- 1Department of Nutrition, Harvard T.H. Chan School of Public Health, Boston, MA, United States
- 2Seed 2 Roots LLC, Mankato, MN, United States
- 3Department of Agricultural and Resource Economics, Rudd Center for Food Policy and Health, University of Connecticut, Storrs, CT, United States
Much of the chronic disease burden in the U.S. population can be traced to poor diet. There has been a sustained focus on influencing children's diets and encouraging healthier eating habits by changing policies for what foods and beverages can be served to children through large federally-funded nutrition assistance programs. Yet without attention to how nutrition policies are implemented, and the surrounding context for these policies, these policy changes may not have the intended results. In this perspective, we used Bullock et al.'s (2021) Process Model of Implementation from a Policy Perspective to analyze how the complexities of the implementation process of large-scale nutrition policies can dilute potential health outcomes. We examine the Child and Adult Care Food Program (CACFP), a federal program focused on supporting the provision of nutritious meals to over 4 million children attending childcare, as a case study. We examine how the larger societal contexts of food insecurity, attitudes towards the social safety net, and a fragmented childcare system interact with CACFP. We review the “policy package” of CACFP itself, in terms of its regulatory requirements, and the various federal, state, and local implementation agencies that shape CACFP's on-the-ground implementation. We then review the evidence for how each component of the CACFP policy implementation process impacts uptake, costs, feasibility, equity, and effectiveness at improving children's nutrition. Our case study demonstrates how public health researchers and practitioners must consider the complexities of policy implementation processes to ensure effective implementation of nutrition policies intended to improve population health.
1. Introduction
The United States (U.S.) faces substantial public health challenges related to poor nutrition. Diet-related chronic diseases (1)—including heart disease, stroke, type II diabetes mellitus, and certain types of cancer (2, 3)– are experienced by most U.S. adults, contributing to poor health and early mortality (4, 5). Moreover, inequities in access to affordable, nutritious foods have resulted in socioeconomic and racial/ethnic disparities in diet quality (6–8). Income and race are also closely linked with a higher risk of food insecurity (9), which further increases the risk of both poor diet and cardiometabolic diseases (10, 11). These problems start in childhood (2, 12, 13).
To address these population-wide challenges, policymakers have leveraged federal child nutrition assistance programs, such as the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), the National School Lunch and Breakfast Programs (NSLP/SBP), and the Child and Adult Care Food Program (CACFP), as policy levers for achieving public health nutrition goals (14–17). These programs, which provide financial support to improve food security and access for Americans, especially those with lower incomes, show promise for improving diet quality and reducing health inequities. In recent years, efforts to bring minimum nutrition standards for WIC and NSLP/SBP in line with current dietary science have resulted in substantial improvements in the diet quality and chronic disease risk of program participants (18–24), suggesting that policy changes to these programs can be a promising approach to population health. However, similar updates to CACFP appear to have had less strong effects (25).
In this perspective, we use a conceptual framework of policy implementation, developed by Bullock et al. (26), to outline the challenges in leveraging federal nutrition policies as public health interventions. We specifically examine CACFP, which provides reimbursements to child and adult daycare providers to support serving meals and snacks meeting basic nutritional standards (27), as a case study (we focus here solely on childcare providers and child-level outcomes, given that these are the majority beneficiaries of CACFP). Given that CACFP appears to have less consistently strong impacts on child nutrition compared to other federal nutrition programs, we seek to understand how its policy implementation process may explain why.
2. Conceptual framework for the analysis
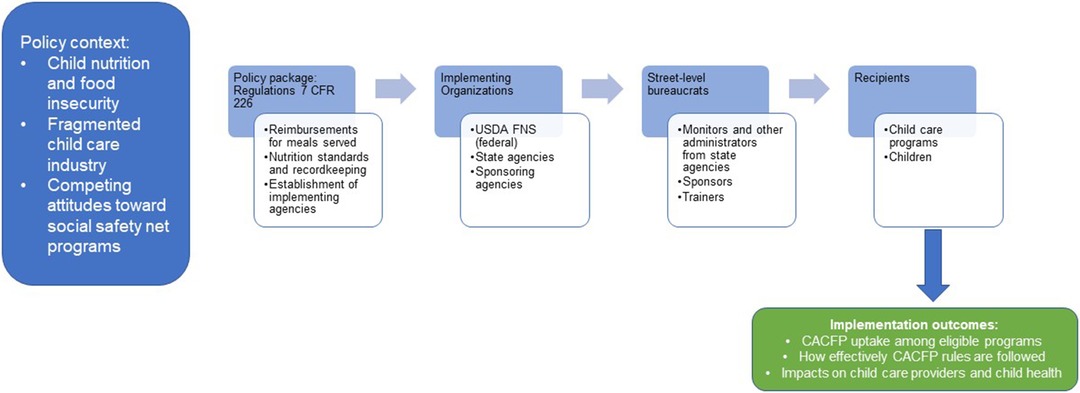
Bullock et al.'s Process Model of Policy Implementation (2021) (26) posits that policies are first borne out of a larger context of existing ideas, interests, and other external factors that determine how a problem is defined and whether it is addressed by policy in the first place. This brings about the development of a policy package, a collection of strategies like regulations or statutes, economic incentives, voluntary guidelines, or information campaigns. The implementation process of the policy package then flows through implementing organizations to street-level bureaucrats to recipients. To evaluate policy implementation, outcomes at several levels can be considered, including implementation outcomes (28) (e.g., fidelity, uptake, acceptability, costs, feasibility, sustainability), service outcomes (e.g., effectiveness, equity, efficiency), recipient outcomes (e.g., changes in actual recipient behavior, satisfaction), and policy/system level outcomes (e.g., reductions in food insecurity at a population level).
