- Faculty of Dentistry, The University of Hong Kong, Hong Kong SAR, China
This concise review provides an update of the use of dental sealants. Dental sealants protect a tooth from caries development by providing a physical barrier to microorganism colonisation and creating a favorable environment for patients to clean. Some sealants release fluoride ions to promote remineralization. Dental sealants can be applied on pits and fissures of primary and permanent teeth to prevent and arrest early enamel caries. They are effective in caries prevention. The preventive fraction of resin sealant is up to 61% after 5 years. Dental sealants can be classified as resin, glass ionomer and hybrid (compomer or giomer) according to the material. Recent studies from 2012 to 2022 showed resin sealant has a high retention rate of up to 80% after 2 years, whereas glass ionomer sealants is 44%. Chemical etching with 37% phosphoric acid is the standard of care, whereas laser or air-abrasion cannot does not increase the sealant retention rate. Moist control is critical and studies found the use of rubber dam and cotton rolls had similar success for sealant retention. The longevity of dental sealant is also associated with clinical operative factors, including approaches of moisture control, enamel pretreatment, selection of dental adhesive, and time of acid etching.
1. Introduction
For Dental caries, commonly known as tooth decay, is a highly prevalent oral disease around the world. More than 2.4 billion people are suffering from permanent teeth caries while 520 million children are affected by primary teeth caries (1). Untreated dental caries gradually extends and irritate the dental pulp, leading to the destruction of the tooth structure, excruciating pain, and eventually tooth extraction (2). Dental caries degrades the quality of life of the patients (3). It can also lead to lower self-esteem (4) and depression (5). Pits and fissure areas in the tooth surface are highly susceptible to dental caries. Dental caries was the demineralization of dental hard tissue caused by acid produced by the fermentation of carbohydrates by cariogenic bacteria in the dental plaque biofilm (6). Because of the anatomical structure, the dental plaque biofilm in the fissure is difficult, if not impossible, to remove through daily oral hygiene practice. The caries risk is higher in teeth with deep fissures (7, 8). An observational study found caries were located in the occlusal fissure areas in 79% of the decayed molars (9).
Because of the susceptibility of pit and fissure areas to dental caries, oral care providers have been trying to eliminate fissures to control caries. The initial approach to eliminate fissures was invasive. Hyatt suggested prophylactic odontotomy in 1923, which was an invasive dental procedure to remove deep fissures with a dental bur and place a filling to prevent caries (10). Three decades later in 1955, Buonocore proposed a fissure sealing procedure with the 85% phosphoric acid etching of enamel followed by a resin material coverage on the fissure area (11). This technique was a foundation for the further development of fissure sealing using different dental materials. Cueto suggested using methyl cyanoacrylate to seal pits and fissures in 1965 (12). Later, Buonocore successfully applied light-cure dental sealant incorporated with Bisphenol A-glycidyl methacrylate (Bis-GMA) in 1970 (13). In the following year, the Council on Dental Materials Devices and Council on Dental Therapeutics of the American Dental Association recognized the use of dental sealant (14). The first glass ionomer sealant appeared in the mid-1970s (15).
As a common preventive strategy for dental caries, the understanding and the application of dental sealant has been shifting in accordance with the contemporary paradigm of caries management, which placed prevention as a priority (16). The clinical application of dental sealant has been broadening when compared to the past. Dental sealant was majorly used in the pits and fissure area of the occlusal surface in the posterior area in the past. It is now a common preventive measure to manage dental caries in the occlusal or approximal surfaces of the anterior or posterior teeth in primary or permanent dentition. It can also be used on exposed root surfaces to prevent root caries. In addition, with the development of dental material sciences, more materials are available as dental sealants. Therefore, the objective of this review is to overview and update the knowledge of dental sealants in the aspect of their classification, the mechanism in caries prevention, clinical indications, effectiveness in caries control, clinical longevity and factors affecting the clinical outcomes in the 2012–2022.
2. Literature search
Keywords ((fissure sealant) OR (dental sealant)) AND (dental caries) are used to search for articles in the PubMed and Scopus databases. Articles published from 2012 to 2022 were selected. After duplicate removal, 886 articles were identified. The titles and abstracts of the identified article were screened. Finally, we included 175 articles on dental sealants and caries for this review. Among the included articles, 27 articles were randomized clinical trials comparing caries prevention and/or retention rate of dental sealant.
3. Classification of dental sealant by material
Dental sealants can be broadly classified into three categories based on the components—resin sealant, glass ionomer sealant and hybrid sealant.
3.1. Resin sealant
Resin sealant contains an organic resin-based oligomer matrix (17). Bis-GMA is the most common monomer for the matrix of resin sealant. Other resin monomers such as Urethane-dimethacrylate (UDMA) and Triethylene glycol dimethacrylate (TEGDMA) are in alternative use (18). Resin sealant may also contain filler, fluoride particles or photoinitiations.
3.1.1. Auto-cure resin sealant or light-cure resin sealant
Based on the ways of polymerization, resin sealant could be further classified as self-cure or light-cured resin sealant. Resin sealant sets after undergoing polymerisation of monomers. The polymerisation occurs in two ways, auto-polymerisation or polymerisation under an external light source. The setting of self-cured resin sealant is an auto-polymerisation reaction initiated by chemical reactions. The chemical reactions of auto-polymerisation process are initiated by the free radicals produced by chemical reactions of tertiary amine and benzoyl peroxide (19). No external light source is required. Light-cured resin sealant requires an external light source to imitate the polymerisation. Photo-initiators in the resin sealant absorb light radiation, dissociating into free radicals, and start the polymerisation process (20). The external light source could be ultraviolet or visible light. However, UV can cause health hazards (21) and is seldom used for resin sealant now (22). Visible light is commonly used for the polymerization of resin sealant (23).
3.1.2. Fluoride-releasing resin sealant or non-fluoride releasing resin sealant
Resin sealant can also be classified by its fluoride-releasing ability. Fluoride particles such as sodium fluoride or fluoride-releasing glass filler, are incorporated into the material in fluoride-releasing resin sealant (24). It provides an additional way to achieve caries prevention.
3.1.3. Filled resin sealant or unfilled resin sealant
Based on the filler content, we can also classify the resin sealant as filled or unfilled resin sealant. The wear resistance of filled resin sealant is higher than unfilled resin sealant (25). However, the viscosity of sealant also increases with the filler added, therefore leading to a lower ability to penetrate fissures and pits (26).
3.1.4. Hydrophobic resin sealant or hydrophilic resin sealant
Based on the sensitivity to moisture, resin sealant can be classified as hydrophobic or hydrophilic resin sealant. Conventional resin sealant is hydrophobic. Recently, a new generation of hydrophilic resin sealant has been developed by adding multifunctional acrylate monomers with a formulation considering the hydrophilic-hydrophobic balance (27). Hydrophilic resin sealant is believed to be able to overcome the moisture challenge during the operative process of sealant application.
3.2. Glass ionomer sealant
Two types of glass ionomer sealants are available, conventional glass ionomer sealant and resin-modified glass ionomer sealant. Conventional glass ionomer sealant is comprised of powders of fluoroaluminosilicate glass and liquids containing polyacrylic acid, tartaric acid and water (28). It sets with the acid-base reactions of powder and liquid when mixed (29). Resin-modified glass ionomer sealant is made by introducing resin-based monomers such as 2-hydroxyethylmethacrylate (HEMA) or UDMA into the conventional glass ionomer (30). The physical properties of resin-modified glass ionomer sealant are improved compared to conventional glass ionomer sealant (31). The resin-modified glass ionomer sealant set with the polymerisation of resin-based monomers followed by acid-base reactions of powder and liquid (32).
