- 1Faculty of Nursing and Midwifery, Royal College of Surgeons Ireland, Dublin, Ireland
- 2Leading Healthcare Providers Skillnet, Skillnet Ireland, Dublin, Ireland
Background: In prosperous nations like Ireland, home support workers (HSWs) play an increasingly vital role in providing person-centred care to ageing populations. However, challenges such as workforce shortages, role ambiguity, low pay, and limited career advancement, hinder workforce development and career building.
Method: A scoping review using key terms for “HSWs” and “career pathways” was conducted following the Joanna Briggs Institute Methodology, examining electronic databases (Web of Science, PubMed, MEDLINE, EMBASE, CINAHL, PscyINFO, Social Care Online, Social Sciences Citation Index). Inclusion criteria were applied, and a thematic analysis followed and inductive-deductive approach.
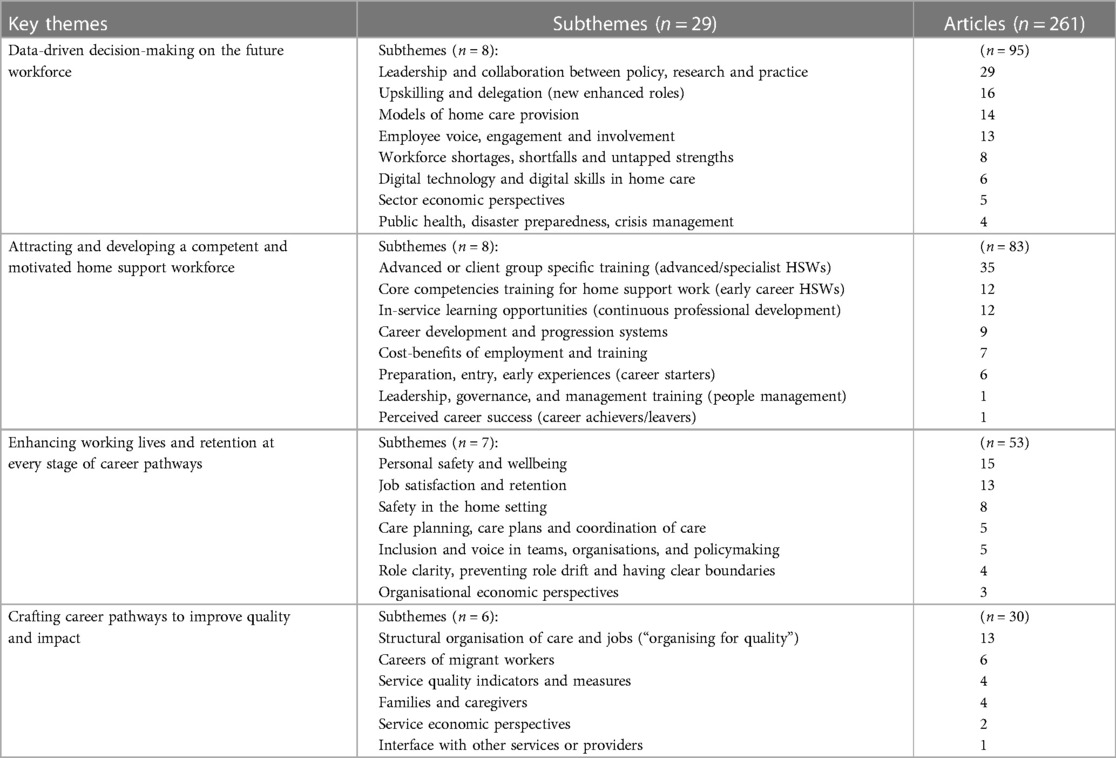
Results: The review encompassed 261 relevant articles from different countries. Four key themes were identified: (1) Data-driven decision-making on the future workforce, (2) Attracting and developing a competent and motivated home support workforce, (3) Enhancing working lives and retention at every stage of career pathways, and (4) Crafting career pathways to improve quality and impact.
Discussion: Leadership, collaboration, and data-driven decision-making across policy, research and practice are pivotal for expanding and enhancing home support. Emphasising a shift towards preventative self-management models, supported by digitally skilled and regulated HSWs, could enhance independence and quality of care. Clear career structures, professional development, and inclusive organisational environments are essential to attract, retain, and empower a competent and motivated workforce, fostering quality and impact.
Conclusion: This scoping review provides foundational evidence to establish career pathways for HSWs, identifying key areas for development such as data collection, care model transformation, career progression structures, and systems for safety and quality improvement.
Highlights
• This scoping review provides a comprehensive view of the evidence on career pathways for home support workers (HSWs) offering insights into key issues and areas for workforce development and career building.
• The evidence highlights the critical need to prioritise leadership, collaboration, and data-driven decision-making to shape the future of the home support sector in line with the needs of ageing populations.
• Clearer career structures could help to attract and retain HSWs, offering opportunities for core competency and advanced training, leadership development, and progression to more skilled work aligned to specific client group needs, and higher grades of renumeration.
• Strategies to cultivate successful careers and a thriving workforce should focus on safeguarding the rights, personal safety, and wellbeing of HSWs and clients as well as involving HSWs more in teams, organisations, and policy decisions.
• Fostering quality and impact in home support work requires developing systems for quality improvement and measures of service evaluation that recognise relational aspects of supportive care.
1 Introduction
Populations globally are ageing rapidly, with at least 35 countries expected to become “super-aged” by 2030. This classification refers to a situation where more than 1 in 6 citizens is over 65 years-of-age, such as the populations of Japan, South Korea, Germany, and Italy. Population ageing can be seen as one of the greatest successes of public health. However, a key challenge is not only the extension of life expectancy but to ensure those extra years are healthy and disability free for as long as possible: the notion of ageing well and independently at home. All countries face major challenges to ensure that their health and social systems are ready to make the most of this demographic shift.
At present prosperous countries are experiencing escalating demand for high-quality home-based support for elders, contributing to a mounting elder care crisis [Global Coalition on (1, 2)]. The United Nations Decade of Healthy Ageing 2021–2030 (3) signifies a concerted effort to address the needs of older people, their families, and communities worldwide with sustainable solutions.
Demand for home support services is driven by multiple socio-demographic factors, including rising numbers of older people with late-life dependency and complex health and care needs. Evidence suggests that person-centred integrated care closer to home can improve health outcomes and maintain independence for older individuals who want to age in place (4–6). Developments in digital health and remote healthcare provision also offer new opportunities for innovation in care and provision of compassion-based support in home settings (7, 8).
In Ireland a rapidly ageing population is projected to increase from 629,800 in 2020 to between 1.53 and 1.6 million by 2051 (9). This situation poses significant challenges to present healthcare and home-based care infrastructures. Despite a significant funding increase to Services for Older People, reaching €665 million in 2021 from €288 million in 2014, demand has surged. Over 20 million hours of home support were delivered to 55,043 service users in 2021 (10), with projections indicating a 50% rise in demand by 2030 (11).
In Ireland and other countries workforce supply challenges, are associated with the stigma of elder care and domestic work, low pay, and poor working conditions (5). A further demographic challenge looms, with many HSWs themselves ageing (42% of HSWs in Ireland were over 60-years-old in 2020). In many countries, rural and low-supply areas, such as districts with high rates of older people, face even worse shortages. Reliance on overseas recruitment and the prevalence of undeclared workers in some countries, has been a focus for political debate regarding the ethical treatment of migrant workers and the regulation of home support work. These pressing challenges underscore the need for comprehensive and transformative evidence-based solutions.
1.1 Rationale
This scoping review aims to investigate international evidence on home support workers (HSW) and career pathways and frameworks. The findings will inform strategies for workforce and career development in Ireland, enhancing the sector's capacity and capabilities. Recognising this is vital for both immediate and long-term population health, as well as the social and economic wellbeing of the nation.
1.2 Objectives
The aim of this scoping review was to provide a comprehensive depth and a balanced perspective of the emerging topic of career pathways for HSWs to inform future policy, research, and practice.
Objectives were:
1) To use a structured scoping review methodology to identify the most relevant evidence internationally on HSWs and career pathways and frameworks.
2) To synthesise available evidence to identify key themes, issues, and gaps in the evidence.
3) To generate actionable recommendations for policy, research and practice on a career pathway for HSWs.
1.3 Approach
The scoping review followed an approach originally proposed by Arksey and O'Malley (12), further enhanced by the work of Levac et al. (13) and consolidated in Joanna Briggs Institute guidelines (14, 15). Presentation of the scoping review conforms with PRISMA-ScR (Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews) (16). Scoping reviews are useful for examining emerging or diverse sources of evidence on a topic to map evidence, concepts, theories, sources or knowledge gaps (17). Unlike a systematic review, scoping reviews do not focus on synthesizing results of studies based on a formal process of methodological appraisal to judge the quality of the evidence (15).
The approach follows five stages: Formulating research questions, Identifying relevant studies, Selecting, charting, collating, Summarizing, Reporting results (12, 18).
1.4 Definitions and scope
The scope of the review was refined by defining the two core concepts of the review based on existing terms and classifications used in the literature (18). A “home support worker” (HSW) was defined as an individual employed to provide support to a person (client or service user) in their private residence. Further detail of the various different terms for HSW is provided separately (Supplementary Material: Home support worker role terminology). A “career pathway” was defined as comprehensive development framework incorporating policy enhancements, best practices, and structural elements to develop the workforce and build careers. The approach emphasised purpose and principles of a career pathway (19, 20). Recognising the importance of economic evaluation in healthcare (21) a separate element of the scoping review (to be published separately) was to seek evidence on economic perspectives using key terms for economic methods and concepts (22, 23).
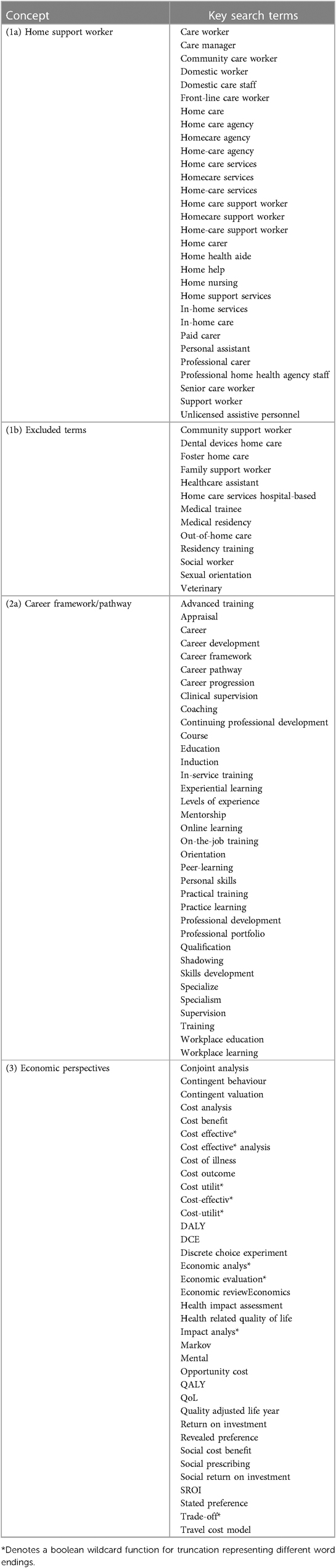
Table 1 shows the key search terms used in the literature searches.
2 Materials and methods
Presentation of the methods follows PRISMA-ScR guidelines. A review protocol was not published for this scoping review. Ethical approval was not required.
2.1 Eligibility criteria (inclusions/exclusions)
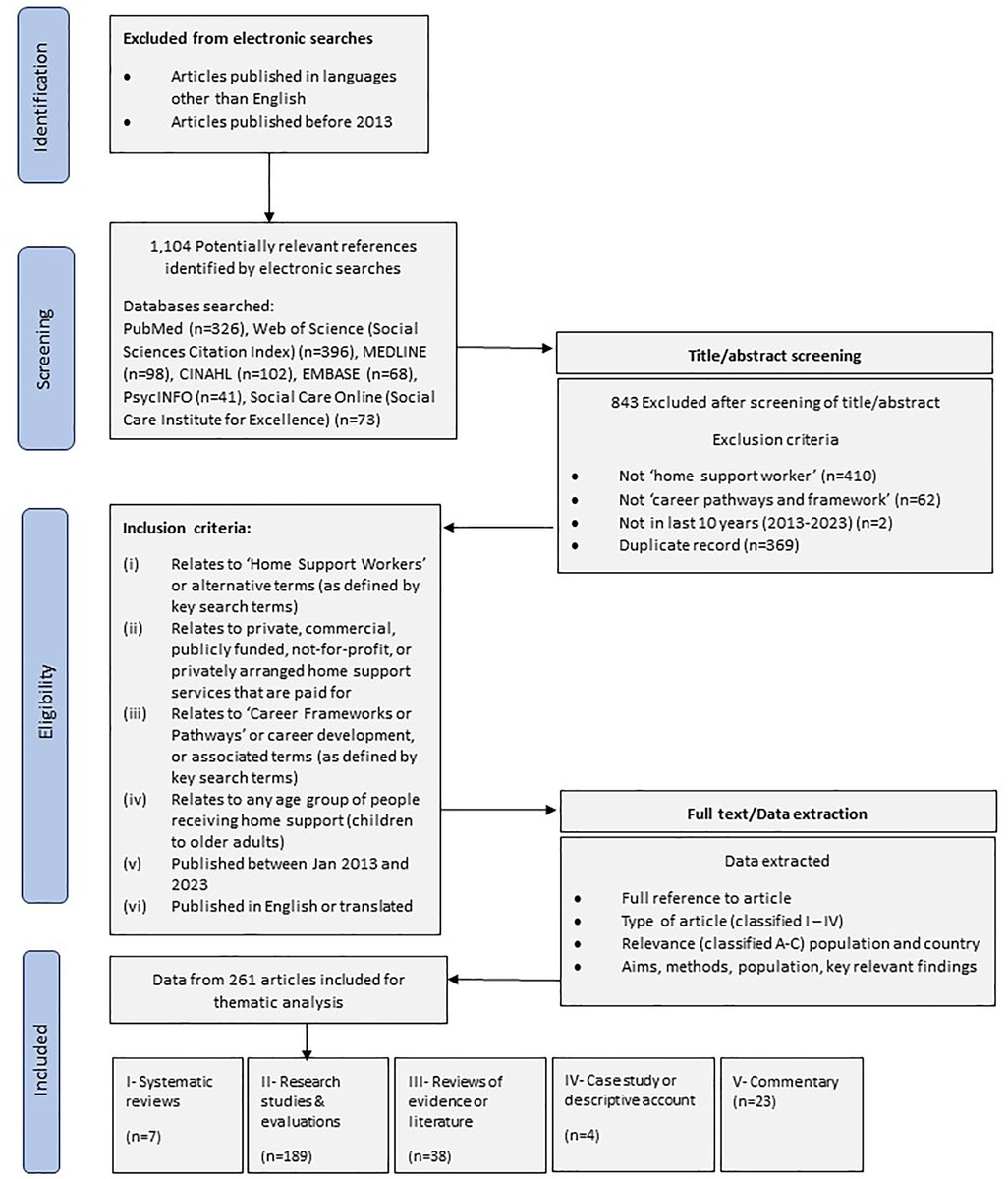
The review is inclusive of all literature published in English language and articles written in other languages when translations were available. To enhance relevance of the included articles, we limited years considered to publication in the last 10 years (2013–2023). Inclusion and exclusion criteria, shown in Figure 1, were developed from the literature.
