
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Health Serv. , 17 October 2024
Sec. Implementation Science
Volume 4 - 2024 | https://doi.org/10.3389/frhs.2024.1405426
 Kathleen Pajer1,2,3*
Kathleen Pajer1,2,3* Christina Honeywell1,2
Christina Honeywell1,2 Heather Howley2
Heather Howley2 Nicole Sheridan2
Nicole Sheridan2 Will Affleck2,3
Will Affleck2,3 Ivan Terekhov2
Ivan Terekhov2 Dhenuka Radhakrishnan2,4,5
Dhenuka Radhakrishnan2,4,5
Background: The precision child and youth mental health (PCYMH) paradigm has great potential to transform CYMH care and research, but there are numerous concerns about feasibility, sustainablity, and equity. Implementation science and evaluation methodology, particularly participatory logic models created with stakeholders, may help catalyze PCYMH-driven system transformation. This paper aims to: (1) report results of a PCYMH logic model scoping review; (2) present a case study illustrating creation of a participatory logic model for a PCYMH start-up; and (3) share the final model plus lessons learned.
Methods: Phase 1: Preparation for the logic model comprised several steps to develop a preliminary draft: scoping review of PCYMH logic models; two literature reviews (PCYMH and implementation science research); an environmental scan of our organization's PCYMH research; a gap analysis of our technological capability to support PCYMH research; and 57 stakeholder interviews assessing PCYMH perspectives and readiness. Phase 2: Participatory creation of the logic model integrated Phase 1 information into a draft from which the final logic model was completed through iterative stakeholder co-creation.
Results: Phase 1: The scoping review identified 0 documents. The PCYMH literature review informed our Problem and Impact Statements. Reviewing implementation and evaluation literature resulted in selection of the Reach, Effectiveness, Adoption, Implementation, Maintenance (RE-AIM) and Behavior Change Wheel (BCW) frameworks to guide model development. Only 1.2% (5/414) of the organization's research projects involved PCYMH. Three technological infrastructure gaps were identified as barriers to developing PCYMH research. Stakeholder readiness interviews identified three themes that were incorporated into the draft. Phase 2: Eight co-creation cycles with 36 stakeholders representing 13 groups and a consensus decision-making process were used to produce the final participatory logic model.
Conclusions: This is the first study to report the development of a participatory logic model for a PCYMH program, detailing involvement of stakeholders from initial planning stages to the final consensus-based product. We learned that creating a participatory logic model is time- and labour-intensive and requires a multi-disciplinary team, but the process produced stakeholder-program relationships that enabled us to quickly build and implement the PCYMH start-up. Our processes and final model can inform similar efforts at other sites.
Child and youth mental health (CYMH) disorders are a significant public health problem. Worldwide, one out of seven 10–19- year-olds experiences a mental health disorder worldwide, accounting for 13% of the global burden of disease in this age group, whilst suicide is the fourth leading cause of death among 15–19 year-olds (1). Mental health care is insufficient to meet these needs in most parts of the world (2–5).
More concerning is that CYMH care, even when received, is not effective for many patients (6). Although the use of evidence-based CYMH psychotherapeutic treatments has grown, there has been no improvement, and for some of these treatments, a decline in effectiveness over time (7).
The same problems are increasingly reported with psychopharmacologic treatments. For example, a recent network meta-analysis of antidepressant medication efficacy in children and youth with depressive disorder reported “Most antidepressants may be associated with a “small and unimportant” reduction in depression symptoms on the CDRS-R scale (range 17 to 113) compared with placebo.” (8). The authors noted that there were likely sub-groups of patients for whom these medications were very effective, but others who received little symptom relief. Similarly, only 55%–60% of adolescents with anxiety disorders achieve remission with medication (9).
Transformation, not incremental change, in CYMH care and research is urgently needed (10). Precision health, which aims to tailor care to the individual's biological (e.g., genomic, metabolic, or neuroimaging biomarkers), lifestyle, psychological, and environmental characteristics holds great promise as a transformational paradigm (11–13). Each person's unique profile on these factors is matched with diagnosis, prognosis, or treatment based on research findings from stratification of large heterogeneous samples into homogenous sub-groups based on outcomes, not just symptoms. However, skepticism and concerns abound regarding the validity, feasibility, ethics, equity, and cost of precision child and youth mental health (PCYMH) care and research (14–16).
Moreover, transformation could easily fail in CYMH care systems that are already complex, i.e., containing multiple competing interdependent components and dysfunctional. To promote success and sustainability of transformation, it is imperative that leaders incorporate best practices from fields of implementation science and evaluation when developing PCYMH programs to improve care or research (17, 18). Furthermore, disseminating the program work they do is a vital component of systems transformation (19).
Logic models are the core of program implementation and evaluation. They are high-level graphic representations of the work to be done, although model structure and components vary by logic model type (20). They serve multiple purposes, e.g., a roadmap for program work and outcomes, a guide for evaluation of program success, or a visual tool to communicate with stakeholders and funders (20). Logic models are associated with more efficient and effective programs, including when used in CYMH settings (21–24).
