- 1School of Health and Welfare, Halmstad University, Halmstad, Sweden
- 2Julie Reed Consultancy Ltd., London, United Kingdom
- 3School of Public Health, Imperial College London, London, United Kingdom
- 4Department of Population Health Sciences, University of Leicester, Leicester, United Kingdom
- 5Institute of Health Policy, Management and Evaluation, University of Toronto, Toronto, ON, Canada
- 6Clinical Operational Research Unit, University College London, London, United Kingdom
- 7Medical Management Centre, Karolinska Institutet (KI), Solna, Sweden
- 8Imperial College London, London, United Kingdom
- 9Centre for Medicines Optimisation Research & Education, University College London Hospitals NHS Foundation Trust, London, United Kingdom
- 10School of Pharmacy, University College London, London, United Kingdom
- 11Associates in Process Improvement, Austin, TX, United States
- 12School of Health and Welfare, Jönköping University, Jönköping, Sweden
- 13The Jönköping Academy for Improvement of Health and Welfare, Jönköping, Sweden
- 14School of Health and Social Care, Swansea University, Swansea, United Kingdom
Improvement science has emerged as an interdisciplinary field of enquiry to provide methodological and scientific rigour to the practice and study of improvements in healthcare, and with contributions from a wide range of stakeholders and perspectives. However, compared to more well-established health-related sciences, the science of improvement remains in relative infancy. Whilst the improvement community has grown considerably, there is no existing articulation of the scope of what matters to the health and social care improvement community, and how this aligns to the enquiries of the field of improvement science. This paper aims to outline key areas of interest to the improvement community, and to propose distinguishing features of improvement science that help differentiate it from other areas of enquiry. Two over-arching research questions are identified, along with ten associated areas of enquiry which are grouped into three clusters: (1) improvement in practice, (2) aligning improvement efforts and (3) advancing the contribution of the improvement community. Four features that collectively define and distinguish the field of improvement science are proposed. The outline of the improvement landscape provides a common language for the diverse improvement community, supporting people to transcend disciplinary interests and constraints, and to consider how, collectively, we can improve health and care. Others are invited to refine and advance mapping of the improvement landscape by identifying gaps and increasing contributions from diverse perspectives.
Introduction
Understanding how to improve healthcare in different settings and diverse contexts is a major global challenge to ensure the fundamental rights of every human being to “the enjoyment of the highest attainable standard of health” (1).
Improvement science has emerged in response to these challenges, seeking to provide methodological and scientific rigour to the practice and study of improvements in healthcare, and engaging contributions from a wide range of stakeholders and perspectives. However, compared to more well-established health-related sciences, the science of improvement remains in relative infancy and was described by Marshall et al. as being in the “pre-paradigm” phase due to the lack of agreed definition of the field (2). Khun defines a scientific paradigm as a community with a shared focus on “what matters”:
“There is room for considerable disagreements within such a field, often about very basic issues. What is shared, however, is a sense of what is at issue, why it matters, and what must be done to resolve it” (2).
Whilst the improvement community has grown considerably since Marshall's 2013 publication, to the best of our knowledge there is no existing articulation of the scope of what matters to the health and social care improvement community, and how this aligns to the enquiries of the field of improvement science.
This paper aims to outline key areas of interest to the improvement community, and to propose distinguishing features of improvement science that help differentiate it from other areas of enquiry. Our intent is that by articulating what matters, this paper can contribute to advancing the science of improvement beyond its “pre-paradigm” phase.
Defining the scope and interests of the improvement community is complicated by the various ways in which the term improvement science has been adopted by different groups, meaning that even the term “improvement science” is contested (3). For example, the term improvement science can be used:
– To represent the classic schools of thought that emerged in non-healthcare industries that provide mental models for thinking about improvement in systems (e.g., Demings system of profound knowledge) (4, 5).
– As a synonym for the term “quality improvement”, with the implication that any given suite of tools and methods utilised for quality improvement (e.g., six sigma, lean, model for improvement) provide a structured scientific approach to make improvements in practice (6).
– To describe the study and evaluation of quality improvement approaches in practice (i.e., to build evidence about what quality improvement approaches work, when, for whom and for what purposes) (7–9).
– To consider the philosophical assumptions of sciences that aim to achieve improvements and their comparison and contrast to more traditional sciences that aim to build knowledge (10–12).
Rather than advocating for one or another of these perspectives on what improvement science is, we believe that all perspectives have value to add. Being explicit about these contributions will help to widen people's awareness of the breath of what the field of improvement science can include, and how these different interpretations support, compliment and at times conflict with each other. It is beyond the scope of this paper to define and lay out all of the factors that need to be considered in this respect—but we invite others to contribute to discussion and reflections on these issues as part of this special issue.
Background
As a group of authors we had the privilege of being exposed to diverse contributions to the study and practice of improvement through our engagement in an international improvement science fellowship community (see Supplementary Material for further details). Through these interactions we became aware that, as an emerging field, improvement science is still defining its scope and its differentiation from other fields of enquiry and practice. There is no doubt that improvement science has been influenced by and draws heavily upon more established fields including patient safety, quality improvement, implementation science, innovation and intervention research, health service research, health economics, complex systems thinking, sociology, psychology, operational research, engineering, design, organisational and management sciences to name but a few.
Given the extensive contributions from and overlap with interests of other fields, common questions we encountered were “what is actually new in the field of improvement science?”, and “how is it different from what has gone before?”.