3.3. Hybrid sealant
Hybrid Sealants include compomer sealant and giomer sealant (33). Compomer is also known as polyacid-modified composite resin. It contains non-reactive inorganic filler particles, reactive silicate glass particles, a polyacid-modified monomer and a photo-initiator (31). Giomer is comprised of pre-reacted glass ionomer (PRG) filler and resin-based monomer matrix (34). Hybrid Sealants are relatively new and not widely used.
Dental sealants can also be classified with colors. Clear, white, and pink are three colors that can be commonly seen for dental sealant. Clear dental sealant allows dentists to see through so that the lesion underneath could be better monitored (35). However, clear sealant itself is more difficult to see, hence potentially leading to a bias repair decision (35).
4. Mechanisms of dental sealant in preventing and arresting caries
Placing dental sealant is an effective approach to preventing and arresting caries. Possible mechanisms include the physical barrier created by the sealant, ease of cleaning for the patient, and release of ions that favours remineralisation of the tooth.
4.1. Physical barrier
Dental sealant covers the fissures and provides a physical barrier. The cariogenic bacteria are difficult to enter and colonize in the fissure area with the physical barrier. This barrier also prevents food debris from getting into fissures which blocks the nutrition intake and inhibits the growth of dental biofilm (22).
4.2. Ease of cleaning
Dental sealant can improve the oral hygiene of patients. Fissures can be deep and narrow. It is difficult or impossible for toothbrush bristles to get into the fissures and clean the area (36). Applying dental sealant can seal the fissures. This turns a plaque retentive occlusal surface into a smoother surface which makes the surface easier to clean (37).
4.3. Ion release
Different types of dental sealants can release ions which can prevent and arrest caries. Glass ionomer sealants, hybrid sealants and some resin sealants are fluoride-releasing. Fluoride ion reduces demineralization, promotes remineralization (38) and inhibits the growth of cariogenic bacteria (39). Fluoride-releasing sealant can prevent and stop the progression of caries of the sealed tooth (40). It can also offer protection to the adjacent tooth (41). Some giomer sealants release antimicrobial borate and strontium that inhibit bacterial growth (42). Borate and strontium ions, together with sodium ions released by giomer, could be a buffer to lactic acid (43).
5. Effects of dental sealant in preventing and arresting caries in the past 10 years
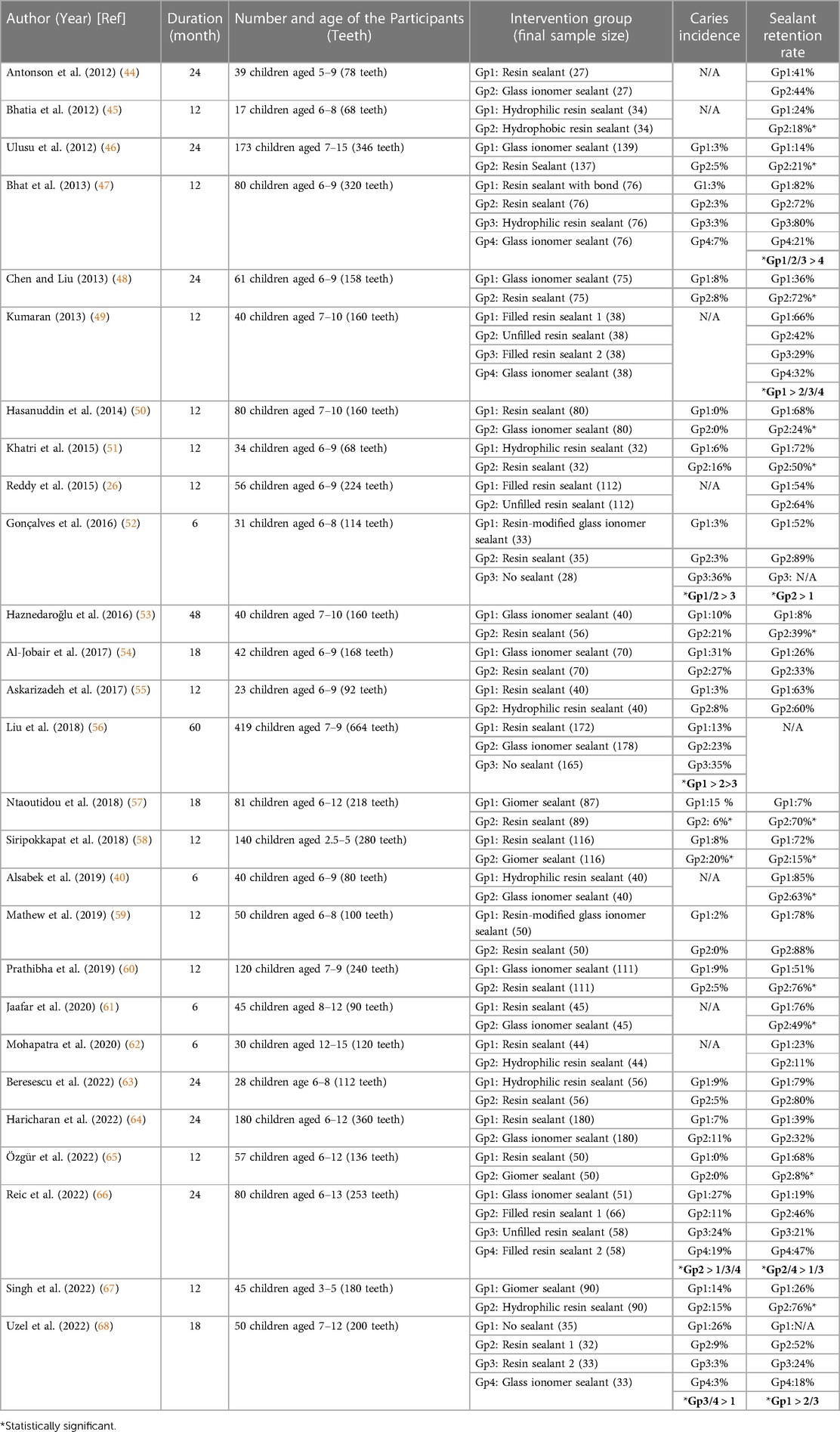
Studies published in the recent ten years (2012–2022) support dental sealant as an effective means of preventing and arresting caries (Table 1). Because of the heterogeneity of the included studies, we did not perform a meta-analysis in this review. Table 1 shows the caries incidence of different dental sealants. With the results of the studies that have blank control groups, we summarize the preventive fractions are 92% for both resin sealant and glass ionomer sealant at a 6-month follow-up (52); 64% - 88% for resin sealant, and 88% for glass ionomer sealant at an 18-month follow-up (68); 61% for resin sealant and 35% for glass ionomer at a 60-month follow-up (56). Results of hybrid sealant were limited in the literature.
6. Longevity of dental sealant
The caries preventive effect of dental sealant largely relies on the retention of the sealant. Table 1 shows the retention rates of dental sealants published in the past ten years (2012–2022). For resin sealant, the retention rate ranges from 11% to 89% at a 6-month follow-up (40, 52, 61, 62); from 18 to 88% at a 12-month follow-up (26, 45, 47, 49–51, 55, 58–60, 65, 67); from 24% to 70% at an 18-month follow-up (54, 57, 68); from 21% to 80% at a 24-month follow-up (44, 46, 48, 63, 64, 66). Studies with longer follow-up periods were limited. For glass ionomer sealant, the retention rate ranges from 49% to 63% at a 6-month follow-up (40, 52, 61); from 21% to 78% at a 12-month follow-up (47, 49, 50, 59, 60); and from 14 to 44% at a 24-month follow-up (44, 46, 48, 64, 66). Studies in other follow-up periods were limited. For hybrid sealant, the retention rates range from 8% to 26% at a 12-month follow-up (58, 65, 67). Studies with longer follow-up periods were limited.