2.2 Search process
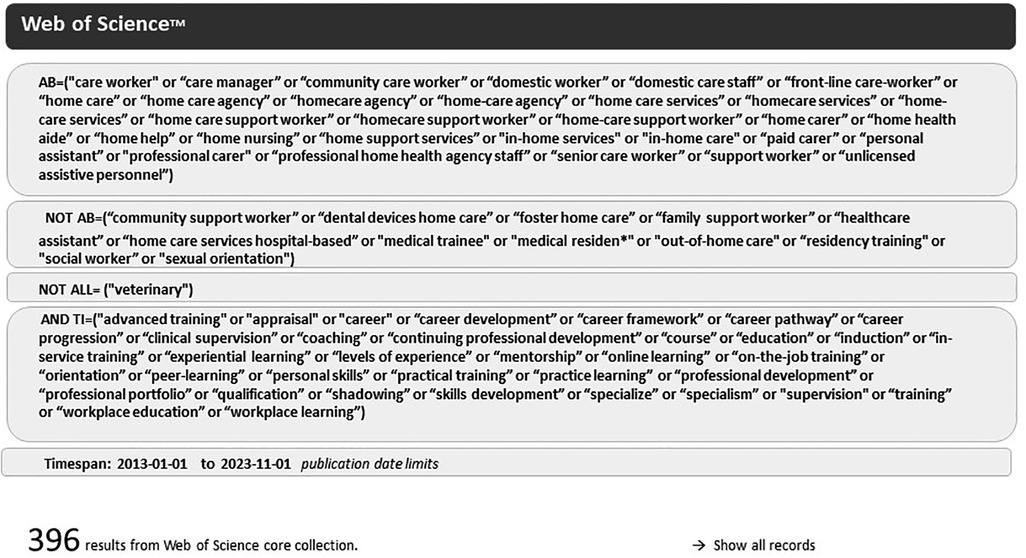
Preliminary searches were undertaken using Google search in August 2023 to develop the review question (15). Searches of electronic databases included literature published in the last 10 years (Jan 2013–Nov 2023). Sources were Web of Science (covering over 12,000 high impact journals and the Social Science Citation Index), PubMed (biomedical literature from MEDLINE, life science journals, and books), EMBASE (medical research), CINAHL (nursing and allied health literature), PscycINFO (behavioural and social sciences), Social Care Online. Source were selected according to the review topic (24). In line with best practices the searches were performed by an experienced researcher (EM) and validated independently (EN, ML) (18). Figure 2 presents an example search strategy for Web of Science (Figure 2).
2.3 Screening
Figure 1 depicts the overall search process. A total of 1,104 articles were identified for screening based on title and abstract, using inclusion/exclusion criteria. Reasons for exclusion of articles were documented for rigor (16).
2.4 Data charting
Data from included articles were extracted into customised tables using Microsoft Word. Tables were piloted with 10 articles, with minor adjustments made. Data included (1) Full article reference, (2) Article type (categories below), (3) Article relevance (categories below), and (4) Summary of aims, methods, and key findings. Data charting included noting population group and context when relevant and training programmes (marked *TP in Supplementary Material: Bibliography).
2.5 Analysis
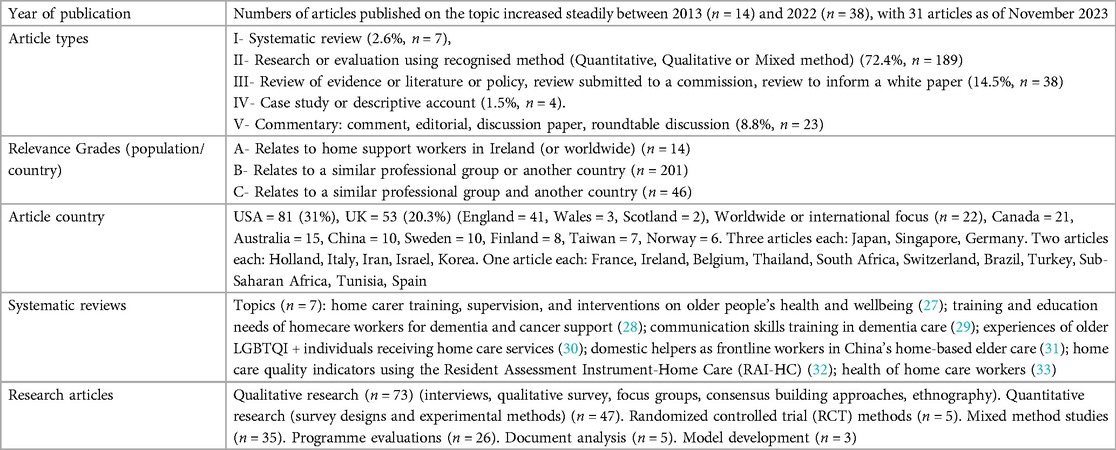
Descriptive analysis of the included articles used date of publication, country of publication, and basic classifications of quality and relevance. Articles were coded following the GRADE system (25) and an assessment of their relevance was based on study population and country (detail in Supplementary Material: Bibliography).
The thematic analysis applied an inductive-deductive approach to explore the research question and the data (17). The analysis followed the review process: familiarization to understand the focus of articles, identification of preliminary themes during data extraction, charting and development of a thematic code framework (Supplementary Material: Thematic code framework). Theme headings were derived from the data. Themes were checked and validated by team members resulting in four key themes, described below.
3 Results
The searches identified 1,104 potentially relevant articles. All were assessed for eligibility based on titles or abstracts. A total of 261 relevant articles were included (Supplementary Material: Bibliography). Included articles were 23.6% of those screened, indicating an accurate search with a high specificity (26). Table 2 provides a description of the included literature (Table 2).
Table 3 summarizes key themes and subthemes and shows the number of articles in each theme (Table 3).
3.1 Theme 1: data-driven decision-making on the future workforce
Leadership and collaboration between policy, research and practice: This prominent theme of the literature unfolds across various countries and time periods. In the US, the Health Workforce Research Center was established to address the long-term care needs of an aging population (34), as well as concerns about safety risks and health hazards (35–37). Leadership and collaboration was needed to establish preventive interventions, inform policy, education, and practice, and set a new course for research (38, 39). These calls to action are underpinned by well-documented challenges internationally associated with low pay and recognition (40, 41), stigma (42–44), work stress (45), and lack of quality standards (46–49). Leadership and multi-agency collaboration efforts focus on workforce planning and sector growth to comprehensively assesses issues in training, recruitment, and retention (50–54).
Upskilling and delegation (new enhanced roles): This theme conveys the need to safely equip HSWs with more advanced skills to transform the model of care, such as responding to the needs of older cancer patients (55, 56). Research has also demonstrated the positive impact of delegation of low risk medication support (57, 58) and home care following stroke (59). Upskilling is essential for improving quality and job satisfaction in the sector (60), provided that the fundamentals of care such as nutrition support and oral care are still met (61–64). There is good reason to believe that allowing time for HSWs to use their support skills, as well as to develop more advanced skills, could improve safety, quality of life for clients and generate healthcare system efficiencies (1, 65). Competencies for more advanced roles and more diverse skillsets need to be clearly defined (66–68), for example, in supporting exercise and reablement (69, 70).
Models of home care and support: Home support needs to expand and develop to encourage supported self-management and build on professional approaches that promote positive health outcomes and innovative interventions that reduce dependency (1, 71, 72). In particular dementia support is recognised as a crucial area for developing the model of home-based person-centred support in partnership with unpaid caregivers (73–78). The Global Coalition on Aging (79) explores relationship-based home care (an outcomes based or person-centred model) advocating for building a caregiving workforce with appropriate skills to deliver different levels of support (80, 81). Changes in the model of care towards client-centred care and reablement have been shown to be feasible (82–84), but the success of changes relates to organisational factors, such as determinants of staff health, service provision, and quality of care measures (69).
Employee voice, engagement and involvement: The literature consistently suggests that employees should be more involved in developing best practices, training, education, and home support workforce development initiatives (85–89). Research advocates a tailored approach, where employee involvement is routinely included yet undertaken flexibly to suit local needs and requirements (90, 91). Employee engagement in decisions about training and continuous professional development (CPD) needs to be encouraged to improve access and relevance (92–96).
Workforce shortages, shortfalls and untapped strengths: The challenge of managing a diverse workforce incudes older women balancing work and care responsibilities (97), and apprenticeship programmes (98). Research has looked into the best practice of employers with less than 10% staff turnover (99) and approaches that combine health and social care approaches to workforce development (100). Workforce issues in rural communities and retention challenges in these areas is an international concern (101–103). Modelling career success is advocated as a way of enhancing recruitment and retention (104).
Digital technology and digital skills in home care: Research has examined training and use of technologies in home support for heart failure patients (105) however the use of assistive technology, robotics, and technologies for optimal workflows is underexplored (106–108). HSWs digital skills are recognised as being crucial to effective use of digital health technologies (109). China's quality supervision indicators for Internet + home care based on the SERVQUAL model, offers a theoretical basis for quality supervision and continuous improvement in Internet + home care (110).
Sector economic perspectives: Research internationally highlights sector challenges of financial sustainability, pay equity, market challenges, and the cost-effectiveness of training programmes (111–113). Economic perspectives include de-investment decisions (114) and the economic benefits of health promoting interventions for prevention of functional loss and promoting quality of life (115).
Public health, disaster preparedness, crisis management: Research conveys the heightened risks and challenges faced by HSWs during the COVID-19 pandemic, and the urgent need for future supportive interventions and policies that address public health issues and involve the home support workforce in preparing for future events (116–118). COVID-19 related issues include economic unevenness across sectors and regions, altered landscapes of healthcare towards more remote and virtual services, increased demand for home-based solutions, and urgency in workforce improvements (119, 120). Solutions offered include sector reform in terms of workforce planning, improved terms and conditions, fair and sustainable funding, and strategies to prevent the perpetuation of existing health and healthcare inequalities.
3.2 Theme 2: attracting and developing a competent and motivated home support workforce
Advanced or client group specific training (advanced/specialist HSWs): Provision of advanced training is a strong theme of the international literature, as well as the development of core competencies in the home support workforce. Within these areas dementia is a key area for advance skills development (27–29, 76, 77, 121–136). In Taiwan trials of virtual reality-based training for dementia have had promising results (137).
Other areas of advanced training being explored are heart failure support (105, 116, 138–144), palliative care (145, 146), end-of-life support (147), mental health (148), hypertension care (149), long-term care (150), and diabetes support (151).
Core competencies training for home support work (early career HSWs): Looking across specific studies and training programmes provides an indication of the necessary core skills training for home support work that involves direct client contact. Topics are:
- Recognising medical emergencies and essential health and support needs (152–155)
- Person centred home support, empathy, and diversity awareness (LGBTQI+, neurodiversity) (30, 156, 157)
- Personal care training, ADL, IADL, infection control, oral health care (158–161)
- Personal assistance (instrumental activities, supervised activities) (160)
- Mental health awareness (depression, loneliness, social anxiety) (162)
- Safety in the home environment (clients and HSWs) including falls prevention (163)
- Communication with clients, cross-cultural communication, cultural competency in the home (164)
- Communication with health care professionals, other services and providers (165)
- Disability/different ability training (hearing loss, visual impairment, learning disability) (166, 167).
In-service learning opportunities (continuous professional development): Various initiatives are contextualised by a wider argument for the need to increase organisational support, supervisor support and peer assistance in the home support sector (168, 169). These arguments are supported by evidence that positive learning outcomes, such as knowledge gained and skills learned, are associated with greater career motivation (170–172) and consolidation of standardised training and competency-based requirements across organisations and sectors (173–176), as well as a climate for innovation (177). Research has shown mixed results for the effectiveness of decision aid training (178) and interprofessional education (179).
Career development and progression systems: Evidence shows multiple barriers to career development and progression in home support work (180, 181). Some researchers argue for equivalency programmes, which take into consideration experience and skills rather than only accepting specific qualifications, to facilitate workforce growth (182). There is some evidence to show the positive impact of appraisals on quality of care provided by support workers, but it is less clear whether appraisals or mentorship support career development or progression (183, 184). There is evidence internationally to show that having opportunities for training, CPD and a supportive work environment, supports employees in their career goals and commitment to stay in home care work (133, 171, 172, 185–187). What is clear is that some provider organisations take a more active approach to career progression than others, emphasising the importance of crafted career pathways for staff advancement and retention of employees and their skills within the organisation (188).
Cost-benefits of employment and training: Research has focused on the cost and benefits of specific courses and training programmes, with some attention to impact on workforce quality and retention issues (180, 181, 189). There is limited evidence of upward career mobility within healthcare occupations in the USA, and other countries, reinforcing the importance of clarifying career pathways for individuals in entry-level positions (190, 191). One training programme evaluation was able to demonstrate a significant reduction in costly adverse events and the positive impact of quality training on patient outcomes (192). Other studies highlight the impact of a workforce training intervention on value-based payment measures (193) and real-life constraints in training programme development (194).
Preparation, entry, early experiences (career starters): A range of factors are known to influence recruitment and early retention to home-based care roles including clarity about specific job roles and fair financial compensation (195, 196), as well as preparatory training, legal protection, and working conditions (31, 197–199).
Leadership, governance, and management training (people management): the need for better governance information and training is a worldwide issue (200). Research shows significant associations between the education level of long-term care administrators and quality indicators, suggesting that promoting further educational attainment of administrators in home support could improve the quality of services provided (201).
Perceived career success (career achievers/leavers): Low status of home care work hinders HSWs feeling valued in their work (202). One USA study showed that HSWs leaving their jobs were more educated, had higher income, and were more likely to be White ethnicity, suggesting low status and pay contribute to high turnover (203).
3.3 Theme 3: enhancing working lives and retention at every stage of career pathways
Personal safety and wellbeing: The physical and emotional nature of the work, lack of safety and support systems, as well as individual client and worker characteristics, contribute to work-related burden in home support work impacting job satisfaction and retention (204–211). Client behaviours in the home, such as occupational tobacco smoke exposure, can create significant health challenges for HSWs, requiring standard terms and agreements to be put in place with clients and families to safeguard employees (212). Workplace health promotion programmes for employees can improve health outcomes and reduce stress (213, 214). Personal social networks can also help HSWs to cope with demanding job roles and emotionally demanding elements of the work such as client bereavement (215–218).
Job satisfaction and retention: Factors underpinning staff motivation and retention include having clear employment terms and conditions (196, 219), as well as enhanced control and support in the role (220, 221), and a positive work culture and modelling successful careers (222–225). The meaning of the work, and recognising the joyful moments of the work, supported HSW's resilience during the COVID-19 pandemic (226). Other research from Germany, UK, Finland and Taiwan, underscores the significance of understanding the factors involved in job satisfaction for retaining employees by developing more tailored and effective job satisfaction strategies (227–230), particularly fair workload and intensity (231).
Safety in the home setting: Safeguarding personal and client safety is a crucial issue that influences job satisfaction and retention of workers in home environments (232). A fundamental client safety concern is the importance of clear organisational protocols and support for HSWs who may be responsible for clients who have acute symptoms so that HSW know when and how to seek emergency assistance for clients (233). Lack of information and education can cause other types of client safety risks, such as the use of physical restraints by family caregivers (234) and dementia-related mitigation interventions (235) or the reduction of falls risk (163, 236). Working in homes and traveling between clients, presents multiple occupational safety risks that can include violence, pests, and driving accidents (237–241).