In our growing appreciation of the diversity of perspectives in the improvement community, we also became aware of the risk that members of the improvement community work in relative isolation, focused on specific areas of enquiry, and opportunities for collaboration and enhanced overall understanding are missed. The diversity of the improvement community reflects the complexity and intricacy of the challenges faced. As well as attracting researchers from various disciplines, patients, practitioners, clinical leaders, educators, management consultants, industry partners, and policy makers, among others, are also key contributors to the improvement community. These different backgrounds influence where people's interests lie, and provide different ways of framing challenges and explaining phenomena along with their associated tools, methodologies, and perspectives—all of which can make it challenging to communicate and collaborate with other members of the improvement community.
As such, we saw value in developing an outline of the improvement landscape to: articulate the breadth of areas that matter to members of the improvement community; illustrate key questions that are at the frontiers of the field of improvement science; and propose a series of features that distinguish improvement science from other fields of enquiry.
First and foremost, we believe that initiating an outline of the field of improvement science and proposing distinguishing features of the field will help to create a common language to foster collaboration and help the community to grow and achieve its goals.
Second, by highlighting questions at the frontiers we leave scope for contributions from different perspectives to address them, enabling people to transcend disciplinary interests and constraints, and to consider how, collectively, we can improve health services.
Third, there is a need to clearly articulate the improvement landscape to be able to communicate and gain traction with those outside of the current improvement community, including other academic disciplines, healthcare leaders, managers and practitioners, funders, governments and the general public.
Finally, we propose that the provision of a structured outline of areas of enquiry can inform decisions concerning the design, conduct and evaluation of improvement initiatives and research enquiries, and inform the development of capacity and capability of improvement community members.
Process of development
The outline of the improvement landscape was developed by drawing on the breadth of our professional backgrounds as authors, and in consultation with the international improvement community. An initial outline of the improvement landscape was developed by the authorship group. It was then further expanded and refined in an iterative process with feedback obtained from the wider improvement community in an opportunistic manner through presentations and workshops delivered by the authorship group as part of existing national and international conferences (the Improvement Science and Research Symposium, UK, International Forum on Quality and Safety in Healthcare, UK; Health Service Research conference, UK; The International Society for Quality in Health Care (ISQua) Malaysia; IHI National Forums Scientific Symposium, USA) and in partnership with the international Improvement Science Development Group supported by the Health Foundation, UK. These community participants had a variety of roles within the health system (e.g., academics, healthcare professionals, quality improvement experts, managers, policy makers, patients, etc.). In total, over 380 stakeholders were involved (with groups ranging from 20 to over 100 participants). Feedback was collected via a mixture of group discussions and electronic feedback (using Mentimeter software). Analysis focused on developing a comprehensive overview of the breadth of concepts raised, and identifying themes to logically group and capture the range of topics discussed. Further details about the process are provided in the Supplementary Material.
In discussions with stakeholders, we focused on topics relating to how to achieve improvement in care, rather than what needs to be improved. We deliberately did not include the specific areas of health, health services, population health, or societal concerns that need improving and are covered extensively by clinical groups, public health and international bodies (13). The outline of the improvement landscape therefore contains generic issues we believe are pertinent to the improvement of any aspect of health and social care.