Figure 1 presents an adaptation of Bullock et al.'s model for this paper's analysis of CACFP. In the following sections, we explore each of the key phases of the implementation process described in the Process Model—context, developing the policy package, processing through implementing organizations, street-level bureaucrats, and recipients, and finally outcomes—for CACFP.
3. CACFP's implementation process and how its attributes determine implementation outcomes
3.1. Outer context: child food insecurity, child development, the childcare industry, and attitudes towards social safety net programs
CACFP exists in a larger context related to child health, and specifically children's nutrition, in the U.S. Food insecurity currently affects 12.5% of households with children in the U.S. (9). Additionally, even for children not experiencing food insecurity, the nutritional quality of foods available to and consumed by children is often poor, with high amounts of inexpensive, highly palatable ultraprocessed foods (29) and inadequate consumption of vegetables, whole grains, and lean protein sources (12, 30). Several decades ago, a key dietary concern was inadequate intake of essential micronutrients; more recently, overconsumption of foods and beverages that can lead to excess weight gain for healthy growth has become a concern for children (31–36).
While social safety net programs have been designed to mitigate these public health nutrition challenges for households with low incomes, there are disagreements on how comprehensive the programs should be (37).CACFP falls within this challenging context.
This struggle can be seen in CACFP's history (38). CACFP's roots lie in a federal pilot program called the Special Food Service Program for Children, started in 1968, at a time in U.S. history when the social safety net was being radically expanded through President Lyndon B. Johnson's “War on Poverty”. This program was expanded and formalized into CACFP across the 1970s and 1980s providing childcare providers with resources to serve free rather than including meal costs in tuition or not serving meals at all (38). However, in the Personal Responsibility and Work Opportunity Reconciliation Act of 1996—a law which made several safety net programs more difficult to access—CACFP was modified to cut costs. This law reduced the number of meals for which providers could receive reimbursements and introduced an income-based tiering system for reimbursements that reduced the overall financial support most providers could receive and also introduced additional administrative burden (39) to the program, as it necessitated providers' collection of income information for the families they served (38). Although future legislative actions allowed for relatively small expansions of the program after this, little changed about CACFP until 2017, when the nutrition standards for CACFP meals were updated as part of the Healthy, Hunger Free Kids Act of 2010 (40, 41). A report by the National Academies of Medicine in 2011 suggested sweeping changes were needed to bring CACFP meal pattern standards in line with dietary science regarding child health and development (38), yet no additional federal funding was appropriated to support these changes (41).
An additional complexity is how fractured and underfunded the childcare system is in the U.S. Unlike most other economically developed countries; the U.S. has no universal public system of childcare (42). The childcare industry mostly relies on tuition payments from families and depressed wages for childcare workers in order to function (43). The industry has been referred to as a “textbook example” of a broken market (44): parents have to pay so much in tuition that it prohibits many from participating in the workforce at all, educators and other staff are underpaid, and owners are often barely able to keep the programs breaking even. Childcare providers and educators, who face substantial physical and mental health challenges personally (45), thus often face multiple intense challenges related to simply maintaining operations and adhering to their state's existing regulatory requirements. In this organizational context, participating in CACFP, or even serving meals in the first place, can add an additional layer of complexity to an already challenging situation.