Care planning, care plans and coordination of care and support: The provision of staff resources on culturally competent care in the home environment has been shown to improve coordination of care (242). Evidence suggests that systems for care planning and associated care planning tools need to recognise the importance of person-centred relational care and the provision of support that facilitates client self-management capabilities, alongside planning and monitoring the delivery of specific tasks such as personal care (243). Assessing, documenting and understanding the needs of specific client groups, such as people with heart failure, is a key issue for care quality, underscoring the need for disease-specific training, care planning, and improved communication of care plans (140, 244, 245).
Inclusion and voice in teams, organisations, and policymaking: Studies from Sweden, Ireland, Belgium, and the USA highlight various inclusion challenges including gender and lack of voice in policy debates (246–248). The literature notes that ambitions to transform healthcare towards more integrated care closer to home, requires HSW to be involved in decision-making, have access to more inclusive training, and to collaborate in initiatives and innovations alongside healthcare teams and other stakeholders (249, 250).
Role clarity, preventing role drift and having clear boundaries: Having clear roles and responsibilities is essential for setting boundaries and protecting HSWs from exploitation and harm (251, 252), including avoiding “market” and “gift” economies of care where HSWs routinely work over their paid hours (253, 254).
Organisational economic perspectives: Economic research on care managers in elderly care shows they are aware of efficiency demands but perceive their role as being to support staff to find ways to use resources better, rather than to enforce efficiency policy (160). Other research has looked into the reasons behind overstretched services, indicating a need to balance development aims with service delivery and to allocate funding for training not only funding for new posts (166, 167).
3.4 Theme 4: crafting career pathways to improve quality and impact
Structural organisation of care and jobs (“organising for quality”): Arguments in the literature stress the critical need to address time constraints, low pay, and inadequate training in the home care sector generally across different countries (255–258). More specifically, studies in the USA and Norway reveal discrepancies in assessing working conditions, scheduling and hours, pointing to the need for standardisation of assessment tools, and improved client data and organisational data collection, and communication regarding the organisation of care and the impact on occupational health outcomes (259–263). Planning tools and work optimisation models can help to assess care plan complexity, revealing congruencies and discrepancies in employee skills and capacity (264–266) and redesign work so that it supports staff recovery (267). Other research emphasises reorganisation of care and new roles for societal needs (268, 269) as well as building in time to deliver interpersonal sensitivity (270).
Careers of migrant workers: Migrant workers play an indispensable role in providing home support work, especially in high-income countries (271, 272). Female migrant domestic workers globally lack opportunities to develop their career and there is a need for tailored employer responses to support fairness and equality (273–276).
Service quality indicators and measures: Safety markers are one indicator of quality in home care and tools such as the International Classification for Patient Safety can be useful (277). In China, a unique set of 77 quality indicators tailored to the Chinese home care context were developed using a modified Delphi technique (278). Despite the widespread implementation of home care quality indicators derived from the Resident Assessment Instrument-Home Care (RAI-HC) research reveals insufficient testing of item validity and reliability in specific countries, underscoring the need for further investigations to enhance the reliability of quality measurement tools (32). However there is recognised need for more work on quality indicators and measures and their implementation (279).
Families and caregivers: Several studies highlight the importance of maintaining healthy family functioning by providing reliable home support (280, 281). Ethnic background can affect experiences of attaining paid help, highlighting the need for enhanced support and targeted interventions for ethnically diverse communities (282). The development of family-centered quality indicators for long-term care, could help to improve the experiences family members and caregivers have of home support services (283).
Service economic perspectives: Key economic issues at a service level relate to the cost benefit of training interventions for workforce retention (284) and to the benefits of service payment models that support quality of care by paying for relational care (285).
Interface with other services or providers: Research from Turkey highlights the complex challenges in medical, nursing, and social welfare aspects of support in the home environment and the necessity to coordinate care between providers (286).
4 Discussion
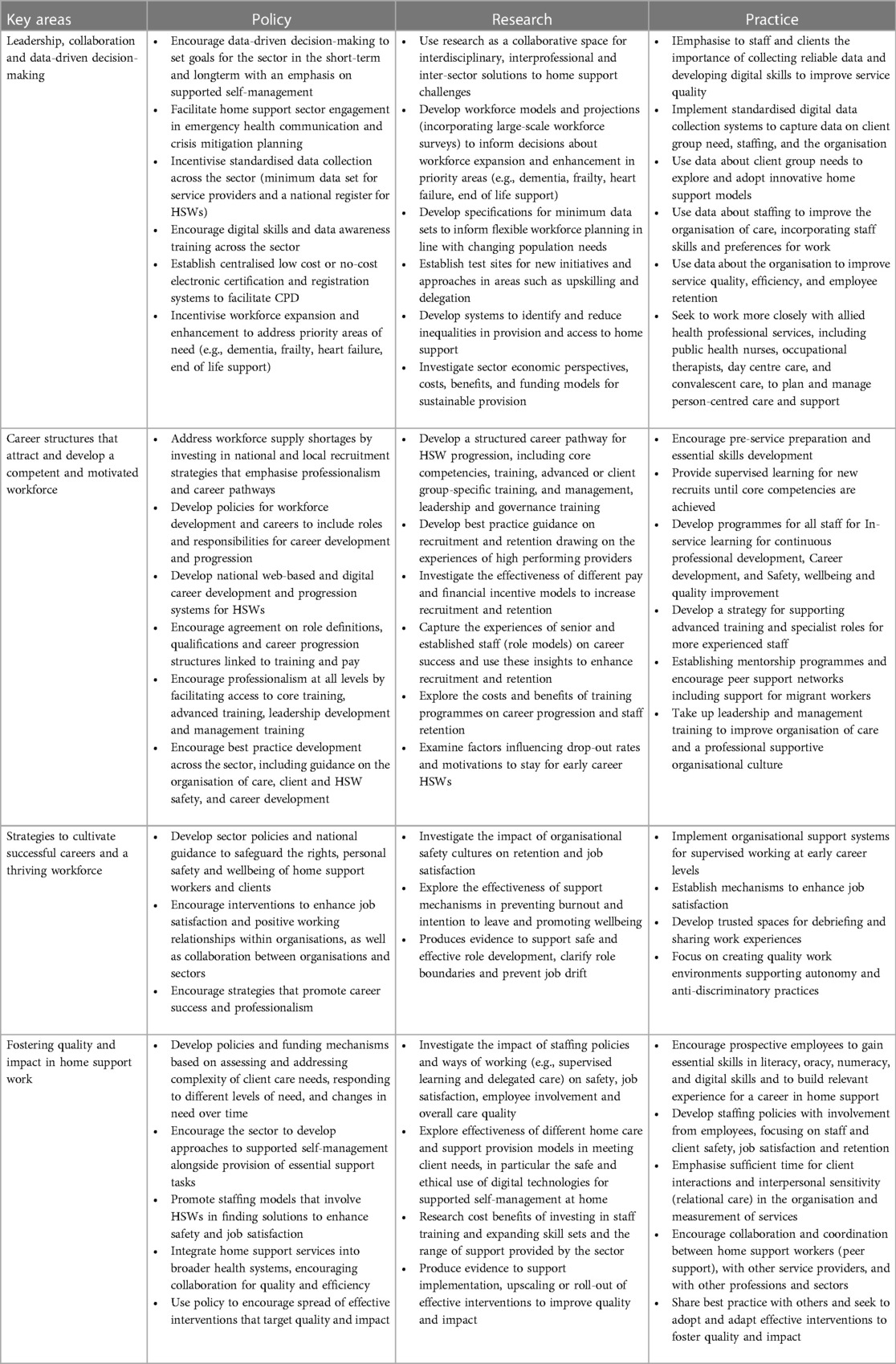
The findings emphasise the pressing need to transform home support services to address the needs of ageing populations. They identify many areas for improvement, such as data collection, care model development, training and qualifications, career structures, opportunities for in-service learning and CPD. Overall there is strong evidence to support the development of career pathways to improve recruitment, retention and job satisfaction, expanding workforce capacity and building successful careers.
4.1 Leadership, collaboration and data-driven decision-making are critical factors in the expansion and enhancement of home support
The international literature demonstrates the critical role of policy, research, and workforce planning processes in shaping the future of home support and transforming the model of home care in line with societal needs. Thus based on these results, policymakers are urged to set clear goals for home support to encourage leadership, collaboration and data collection across the sector (e.g., a minimum data set), prioritise the sector as part of the solution to overburdened healthcare systems, and address sector workforce development priorities. A well-skilled and well-regulated workforce will be invaluable to advancing home-based digital health, harnessing the advantages of AI technologies and implementing Human-AI Intelligent Caring (7, 8).
Part of developing a sustainable model of healthcare is to clarify expectations around home support. The aim should be to counter avoidable paternalism and dependency by promoting a model of preventative supported self-management as far as possible. Policy frameworks that help to bridge research gaps, enable different stakeholders to adopt systems thinking approaches, and find collaborative solutions, are crucial for sector growth. In this literature, dynamic workforce planning linked to outcomes is consistently recommended for positive sector-wide impact. Policymakers should be aware that international perspectives from diverse settings stress the need for collaborative and HSW-inclusive approaches to address supply and demand challenges. In particular, occupational health risks and challenges faced by HSWs all over the world highlight the urgency of implementing a protective human rights-based framework education, and standards to protect employee safety and rights as well as the rights of clients, unpaid carers and families.
Ongoing struggles internationally to combat stigma and role ambiguity associated with aged care work generally, underline the need to encourage professionalism and professional development interventions to challenge societal perceptions of home support. The health professions need to be made more aware of the marginalization of the home support workforce and encourage inclusion of HSW representatives in conversations about integrated care systems. With these strategies and investments, home support stands to be a dynamic sector that has a central role in integrated person-centred care.
4.2 Clearer career structures could help to attract and develop a competent and motivated home support workforce
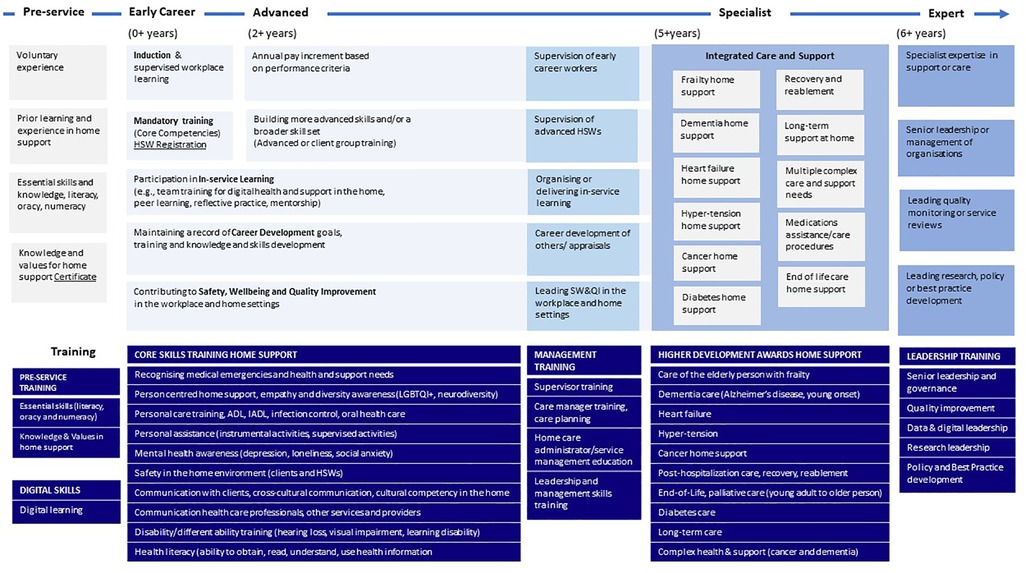
Drawing the evidence together visually, Figure 3 sets out a tentative career structure for HSWs that involves provision of a range of training (preparatory, digital skills, core competency, advanced training, leadership, governance and management), linked to career opportunities, and supported by CPD and in-service learning.
Progression towards advanced roles and specialised training, particularly in dementia, is a robust subtheme internationally, and marks a clear direction for workforce development (one area for advance roles illustrated by Figure 3). Positive impacts on the workforce are observed with career focused interventions like goal setting, carer training, and supervision frameworks, supported by studies from Taiwan, Sweden, and the USA. More advanced heart failure and end-of-life training, along with broader core competencies training for early-career HSWs, appear to be crucial components of expanding and enhancing the capabilities of a home support workforce nationally.
Home support providers should be made aware that successful careers are not only achieved through training and qualifications, but they are also underpinned by in-service learning opportunities and positive inclusive organisational environments. Building robust research into the cost-benefits of employment and training is critical for enabling stakeholders to understand the benefits of sector growth, drawing on global examples from Finland, Canada, the USA, China, and the UK. Entry experiences for career starters need exploration with stakeholders and applied research, to ensure role clarity, fair compensation, and preparatory training become standard practice within employing organisations and nations.
Education and training providers should be aware that gaps exist in leadership training at all levels, as well as governance, and management training in the home support sector. It is unclear whether this is due to lack of tailored courses, barriers to access, or low expectations and engagement with skills development and this requires further investigation at a national level. The impact of educational attainment on service quality remains unclear and requires future research. In many countries low status of home support work and poor pay hinder perceived career success, impacting recruitment and turnover. The status quo could be challenged by future research to establish clear pay grades and promote understanding and recognition for markers of progression and career success within the sector.
4.3 Strategies to cultivate successful careers and a thriving home support workforce
The results demonstrate the value of reframing HSW jobs as a career that has meaning, purpose, and structures for progression. Clearer career structures are likely to attract and retain a competent workforce. However, evidence on employee voice, engagement and involvement provides further important considerations to inform future research into successful careers and a thriving workforce.
The literature on improving working lives and retention of HSWs provides key insights to inform effective career pathways. International challenges in personal safety and wellbeing illustrate the importance of addressing grief, hazards, violence, and stress for a resilient workforce. Globally, job satisfaction and retention are influenced by factors such as control, support, and working conditions and these factors play into perceived career success. Thus, development of national policies for training, supervision, and risk mitigation will be vital for safety at home, impacting both job satisfaction and retention. Organisational economic perspectives stress the interplay between balancing efficiency demands, investing in career development, and funding availability for jobs, necessitating strategic approaches for HSW's workforce planning and progression. These insights contribute to a nuanced understanding for a relevant and impactful career pathway for HSWs. Nurturing a professional narrative could be a very powerful way of addressing many of the issues faced by HSWs. For example, in medicine and nursing e-portfolios provide a mechanism for spotting what is and is not working, as well as guiding professional development.
4.4 Fostering quality and impact in home support work
The evidence underlines the necessity of an effective career pathway to address structural challenges, like time constraints and low pay, and the negative effects on quality. Home support provider organisations and nations, could benefit from future research and development work that draws on a broad range of existing expertise in healthcare quality improvement, CPD in the health professions, career development theory, Lean Thinking techniques (increasing value and reducing waste), and organisational change methodologies. Essential elements of organising for quality include HSW tailored training and support to deliver increasingly complex and skilled work.
Economic perspectives in this topic area, stress recognising relational care in payment models. This is a direct challenge to the apparent efficiencies of time-task commissioning. They also emphasise the indicative cost benefits of investing in staff training and CPD, which may have benefits for healthcare savings. Ultimately, improved efficiencies and coordination at a health system level requires collaborative initiatives that bring HSWs together with healthcare providers and family caregivers for innovation and improvement.