We made a concerted effort to value different perspectives and vocabularies and invested time to understand the diverse theories and disciplines, rather than negotiating away nuance in favour of quick compromise. We paid particular attention to the use of language that was accessible and enabled diverse disciplines to engage.
An outline of the improvement landscape
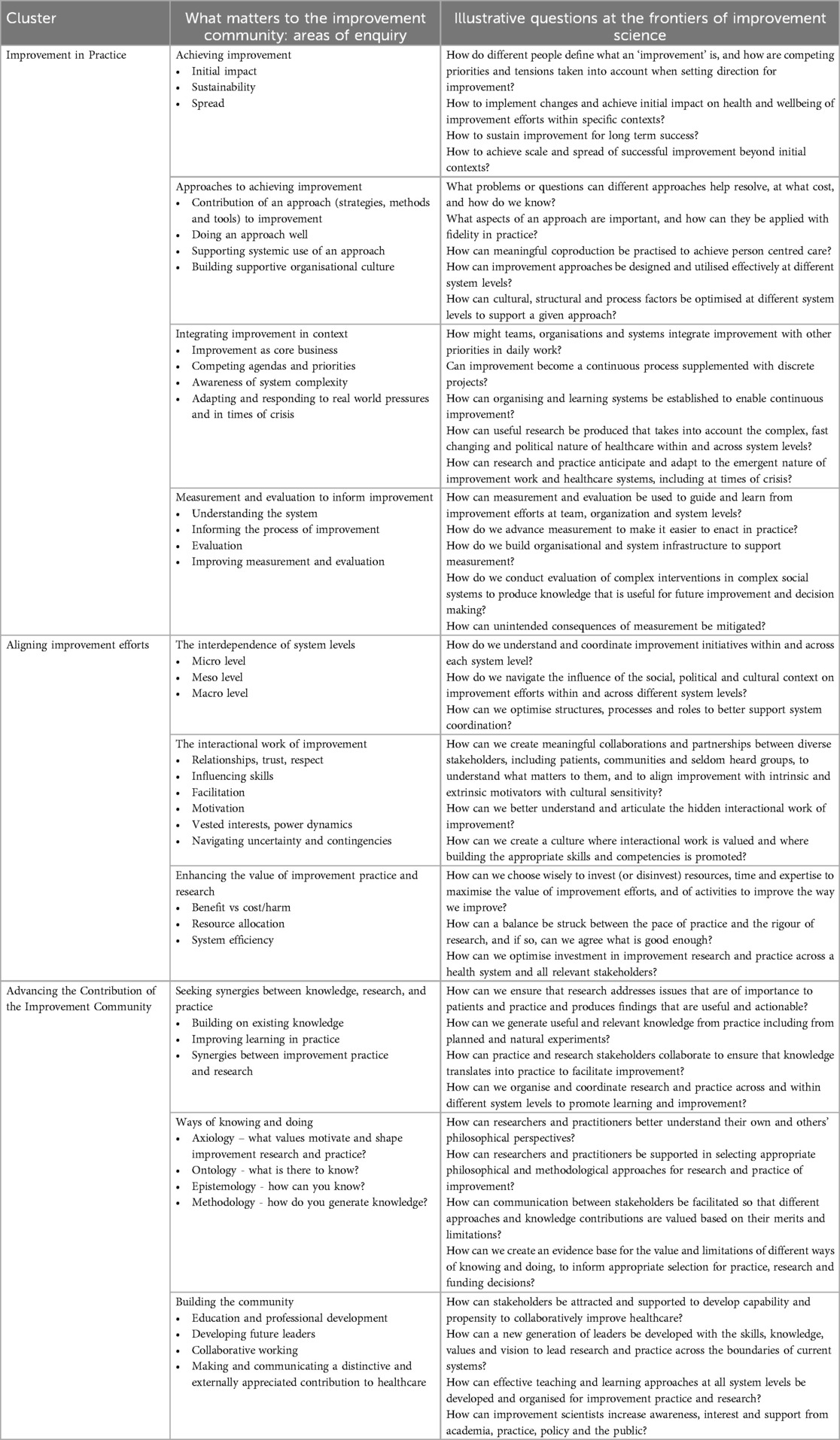
In reviewing feedback about what matters to members of the health service improvement community, we identified two over-arching questions, and ten associated areas of enquiry (Table 1).
The two over-riding questions that matter to the improvement community are:
• “How can we achieve improvements in complex systems?”
• “How can we improve the way we improve?”
The ten areas of enquiry vary in character from the practical to the more philosophical. Whilst each area of enquiry is presented as somewhat discrete, there are important interconnections, overlaps, and tensions. This led us to group the areas of enquiry into three clusters: (1) Improvement in Practice (2) Aligning Improvement Efforts (3) Advancing the Contribution of the Improvement Community.
Within each area we identified key questions that illustrate issues of major interest to the field of improvement science (Table 1). Many of these questions have been partially addressed by contributions in the academic literature or by examples in practice. However, none of them have been fully resolved and barriers remain to effective application and spread of improvement knowledge. For example, there is evidence of both successful and unsuccessful attempts at using various quality improvement approaches to support change, but it is not yet clear which approaches are best suited for different problem types, and in different contexts (14). Evidence also demonstrates that quality improvement approaches are not used with high fidelity, but it is not yet clear how to reliably improve the fidelity of their use in diverse settings (15). Therefore, all questions represent areas at the frontiers of current knowledge, with active and ongoing enquiry in research and practice.
Cluster 1—improvement in practice
Achieving improvements
The first area reflects the focal point that all other areas are working towards, the desired outcome of improvement efforts. People work to improve different facets of quality of care including safety, efficiency, effectiveness, timeliness, patient-centeredness, staff-wellbeing, and equality (16–18). Whole fields of study have developed to explore improving aspects of quality in more detail, including patient safety focusing on the reduction of harm, implementation science focusing the delivery of evidence-based care, and coproduction focusing on patient and person centred care. Other areas have received notably less attention such as equality and equity of health services, although this is gradually changing. Central to this area of enquiry is the question of what is being improved, who sets the agenda, and the trade-offs and balance between different facets of quality e.g., efficiency and effectiveness. Despite advances in understanding of how to achieve improvements, challenges still remain in knowing how to reliably achieve an impact on care quality and how improvements can be sustained. In addition there are recognised challenges to the spread and reproduction of successful initiatives beyond their initial setting, including understanding how to adapt interventions and initiatives to work in different contexts (19, 20).
Approaches to achieving improvement
In seeking to achieve these quality gains people have explored the use of a wide range of quality improvement approaches (e.g., quality improvement methods, national quality registries, audit and feedback, policy changes). Research is exploring the impact and mechanisms of action of different approaches. This includes understanding their benefits and limitations, knowing what approaches to use in different settings and for different improvement goals, and how approaches can be optimised for greatest impact in healthcare settings. It has been demonstrated that approaches are adopted with varying degrees of fidelity (21) and that effective use is influenced by organisational context including infrastructure, leadership and learning culture (22). As such there is a need to understand how best to support the approaches for optimal use, including understanding how to improve fidelity of use, understanding what aspects of an approach are most important to adhere to for successful use, and how approaches can be adapted to work in a variety of settings and constraints. This understanding is necessary to support the successful application, evaluation, attribution, spread and reproducibility of improvement approaches (23).
