- 1Directorate of Nursing, NHS Forth Valley, Larbert, United Kingdom
- 2School of Medicine, Veterinary and Life Sciences, University of Glasgow, Glasgow, United Kingdom
- 3The Royal Marsden NHS Foundation Trust, London, United Kingdom
- 4Faculty of Social Sciences, University of Stirling, Stirling, United Kingdom
Introduction: In Scotland, prostate cancer services have struggled to meet demand, and urological cancer services have missed Scottish Government waiting time targets to a greater extent than other cancer services. This study provides understanding of the capacity development needs of a national prostate cancer service including why the service had been unable to adapt to meet demand and how capacity could be developed.
Methods: Delphi technique was applied to a purposive sample of prostate cancer clinicians working across Scotland between 2015 and 2017. Interviews were conducted with healthcare professionals involved in delivery of care to people with prostate cancer including General Practitioners, followed by questionnaires which were distributed to Specialist Nurses, Oncologists and Urologists involved in delivering specialist prostate cancer services within NHS Scotland. Findings are reported from interviews analysed using a directed approach to content analysis, followed by three rounds of iterative online questionnaires analysed using descriptive statistics.
Results: Reform is needed to meet demand within prostate cancer services in Scotland. Barriers to capacity development included: lack of shared understanding of quality of care between policy makers and healthcare professionals; lack of leadership of service developments nationally and regionally; and difficulties in drawing on other capacities to support the service. Cohesive working and a need for efficient training for nurse specialists were needed to develop capacity. Consensus was reached for development of national working groups to set standards for quality care (100% agreement) and further development of existing regional working groups (100% agreement) to implement this care (91% agreement), which should include input from primary and community care practitioners (100% agreement) to meet demand.
Discussion: This work provides important understanding of barriers and facilitators to service development across a national service, including highlighting the importance of a shared vision for quality care between policy makers and healthcare professionals. Mechanisms to support service change are identified.
1. Introduction
Health systems report varying levels of success in developing health services to manage demand following the emergence of COVID-19 (1–4). Recovery and remobilisation plans following the pandemic have led to further significant investment in health service development (5, 6), offering an opportunity to improve health systems towards a “new normal” for healthcare delivery rather than reverting systems back to their pre-pandemic forms (7, 8). This paper presents findings from a study that identified barriers and facilitators to development of a national cancer service to support successful development of health services.
In Scotland, incidence of prostate cancer has increased steadily over a number of years (9) and Scottish prostate cancer services have been unable to adapt to meet demand. Most evidently, the quality of cancer care was measured nationally using waiting time targets in Scotland (10, 11), and urological services have missed these waiting time targets to a greater extent than any other cancer care service (12). Further, capacity shortage within Scottish prostate cancer services resulted in delayed adoption of pre-biopsy MRI following updating of NICE guidelines in 2019. Prostate cancer services in Scotland have been identified as lacking capacity to deliver quality prostate cancer care in line with NHS Scotland cancer policy (11, 13). With no literature explaining why prostate cancer services in Scotland had been unable to develop to meet demand, this study was guided by limited availability of literature and existing datasets.
This study gained understanding of the capacity development needs of the NHS Scotland prostate cancer service. Specifically:
1. How is use of the NHS Scotland prostate cancer service predicted to change?
2. Why has the NHS Scotland prostate cancer service been unable to meet demand?
3. How should capacity be developed within the NHS Scotland prostate cancer service to meet demand?
2. Methods
2.1. Study design
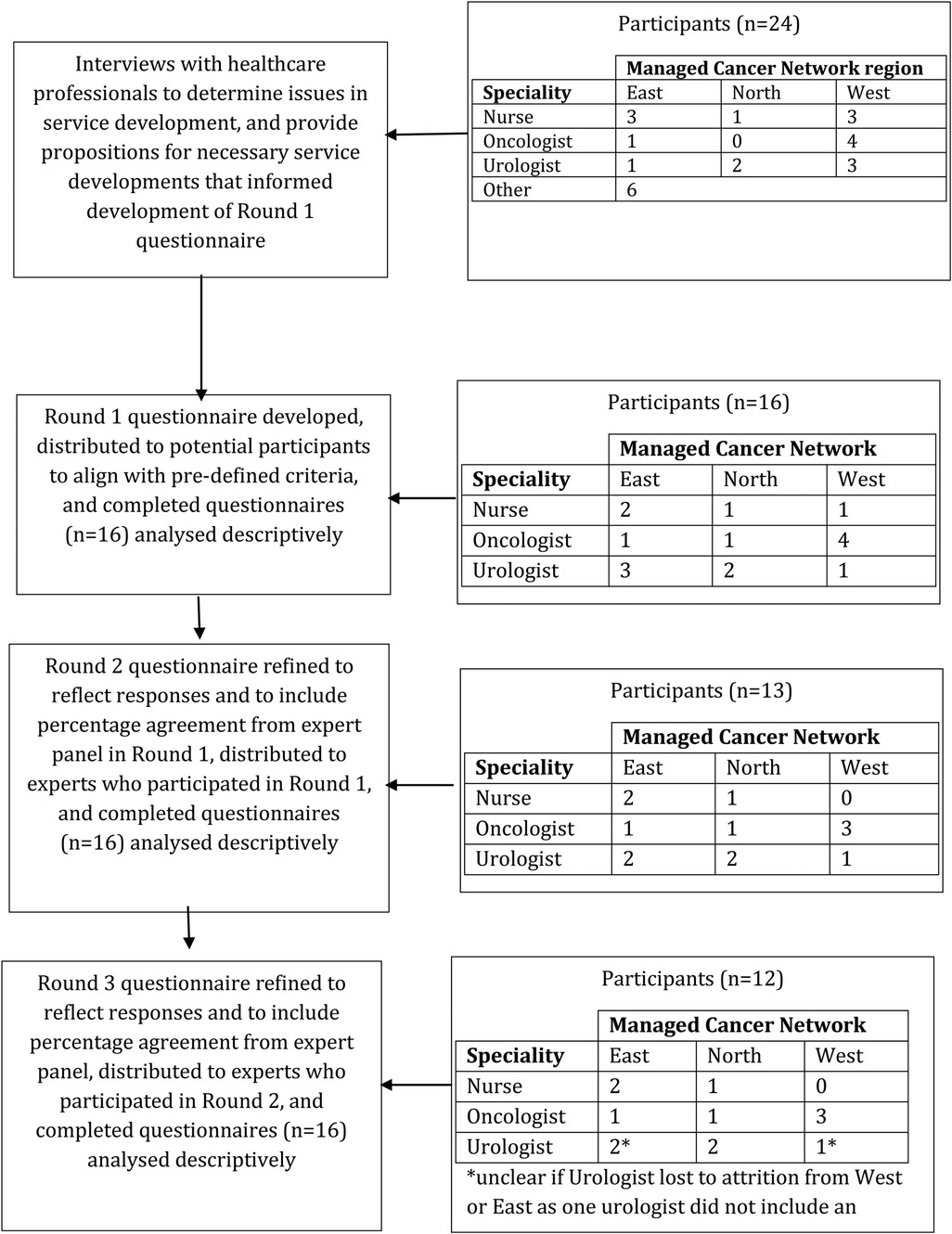
Delphi technique was used to gain understanding of the capacity development needs within the Scottish prostate cancer service from a pragmatic, pluralist perspective. Delphi technique is a commonly used methodology in healthcare research (14) and provided a feasible framework for exploiting existing experience of prostate cancer services in Scotland to facilitate consensus on capacity need. When using Delphi, consensus is generally facilitated across two key steps. Firstly, a range of methods are used to generate ideas or determine issues related to the research problem. Then, findings are used to inform development of closed-question questionnaires that are distributed, analysed, revised and re-distributed iteratively until consensus is reached, attrition occurs, or over a pre-determined number of questionnaire “Rounds”. In this study, interviews with healthcare professionals were followed by an iterative questionnaire process with urologists, oncologists and nurses across a multiphase study. A flowchart of this study design is provided in Figure 1.