Many program logic models are created by leaders and program planners or implementation experts, often with confirmatory stakeholder input obtained near the end of the process. In contrast, a participatory logic model engages stakeholder groups from the beginning and works with them throughout to co-create the model. This process increases engagement and outcome delivery, as well as contributes unique perspectives and ideas through the continuous collaboration on inputs, activities, outputs, and outcomes (25–28). Moreover, participatory logic models have been associated with greater effectiveness in outcomes in complex settings such as healthcare systems (29).
In 2022, the CHEO Research Institute (RI) in Ontario, Canada received donor funding to build the foundation for data-driven discovery and clinical PCYMH care through an 18-month start-up, called the PCYMH Initiative (PCYMHI). The RI is attached to CHEO, a 167-bed pediatric academic tertiary care hospital in Eastern Ontario. The RI and hospital are affiliated with the University of Ottawa.
To ensure optimal effectiveness and efficiency in a short period of time, we developed a participatory logic model to guide the PCYMHI build. The goals of this paper are to:
1. Report the results of a scoping review on PCYMH logic models.
2. Present a case study of the process involved in creating the PCYMHI participatory logic model.
3. Share the final model and lessons learned to aid other organizations in developing participatory PCYMH program logic models.
This case study of logic model development was done in two phases: Phase 1 - Preparation for logic model development and Phase 2 - Participatory creation of the final logic model. The project was run by a three-person core working group (KP, CH, and HH), intentionally small for efficiency and agility. However, co-authors participated in myriad tasks on the project and two evaluation consultants assisted with part of the work (SS and DH, see Acknowledgements). This project was deemed continuous quality improvement by the RI Research Ethics Board, not requiring Board review.
This phase was organized around six questions to inform design of the preliminary draft of the model for Phase 2 work. Table 1 lists the six questions, methods used to answer them, and how the information was used. Each of the components of Phase 1 are briefly described in the following sections.
We conducted a scoping review of the literature to investigate whether any other programs doing PCYMH care or research had disseminated information about their logic model (Table 1, question 1). Scoping reviews are designed to 1) identify and characterize studies to determine feasibility of a systematic review, 2) summarize how research has been conducted, 3) identify factors affecting findings, 4) delineate research gaps, and 5) present recommendations for researchers (30). We adhered to the Joanna Briggs Institute structure for scoping reviews (31) and followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses-Scoping Reviews (PRisMA-ScR) guidelines, as detailed in the PRisMA-ScR checklist (Supplementary Table S1) (32).
Our search strategy (Supplementary Table S2) used terms mapping onto constructs of age (e.g., “child”, “youth”, “adolescent”); mental health (e.g., “mental health”, “behavioral health”, “psychiatry”); precision health, (e.g., “precision health”, “precision medicine”); and “logic model”. Medical Subject Headings (MeSH terms) and keywords were incorporated into the strategy. Searches were conducted in PubMed and Embase from 1946 – March 3, 2023 and updated on August 15, 2023. Retrieved documents were combined to yield a dataset which has been shown to comprise academic publications, conferences, published abstracts, and books (33).
Eligibility criteria were established a priori to identify documents with the following characteristics: (1) description of a precision medicine or precision health logic model; (2) focus on mental health, psychiatry, or behavioural health; (3) focus on children or youth (0–23 years of age); and (4) written in English. There were no restrictions on study location, year of publication, or type of document. We planned to conduct blinded two-person abstract, title, and document reviews, followed by full text review for any documents meeting inclusion criteria. We then planned to synthesize the information from the final document data extraction. Disagreements were to be handled by consensus.
We conducted informal systematic reviews of two additional bodies of literature through PubMed searches (Table 1, questions 2 & 3). The first pertained to PCYMH, which informed the Problem and Impact Statements for the PCYMHI build. Such statements are critical for a program to determine its goals and shape the overall direction for a logic model (20).
The second review investigated the implementation science and evaluation research published to date to select a type of logic model (20) and an implementation framework, theory, or model (34). This selection process was guided by five questions suggested for this purpose by Lynch and colleagues (35): (1) Why? (your program aim); (2) Who? (individuals, groups, or organizations affected); (3) What? (what will be done & resources needed); (4) When? (timeframe for planning, implementation, & evaluation); and (5) How? (data sources). In synthesizing this literature to make our decisions, we prioritized institutional expectations that PCYMHI outcomes would be delivered within 18 months.
An environmental scan (Table 1, question 4) was conducted to determine the number of active PCYMH research projects at the CHEO RI using the institution's grant administration database (ROMEO, https://www.processpathways.com/). Similar information about PCYMH-related clinical services, improvement projects, or clinical research at the hospital was solicited through an online survey emailed to department leaders.
The Technical and Medical Directors of the RI Informatics Core assessed the extant hardware, software, cloud, and personnel infrastructure components in a gap analysis to determine the capacity and readiness to develop PCYMH research (Table 1, question 5). They benchmarked our infrastructure with comparable Canadian healthcare research institutes working towards similar goals.
Identifying our stakeholders and understanding their views on PCYMH and readiness for this paradigm (Table 1, question 6) was crucial. Engaging them at the start of the model development process was essential for creating a participatory logic model. To that end, using a combination of purposive and snowball sampling strategies, the core working group invited 58 stakeholders to 18 virtual meetings.