3.2. Policy package: what are the regulations and unofficial rules that make up CACFP?
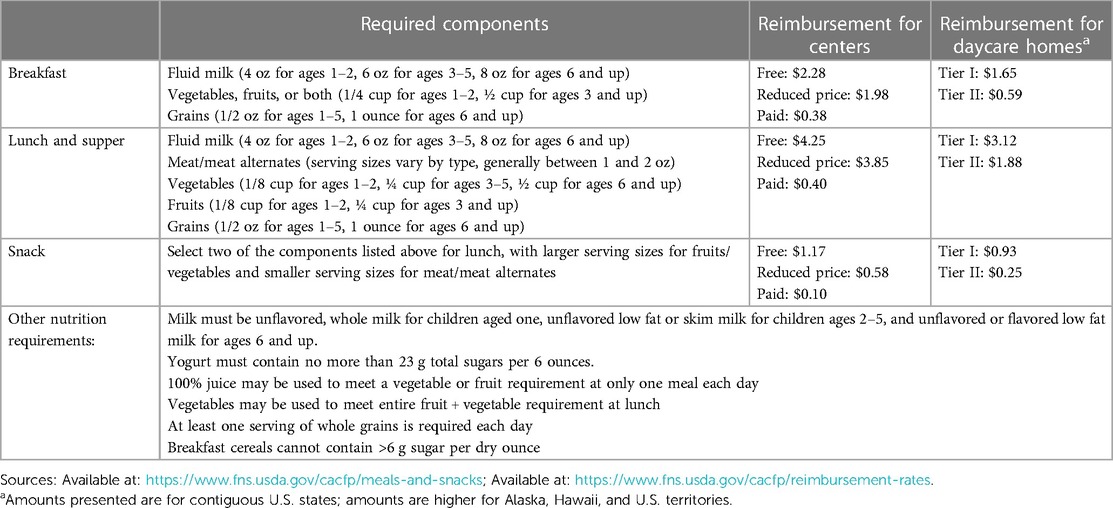
The regulations for CACFP (7 CFR Part 226) (46) outline minimum requirements for foods and beverages served for various age groups (see Table 1). Participating providers can receive reimbursements for up to three meals and/or snacks. The reimbursement amount for centers varies according to the household income status of the recipient child; reimbursements for family childcare providers (who provide care in their home to a smaller group of children compared to childcare centers) vary based on neighborhood-level income metrics (using either Census or local school meals data) (46). To participate in CACFP, providers must prove that they either have a nonprofit status or that they serve at least 25% of children from low income households (47) and must prove financial viability (46). They must submit paperwork on the foods and beverages served for each meal, the amounts served, and child attendance as well as documentation of receipts and compliance with civil rights law. Providers and key staff participate in annual trainings and periodic monitoring visits from state auditors to assess compliance (46).
3.3. Implementing organizations and street-level bureaucrats: who implements CACFP?
CACFP is a federal program that is administered by state agencies. At the federal level, the U.S. Department of Agriculture Food and Nutrition Service (USDA FNS) tracks participation, issues guidance to state agencies on how to comply with regulations, releases technical assistance tools (like recipes and worksheets), and commissions program evaluations. State agencies, however—typically education or public health agencies—are the organizations that are responsible for most administrative activities, including approving and onboarding new participating providers, disbursing reimbursements, monitoring compliance, providing technical assistance, and maintaining participation records (48).
The state agency is also responsible for registering and working with sponsoring agencies or sponsors, which also support implementation. Family childcare providers are required to work with sponsors so that these agencies can complete some of their administrative paperwork and provide technical assistance; depending on the state, some centers can also work with sponsors, or operate independently (49).
The “street-level bureaucrats” involved in implementing CACFP on the ground are state agency staff responsible for auditing participating programs and sponsors, as well as sponsors themselves, who help participating providers comply with program rules.
3.4. Recipients: childcare programs and children
One unusual aspect of CACFP is that childcare providers can be thought of both as the recipients of the program—they receive the reimbursements for the meals they serve—and also a type of “street-level bureaucrat” as they are implementing the program day-to-day: planning menus, obtaining or preparing food, gathering families' income-eligibility information, participating in training, maintaining paperwork, and submitting to monitoring visits. The other recipients of the program are the children receiving the meals and snacks.
3.5. Outcomes: what do we know about CACFP's impact?
3.5.1. Implementation outcomes
These include acceptability, adoption, appropriateness, costs, feasibility, fidelity, uptake (penetration), and sustainability (26, 28). We present evidence for four of these constructs with existing evidence below.
3.5.1.1. Penetration
While the USDA estimates that CACFP served up to 4.6 million children in 2021, it does not track the percentage of eligible programs that participate. A recent analysis of state administrative records, however, estimated that only about a third of licensed childcare centers participate in CACFP nation-wide, with large variability across states (16%–86%) (50).
3.5.1.2. Fidelity
Studies of the degree to which programs adhere to CACFP's regulatory standards generally suggest that programs meet the standards most of the time, but not perfectly (25, 51, 52).
3.5.1.3. Feasibility
Providers have consistently reported that CACFP is difficult to use, citing the burden of paperwork, inadequate staff, insufficient reimbursements, mismatch of the meal pattern standards with child preferences, and inflexibility of the standards for cultural foods as being key barriers to feasibility (53–56).