Integrating improvement in context
Improvement takes place alongside “business as usual” and is influenced by institutional factors such as staffing, busy-ness, and the need to respond to crises such as the Covid-19 pandemic. We need to understand how improvement can become an integral, core activity, and how it fits with the daily practice, operational management and strategic planning of health services. Consideration needs to be given to how improvement initiatives and improvement approaches are experienced by healthcare staff including understanding their prior experiences and receptivity to improvement work, the extent to which initiatives align with or compete with other responsibilities, and how to manage time constraints for improvement work alongside the delivery of care. Improvement approaches and research studies needs to be optimised to work in complex and dynamic health care systems (24), recognising the fast pace of change and emergent issues that require consistent adaptation and revised responses. Understanding how to build individual, organisational and system resilience to adapt and align improvement activities to a constantly changing workplace is essential to embed and sustain improvements (20).
Measurement and evaluation to inform improvement
Critical to all improvement efforts is the need to know whether the changes made have resulted in the desired improvement, and what other intended or unintended consequences the changes have resulted in. It is also desirable to know how an initiative has achieved improvements, to support effective implementation, and learn how to reproduce success in other settings. For instance, theory and methods developed by Walter Shewhart have been used effectively to inform and support improvement efforts (25, 26). This approach differs from statistical approaches more traditionally used in research, such as frequentist hypothesis testing, in accepting and quantifying the variation inherent to the messy reality of health systems, rather than attempting to isolate one cause of variation, enabling teams to identify important signals in data in close to real time, to inform and support improvement efforts. Existing methods of measurement and evaluation are often poorly used, and frequently do not answer the salient questions (25). Teams working to improve care typically do not have the necessary skills to set up a robust measurement approach, and often end up collecting or extracting data that is inadequate to address the above needs. It is necessary to understand how to develop measurement training, support and infrastructure required to operate such approaches in routine healthcare practice (27). Further work is also needed to advance methodology capable of evaluating complex interventions in complex systems that enable timely and reliable assessment of system performance. It is also necessary to learn how best to report and synthesise evaluations to support future improvement efforts (28, 29), and to establish the best approaches to share learning and experiences between settings (30).
The areas in this cluster are closely related—improvement initiatives and research studies need to be conducted within existing healthcare systems to understand how improvements will be integrated into routine care, and how they compete against other priorities and workstreams. Leaders who select improvement goals and approaches need to work with what is already present in the system (skills, capacity, resources, experience, relationships, tensions). They need to understand the culture and context for improvement, including past experiences and their results, within each setting. While these areas are closely related, tensions can also exist between them. For example, evaluation and measurement agendas can conflict with improvement when the launch of an intervention is prioritised over establishing a clear baseline.
Cluster 2—aligning improvement efforts
The interdependence of system levels
As well as considering the requirements of any individual improvement effort it is necessary to consider improvement efforts within the wider health system. Any specific initiatives are part of a wider system that is influenced at individual, micro- (team or department), meso- (organisation) and macro-system (policy and regulation) levels (31). Initiatives targeting one level of the system will interact with other initiatives and other system levels. While some may be aligned, the misalignment of others causes tension and duplication which is often experienced most acutely by those at the sharp end of care delivery (11). Work is required in practice and research to understand the complex array of initiatives taking place and to inform the orchestration of such alignment, balancing the need for entrepreneurship and coordinated direction.
The interactional work of improvement
Fundamental to all improvement efforts is the human dimension of change including issues of relationships, trust, and motivation to change. These issues are critical for successful improvement but are often under recognised in teaching, planning and evaluation of improvement approaches. The interpersonal and interactive aspects of improvement often require skills such as negotiation, facilitation, building relationships and the ability to create a trusting environment (32). These are essential for sharing knowledge, seeking agreement, changing behaviours, and challenging the status quo resulting from organisational hierarchies and vested interests (33). It is necessary to understand the time, skill and support required for the interactional work of improvement, and the implications this has for the design, conduct and evaluation of improvement initiatives, improvement approaches, and research studies.
Enhancing the value of improvement practice and research
An important consideration for the improvement community is where to invest resources. Not all improvement or research activities are of equal value and some may be wasteful or harmful (34). Given the finite resources in terms of time, capacity and expertise, these need to be used as effectively as possible. Effective use of resources needs to be considered within individual improvement initiatives and research studies, within organisations, and across the whole system that influences healthcare improvement (35). Study designs that can address system complexity and learn from multiple variables in single studies need to be more extensively deployed (36). There is a need to understand what resources are already in place, how the value of investments can be assessed, and how to disincentive low value or duplicative work whilst incentivising high value, synergistic work.
The three areas in this cluster have the potential to facilitate or hinder any improvement approach depending on whether they are aligned with, or disruptive to, “normal” work.
Cluster 3—advancing the contribution of the improvement community
Seeking synergies between knowledge, research, and practice to achieve improvement
The two-way relationship between research and practice is critical in advancing contributions from the improvement community. However, currently practitioners and researchers tend to work in relative isolation from each other and there is a recognised gap between the production of evidence and new knowledge and its use in practice (37). Practitioners rarely have the time or inclination to keep up to date with the latest research findings, and researchers typically design their studies to address issues of academic interest rather than practical importance. There is a need to understand how best to achieve synergy between research and practice and to learn what active approaches are needed to support the mobilisation of knowledge into changes in practice (38). Improved infrastructure, development of new roles and career pathways, and incentives to enhance relationships and partnerships could benefit everyone: practitioners could benefit from access to knowledge to inform improvement attempts, and researchers need access to practice settings where improvement efforts take place to generate useful new knowledge (39). Such access enables two-way exchange of needs, ideas and theories to inform future improvement efforts, and to generate refined theories, actionable findings, and ultimately to improve the quality of patient care.