Eleven stakeholder groups were represented: (1) Research Administrators, e.g., of the RI Informatics Core, the Clinical Research Unit; (2) PCYMH Researchers; (3) RI Leaders of relevant research programs, e.g., Genetics; (4) Outside Research Organizations; (5) the RI Healthcare Innovation Program; (6) Mental Health (MH) Clinical Researchers; (7) Clinicians; (8) Clinical Managers; (9) MH Program Administrators; (10) Youth MH Peer Support Group Leaders; and (11) Community Mental Health Agencies. The groups were selected because they comprised people or organizations impacted by PCYMHI, e.g., researchers and clinicians, or could contribute to PCYMHI as Inputs in the model, e.g., the RI Informatics Core. We did not include patients or caregivers in this phase, as we were focused on collecting internal and external organizational information.
The core working group used a semi-structured interview to gather information about PCYMH perceived benefits and concerns, suggestions for success, and participants’ “wish” lists for improving CYMH research or care. This method was selected to put people at ease and balance rapport-building with data collection in brief (45–60 min) virtual meetings with individuals or small groups (36).
Some of the first participants expressed discomfort in having the video recorded, so we did not tape meetings. Instead, we assigned a scribe to take detailed notes, for which we assured participants anonymity. The notes were then reviewed with participants before concluding each meeting, e.g., “So in summary, what we talked about was...”. Two co-authors (CH and WA) independently used inductive reasoning to informally identify themes in these notes and then used consensus to produce a final list of themes.
The core working group synthesized information from the literature reviews, environmental scan, and gap analysis, integrating this with the themes from the stakeholder interviews to develop a preliminary draft of the logic model. The consultants advised the working group on several revisions of this draft in preparation for stakeholder co-creation of a final logic model. The starting draft for the Phase 2 work was the result of several revisions based on discussion and consensus from the core working group and consultants.
Invitations were sent to 57 stakeholders across 13 groups to participate in the creation of the final logic model. Some of these groups had participated in Phase 1 stakeholder interviews, but new groups were included: youth, caregivers, RI Executive Leaders, Hospital Executive Leaders, PCYMHI-funded researchers, RI and Hospital Core Services, and the RI Foundation. These groups were added now because they would either be directly affected by, e.g., youth, caregivers, or need to contribute to the operationalization of PCYMHI, e.g., RI and Hospital Core Services such as Human Resources and Finance. Among the re-invited stakeholder groups, approximately 30% sent new representatives and the remainder were people who had been interviewed in Phase 1.
The participatory phase work was conducted in focus groups and through email dialogue. Four in-person groups were planned, but a COVID-19 surge with attendant restrictions and high clinical demands thwarted this plan, resulting in two in-person meetings, one virtual, and a transition to email conversations thereafter. The evaluation consultants facilitated the meetings, posing open-ended questions such as “Do you see yourself in this logic model?”, “What would you add or remove from any of the model's components?” and “How can we improve the model?”. Stakeholder input from each meeting or email discussion was incorporated into the subsequent draft. The model was declared complete when participants and the working group reached a consensus.
In addition to recording changes made in each iteration, we also gathered data to examine the content generated during the co-creation process. Our goal was to gain insights into potential issues that could influence behavior changes during implementation. To achieve this, we recorded the sessions, had them professionally transcribed, and combined the information with the email discussions. WA employed inductive reasoning to perform a thematic analysis on all the information, searching for recurring themes.
Our original search strategy identified 0 documents. Therefore, we broadened the search by eliminating the age criterion and 6 documents were identified (see Figure 1). However, after removing 2 duplicates and conducting title and abstract screening of the remaining 4, we again found that 0 documents met inclusion criteria.
Based on our review of the PCYMH literature, we wrote the following PCYMHI Problem and Impact statements (20).
Child and youth mental health disorders are widespread and, if left untreated, can lead to long-term suffering, disability, and even mortality. Unfortunately, up to 50% of patients do not respond to recommended interventions due to inadequate treatment specificity for their needs. This lack of specificity stems from limitations in mental health research methodology, which hinders our ability to (a) understand the interaction between biological, psychosocial, and environmental factors in the development of mental health disorders and (b) discover effective treatments tailored to individual needs.
PCYMHI's overarching goal is to build a foundation for an efficient, effective, and sustainable PCYMH program producing ground-breaking research that is integrated with clinical care transformation to transform the mental health of Ontario's children and youth.
The review of implementation science and evaluation literature, combined with the requirement for quick delivery of outcomes, led us to select an outcomes type of logic model (20). To ensure a logic model relevant to program planning, implementation and evaluation, we chose the Reach, Effectiveness, Adoption, Implementation, and Maintenance (RE-AIM) framework (https://re-aim.org/). This decision was guided by criteria developed in a study of how > 200 implementation scientists choose implementation frameworks, theories, or models (37). The selection criteria most relevant to our needs were an implementation framework, theory, or model that: (1) would accommodate multiple analytic levels, e.g., individuals, teams, services; (2) had logical relationships between components; (3) provided utilization guidance; (4) had good empirical support; (5) was outcomes-focused; (6) provided a structure for program planning, implementation, and evaluation; (7) was easy for stakeholders to understand; and (8) included behavior change-driven Activities and Outputs.
In use since 1999 (38), the RE-AIM framework provides a planning, implementation, and evaluation structure that can lead to a value-based, pragmatic, outcomes-oriented logic models and programs in which implementation and evaluation are measured from the outset (39). Table 2 displays how each RE-AIM module helped shape components of our logic model.