2.2. Setting
Within Scotland, the Scottish Government Directorate for Health and Social Care implement healthcare policy to direct healthcare development and are responsible for the administration of the NHS (15). Regional responsibility of healthcare is then devolved to 14 Health Boards who deliver care in collaboration with 32 local authority areas across Scotland. The delivery of disease-specific, specialised care is coordinated by three Managed Cancer Networks (MCN) in the East, North and West of Scotland, who are directly answerable to Health Boards (16). Each Health Board must meet local need (17) and so, service design and priorities differ across regions (18). As a result, some roles or services exist in one Health Board that do not exist in another, and there is a general lack of clarity on how each service was composed including the disciplines and roles present.
2.3. Interview participant sampling and recruitment
All healthcare professionals with an interest in prostate cancer serviceswithin NHS Scotland were invited to participate across all Managed Clinical Network (MCN) regions to ensure that the experience captured was reflective of the needs of the service across Scotland. Participants were invited to interview via email using an extensive list of healthcare professional contact details which had been collated from the research funder, professional networks, national conferences and networking events. Snowball sampling was also used. Recruitment continued until a diverse population has been interviewed and no new information was apparent (19).
2.4. Interview data collection
A structured interview schedule was developed to elicit a comprehensive understanding of service need. Scottish prostate cancer service use trends (20) were summarised to interviewees who were then asked four questions: (i) how do you explain this change in usage, (ii) how do you expect this to change in the future, (iii) what impact will this have on service delivery and organization, and (iv) how can services better plan to accommodate this change? Then, to ensure all service developments were accounted for, participants were asked to predict the main service development issues in the coming 10 years, and the impact of developments that were currently being implemented, such as the implementation of robotic prostatectomy technologies. Where participants had limited understanding of all parts of the service, participants were asked to describe their role within the Service and were asked only questions from the interview schedule relevant to their role.
2.5. Content analysis
A directed approach to content analysis was used to enable the understanding, construction, and development of the participant's perspective only (Bengtsson, 2016). Analysis was structured around a framework (21) developed from the known structure and usage of the service (Ward, 2020). Content analysis has proven useful in guiding analysis and reporting of findings from similar types of exploratory research (22), and is an “unobtrusive” method of data analysis (23).
All interviews were transcribed verbatim excluding non-speech and intonation sounds such as laughter, emphasis and pauses. Data were coded to the framework using NVivo (24), which allowed the coding process to stay rooted in the service and minimised opportunity for meaning or context being inferred from other sources. The framework was then developed to fit all relevant data. Relevant data were then condensed to meaning units by describing each datum in fewer words, but without losing its meaning (25). Mind mapping tool, GoConqur, was then used to map meaning units around codes. Mind mapping has been shown to be reflective of thought processes in qualitative analysis, which are usually non-linear and random (26) so data visualisation helped with categorisation. Further, as the first step in development of themes involves grouping similar meaning units (27), the data visualisation resulting from the initial mapping exercise proved useful in identifying similarities in meaning units between codes. The meaning units that emerged from the data around each service or code, provided understanding of the capacity development issues of that service, which were then compared to support understanding of the service.
2.6. Questionnaire participant sampling and recruitment
Healthcare professionals were recruited across all MCN regions. Given the focus of questionnaires on service design, recruitment during this phase was limited to specialist nurses, oncologists, and urologists only, to ensure that participants had the relevant expertise needed to complete questionnaires. Participants were invited to interview via email and were encouraged to forward the invite to participate to relevant colleagues.
2.7. Questionnaire development
Analysis of interview data was used to construct the initial questionnaire. An a priori decision was made to collect data using three iterative questionnaire rounds to prevent participant fatigue (28). An online survey platform was used to distribute the questionniare.
The Round 1 (R1) questionnaire was structured around three topics: the organisation of secondary and tertiary care, multidisciplinary working, and patient follow-up to include all service developments proposed by healthcare professionals at interview for diagnosis or treatment services; propositions given in the interview data were reduced to its simplest form before inclusion, for example, “diagnostic services should be a one stop shop” and “orchidectomy should be discussed as a treatment option with patients”.
Following R1, Round 2 (R2) and Round 3 (R3) questionnaires were restructured to reflect service design and the emerging consensus, and group feedback was provided to individuals within the questionnaires. R2 topics were the multidisciplinary team, diagnostics and active surveillance, radical treatment, and palliative oncology and included all propositions that had not reached consensus and any new propositions proposed by participants in R1. Participants were asked in comment boxes why they agreed or disagreed with each proposition to gain understanding of potential barriers to service development.
R3 topics were service delivery, the diagnostic pathway, active treatments, and palliative treatments. As little guidance is provided on the purpose of, or how to develop an R3 questionnaire (29, 30), the R3 questionnaire was used to ensure that (i) all topics of consensus were compatible, and (ii) to re-evaluate topics of dissensus considering the emerging consensus. To do this, statements that had reached consensus in either R1 or R2 were grouped and presented as a single proposition. For example, the following statement grouped 9 propositions that had reached consensus in R1 or R2, and asked participants whether they agreed or disagreed:
“The management of side effects requires a dedicated team that is nurse- led. This team should be responsible for the treatment and management of erectile dysfunction, incontinence, bladder irritability and bowel issues across both surgical and radiotherapy services as required. This team should also be involved with patients both pre and post treatment and should be organised around tertiary and sub-specialist services.”
In addition to shortening the length of the questionnaire, this afforded healthcare professionals the opportunity to consider the emerging consensus as a service and not as a series of isolated propositions. Relevant statements that had not reached consensus in R1 or R2 were then listed to allow participants to consider these alongside the proposed service.
During development of the R3 questionnaire it became apparent that no mechanism was being identified that could support the service to develop. Interview data, questionnaire comments and the emerging consensus were reviewed and a section was added to the end of the R3 questionnaire titled “further consideration” to propose mechanisms of capacity development within the service.
A variety of question styles were used to suit each question asked: participants were provided with multiple propositions and asked to select the proposition that they most agreed with; participants were asked to select all relevant propositions; five-point Likert scales (R1 only); and open-ended questions were used in the final section of the questionnaire. Each question also included the option to select “not relevant to my expertise” and comment boxes were included after each question to collect open feedback, disagree with questions asked and suggest new propositions.
2.8. Piloting questionnaires
To ensure clarity in questions asked without introducing bias or impacting on recruitment to the study, the R1 questionnaire was piloted, which resulted in two changes in addition to minor rephrasing of statements.
