
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Health Serv., 22 March 2023
Sec. Health Policy and Management
Volume 3 - 2023 | https://doi.org/10.3389/frhs.2023.1071517
This article is part of the Research TopicGlobal Excellence in Health Policy and Management: AfricaView all 8 articles
Background: Non-compliance with infection control guidelines of healthcare workers may increase their risk of exposure to infectious diseases but can be prevented through adherence to standard precautionary practices in healthcare settings.
Objective: This study aimed to assess the magnitude of standard precautions practice and its associated factors among healthcare workers in government hospitals of South Wollo Zone, northeastern Ethiopia
Methods: An institutional-based cross-sectional study was conducted among 1,100 healthcare workers. Proportional sample size allocation for each selected government hospital was conducted followed by simple random sampling to select study participants using human resource records from each hospital. Data were collected using structured and self-administered pretested questionnaires. The data were analyzed using descriptive statistics, bivariable binary, and multivariable logistic regression models. Variables with a p-value <0.05 with a 95% CI were considered as having statistical significance
Results: The overall magnitude of compliance with standard precautions among healthcare workers was 19.2%. The result indicated that work experience of <5 years (AOR = 2.51; 95% CI: 1.07–5.89), absence of continuous water supply (AOR = 2.24; 95% CI: 1.95–5.29), and negative attitude (AOR = 2.37; 95% CI: 1.17–4.79) were significantly associated with poor compliance of standard precautions practice.
Conclusion: The overall magnitude of compliance with standard precautions among healthcare workers was low compared to the national magnitude of infection prevention practice. Interventions including consistent and effective training on infection prevention healthcare workers should be given regularly. Providing continuous water supply and building a positive attitude toward infection prevention practices among healthcare workers are also required.
Standard precautions (SP) also known as universal precautions are the primary method for securing worker safety and preventing Health Care Associated Infections (HCAI) including the COVID-19 pandemic. Evidence from national and international literature indicates that few professionals properly applied these guidelines (1). Various reasons contribute to the behavior of non-adherence, including institutional elements like material, human resources, and managerial commitment as well as individual factors like understanding of the SP measures (2, 3).
Hospitals are the main source of infection risk when delivering healthcare services. HCAIs are frequently disseminated by contact, airborne transmission, and droplets. They can also transmit between healthy people and the infected person, especially during hospitalization (4, 5). A significant portion of occurrences of HCAI is linked to workplace exposures (4, 6). The health and well-being of our healthcare workers and the public at large determine the nation's health, security, and economic progress in Ethiopia.
According to the World Health Organization (WHO), HCAI or “nosocomial” and “hospital” infections are the most frequent adverse event in healthcare delivery worldwide. Those infections are acquired in hospitals or healthcare service units, that first appear 48 h or more after hospital admission or within 30 days after discharge following in-patient care. They are a significant public health issue that raises morbidity, mortality, and financial losses for healthcare systems (4).
Around 3 million healthcare workers are exposed to bloodborne infections through percutaneous means each year globally of which two million of these workers are exposed to the hepatitis B virus (HBV), about one million to the hepatitis C virus (HCV), and 170,000 to the human immunodeficiency virus (7).
According to a systematic review and meta-analysis on the burden of HCAIs in Southeast Asia, the pooled prevalence of all HAIs was 9.0%, while the combined incidence density was 20 cases per 1,000 intensive care units (8). About 7 patients in industrialized countries and 10 individuals in poor nations out of every 100 hospitalized patients at any given moment acquire at least one HCAI. It affects 5% to 15% of hospitalized patients in ordinary wards and up to 50% or more of patients in intensive care units in developed nations (9).
In low and middle-income countries the frequency of intensive care unit-acquired infections is at least 2–3 times higher than in high-income countries, and healthcare-associated infection densities might be up to 13 times greater than in the USA (4, 10). Yet the size of the issue is currently underappreciated or even unknown, largely due to the complexity of HCAI diagnosis and the need for knowledge and resources for surveillance operations to inform solutions (11).
However, it was discovered in a meta-analysis to evaluate the burden of HCAI in poor nations that the proportion of HCAI was substantially higher (15•5 per 100 patients) than proportions reported from Europe and the USA (12). HCAIs account for 4% to 56% of all neonatal period deaths among hospital-born infants in underdeveloped countries, and 75% in South-East Asia and Sub-Saharan Africa (11, 12). The prevalence of healthcare-associated infections in teaching hospitals of Ethiopia's Amhara region was 14.9% (13).
Local reports revealed that there is still a high incidence of HCAIs despite a major development in the infrastructure of health institutions and the number and kind of health task forces, especially in Ethiopia, during the past 20 years (13, 14).
Healthcare-associated infections cause additional pain and have a significant financial impact on patients and their families, as is the case with many other patient safety issues. Infections prolong hospital stays, create long-term disability, increase resistance to antimicrobials, represent a massive additional financial burden for health systems, generate high costs for patients and their families, and cause unnecessary deaths.