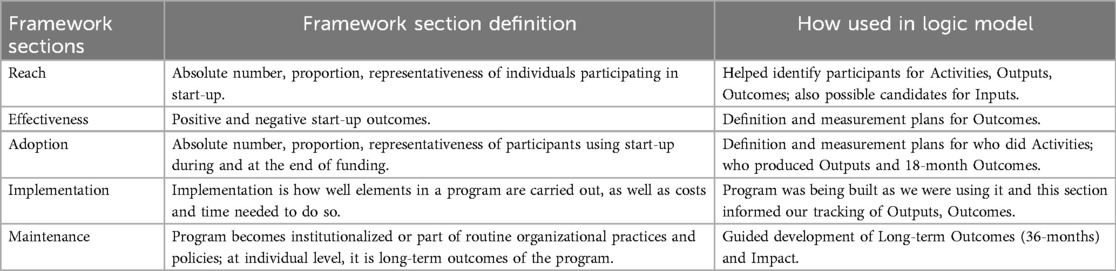
Table 2. Phase 1: reach, effectiveness, adoption, implementation, maintenance (RE-AIM) framework-informed logic model development.
The RE-AIM framework met our criteria well, but given that we needed to change behavior in 18 months and that behaviour change is necessary for successful implementation (40), we wanted additional focus on this construct. The need to use more than one implementation framework, theory or model in planning a program and its logic model is not unusual and actually encouraged (41).
Therefore, to help us plan Activities grounded in behaviour science research, we also used the Behavior Change Wheel (BCW) framework (42, 43). Using a structured approach, the BCW posits that behaviour change is a consequence of interactions between Capability (physical and psychological), Opportunity (physical and social), and Motivation (automatic and reflective). To change behaviour of an individual or an organization, we need to operationalize the desired behaviour, define the actor(s), determine the best behavioural facilitator to target, i.e., Capability, Opportunity, Motivation, or some combination, determine the intervention types mapped to the behavioural facilitator targets, and plan intervention content that will match the best intervention types. It is important to optimize the likelihood that the intervention will succeed by evaluating it on Acceptability, Practicability, Effectiveness, Affordability, Side Effects, and Equity (APEASE).
We developed our desired organizational behaviors through the synthesis of the Phase 1 information, (44). Table 3 displays those desired organizational behaviours, who would change, the behavioural facilitator targets involved, the best type of interventions to be used and their definitions, and the interventions we created for the logic model Activities section. The APEASE checklist was used to ensure the activities were implementable.
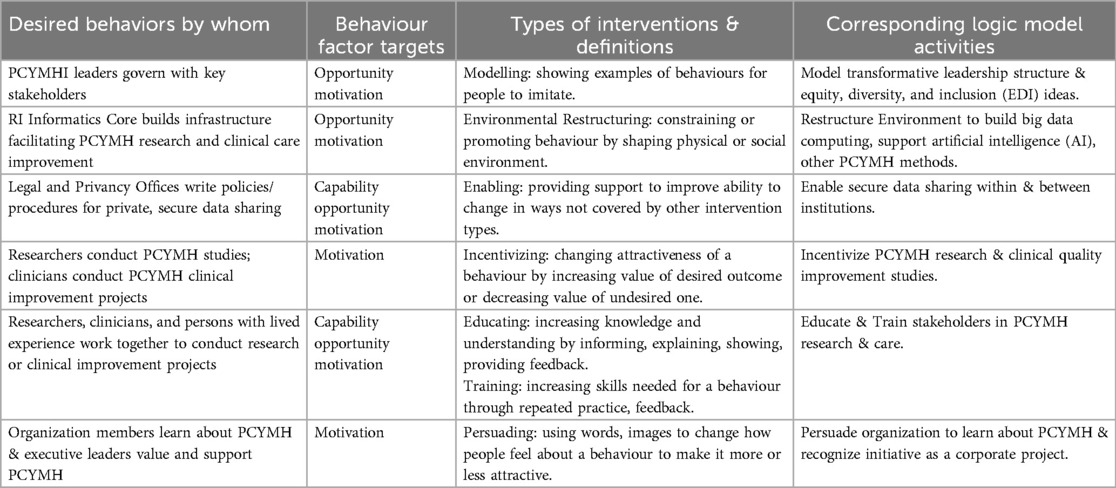
Table 3. Phase 1: behavior change wheel (BCW) - desired organizational behaviours, behaviour targets, intervention types and definitions, corresponding logic model activities.
The combined output of the environmental scan of research revealed that only 1.2% (5/414) of active projects were about PCYMH. Similarly, there was only 1 clinical program using PCYMH methods.
The RI Informatics Core gap analysis identified three key components necessary for the data analytics requirements to facilitate PCYMH research: (1) a robust high-performance computing environment, (2) a dedicated data analytics and computing team skilled in business systems analysis, record extraction, AI data science, and biostatistics to work with electronic health record (EHR) and research data, and (3) a strong partnership between the RI and the hospital for PCYMH research and practice, which could challenge standard privacy and security practices through large-scale, multi-source data sharing or the use of EHR data. To enhance data access and facilitate new data sharing for local projects and external research collaborations, policies and standard operating procedures were needed. These policies would enable collaboration with hospital leadership, clinical care teams, the Research Ethics Board, legal counsel, privacy officers, and the EHR clinical operations team.