7. Indications for dental sealant placement based on the evidence
7.1. Caries risk of the patient
Dental sealant is indicated for patients with high caries risk. The effectiveness of dental sealant was proved to be higher in high caries risk patients when compared with low caries risk patients (37, 69). The benefits of dental sealant exceed the cost when children with high caries risk were targeted (70). The cost-effectiveness of dental sealants is higher in patients with high caries risk can be concluded.
7.2. Types of the dentitions
Dental sealant is suggested for permanent teeth. A systematic review found that resin sealants placed on occlusal surfaces of permanent molars could reduce caries for up to 4 years when compared to no treatment (22). Another systematic review and meta-analysis also found that resin sealant reduced caries incidence in permanent teeth at a follow-up period of up to 4 years (71). Dental sealant is suggested for primary teeth. A randomized clinical trial shows that resin sealant can arrest dentinal caries in primary teeth (72). A systematic review concluded dental sealant had caries preventive effects in primary teeth when compared to no treatment with low-certainty evidence (36). In addition, it is a cost-effective approach to applying dental sealant in primary dentition (69).
7.3. Caries status of the tooth
Dental sealant is effective in preventing caries on sound tooth surfaces. Studies supported the application of dental sealant in preventing caries on sound tooth surfaces (22, 71). A 3-year randomized clinical trial reported that non-sealed molars exhibited a caries incidence of 98.9% while it was only 25.7% for the sealed molars (73). A systematic review showed that the caries risk of sound teeth sealed with resin sealant occlusally is 76% less within 24 to 48 months follow up, and 85% less in 84 months follow up compared to no treatment (74). Dental sealant is effective in arresting non-cavitated caries (40, 61). A systematic review showed that the chance of arresting or reversing non-cavitated occlusal caries with dental sealants is 2–3 times higher when compared with no treatment (75). A clinical study over 44 months suggests that caries without frank cavitation can be arrested with dental sealant (35). Dental sealant was also shown to arrest non-cavitated dentinal occlusal caries 36 months after placement (76). In addition, dental sealants placed on sound surfaces and carious surfaces showed similar survival rates (77). Therefore, dental sealant is effective in arresting non-cavitated caries.
The effectiveness of dental sealant in arresting cavitated caries is controversial. A clinical study showed that caries progression was rarely detected for initial caries (ICDAS 2) to moderate caries (ICDAS 4) sealed with resin dental sealant at the 24-month follow-up (78). Dental sealant was found to be effective in arresting ICDAS 3 micro-cavitated caries in permanent molars after a 2-year follow-up (79). However, another study found that dental sealant could arrest non-cavitated caries but not micro-cavitated caries (ICDAS 3) (80).
7.4. Types of tooth surfaces
A dental sealant can be applied on occlusal fissure surfaces. The effectiveness of dental sealant in preventing dental caries in occlusal surfaces has been approved in a number of studies (22). Dental sealant could also be applied on axial smooth surfaces. The application of dental sealant in sound or carious smooth surfaces is also supported by recent studies. A 3.5-year study on children found out dental sealant applied on sound mesial smooth surfaces of first permanent molars can prevent distal caries on primary second molars (81). Dental sealants can also arrest non-cavitated and micro-cavitated caries on proximal surfaces (82, 83).
7.5. Eruption status of the tooth
Dental sealant can be applied on fully erupted or partially erupted molars. However, the retention rate of the sealant in the partially erupted molars is lower due to saliva contamination and the difficulty in moisture control (44). A randomized 24-month clinical trial revealed that the retention of dental sealants is significantly related to the occlusal eruption stage (84). In this study, researchers found that the retention rate of dental sealants placed on partially erupted teeth was lower than on fully erupted teeth. If a partially erupted molar is to be sealed, glass ionomer sealant is a better choice than resin sealant.
7.6. Presence of dental fluorosis
Dental sealant can be applied on teeth with dental fluorosis. The choice of sealant material is the key to success. A study found out the total retention of resin sealant (68%) is much higher than glass ionomer sealant (24%) on fluorotic permanent molars of 7- to 10-year-old children after one year (50).
8. Operative factors affecting the longevity of dental sealant
The longevity of the dental sealant is affected by several operative factors when applying dental sealant, including moisture control of the operative field, tooth surface preparation, and the application of dental adhesives. These factors should be taken into consideration when applying sealants to enhance the retention and extend the longevity of the sealants.
8.1. Moisture control
Moisture control should be achieved when placing dental sealants with no difference for rubber dams, cotton rolls or dental isolation systems. Studies found out the dental sealant placed on saliva-contaminated tooth surfaces would significantly increase the microleakage and reduce shear bond strength (85–88). These provide us with evidence that moisture control is critical when placing dental sealant. There is no difference in the retention rate of dental sealant when using rubber dams, cotton rolls, or dental isolation systems as moisture control. A randomized clinical trial studied the difference in retention of resin dental sealant placed with rubber dam isolation or cotton roll (89). At the 12-month follow-up, no statistical significance was found.Another randomized clinical trial compared cotton roll and the Isolite system (an illuminated dental isolation system with a bite block that provides suction and retraction) as isolation for resin dental sealant and followed for 12 months after placement (90). The result was not statistically significant, indicating the cotton and Isolite system are comparable in placing dental sealant. A randomized clinical trial compared Isolite system, cotton roll and rubber dam at the same time (91). The result agreed with the above two studies. There was no statistically significant difference between these three strategies. However, most patients preferred cotton roll isolation and most patients were less likely to have rubber dam as isolation again (92).
8.2. Tooth surface preparation
Tooth surfaces cleaned with pumice and prepared with 37% phosphoric acid for 30 s are suggested.
8.2.1. Surface cleaning
Cleaning the tooth surface is required before applying dental sealant. It is because tooth surfaces are covered by salivary pellicles and products of carbohydrate metabolism which inhibit the penetration of dental sealant into the pits and fissure area (93). Therefore, Sealant placed without tooth surface cleaning was having a low retention rate (94). Resin sealant applied on tooth surfaces brushed with pumice slurry showed a significantly higher retention rate when compared with no treatment and brushing only. Another in vitro study compared the microleakage of resin dental sealant placed after dry brushing, pumice slurry cleaning, air polishing and prophylaxis paste polishing (95). Researchers found that air polishing is superior to other treatment. It was followed by pumice; prophylaxis paste and dry brushing. However, air polishing is a risk factor for subcutaneous emphysema when it is not meticulously handled (96). Therefore, using pumice is suggested.
8.2.2. Mechanical preparation with dental burs
Mechanical preparation with burs is not recommended. A clinical study found out the difference in the retention rate of dental sealant between teeth with or without fissurotomy bur preparation was not statistically significant (97). When comparing fissurotomy bur, pumice and no preparation, there was no statistical difference between using fissurotomy bur and pumice (98). However, the resin sealant placed after both treatments were having much lower microleakage than no preparation. An in vitro study compared microleakage of resin sealants placed on tooth surfaces treated with round carbide bur, air polishing, air abrasion, pumice, brushing only and longer etching time (99). The microleakage of dental sealant after bur preparation was superior. However, fissures opened with mechanical burs might be more susceptible to caries after the sealant is lost (100).