3.5.1.4. Cost
Although CACFP reimburses providers for each qualifying meal and snack served (as described above), many studies have found that the reimbursement is not adequate. While some studies have found that the reimbursement covers the costs of food (57–59), studies have also found that the reimbursement is not adequate for supporting foods with more variety that can improve diet quality and support children's preferences (60, 61), and that the reimbursement is not adequate to cover labor costs (59).
3.5.2. Service outcomes
Include efficiency, safety, effectiveness, equity, client-centeredness, and timeliness (26, 28). We present analysis for four of these constructs with existing evidence below.
3.5.2.1. Efficiency
As described above, there are substantial monitoring activities involved that make CACFP's efficiency questionable. Daily meal and attendance counts, menu planning, managing food receipts to demonstrate compliance, reviewing food labels to assess whether foods are creditable, and also the work involved in soliciting and organizing income-eligibility paperwork from parents all contribute to substantial administrative burden (39).
3.5.2.2. Effectiveness
A recent systematic review of studies of the impact of CACFP on the nutritional quality of meals served in childcare programs found mixed evidence overall for a beneficial impact of CACFP, partly due to a lack of rigorous, large-scale studies. Existing studies either find null associations between CACFP and nutritional quality or typically very small positive associations (62).
3.5.2.3. Equity
It is unknown whether CACFP is accessed inequitably. There are concerns, however, in how programs located in food deserts—which often track with both rural locale and with areas subjected to racialized segregation (63, 64)—may have difficulty accessing foods compliant with CACFP meal pattern standards. Additionally, the administrative burden of this program itself may produce inequities. Childcare providers serving higher income families can opt out of CACFP. Such programs can either have parents provide meals themselves, or pay extra in tuition to cover meal service costs. Therefore, the administrative burden is borne by providers serving children from households with lower income.
3.5.3. Recipient outcomes
3.5.3.1. Providers
It is unclear the extent to which CACFP benefits providers themselves; most studies evaluate the impacts of CACFP on childcare program practices and policies. For example, it is unclear whether CACFP actually helps providers financially so that they have less business challenges or are able to keep program tuition lower. It is also unclear whether CACFP helps with providers' own health and wellness. Notably, despite the fact that childcare teachers are strongly encouraged to sit and eat with children during mealtimes, meals for teachers are not reimbursable through CACFP currently.
3.5.3.2. Children
Similar to what has been found in evaluations of CACFP's impact on childcare program-level food practices and policies, evidence for a beneficial impact of CACFP on child-level outcomes, including diet quality, food security, and healthy weight, are mixed, with studies either finding null or very slightly positive associations (62).
3.5.4. Policy outcomes
Overall, it is unclear whether CACFP has population-level impacts on childcare meal quality or child health.
4. Discussion
Nutrition policies, especially federal nutrition assistance programs, show enormous potential for supporting children's nutrition on a population level. CACFP could be particularly promising given that it focuses on supporting healthy meals for young children, who are at a crucial stage of development. Yet despite its promise, it has not been shown to have strong impacts on child food insecurity, growth, or diet quality (62) While it is often suggested that CACFP participants need more training or technical assistance to support better adoption of CACFP, the analysis above suggests that simply providing training or technical assistance is not enough; rather, we argue that several key misalignments between CACFP's policy implementation process and the current structure of the childcare industry have contributed to weaker impacts. These include:
4.1. Fractured childcare industry and conflict over resources for safety net programs
The daily challenges that childcare providers face in maintaining operations—low wages, high staff turnover, high operating costs, and the need to comply with multiple regulations outside of food-related rules—may make participation in CACFP infeasible for many programs; they just may not have the bandwidth given the current structure of childcare. While increasing operational and financial support given through CACFP could increase its feasibility for programs, as well as providing more support and structure to the childcare industry in general, this would require expansions of the existing social safety net that are controversial in the current political climate.
4.2. Insufficient financial support for providers to effectively implement the program
While existing reimbursements may cover food costs on average, they do not appear to be adequate for covering the cost of the labor needed to complete CACFP's administrative requirements or to plan and prepare meals. They also may not be adequate for supporting a variety of foods that can fit children's preferences or help towards introducing children to new foods, leaving providers with a situation where they are repeating the same few meals and reducing satisfaction with the program. Reimbursements that fairly cover the costs of labor and can support a truly healthful food service—with the provision of a variety of foods that meet CACFP's nutritional standards and children's preferences—are needed.
4.3. Inadequate implementation structure for some programs
An implementation structure more similar to that of the NSLP/SBP—where there are agencies with dedicated staff for overseeing compliance paperwork, planning meals, and preparing and serving meals—could be helpful. For many childcare providers, especially those without a sponsor, participating in CACFP would be akin to asking school principals and teachers to add school meal compliance paperwork and food service to their workloads. Sponsoring agencies help support family childcare providers and some centers in overseeing administrative duties; perhaps a more robust role for these agencies, with support available for more center-based programs and more help with the meal planning and food preparation tasks necessary for participation, could be a solution.