Participation in the interviews was high, with 93% (54/58) of invitees attending interviews. Supplementary Table S3 lists the three stakeholder themes extracted about PCYMH readiness and perspectives: Potential Benefits of PCYMH; Barriers to PCYMH implementation; and Ethics Concerns. Participants were generally positive about the PCYMH opportunity, but were skeptical about the validity, feasibility, privacy and ethics. They also worried that the current EHR would be a major barrier because it was neither user-friendly nor set up for measurement-based care. Research concerns were the lack of adequate access to the EHR, lack of artificial intelligence (AI) and data science expertise, and an inadequate computing environment.
In addition, we received many suggestions for optimizing implementation success (Supplementary Table S4), which were grouped into three categories: (1) Engaging Patients and Families; (2) Communications About the PCYMH Program and Progress; and (3) Obtaining Buy-In from Clinicians, Researchers, and Staff.
Of 57 stakeholders invited to give feedback on the logic model draft, 63% (36/57) participated in one or more focus group sessions and email dialogues. Descriptions of the stakeholders are listed in Table 4. At least one representative from every stakeholder group participated. As mentioned in section 2.2, this list differed somewhat from the groups interviewed in the Phase 1, as the task of creating the model differed from determining PCYMH readiness. For example, this work included caregivers and youth, our internal executive sponsors, the CEO of the RI, and the hospital VP for Mental Health and Addictions.
All stakeholder suggestions for each of the 8 iterations were incorporated immediately to create the next iteration until everyone was satisfied by consensus with the final product.
Over the course of the eight versions, the logic model evolved to become more inclusive, sophisticated, and detailed, providing greater clarity to address stakeholder concerns. The final version prominently featured equity, diversity, and inclusion, along with enhanced robustness in outputs and outcomes related to EHR privacy and security, research data sharing, and computing and data analytic infrastructure (Figure 2). Additionally, a unique quadripartite care model that connects patients, clinicians, researchers, and operations personnel emerged from discussions. Table 5 shows two major categories of themes that arose in the analysis of the content of the co-creation process: Potential of PCYMH (3 sub-themes) and Concerns About PCYMH (eight sub-themes).
For example, all stakeholders were enthusiastic about PCYMH and excited about the downstream potential to predict an individual's future mental health problems and public health opportunities for prevention. Stakeholders were also excited by the potential of PCYMH to improve treatment, especially in the use of medications. By offering a more individualized approach, stakeholders felt that PCYMH would significantly improve the current trial-and-error approach to medication, which is both lengthy, and physically and emotionally taxing on patients and their families. A person with lived experience stated:
"Well, I mean, I think for a lot of parents, they very much see that with medication in particular, it’s a trial-and-error thing for getting it right... And, I too have lived experience. So, I’m very much both, you know, someone who has lived that, you know, trying medication, go off of medication, you know, that’s sort of my, part of my story as well.”
Common concerns were related to factors that could undermine the permanent PCYMH program or potentially do harm to patients or families. For example, if one type of PCYMH research relies on data from the EHR, concerns were raised about the quality of data. As one clinician stated:
"I wonder if there’s another activity under Data... not related to the cleaning of the data, but if people don’t trust the data. So, do we need to scrub data? is that a thing?... Or like something about ensuring data quality or develop a process to ensure data quality. Maybe that’s the activity?” And a researcher later voiced, “ What ____ [another participant] was saying is if we’re talking about the validity of the [data] input training, the providers that were talking about EHR, that should, I think, be captured about making it usable. Because it’s not usable if they, you know, put the wrong things in the wrong places.”
An example of concerns about avoiding harm with PCYMH was a theme about sensitivity of personal data, captured well by a comment made by a research administrator:
"One of the things that I’ve learned from ____[another participant], one of our senior scientists, is that we also need to make sure that people feel it’s in their best interest to provide ethnicity [information] because there are a lot of people who feel that it may not be in their interest to raise their hand and say, ‘I’m of this ethnicity or this background.’ So it may just not be as simple as gathering data... just another thing to add a little more complexity...”
Once the logic model was completed, we distributed it to stakeholders and used it to create a PCYMHI dashboard to begin tracking implementation and collecting data for the evaluation.
The purpose of this project was to conduct a scoping review about PCYMH logic models, present the case study of our participatory logic model creation for the PCYMHI, and share our final model and lessons learned to assist others wanting to do the same at their sites.
We were surprised to find no existing logic models for PCYMH program planning in the scientific literature, meeting abstracts, or books. Initially, we thought this might be due to the novelty of focusing on child and youth precision psychiatry or mental health. To investigate further, we removed the age criterion and conducted another search, but still found no relevant documents.
The absence of other logic models in the precision mental health literature is concerning given the burgeoning number of new precision psychiatry/mental health programs and centers. Attention should be paid to implementation science and evaluation research in the development of these programs to maximize the likelihood of long-term success. Creating and using participatory logic models ensures that stakeholder perspectives remain the focus and that those affected and/or contributing to a program remain fully engaged (25, 26, 28). Moreover, PCYMH transformation of the mental health system of care and related research depends on cross-fertilization and communication between programs (19). Logic models are particularly valuable tools for sharing program information and although they may be organization-specific, can be readily adapted for other sites.