Ways of knowing and doing
Advancing the contribution of the improvement community depends on how well people are able to work together when they come from diverse backgrounds, disciplines and specialities. This depends on understanding how collaboration can take place between people who hold different world views and perspectives, who work to different standards, and prioritise different outputs and outcomes. Differences between stakeholders in ways of knowing and doing can make such synergies challenging to achieve (40). Particular fields have well founded traditions of enquiry that have enabled knowledge generation within them—as exemplified by debate regarding the hierarchy of evidence and the role of randomised controlled trials in improvement (7, 41)—but these traditions may hinder exchange of knowledge between fields. For example, quality improvement approaches tend to emphasise the importance of building local capacity and drawing on internal knowledge and expertise to guide improvement efforts whilst implementation science approaches tend to rely on external expertise to design and then disseminate interventions. These differences in perspective reflect distinctions in the origins and philosophy of each approach regarding what types of knowledge are valued and the extent to which people working in the system are viewed as having agency or requiring assistance. Whilst both quality improvement and implementation science have value to offer the improvement community, these fundamental differences can create tension and conflict between different perspectives. It is important that such philosophical distinctions are understood and valued to facilitate meaningful dialogue and exchange between different disciplines and perspectives. It takes time to build a depth of understanding and appreciation of how different disciplines and approaches can work together for the benefit of the improvement community, and this can be supported by reflective practice and empirical enquiries to explore the benefits and limitations of different approaches.
Building the community
Building a community that is skilled in improvement practice and research, and able to converse across diverse professional, patient and academic perspectives, is critical. The complexity of healthcare improvement makes contributions from a diverse range of disciplines valuable, but also challenging to teach, study and learn (42). Many questions remain around how to build such capacity and capability. For example, it is not yet clear what breadth and depth of improvement knowledge and competencies are optimal across a healthcare system, or how best to develop and distribute expertise across the workforce. There is also a need to understand how to build career pathways for the improvement community, and how these fit with existing pathways in healthcare organisations, academia, and policy. If the improvement community is going to extend its contribution outside of dedicated specialists and aficionados it must be able to communicate the value of the field to external stakeholders including politicians, funders, healthcare leaders. Tackling this issue is important for the future of improvement and, therefore, should influence the design of communication, education and professional development for academics, practitioners, local and system leaders, policy makers, patients and members of the public (43).
Distinguishing features of improvement science
We propose there are four features that collectively define and distinguish the field of improvement science: the conceptualisation of health services as complex social systems; the promotion of a holistic person and system perspective; a focus on the practical applicability of knowledge; and the acknowledgement of both the necessity and challenges of engaging people from diverse backgrounds to collaborate.
These distinguishing features, whilst they might individually share overlaps with other fields of study, collectively start to illustrate the scope of interest and nature of enquiry of improvement science field in transcending traditional boundaries of academic and health service practices.
First, as illustrated by the ten areas of enquiry, improvement science conceptualises health services as complex social systems, defined by the agency of people within the system, the interconnectedness of system parts, and the dynamics of people and systems that change over time and are influenced by historic events (44).
Second, and as a consequence of adopting a complex systems view, improvement science encourages a move away from the relative comfort of focusing on single issues, interventions or aspects of quality at a time, or working in controlled or remote environments—as often practiced by academics, innovators, policy makers and service planners—towards a holistic view of how different aspects of the system work together in routine practice. In doing so, improvement science promotes a holistic person and system perspective, viewing the system as it is experienced by those embedded in the system, namely the staff who deliver and the people who receive health services (45). By placing primacy on the perspective of those embedded in the systems it is necessary to recognise that work is often conducted in imperfect and high-pressured environments, with competing demands and priorities that cannot easily be resolved. Central to adopting a holistic system perspective is the recognition of the causes and consequences of variation, and how these can be understood and responded to (26).
Third, the practical relevance and application of knowledge is a central concern. Knowledge about how to improve any given system can only emerge from intervening in the system and learning from and responding to what emerges (46). Improvement science must move beyond descriptions of enablers and barriers, and demonstrations of one-off successes or isolated pockets of excellence, to clearly show how such knowledge can be applied to achieve improvements reliably and equitably across diverse contexts and settings. In doing so improvement places greater emphasis on the practical and context specific issues of translating, mobilising and applying knowledge, than in any inherent value of knowledge in its own right. Advances in how we can improve the way we improve require a critical exploration of the relationships between knowledge and practice, between academic and healthcare organisations, and between science and society.
Finally, as the breadth of the improvement landscape indicates, an enormous range of knowledge and expertise is required to advance the understanding and practice of improvement. Meaningful progress—where we are learning from each other and building on prior evidence and experience—depends heavily upon collaboration and co-production. However, it is important to acknowledge both the necessity and challenges of engaging people from diverse backgrounds to work together collaboratively. Whilst each area of enquiry in the improvement landscape is of importance, we believe the need to collaborate to collectively address the breadth of issues in a synergistic manner is the greatest challenge of all. Knowing that different areas of expertise exist is a start, but truly valuing and understanding diverse and often conflicting perspectives, and the ability to communicate across (professional and disciplinary) language and cultural barriers to build trusting and respectful relationships is required if we are to work synergistically across the improvement landscape.