To prevent infections during patient care and invasive operations, the implementation of fundamental standard precautions is easy and inexpensive, but it necessitates staff accountability and behavioral change (4, 6, 15). To improve the safety of patients, visitors, attendants, HCWs, and the general community in healthcare facilities, WHO launched different programs like “clean care is safe care” as a key strategy to promote infection prevention practice at all levels of healthcare settings (5, 16).
To prevent potential ease of transmission and thereby the illness, routine standard precautions are also advised by the WHO and other national and international public health organizations (17, 18). Healthcare regulations are not always followed in many healthcare institutions, and this indicates that compliance should be routinely examined to determine the elements that may help or hinder it. However, there is a large disparity in the level of compliance with standard precautions (5).
Due to the rising need for modern healthcare, Ethiopia is experiencing a significant increase in the number of healthcare facilities, so the government has implemented favorable laws to promote the establishment of both public and private hospitals. Even though the northeastern portions of Ethiopia have many hospitals and a considerable number of healthcare professionals, the state of compliance with standard precaution procedures and its determinant factors remains unexplored.
Due to the lack of scientific evidence, two obvious research questions arise:
Firstly, what is the level of compliance with standard precautions measures? and secondly, what are the predictors of inadequate adherence to standard precautionary measures?
The results of this study would help policymakers and planners to create effective intervention and control strategies for healthcare-acquired infections. Therefore, the purpose of this study was to evaluate how well healthcare professionals in public hospitals in the South Wollo zone in northeastern Ethiopia complied with standard precautions practice and the associated factors.
South Wollo is one of ten zones in the Amhara Region of Ethiopia. South Wollo is bordered on the south by North Shewa and the Oromia Region, on the west by West Gojjam, on the northwest by South Gondar, on the north by North Wollo, on the northeast by Afar Region, and on the east by the Oromia Zone and the Argobba special woreda (Figure 1).
South Wollo Zone has eleven (11) hospitals with a catchment population of 2,518,862. Of which 301,638 (11.98%) are urban inhabitants, a further 2,217.224 (88.02%) inhabitants were reported to be rural; it also has an area of 17,067.45 square kilometers, with a population density of 147.58.
An institutional-based cross-sectional study was conducted to assess the magnitude of compliance with standard precautions practice and its associated factors among healthcare workers in public hospitals of South Wollo zone in northeastern Ethiopia from June to July 2021.
In this study, healthcare workers were defined as regularly employed hospital staff who provided direct patient care or had regular direct contact with patients, as well as graduating class intern doctors. The source population of this study was all healthcare workers working in hospitals while the study population was all selected healthcare workers in hospitals of South Wollo zone in northeastern Ethiopia. From the study population, all permanent healthcare workers employed in the hospitals were included in the study.
The sample size was determined using the single population proportion formula with the following assumptions: Magnitude of compliance with standard precaution practice (p = 12%) was taken from a study conducted in Gondar University comprehensive specialized hospital, northwest Ethiopia (19)
(20) Where: n: is the optimum sample size required.
P: is an estimate of the magnitude of compliance with standard precaution.
Z: is the standard normal variable at (1-α) % confidence level and α is mostly 0.05 i.e. with 95% CI (z = 1.96) and d: is the margin of error to be tolerated (%).
The determination of the margin of error is based on the optimum sample size and availability of resources.1% giving the largest sample size and 5% giving the smallest sample size. For this study, it was used a margin of 2% based on the proportion of 12% taken from a similar study mentioned above, which gives an adequate sample size.
After adding 10% non-response rate the final sample size was n = 102 + 1014 = 1116.
There are eleven hospitals in the South Wollo zone from which four hospitals were selected randomly. All 1,116 estimated participants were proportionally allocated to each hospital-based upon their respective numbers of healthcare workers. The study participants were selected using a simple random sampling method. Those study participants that were not available at the first visit, the study participants were revisited once the same day or following day. Those who were not available again, the study participants were considered as a non-respondent.
• Compliance with standard precaution practice (Compliant/Non-compliant)
• Socio demographic factors
Age of respondent, marital status, type of profession sex, work experience, and assigned place (ward).
• Institutional and behavioral factors
Availability of PPE, Presence of IP guidelines, availability of continuous running water supply, Training on infection prevention, attitude towards infection prevention practice, Knowledge of standard precautions, job satisfaction, and Chewing chat(khat) since most residents including healthcare workers in South Wollo zone practice consuming khat and this culture is rapidly expanding.
Compliance of standard precaution practice: At the beginning of the analysis, those who reported that they were always compliant were taken as “compliant” and those who reported that they were sometimes and never compliant were taken as “non-compliant.” Next, the summation of the 22 compliance items was made. Then, the variable was recoded and dichotomized (compliant/non-compliant).