Our case study of creating a participatory logic model demonstrates the authentic, active involvement of researchers, clinicians, managers, administrators, community agencies, caregivers and patients, and various other external stakeholders. While stakeholder feedback may be setting-based, much of what stakeholders put into the model and what we shared can provide a starting point for other sites, e.g., suggestions for effective implementation and concerns about ethical issues, privacy, security, equity, and inclusion.
Although the scoping review did not identify logic models for precision psychiatry or mental health in any age group, we did find one participatory precision medicine logic model produced for a national genomic medicine program within the U.S. Veteran's Health Administration. It was informed by implementation science and stakeholder input collected during a one-day conference (45).
Despite not having a mental health focus, there were numerous similarities with our logic model. For example, their Activities included a Research category in which data sharing issues were listed, similar to our Activity of “Enable data sharing within and between institutions” (see Figure 2). They also created an Activities section for Precision Medicine Education, akin to our “Educate & Train stakeholders in PCYMH research & care”. And although they organized concepts and goals differently than we did, effects on ethics, equity, diversity, and inclusion were listed in their Key Impacts, which were included in our Outputs and Outcomes sections. These similarities offer some validation of our logic model for the broader program work needed for precision health programs.
There are three limitations to this case study. First, we were unable to conduct a full qualitative analysis of the preparatory work with stakeholders, as some were not comfortable being recorded. Although compensating by using a scribe who confirmed content of the notes taken at the end of sessions, it is possible that we may have missed some information. Second, only 63% (36/57) of invited stakeholders worked on Phase 2 due to increased clinical patient care and administrative demands during a concurrent surge of COVID-19, respiratory illnesses, and mental health emergencies. However, at least one representative of all stakeholder groups engaged in the process. Therefore, we believe that the likelihood of bias low, the final model being a a relatively accurate reflection of stakeholders’ ideas and opinions. Third, the logic model was created for a single pediatric tertiary care organization, which could reduce generalization to other settings or adult MH programs.
Creating a participatory logic model is time-consuming. Ensure enough preparation time to conduct literature reviews, obtain baseline data for output and outcomes, and identify and fully engage all your stakeholders at the beginning of the process. Even more important is to allow enough time for the numerous iterations needed to produce a consensus model. Protected time or compensation for participation of stakeholders, including persons with lived experience may be necessary.
A multi-disciplinary team is necessary to create a participatory logic model. In our project, the process required scoping review expertise, content knowledge, skills in collecting interview data, facilitation experience, qualitative data analysis skills, and capability to integrate stakeholder information and feedback, results from literature reviews, and results of the environmental scan and gap analysis to produce the final logic model with the stakeholders.
The participatory logic model process significantly enhanced the implementation of PCYMHI. It fostered mutual trust and respect, quickly forming a cohesive team dynamic. This facilitated behavior change more smoothly than anticipated, as strong relationships were established between the PCYMHI leadership and over 60 individuals within the RI, hospital, and community.
PCYMH holds great promise for transforming mental health care and research, but there are numerous threats to the realization of that potential. Using a participatory logic model for program planning, guided by methods from the fields of implementation and evaluation science and disseminating the results could significantly increase the likelihood for PCYMH-driven system transformation.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
KP: Conceptualization, Methodology, Investigation, Formal Analysis, Writing – original draft, Writing – review & editing, Supervision, Project Administration. CH: Methodology, Formal Analysis, Writing – review & editing, Project Administration, Supervision. HH: Methodology, Formal Analysis, Writing – review & editing, Project Administration, Supervision. NS: Methodology, Investigation, Data Curation, Writing – review & editing. WA: Formal Analysis, Writing – review & editing. IT: Writing – review & editing. DR: Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the PCYMHI and funded through an anonymous donation to the CHEO Foundation.
We thank two evaluation consultants, Stephanie Sutherland and Dennis Newhook for guidance on the logic model development, including facilitation of Phase 2 focus groups. In addition, we are grateful for stakeholder time and effort in both phases of the project and Amanda Helleman for formatting and uploading the initial manuscript.
All authors declare that the research was conducted in the absence of any commercial or financial relationships that constitute a conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frhs.2024.1405426/full#supplementary-material
AI, artificial intelligence; APEASE, Acceptability, Practicability, Effectiveness, Affordability, Side Effects, and Equity; BCW, Behavior Change Wheel; CYMH, child and youth mental health; EHR, electronic health record; MeSH, Medical Subject Headings; MH, mental health; PCYMH, precision child and youth mental health; PCYMHI, precision child and youth mental health initiative; PRisMA-ScR, Preferred Reporting Items for Systematic Reviews and Meta-Analyses-Scoping; RE-AIM, Reach, Effectiveness, Adoption, Implementation, and Maintenance; RI, research institute.
1. World Health Organization. Mental health of adolescents (2021). Available online at: https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health#:∼:text=Key%20facts,illness%20and%20disability%20among%20adolescents (accessed February 3, 2024).