Where next for practice and research?
To our knowledge this is the first attempt to outline the breadth of areas of enquiry that are of importance to the improvement community and the field of improvement science. We believe this outline serves as a foundation stone for defining the breadth and interests of the field, and for further exploring how it overlaps with and is distinguished from other fields of study and practice.
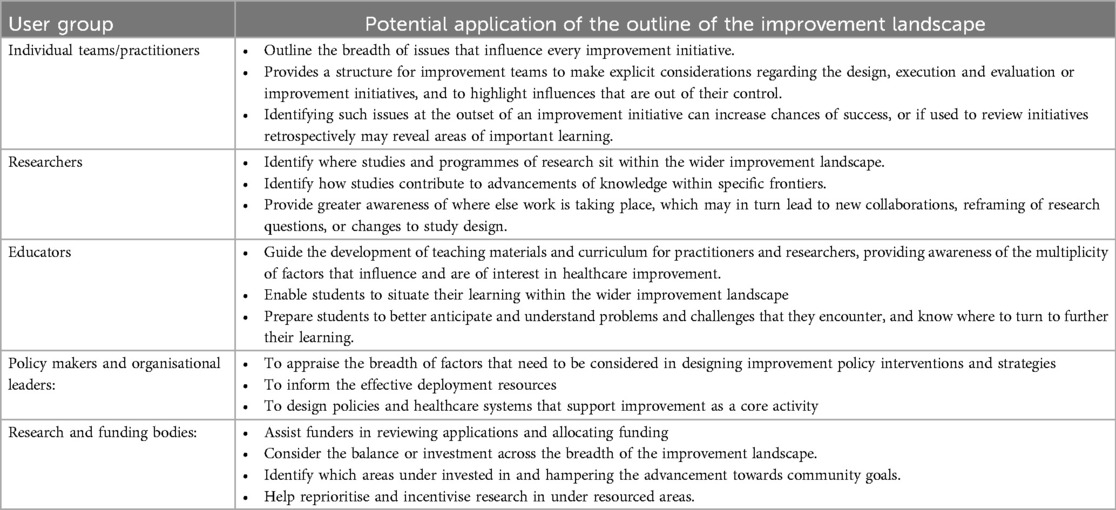
Bringing the breadth of areas of enquiry together into a single outline highlights the diverse experience and expertise required to achieve improvements in practice, align improvement efforts, and advance the contribution of the improvement community. Whilst each of the areas, clusters and questions presented maybe very familiar to some people, there are very few people who are expert or even conversant in all of the areas presented. In this respect, we hope this paper can act as a call to the improvement community to look beyond their traditional areas of interest and to start to explore how insights and expertise from different areas can support and enhance each other, and in turn advance the study and practice of healthcare improvement. The potential applications of the outline of the improvement landscapes for different user groups is considered in Table 2.
We invite others to refine and advance mapping of the improvement landscape by identifying additional gaps and increasing contributions from diverse perspectives. We recognise the limitation that the authors provide a European and North American perspective and, whilst international conference communities were engaged in its development, the work would be enhanced by further exploration from wider geographical and sociodemographic perspectives.
We hope the outline of the improvement landscape starts to provide a common language for the diverse improvement community, enabling people to transcend disciplinary interests and constraints, and to consider how, collectively, we can improve health and care.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
JR: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Visualization, Writing – original draft, Writing – review & editing. GA: Data curation, Formal Analysis, Investigation, Project administration, Software, Visualization, Writing – original draft, Writing – review & editing. NA: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. GB: Conceptualization, Data curation, Formal Analysis, Investigation, Writing – original draft, Writing – review & editing. SC: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. KH: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. DH: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. YJ: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. LP: Conceptualization, Data curation, Formal Analysis, Investigation, Writing – original draft, Writing – review & editing. MR: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. CS: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. JT: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. SW: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. TW: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Software, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by a Health Foundation grant for advancing the frontiers of improvement science. JR, NA, SC, DH, YJ, SW, TW were supported by a Health Foundation Improvement Science Fellowships. KPH, MR, JT were supported by Vinnvard Improvement Science Fellowships. This research was supported by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care Northwest London (CLAHRC NWL), now recommissioned as NIHR Applied Research Collaboration Northwest London (ARC NWL). The views expressed in this publication are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care.
Acknowledgments
The authors thank Paul Batalden for his help with the manuscript editorial process.
Conflict of interest
Author JR is the director of Julie Reed Consultancy Ltd. Author LP was employed by company Associates in Process Improvement.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frhs.2024.1454658/full#supplementary-material
References
1. Health in the 2030 Agenda for Sustainable Development. Sixty-Ninth World Health Assembly. (2016). Available online at: https://apps.who.int/gb/ebwha/pdf_files/WHA69/A69_R11-en.pdf (cited September 1, 2022).
2. Rouse J. Knowledge and Power: Toward a Political Philosophy of Science. Ithaca: Cornell University Press (1987). p. 31–2.
3. Lemire S, Christie CA, Inkelas M. The methods and tools of improvement science. In: Christie CA, Inkelas M, Lemire S, editors. Improvement Science in Evaluation: Methods and Uses. Hoboken, NJ: New Directions for Evaluation (2017) 153. p. 23–33.
4. Langley GJ, Moen RD, Nolan KM, Nolan TW, Norman CL, Provost LP. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. 2nd ed. San Francisco: Wiley (2009).