Knowledge: Knowledge of infection prevention and control practices was measured using 10 knowledge assessment questions. Each correct answer “yes” scored “1” and “no” scored “0” points for each knowledge question. If a HCW scored less than or equal to eight (≤80%) of all knowledge questions, it was considered to have poor knowledge (21).
Attitude: It was determined by computing the outcome of all 10 attitude assessment questions. Each criterion was given a value of 1 for agree and 0 for disagree. If a HCW scored less than or equal to eight (≤80%) of all attitude questions, it was considered to have a negative attitude (21).
Continuous running water supply: availability of continuously running water supply means that water is delivered continuously to every ward in need for 24 h a day, every day of the year.
A structured questionnaire was adapted from related literature (22–24). The questionnaire was first be prepared in English, translated to Amharic (the local language), and translated back to English to ensure consistency.
Training of the data collectors was provided by the principal investigator. It was taken two days focused on the questions in the survey instrument plus additional time for performing the observation of the practice and considering ethical issues. A pre-test was conducted using a 5% sample size of the total study sample in Woldeya hospital to establish the validity of the questionnaire. The questionnaire was amended based on the findings of the pre-test. The pre-test also served to familiarize the data collectors with the questionnaire and give them experience with data collection.
Six BSc nurses collected the data through a self-administered pretested and structured questionnaire. First, healthcare workers were asked to report each question about standard precautions and secondly, observation of certain practices during the time of data collection. Study participants were aware that they will be observed at some period, but they did not know exactly when they will be observed to reduce HCWs' behavior (Hawthorne effect). A single observer, who is also a co-investigator, was present at the study site to gather the data. The data were collected over a period of 30-minute sessions spread out across the day and night. If there was a privacy curtain drawn over the patient's bed, the normal precautionary measure was not followed. If the practice is carried out during times that are not designated by the WHO's recommended standard precaution practices, it is regarded as complementary and the observer did not keep track of it Three public health experts supervised the collection process for data quality control. The completeness and consistency of the questionnaires were checked daily before data entry.
Data were entered using EpiData version 3.1 and exported to Statistical Package of Social Science (SPSS) version 25.0 for data cleaning and analysis. Once the data were entered, basic quality assurance measures including data cleaning using browsing of data tables after sorting, frequency distributions, cross-tabulations, summary statistics, and statistical outlier detection using sorting were performed. Descriptive statistics were used for categorical variables and mean ± SD (standard deviations) for continuous variables. Continuous variables were categorized using information from the literature, and categorical variables were re-categorized accordingly.
Bivariate [crude odds ratio (COR)] and multivariable [adjusted odds ratio (AOR)] values were calculated using logistic regression analysis with a 95% confidence interval [CI]. From the bivariate analysis, variables with p < 0.25 were considered as candidate variables for multivariable analysis. From the multivariable logistic regression analysis, variables with a significance level of p < 0.05 were taken as statistically significant and independently associated with compliance with standard precaution practice.
The presence of multi-collinearity among independent variables was checked using standard error at the cutoff value of 2. Model fitness was checked using the Hosmer-Lemeshow test which had a p-value > 0.05.
One thousand one hundred (98.6%) of the 1,116 healthcare professionals who participated in the study completed self-administered questionnaires. Regarding the gender of the study participants, 536 (50.7%) of the HCWs were married, and 620 (56.4%) of the participants were females. The majority of participants (657, or 59.7% of the total number of health care employees) were nurses, while approximately quarters (274, or 24.9%) were doctors. Seven hundred seventy-two respondents (70.2%) had bachelor's degrees, whereas 214 respondents (19.4%) had five to ten years of experience, and 826 respondents (75.1%) had more than ten years of work experience (Table 1).

Table 1. Socio-demographic characteristics of the health care worker in government hospitals of South Wollo zone, northeastern Ethiopia, 2021.
Only 222 (20.2%) of healthcare workers reported having a constant water supply for infection prevention practices, despite the fact that nearly three-quarters of 812 (73.8%) healthcare workers reported having an infection prevention guideline as a working protocol for preventing HCAIs.
More than seven in ten (77.9%) healthcare workers reported having personal protective equipment in their workplaces, and more than half (52.4%) of HCWs reported having completed training in infection prevention and control. However, 38.7% or more of the HCW population, or 426 people, still exhibited a negative attitude toward infection control measures. (Table 2).
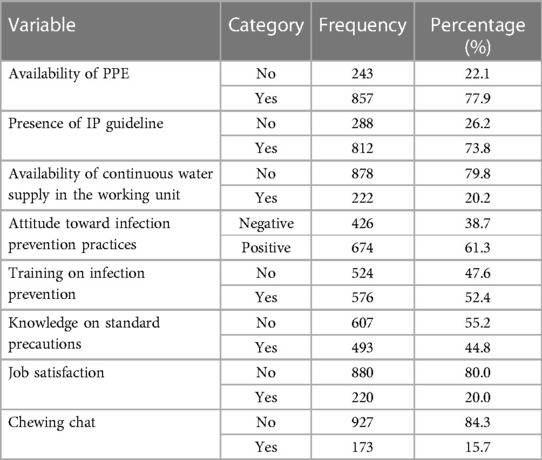
Table 2. Institutional and behavioural factors of the healthcare worker in government hospitals of South Wollo zone, northeastern Ethiopia, 2021.