2.9. Questionnaire data analysis
Consensus was quantified as ≥80% agreement and dissensus was quantified as <80% agreement. Using these thresholds, data were categorised as “statement accepted” (80%–100% agreement), “dissensus” (21%–79% agreement), and “statement rejected” (0%–20% agreement).
3. Results
3.1. Participants
As the service was composed of a diverse range of healthcare professionals, gaining an understanding of the full complement of healthcare professionals working within the service was challenging. Participants at interview identified very small numbers of healthcare professionals specialising in prostate cancer care outside of nursing and medicine, and so care was taken in reporting of results to ensure participant anonymity.
24 healthcare professionals were interviewed from across Scotland (Figure 1). 21 were interviewed in person, two via telephone and one participant provided written responses.
In questionnaire rounds, 16 healthcare professionals participated from across Scotland (Figure 1). Of these participants, 10 had participated in the interview phase of this study.
3.2. Findings from interviews
3.2.1. Service reform
Healthcare professionals identified substantial capacity shortage across the entire service and raised concerns that finite resources had not increased at the same rate as incidence or treatment usage. Participants had “redesigned as much as [they] probably [could], and we’re struggling” (Participant 1) meaning that “radical changes that are needed to say, new models of working… making small changes is important… but at a fundamental level for us to deal with capacity we need to look at bigger changes” (Participant 9). Any predicted decline in treatment usage was predicted to be the result of changing patterns of presentation, the implementation of technological advances, or the integration of new technologies, and not due to a decrease in the number of patients requiring treatment. However, these changes were unlikely to be imminent, and so all healthcare professionals were anticipating increased demand.
3.2.2. Shared vision
Though healthcare professionals and government were striving for a quality service, a shared vision for quality care was lacking. For example, healthcare professionals described government measures of quality such as waiting time targets as “stifling” (Participant 22) service development, were understood to be without scientific rationale, diverted focus from the development of quality services, and “compromise[d] innovation and change in practice” (Participant 17). With limited evidence to inform service development, healthcare professional's understanding of quality care was found to be a primary driver in service development, and services were developed only where healthcare professionals believed that the quality of the service could be maintained or improved rather than to meet government objectives as “you don’t want to arrange [treatment] too early in the pathway to feed, to, to meet a necessity rather than what is correct” (Participant 1). Healthcare professionals believed that their approach to quality care was now being “validated” (Participant 16) by recent evidence.
3.2.3. Leadership
At interview, a lack of leadership or oversight of service developments resulted in wasted capacity as “everybod[y] reinvent[ed] that wheel” (Participant 5). Service developments were generally designed and implemented within each Health Board, putting significant pressure on local services to resolve capacity shortage issues without the support of the wider service to know “what works, what doesn’t work” (Participant 5). In part, this local approach was perpetuated within the structure of healthcare within Scotland, for example:
“Why do we have 14 different area drug and therapeutic committees that decide what should and should not be prescribed in a way that leads to post, post book prescribing. In Scotland 5 and a half million people should be one overarching strategic approach to healthcare that is broadly standardised across Scotland.” Participant 16
Healthcare professionals were unified in wanting more oversight of service developments, and a unified approach to service development. MCNs were identified as best placed to “shape and design” (Participant 16) service developments, but were described as underdeveloped, often guided by the larger Health Boards within the region and with little power to make a difference as they were “just a titch of a role that has no teeth… it's just token shop I think” (Participant 17). Further, each MCN was in a different stage of development, with the most advanced, considered “integrated” (Participant 4) and the least advanced considered “broken” (Participant 4), further complicating possibility of oversight of service development.
3.2.4. Cohesion
When service development issues were described, specialities were described as working in isolation and often competing for resource, resulting in “petty politics” (Participant 22) and hindered the ability of service to plan ahead and develop, as specialisms put the needs of their part of the service before the needs of the service as a whole:
“If we could get people talking together, staff, on the way forward, it would be great. And it has been tried, but it never works, sadly because they all want the best for their patients, whether that's surgery or oncology, so they’re always fighting. Sad. Sad but true.” Participant 14
And healthcare professionals, including some within the speciality, raised concerns over one speciality being dominant within the service and the subsequent risk of “bias” (Participant 24) in patient care. Many healthcare professionals identified that “more together working” (Participant 5), and more “cohesive working to plan ahead” (Participants 14) was needed.
3.2.5. Recruitment and training
More nurse specialists and further development of the nurse specialist and allied healthcare professional roles was found to be integral to capacity development within the service. However, recruitment and training were significant concerns for service development as “how do you broadly train someone for a specialist role?” (Participant 12). Currently, training of nurse specialists required significant investment of service capacities over years. Further, concerns were raised because of changes in undergraduate curricula in some disciplines and healthcare professionals identified specialist vacancies elsewhere in the UK that recruiters had been unable to fill.
3.2.6. Lack of other capacities to use
Healthcare professionals were being encouraged by Scottish Government to use capacities of other services and were also looking to identify available capacities beyond NHS services that could be used. Policy drivers encouraged use of primary care services to alleviate capacity within the service. However, healthcare professionals raised concerns over General Practitioners (GP) capabilities to fulfil their current roles, namely PSA screening and general patient support during and following specialist treatment, and it was unlikely that this would change. Reasons given for this included short appointment times, “their current numbers and as well as that, to educate them. A GP might have 2 patients with prostate cancer in his books or whatever, you can’t expect them to be an expert on that” (Participant 5), pressures to adopt roles from other specialities, “non-clinical issues really, the paperwork, chasing the points and all this sort of stuff” (Participant 8). Healthcare professionals interviewed were divided over whether follow-up with primary care specialists was appropriate as “it's just as expensive to have a GP seeing a patient as it is to have [a medical consultant] seeing a patient, where it's, if you can have in the hospital, you’ll have speciality doctors, you can have nurse practitioners where that is their clinical expertise” (Participant 4); whilst some healthcare professionals believed that follow-up in community supported “normal life” (Participant 5), other healthcare professionals believed that “they’ve had specialist treatment and they should have specialist follow-up… its quite a specialist follow-up regime” (Participant 10). Further, healthcare professionals recognised that patients had capacities that could be used to meet demand and were “expecting more from our patients” (Participant 14). However, healthcare professionals were also concerned that not all patients would manage greater responsibility in their care and were hesitant to adopt individualised follow-up protocols.