8.2.3. Mechanical preparation with laser
Current evidence regarding laser as a surface preparation method remains inconclusive. Using laser may not be a better way to increase retention or shear bond strength of dental sealant than acid etching. A randomized clinical trial was done to compare the effect of conventional acid etching and Er,Cr:YSGG laser on the retention rate of dental sealant (101). There was no statistically significant difference between the two groups after 24 months. Another randomized clinical trial comparing Er: YAG, acid etching and Er:YAG before acid etching (102). No statistically significant difference could be found between the groups. Lower shear bond strength was reported when applying dental sealant with Er:YAG instead of acid etching (103). A systematic review and meta-analysis also concluded that using Er:YAG before applying dental sealant is not giving a better retention rate than conventional phosphoric acid etching (104). While there are studies found out Er:YAG laser combined with acid etching can achieve a higher retention rate and less microleakage (105, 106). However, when considering the technical difficulties, the extra cost and the lengthened procedures, the cost-effectiveness of laser is questionable (107).
8.2.4. Mechanical preparation with air abrasion
Air abrasion is also not superior to acid etching in increasing the retention and penetrability of dental sealant. A clinical study compared the retention rate of dental sealants placed with phosphoric acid etching and air abrasion (108). The time allowed for the two treatments was the same. The difference in retention was statistically insignificant. Another study came up with the result that air abrasion prior to acid etching does not increase the retention rate (109). Air abrasion also does not improve the penetrability of dental sealant from the result of an in vitro study (110).
A systematic review and meta-analysis comparing acid etching, laser, and air abrasion showed that dental sealant applied with phosphoric acid etching would have a lower microleakage than Er:YAG laser treatment and air abrasion treatment (111).
8.2.5. Chemical preparation with acid etching
Acid etching cannot be replaced by any other tooth surface preparation (100). 37% phosphoric acid etching for resin sealant is suggested (112). A study compared resin dental sealant placed with 15 s, 30 s, 45 s and 60 s acid etching time with 37% phosphoric acid gel (113). Dental sealant applied with 60 s etching time gave out a significantly better shear bond strength. However, when considering the small difference between 30s and 60s, 30s etching time could provide a clinically acceptable result.
8.2.6. Fluoride varnish pre-treatment
Current studies do not support the use of fluoride varnish prior to dental sealant treatment. Use of fluoride does not increase the caries preventive effect and retention of dental sealant. The shear bond strength was adversely affected and the microleakage increased. A clinical study compared dental sealant placed 48 h after fluoride varnish application and dental sealant placed without prior fluoride varnish and no difference in the retention rate was found (114). There was an in vitro study compared dental sealant placed 5 min after applying fluoride varnish and sealant placed without fluoride varnish. The result showed that the mean shear bond strength of dental sealant was hugely reduced with the use of fluoride varnish (115). Another in vitro study found that applying fluoride varnish 24 h before placing resin or resin modified glass ionomer sealant increases the microleakage (116).
8.3. Application of dental adhesive
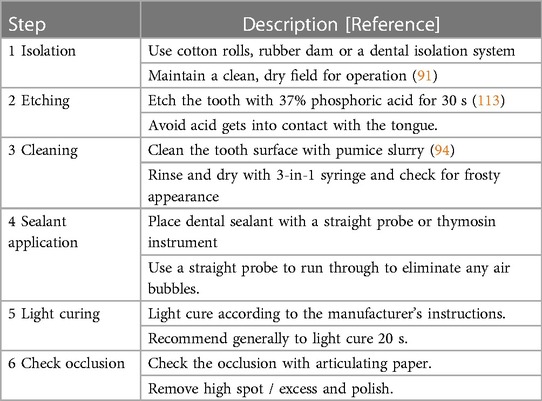
Current evidence about dental adhesives application prior to dental sealant placement is inconclusive. Several studies showed that dental adhesives increase bond strength and reduce the microleakage of resin sealant (88, 117, 118). Among the dental adhesive systems, the etch-and-rinse dental adhesive system showed a better effect in increasing the bond strength of resin sealant when compared with the self-etching system (118–120). On the other hand, a clinical study found the retention rate of resin sealant with dental adhesives was better than resin sealant without dental adhesives at the 3-month follow-up. However, this difference disappeared at 6-month and 12-month follow-ups (121). Some other studies did not find an enhancement in the retention rate of dental sealant with the addition of dental adhesives (122, 123). Literature shows strong evidence on the operative factors affecting the longevity of dental sealant. Thus, we recommend a step-by-step clinical protocol for sealant placement in Table 2.
9. Summary
Dental sealants can be classified into resin, glass ionomer and hybrid sealant with corresponding subgroups. Caries risk, type of dentition, caries status of a tooth, type of tooth surfaces, eruption status and dental fluorosis are the considering factors. The effect of dental sealants on preventing and arresting caries is supported by studies published in the recent 10 years. They can effectively prevent and arrest caries by providing a physical barrier, improving the ease of cleaning, and releasing ions. Among different sealants, resin sealant is suggested because of its superior retention and good caries-preventive effect while glass ionomer can be considered when encountering difficult moisture control. Various operative factors, including moisture control, surface preparation and application of dental adhesive, affect the clinical outcomes.
Author contributions
Conceptualization, writing, proofreading: TN, OY. Proofreading: CC. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the General Research Fund of Research Grants Council of Hong Kong SAR, China (No. 17100019).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) Results, Institute for Health Metrics and Evaluation (IHME), Seattle, United States (2019).
2. Passarelli PC, Pagnoni S, Piccirillo GB, Desantis V, Benegiamo M, Liguori A, et al. Reasons for tooth extractions and related risk factors in adult patients: a cohort study. Int J Environ Res Public Health. (2020) 17:2575. doi: 10.3390/ijerph17072575
3. Bukhari OM. Dental caries experience and oral health related quality of life in working adults. Saudi Dent J. (2020) 32:382–9. doi: 10.1016/j.sdentj.2019.11.003
4. Kaur P, Singh S, Mathur A, Makkar DK, Aggarwal VP, Batra M, et al. Impact of dental disorders and its influence on self esteem levels among adolescents. J Clin Diagn Res. (2017) 11:ZC05–8. doi: 10.7860/JCDR/2017/23362.9515
5. Kastenbom L, Falsen A, Larsson P, Sunnegardh-Gronberg K, Davidson T. Costs and health-related quality of life in relation to caries. BMC Oral Health. (2019) 19:187. doi: 10.1186/s12903-019-0874-6
6. Pitts NB, Zero DT, Marsh PD, Ekstrand K, Weintraub JA, Ramos-Gomez F, et al. Dental caries. (2017) 3(1):17030. doi: 10.1038/nrdp.2017.30
7. Sánchez-Pérez L, Irigoyen-Camacho ME, Molina-Frechero N, Zepeda-Zepeda M. Fissure depth and caries incidence in first permanent molars: a five-year follow-up study in schoolchildren. Int J Environ Res Public Health. (2019) 16:3550. doi: 10.3390/ijerph16193550
8. Yijie L, Ying W, Xiaonan W, Meng W, Xiulari Z, Wensheng R. Fissure morphology and caries prevalence in the first permanent molars of children in the Dalian development area. West China J Stomatol. (2013) 31:578–82.
9. Basha S, Swamy HS. Dental caries experience, tooth surface distribution and associated factors in 6-and 13-year-old school children from Davangere, India. J Clin Exp Dent. (2012) 4:e210. doi: 10.4317/jced.50779
10. Hyatt TP. Prophylactic odontotomy: the cutting into the tooth for the prevention of disease. Dent Regist. (1923) 77:196–228.33703822
11. Buonocore MG. A simple method of increasing the adhesion of acrylic filling materials to enamel surfaces. J Dent Res. (1955) 34:849–53. doi: 10.1177/00220345550340060801
12. Cueto EI. Adhesive sealing of pits and fissures for caries prevention, Dentistry and Dental Research, University of Rochester (1965).