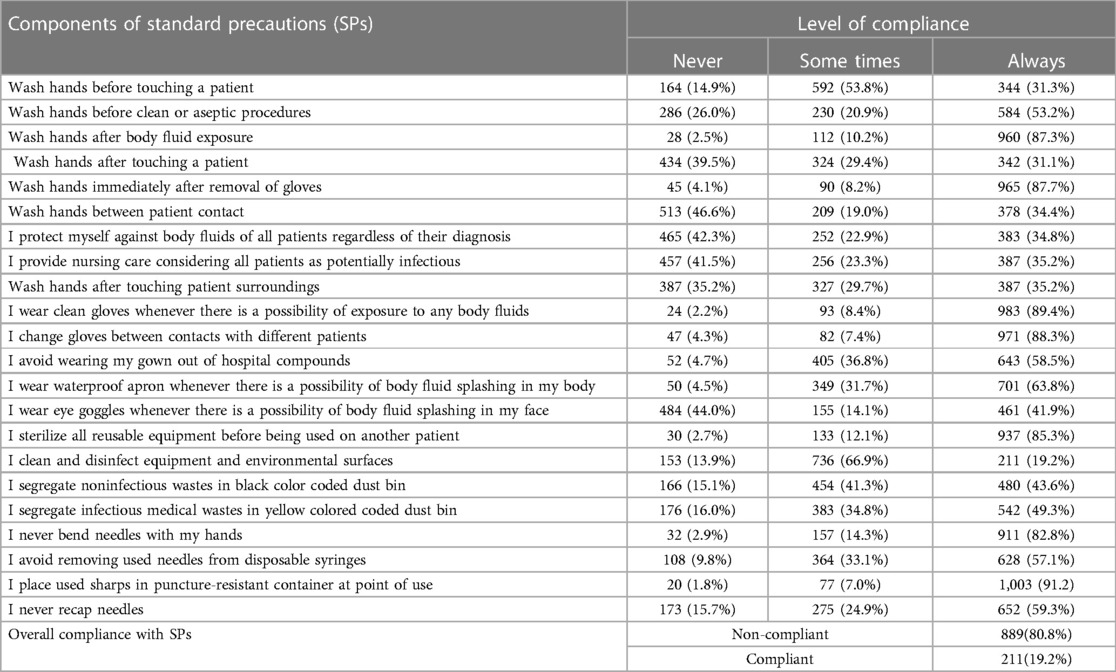
Table 3. Level of compliance with standard precautions among healthcare worker in government hospitals of South Wollo zone, northeastern Ethiopia, 2021.
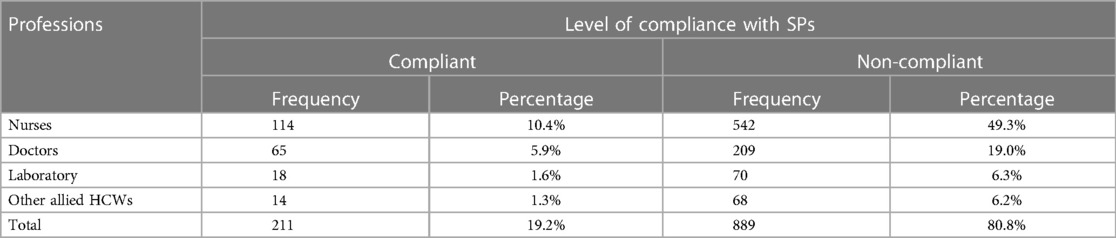
Table 4. Proportion of HCWs compliance with standard precaution practice by professionals in government hospitals of northeastern Ethiopia, 2021.
We estimated a mean score of 30.38 ± 7.07 for the cumulative standard precautions compliance measuring domain, with a possible range of 0–44. Only one-third of them 344(31.3%), more than half 585(53.2%), and much more than three quarters 960(87.3%) of them always performed hand washing before handling a patient, before clean or aseptic operations, and after bodily fluid exposure respectively. Moreover, 342 (31.1%) of the HCWs practiced hand washing after making physical contact with a patient, 965 (87.7%) of HCWs washed their hands right after taking off their gloves, and 378 (34.4%) of HCWs applied hand washing in between patient contacts,.
About 35% of healthcare workers protected themselves against body fluids of all patient types regardless of their diagnosis and provided nursing care considering all patients as potentially infectious concurrently (Table 3). The overall proportion of HCWs who had good compliance with standard precaution practice was found to be 211(19.2%), 95% CI: 15.8–22.6) (Figure 2 and Table 4).