3.3. Findings from the consensus questionnaires
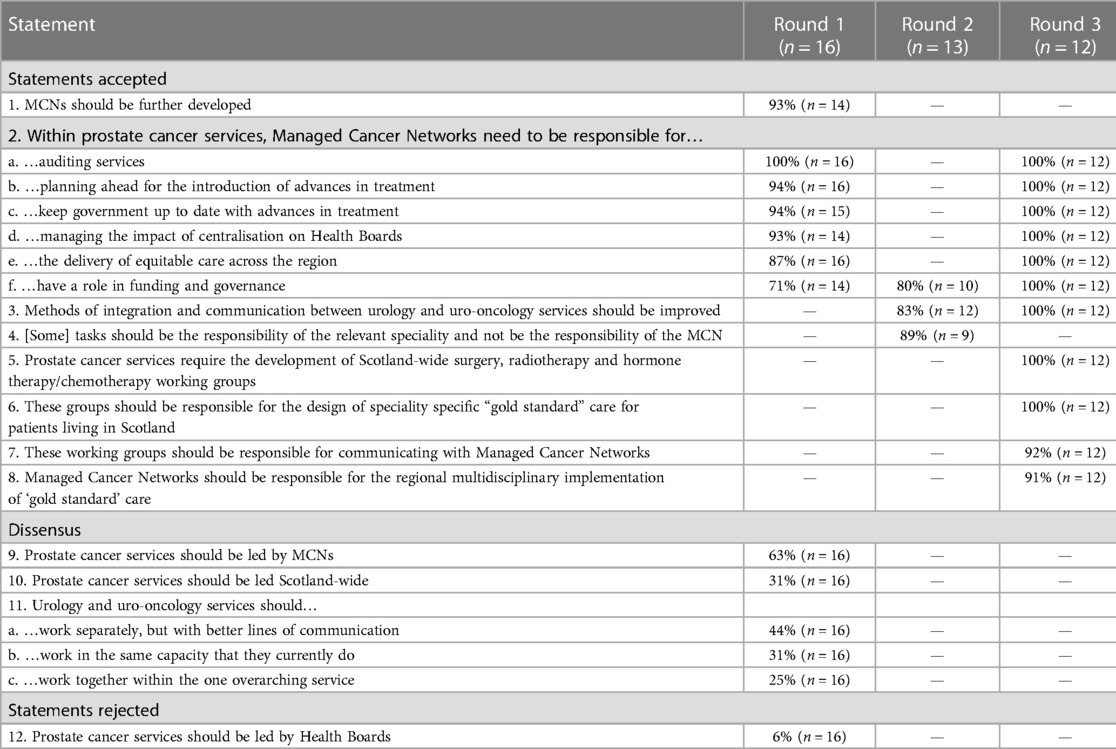
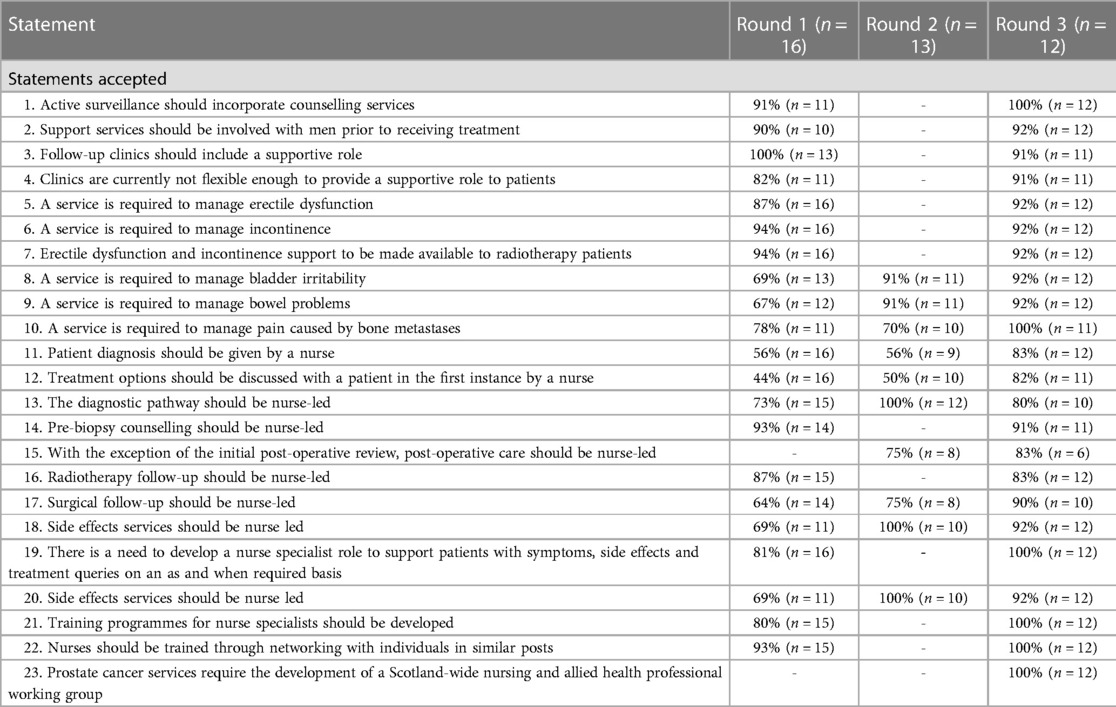
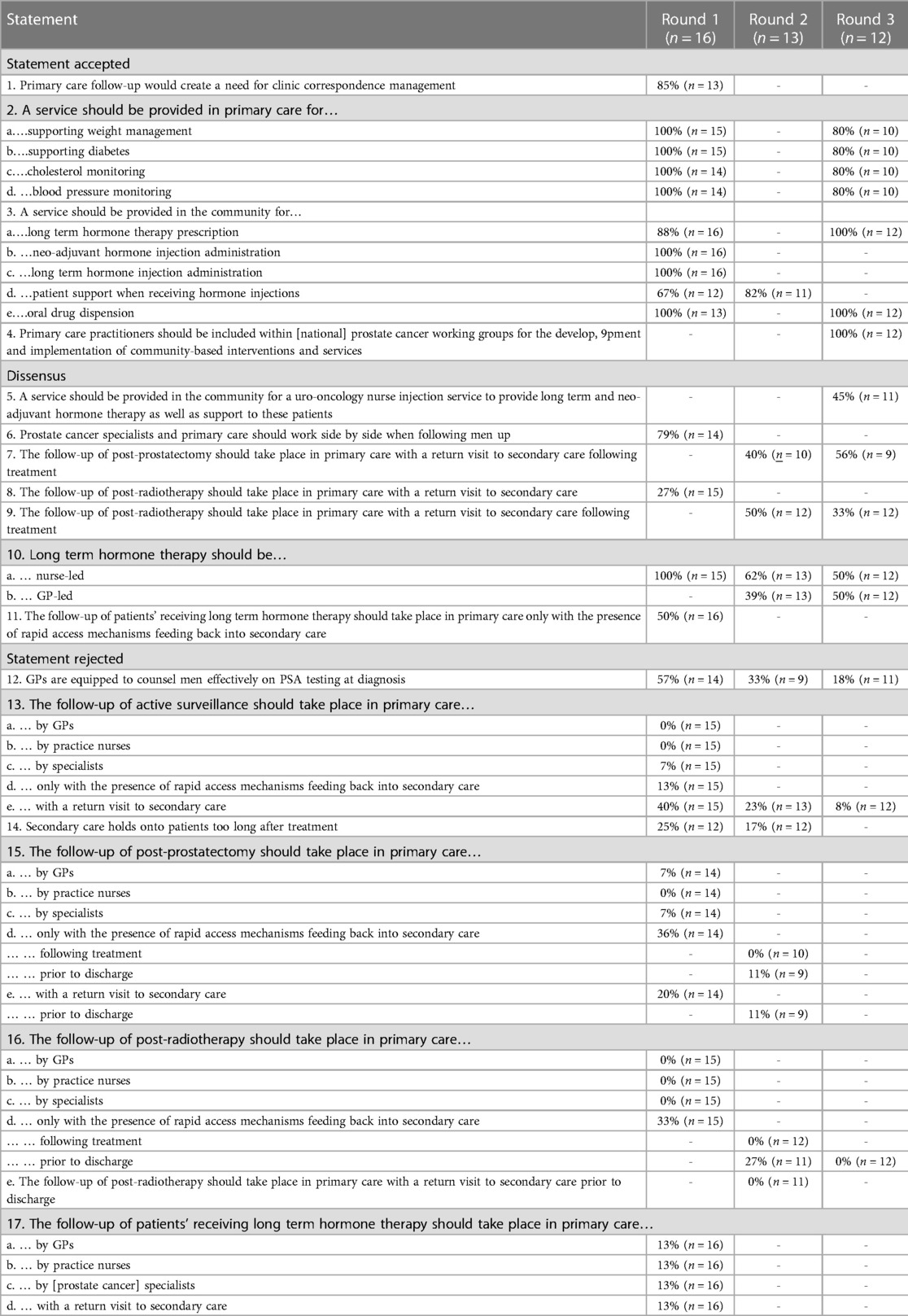
Data are presented in Tables 1–4. In each table, statements accepted are presented first, followed by statements where dissensus remained and finally, statements that were rejected. Percentage agreement with the statement is also provided for each Round. The number of participants who responded to each statement excluding the number of participants who selected “not relevant to my experience” is given as “n”.