5. Fischbacher CM, Lewsey J, Muirie J, McCartney G. A critical reflection on the use of improvement science approaches in public health. Scand J Public Health. (2022) 50(3):389–94. doi: 10.1177/1403494821990245
6. Institute for Healthcare Improvement. Improvement Capability. Available online at: https://www.ihi.org/improvement-areas/improvement-capability (cited June 21, 2024).
7. Berwick DM. The science of improvement. JAMA. (2008) 299(10):1182–4. doi: 10.1001/jama.299.10.1182
8. Marshall M, Pronovost P, Dixon-Woods M. Promotion of improvement as a science. Lancet. (2013) 381(9864):419–21. doi: 10.1016/S0140-6736(12)61850-9
9. Nilsen P, Thor J, Bender M, Leeman J, Andersson-Gäre B, Sevdalis N. Bridging the silos: a comparative analysis of implementation science and improvement science. Front Health Serv. (2021) 1:817750. doi: 10.3389/frhs.2021.817750
10. Cribb A. Improvement science meets improvement scholarship: reframing research for better healthcare. Health Care Anal. (2018) 26(2):109–23. doi: 10.1007/s10728-017-0354-6
11. Perla RJ, Provost LP, Parry GJ. Seven propositions of the science of improvement: exploring foundations. Qual Manag Health Care. (2013) 22(3):170–86. doi: 10.1097/QMH.0b013e31829a6a15
12. Junghans T. “Don’t mind the gap!” reflections on improvement science as a paradigm. Health Care Anal. (2018) 26(2):124–39. doi: 10.1007/s10728-017-0353-7
13. WHO. Quality of care. Available online at: https://www.who.int/health-topics/quality-of-care#tab=tab_1 (cited September 1, 2022).
14. Wells S, Tamir O, Gray J, Naidoo D, Bekhit M, Goldmann D. Are quality improvement collaboratives effective? A systematic review. BMJ Qual Saf. (2018) 27(3):226–40. doi: 10.1136/bmjqs-2017-006926
15. Taylor MJ, McNicholas C, Nicolay C, Darzi A, Bell D, Reed JE. Systematic review of the application of the plan–do–study–act method to improve quality in healthcare. BMJ Qual Saf. (2013) 23(4):290–8. doi: 10.1136/bmjqs-2013-001862
16. Institute of Medicine (US) Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington (DC): National Academies Press (US) (2001). Available online at: http://www.ncbi.nlm.nih.gov/books/NBK222274/ (cited February 1, 2022).
17. Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. (2014) 12(6):573–6. doi: 10.1370/afm.1713
18. Organization WH. Monitoring the Building Blocks of Health Systems: A Handbook of Indicators and Their Measurement Strategies. Geneva: World Health Organization (2010).
19. Dixon-Woods M. How to improve healthcare improvement-an essay by mary dixon-woods. Br Med J. (2019) 367:l5514. doi: 10.1136/bmj.l5514
20. Lennox L, Maher L, Reed J. Navigating the sustainability landscape: a systematic review of sustainability approaches in healthcare. Implement Sci. (2018) 13(1):27. doi: 10.1186/s13012-017-0707-4
21. Walshe K. Pseudoinnovation: the development and spread of healthcare quality improvement methodologies. Int J Qual Health Care. (2009) 21(3):153–9. doi: 10.1093/intqhc/mzp012
22. Reed JE, Kaplan HC, Ismail SA. A new typology for understanding context: qualitative exploration of the model for understanding success in quality (MUSIQ). BMC Health Serv Res. (2018) 18(1):584. doi: 10.1186/s12913-018-3348-7
23. Radnor ZJ, Holweg M, Waring J. Lean in healthcare: the unfilled promise? Soc Sci Med. (2012) 74(3):364–71. doi: 10.1016/j.socscimed.2011.02.011
24. Reed JE, Howe C, Doyle C, Bell D. Simple rules for evidence translation in complex systems: a qualitative study. BMC Med. (2018) 16(1):92. doi: 10.1186/s12916-018-1076-9
25. Thor J, Lundberg J, Ask J, Olsson J, Carli C, Härenstam KP, et al. Application of statistical process control in healthcare improvement: systematic review. BMJ Qual Saf. (2007) 16(5):387–99. doi: 10.1136/qshc.2006.022194
26. Shewhart WA. The Economic Control of Quality of Manufactured Product. New York: D Van Nostrand (1931).
27. Portela MC, Pronovost PJ, Woodcock T, Carter P, Dixon-Woods M. How to study improvement interventions: a brief overview of possible study types. BMJ Qual Saf. (2015) 24(5):325–36. doi: 10.1136/bmjqs-2014-003620
28. Ferlie EB, Shortell SM. Improving the quality of health care in the United Kingdom and the United States: a framework for change. Milbank Q. (2001) 79(2):281–315. doi: 10.1111/1468-0009.00206
29. Goodman D, Ogrinc G, Davies L, Baker GR, Barnsteiner J, Foster TC, et al. Explanation and elaboration of the SQUIRE (standards for quality improvement reporting excellence) guidelines, V.2.0: examples of SQUIRE elements in the healthcare improvement literature. BMJ Qual Saf. (2016) 25(12):e7. doi: 10.1136/bmjqs-2015-004480
30. Lennox L, Barber S, Stillman N, Spitters S, Ward E, Marvin V, et al. Conceptualising interventions to enhance spread in complex systems: a multisite comprehensive medication review case study. BMJ Qual Saf. (2022) 31(1):31–44. doi: 10.1136/bmjqs-2020-012367
31. Øvretveit J, Leviton L, Parry G. Increasing the generalisability of improvement research with an improvement replication programme. BMJ Qual Saf. (2011) 20(1):i87–91. doi: 10.1136/bmjqs.2010.046342
32. Rycroft-Malone J, Seers K, Chandler J, Hawkes CA, Crichton N, Allen C, et al. The role of evidence, context, and facilitation in an implementation trial: implications for the development of the PARIHS framework. Implement Sci. (2013) 8(1):28. doi: 10.1186/1748-5908-8-28
33. Davies H, Powell A, Rushmer R. Why don’t clinicians engage with quality improvement? J Health Serv Res Policy. (2007) 12(3):129–30. doi: 10.1258/135581907781543139
34. Dixon-Woods M, Martin G. Does quality improvement improve quality? (2016). Available online at: https://www.repository.cam.ac.uk/handle/1810/260182 (cited February 1, 2022).