Table 4 draws these discussion points together into a Recommendations Framework, which highlights the coordinated development of home support around four key areas, across policy, research and practice (Table 4).
5 Conclusion
This scoping review highlights the importance of establishing a clear career pathway for home support workers in Ireland and other countries with ageing populations. The review identifies key areas for future focus, such as data collection, digital integration, care model transformation, career structures, training, and leadership development. It stresses the importance of comprehensive best practices, including safety measures, a range of training, and collaborative initiatives, for a high quality and sustainable home support workforce.
The recommendations framework developed for policy, research, and practice provides a set of clear guidelines for developing a home support workforce. Investing in data and decision-making is crucial for shaping the future of home support and transforming the model of care in line with societal needs. Attracting and developing a competent and motivated home support workforce is essential for expanding capacity, enhancing skills, improving job satisfaction, and achieving the goal of providing effective home-based support. The results stress the importance of comprehensive best practices, including safety measures, a range of training, and collaborative initiatives, for a high-quality and sustainable home support workforce.
However, there are limitations to this scoping review, such as generalisability, publication bias, scope, implementation challenges, and long-term impact. Therefore, ongoing monitoring and evaluation are necessary for sustainability and effectiveness of specific interventions. Furthermore the recommendations framework developed for policy, research, and practice must be validated as a Green Paper (287), with a range of local stakeholders across Ireland, before being developed into a White Paper (due April 2024) that reflects and responds to the national context and needs of the population. These recommendations can be discussed by stakeholders internationally and inform career pathways in other countries and contexts.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
EM: Conceptualization, Data curation, Formal Analysis, Investigation, Project administration, Visualization, Writing – original draft, Writing – review & editing. CaK: Conceptualization, Validation, Writing – review & editing. ClK: Conceptualization, Validation, Writing – review & editing. EN: Validation, Writing – review & editing. ML: Conceptualization, Funding acquisition, Methodology, Project administration, Validation, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article.
The scoping review was funded by Leading Healthcare Providers Skillnet, Ireland (https://www.skillnetireland.ie/networks/leading-healthcare-providers-skillnet/).
Acknowledgments
Prof Mark White, FNM, RCSI, provided insights into supporting the emerging care economy deliver safe and effective care. Mr. Joseph Musgrave, Chief Executive Officer, Home & Community Care Ireland, contributed impetus for this research and provided expert insights into the sector.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frhs.2024.1360920/full#supplementary-material
References
1. Ageing well at home. Emergent models of home care provision and the professionalisation of the home care workforce. (2018). Available online at: https://drive.google.com/file/d/1ikHAedrFkH_J5lNc4b4I53fFcBuph4RZ/view (accessed February 28, 2024).
2. Lipszyc B, Sail E, Xavier A. Long-term care: need, use and expenditure in the EU-27. Eur Comm Econ Pap. (2012) 469:10. doi: 10.2765/19991
3. United Nations. Decade of healthy ageing (2021–2030). (2024). Available online at: https://www.decadeofhealthyageing.org/about/about-us/what-is-the-decade (Accessed 23.02.2024).
4. Boland L, Légaré F, Perez MMB, Menear M, Garvelink MM, McIsaac DI, et al. Impact of home care versus alternative locations of care on elder health outcomes: an overview of systematic reviews. BMC Geriatr. (2017) 17:20. doi: 10.1186/s12877-016-0395-y
5. Ross F, Harris R, Fitzpatrick J, Abley C, editors. Redfern’s Nursing Older People, 5th edn. Glasgow: Elsevier Health Sciences (2023). p. 1–608. Available online at: https://www.uk.elsevierhealth.com/redferns-nursing-older-people-9780702082467.html
6. Sheehan A, O’Sullivan R. Draft regulations for providers of home support services: an overview of the findings of the department of health’s public consultation. Report by Institute of Public Health, Dublin Ireland (2023). p. 1–93. ISBN: 978-1-913829-25-4. https://publichealth.ie/sites/default/files/resources/Draft%20Regulations%20for%20Providers%20of%20Home%20Support%20Services%20%20An%20Overview%20of%20the%20Findings%20of%20the%20Departm.pdf (accessed February 28, 2024).
7. Morrow E, Zidaru T, Ross F, Mason C, Patel KD, Ream M, et al. Artificial intelligence technologies and compassion in healthcare: a systematic scoping review. Front Psychol. (2023a) 13:1–31. doi: 10.3389/fpsyg.2022.971044
8. Morrow E, Ross F, Mason C. Editorial: education and learning for digital health. Front Digit Health. (2023b) 5:1165504. doi: 10.3389/fdgth.2023.1165504
9. Eurostat. Ageing Europe—looking at the lives of older people in the EU. (2020). Available online at: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Ageing_Europe_-_looking_at_the_lives_of_older_people_in_the_EU (accessed February 28, 2024).
10. HSE. Board Meeting Minutes. Ireland: Health Service Executive (2021). Available online at: https://www.hse.ie/eng/about/who/board-members/board-meetings/may-2022/4-1-d-2021-operating-and-financial-review-f-250522.pdf
11. ESRI. Demand for the Statutory Home Support Scheme. Dublin: Economic and Social Research Institute (2021). pp. 122. (Research Series). Available online at: https://www.esri.ie/system/files/publications/RS122.pdf
12. Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. (2005) 8(1):19–32. doi: 10.1080/1364557032000119616
13. Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Imple Sci. (2010) 5:69. doi: 10.1186/1748-5908-5-69
14. JBI. Manual for evidence synthesis. (2020). Available online at: https://synthesismanual.jbi.global. doi: 10.46658/JBIMES-20-12 (accessed February 28, 2024).
15. Peters MDJ, Marnie C, Tricco AC, Pollock D, Munn Z, Alexander L, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth. (2020) 18(10):2119–26. doi: 10.11124/JBIES-20-00167
16. Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Int Med. (2018) 169:467–73. doi: 10.7326/M18-0850
17. Mays N, Roberts E, Popay J. Synthesising research evidence. In: Fulop N, Allen P, Clarke A, Black N, editors. Studying the Organisation and Delivery of Health Services: Research Methods. London: Routledge (2001). p. 1–244.
18. Lockwood C, Dos Santos KB, Pap R. Practical guidance for knowledge synthesis: scoping review methods. Asian Nurs Res (Korean Soc Nurs Sci). (2019) 13(5):287–94. doi: 10.1016/j.anr.2019.11.002
19. Hedge JW, Rineer JR. Improving Career Development Opportunities Through Rigorous Career Pathways Research. North Carolina: RTI Press Publication (2017). p. 1–20. doi: 10.3768/rtipress.2017.op.0037.1703
20. McKinsey. The state of organizations (2023). Available online at: https://www.mckinsey.com/capabilities/people-and-organizational-performance/our-insights/the-state-of-organizations-2023 (accessed February 28, 2024).
21. Cunningham SJ. Economics: economic evaluation of healthcare–is it important to US? Br Dent J. (2000) 188(5):250. doi: 10.1038/sj.bdj.4800444
22. Blumenschein K, Johannesson M. Economic evaluation in healthcare. Pharmacoeconomics. (1996) 10(2):114–22. doi: 10.2165/00019053-199610020-00003
23. Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the Economic Evaluation of Health Care Programmes. Oxford: Oxford University Press (2015).
24. Bramer WM, Rethlefsen ML, Kleijnen J, Franco OH. Optimal database combinations for literature searches in systematic reviews: a prospective exploratory study. Syst Rev. (2017) 6:245. doi: 10.1186/s13643-017-0644-y
25. Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, et al. Grading quality of evidence and strength of recommendations. Br Med J. (2004) 328(7454):1490. doi: 10.1136/bmj.328.7454.1490
26. Bramer WM, de Jonge GB, Rethlefsen ML, Mast F, Kleijnen J. A systematic approach to searching: an efficient and complete method to develop literature searches. J Med Libr Assoc. (2018) 106(4):531–41. doi: 10.5195/jmla.2018.283
27. Cooper C, Cenko B, Dow B, Rapaport P. A systematic review evaluating the impact of paid home carer training, supervision, and other interventions on the health and well-being of older home care clients. Int Psychogeriatr. (2017) 29(4):595–604. doi: 10.1017/S1041610216002386
28. Cunningham N, Cowie J, Watchman K, Methven K. Understanding the training and education needs of homecare workers supporting people with dementia and cancer: a systematic review of reviews. Dementia. (2020) 19(8):2780–803. doi: 10.1177/1471301219859781
29. Eggenberger E, Heimerl K, Bennett MI. Communication skills training in dementia care: a systematic review of effectiveness, training content, and didactic methods in different care settings. Int Psychogeriatr. (2013) 25(3):345–58. doi: 10.1017/S1041610212001664
30. Smith R, Wright T. Older lesbian, gay, bisexual, transgender, queer and intersex peoples’ experiences and perceptions of receiving home care services in the community: a systematic review. Int J Nurs Stud. (2021) 118:103907. doi: 10.1016/j.ijnurstu.2021.103907
31. Wang J, Wu B. Domestic helpers as frontline workers in China’s home-based elder care: a systematic review. J Women Aging. (2017) 29(4):294–305. doi: 10.1080/08952841.2016.1187536
32. Wagner A, Schaffert R, Möckli N, Zúñiga F, Dratva J. Home care quality indicators based on the resident assessment instrument-home care (RAI-HC): a systematic review. BMC Health Serv Res. (2020) 20(1):366. doi: 10.1186/s12913-020-05238-x
33. Gebhard D, Herz M. How to address the health of home care workers: a systematic review of the last two decades. J Appl Gerontol. (2023) 42(4):689–703. doi: 10.1177/07334648221141084
34. Darby Rauch K. Finding and Training a Workforce that can Address Older Adults’ Long-Term Care Needs. Science of Caring. San Francisco: University of California (2014). Available online at: https://nursing.ucsf.edu/scienceofcaring/news/finding-and-training-workforce-can-address-older-adults-long-term-care-needs
35. Markkanen P, Quinn M, Galligan C, Sama S, Brouillette N, Okyere D. Characterizing the nature of home care work and occupational hazards: a developmental intervention study. Am J Ind Med. (2014) 57(4):445–57. doi: 10.1002/ajim.22287
36. Quinn MM, Markkanen PK, Galligan CJ, Sama SR, Kriebel D, Gore RJ, et al. Occupational health of home care aides: results of the safe home care survey. Occup Environ Med. (2016) 73(4):237–45. doi: 10.1136/oemed-2015-103031
37. Quinn MM, Markkanen PK, Galligan CJ, Sama SR, Lindberg JE, Edwards MF. Healthy aging requires a healthy home care workforce: the occupational safety and health of home care aides. Curr Environ Health Rep. (2021) 8(3):235–44. doi: 10.1007/s40572-021-00315-7
38. Jarrín OF, Pouladi FA, Madigan EA. International priorities for home care education, research, practice, and management: qualitative content analysis. Nurse Educ Today. (2019) 73:83–7. doi: 10.1016/j.nedt.2018.11.020
39. Spetz J, Dudley N. Consensus-based recommendations for an adequate workforce to care for people with serious illness. J Am Geriatr Soc. (2019) 67(S2):S392–9. doi: 10.1111/jgs.15938
40. Nisbet E, Morgan JC. Constructing legality: theorizing work and the challenges for mobilization of home care workers. Int J Care Caring. (2021) 5(1):45–63. doi: 10.1332/239788220X16020939280487
41. Scales K. Transforming direct care jobs, reimagining long-term services and supports. J Am Med Dir Assoc. (2022) 23(2):207–13. doi: 10.1016/j.jamda.2021.12.005
42. Manchha AV, Walker N, Way KA, Dawson D, Tann K, Thai M. Deeply discrediting: a systematic review examining the conceptualizations and consequences of the stigma of working in aged care. Gerontologist. (2021) 61(4):e129–46. doi: 10.1093/geront/gnaa166
43. Manchha AV, Way KA, Tann K, Thai M. The social construction of stigma in aged-care work: implications for health Professionals’ work intentions. Gerontologist. (2022) 62(7):994–1005. doi: 10.1093/geront/gnac002
44. Manchha AV, Way KA, Thai M, Tann K. “The stigma is what you do”: examining the relationship between occupational stigma and worker outcomes in the aged care context. J Appl Gerontol. (2023) 42(2):221–30. doi: 10.1177/07334648221129849
45. Tsui EK, LaMonica M, Hyder M, Landsbergis P, Zelnick J, Baron S. Expanding the conceptualization of support in low-wage carework: the case of home care aides and client death. Int J Environ Res Public Health. (2021) 19(1):367. doi: 10.3390/ijerph19010367
46. Donovan T. Ready, Steady, Go! Driving Stability and Innovation in the Adult Social Care Market. London, UK: Association of Directors of Adult Social Services (2017). pp. 8. Available online at: https://www.adass.org.uk/media/5861/new-dialogues-ready-steady-go-may-2017.pdf
47. Friedman EM, Ghosh-Dastidar M, Ruder T, Siconolfi D, Shih RA. Trends in home care versus nursing home workforce sizes: are states converging or diverging over time? Study examines trends in home care versus nursing home workforce sizes. Health Aff. (2021) 40(12):1875–82. doi: 10.1377/hlthaff.2021.00749
48. Koehler I. Key to Care: Report of the Burstow Commission on the Future of the Home Care Workforce. London: Local Government Information Unit (2014). pp. 44. Available online at: https://lgiu.org/wp-content/uploads/2014/12/Key-to-Care_FINAL-VERSION.pdf
49. Koehler I. Key to Care Report Card. London: Local Government Information Unit (2015). Available online at: https://lgiu.org/publication/key-to-care-one-year-on/
50. Gary M, Berlinger N. Centering home care in bioethics scholarship, education, and practice. Hastings Cent Rep. (2023) 53(3):34–6. doi: 10.1002/hast.1488
51. Great Britain Parliament, House of Commons, Health and Social Care Committee. (2022). Workforce: Recruitment, Training and Retention in Health and Social Care: Third Report of Session 2022–23. London, UK. pp. 79. Available online at: https://publications.parliament.uk/pa/cm5803/cmselect/cmhealth/115/report.html
52. Institute of Health and Social Care Management. A People Plan for Social Care: a Special Insight. London, UK: Social Care Innovators Subcommittee (2021). pp. 54. Available online at: https://ihscm.org.uk/wp-content/uploads/2021/12/A-People-Plan-for-Social-Care-A-special-Insight-November-2021-1.pdf
53. Luijnenburg O, Manthorpe J, Samsi K. Skills at the Heart of Care: a Scoping Review of Evidence on Skills Gaps in the Social Care Workforce. London, UK: NIHR Policy Research Unit in Health and Social Care Workforce, The Policy Institute, King’s College London (2022). pp. 64. Available online at: https://kclpure.kcl.ac.uk/ws/portalfiles/portal/172111450/Luijnenburg_et_al_2022_Scoping_review_skills_gaps.pdf
54. Molyneux P. Career Opportunities: Understanding the Opportunity to Develop the Health and Care Workforce Together. London, UK: Housing Associations’ Charitable Trust (HACT) (2021). pp. 16. Available online at: https://www.housinglin.org.uk/_assets/Resources/Housing/OtherOrganisation/Report_CareerOpportunitiesHACTRegenda.pdf
55. Connolly C. Advanced direct care worker: a role to improve quality and efficiency of care for older adults and strengthen career ladders for home care workers. Ann Long-Term Care. (2014):1–5. Available online at: https://www.hmpgloballearningnetwork.com/site/altc/articles/advanced-direct-care-worker-role-improve-quality-and-efficiency-care-older-adults-and
56. Hendrix CC, Landerman R, Abernethy AP. Effects of an individualized caregiver training intervention on self-efficacy of cancer caregivers. West J Nurs Res. (2013) 35(5):590–610. doi: 10.1177/0193945911420742
57. Lee CY, Beanland C, Goeman D, Johnson A, Thorn J, Koch S, et al. Evaluation of a support worker role, within a nurse delegation and supervision model, for provision of medicines support for older people living at home: the workforce innovation for safe and effective (WISE) medicines care study. BMC Health Serv Res. (2015) 15:460. doi: 10.1186/s12913-015-1120-9
58. Walsh JE, Lane SJ, Troyer JL. Impact of medication aide use on skilled nursing facility quality. Gerontologist. (2014) 54(6):976–88. doi: 10.1093/geront/gnt085
59. Leonhardt Caprio AM, Burgen DM, Benesch CG. Reducing stroke readmissions utilizing a home care based transitions coaching program. Stroke. (2017) 48(suppl_1):A23. doi: 10.1161/str.48.suppl_1.23
60. Skills for Care. There for Carers: the Workforce Development Needs of Carer Support Workers. Leeds: Skills for Care (2013). p. 20.