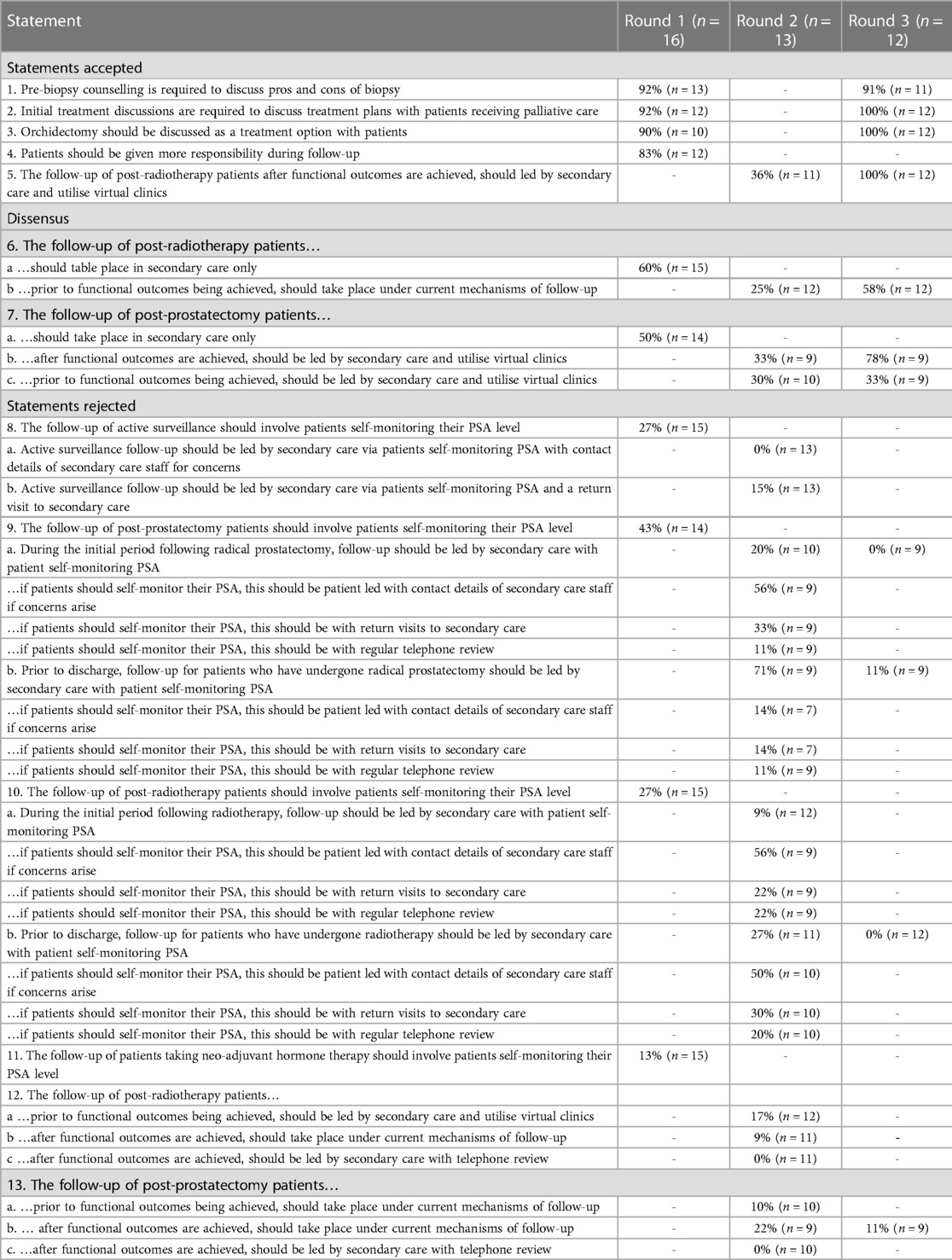
Table 4. Consensus on other capacities (patient choice and responsibilities) to support service development.
3.3.1. Leadership and cohesion
Healthcare professionals rejected the current model of Health Board-led care (Table 3, Statement 12) in place of a centralised leadership structure (Table 1, Statement 9–10) and consensus was reached for the further development of MCNs (Table 1, Statements 1–2). However, healthcare professionals were divided over the need for specialisms to work together (Table 1, Statement 11) though consensus was reached for improved methods of integration and communication between specialities (Table 1, Statement 3). In R3, healthcare professionals were asked to consider mechanisms for service development and consensus was reached for all of these: national, speciality-specific working groups are needed to design quality care and communicate this with MCNs, with MCNs responsible for the regional, multidisciplinary implementation of quality care (Table 1, Statements 4–8).
3.3.2. Recruitment and training
Healthcare professionals reached consensus for the further development of specialist nurse roles across the Service, including the development of multiple nurse-led services (Table 2, Statements 1–19). Training of specialist nurses and allied health professionals should be multi-faceted; nurses should be trained through engaging with a training programme, networking with individuals in similar posts, and supported through the development of a national nursing and allied health professional working group (Table 2, Statements 20–22).
3.3.3. Other capacities
Healthcare professionals reached consensus that primary care practitioners did not have the capabilities to counsel men in relation to most aspects of prostate cancer care including PSA testing at diagnosis and treatment follow-up (Table 3, Statements 6–17), and moving services to primary care would create increased workload in secondary care through correspondence management (Table 3, Statement 1). Support for developing the role of primary care was most evident in the delivery of palliative care pathways and for tertiary health promotion purposes (Table 3, Statements 2–3, 5), though healthcare professionals were divided over who should then be ultimately responsible for the management of this patient population (Table 3, Statements 10). In R3, healthcare professionals reached consensus that primary care practitioners should be included within national prostate cancer working groups providing opportunities to explore capacity development needs jointly going forward (Table 3, Statement 4).
Further, whilst healthcare professionals were keen to improve opportunity for patients to have increased autonomy and responsibility in their own care (Table 4, Statements 1–4), healthcare professionals rejected that patients should have a role in monitoring their own Prostate Specific Antigen (PSA) levels even with regular specialist support (Table 4, Statements 5–13). Rather, consensus was reached for follow-up to remain in secondary care (Table 4, Statements 5–13) possibly with use of virtual clinics (Table 4, Statement 5).