2. Kaku SM, Sibeoni J, Basheer S, Chang JP-C, Dahanayake DMA, Irarrazaval M, et al. Global child and adolescent mental health perspectives: bringing change locally, while thinking globally. Child Adolesc Psychiatry Ment Health. (2022) 16(1):82. doi: 10.1186/s13034-022-00512-8
3. Bitsko RH, Claussen AH, Lichstein J, Black LI, Jones SE, Danielson M, et al. Mental Health Surveillance Among Children—United States, 2013–2019. Atlanta, GA: CDC (2022). Contract No.: Suppl 2.
4. Georgiades K, Duncan L, Wang L, Comeau J, Boyle MH, Ontario Child Health Study. Six-month prevalence of mental disorders and service contacts among children and youth in Ontario: evidence from the 2014 Ontario child health study. Can J Psychiatry. (2019) 64(4):246–55. doi: 10.1177/0706743719830024
5. Grimm F, Alcock B, Butler J, Crespo R, Davies A, Peytrignet S, et al. Improving Children and Young People’s Mental Health Services: Local Data Insights from England, Scotland and Wales. London, UK: The Health Foundation (2022).
6. Roest AM, de Vries YA, Wienen AW, de Jonge P. Editorial perspective: are treatments for childhood mental disorders helpful in the long run? An overview of systematic reviews. J Child Psychol Psychiatry. (2023) 64(3):464–9. doi: 10.1111/jcpp.13677
7. Weisz JR, Kuppens S, Ng MY, Vaughn-Coaxum RA, Ugueto AM, Eckshtain D, et al. Are psychotherapies for young people growing stronger? Tracking trends over time for youth anxiety, depression, attention-deficit/hyperactivity disorder, and conduct problems. Perspect Psychol Sci. (2019) 14(2):216–37. doi: 10.1177/1745691618805436
8. Hetrick SE, McKenzie JE, Bailey AP, Sharma V, Moller CI, Badcock PB, et al. New generation antidepressants for depression in children and adolescents: a network meta-analysis. Cochrane Database Syst Rev. (2021) 5(5):CD013674. doi: 10.1002/14651858.CD013674.pub2
9. Dobson ET, Bloch MH, Strawn JR. Efficacy and tolerability of pharmacotherapy for pediatric anxiety disorders: a network meta-analysis. J Clin Psychiatry. (2019) 80(1):17r12064. doi: 10.4088/JCP.17r12064
10. Raballo A, Poletti M, McGorry P. Architecture of change: rethinking child and adolescent mental health. Lancet Psychiatry. (2017) 4(9):656–8. doi: 10.1016/S2215-0366(17)30315-2
11. Ng MY, Weisz JR. Annual research review: building a science of personalized intervention for youth mental health. J Child Psychol Psychiatry. (2016) 57(3):216–36. doi: 10.1111/jcpp.12470
12. Bickman L, Lyon AR, Wolpert M. Achieving precision mental health through effective assessment, monitoring, and feedback processes: introduction to the special issue. Adm Policy Ment Health. (2016) 43(3):271–6. doi: 10.1007/s10488-016-0718-5
13. Bickman L. Improving mental health services: a 50-year journey from randomized experiments to artificial intelligence and precision mental health. Adm Policy Ment Health. (2020) 47(5):795–843. doi: 10.1007/s10488-020-01065-8
14. Passos IC, Ballester P, Rabelo-da-Ponte FD, Kapczinski F. Precision psychiatry: the future is now. Can J Psychiatry. (2022) 67(1):21–5. doi: 10.1177/0706743721998044
15. Posner J. The role of precision medicine in child psychiatry: what can we expect and when? J Am Acad Child Adolesc Psychiatry. (2018) 57(11):813–7. doi: 10.1016/j.jaac.2018.07.874
16. Szatmari P, Susser E. Being precise about precision mental health. JAMA Psychiatry. (2022) 79(12):1149–50. doi: 10.1001/jamapsychiatry.2022.3391
17. Kilbourne AM, Glasgow RE, Chambers DA. What can implementation science do for you? Key success stories from the field. J Ge Intern Med. (2020) 35(2):783–7. doi: 10.1007/s11606-020-06174-6
18. Bauer MS, Kirchner J. Implementation science: what is it and why should I care? Psychiatry Res. (2020) 283:112376. doi: 10.1016/j.psychres.2019.04.025
19. Gomme J, Hill-Landolt J. Unlocking systems transformation. Vision 2050 issue brief. Geneva, Switzerland (2020). Available online at: https://www.wbcsd.org (accessed May 5, 2024).