61. Fernández-Barrés S, García-Barco M, Basora J, Martínez T, Pedret R, Arija V, et al. The efficacy of a nutrition education intervention to prevent risk of malnutrition for dependent elderly patients receiving home care: a randomized controlled trial. Int J Nurs Stud. (2017) 70:131–41. doi: 10.1016/j.ijnurstu.2017.02.020
62. Johansson L, Björklund A, Sidenvall B, Christensson L. Staff views on how to improve mealtimes for elderly people with dementia living at home. Dementia (London, England). (2017) 16(7):835–52. doi: 10.1177/1471301215619083
63. Mole L, Kent B, Hickson M, Abbott R. “It’s what you do that makes a difference” an interpretative phenomenological analysis of health care professionals and home care workers experiences of nutritional care for people living with dementia at home. BMC Geriatr. (2019) 19(1):250. doi: 10.1186/s12877-019-1270-4
64. Watkinson-Powell A, Barnes S, Lovatt M, Wasielewska A, Drummond B. Food provision for older people receiving home care from the perspectives of home-care workers. Health Soc Care Community. (2014) 22(5):553–60. doi: 10.1111/hsc.12117
65. Denton M, Brookman C, Zeytinoglu I, Plenderleith J, Barken R. Task shifting in the provision of home and social care in Ontario, Canada: implications for quality of care. Health Soc Care Community. (2015) 23(5):485–92. doi: 10.1111/hsc.12168
66. Saari M, Xiao S, Rowe A, Patterson E, Killackey T, Raffaghello J, et al. The role of unregulated care providers in home care: a scoping review. J Nurs Manag. (2018) 26(7):782–94. doi: 10.1111/jonm.12613
67. Saari M, Patterson E, Kelly E, Tourangeau AE. The evolving role of the personal support worker in home care in Ontario, Canada. Health Soc Care Community. (2018) 26(2):240–9. doi: 10.1111/hsc.12514
68. Saari M, Patterson E, Killackey T, Raffaghello J, Rowe A, Tourangeau AE. Home-based care: barriers and facilitators to expanded personal support worker roles in Ontario, Canada. Home Health Care Serv Q. (2017) 36(3–4):127–44. doi: 10.1080/01621424.2017.1393482
69. Darwich AS, Boström AM, Guidetti S, Raghothama J, Meijer S. Investigating the connections between delivery of care, reablement, workload, and organizational factors in home care services: mixed methods study. JMIR Hum Factors. (2023) 10:e42283. doi: 10.2196/42283
70. Henwood T, Hetherington S, Purss M, Rouse K, Morrow J, Smith M. active@home: investigating the value of a home care worker-led exercise program for older adults with Complex care needs. J Aging Phys Act. (2019) 27(2):284–9. doi: 10.1123/japa.2017-0443
71. Walters K, Frost R, Kharicha K, Avgerinou C, Gardner B, Ricciardi F, et al. Home-based health promotion for older people with mild frailty: the HomeHealth intervention development and feasibility RCT. Health Technol Assess. (2017) 21(73):1–128. doi: 10.3310/hta21730
72. Whitehead PJ, Worthington EJ, Parry RH, Walker MF, Drummond AE. Interventions to reduce dependency in personal activities of daily living in community dwelling adults who use homecare services: a systematic review. Clin Rehabil. (2015) 29(11):1064–76. doi: 10.1177/0269215514564894
73. Abdi S, Spann A, Borilovic J, de Witte L, Hawley M. Understanding the care and support needs of older people: a scoping review and categorisation using the WHO international classification of functioning, disability and health framework (ICF). BMC Geriatr. (2019) 19:195. doi: 10.1186/s12877-019-1189-9
74. Hallberg IR, Cabrera E, Jolley D, Raamat K, Renom-Guiteras A, Verbeek H, et al. Professional care providers in dementia care in eight European countries; their training and involvement in early dementia stage and in home care. Dementia (London, England). (2016) 15(5):931–57. doi: 10.1177/1471301214548520
75. Kane L, Leighton C, Limbrick H, Kilinc S, Ling J, Eberhardt J. You clapped, you cheered, but did anybody hear? A mixed-methods systematic review of dementia homecare workers’ training and psychosocial needs. Home Health Care Serv Q. (2023) 42(4):282–310. doi: 10.1080/01621424.2023.2246415
76. Leverton M, Burton A, Beresford-Dent J, Rapaport P, Manthorpe J, Mansour H, et al. “You can’t just put somebody in a situation with no armour”. an ethnographic exploration of the training and support needs of homecare workers caring for people living with dementia. Dementia (London, England). (2021a) 20(8):2982–3005. doi: 10.1177/14713012211023676
77. Leverton M, Burton A, Beresford-Dent J, Rapaport P, Manthorpe J, Azocar I, et al. Supporting independence at home for people living with dementia: a qualitative ethnographic study of homecare. Soc Psychiatry Psychiatr Epidemiol. (2021b) 56(12):2323–36. doi: 10.1007/s00127-021-02084-y
78. Social Care Wales. Development of a Strategic Plan for Care and Support at Home: Literature Review. Cardiff: Social Care Wales (2017). pp. 50. Available online at: https://socialcare.wales/cms-assets/documents/Care-and-support-at-home-in-Wales-Literature-review.pdf
79. Global Coalition on Aging. Relationship-Based Home Care: a Sustainable Solution for Europe’s Elder Care Crisis. London: Global Coalition on Aging (2018). pp. 36. Available online at: https://globalcoalitiononaging.com/wp-content/uploads/2018/06/RHBC_Report_DIGITAL.pdf
80. Ordway A, Johnson KL, Kneale L, Amtmann D, Demiris G. The experience of home care providers and beneficiaries with enhanced training requirements in Washington state. J Aging Health. (2019) 31(10_suppl):124S–44. doi: 10.1177/0898264319860298
81. Scales K. Meeting the integration mandate: the implications of Olmstead for the home care workforce. Geo J on Poverty L Pol’y. (2019) 27:261.
82. Rooijackers TH, Zijlstra GAR, van Rossum E, Vogel RGM, Veenstra MY, Kempen GIJM. Process evaluation of a reablement training program for homecare staff to encourage independence in community-dwelling older adults. BMC Geriatr. (2021) 21(1):5. doi: 10.1186/s12877-020-01936-7
83. Sanerma P, Miettinen S, Paavilainen E, Åstedt-Kurki P. A client-centered approach in home care for older persons—an integrative review. Scand J Prim Health Care. (2020) 38(4):369–80. doi: 10.1080/02813432.2020.1841517
84. Wang J, Wang Y, Cai H, Zhang J, Pan B, Bao G, et al. Analysis of the status quo of the elderly’s demands of medical and elderly care combination in the underdeveloped regions of western China and its influencing factors: a case study of Lanzhou. BMC Geriatr. (2020) 20:338. doi: 10.1186/s12877-020-01616-6
85. Bluestone J, Ricca J, Traicoff D, Tchoualeu D. It’s time to move beyond traditional health care worker training approaches. Glob Health Sci Pract. (2021) 9(3):431–2. doi: 10.9745/GHSP-D-21-00553
86. Morgan JC, Edris N, Luz CC, Ochylski DP, Stineman A, Winchester L, et al. Testing US state-based training models to meet health workforce needs in long-term care. Ageing Int. (2018) 43:123–40. doi: 10.1007/s12126-017-9286-6
87. Spetz J, Stone RI, Chapman SA, Bryant N. Home and community-based workforce for patients with serious illness requires support to meet growing needs. Health Aff. (2019) 38(6):902–9. doi: 10.1377/hlthaff.2019.00021
88. Guerrero LR, Richter Lagha R, Shim A, Gans D, Schickedanz H, Shiner L, et al. Geriatric workforce development for the underserved: using RCQI methodology to evaluate the training of IHSS caregivers. J Appl Gerontol. (2020) 39(7):770–7. doi: 10.1177/0733464818780635
89. Stone R. Developing a quality home care workforce to complement family caregivers and bridge the emerging care gap. In: Gaugler JE, editor. Bridging the Family Care Gap. Cambridge: Academic Press (2021). pp. 321–40.
90. Rycroft-Malone J, Burton CR, Williams L, Edwards S, Fisher D, Hall B, et al. Improving skills and care standards in the support workforce for older people: a realist synthesis of workforce development interventions. NIHR J Lib. (2016) 4(12):1–116. doi: 10.3310/hsdr04120
91. Williams L, Rycroft-Malone J, Burton CR, Edwards S, Fisher D, Hall B, et al. Improving skills and care standards in the support workforce for older people: a realist synthesis of workforce development interventions. BMJ Open. (2016) 6(8):e011964. doi: 10.1136/bmjopen-2016-011964
92. Pavloff M, Labrecque ME. Continuing education for home care nurses: an integrative literature review. Home Healthc Now. (2021) 39(6):310–9. doi: 10.1097/NHH.0000000000001005
93. Lawani MA, Turgeon Y, Côté L, Légaré F, Witteman HO, Morin M, et al. User-centered and theory-based design of a professional training program on shared decision-making with older adults living with neurocognitive disorders: a mixed-methods study. BMC Med Inform Decis Mak. (2021) 21(1):59. doi: 10.1186/s12911-021-01396-y
94. Savassi LCM, Dias MB, Boing AF, Verdi M, Lemos AF. Educational strategies for human resources in home health care: 8 years’ experience from Brazil. Rev Panam Salud Publica. (2020) 44:e103. doi: 10.26633/RPSP.2020.103
95. Attenborough J, Abbott S, Brook J, Knight RA. Everywhere and nowhere: work-based learning in healthcare education. Nurse Educ Pract. (2019) 36:132–8. doi: 10.1016/j.nepr.2019.03.004
96. Palesy D. Learning in the absence of direct supervision: person-dependent scaffolding. Vocat Learn. (2017) 10(3):365–82. doi: 10.1007/s12186-017-9176-9
97. Ben-Galim D, Silim A. The Sandwich Generation: Older Women Balancing Work and Care. London: Institute for Public Policy Research (2013). pp. 43. Available online at: https://www.ippr.org/publications/the-sandwich-generation-older-women-balancing-work-and-care