4. Discussion
4.1. Wider context
This study drew on expertise from within a national cancer service that had been unable to develop to meet demand. Interviews found that reform was needed within prostate cancer services in Scotland as services had been “redesigned as much as [they] probably [could], and we’re struggling” (Participant 1), and identified tensions between healthcare professionals and policy makers rooted in different understandings of quality care. Further, a lack of leadership of service developments nationally and regionally; cohesive working; recruitment and training of nurse specialists; and other capacities to meet demand, were identified as barriers to service development. Healthcare professionals identified a need for national, multidisciplinary working groups to develop capacity and meet demand.
Results from this study shed light on important barriers and facilitators in health service development. Whilst it is common for tensions to exist between policy-makers and those delivering health services (30–33), this study adds to the growing body of evidence that top-down approaches to the development of strategic visions for healthcare hinder service development. Collaboration between policy makers and healthcare professionals promise visions ready for application to health service development contexts (34). Braithwaite (35) describes change in health services as moving “to its own rhythm” (pp. 1) and advocates that services need to be empowered to realise change.
The use of working groups or networks have been an important mechanism in facilitating service development throughout the COVID-19 pandemic (4, 36, 37). As such, findings are consistent with other studies which found that leadership of service development nationally do not require traditional healthcare leadership styles and structures (38, 39). Rather, leadership of national service developments should be systemic, service-wide processes based on shared values (40, 41), where a group works to coordinate development towards a new vision (41). Working groups have been found to lead to greater degree of structural and psychological empowerment within the services through encouraging innovation in development (42–45). Importantly, findings recognised the need for different “levels” of working groups with clear terms of reference: higher level groups to set the standard for quality care, and regional groups to implement this standard within the local context.
Further, whilst there are many ways of fostering collaboration to support service development, such as through team building, organisational strengthening and relationship building, cohesion was the model described by participants. Cohesion refers to the strength of relationships and solidarity within a community (46, 47) or the unitedness of a group in obtaining its goal or purpose (48, 49) and includes factors such as interpersonal trust, norms of reciprocity and mutual aid (46, 50–53). Studies have found that high cohesion relates to the absence of latent conflict from longstanding difference that can result from inequities (46) or functional diversity (49), and functional diversity has been found to have a curvilinear relationship with cohesion, where little diversity and high diversity can strengthen cohesion (50–55). In health service development, cohesion has been found to support investment in group activities (53–55) and working towards a shared vision (54, 55).
Consensus reached reflects wider literature (56–65) that identifies support for shift of prostate cancer care services to primary care only where healthcare professionals working in primary care are perceived to have the capacities to best meet patient need when compared with secondary care, though wider literature relating to care for patients who are palliative relates to end of life care only (59–65). With healthcare professionals struggling to realise the widespread shift given current capacities in primary care, and the imperative to deliver specialist care locally has had a substantial impact on the wellbeing of healthcare professionals working in primary care and has led to widespread recruitment concerns (66, 67). Whilst shifting care to primary care is a key policy objective of Scottish health and social care policy (11, 13, 68–70), findings highlight a need for reconsideration of widespread integration of healthcare services considering the new health and social care landscape and echo the Christie commission's (71) emphasis on the development of function-led over form-led care as well as Weir's (72) caution that shifting care to primary care was not a solution for all service delivery issues.
Whilst there is a plethora of literature advocating for participation of patients in their own care including the Patient Rights (Scotland) Act (73), Scottish health policy, the Christie Commission report (72), and evidence showing improvements in measures of care quality including survival (74–76), healthcare professionals were hesitant to use patient capacities to meet demand. The right of a patient to participate as fully as possible in their own care has been identified as a pertinent area of reform in Scottish healthcare in the last 10 years (77, 78). However, practical guidance supporting healthcare professionals to ethically translate this into practice is limited. Recent recommendations for change in Scottish cancer policy identified a need for clearer guidance on use of patient capabilities within cancer services to inform service development (79).
4.2. Strengths and limitations
Healthcare professional expertise is an asset in health service development (80, 81). This study exploited existing expertise of service need across a multi-disciplinary sample of healthcare professionals working across Scotland to reach consensus on how a national cancer service should be developed to meet demand. Apart from two GPs who participated in interviews, all healthcare professionals were prostate cancer specialists and so expertise was limited by lack of exposure to good practice in service development in other specialities. While it is not possible to know the total potential sample size for this study, this study represents a small, but diverse population of relevant healthcare professionals.
4.3. Implications
Findings from this study highlight a need for policy makers to work cohesively with healthcare professionals. Wider literature shows that where healthcare professionals are not supported by policy makers, potential for service development is likely to be limited (80–83). Findings also provide policy makers and healthcare professionals with consensus on the need for national, multidisciplinary working groups, which will facilitate capacity development across services. Further, the development of working groups provide opportunity for coproduction of services with varied stakeholder involvement (82, 83), and it has been found cohesive working within groups supports development and implementation of shared visions for health services (54, 55) and so have potential to support services to overcome further barriers to development.
5. Conclusions
As health systems recover and remobilise towards a “new normal” in health service delivery, understanding of barriers and facilitators to service development within already under pressure services is important. This work highlights how lack of shared vision between policy makers and healthcare professionals can hinder service development and identifies key mechanisms to support service change.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical review and approval was obtained from School of Health Sciences Ethical Committee, University of Stirling, Scotland, UK. Written informed consent was obtained from the participants for their participation in this study.
Author contributions
All authors: made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work drafting the work or revising it critically for important intellectual content provide approval for publication of the content agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors contributed to the article and approved the submitted version.
Funding
This research was jointly funded by Prostate Scotland and University of Stirling.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Vindrola-Pardos C, Johnson GA. Caring on the frontline during COVID-19: Contributions from rapid qualitative research. Singapore: Palgrave Macmillan (2022).
2. Assefa N, Hassen JY, Admassu D, Brhane M, Deressa M, Marami D, et al. COVID-19 testing experience in a resource-limited setting: the use of existing facilities in public health emergency management. Front Public Health. (2021) 9:675553. doi: 10.3389/fpubh.2021.675553
3. Chua A, Al Knawy B, Grant B, Legido-Quigley H, Lee W, Leung GM, et al. How the lessons of previous epidemics helped successful countries to fight COVID-19. Br Med J. (2021) 11(372):n486. doi: 10.1136/bmj.n486
4. Taylor L. Work health organisation to begin negotiating international pandemic treaty. Br Med J. (2021) 2(375):n2991. doi: 10.1136/bmj.n2991
5. Kurowski C, Evans DB, Tandon A, Eozenou PH, Schmidt M, Irwin A, et al. From double shock to double recovery—implications and options for health financing in the time of COVID-19. Washington DC: World Bank Group (2021). Available at: http://hdl.handle.net/10986/35298
6. Wang C, Wang D, Abbas J, Duan K, Mubeen R. Global financial crisis, smart lockdown strategies, and the COVID-19 spillover impacts: a global perspective implications from Southeast Asia. Front Psychiatry. (2021) 12:643783. doi: 10.3389/fpsyt.2021.643783
7. Taylor P, McCarthy M. Building a better world: the crisis and opportunity of COVID-19. Inst Dev Stud Bulletin. (2021) 52(1):1–186.
