):495–503. doi: 10.1097/DBP.0b013e318258bdb8
158. Fisher-Owens SA, Gansky SA, Platt LJ, Weintraub JA, Soobader M-J, Bramlett MD, et al. Influences on children’s oral health: a conceptual model. Pediatrics. (2007) 120(3):e510–20. doi: 10.1542/peds.2006-3084
Keywords: dental caries, adolescents, systems science, system dynamics, causal loop diagram
Citation: Sadjadpour F, Hosseinichimeh N, Pahel BT and Metcalf SS (2024) Systems mapping of multilevel factors contributing to dental caries in adolescents. Front. Oral. Health 4:1285347. doi: 10.3389/froh.2023.1285347
Received: 1 September 2023; Accepted: 30 December 2023;
Published: 31 January 2024.
Edited by:
Morenike Oluwatoyin Folayan, Nigerian Institute of Medical Research (NIMR), NigeriaReviewed by:
Anna-Lena Östberg, University of Gothenburg, SwedenMaria Cristina Cangussu, Federal University of Bahia (UFBA), Brazil
© 2024 Sadjadpour, Hosseinichimeh, Pahel and Metcalf. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fatima Sadjadpour ZnNhZGphZHBvdXJAdnQuZWR1
 Fatima Sadjadpour
Fatima Sadjadpour Niyousha Hosseinichimeh
Niyousha Hosseinichimeh Bhavna T. Pahel
Bhavna T. Pahel Sara S. Metcalf
Sara S. Metcalf