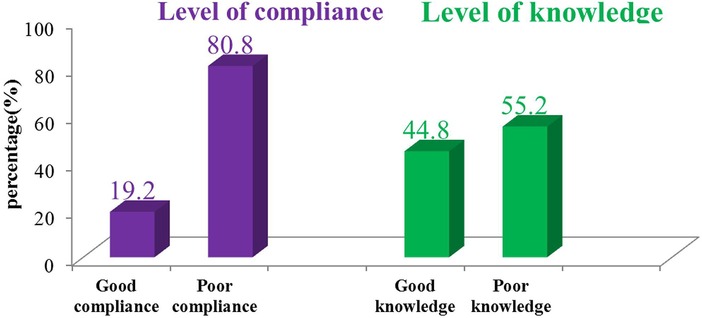
Figure 2. The magnitude of compliance with standard precaution practice and knowledge among healthcare workers in public hospitals of South Wollo zone, northeastern Ethiopia, April-May 2021 (n = 1,100).
Adjusted logistic regression analysis results indicated that work experience with less than 5 years (AOR = 2.51; 95% CI: 1.07–5.89), absence of continuous water supply (AOR = 2.24; 95% CI: 1.95–5.29), and negative attitudes toward infection prevention practices (AOR = 2.37; 95% CI: 1.17–4.79) were significantly associated with poor compliance of standard precautions practice (Table 5).
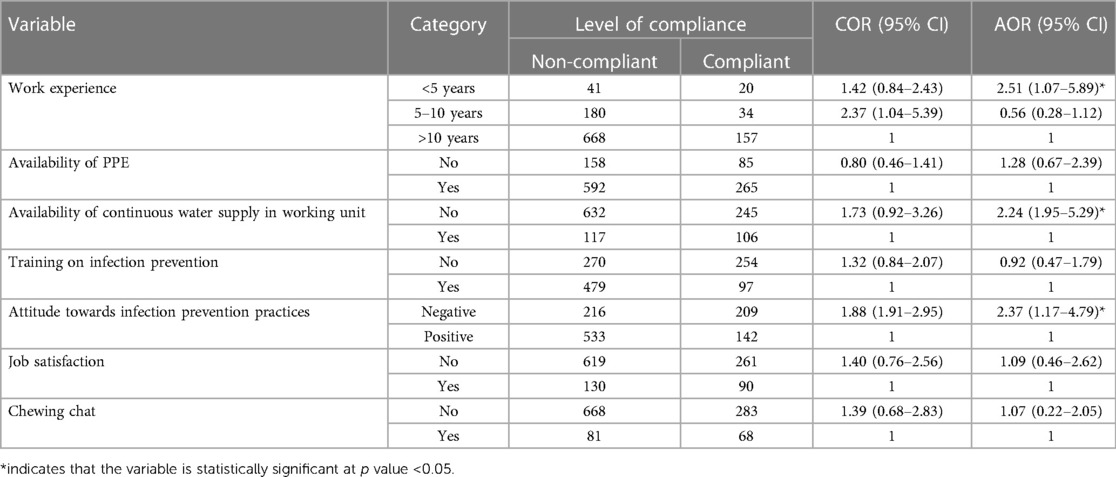
Table 5. Factors associated with standard precautions practice among healthcare workers in government hospitals of northeastern Ethiopia .
Understanding reasons for non-compliance are the most important point to plan and to design interventions and strategies for improving behavior and programs that target conditions to prevent HCAI (6, 11, 25) and it is also critical to examine factors that influence compliance so that this study evaluated the compliance and determinant factors with conventional measures among 1,100 healthcare professionals in government hospital settings.
The best and most affordable method for preventing and controlling the transmission of HCAIs between patients and healthcare workers, patient attendants, and the general public has been thought to be HCW compliance with conventional precaution practices (6, 12, 14, 25).
The findings of this study showed that healthcare professionals generally adhered to standard precautions practices at a relatively low level. In contrast to earlier studies conducted in Gondar, Ethiopia (12%) (19), Hadiya, Ethiopia (15.0%) (26), Nigeria (14.85%) (27), and northeastern USA (17.4%) (28), the self-reported compliance of standard precaution practice among healthcare workers in this study was 19.2%.
The reasons for this non-adherence to SPs practice might be due to differences in a wide range of factors, including culture, economic and social factors, management commitment on the part of the institution, human resources, and individual factors like self-efficacy, beliefs, and knowledge of SPs measures, as well as professionals' lack of knowledge or resources.
The results of this study were, however, less favorable than those of studies carried out in Bahir Dar Town (41%) (29), Dawuro Zone, southwest Ethiopia (65%) (30), Hawassa Comprehensive Hospital, Sidama Ethiopia (56.5%) (31), North Shewa, Oromia (46.8%) (21), Addis Ababa, Ethiopia (66.1%), public hospitals in Abuja, Nigeria (76.2%) (32), and other two tertiary hospitals in Nigeria (50.8%) (33).