13. Buonocore M. Adhesive sealing of pits and fissures for caries prevention, with use of ultraviolet light. J Am Dent Assoc. (1970) 80:324–8. doi: 10.14219/jada.archive.1970.0061
14. Council on dental materials devices, and council on dental therapeutics, pit and fissure sealants. The J Am Dent Assoc. (1971) 82:1101–3. doi: 10.14219/jada.archive.1971.0194
15. McLean J, Wilson A. Fissure sealing and filling with an adhesive glass-ionomer cement. Br Dent J. (1974) 136:269–76. doi: 10.1038/sj.bdj.4803174
16. Yu OY, Lam WY, Wong AW, Duangthip D, Chu CH. Nonrestorative management of dental caries. Dent J (Basel. (2021) 9:121. doi: 10.3390/dj9100121
17. Gizani S. Pit and fissure sealants. In: Bekes K, editors. Pit and fissure sealants. Cham: Springer International Publishing (2018). p. 23–34.
18. Pratap B, Gupta RK, Bhardwaj B, Nag M. Resin based restorative dental materials: characteristics and future perspectives. Jpn Dent Sci Rev. (2019) 55:126–38. doi: 10.1016/j.jdsr.2019.09.004
19. Sanders BJ. Pit-and-Fissure sealants and preventive resin restorations. McDonald and avery's dentistry for the child and adolescent: Tenth edition. St. Louis, MI: Elsevier (2016). p. 177–84.
20. Worzakowska M. UV polymerization of methacrylates—preparation and properties of novel copolymers. Polymers (Basel). (2021) 13:1659. doi: 10.3390/polym13101659
21. Alasiri RA, Algarni HA, Alasiri RA. Ocular hazards of curing light units used in dental practice—a systematic review. Saudi Dent J. (2019) 31:173–80. doi: 10.1016/j.sdentj.2019.02.031
22. Ahovuo-Saloranta A, Forss H, Walsh T, Nordblad A, Mäkelä M, Worthington HV. Pit and fissure sealants for preventing dental decay in permanent teeth. Cochrane Database Syst Rev. (2017) 7:Cd001830. doi: 10.1002/14651858.CD001830.pub5
23. Kowalska A, Sokolowski J, Bociong K. The photoinitiators used in resin based dental composite—a review and future perspectives. Polymers (Basel). (2021) 13:470. doi: 10.3390/polym13030470
24. Poggio C, Andenna G, Ceci M, Beltrami R, Colombo M, Cucca L. Fluoride release and uptake abilities of different fissure sealants. J Clin Exp Dent. (2016) 8:e284. doi: 10.4317/jced.52775
25. Faria M, Guedes A, Rompante P, Carvalho O, Silva F, Henriques B, et al. Wear pathways of tooth occlusal fissure sealants: an integrative review. Biotribology. (2021) 27:100190. doi: 10.1016/j.biotri.2021.100190
26. Reddy VR, Chowdhary N, Mukunda KS, Kiran NK, Kavyarani BS, Pradeep MC. Retention of resin-based filled and unfilled pit and fissure sealants: a comparative clinical study. Contemp Clin Dent. (2015) 6:S18–23. doi: 10.4103/0976-237X.152932
27. Alharthy H, Elkhodary H, Nahdreen A, Al Tuwirqi A, Baghlaf K. Comparative evaluation of retention and cariostatic effect of hydrophilic and hydrophobic resin-based sealants: a systematic review and meta-analysis. Niger J Clin Pract. (2022) 25:861–84. doi: 10.4103/njcp.njcp_1863_21
28. Nicholson JW. The history and background to glass-ionomer dental cements, glass-ionomers in dentistry. Springer. (2016):1–24. doi: 10.1007/978-3-319-22626-2_1
29. Shahid S, Duminis T. 8—glass-ionomer Cement: chemistry and its applications in dentistry. In: Khurshid Z, Najeeb S, Zafar MS, Sefat F, editors. Advanced dental biomaterials. Woodhead Publishing (2019). p. 175–95.
30. Ana ID, Anggraeni R. Development of bioactive resin modified glass ionomer cement for dental biomedical applications. Heliyon. (2021) 7:e05944. doi: 10.1016/j.heliyon.2021.e05944
31. Shen C, Rawls HR, Esquivel-Upshaw JF. Phillips’ science of dental materials. St. Louis, Mo: Elsevier/Saunders (2022).
32. Kim YK, Kim K-H, Kwon T-Y. Setting reaction of dental resin-modified glass ionomer restoratives as a function of curing depth and postirradiation time. J Spectrosc (Hindawi). (2015) 2015:1–8.
33. Ramamurthy P, Rath A, Sidhu P, Fernandes B, Nettem S, Muttalib K, et al. Sealants for preventing dental caries in primary teeth. Cochrane Db Syst Rev. (2018) 2018(3):CD012981. doi: 10.1002/14651858.CD012981
34. Rusnac ME, Gasparik C, Irimie AI, Grecu AG, Mesaroş AŞ, Dudea D. Giomers in dentistry–at the boundary between dental composites and glass-ionomers. Med Pharm Rep. (2019) 92:123. doi: 10.15386/mpr-1169
35. Fontana M, Platt JA, Eckert GJ, González-Cabezas C, Yoder K, Zero DT, et al. Monitoring of sound and carious surfaces under sealants over 44 months. J Dent Res. (2014) 93:1070–5. doi: 10.1177/0022034514551753
36. Ramamurthy P, Rath A, Sidhu P, Fernandes B, Nettem S, Fee PA, et al. Sealants for preventing dental caries in primary teeth. Cochrane Database Syst Rev. (2022) 2022(2):CD012981. doi: 10.1002/14651858.CD012981.pub2
37. Balian A, Campus G, Bontà G, Esteves-Oliveira M, Salerno C, Cirio S, et al. Long-term caries prevention of dental sealants and fluoride varnish in children with autism spectrum disorders: a retrospective cohort study. Sci Rep. (2022) 12:8478–8478. doi: 10.1038/s41598-022-12176-7
38. Philip N. State of the art enamel remineralization systems: the next frontier in caries management. Caries Res. (2019) 53:284–95. doi: 10.1159/000493031
39. Johnston NR, Strobel SA. Principles of fluoride toxicity and the cellular response: a review. Arch Toxicol. (2020) 94:1051–69. doi: 10.1007/s00204-020-02687-5
40. Alsabek L, Al-Nerabieah Z, Bshara N, Comisi JC. Retention and remineralization effect of moisture tolerant resin-based sealant and glass ionomer sealant on non-cavitated pit and fissure caries: randomized controlled clinical trial. J Dent. (2019) 86:69–74. doi: 10.1016/j.jdent.2019.05.027
41. Cagetti MG, Carta G, Cocco F, Sale S, Congiu G, Mura A, et al. Effect of fluoridated sealants on adjacent tooth surfaces: a 30-mo randomized clinical trial. J Dent Res. (2014) 93:59s–65s. doi: 10.1177/0022034514535808
42. Kaga M, Kakuda S, Ida Y, Toshima H, Hashimoto M, Endo K, et al. Inhibition of enamel demineralization by buffering effect of S-PRG filler-containing dental sealant. Eur J Oral Sci. (2014) 122:78–83. doi: 10.1111/eos.12107