20. W.K. Kellogg Foundation. Logic Model Development Guide. Battle Creek, MI: W.K. Kellogg Foundation (2004).
21. O'Keefe CM, Head RJ. Application of logic models in a large scientific research program. Eval Program Plann. (2011) 34(3):174–84. doi: 10.1016/j.evalprogplan.2011.02.008
22. Williams NJ, Beidas RS. Annual research review: the state of implementation science in child psychology and psychiatry: a review and suggestions to advance the field. J Child Psychol Psychiatry. (2019) 60(4):430–50. doi: 10.1111/jcpp.12960
23. Carrion AJ, Miles JD, Thompson MD, Journee B, Nelson E. Program evaluation through the use of logic models. Curr Pharm Teach Learn. (2021) 13(7):789–95. doi: 10.1016/j.cptl.2021.03.006
24. McCoy CA, Castner J. Logic models for program evaluation in emergency nursing. J Emerg Nurs. (2020) 46(1):12–5. doi: 10.1016/j.jen.2019.11.005
25. Meyer M, Louder C, Nicolas G. Creating with, not for people: theory of change and logic models for culturally responsive community-based interventions. Am J Eval. (2022) 43(3):378–93. doi: 10.1177/10982140211016059
26. Smits P, Champagne F. An assessment of the theoretical underpinnings of practical participatory evaluation. Am J Eval. (2008) 29(4):427–42. doi: 10.1177/1098214008325023
27. Easterling DV, Jacob RR, Brownson RC, Haire-Joshu D, Gundersen DA, Angier H, et al. Participatory logic modeling in a multi-site initiative to advance implementation science. Implement Sci Commun. (2023) 4(1):106. doi: 10.1186/s43058-023-00468-6
28. Afifi RA, Makhoul J, El Hajj T, Nakkash RT. Developing a logic model for youth mental health: participatory research with a refugee community in Beirut. Health Policy Plan. (2011) 26(6):508–17. doi: 10.1093/heapol/czr001
29. Mills T, Lawton R, Sheard L. Advancing complexity science in healthcare research: the logic of logic models. BMC Med Res Methodol. (2019) 19(1):55. doi: 10.1186/s12874-019-0701-4
30. Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. (2018) 18(1):143. doi: 10.1186/s12874-018-0611-x
31. Peters MDJ, Casey M, Tricco A, Pollack D, Munn Z, Alexander L, et al. Updated methodologic guidance for the conduct of scoping reviews. JBI Evid Syn. (2020) 18(10):2119–26. doi: 10.11124/JBIES-20-00167
32. Tricco AC, Lillie E, Zarin W, O'Brien K, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. (2018) 169:467–73. doi: 10.7326/M18-0850
33. Frandsen TF, Eriksen MB, Hammer DMG, Christensen JB, Wallin JA. Using embase as a supplement to PubMed in cochrane reviews differed across fields. J Clin Epidemiol. (2021) 133:24–31. doi: 10.1016/j.jclinepi.2020.12.022
34. Moullin JC, Dickson KS, Stadnick NA, Albers B, Nilsen P, Broder-Fingert S, et al. Ten recommendations for using implementation frameworks in research and practice. Implement Sci Commun. (2020) 1:42. doi: 10.1186/s43058-020-00023-7
35. Lynch EA, Mudge A, Knowles S, Kitson AL, Hunter SC, Harvey G. There is nothing so practical as a good theory": a pragmatic guide for selecting theoretical approaches for implementation projects. BMC Health Serv Res. (2018) 18(1):857. doi: 10.1186/s12913-018-3671
36. DeJonckheere M, Vaughn LM. Semistructured interviewing in primary care research: a balance of relationship and rigour. Fam Med Community Health. (2019) 7(2):e000057. doi: 10.1136/fmch-2018-000057
37. Birken SA, Powell BJ, Shea CM, Haines ER, Alexis Kirk M, Leeman J, et al. Criteria for selecting implementation science theories and frameworks: results from an international survey. Implement Sci. (2017) 12(1):124. doi: 10.1186/s13012-017-0656-y
38. Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. (1999) 89(9):1322–7. doi: 10.2105/AJPH.89.9.1322
39. Kwan BM, McGinnes HL, Ory MG, Estabrooks PA, Waxmonsky JA, Glasgow RE. RE-AIM in the real world: use of the RE-AIM framework for program planning and evaluation in clinical and community settings. Front Public Health. (2019) 7:345. doi: 10.3389/fpubh.2019.00345
40. Sales AE, Farr SL, Spertus JA. The influence of health behavior theory on implementation practice and science: brief review and commentary. Pharmacy. (2022) 10(5):115. doi: 10.3390/pharmacy10050115
41. Damschroder LJ. Clarity out of chaos: use of theory in implementation research. Psychiatry Res. (2020) 283:112461. doi: 10.1016/j.psychres.2019.06.036
42. Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. (2011) 6:42. doi: 10.1186/1748-5908-6-42
43. Michie S, Atkins L, West R. The Behaviour Change Wheel—a Guide to Designing Interventions. London: Silverback Publishers (2014).
44. West R, Michie S, Atkins L, Chadwick P, Lorencatto F. Achieving Behavior Change. A Guide for Government and Local Partners. London, UK: Public Health England (2019). Contract No.: PHE publications reference number GW-834.
Keywords: precision mental health, precision health, children, youth, participatory logic model, implementation science, evaluation
Citation: Pajer K, Honeywell C, Howley H, Sheridan N, Affleck W, Terekhov I and Radhakrishnan D (2024) Participatory logic model for a precision child and youth mental health start-up: scoping review, case study, and lessons learned. Front. Health Serv. 4:1405426. doi: 10.3389/frhs.2024.1405426
Received: 22 March 2024; Accepted: 24 September 2024;
Published: 17 October 2024.
Edited by:
Obasanjo Bolarinwa, York St John University, United KingdomReviewed by:
Victor Igharo, Johns Hopkins Center for Communication Programs, United StatesCopyright: © 2024 Pajer, Honeywell, Howley, Sheridan, Affleck, Terekhov and Radhakrishnan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kathleen Pajer, a3BhamVyQGNoZW8ub24uY2E=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.