The primary factor contributing to the low rate of compliance with typical precautionary measures in this study might be a lack of training regarding their use and purpose in preventing HCAI (only half of HCWs reported that they received infection prevention training). Compliance with recommended safety measures can be improved via infection prevention training (34) and can reduce the perception of risk (35). Insufficient time, carelessness, discomfort, forgetfulness, lack of habit, and the belief that there is a low danger of infection may also contribute to limited compliance with routine precautionary measures.
The habit of hand washing practice in this study was a little higher than it was in previous studies done in comprehensive specialized hospitals in Gondar and Hawassa (19, 31). In those studies, it was found that hand washing was always practiced before touching a patient in Gondar (18.2%) and Hawassa (18.9%), between patient contacts in Gondar (19.4%) and Hawassa (27.1%). This difference might be brought on by varying workloads, a lack of hand washing facilities, difficulty accessing them, a lack of awareness of the need for hand hygiene in preventing infections, and a lack of a culture of safety that provides feedback.
The results of this study showed that HCWs’ compliance with recommended precautions was positively impacted by their job experience. In comparison to HCWs with less than five years of experience, those with more than ten years of experience were 2.51 times more likely to comply with standard precaution practices.
It is consistent with earlier findings from study conducted in Tanzania concerning, Egypt (36) compliance in segregation of non-sharp infectious waste from injection or blood draw (18.7%) (37), Abuja, Nigeria with mean compliance of standard precaution practice (23.2%) (32), Jordan (38) China (28.7%) (39), Shiraz, Iran (22.2%) and Italy (35).
Healthcare workers were 2.24 times more likely to be non-compliant with standard precaution measures than their counterparts if there was no continuous flowing water in the working department. A constant running water supply in the working area might directly promote compliance with standard precaution practices among HCWs because access to poor or interrupted water supply can hamper infection prevention practices in healthcare facilities. This association is consistent with the earlier studies done in Bahir Dar, Ethiopia (29), Hawassa, Ethiopia (31), Addis Ababa, Ethiopia (40) and Nigeria (33).
Healthcare workers with a negative attitude towards standard precaution practice were more than two times (AOR = 2.37) more likely to be non-compliant with standard precaution practice. This result is in line with studies done in Addis Ababa, Ethiopia (41) Shewa, Ethiopia (21) and Italy (35). This showed that having a positive attitude is essential for increasing compliance with infection prevention and control practices which may encourage healthcare workers to follow recommended precautions against the disease.
Inadequate adherence to established precautionary procedures by healthcare professionals was found in South Wollo Zone government hospitals. The results of multivariable logistic regression analysis showed that lack of a continuous water supply, negative attitudes towards standard precaution practice, and work experience of less than five years were the key predictor variables for non-compliance with standard precaution practice.
The findings of this study highlight the urgent need for decision-makers to address inadequate compliance with basic precaution practices among HCWs in hospital settings. These findings should guide the development of efforts to promote the accessibility of a continuous water supply and alter the mindset of healthcare professionals through infection control training. We firmly urge national governments, the commercial sector, and the general public to pay close attention to healthcare worker safety.
This study did not use a longitudinal follow-up design; instead, data were collected using a self-administered questionnaire and a single practice observation, raising the possibility of observer and responder bias. To ensure the quality of the data, we operationalized variables, followed the right procedures, and trained skilled data collectors.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The study was conducted in accordance with the Helsinki declaration. The ethical approval letter was obtained from the Institutional Ethical Review Committee of the College of Medicine and Health Sciences of Wollo University with the issue number of CMHS/368/13/21. Written informed consent was obtained from the participants before commencement of the study.
AK, ML, AA, and MA contributed to the conception and design of the study. AK, ML, and AA conducted the investigation. AK, AA, TS, ML, GB, and MA performed data management and analysis. AK, AA, GB, and MA wrote and edited the manuscript. All authors contributed to the article and approved the submitted version.
This research was supported by Wollo University (Grant No: WU/2441/13).
The authors express their heartfelt gratitude to Wollo University for funding and to Zonal health officers for giving valuable information for this study. We are also grateful for data collectors, supervisors, and hospital administrators.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
AOR, Adjusted Odds Ratio; CI, Confidence Interval; COR, Crude Odds Ratio; HCAI, Health Care Associated Infection; HCWs, Health Care Workers; SP, Standard Precautions; SPSS, Statistical Package for Social Science; WHO, World Health Organization.
1. CDC. Guidelines for infection control in health care facilities. Available at: https://www.health.qld.gov.au/clinical-practice/guidelines-procedures/diseases-infection/infection-prevention/management-plans-guidance/guidelines (2019).