43. Ogawa Y, Sayed M, Hiraishi N, Al-Haj Husain N, Tagami J, Özcan M, et al. Effect of surface pre-reacted glass ionomer containing dental sealant on the inhibition of enamel demineralization. J Funct Biomater. (2022) 13:189. doi: 10.3390/jfb13040189
44. Antonson SA, Antonson DE, Brener S, Crutchfield J, Larumbe J, Michaud C, et al. Twenty-four month clinical evaluation of fissure sealants on partially erupted permanent first molars: glass ionomer versus resin-based sealant. J Am Dent Assoc. (2012) 143:115–22. doi: 10.14219/jada.archive.2012.0121
45. Bhatia MR, Patel AR, Shirol DD. Evaluation of two resin based fissure sealants: a comparative clinical study. J Indian Soc Pedodontics Prev Dent. (2012) 30:227–30. doi: 10.4103/0970-4388.105015
46. Ulusu T, Odabaşv ME, Tüzüner T, Baygin Ö, Sillelioǧlu H, Deveci C, et al. The success rates of a glass ionomer cement and a resin-based fissure sealant placed by fifth-year undergraduate dental students. Eur Arch Paediatr Dent. (2012) 13:94–7. doi: 10.1007/BF03262852
47. Bhat PK, Konde S, Raj SN, Kumar NC. Moisture-tolerant resin-based sealant: a boon. Contemp Clin Dent. (2013) 4:343–8. doi: 10.4103/0976-237X.118394
48. Chen XX, Liu XG. Clinical comparison of Fuji VII and a resin sealant in children at high and low risk of caries. Dent Mater J. (2013) 32:512–8. doi: 10.4012/dmj.2012-300
49. Kumaran P. Clinical evaluation of the retention of different pit and fissure sealants: a 1-year study. Int J Clin Pediatr Dent. (2013) 6:183–7. doi: 10.5005/jp-journals-10005-1215
50. Hasanuddin S, Reddy ER, Manjula M, Srilaxmi N, Rani ST, Rajesh A. Retention of fissure sealants in young permanent molars affected by dental fluorosis: a 12-month clinical study. Eur Arch Paediatr Dent. (2014) 15:309–15. doi: 10.1007/s40368-014-0116-1
51. Khatri SG, Samuel SR, Acharya S, Patil S, Madan K. Retention of moisture-tolerant and conventional resin-based sealant in six- to nine-year-old children. Pediatr Dent. (2015) 37:366–70.26314605
52. Gonçalves PSP, Kobayashi TY, de Oliveira TM, Honório HM, Rios D, da Silva SMB. Pit and fissure sealants with different materials: resin based x glass ionomer cement—results after six months. Pesqui Bras Odontope. (2016) 16:15–23. doi: 10.4034/PBOCI.2016.161.02
53. Haznedaroğlu E, Güner Ş, Duman C, Menteş A. A 48-month randomized controlled trial of caries prevention effect of a one-time application of glass ionomer sealant versus resin sealant. Dent Mater J. (2016) 35:532–8. doi: 10.4012/dmj.2016-084
54. Al-Jobair A, Al-Hammad N, Alsadhan S, Salama F. Retention and caries-preventive effect of glass ionomer and resin-based sealants: an 18-month-randomized clinical trial. Dent Mater J. (2017) 36(5):2016–225. doi: 10.4012/dmj.2016-225
55. Askarizadeh N, Heshmat H, Zangeneh N. One-Year clinical success of embrace hydrophilic and helioseal-F hydrophobic sealants in permanent first molars: a clinical trial. J Dent (Tehran). (2017) 14:92–9.29104600
56. Liu YJ, Chang Q, Rong WS, Zhao XL. Caries prevention effectiveness of aresin based sealant and a glass ionomer sealants: a report of 5-year-follow-up. Zhonghua Kou Qiang Yi Xue Za Zhi. (2018) 53:437–42. doi: 10.3760/cma.j.issn.1002-0098.2018.07.002
57. Ntaoutidou S, Arhakis A, Tolidis K, Kotsanos N. Clinical evaluation of a surface pre-reacted glass (S-PRG) filler-containing dental sealant placed with a self-etching primer/adhesive. Eur Arch Paediatr Dent. (2018) 19:431–7. doi: 10.1007/s40368-018-0379-z
58. Siripokkapat K, Nakornchai S, Vichayanrat T. Comparison of giomer and fluoride releasing resin sealants in caries prevention among primary molars. Southeast Asian J Trop Med Public Health. (2018) 49:527–36.
59. Mathew SR, Narayanan RK, Vadekkepurayil K, Puthiyapurayil J. One-year clinical evaluation of retention ability and anticaries effect of a glass ionomer-based and a resin-based fissure sealant on permanent first molars: an in vivo study. Int J Clin Pediatr Dent. (2019) 12:553. doi: 10.5005/jp-journals-10005-1702
60. Prathibha B, Reddy P, Anjum M, Monica M, Praveen B. Sealants revisited: an efficacy battle between the two major types of sealants—a randomized controlled clinical trial. Dent Res J (Isfahan). (2019) 16:36–41. doi: 10.4103/1735-3327.249551
61. Jaafar N, Ragab H, Abedrahman A, Osman E. Performance of fissure sealants on fully erupted permanent molars with incipient carious lesions: a glass-ionomer-based versus a resin-based sealant. J Dent Res Dent Clin Dent Prospects. (2020) 14:61–7. doi: 10.34172/joddd.2020.009
62. Mohapatra S, Prabakar J, Indiran MA, Kumar RP, Sakthi DS., comparison and evaluation of the retention, cariostatic effect, and discoloration of conventional clinpro 3M ESPE and hydrophilic ultraseal XT hydro among 12-15-year-old schoolchildren for a period of 6 months: a single-blind randomized clinical trial. Int J Clin Pediatr Dent. (2020) 13:688–93. doi: 10.5005/jp-journals-10005-1859
63. Beresescu L, Păcurar M, Vlasa A, Stoica AM, Dako T, Petcu B, et al. Comparative assessment of retention and caries protective effectiveness of a hydrophilic and a conventional sealant-A clinical trial. Children. (2022) 9:646. doi: 10.3390/children9050646
64. Haricharan PB, Voruganti S, Kotha A, Shivanna MM, Gandhi B, Suresh N. An efficacy study between high viscosity glass ionomers and resin sealants in fissure caries prevention: a 2-year split mouth randomized controlled trial. Eur J Dent. (2022) 16:137–44. doi: 10.1055/s-0041-1731925
65. Özgür B, Kargın ST, Ölmez MS. Clinical evaluation of giomer- and resin-based fissure sealants on permanent molars affected by molar-incisor hypomineralization: a randomized clinical trial. BMC Oral Health. (2022) 22:275. doi: 10.1186/s12903-022-02298-9
66. Reic T, Galic T, Negovetic Vranic D. Retention and caries-preventive effect of four different sealant materials: a 2-year prospective split-mouth study. Int J Paediatr Dent. (2022) 32:449–57. doi: 10.1111/ipd.12924