Additionally, increasing communication across levels of implementation (federal, state, sponsor, provider) is needed. The agency involved in setting policy—USDA—is far removed from the day-to-day activities involved in implementation. One implication of this is that some of the policy memorandums that USDA provides to try to support implementation, as well as informational resources designed to help providers comply, may be out of sync with what providers need. For example, one co-author, who is involved in providing food service for CACFP-participating programs, has found that USDA's example recipes often include foods that are too expensive (like nuts or dried fruits) and/or foods that are not creditable for that dish. Communication between state agencies and food vendors could be further developed, rather than relying on childcare centers to navigate those communications. Finally, supporting newly-formed childcare providers in the transition of opening could be a useful investment to ensure the food programs are a support rather than a burden to newly-formed business enterprises.
5. Conclusions
Policymakers and others involved in policy formulation and implementation processes should consider strategies to reshape CACFP's implementation to better fit the existing context of childcare in the U.S.—not only through more robust financial support, but also through perhaps a reconsideration of what administrative paperwork is truly necessary for program participation and a retooling of existing implementation supports, like training, technical assistance, and meal planning, that are available to childcare programs. Meanwhile, as this analysis demonstrates, we suggest that researchers, policymakers, and public health practitioners who want to leverage food policies to promote public health nutrition must go beyond focusing only on requiring the provision of foods and beverages in line with dietary science—we must also carefully consider the context in which these policies operate, and the implementation process that can determine their success.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
EK: Conceptualization, Data curation, Funding acquisition, Investigation, Project administration, Writing – original draft, Writing – review & editing. MP: Conceptualization, Writing – original draft, Writing – review & editing. NF: Conceptualization, Data curation, Investigation, Writing – review & editing. KK: Data curation, Writing – review & editing. RM: Data curation, Formal Analysis, Project administration, Writing – review & editing. TA: Conceptualization, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
This study was supported by a National Institute of Diabetes and Digestive and Kidney Diseases Career Development Award (K01DK125278) and a training grant (5T32HL098048-14) of the National Heart, Lung, and Blood Institute.
Acknowledgments
The authors would like to acknowledge the CACFP-participating childcare providers and sponsors that they have engaged with over the past several years in their research and practice. Without their sharing their experiences and insights with us, we would not have been able to conceptualize this article. We would also like to dedicate this paper to Dianne S. Ward, an irreplaceable mentor to several of us, whose scientific leadership and dedication to improving the health of young children and childcare workers have shaped the field of early childhood nutrition and public health. Without her pioneering work and her commitment to bringing more researchers and practitioners into the field, it is unlikely that much of the work and analysis we present in this paper would have been possible.
Conflict of interest
NF is employed by Seed 2 Roots LLC.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. GBD 2017 Diet Collaborators. Health effects of dietary risks in 195 countries, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet. (2019) 393(10184):1958–72. doi: 10.1016/S0140-6736(19)30041-8
2. Liu J, Rehm CD, Onopa J, Mozaffarian D. Trends in diet quality among youth in the United States, 1999-2016. JAMA. (2020) 323(12):1161–74. doi: 10.1001/jama.2020.0878
3. Rehm CD, Peñalvo JL, Afshin A, Mozaffarian D. Dietary intake among US adults, 1999–2012. JAMA. (2016) 315(23):2542–53. doi: 10.1001/jama.2016.7491
4. Centers for Disease Control and Prevention. About chronic diseases (2023). Available at: https://www.cdc.gov/chronicdisease/about/index.htm (Accessed July 31, 2023).
5. Centers for Disease Control and Prevention. Leading causes of death (2023). Available at: https://www.cdc.gov/nchs/fastats/leading-causes-of-death.htm (Accessed July 31, 2023).
6. Odoms-Young AM. Examining the impact of structural racism on food insecurity: implications for addressing racial/ethnic disparities. Fam Commun Health. (2018) 41:S3–6. doi: 10.1097/FCH.0000000000000183
7. Cooksey Stowers K, Jiang Q, Atoloye AT, Lucan S, Gans K. Racial differences in perceived food swamp and food desert exposure and disparities in self-reported dietary habits. Int J Environ Res Public Health. (2020) 17(19):7143. doi: 10.3390/ijerph17197143
8. Carroll-Scott A, Gilstad-Hayden K, Rosenthal L, Peters SM, McCaslin C, Joyce R, et al. Disentangling neighborhood contextual associations with child body mass index, diet, and physical activity: the role of built, socioeconomic, and social environments. Soc Sci Med. (2013) 95:106–14. doi: 10.1016/j.socscimed.2013.04.003
9. Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A. Household food security in the United States. Econ Res Rep. (2022) 155.