98. Pratt J. Career Progression in Care Project, End of Project Report. Leeds, UK: Skills for Care (2016). pp. 27.
99. Skills for Care. Recruitment and retention in adult social care: secrets of success. Learning from employers what works well. (2017). Available online at: https://www.skillsforcare.org.uk/resources/documents/Recruitment-support/Retaining-your-staff/Secrets-of-Success/Recruitment-and-retention-secrets-of-success-report.pdf
100. Bryant J. Workforce to Care Force: Who Cares? Oxford: Oxford Brookes University, Institute of Public Care (2018). pp. 18. (IPC discussion paper). Available online at: https://ipc.brookes.ac.uk/files/publications/Workforce_to_Care_Force-IPC_Discussion_Paper_John_Bryant.pdf
101. Sharman Z. Recruitment and retention of home support workers in rural communities. Home Health Care Serv Q. (2014) 33(4):229–43. doi: 10.1080/01621424.2014.964897
102. Chapman SA, Greiman L, Bates T, Wagner LM, Lissau A, Toivanen-Atilla K, et al. Personal care aides: assessing self-care needs and worker shortages in rural areas. Health Aff (Millwood). (2022) 41(10):1403–12. doi: 10.1377/hlthaff.2022.00483
103. Kelly C, Craft Morgan J, Kemp CL, Deichert J. A profile of the assisted living direct care workforce in the United States. J Appl Gerontol. (2020) 39(1):16–27. doi: 10.1177/0733464818757000
104. Gatherum B, O’Reilly P, Ross K. The Experience of the Experienced: Exploring Employment Journeys of the Social Care Workforce. Ayr, Scotland: Scottish Care (2018). pp. 26. Available online at: https://scottishcare.org/wp-content/uploads/2020/03/Qualifying-Care-Final.pdf)
105. Sterling MR, Cho J, Ringel JB, Avgar AC. Heart failure training and job satisfaction: a survey of home care workers caring for adults with heart failure in New York city. Ethn Dis. (2020) 30(4):575–82. doi: 10.18865/ed.30.4.575
106. Welch V, Mathew CM, Babelmorad P, Li Y, Ghogomu ET, Borg J, et al. Health, social care and technological interventions to improve functional ability of older adults living at home: an evidence and gap map. Campbell Syst Rev. (2021) 17(3):e1175. doi: 10.1002/cl2.1175
107. Bandini JI, Siconolfi D, Feistel K, Etchegaray J. Low tech, high potential: using technology to improve communication across home care workers. J Appl Gerontol. (2023) 42(4):776–81. doi: 10.1177/07334648221144027
108. Turjamaa R, Vaismoradi M, Kajander-Unkuri S, Kangasniemi M. Home care professionals’ experiences of successful implementation, use and competence needs of robot for medication management in Finland. Nurs Open. (2023) 10(4):2088–97. doi: 10.1002/nop2.1456
109. Oung C, Rolewicz L, Crellin N, Kumpunen S. Developing the Digital Skills of the Social Care Workforce: Evidence from the Care City Test Bed. London, UK: Nuffield Trust (2021). pp. 32. Available online at: https://www.nuffieldtrust.org.uk/sites/default/files/2021-09/workforce-research-summary-final.pdf
110. Ma G, Hou J, Peng S, Liu Y, Shi Z, Fan Y, et al. Construction of internet+home care quality supervision indicators in China based on the Delphi method. Risk Manag Healthc Policy. (2022) 15:1325–41. doi: 10.2147/RMHP.S368592
111. Lu J. Status quo, problems and countermeasure research of home-based care service market in China—a case study of Sichuan province. Open J Soc Sci. (2015) 3:150–6. doi: 10.4236/jss.2015.311020
112. Community Integrated Care. Unfair to Care: Understanding the Social Care Pay Gap and How to Close It: Full Report. Epsom, UK: Community Integrated Care (2021). pp. 64. Available online at: https://www.unfairtocare.co.uk/wp-content/uploads/2021/07/Unfair-To-Care-Full-Report-Single-Pages.pdf
113. Velazquez F, Fox S, Chatha D. Adaptive strategies to building a sustainable workforce: health care support worker (HCSW) and the health career access program (HCAP). Int J Integr Care. (2022) 22:108. doi: 10.5334/ijic.ICIC21337
114. Rooijackers TH, Metzelthin SF, van Rossum E, Kempen GIJM, Evers SMAA, Gabrio A. Economic evaluation of a reablement training program for homecare staff targeting sedentary behavior in community-dwelling older adults compared to usual care: a cluster randomized controlled trial. Clin Interv Aging. (2021) 16:2095–109. doi: 10.2147/CIA.S341221
115. Ramos LR, d’Orsi E, Simões EJ. Editorial: longevity with functionality and quality of life. Front Aging. (2023) 4:1281737. doi: 10.3389/fragi.2023.1281737
116. Sterling MR, Dell N, Tseng E, Okeke F, Cho J, Piantella B, et al. Home care workers caring for adults with heart failure need better access to training and technology: a role for implementation science. J Clin Transl Sci. (2020) 4(3):224–8. doi: 10.1017/cts.2020.36
117. Franzosa E, Wyte-Lake T, Tsui E, Reckrey J, Sterling M. Essential but excluded: building disaster preparedness capacity for home health care workers and home care agencies. J Am Med Dir Assoc. (2022) 23(12):1990–6. doi: 10.1016/j.jamda.2022.09.012
118. Lethin C, Kenkmann A, Chiatti C, Christensen J, Backhouse T, Killett A, et al. Organizational support experiences of care home and home care staff in Sweden, Italy, Germany and the United Kingdom during the COVID-19 pandemic. Healthcare. (2021) 9(6):767. (MDPI). doi: 10.3390/healthcare9060767
119. Sterling MR, Tseng E, Poon A, Cho J, Avgar AC, Kern LM, et al. Experiences of home health care workers in New York city during the coronavirus disease 2019 pandemic: a qualitative analysis. JAMA Intern Med. (2020) 180(11):1453–9. doi: 10.1001/jamainternmed.2020.3930
120. Association of Directors of Adult Social Services. The Legacy of COVID: What Might the Pandemic’s Long-Term Impact be for Adult Social Care? Eastern Region, England. London, UK: Association of Directors of Adult Social Services Eastern Region (2021). pp. 24. Available online at: https://www.scie-socialcareonline.org.uk/the-legacy-of-covid-what-might-the-pandemics-long-%C2%ADterm-impact-be-for-adult-social-care/r/a116f00000Um0yUAAR
121. Yang YY, Yang YP, Chen KM, Wang CJ, Chang SH, Wang JJ. A feasibility evaluation of the need-centered watch-assess-need intervention-think education and training program for behavioral and psychological symptoms of dementia. J Nurs Res. (2023) 31(2):e266. doi: 10.1097/jnr.0000000000000548
122. Newbould L, Samsi K, Wilberforce M. Developing effective workforce training to support the long-term care of older adults: a review of reviews. Health Soc Care Community. (2022) 30(6):2202–17. doi: 10.1111/hsc.13897
123. Goh AM, Doyle C, Gaffy E, Batchelor F, Polacsek M, Savvas S, et al. Co-designing a dementia-specific education and training program for home care workers: the “promoting independence through quality dementia care at home” project. Dementia (London, England). (2022a) 21(3):899–917. doi: 10.1177/14713012211065377
124. Goh AMY, Polacsek M, Malta A, Doyle C, Hallam B, Gahan L, et al. What constitutes “good” home care for people with dementia? An investigation of the views of home care service recipients and providers. BMC Geriatr. (2022b) 22:42. doi: 10.1186/s12877-021-02727-4
125. Zabihi S, Duffy L, Kelleher D, Lord K, Dar A, Koutsoubelis F, et al. Feasibility and acceptability of NIDUS-professional, a training and support intervention for homecare workers caring for clients living with dementia: a cluster-randomised feasibility trial protocol. BMJ Open. (2022) 12(12):e066166. doi: 10.1136/bmjopen-2022-066166
126. Stargatt J, Bhar S, Petrovich T, Bhowmik J, Sykes D, Burns K. The effects of virtual reality-based education on empathy and understanding of the physical environment for dementia care workers in Australia: a controlled study. J Alzheimer’s Dis. (2021) 84(3):1247–57. doi: 10.3233/JAD-210723
127. Su HF, Koo M, Lee WL, Sung HC, Lee RP, Liu WI. A dementia care training using mobile e-learning with mentoring support for home care workers: a controlled study. BMC Geriatr. (2021) 21(1):126. doi: 10.1186/s12877-021-02075-3
128. Sung HC, Su HF, Wang HM, Koo M, Lo RY. Psychometric properties of the dementia knowledge assessment scale-traditional Chinese among home care workers in Taiwan. BMC Psychiatry. (2021) 21(1):515. doi: 10.1186/s12888-021-03530-6
129. Fallahpour M, Borell L, Sandberg L, Boström AM. Dementia care education targeting job strain and organizational climate among dementia care specialists in Swedish home care services. J Multidiscip Healthc. (2020) 13:85–97. doi: 10.2147/JMDH.S214378
130. Guerrero LR, Shim A, Gans D, Schickedanz HB, Tan ZS. Training for in-home supportive services caregivers in an underserved area. J Health Care Poor Underserved. (2019) 30(2):739–48. doi: 10.1353/hpu.2019.0053
131. Goh AMY, Gaffy E, Hallam B, Dow B. An update on dementia training programmes in home and community care. Curr Opin Psychiatry. (2018) 31(5):417–23. doi: 10.1097/YCO.0000000000000438
132. Smith R, Ooms A, Greenwood N. Supporting people with young onset dementia and their families: an evaluation of a training course for care workers. Nurse Educ Pract. (2017) 27:7–12. doi: 10.1016/j.nepr.2017.08.007
133. Kosteniuk J, Morgan D, O’Connell M, Dal Bello-Haas V, Stewart N. Focus on dementia care: continuing education preferences, challenges, and catalysts among rural home care providers. Educ Gerontol. (2016) 42(9):608–20. doi: 10.1080/03601277.2016.1205404
134. Gaugler JE, Hobday JV, Robbins JC, Barclay MP. Direct care worker training to respond to the behavior of individuals with dementia: the CARES® dementia-related behavior™ online program. Gerontol Geriatr Med. (2016) 2:2333721415626888. doi: 10.1177/2333721415626888
135. Morgan D, Kosteniuk J, O’Connell M, Dal Bello-Haas V, Stewart N, Karunanayake C. Dementia-related work activities of home care nurses and aides: frequency, perceived competence, and continuing education priorities. Educ Gerontol. (2016) 42(2):120–35. doi: 10.1080/03601277.2015.1083390
136. Yeh J, Pond B, Beld M, Garcia A, Mauricio J, Mata-Pacheco J, et al. Enhancing dementia knowledge and self-efficacy of in-home supportive services caregivers through online training. J Appl Gerontol. (2023) 42(4):617–26. doi: 10.1177/07334648221144023
137. Sung HC, Su HF, Lee WL, Yamakawa M, Wang HM. Effects of a dementia virtual reality-based training with peer support for home care workers: a cluster randomized controlled trial. Int J Geriatr Psychiatry. (2022) 37(9):10.1002/gps.5799. doi: 10.1002/gps.5799
138. Stawnychy MA, Ringel JB, Riegel B, Sterling MR. Better preparation and training determine home care Workers’ self-efficacy in contributing to heart failure self-care. J Appl Gerontol. (2023) 42(4):651–9. doi: 10.1177/07334648221113322
139. Leung PB, Silva AF, Cho J, Kaur H, Lee A, Escamilla Y, et al. Eliciting the educational priorities of home care workers caring for adults with heart failure. Gerontol Geriatr Educ. (2022) 43(2):239–49. doi: 10.1080/02701960.2020.1793760
140. Sterling MR, Silva AF, Leung PBK, Shaw AL, Tsui EK, Jones CD, et al. “It’s like they forget that the word ‘health’ is in ‘home health aide’”: understanding the perspectives of home care workers who care for adults with heart failure. J Am Heart Assoc. (2018) 7(23):e010134. doi: 10.1161/JAHA.118.010134
141. Sterling MR, Barbaranelli C, Riegel B, Stawnychy M, Ringel JB, Cho J, et al. The influence of preparedness, mutuality, and self-efficacy on home care workers’ contribution to self-care in heart failure: a structural equation modeling analysis. J Cardiovasc Nurs. (2022) 37(2):146–57. doi: 10.1097/JCN.0000000000000768
142. Sterling MR, Cho J, Leung PB, Silva AF, Ringel J, Wiggins F, et al. Development and piloting of a community-partnered heart failure training course for home health care workers. Circ Cardiovasc Qual Outcomes. (2022) 15(11):e009150. doi: 10.1161/CIRCOUTCOMES.122.009150
143. Baik D, Leung PB, Sterling MR, Russell D, Jordan L, Silva AF, et al. Eliciting the educational needs and priorities of home care workers on end-of-life care for patients with heart failure using nominal group technique. Palliat Med. (2021) 35(5):977–82. doi: 10.1177/0269216321999963
144. Padula MS, D’Ambrosio GG, Tocci M, D’Amico R, Banchelli F, Angeli L, et al. Home care for heart failure: can caregiver education prevent hospital admissions? A randomized trial in primary care. J Cardiovasc Med (Hagerstown). (2019) 20(1):30–8. doi: 10.2459/JCM.0000000000000722
145. McPherson CJ, Etele J, Ta VCY, Raghubir A. Unregulated care providers’ engagement in palliative care to older clients and their families in the home setting: a mixed methods study. BMC Palliat Care. (2019) 18(1):1–15. doi: 10.1186/s12904-019-0442-5
146. Herber OR, Johnston BM. The role of healthcare support workers in providing palliative and end-of-life care in the community: a systematic literature review. Health Soc Care Community. (2013) 21(3):225–35. doi: 10.1111/j.1365-2524.2012.01092.x
147. Tsui EK, Wang WQ, Franzosa E, Gonzalez T, Reckrey JM, Sterling MR, et al. Training to reduce home care aides’ work stress associated with patient death: a scoping review. J Palliat Med. (2020) 23(9):1243–9. doi: 10.1089/jpm.2019.0441
148. Booi L, Sixsmith J, Chaudhury H, O’Connor D, Surr C, Young M, et al. “I didn’t know it was going to be like this”: unprepared for end-of-life care, the experiences of care aides care in long-term care. BMC Palliat Care. (2023) 22(1):132. doi: 10.1186/s12904-023-01244-y
149. Alvarez C, Ibe C, Dietz K, Carrero ND, Avornu G, Turkson-Ocran RA, et al. Development and implementation of a combined nurse care manager and community health worker training curriculum to address hypertension disparities. J Ambul Care Manage. (2022) 45(3):230–41. doi: 10.1097/JAC.0000000000000422
150. Russell D, Fong MC, Gao O, Lowenstein D, Haas M, Wiggins F, et al. Formative evaluation of a workforce investment organization to provide scaled training for home health aides serving managed long-term care plan clients in New York state. J Appl Gerontol. (2022) 41(7):1710–21. doi: 10.1177/07334648221084182
151. Gregory S. Diabetes care in care home and residential settings. Br J Community Nurs. (2018) 23(10):510–3. doi: 10.12968/bjcn.2018.23.10.510
152. Kajander-Unkuri S, Kämäräinen P, Hartikainen T, Turjamaa R. Effectiveness of a combined web-based and simulation-based continuing education on home-care professionals’ competence to evaluate older people’s acute care needs in Finland. Health Soc Care Community. (2022) 30(5):e1765–74. doi: 10.1111/hsc.13605
153. Palesy D, Jakimowicz S, Saunders C, Lewis J. Australian Home care work: an integrative review. Home Health Care Serv Q. (2018) 37(2):113–39. doi: 10.1080/01621424.2018.1438952
154. Palesy D, Jakimowicz S. Health literacy training for Australian home care workers: enablers and barriers. Home Health Care Serv Q. (2019) 38(2):80–95. doi: 10.1080/01621424.2019.1604458
155. Palesy D, Jakimowicz S. Health literacy support for Australian home-based care recipients: a role for homecare workers? Home Health Care Serv Q. (2020) 39(1):17–32. doi: 10.1080/01621424.2019.1691698
156. Daley A, MacDonnell JA. “That would have been beneficial”: LGBTQ education for home-care service providers. Health Soc Care Community. (2015) 23:282–91. doi: 10.1111/hsc.12141
157. Kim H, Park C, Lee N. Effects of health perception, generativity and wisdom on job competency of Korean care workers. Medico Legal Update. (2020) 20(2):718–23. doi: 10.37506/mlu.v20i2.1199
158. Edman K, Wårdh I. Oral health care beliefs among care personnel working with older people—follow-up of oral care education provided by dental hygienists. Int J Dent Hyg. (2022) 20(2):241–8. doi: 10.1111/idh.12588
159. Hsu WC, Hsieh YP, Lan SJ. Home care aides’ attitudes to training on oral health care. PLoS One. (2021) 16(4):e0249021. doi: 10.1371/journal.pone.0249021
160. Julin A. (2020). “We Don’t have a Choice–We Need to Change!” A Case Study on Experienced Efficiency and the Manager Role in the Home Care. Thesis. Lund University, Department of Political Science. Available online at: https://lup.lub.lu.se/luur/download?func=downloadFile&recordOId=9009734&fileOId=9016272
161. Kelly CM, Morgan JC, Jason KJ. Home care workers: interstate differences in training requirements and their implications for quality. J Appl Gerontol. (2013) 32(7):804–32. doi: 10.1177/0733464812437371