67. Singh D, Malik M, Mathur S. Comparative evaluation of clinical performance of giomer based and hydrophilic resin based pit and fissure sealant in primary molars: a split mouth clinical trial. J Pharm Negat Results. (2022) 13:1883–9. doi: 10.47750/pnr.2022.13.S04.229
68. Uzel I, Gurlek C, Kuter B, Ertugrul F, Eden E. Caries-Preventive effect and retention of glass-ionomer and resin-based sealants: a randomized clinical comparative evaluation. BioMed Res Int. (2022) 2022:1–7. doi: 10.1155/2022/7205692
69. Akinlotan M, Chen B, Fontanilla TM, Chen A, Fan VY. Economic evaluation of dental sealants: a systematic literature review. Community Dent Oral Epidemiol. (2018) 46:38–46. doi: 10.1111/cdoe.12326
70. Griffin SO, Wei L, Gooch BF, Weno K, Espinoza L. Vital signs: dental sealant use and untreated tooth decay among U.S. School-aged children. Morb Mortal Wkly Rep. (2016) 65:1141–5. doi: 10.15585/mmwr.mm6541e1
71. Lam PPY, Sardana D, Lo ECM, Yiu CKY. Fissure sealant in a nutshell. Evidence-based meta-evaluation of sealants’ effectiveness in caries prevention and arrest. J Evid Based Dent Pract. (2021) 21:101587. doi: 10.1016/j.jebdp.2021.101587
72. Hesse D, Bonifácio CC, Mendes FM, Braga MM, Imparato JCP, Raggio DP. Sealing versus partial caries removal in primary molars: a randomized clinical trial. BMC Oral Health. (2014) 14:58. doi: 10.1186/1472-6831-14-58
73. Godhi B, Shanbhog R, Nandlal B, Rashmi S, Gopi A. Retention and caries preventive effect of GC fuji VII sealant on the first permanent molars among high-risk residential school children-A three year follow up study. J Nat Sci Biol Med. (2021) 12:155–60. doi: 10.4103/jnsbm.JNSBM_154_20
74. Wright JT, Tampi MP, Graham L, Estrich C, Crall JJ, Fontana M, et al. Sealants for preventing and arresting pit-and-fissure occlusal caries in primary and permanent molars: a systematic review of randomized controlled trials-a report of the American dental association and the American academy of pediatric dentistry. J Am Dent Assoc (1939). (2016) 147:631–645.e18. doi: 10.1016/j.adaj.2016.06.003
75. Urquhart O, Tampi MP, Pilcher L, Slayton RL, Araujo MWB, Fontana M, et al. Nonrestorative treatments for caries: systematic review and network meta-analysis. J Dent Res. (2019) 98:14–26. doi: 10.1177/0022034518800014
76. Borges BCD, de Souza Borges J, Braz R, Montes MAJR, de Assunção Pinheiro IV. Arrest of non-cavitated dentinal occlusal caries by sealing pits and fissures: a 36-month, randomised controlled clinical trial. Int Dent J. (2012) 62:251–5. doi: 10.1111/j.1875-595X.2012.00117.x
77. Soto-Rojas AE, EscoffiÉ-RamÍRez M, PÉRez-Ferrera G, Guido JA, Mantilla-Rodriguez AA, Martinez-Mier EA. Retention of dental sealants placed on sound teeth and incipient caries lesions as part of a service-learning programme in rural areas in Mexico: retention of dental sealants placed on sound teeth. Int J Paediatr Dent. (2012) 22:451–8. doi: 10.1111/j.1365-263X.2011.01216.x
78. Kasemkhun P, Nakornchai S, Phonghanyudh A, Srimaneekarn N. The efficacy of dental sealant used with bonding agent on occlusal caries (ICDAS 2-4): a 24-month randomized clinical trial. Int J Paediatr Dent. (2021) 31:760–6. doi: 10.1111/ipd.12758
79. Muñoz-Sandoval C, Gambetta-Tessini K, Giacaman RA. Microcavitated (ICDAS 3) carious lesion arrest with resin or glass ionomer sealants in first permanent molars: a randomized controlled trial. J Dent. (2019) 88:103163. doi: 10.1016/j.jdent.2019.07.001
80. Beresescu L, Păcurar M, Bica CI, Vlasa A, Stoica OE, Dako T, et al. The assessment of Sealants’ effectiveness in arresting non-cavitated caries lesion—a 24-month follow-up. Healthcare. (2022) 10:1651. doi: 10.3390/healthcare10091651
81. Basili CP, Emilson CG, Corvalan GC, Moran MP, Torres C, Quiroz MD, et al. Preventive and therapeutic proximal sealing: a 3.5-year randomized controlled clinical trial follow-up. Caries Res. (2017) 51:387–93. doi: 10.1159/000470851
82. Chen Y, Chen D, Lin H. Infiltration and sealing for managing non-cavitated proximal lesions: a systematic review and meta-analysis. BMC Oral Health. (2021) 21:13–13. doi: 10.1186/s12903-020-01364-4
83. Lindquist B, Emilson C-G. Sealing proximal non- and micro-cavitated carious lesions using a one-session separator technique: a 2-year randomised clinical study. Caries Res. (2020) 54:483–90. doi: 10.1159/000509679
84. Moreira KMS, Kantovitz KR, Aguiar JPD, Borges AFS, Pascon FM, Puppin-Rontani RM. Impact of the intermediary layer on sealant retention: a randomized 24-month clinical trial. Clin Oral Investig. (2017) 21:1435–43. doi: 10.1007/s00784-016-1890-4
85. Memarpour M, Rafiee A, Shafiei F, Dorudizadeh T, Kamran S. Adhesion of three types of fissure sealant in saliva-contaminated and noncontaminated conditions: an in vitro study. Eur Arch Paediatr Dent. (2021) 22:813–21. doi: 10.1007/s40368-021-00626-1
86. Paryab M. Sealant microleakage after using nano-filled bonding agents on saliva-contaminated enamel. J Dent (Tehran). (2013) 10:227–32.25512749
87. Memarpour M, Shafiei F, Zarean M, Razmjoei F. Sealing effectiveness of fissure sealant bonded with universal adhesive systems on saliva-contaminated and noncontaminated enamel. J Clin Exp Dent. (2018) 10:e1–6. doi: 10.4317/jced.54471
88. Bao Z, Sun H, Fan D, Wang X, Wang Q. Shear bond strength and microleakage of pit and fissure sealants placed after saliva-contaminated etched enamel. Coatings. (2022) 12:441. doi: 10.3390/coatings12040441
89. Bandi M, Mallineni SK, Nuvvula S. Influence of isolation methods on retention of pit and fissure sealants in young permanent teeth based on simonsen's criteria: a randomised clinical trial. J Clin Diagn Res. (2021) 15:ZC06–ZC09. doi: 10.7860/JCDR/2021/44929.14734
90. Lyman T, Viswanathan K, McWhorter A. Isolite vs. cotton roll isolation in the placement of dental sealants. Pediatr Dent. (2013) 35:95E–9E.