2. Efstathiou G, Papastavrou E, Raftopoulos V, Merkouris A. Factors influencing nurses’ compliance with standard precautions in order to avoid occupational exposure to microorganisms: a focus group study. BMC Nurs. (2011) 10:1–12. doi: 10.1186/1472-6955-10-1
3. Valim MD. Instruments and impacting factors on standard precautions knowledge among health workers/instrumentos e fatores impactantes sobre o conhecimento das medidas de precauções-padrão entre trabalhadores de saúde/instrumentos y factores impactantes en conocimie. Enfermería Global. (2016) 15(1):305–21. Available at: https://search.proquest.com/docview/1784042521?accountid=17242 doi: 10.6018/eglobal.15.1.223561
4. WHO. Report on the Burden of Endemic Health Care-Associated Infection Worldwide: A systematic review of the literature (2011). WHO: Geneva, Switzerland. https://www.who.int/publications/i/item/report-on-the-burden-of-endemic-health-care-associated-infection-worldwide (Accessed 10 October, 2022).
5. Pan American Health Organization and WHO. Prevention and control of healthcare-associated infections: Basic recommendations. Washington, D.C.: PAHO (2018).
6. Al-Tawfiq JA, Tambyah PA. Healthcare associated infections (HAI) perspectives. J Infect Public Health. King Saud Bin Abdulaziz University for Health Sciences (2014) 7(4):339–44. doi: 10.1016/j.jiph.2014.04.003
7. Coppola N, De Pascalis S, Onorato L, Caló F, Sagnelli C, Sagnelli E. Hepatitis B virus and hepatitis C virus infection in healthcare workers. World J Hepatol. (2016) 8(5):273–81. doi: 10.4254/wjh.v8.i5.273
8. Ling ML, Apisarnthanarak A, Madriaga G. The burden of healthcare-associated infections in Southeast Asia: a systematic literature review and meta-analysis. Clin Infect Dis. (2015) 60(11):1690–9. doi: 10.1093/cid/civ095
9. Vincent J, Marshall J, Anzueto A, Martin CD, Moreno R, Lipman J, Gomersall C, Sakr Y, Reinhart K. International study of the prevalence and outcomes of infection in intensive care units. Jama. (2009) 302(21):2323–9. doi: 10.1001/jama.2009.1754
10. Klevens RM, Edwards JR, Richards CL Jr., Horan TC, Gaynes RP, Pollock DA, Cardo DM. Estimating health care-associated infections and deaths in U.S. Hospitals, 2002. Public Health Rep. (2007) 122(2):160–6. doi: 10.1177/003335490712200205
11. Nejad SB, Allegranzi B, Syed SB, Ellisc B, Pittet D. Health-care-associated infection in Africa: a systematic review. Bull W H O. (2011) 89(10):757–65. doi: 10.2471/BLT.11.088179
12. Allegranzi B, Nejad SB, Combescure C, Graafmans W, Attar H, Donaldson L, Pittet D. Burden of endemic health-care-associated infection in developing countries: systematic review and meta-analysis. Lancet. Elsevier Ltd (2011) 377(9761):228–41. doi: 10.1016/S0140-6736(10)61458-4
13. Yallew WW, Kumie A, Yehuala FM. Point prevalence of hospital-acquired infections in two teaching hospitals of amhara region in Ethiopia. Drug Healthc Patient Saf. (2016) 8:71–6. doi: 10.2147/DHPS.S107344
14. Ali S, Birhane M, Bekele S, Kibru G, Teshager L, Yilma Y, et al. Healthcare associated infection and its risk factors among patients admitted to a tertiary hospital in Ethiopia: longitudinal study. Antimicrob Resist Infect Control. (2018) 7(2):1–9. doi: 10.1186/s13756-017-0298-5
15. Bolyard EA, Tablan OC, Williams WW, Pearson ML, Shapiro CN, Deitchman SD. Erratum: guideline for infection control in health care personnel, 1998 (American journal of infection control (1998) 26 (289-354)). Am J Infect Control. (1998) 26(4):430. doi: 10.1016/S0196-6553(98)70049-5
16. Federal Ministry of Health. Infection Prevention and Patient Safety: Reference Manual for Service Providers and Managers in Healthcare Facilities of Ethiopia. (2012) FMOH: Addis Ababa, Ethiopia. http://repository.iifphc.org/bitstream/handle/123456789/651/8%20Infection%20prevention%20and%20patient%20safety%20Reference%20manual%20for%20service%20providers%20and%20Managers%20in%20healthcare%20facilities%20second%20edition%20February%2C%202012.pdf?sequence=1&isAllowed=y (Accessed 8 October, 2022).
17. Delgado D, Quintana FW, Perez G, Sosa Liprandi A, Ponte-Negretti C, Mendoza I, Baranchuk A. Personal safety during the COVID-19 pandemic : realities and perspectives of healthcare workers in Latin America. Int J Environ Res Public Health. (2020) 17(2798):1–8. doi: 10.3390/ijerph17082798
18. WHO. Laboratory testing for 2019 novel coronavirus (2019-nCoV) in suspected human cases: Interim guidance. (2020). WHO: Geneva, Switzerland. https://www.who.int/publications/i/item/10665-331501 (Accessed 8 October, 2022).