162. Hoge MA, McFaul M, Cauble LL, Craft KL, Paris M Jr, Calcote RM. Building the skills of direct care workers: the Alaskan core competencies initiative. J Rural Mental Health. (2016) 40(1):31–9. doi: 10.1037/rmh0000045
163. Walsh W, Meyer C, Cyarto E V. Home care worker-supported exercise program to address falls: a feasibility study. Aust J Prim Health. (2023) 29:650–60. (Advance online publication). doi: 10.1071/PY22248
164. Filmer T, Herbig B. A training intervention for home care nurses in cross-cultural communication: an evaluation study of changes in attitudes, knowledge and behaviour. J Adv Nurs. (2020) 76(1):147–62. doi: 10.1111/jan.14133
165. Meyer-Kühling I, Wendelstein B, Pantel J, Specht-Leible N, Zenthöfer A, Schröder J. A contribution to improve communication between professional caregivers and physicians. Pflege. (2015) 28(5):277–85. doi: 10.1024/1012-5302/a000447
166. Kessler I, Steils N, Esser A, Grant D. Understanding career development and progression from a healthcare support worker perspective. Part 1/2. Br J Healthc Assist. (2021) 15(11):526–31. doi: 10.12968/bjha.2021.15.11.526
167. Kessler I, Steils N, Esser A, Grant D. Understanding career development and progression from a healthcare support worker perspective. Part 2. Br J Healthc Assist. (2022) 16(1):6–10. doi: 10.12968/bjha.2022.16.1.6
168. Palesy D. Home health aide training: an appeal for organizational support. Home Healthc Now. (2016) 34(7):381–7. doi: 10.1097/NHH.0000000000000418
169. Kelleher D, Lord K, Duffy L, Rapaport P, Barber J, Manthorpe J, et al. Time to reflect is a rare and valued opportunity; a pilot of the NIDUS-professional dementia training intervention for homecare workers during the COVID-19 pandemic. Health Soc Care Community. (2022) 30(5):e2928–39. doi: 10.1111/hsc.13737
170. Josset JM, Lavoyer F, Pâme P. Humanizing care through self-observation and the sharing of professional practices. Feedback from a training session in home caregiving services. Rech Soins Infirm. (2018) 135(4):55–9. doi: 10.3917/rsi.135.0055
171. Blau G, Chapman SA, Neri M. Testing the impact of career motivation on knowledge gained versus skills learned for a sample of personal/home care aide trainees. Career Dev Int. (2016a) 21(2):144–59. doi: 10.1108/CDI-11-2015-0149
172. Blau G, Chapman SA, Neri MT. Testing the relationship between personal/home care aide trainees’ career goals and their commitment to home care. Home Health Care Manag Pract. (2016b) 28:150–4. doi: 10.1177/1084822315620146
173. Stone RI, Bryant NS. The future of the home care workforce: training and supporting aides as members of home-based care teams. J Am Geriatr Soc. (2019) 67:S444–8. doi: 10.1111/jgs.15846
174. Olson R, Hess JA, Parker KN, Thompson SV, Rameshbabu A, Luther Rhoten K, et al. From research-to-practice: an adaptation and dissemination of the COMPASS program for home care workers. Int J Environ Res Public Health. (2018) 15(12):2777 . doi: 10.3390/ijerph15122777
175. Pitkälä KH, Finne-Soveri H, Immonen S, Lehti T, Tiilikainen I, Vesterinen T, et al. Interdisciplinary team education promotes innovations in the home care of older people. Educ Gerontol. (2018) 44(4):276–87. doi: 10.1080/03601277.2018.1465283
176. Boscart V, McCleary L, Stolee P, Taucar LS, Wilhelm J, Johnson K, et al. Enhancing nursing home care for seniors: impact of a living classroom on nursing assistant’s education. Educ Gerontol. (2020) 46(8):461–72. doi: 10.1080/03601277.2020.1774842
177. Tafvelin S, Stenling A, Lundmark R, Westerberg K. Aligning job redesign with leadership training to improve supervisor support: a quasi-experimental study of the integration of HR practices. Eur J Work Org Psychol. (2019) 28(1):74–84. doi: 10.1080/1359432X.2018.154188
178. Adisso ÉL, Taljaard M, Stacey D, Brière N, Zomahoun HTV, Durand PJ, et al. Shared decision-making training for home care teams to engage frail older adults and caregivers in housing decisions: stepped-wedge cluster randomized trial. JMIR Aging. (2022) 5(3):e39386. doi: 10.2196/39386
179. Bookey-Bassett S. Feasibility testing of an interprofessional education intervention to support collaborative practice in home care for older stroke survivors with multiple chronic conditions. J Interprof Care. (2023) 38(1):121–32. (Advance online publication). doi: 10.1080/13561820.2023.2262511
180. Luz C, Hanson K. Filling the care gap: personal home care worker training improves job skills, status, and satisfaction. Home Health Care Manag Pract. (2015a) 27(4):230–7. doi: 10.1177/1084822315584316
181. Luz C, Hanson K. Training the personal and home care aide workforce: challenges and solutions. Home Health Care Manag Pract. (2015b) 27(3):150–3. doi: 10.1177/1084822314566301
182. Akaragian S, Crooks H, Pieters HC. Perspectives of unlicensed assistive personnel on career development. J Contin Educ Nurs. (2013) 44(9):415–23. doi: 10.3928/00220124-20130716-48
183. Stonehouse D. Appraisal and its benefits for the support worker. Br J Healthc Assist. (2013) 07:246–9. doi: 10.12968/bjha.2013.7.5.246
184. Liao L, Xiao LD, Chen H, Wu XY, Zhao Y, Hu M, et al. Nursing home staff experiences of implementing mentorship programmes: a systematic review and qualitative meta-synthesis. J Nurs Manag. (2020) 28(2):188–98. doi: 10.1111/jonm.12876
185. Fitzpatrick JM, Bianchi LA, Hayes N, Da Silva T, Harris R. Professional development and career planning for nurses working in care homes for older people: a scoping review. Int J Older People Nurs. (2023) 18:e12519. doi: 10.1111/opn.12519
186. Donovan P, Haydon A. From support worker to district nurse team manager: a narrative. Br J Healthc Assist. (2020) 14(3):110–4. doi: 10.12968/bjha.2020.14.3.110
187. Burger S, Hay H, Casañas i, Comabella C, Poots A, Perris A. Exploring Education and Training in Relation to Older People’s Health and Social Care. Oxford, UK: Picker Institute Europe (2018). pp. 118. Available online at: https://dunhillmedical.org.uk/wp-content/uploads/2021/08/18-08P1.pdf
188. Kaldy J. Building the Way to Advancement with Career Pathways. Washington, DC: Provider Magazine (2023). Available online at: https://www.providermagazine.com/Issues/2023/Fall/Pages/Building-the-Way-to-Advancement-with-Career-Pathways.aspx
189. Bradley P. How to do the care certificate standards in 10h, for £36. Br J Healthc Assist. (2015) 9:11. (Health Matters). doi: 10.12968/bjha.2015.9.11.530
190. Snyder CR, Dahal A, Frogner BK. Occupational mobility among individuals in entry-level healthcare jobs in the USA. J Adv Nurs. (2018) 74(7):1628–38. doi: 10.1111/jan.13577
191. Kemeny ME, Mabry JB. Making meaningful improvements to direct care worker training through informed policy: understanding how care setting structure and culture matter. Gerontol Geriatr Educ. (2017) 38(3):295–312. doi: 10.1080/02701960.2015.1103652
192. Luz CC, Hanson KV, Hao Y, Spurgeon E. Improving patient experiences and outcomes through personal care aide training. J Patient Exp. (2018) 5(1):56–62. doi: 10.1177/2374373517724349
193. Fong MC, Russell D, Brickner C, Gao O, Vito S, McDonald M. Medicaid long-term care workforce training intervention and value-based payment metrics. Health Serv Res. (2022) 57(2):340–50. doi: 10.1111/1475-6773.13930
194. Ayalon L, Shinan-Altman S. Tension between reality and visions: lessons from an evaluation of a training program of paid elder care workers. Health Soc Care Community. (2021) 29(6):1915–24. doi: 10.1111/hsc.13305
195. Shinan-Altman S, Riabzev A, Ayalon L. Mixed motivations to provide formal care to older adults: lessons from a training program. Int Psychogeriatr. (2019) 31(3):341–9. doi: 10.1017/S1041610218000868
196. Atkinson C, Crozier S, Lewis L. Factors that Affect the Recruitment and Retention of Domiciliary Care Workers and the Extent to which These Factors Impact Upon the Quality of Domiciliary Care: Interim Findings Summary. Cardiff, Wales: Welsh Government Social Research (2016). pp. 10. Available online at: https://www.gov.wales/sites/default/files/statistics-and-research/2019-07/160118-factors-affect-recruitment-retention-domiciliary-care-workers-interim-en.pdf
197. Zhang T, Zhang L, Wen X, Li H. Level of humanistic care ability and its influencing factors among nursing aides in long-term care facilities. Geriatric Nurs (New York, N.Y.). (2023) 52:56–62. doi: 10.1016/j.gerinurse.2023.05.007
198. Skills for Care. Being a Personal Assistant. Leeds, UK: Skills for Care (2020). pp. 28. Available online at: https://www.skillsforcare.org.uk/Recruitment-support/Support-individual-employers-PAs/Personal-Assistant/Hear-from-personal-assistants.aspx
199. Martyn J, Wilkinson A, Zanella S. Identifying the continuing education needs of personal care workers in two residential aged care facilities by an appreciative inquiry study. Collegian. (2022) 29(6):887–93. doi: 10.1016/j.colegn.2022.09.009
200. Poh L, Tan SY, Lim J. Governance of assisted living in long-term care: a systematic literature review. Int J Environ Res Public Health. (2021) 18(21):11352. doi: 10.3390/ijerph182111352
201. Castle NG, Furnier J, Ferguson-Rome JC, Olson D, Johs-Artisensi J. Quality of care and long-term care administrators’ education: does it make a difference? Health Care Manage Rev. (2015) 40(1):35–45. doi: 10.1097/HMR.0000000000000007
202. Timonen V, Lolich L. “The poor carer”: ambivalent social construction of the home care worker in elder care services. J Gerontol Soc Work. (2019) 62(7):728–48. doi: 10.1080/01634372.2019.1640334
203. Banijamali S, Jacoby D, Hagopian A. Characteristics of home care workers who leave their jobs: a cross-sectional study of job satisfaction and turnover in Washington state. Home Health Care Serv Q. (2014) 33(3):137–58. doi: 10.1080/01621424.2014.929068
204. Gebhard D, Wimmer M. The hidden script of work-related burdens in home care—a cross over mixed analysis of audio diaries. J Appl Gerontol. (2023) 42(4):704–16. doi: 10.1177/07334648221130747
205. Phoo NNN, Reid A. Determinants of violence towards care workers working in the home setting: a systematic review. Am J Ind Med. (2022) 65(6):447–67. doi: 10.1002/ajim.23351
206. Solis C, Mintz KT, Wasserman D, Fenton K, Danis M. Home care in America: the urgent challenge of putting ethical care into practice. Hastings Cent Rep. (2023) 53(3):25–34. doi: 10.1002/hast.1487
207. Womack KN, Alvord TW, Trullinger-Dwyer CF, Rice SPM, Olson R. Challenging aggressive behaviors experienced by personal support workers in comparison to home care workers: relationships between caregiver experiences and psychological health. Int J Environ Res Public Health. (2020) 17(15):5486. doi: 10.3390/ijerph17155486
208. Yeh IL, Samsi K, Vandrevala T, Manthorpe J. Constituents of effective support for homecare workers providing care to people with dementia at end of life. Int J Geriatr Psychiatry. (2019) 34(2):352–9. doi: 10.1002/gps.5027
209. Byon HD, Lee M, Choi M, Sagherian K, Crandall M, Lipscomb J. Prevalence of type II workplace violence among home healthcare workers: a meta-analysis. Am J Ind Med. (2020) 63(5):442–55. doi: 10.1002/ajim.23095
210. Bien E, Davis K, Gillespie G. Home healthcare workers’ occupational exposures. Home Healthc Now. (2020) 38(5):247–53. doi: 10.1097/NHH.0000000000000891
211. Bien EA, Davis KG, Small TF, Reutman S, Gillespie GL. Design and development of the home healthcare worker observation tool. J Nurs Educ Pract. (2021) 11(9):29–38. doi: 10.5430/jnep.v11n9p29
212. Huang SF, Liao JY. Home care aides’ perspectives of occupational tobacco smoke exposure: a Q methodology study. Nicotine Tob Res. (2023) 25(10):1641–7. doi: 10.1093/ntr/ntad087
213. Muramatsu N, Yin L, Lin TT. Building health promotion into the job of home care aides: transformation of the workplace health environment. Int J Environ Res Public Health. (2017) 14(4):384. doi: 10.3390/ijerph14040384
214. Muramatsu N, Sokas RK, Lukyanova VV, Zanoni J. Perceived stress and health among home care aides: caring for older clients in a medicaid-funded home care program. J Health Care Poor Underserved. (2019) 30(2):721–38. doi: 10.1353/hpu.2019.0052
215. Tang B, Mamubieke M, Jilili M, Liu L, Yang B. Amelioration and deterioration: social network typologies and mental health among female domestic workers in China. Front Public Health. (2022) 10:899322. doi: 10.3389/fpubh.2022.899322
216. Beavis J, Davis L, McKenzie S. Clinical supervision for support workers in paediatric palliative care: a literature review. Clin Child Psychol Psychiatry. (2021) 26(1):191–206. doi: 10.1177/1359104520961431
217. Beavis J, McKenzie S, Davis L, Ellison N. Implementation and evaluation of clinical supervision for support workers in a paediatric palliative care setting. Clin Child Psychol Psychiatry. (2022) 27(2):369–84. doi: 10.1177/13591045211055565
218. Tsui EK, Franzosa E, Cribbs KA, Baron S. Home care workers’ experiences of client death and disenfranchised grief. Qual Health Res. (2019) 29(3):382–92. doi: 10.1177/1049732318800461
219. Carr S. Pay, Conditions and Care Quality in Residential, Nursing and Domiciliary Services. York, UK: Joseph Rowntree Foundation (2014). pp. 8. Available online at: https://myhomelife.org.uk/wp-content/uploads/2015/02/JRF-report-on-care-pay-conditions-summary.pdf
220. Gleason HP. The Effect of Job Demands, Control, and Support on Job Satisfaction and Intent to Leave Among Massachusetts Home Health and Supportive Home Care Aides. Boston: University of Massachusetts Boston (2020). (Doctoral dissertation).
221. Gleason HP, Miller EA, Boerner K. Focusing on the positive: home health aides’ desire for autonomy and control. J Appl Gerontol. (2023) 42(4):728–36. doi: 10.1177/07334648221145177
222. Karmacharya I, Janssen LM, Brekke B. “Let them know that they’re appreciated”: the importance of work culture on direct care worker retention. J Gerontol Nurs. (2023) 49(8):7–13. doi: 10.3928/00989134-20230706-03
223. Tangchitnusorn K, Prachuabmoh V. Motivation and quality of work life of in-home paid caregivers of older adults. J Appl Gerontol. (2023) 42(4):737–46. doi: 10.1177/07334648221145167
224. Boström AM, Lundgren D, Kabir ZN, Kåreholt I. Factors in the psychosocial work environment of staff are associated with satisfaction with care among older persons receiving home care services. Health Soc Care Community. (2022) 30(6):e6080–90. doi: 10.1111/hsc.14045
225. Assander S, Bergström A, Olt H, Guidetti S, Boström AM. Individual and organisational factors in the psychosocial work environment are associated with home care staffs’ job strain: a Swedish cross-sectional study. BMC Health Serv Res. (2022) 22(1):1418. doi: 10.1186/s12913-022-08699-4
226. Gebhard D, Neumann J, Wimmer M, Mess F. The second side of the coin-resilience, meaningfulness and joyful moments in home health care workers during the COVID-19 pandemic. Int J Environ Res Public Health. (2022) 19(7):3836. doi: 10.3390/ijerph19073836
227. Hsu W, Shih FP. Key factors for enhancing home care workers’ intention to stay by multiple-criteria decision analysis. Healthcare (Basel, Switzerland). (2023) 11(5):750. doi: 10.3390/healthcare11050750
228. Work Foundation Total Jobs. Social Care: a Guide to Attracting and Retaining a Thriving Workforce. London, UK: University of Lancaster (2021). pp. 20. Available online at: https://www.lancaster.ac.uk/media/lancaster-university/content-assets/documents/lums/work-foundation/reports/SocialCareGuide.pdf
229. McCreary DDJ. Home health nursing job satisfaction and retention: meeting the growing need for home health nurses. Nurs Clin North Am. (2020) 55(1):121–32. doi: 10.1016/j.cnur.2019.11.002
230. Ruotsalainen S, Jantunen S, Sinervo T. Which factors are related to Finnish home care workers’ job satisfaction, stress, psychological distress and perceived quality of care?—a mixed method study. BMC Health Serv Res. (2020) 20:896. doi: 10.1186/s12913-020-05733-1
231. Sayin FK, Denton M, Brookman C, Davies S, Chowhan J, Zeytinoglu IU. The role of work intensification in intention to stay: a study of personal support workers in home and community care in Ontario Canada. Econ Ind Democr. (2021) 42(4):917–36. doi: 10.1177/0143831X18818325
232. Hamblin K, Manthorpe J. How Can We Create Better Jobs in Care? Sheffield, UK: University of Sheffield (2018). p. 4. (CIRCLE).