8. Filho WL, Brandli LL, Salvia AL, Rayman-Bacchus L, Platje J. COVID-19 and the UN sustainable development goals: threat to solidarity or an opportunity? Sustainability. (2020) 12(13):5343. doi: 10.3390/su12135343
10. Scottish government. Our national health: A plan for action, a plan for change. Scottish Government (2000).
14. Humphrey-Murto S, Varpio L, Wood TJ, Gonsalves C, Ufholz LA, Mascioli K, et al. The use of the delphi and other consensus group methods in medical education research: a review. Acad Med. (2017) 92:1491–8. doi: 10.1097/ACM.0000000000001812
15. Scottish Executive Health Department Letter. NHS Scotland health boards and special health boards—blueprint for good governance. Scottish Government (2019).
16. Guthrie B, Davies H, Greig G, Rushmer R, Walter I, Duguid A, et al. Delivering health care through managed clinical networks (MCNs): Lessons from the North. Report for the National Institute for Health Research Service Delivery and Organisation programme (2010).
18. Godden N. Rural health care in the U.K.: a rapidly changing scene. J Agric Saf Health. (2005) 11:205–10. doi: 10.13031/2013.18187
19. Saunders B, Sim J, Kingstone T, Baker S, Waterfield J, Bartlam B. Saturation in qualitative research: exploring its conceptualisation and operationalisation. Qual Quant. (2018) 52:1893–907. doi: 10.1007/s11135-017-0574-8
20. Ward A. Understanding capacity development needs within the NHS Scotland prostate cancer service: a delphi study. UK: University of Stirling (2020).
21. Hseih HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. (2005) 15:1277–88. doi: 10.1177/1049732305276687
22. Green J, Thorogood N. Analysing qualitative data. In: Silverman D, editors. Qualitative methods for health research (1st eds). London: Sage Publications (2004). p. 173–200.
23. Vaismoradi M, Turunen H, Bondas T. Content analysis and thematic analysis: implications for conducting a qualitative descriptive study. Nurs Health Sci. (2013) 15(3):398–405. doi: 10.1111/nhs.12048
25. Bengtsson M. How to plan and perform a qualitative study using content analysis. NursingPlus Open. (2016) 2:8–14. doi: 10.1016/j.npls.2016.01.001
26. Meier PS. Mind-mapping: a tool for eliciting and representing knowledge held by diverse informants. Soc Res Update. (2007) 52:1–4.
27. Erlingsson CL, Brysiewicz PA. Hands-on guide to doing content analysis. Afr J Emerg Med. (2014) 7(3):93–9. doi: 10.1016/j.afjem.2017.08.001
28. McMillan S, King M, Tully MP. How to use the nominal group and Delphi techniques. Int J Clin Pharm. (2016) 8(3):655–62. doi: 10.1007/s11096-016-0257-x
29. Linstone HA, Turoff M. The Delphi method. Techniques and applications. Reading: Addison-Wesley (1975).
30. Green A, Bennett S. Sound choices: enhancing capacity for evidence-informed health policy. Geneva, Switzerland: World Health Organisation (2007).
31. Meriade L, Rochette C. Governance tensions in the healthcare sector: a contrasting case study in France. BMC Health Serv Res. (2022) 22(1):39. doi: 10.1186/s12913-021-07401-4
32. Beland D, Marchildon GP, Medrano A, Rocco P. COVID-19, federalism, and health care financing in Canada, the United States, and Mexico. J Comp Policy Anal. (2021) 2:143–56. doi: 10.1080/13876988.2020.1848353
33. Perna R. Street-level workers, managers and institutional tensions: a comparative ethnography of healthcare practices of in/exclusion in three Italian public organisations. Comp M Stud. (2021) 9(16). doi: 10.1186/s40878-021-00224-6
34. Ryecroft-Malone J, Burton CR, Bucknall T, Graham ID, Hutchison AM, Stacey D. Collaboration and co-production of knowledge in healthcare: opportunities and challenges. Int J Health Policy. (2016) 5(4):221–3. doi: 10.15171/ijhpm.2016.08
35. Braithwaite J. Changing how we think about healthcare improvement. Br Med J. (2018) 361:k2014. doi: 10.1136/bmj.k2014
36. Esposito S, Marchetti F, Lanari M, Caramelli F, De Fanti A, Vergine G, et al. COVID-19 management in the pediatric age: consensus deocument of the COVID-19 working group in pediatrics of the Emilia-romagna region (RE-CO-PED), Italy. Int J Environ Res Public Health. (2021) 18(8):3919. doi: 10.3390/ijerph18083919
37. Jamrozik E, Littler K, Bull S, Emerson C, Kang G, Kapulu M, et al. Key criteria for the ethical acceptability of COVID-19 human challenge studies: report of WHO working group. Vaccine. (2021) 39(4):633–40. doi: 10.1016/j.vaccine.2020.10.075
38. Fruend M. Shared leadership: research and implications for non-profit leadership, capacity building, and education. J Nonprofit Educ Leadersh. (2017) 7(1):13–23. doi: 10.18666/JNEL-2017-V7-11-8022
39. Brewer ML, Flavell H, Trede F, Smith M. Creating change agents for interprofessional education and practice: a leadership programme for academic staff and health practitioners. Int J Leadersh Educ. (2018) 5:580–92. doi: 10.1080/13603124.2017.1279349
40. Denhardt RB, Denhart JV. Leadership for change: case studies in American local government. In: Abramson MA, Bacon K, editors. Leaders. Lanham, MD: Rowman & Littlefield (2002). p. 143–72.
41. Berwick D, Ham C, Smith R. Would the NHS benefit from a single, identifiable leader? An email conversation. Br Med J. (2003) 327(7429):1421–4. doi: 10.1136/bmj.327.7429.1421
42. Laschinger HKS, Finegan J, Shamian J, Wilk P. A longitudinal analysis of the impact of workplace empowerment on work satisfaction. J Organ Behaviour. (2004) 25:527–45. doi: 10.1002/job.256
43. Knol J, Van Linge R. Innovative behaviour: the effect of structural and psychological empowerment on nurses. J Adv Nurs. (2009) 65(2):359–70. doi: 10.1111/j.1365-2648.2008.04876.x
44. Bonias D, Bartram T, Leggat SG, Stanton P. Does psychological empowerment mediate the relationship between high performance work systems and patient care quality in hospitals? Asia Pac J Hum Res. (2010) 48:319–37. doi: 10.1177/1038411110381667
45. Solansky S. Education and experience impact leadership development psychological empowerment. Leadersh Organ Dev J. (2014) 35:637–48. doi: 10.1108/LODJ-07-2012-0091
46. Kawachi I, Berkman L. Social cohesion, social capital, and health. In: Berkman LF, Kawachi I, editors. Social epidemiology. Oxford, United Kingdom: Oxford University Press (2000).
47. Office of Disease Prevention and Health Promotion. Social cohesion. Office of Disease Prevention and Health Promotion (2010). p. 290–319.
48. Carron AV, Brawley LR, Widmeyer WN. The measurement of cohesiveness in sport groups. In: Duda JL, editors. Advances in sport and exercise psychology measurement. Morgantown, WV: Fitness Information Technology (1998).