10. Seligman HK, Berkowitz SA. Aligning programs and policies to support food security and public health goals in the United States. Annu Rev Public Health. (2019) 40:319–37. doi: 10.1146/annurev-publhealth-040218-044132
11. Te Vazquez J, Feng SN, Orr CJ, Berkowitz SA. Food insecurity and cardiometabolic conditions: a review of recent research. Curr Nutr Rep. (2021) 10(4):243–54. doi: 10.1007/s13668-021-00364-2
12. Welker EB, Jacquier EF, Catellier DJ, Anater AS, Story MT. Room for improvement remains in food consumption patterns of young children aged 2–4 years. J Nutr. (2018) 148(9S):1536S–46S. doi: 10.1093/jn/nxx053
13. Larson N, Story M. Barriers to equity in nutritional health for US children and adolescents: a review of the literature. Curr Nutr Rep. (2015) 4(1):102–10. doi: 10.1007/s13668-014-0116-0
14. Mozaffarian D, Angell SY, Lang T, Rivera JA. Role of government policy in nutrition—barriers to and opportunities for healthier eating. Br Med J. (2018) 361:k2426. doi: 10.1136/bmj.k2426
15. Bleich SN, Moran AJ, Vercammen KA, Frelier JM, Dunn CG, Zhong A, et al. Strengthening the public health impacts of the supplemental nutrition assistance program through policy. Annu Rev Public Health. (2020) 41:453–80. doi: 10.1146/annurev-publhealth-040119-094143
16. Koleilat M, Whaley SE, Esguerra KB, Sekhobo JP. The role of WIC in obesity prevention. Curr Pediatr Rep. (2017) 5:132–41. doi: 10.1007/s40124-017-0135-6
17. World Health Organization. Assessing the existing evidence base on school food and nutrition policies: a scoping review. (2021).
18. Daepp MIG, Gortmaker SL, Wang YC, Long MW, Kenney EL. WIC Food package changes: trends in childhood obesity prevalence. Pediatrics. (2019) 143(5):e20182841. doi: 10.1542/peds.2018-2841
19. Tester JM, Leung CW, Crawford PB. Revised WIC food package and childrens diet quality. Pediatrics. (2016) 137(5):e20153557. doi: 10.1542/peds.2015-3557
20. Schultz DJ, Byker Shanks C, Houghtaling B. The impact of the 2009 special supplemental nutrition program for women, infants, and children food package revisions on participants: a systematic review. J Acad Nutr Diet. (2015) 115(11):1832–46. doi: 10.1016/j.jand.2015.06.381
21. Kenney EL, Barrett JL, Bleich SN, Ward ZJ, Cradock AL, Gortmaker SL. Impact of the healthy, hunger-free kids act on obesity trends. Health Aff (Millwood). (2020) 39(7):1122–9. doi: 10.1377/hlthaff.2020.00133
22. Mozer L, Johnson DB, Podrabsky M, Rocha A. School lunch entrees before and after implementation of the healthy, hunger-free kids act of 2010. J Acad Nutr Diet. (2019) 119(3):490–9. doi: 10.1016/j.jand.2018.09.009
23. Kinderknecht K, Harris C, Jones-Smith J. Association of the healthy, hunger-free kids act with dietary quality among children in the US national school lunch program. JAMA. (2020) 324(4):359–68. doi: 10.1001/jama.2020.9517
24. Johnson DB, Podrabsky M, Rocha A, Otten JJ. Effect of the healthy hunger-free kids act on the nutritional quality of meals selected by students and school lunch participation rates. JAMA Pediatr. (2016) 170(1):e153918. doi: 10.1001/jamapediatrics.2015.3918
25. Andreyeva T, Mozaffarian RS, Kenney EL. Updated meal patterns in the child and adult care food program and changes in quality of food and beverages served: a natural experimental study. Nutrients. (2022) 14(18):3786. doi: 10.3390/nu14183786
26. Bullock HL, Lavis JN, Wilson MG, Mulvale G, Miatello A. Understanding the implementation of evidence-informed policies and practices from a policy perspective: a critical interpretive synthesis. Implement Sci. (2021) 16:1–24. doi: 10.1186/s13012-021-01082-7
27. United States Department of Agriculture. Child and adult care food program (CACFP) (2018). Available at: https://www.fns.usda.gov/cacfp/child-and-adult-care-food-program
28. Proctor EK, Landsverk J, Aarons G, Chambers D, Glisson C, Mittman B. Implementation research in mental health services: an emerging science with conceptual, methodological, and training challenges. Adm Policy Ment Health. (2009) 36(1):24–34. doi: 10.1007/s10488-008-0197-4
29. Wang L, Steele EM, Du M, Pomeranz JL, O’Connor LE, Herrick KA, et al. Trends in consumption of ultraprocessed foods among US youths aged 2–19 years, 1999–2018. JAMA. (2021) 326(6):519–30. doi: 10.1001/jama.2021.10238
30. Banfield EC, Liu Y, Davis JS, Chang S, Frazier-Wood AC. Poor adherence to US dietary guidelines for children and adolescents in the national health and nutrition examination survey population. J Acad Nutr Diet. (2016) 116(1):21–7. doi: 10.1016/j.jand.2015.08.010
31. Centers for Disease Control and Prevention. Childhood overweight and obesity (2022). Available at: https://www.cdc.gov/obesity/childhood/index.html (Accessed August 1, 2023).