233. Ohta R, Ryu Y, Katsube T. Home care workers’ judgments about users’ acute conditions: a qualitative study on interprofessional collaboration. Home Health Care Serv Q. (2020) 39(3):184–95. doi: 10.1080/01621424.2020.1736228
234. Kurata S, Ojima T. Knowledge, perceptions, and experiences of family caregivers and home care providers of physical restraint use with home-dwelling elders: a cross-sectional study in Japan. BMC Geriatr. (2014) 14:1–11. doi: 10.1186/1471-2318-14-39
235. Backhouse T, Ruston A, Killett A, Ward R, Rose-Hunt J, Mioshi E. Risks and risk mitigation in homecare for people with dementia-a two-sided matter: a systematic review. Health Soc Care Community. (2022) 30(6):2037–56. doi: 10.1111/hsc.13865
236. Koru G, Alhuwail D, Jademi O, Uchidiuno U, Rosati RJ. Technology innovations for better fall risk management in home care. J Gerontol Nurs. (2018) 44(7):15–20. doi: 10.3928/00989134-20180412-01
237. Brouillette NM, Markkanen PK, Quinn MM, Galligan CJ, Sama SR, Lindberg JE, et al. Aide and client safety “should go hand-in-hand”: qualitative findings from home care aides, clients, and agency leaders. J Appl Gerontol. (2023) 42(4):571–80. doi: 10.1177/07334648221146769
238. Grønoset Grasmo S, Frostad Liaset I, Redzovic SE. Home health aides’ experiences of their occupational health: a qualitative meta-synthesis. Home Health Care Serv Q. (2021) 40(2):148–76. doi: 10.1080/01621424.2021.1921650
239. Small T. Occupational hazards in home care. Home Healthc Now. (2020) 38(4):221. doi: 10.1097/NHH.0000000000000895
240. Schoenfisch AL, Lipscomb H, Phillips LE. Safety of union home care aides in Washington state. Am J Ind Med. (2017) 60(9):798–810. doi: 10.1002/ajim.22747
241. Swedberg L, Chiriac EH, Törnkvist L, Hylander I. From risky to safer home care: health care assistants striving to overcome a lack of training, supervision, and support. Int J Qual Stud Health Well-Being. (2013) 8:20758. doi: 10.3402/qhw.v8i0.20758
242. Hines D. Cultural competence: assessment and education resources for home care and hospice clinicians. Home Healthc Nurse. (2014) 32(5 Suppl):S4–11. doi: 10.1097/NHH.0000000000000080
243. Puustinen J, Kangasniemi M, Pasanen M, Turjamaa R. Recognising older people’s individual resources and home-care-specific tasks in home care in Finland: a document analysis of care and service plans. Scand J Caring Sci. (2023) 37(2):507–23. doi: 10.1111/scs.13135
244. Turjamaa R, Hartikainen S, Kangasniemi M, Pietilä AM. Is it time for a comprehensive approach in older home care clients’ care planning in Finland? Scand J Caring Sci. (2015) 29(2):317–24. doi: 10.1111/scs.12165
245. Brown P, Leverton M, Burton A, Harrison-Dening K, Beresford-Dent J, Cooper C. How does the delivery of paid home care compare to the care plan for clients living with dementia? Health Soc Care Community. (2022) 30(5):e3158–70. doi: 10.1111/hsc.13761
246. Sjöberg Forssberg K, Parding K, Vänje A. Conditions for workplace learning: a gender divide? J Workplace Learn. (2021) 33(4):302–14. doi: 10.1108/JWL-08-2020-0134
247. Faul AC, Schapmire TJ, D’Ambrosio J, Feaster D, Oak CS, Farley A. Promoting sustainability in frontline home care aides: understanding factors affecting job retention in the home care workforce. Home Health Care Manag Pract. (2010) 22(6):408–16. doi: 10.1177/1084822309348896
248. Lolich L, Timonen V. Fortunate and fearful: emotions evoked by home-care policies for older people in Ireland. Emot Soc. (2020) 2(1):61–78. doi: 10.1332/263169020X15843025702815
249. Snyder RE. Commentary on the future of the home care workforce: training and supporting aides as members of home-based care teams. J Am Geriatr Soc. (2019) 67(S2):S449–50. doi: 10.1111/jgs.15868
250. Bensliman R, Casini A, Mahieu C. “Squeezed like a lemon”: a participatory approach on the effects of innovation on the well-being of homecare workers in Belgium. Health Soc Care Community. (2022) 30(4):e1013–24. doi: 10.1111/hsc.13506
251. Wilberforce M, Abendstern M, Tucker S, Ahmed S, Jasper R, Challis D. Support workers in community mental health teams for older people: roles, boundaries, supervision and training. J Adv Nurs. (2017) 73(7):1657–66. doi: 10.1111/jan.13264
252. Karlsson ND, Markkanen PK, Kriebel D, Galligan CJ, Quinn MM. “That’s not my job”: a mixed methods study of challenging client behaviors, boundaries, and home care aide occupational safety and health. Am J Ind Med. (2020) 63(4):368–78. doi: 10.1002/ajim.23082
253. Torres JM, Kietzman KG, Wallace SP. Walking the line: navigating market and gift economies of care in a consumer-directed home-based care program for older adults. Milbank Q. (2015) 93(4):732–60. doi: 10.1111/1468-0009.12163
254. Turner N, Schneider J, Pollock K, Travers C, Perry-Young L, Wilkinson S. “Going the extra mile” for older people with dementia: exploring the voluntary labour of homecare workers. Dementia (London, England). (2020) 19(7):2220–33. doi: 10.1177/1471301218817616
255. Guardian Professional. Attitudes to Homecare in England: Research Conducted by Guardian Professional in Association with Department of Health: Top Line Findings. London, UK: Guardian Professional (2013). pp. 38. Available online at: https://static.guim.co.uk/ni/1383067901570/Homecare-survey-full-result.pdf?guni=Article:in%20body%20link
256. Kelly C. Exploring experiences of personal support worker education in Ontario, Canada. Health Soc Care Community. (2017) 25(4):1430–8. doi: 10.1111/hsc.12443
257. Cataldo F, Kielmann K, Kielmann T, Mburu G, Musheke M. ‘Deep down in their heart, they wish they could be given some incentives’: a qualitative study on the changing roles and relations of care among home-based caregivers in Zambia. BMC Health Serv Res. (2015) 15:36. doi: 10.1186/s12913-015-0685-7
258. Chabouh S, El-Amraoui A, Hammami S, Bouchriha H. A systematic review of the home health care planning literature: emerging trends and future research directions. Decis Anal J. (2023) 7:100215. doi: 10.1016/j.dajour.2023.100215
259. Nisbet E, Morgan JC. Where policy meets practice: employer perspectives on scheduling and hours for home care aides. J Appl Gerontol. (2019) 38(11):1615–34. doi: 10.1177/0733464817739153
260. Andersen GR, Westgaard RH. Understanding significant processes during work environment interventions to alleviate time pressure and associated sick leave of home care workers–a case study. BMC Health Serv Res. (2013) 13:477. doi: 10.1186/1472-6963-13-477
261. Andersen GR, Westgaard RH. Discrepancies in assessing home care workers’ working conditions in a Norwegian home care service: differing views of stakeholders at three organizational levels. BMC Health Serv Res. (2015) 15:286. doi: 10.1186/s12913-015-0945-6
262. Johannessen T, Ree E, Aase I, Bal R, Wiig S. Exploring challenges in quality and safety work in nursing homes and home care—a case study as basis for theory development. BMC Health Serv Res. (2020) 20:277. doi: 10.1186/s12913-020-05149-x
263. Grasmo SG, Liaset IF, Redzovic SE. Home care workers’ experiences of work conditions related to their occupational health: a qualitative study. BMC Health Serv Res. (2021) 21(1):962. doi: 10.1186/s12913-021-06941-z
264. Busnel C, Vallet F, Ashikali EM, Ludwig C. Assessing multidimensional complexity in home care: congruencies and discrepancies between patients and nurses. BMC Nurs. (2022) 21(1):166. doi: 10.1186/s12912-022-00942-x
265. Habibnejad-Ledari H, Rabbani M, Ghorbani-Kutenaie N. Solving a multi-objective model toward home care staff planning considering cross-training and staff preferences by NSGA-II and NRGA. Scientia Iranica. (2019) 26(5):2919–35. doi: 10.24200/sci.2018.20800
266. Shiri M, Ahmadizar F, Thiruvady D, Farvaresh H. A sustainable and efficient home health care network design model under uncertainty. Expert Syst Appl. (2023) 211:118185. doi: 10.1016/j.eswa.2022.118185
267. Liaset IF, Fimland MS, Holtermann A, Mathiassen SE, Redzovic S. Can home care work be organized to promote health among the workers while maintaining productivity? An investigation into stakeholders’ perspectives on organizational work redesign concepts based on the goldilocks work principles. BMC Health Serv Res. (2023) 23(1):667. doi: 10.1186/s12913-023-09691-2
268. Polacsek M, Goh A, Malta S, Hallam B, Gahan L, Cooper C, et al. “I know they are not trained in dementia”: addressing the need for specialist dementia training for home care workers. Health Soc Care Community. (2020) 28(2):475–84. doi: 10.1111/hsc.12880
269. Costa C, Girace E, Fanton E, Stevanin S, Tasca T, Mantoan D. National survey to verify the implementation of state-regions agreements introducing the professional profile of health social care worker and instituting a complementary training program for nursing assistants, Italy. Ig Sanita Pubbl. (2019) 75(3):201–10.31645062
270. Backhouse T, Ruston A. Home-care workers’ experiences of assisting people with dementia with their personal care: a qualitative interview study. Health Soc Care Community. (2022) 30(3):e749–59. doi: 10.1111/hsc.13445
271. Gallotti M. Migrant Domestic Workers Across the World. Geneva, Switzerland: International Labour Organization (2015). (Based on the ILO Report on Global Estimates on Migrant Workers). Available online at: https://associazionedomina.it/wp-content/uploads/2017/05/Migrant-Domestic-Workers-Across-the-World.pdf
272. Yuan Q, Zhang Y, Samari E, Jeyagurunathan A, Tan GTH, Devi F, et al. The impact of having foreign domestic workers on informal caregivers of persons with dementia—findings from a multi-method research in Singapore. BMC Geriatr. (2022) 22(1):305. doi: 10.1186/s12877-022-03002-w
273. Malhotra R, Arambepola C, Tarun S, de Silva V, Kishore J, Østbye T. Health issues of female foreign domestic workers: a systematic review of the scientific and gray literature. Int J Occup Environ Health. (2013) 19(4):261–77. doi: 10.1179/2049396713Y.0000000041
274. Tam WJ, Koh GC, Legido-Quigley H, Ha NHL, Yap PLK. “I can’t do this alone”: a study on foreign domestic workers providing long-term care for frail seniors at home. Int Psychogeriatr. (2018) 30(9):1269–77. doi: 10.1017/S1041610217002459
275. Ha NHL, Chong MS, Choo RWM, Tam WJ, Yap PLK. Caregiving burden in foreign domestic workers caring for frail older adults in Singapore. Int Psychogeriatr. (2018) 30(8):1139–47. doi: 10.1017/S1041610218000200
276. Ow Yong B, Manthorpe J. The experiences of Indian migrant care home staff working with people with dementia: a pilot study exploring cultural perspectives. WWOP. (2016) 20(1):3–13. doi: 10.1108/WWOP-07-2015-0012
277. Macdonald MT, Lang A, Storch J, Stevenson L, Barber T, Iaboni K, et al. Examining markers of safety in homecare using the international classification for patient safety. BMC Health Serv Res. (2013) 13:191. doi: 10.1186/1472-6963-13-191
278. Tang X, Chen X, Pang Y, Zhou L. The development of quality indicators for home care in China. Int J Qual Health Care. (2018) 30(3):208–18. doi: 10.1093/intqhc/mzx202
279. Foong HY, Siette J, Jorgensen M. Quality indicators for home- and community-based aged care: a critical literature review to inform policy directions. Australas J Ageing. (2022) 41(3):383–95. doi: 10.1111/ajag.13103
280. Kim EY, Yeom HE. Influence of home care services on caregivers’ burden and satisfaction. J Clin Nurs. (2016) 25(11-12):1683–92. doi: 10.1111/jocn.13188
281. Ramaboa KKKM, Fredericks I. Demographic characteristics associated with the likelihood to use paid home care for people with dementia among South African Muslims. Dement Geriatr Cogn Disord. (2019) 48(5-6):337–48. doi: 10.1159/000506511
282. Fabius CD, Parker LJ. Paid help and caregiving experiences of black caregivers of community-dwelling older adults. Clin Gerontol. (2023) 46(1):91–100. doi: 10.1080/07317115.2022.2099776
283. Eltaybani S, Kitamura S, Fukui C, Igarashi A, Sakka M, Noguchi-Watanabe M, et al. Toward developing care outcome quality indicators for home care for older people: a prospective cohort study in Japan. Geriatr Gerontol Int. (2023) 23(5):383–94. doi: 10.1111/ggi.14578
284. McGilton KS, Rochon E, Sidani S, Shaw A, Ben-David BM, Saragosa M, et al. Can we help care providers communicate more effectively with persons having dementia living in long-term care homes? Am J Alzheimer’s Dis Dement. (2017) 32(1):41–50. doi: 10.1177/1533317516680899
285. Franzosa E, Tsui EK, Baron S. Home health aides’ perceptions of quality care: goals, challenges, and implications for a rapidly changing industry. New Solut. (2018) 27(4):629–47. doi: 10.1177/1048291117740818
286. Colak M, Gokdemir O, Yaprak S, Kartal M. Evaluation of home care services at a training and research hospital in izmir. Marmara Med J. (2016) 23(3):170–6. doi: 10.5472/marumj.281397
287. Green Paper on Home Support Workers. Royal College of Surgeon's Ireland, Funded by Leading Healthcare Partners Skillnet. Dublin (2023). https://www.lhpskillnet.ie/wp-content/uploads/2024/02/Green-Paper-on-Home-Support-Workers-Leading-Healthcare-Providers-Skillnet-December-2023.pdf (accessed February 29, 2024).
Keywords: home support workers, home care, workforce planning, career pathway, ageing population, person-centred care, ageing in place, digital health
Citation: Morrow E, Kelly C, Killeen C, Naessens E and Lynch M (2024) Exploring a career pathway for home support workers in Ireland: a systematic scoping review of the international evidence. Front. Health Serv. 4:1360920. doi: 10.3389/frhs.2024.1360920
Received: 24 December 2023; Accepted: 20 February 2024;
Published: 13 March 2024.
Edited by:
Euan Sadler, University of Southampton, United KingdomReviewed by:
Nina Fudge, Queen Mary University of London, United KingdomAnne Elizabeth Rogers, University of Southampton, United Kingdom
© 2024 Morrow, Kelly, Killeen, Naessens and Lynch. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Elizabeth Morrow ZWxpemFiZXRobW9ycm93QHJjc2kuY29t
 Elizabeth Morrow
Elizabeth Morrow Carmel Kelly2
Carmel Kelly2 Edward Naessens
Edward Naessens Mary Lynch
Mary Lynch