49. Tekleab AG, Karaca A, Quigley NR, Tsang EWK. Re-examining the functional diversity-performance relationship: the roles of behavioural integration, team cohesion, and team learning. J Bus Res. (2016) 69:3500–7. doi: 10.1016/j.jbusres.2016.01.036
51. Lau DC, Murnighan JK. Demographic diversity and faultlines: the compositional dynamics of organisational groups. Acad Manage Rev. (1998) 23:325–240. doi: 10.5465/amr.1998.533229
53. Webber SS, Donahue LM. Impact of highly and less job-related diversity on work group cohesion and performance: a meta-analysis. J Manage. (2001) 27:141–62. doi: 10.1177/014920630102700202
54. Salas E, Grossman R, Hughes AM, Coultas CW. Measuring team cohesion: observations from the science. Hum Factors. (2015) 57(3):365–74. doi: 10.1177/0018720815578267
55. Patel H, Damush TM, Meich EJ, Rattray NA, Martin HA, Savoy A, et al. Building cohesion in distributed telemedicine teams: findings from the department of veterans affairs national telestroke program. BMC Health Serv Res. (2021) 1(1):124. doi: 10.1186/s12913-021-06123-x
56. Rai T, Clements A, Bukach C, Shine B, Austoker J, Watson E. What influences men’s decision to have a prostate-specific antigen test? A qualitative study. Fam Pract. (2007) 24(4):365–71. doi: 10.1093/fampra/cmm033
57. National Screening Committee Prostate Cancer Risk Management Programme. Prostate cancer risk management programme: Overview. Public Health England (2016).
58. Gold Standards Framework. The national Gold Standards Framework (GSF) centre in end of life care statement of clarification of services and resources available and copyright licensing policy. Gold Standards Framework (2012).
59. Abel J, Kellehear A. Palliative care reimagined: a needed shift. Br Med J Support Palliat Care. (2016) 6:21–6. doi: 10.1136/bmjspcare-2015-001009
60. Meiklejohn J, Mimery A, Martin JH, Bailie RS, Garvey G, Walpole E, et al. The role of the GP in follow-up cancer care: a systematic literature review. J Cancer Surviv. (2016) 10:990–1011. doi: 10.1007/s11764-016-0545-4
61. Foster C, Calman L, Richardson A, Pimperton H, Nash R. Improving the lives of people with and beyond cancer: generating the evidence needed to inform policy and practice. J Cancer Policy. (2018) 15:92–5. doi: 10.1016/j.jcpo.2018.02.004
62. Millington-Sanders C, Noble B. New UK general practice core standards for advanced serious and end of life care. Br J Gen Pract. (2018) 68:114–5. doi: 10.3399/bjgp18X694913
63. Le B, Eastman P, Vij S, McCormack F, Duong C, Philip J. Palliative care in general practice: gP integration in caring for patients with advanced cancer. Aust Fam Physician. (2017) 46:51–5. doi: 10.3316/INFORMIT.609427035167544
64. Clarke S, Nightingale P, Cunliffe A. How can the GP support the patient through the whole cancer journey? In: Velikova G, Fallowfield L, Younger J, Board RE, Selby P, editors. Problem solving in patient-centred and integrated cancer care. Evidence-based nursing health. Oxford, UK: EBN Health (2018). p. 31–5.
65. Meier DE, Back AL, Berman A, Block SD, Corrigan JM, Morrison RS. A national strategy for palliative care. Health Aff. (2017) 36(7):1265–73. doi: 10.1377/hlthaff.2017.0164
66. British Medical Association. British Medical Association quarterly tracker survey. British Medical Association (2014).
67. Royal College of General Practitioners. Over 500 surgeries at risk of closure as GP workforce crisis deepens. Royal College of General Practitioners (2014).
68. Scottish Government. The healthcare quality strategy for NHSScotland. Scottish Government (2010).
69. Scottish government. A route map to the 2020 vision for health and social care. Scottish Government (2012).
71. Christie C. Commission on the future delivery of public services. Edinburgh, Scotland: APS Group Scotland (2011).
74. Efficace F, Collins GS, Cottone F, Giesinger JM, Sommer K, Anota A, et al. Patient-Reported outcomes as independent prognostic factors for survival in oncology: systematic review and meta-analysis. Value Health. (2021) 24(2):250–67. doi: 10.1016/j.jval.2020.10.017
75. Denis F, Lethrosne C, Pourel N, Molinier O, Pointeau Y, Domont J, et al. Randomized trial comparing a web-mediated follow-up with routine surveillance in lung cancer patients. J Natl Cancer Inst. (2017) 109:9. doi: 10.1093/jnci/djx029
76. Maguire R, McCann L, Kotronoulas G, Kearney N, Ream E, Armes J, et al. Real time remote symptom monitoring during chemotherapy for cancer: european multicentre randomised controlled trial. (eSMART). Br Med J. (2021) 374:n1647. doi: 10.1136/bmj.n1647
77. Bolton H. The montgomery ruling extends patient autonomy. Int J Obstet Gynaecol. (2015) 122(9):1273. doi: 10.1111/1471-0528.13467
78. Chan SW, Tulloch E, Cooper ES, Smith A, Wojcik W, Norman JE. Montgomery and informed consent: where are we now? Br Med J. (2017) 357:j2224. doi: 10.1136/bmj.j2224
79. Ward AL, Forbat L. Five changes needed to Scottish cancer policy to support necessary transformation of services. J Cancer Policy. (2023) 36:100420. doi: 10.1016/j.jcpo.2023.100420
80. Zachariadis M, Oborn E, Barrett M, Zollinger-Read P. Leadership of healthcare commissioning networking in England: a mixed-methods study on clinical commissioning. Health Serv Res. (2013) 3:1–14. doi: 10.1136/bmjopen-2012-002112
81. Anderson T. The medical leadership challenge in healthcare is an identity challenge. Leadersh Health Sci. (2015) 28:83–99. doi: 10.1108/LHS-04-2014-0032
82. Wieringa S, Engebretsen E, Heggen K, Greenhalgh T. Rethinking bias and truth in evidence-based health care. J Eval Clin Pract. (2018) 24(5):930–8. doi: 10.1111/jep.13010
Keywords: qualitative research and analysis, survey research and questionnaire design, clinical practice patterns/guidelines/resource used/evidence based practice, comparative health systems/international health, health care organisations and systems, nursing, medical decision-making, cancer service improvement
Citation: Ward AL, Cruickshank S and Forbat L (2023) Features that hindered the capacity development of a national prostate cancer service. Front. Health Serv. 3:1173143. doi: 10.3389/frhs.2023.1173143
Received: 24 February 2023; Accepted: 15 May 2023;
Published: 18 July 2023.
Edited by:
Chris Sampson, Office of Health Economics (OHE), United KingdomReviewed by:
Mats Brommels, Karolinska Institutet (KI), SwedenMark Emberton, University College London, United Kingdom
© 2023 Ward, Cruickshank and Forbat. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Liz Forbat ZWxpemFiZXRoLmZvcmJhdDFAc3Rpci5hYy51aw==
Abbreviations GP, General practitioner; MCN, Managed Clinical Network; NHS, National Health Service; NoSCAN, North of Scotland MCN; R1, Round 1 questionnaire; R2, Round 2 questionnaire; R3, Round 3 questionnaire; SCAN, East of Scotland MCN; WoSCAN, West of Scotland MCN.
 Ashleigh Lauren Ward
Ashleigh Lauren Ward Susanne Cruickshank
Susanne Cruickshank Liz Forbat
Liz Forbat