91. Mattar RE, Sulimany AM, Binsaleh SS, Hamdan HM, Al-Majed IM. Evaluation of fissure sealant retention rates using isolite in comparison with rubber dam and cotton roll isolation techniques: a randomized clinical trial. Int J Paediatr Dent. (2023) 33(1):12–19. doi: 10.1111/ipd.13008
92. Mattar RE, Sulimany AM, Binsaleh SS, Al-Majed IM. Comparison of fissure sealant chair time and Patients’ preference using three different isolation techniques. Children (Basel). (2021) 8:444. doi: 10.3390/children8060444
93. Sridhar LP, Moses J, Rangeeth BN, Sivakumar S. Comparative evaluation of the marginal sealing ability of two commercially available pit and fissure sealants. J Clin Diagn Res. (2016) 10:ZC01–4. doi: 10.1111/crj.12367
94. Hegde RJ, Coutinho RC. Comparison of different methods of cleaning and preparing occlusal fissure surface before placement of pit and fissure sealants: an in vivo study. J Indian Soc Pedod Prev Dent. (2016) 34:111. doi: 10.4103/0970-4388.180403
95. Ansari MT, Verma MK, Abdullah A. A comparative evaluation of different methods PF cleaning and preparing occlusal fissures, before placement of pit and fissure sealant: a stereomicroscopic study. Univ J Dent Sci. (2022) 8:10–15. doi: 10.21276/ujds.2022.8.3.3
96. Alonso V, García-Caballero L, Couto I, Diniz M, Diz P, Limeres J. Subcutaneous emphysema related to air-powder tooth polishing: a report of three cases. Aust Dent J. (2017) 62:510–5. doi: 10.1111/adj.12537
97. Nahid A, Zahra BG, Yasaman R. Evaluation of the effect of enamel preparation on retention rate of fissure sealant. Contemp Clin Dent. (2012) 3:380–2. doi: 10.4103/0976-237X.107418
98. Bagherian A, Akbari M, Rezaeian M, Ansari G. Microleakage assessment of fissure sealant following fissurotomy bur or pumice prophylaxis use before etching. Dent Res J (Isfahan). (2013) 10:643–6.24348623
99. Agrawal A, Shigli A. Comparison of six different methods of cleaning and preparing occlusal fissure surface before placement of pit and fissure sealant: an in vitro study. J Indian Soc Pedod Prev Dent. (2012) 30:51–5. doi: 10.4103/0970-4388.95582
100. Bagherian A, Sarraf Shirazi A. Preparation before acid etching in fissure sealant therapy: yes or no? A systematic review and meta-analysis. J Am Dent Assoc (1939). (2016) 147:943–51. doi: 10.1016/j.adaj.2016.08.003
101. Karaman E, Yazici A, Baseren M, Gorucu J. Comparison of acid versus laser etching on the clinical performance of a fissure sealant: 24-month results. Oper Dent. (2013) 38:151–8. doi: 10.2341/11-435-C
102. Yilmaz H, Keles S. The effect of the er: yAG laser on the clinical success of hydrophilic fissure sealant: a randomized clinical trial. Eur Oral Res. (2020) 54:148–53. doi: 10.26650/eor.20200029
103. Rattanacharoenthum A, Phun P, Kantrong N. Altered adhesion of dental sealant to tooth enamel microscopically modified by er:Yag laser irradiation: an in vitro study. Laser Ther. (2019) 28:19–25. doi: 10.5978/islsm.28_19-OR-02
104. Zhang Y, Wang Y, Chen Y, Chen Y, Zhang Q, Zou J. The clinical effects of laser preparation of tooth surfaces for fissure sealants placement: a systematic review and meta-analysis. BMC Oral Health. (2019) 19:203. doi: 10.1186/s12903-019-0892-4
105. Khogli AE, Cauwels R, Vercruysse C, Verbeeck R, Martens L. Microleakage and penetration of a hydrophilic sealant and a conventional resin-based sealant as a function of preparation techniques: a laboratory study. Int J Paediatr Dent. (2013) 23:13–22. doi: 10.1111/j.1365-263X.2011.01218.x
106. Durmus B, Giray F, Peker S, Kargul B. Clinical evaluation of a fissure sealant placed by acid etching or er: yAG laser combined with acid etching. Oral Health Prev Dent. (2017) 15:157–62. doi: 10.3290/j.ohpd.a37927
107. Ciucchi P, Neuhaus KW, Emerich M, Peutzfeldt A, Lussi A. Evaluation of different types of enamel conditioning before application of a fissure sealant. Lasers Med Sci. (2015) 30:1–9. doi: 10.1007/s10103-013-1333-2
108. Reddy PVR, Shigli A, Shirol D, Deshpande S, Hugar S, Poonacha KS. The evaluation of different methods viz., acid etch and by air abrasion on retentivity of fissure sealant after 6 months: a clinical study. J Sci Soc. (2014) 41:16–21. doi: 10.4103/0974-5009.126709
109. Bhushan U, Goswami M. Evaluation of retention of pit and fissure sealants placed with and without air abrasion pretreatment in 6-8 year old children–an in vivo study. J Clin Exp Dent. (2017) 9:e211. doi: 10.4317/jced.53259
110. Cho JS, Covey D, Abdelmegid F, Salama F. Effects of the preparation technique and type of material on the penetrability of sealants. Gen Dent. (2015) 63:e18–22.26147176
111. Fumes AC, Longo DL, De Rossi A, Fidalgo TKdS, de Paula e Silva FWG, Borsatto MC, et al. Microleakage of sealants after phosphoric acid, er: yAG laser and air abrasion enamel conditioning: systematic review and meta-analysis. J Clin Pediatr Dent. (2017) 41:167–72. doi: 10.17796/1053-4628-41.3.167
112. Markovic DL, Petrovic BB, Peric TO, Trisic D, Kojic S, Kuljic BL, et al. Evaluation of sealant penetration in relation to fissure morphology, enamel surface preparation protocol and sealing material. Oral Health Prev Dent. (2019) 17:349–55. doi: 10.3290/j.ohpd.a42689
113. Lo Y-F, Pitchika V, Ilie N, Hickel R, Kuehnisch J. Does etching time affect the in vitro performance of a sealant material? Dent Mater J. (2020) 39:862–8. doi: 10.4012/dmj.2019-133
114. Lakshmi MS, Srilatha KT, Nandlal B, Deshmukh S. Clinical evaluation of preventive effect of fissure sealants on initial carious lesion of permanent mandibular molars pretreated with and without fluoride varnish by fluorescence camera. Int J Clin Pediatr Dent. (2018) 11:89–93. doi: 10.5005/jp-journals-10005-1491
115. Frazer RA, Platt JA, Sanders BJ, Yepes JF, Jones JE. The effect of fluoride varnish on enamel shear bond strength of pit and fissure sealants. Pediatr Dent. (2017) 39:155–8.28390467
116. Germán-Cecilia C, Reyes SMG, Silva AP, Muñoz CS, Ortiz-Ruiz AJ. Microleakage of conventional light-cure resin-based fissure sealant and resin-modified glass ionomer sealant after application of a fluoride varnish on demineralized enamel. PLoS ONE. (2018) 13:e0208856. doi: 10.1371/journal.pone.0208856
117. Attar MH, Abdallah MA, Alharthy HA, El Meligy OA. Effect of bonding agent on retention of different sealants: an in vitro study. J Clin Pediatr Dent. (2021) 45:177–85. doi: 10.17796/1053-4625-45.3.6
118. Bagherian A, Shirazi AS, Sadeghi R. Adhesive systems under fissure sealants: yes or no? A systematic review and meta-analysis. J Am Dent Assoc. (2016) 147:446–56. doi: 10.1016/j.adaj.2016.01.014
119. Botton G, Morgental CS, Scherer MM, Lenzi TL, Montagner AF, Rocha RdO. Are self-etch adhesive systems effective in the retention of occlusal sealants? A systematic review and meta-analysis. Int J Paediatr Dent. (2016) 26:402–11. doi: 10.1111/ipd.12214
120. Martignon S, Zarta OL. The use of adhesive systems under fissure sealants improves their retention, with etch-and-rinse performing better than self-etching adhesive systems. J Evid Based Dent Pract. (2017) 17:56–8. doi: 10.1016/j.jebdp.2017.01.012
121. Khare M, Suprabha BS, Shenoy R, Rao A. Evaluation of pit-and-fissure sealants placed with four different bonding protocols: a randomized clinical trial. Int J Paediatr Dent. (2017) 27:444–53. doi: 10.1111/ipd.12281
122. Bandi M, Mallineni S, Nuvvula S. Retention and effectiveness of pit and fissure sealants placed with or without bonding agent in young permanent teeth: a randomized clinical trial with a year follow-up. Indian J Dent Res. (2020) 31:877–82. doi: 10.4103/ijdr.IJDR_779_19
Keywords: dental sealant, dental caries, caries management, cariology, preventive dentistry, oral health
Citation: Ng Toby Cheuk-Hang, Chu C-H and Yu OY (2023) A concise review of dental sealants in caries management. Front. Oral. Health 4:1180405. doi: 10.3389/froh.2023.1180405
Received: 6 March 2023; Accepted: 29 March 2023;
Published: 17 April 2023.
Edited by:
May Lei Mei, University of Otago, New ZealandReviewed by:
Bhojraj Nandlal, JSS Dental College and Hospital, India© 2023 Ng, Chu and Yu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ollie Yiru Yu b2xsaWV5dUBoa3UuaGs=
Specialty Section: This article was submitted to Preventive Dentistry, a section of the journal Frontiers in Oral Health
 Toby Cheuk-Hang Ng
Toby Cheuk-Hang Ng Chun-Hung Chu
Chun-Hung Chu Ollie Yiru Yu
Ollie Yiru Yu