32. World Health Organization. Commission on ending childhood obesity: facts and figures on childhood obesity (2017). Available at: https://www.who.int/end-childhood-obesity/facts/en/ (Accessed August 1, 2023).
33. Must A, Strauss RS. Risks and consequences of childhood and adolescent obesity. Int J Obes Relat Metab Disord. (1999) 23(Suppl 2):S2–11. doi: 10.1038/sj.ijo.0800852
34. Ward ZJ, Long MW, Resch SC, Giles CM, Cradock AL, Gortmaker SL. Simulation of growth trajectories of childhood obesity into adulthood. N Engl J Med. (2017) 377(22):2145–53. doi: 10.1056/NEJMoa1703860
35. May AL, Kim SA, Sherry B, Blanck HM. Childhood obesity task forces established by state legislatures, 2001-2010. Prev Chronic Dis. (2013) 10:E144. doi: 10.5888/pcd10.120153
36. Geserick M, Vogel M, Gausche R, Lipek T, Spielau U, Keller E, et al. Acceleration of BMI in early childhood and risk of sustained obesity. N Engl J Med. (2018) 379(14):1303–12. doi: 10.1056/NEJMoa1803527
37. Pew Research Center. Views of the economic system and social safety net (2019). Available at: https://www.pewresearch.org/politics/2019/12/17/views-of-the-economic-system-and-social-safety-net/#long-term-opinion-trends-views-of-the-social-safety-net-and-nations-economic-system (Accessed August 1, 2023).
38. Murphy SP, Yaktine AL, West Suitor C, Moats S. Child and adult care food program: aligning dietary guidance for all. In: Murphy SP, Yaktine AL, West Suitor C, Moats S, editors. Child and adult care food program: Aligning dietary guidance for all. Washington: National Academies Press (2010). p. xiv+258. doi: 10.17226/12959.
39. Herd P, Moynihan DP. Administrative burden: policymaking by other means. New York, NY: Russell Sage Foundation (2019).
40. Healthy, Hunger-Free Kids Act of 2010, Public Law 296, U.S. Statutes at Large 124 (2010). p. 3183–266.
41. United States Department of Agriculture F and NS. Child and adult care food program: meal pattern revisions related to the healthy, hunger-free kids act of 2010. Washington, DC (2015). Available at: Available from: Available at: https://www.federalregister.gov/articles/2015/01/15/2015-00446/child-and-adult-care-food-program-meal-pattern-revisions-related-to-the-healthy-hunger-free-kids-act
42. U.S. Department of the Treasury. The economics of child care supply in the United States. Washington, DC: U.S. Department of Treasury (2021).
43. Child Care Aware of America. Demanding change: repairing our child care system (2022). Available at: https://info.childcareaware.org/hubfs/2022-03-FallReport-FINAL%20(1).pdf (Accessed August 1, 2023).
44. Yellen J. Remarks by secretary of the treasury Janet L. Yellen on shortages in the child care system (2021). Available at: https://home.treasury.gov/news/press-releases/jy0355 (Accessed August 1, 2023).
45. Lessard LM, Wilkins K, Rose-Malm J, Mazzocchi MC. The health status of the early care and education workforce in the USA: a scoping review of the evidence and current practice. Public Health Rev. (2020) 41(1):2. doi: 10.1186/s40985-019-0117-z
46. Part 226–Child and Adult Care Food Program. Washington, DC: U.S. Congress; 2023. Available at: https://www.ecfr.gov/current/title-7/subtitle-B/chapter-II/subchapter-A/part-226
47. United States Department of Agriculture Food and Nutrition Service. Final rule: for-profit center participation in the CACFP (2006). Available at: https://www.fns.usda.gov/cacfp/fr-102306 (Accessed August 1, 2023).
48. United States Department of Agriculture Food and Nutrition Service. Child and adult care food program: state agency (2021). Available at: https://www.fns.usda.gov/cacfp/state-agency (Accessed August 1, 2023).
49. United States Department of Agriculture Food and Nutrition Service. Child and adult care food program: program operator (2021). Available at: https://www.fns.usda.gov/cacfp/program-operator (Accessed August 1, 2023).