35. Shiell A, Hawe P, Gold L. Complex interventions or complex systems? Implications for health economic evaluation. Br Med J. (2008) 336(7656):1281–3. doi: 10.1136/bmj.39569.510521.AD
36. Neuhauser D, Provost SM, Provost LP. It is time to reconsider factorial designs: how Bradford Hill and R. A. Fisher shaped the standard of clinical evidence. Qual Manag Health Care. (2020) 29(2):109–22. doi: 10.1097/QMH.0000000000000243
37. Westerlund A, Sundberg L, Nilsen P. Implementation of implementation science knowledge: the research-practice gap paradox. Worldviews Evid Based Nurs. (2019) 16(5):332–4. doi: 10.1111/wvn.12403
38. Blanco-Mavillard I, Bennasar-Veny M, De Pedro-Gómez JE, Moya-Suarez AB, Parra-Garcia G, Rodríguez-Calero MÁ, et al. Implementation of a knowledge mobilization model to prevent peripheral venous catheter-related adverse events: PREBACP study—a multicenter cluster-randomized trial protocol. Implement Sci. (2018) 13(1):100. doi: 10.1186/s13012-018-0792-z
39. Davidoff F, Dixon-Woods M, Leviton L, Michie S. Demystifying theory and its use in improvement. BMJ Qual Saf. (2015) 24(3):228–38. doi: 10.1136/bmjqs-2014-003627
40. Brown JS, Duguid P. Organizational learning and communities-of-practice: toward a unified view of working, learning, and innovation. Organization Sci. (1991) 2(1):40–57. doi: 10.1287/orsc.2.1.40
41. Auerbach AD, Landefeld CS, Shojania KG. The tension between needing to improve care and knowing how to do it. N Engl J Med. (2007) 357(6):608–13. doi: 10.1056/NEJMsb070738
42. McNicholas C, Lennox L, Woodcock T, Bell D, Reed JE. Evolving quality improvement support strategies to improve plan-do-study-act cycle fidelity: a retrospective mixed-methods study. BMJ Qual Saf. (2019) 28(5):356–65. doi: 10.1136/bmjqs-2017-007605
43. Lucas B. Getting the improvement habit. BMJ Qual Saf. (2016) 25(6):400–3. doi: 10.1136/bmjqs-2015-005086
44. Greenhalgh T, Papoutsi C. Studying complexity in health services research: desperately seeking an overdue paradigm shift. BMC Med. (2018) 16(1):95. doi: 10.1186/s12916-018-1089-4
45. Reed JE, Green S, Howe C. Translating evidence in complex systems: a comparative review of implementation and improvement frameworks. Int J Qual Health Care. (2019) 31(3):173–82. doi: 10.1093/intqhc/mzy158
Keywords: improvement science, quality improvement, healthcare, complex system, implementation sceince, patient safety, knowledge mobilisation
Citation: Reed JE, Antonacci G, Armstrong N, Baker GR, Crowe S, Harenstam KP, Hargreaves D, Jani YH, Provost L, Rejler M, Savage C, Thor J, Williams S and Woodcock T (2025) What is improvement science, and what makes it different? An outline of the field and its frontiers. Front. Health Serv. 4:1454658. doi: 10.3389/frhs.2024.1454658
Received: 26 June 2024; Accepted: 24 December 2024;
Published: 20 February 2025.
Edited by:
Nick Sevdalis, National University of Singapore, SingaporeReviewed by:
Frances Revere, University of Florida, United StatesCopyright: © 2025 Reed, Antonacci, Armstrong, Baker, Crowe, Harenstam, Hargreaves, Jani, Provost, Rejler, Savage, Thor, Williams and Woodcock. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Julie E. Reed, anVsaWUucmVlZEBqdWxpZXJlZWRjb25zdWx0YW5jeS5jb20=
†Present Addresses: Julie E. Reed, Högskolan i Halmstad, Halmstad, Sweden
Natalie Armstrong, School of Health & Medical Sciences, City St George's, University of London, London, United Kingdom
‡Deceased
 Julie E. Reed
Julie E. Reed Grazia Antonacci
Grazia Antonacci Natalie Armstrong4,†
Natalie Armstrong4,† Yogini H. Jani
Yogini H. Jani Carl Savage
Carl Savage Johan Thor
Johan Thor Sharon Williams
Sharon Williams Thomas Woodcock
Thomas Woodcock