50. Andreyeva T, Moore TE, da Cunha Godoy L, Kenney EL. Federal nutrition assistance for young children: under-utilized and unequally accessed. Am J Prev Med. (2023) 13:S0749-3797(23)00354-9. doi: 10.1016/j.amepre.2023.09.008
51. Chriqui JF, Leider J, Schermbeck RM, Sanghera A, Pugach O. Changes in child and adult care food program (CACFP) practices at participating childcare and education centers in the United States following updated national standards, 2017–2019. Nutrients. (2020) 12(9):2818. doi: 10.3390/nu12092818
52. Dave JM, Cullen KW. Foods served in child care facilities participating in the child and adult care food program: menu match and agreement with the new meal patterns and best practices. J Nutr Educ Behav. (2018) 50(6):582–8. doi: 10.1016/j.jneb.2018.01.010
53. Earnesty D, Mphwanthe G, Rau K, Weatherspoon L. A qualitative study: perceived barriers and facilitators to nutrition standard adherence by in-home childcare providers. J Acad Nutr Diet. (2022) 122(4):786–96.e4. doi: 10.1016/j.jand.2021.08.104
54. Jana B, Loefstedt K, Vu M, Ward D, Erinosho T. “It has a lot to do with the cumbersome paperwork”: barriers and facilitators of center-based early care and education program participation in the child and adult care food program. J Acad Nutr Diet. (2023) 123(8):1173–1186.e1. doi: 10.1016/j.jand.2023.03.014
55. Andreyeva T, Sun X, Cannon M, Kenney EL. The child and adult care food program: barriers to participation and financial implications of underuse. J Nutr Educ Behav. (2022) 54(4):327–34. doi: 10.1016/j.jneb.2021.10.001
56. Lee DL, Gurzo K, Yoshida S, Homel Vitale E, Hecht K, Ritchie LD. Compliance with the new 2017 child and adult care food program standards for infants and children before implementation. Child Obes. (2018) 14(6):393–402. doi: 10.1089/chi.2018.0092
57. Poole MK, Cradock AL, Kenney EL. Implementing the new child and adult care food program’s nutrition standards in Boston. Prev Chronic Dis. (2020) 17:E44. doi: 10.5888/pcd17.190426
58. Poole MK, Cradock AL, Kenney EL. Changes in foods served and meal costs in Boston family child care homes after one year of implementing the new child and adult care food program nutrition standards. Nutrients. (2020) 12(9):2817. doi: 10.3390/nu12092817
59. Logan CW, Connor P, LeClair L, Patlan K, Glenn M, Stidsen C, et al. Study of nutrition and activity in childcare settings. Alexandria, VA (2021). Available at: https://fns-prod.azureedge.us/sites/default/files/resource-files/SNACS-AppendixE.pdf (Accessed August 1, 2023).
60. Monsivais P, Johnson DB. Improving nutrition in home child care: are food costs a barrier? Public Health Nutr. (2011) 15(2):370–6. doi: 10.1017/S1368980011002382
61. Monsivais P, Kirkpatrick S, Johnson DB. More nutritious food is served in child-care homes receiving higher federal food subsidies. J Am Diet Assoc. (2011) 111(5):721–6. doi: 10.1016/j.jada.2011.02.007
62. Kenney EL, Tucker K, Plummer RS, Mita C, Andreyeva T. The child and adult care food program and young children’s health: a systematic review. Nutr Rev. (2023) 81(11):1402–13. doi: 10.1093/nutrit/nuad016.
63. Dutko P, Ver Ploeg M, Farrigan T. Characteristics and influential factors of food deserts (2012). [Report] Economic research report number 140. p. 36. doi: 10.22004/ag.econ.262229
Keywords: policy, implementation science, nutrition assistance, childcare, public health
Citation: Kenney EL, Poole MK, Frost N, Kinderknecht K, Mozaffarian RS and Andreyeva T (2023) How policy implementation shapes the impact of U.S. food assistance policies: the case study of the Child and Adult Care Food Program. Front. Health Serv. 3:1286050. doi: 10.3389/frhs.2023.1286050
Received: 30 August 2023; Accepted: 18 October 2023;
Published: 2 November 2023.
Edited by:
Yanfang Su, University of Washington, United StatesReviewed by:
Heather Brown, Lancaster University, United Kingdom© 2023 Kenney, Poole, Frost, Kinderknecht, Mozaffarian and Andreyeva. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Erica L. Kenney ZWtlbm5leUBoc3BoLmhhcnZhcmQuZWR1
 Erica L. Kenney
Erica L. Kenney Mary Kathryn Poole
Mary Kathryn Poole Natasha Frost2
Natasha Frost2 Kelsey Kinderknecht
Kelsey Kinderknecht