19. Haile TG, Engeda EH, Abdo AA. Compliance with standard precautions and associated factors among healthcare workers in gondar university comprehensive specialized hospital, northwest Ethiopia. J Environ Public Health. (2017) 2017:1–8. doi: 10.1155/2017/2050635
20. Kelsey J, Whittemore A, Evans A, Thompson W. Methods of sampling and estimation of sample size. Methods in observational epidemiology. New York: Oxford University Press (1996).
21. Jemal K, Gashaw K, Kinati T, Bedada W, Getahun B. Clean and safe healthcare environment: knowledge, attitude, and practice of infection prevention and control among health workforce at north showa zone oromiya region. J Environ Public Health. (2020) 2020:1–10. doi: 10.1155/2020/6021870
22. Duarte Valim M, Aparecida Pinto P, Helena Palucci Marziale M. Questionnaire on standard precaution knowledge: validation study for Brazilian nurses use. Texto Contexto Enferm. (2017) 26(3):1–8. doi: 10.1590/0104-07072017001190016
23. Federal Ministry of Health. Infection Prevention Guidelines for Healthcare Facilities in Ethiopia. (2004) FMOH: Addis Ababa, Ethiopia. http://repository.iifphc.org/handle/123456789/1418?show=full (Accessed 9 October, 2022).
24. Gershon RRM, Vlahov D, Felknor SA, Vesley D, Johnson PC, Delclos GL, et al. Compliance with universal precautions among health care workers at three regional hospitals. Am J Infect Control. (1995) 23(4):225–36. doi: 10.1016/0196-6553(95)90067-5
25. Van Kleef E, Robotham JV, Jit M, Deeny SR, Edmunds WJ. Modelling the transmission of healthcare associated infections: a systematic review. BMC Infect Dis. (2013) 13(1):1. doi: 10.1186/1471-2334-13-294
26. Yohannes T, Kassa G, Laelago T, Guracha E. Health-Care Workers’ compliance with infection prevention guidelines and associated factors in hadiya zone, southern Ethiopia: hospital based cross sectional study. Epidemiol Int J. (2019) 3(1):1–13. doi: 10.23880/eij-16000117
27. Ogbonda PN, Douglas K, Moore BM. Knowledge and compliance with standard precautions amongst healthcare workers in selected hospitals in rivers state, Nigeria. Asian J Med Health. (2020) 18(2):11–22. doi: 10.9734/ajmah/2020/v18i230181
28. Powers D, Armellino D, Dolansky M, Fitzpatrick J. Factors in fl uencing nurse compliance with standard precautions. Am J Infect Control. (2016) 44(1):4–7. doi: 10.1016/j.ajic.2015.10.001
29. Mulat Endalew S, Abebe Melake B, Geremew A, Baraki N, Adare Mengistu D, Sintie Alamirew T, et al. Healthcare Workers’ compliance with standard precautions and associated factors in bahir dar town, Ethiopia. Environ Health Insights. (2022) 16:1–11. doi: 10.1177/11786302221117071
30. Beyamo A, Dodicho T, Facha W. Compliance with standard precaution practices and associated factors among health care workers in dawuro zone, south west Ethiopia, cross sectional study. BMC Health Serv Res. (2019) 19(1):4–9. doi: 10.1186/s12913-019-4172-4
31. Bekele T, Ashenaf T, Ermias A, Arega Sadore A. Compliance with standard safety precautions and associated factors among health care workers in hawassa university comprehensive, specialized hospital. PLoS ONE. (2020) 15(10):1–11. doi: 10.1371/journal.pone.0239744
32. Esu I, Okeke C, Gobir A. Factors affecting compliance with standard precautions among healthcare workers in public hospitals Abuja, Nigeria. Int J Trop Dis Health. (2019) 36(2):1–11. doi: 10.9734/ijtdh/2019/v36i230141
33. Ogoina D, Pondei K, Adetunji B, Chima G, Isichei C, Gidado S. Knowledge, attitude and practice of standard precautions of infection control by hospital workers in two tertiary hospitals in Nigeria. J Infect Prev. (2015) 16(1):16–22. doi: 10.1177/1757177414558957
34. Verbeek JH, Rajamaki B, Ijaz S, Sauni R, Toomey E, Blackwood B, et al. Personal protective equipment for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare staff. Emergencias. (2021) 33(1):59–61. doi: 10.1136/oemed-2018-icohabstracts.500
35. Savoia E, Argentini G, Gori D, Neri E, Piltch-Loeb R, Pia Fantini M. Factors associated with access and use of PPE during COVID-19 : a cross-sectional study of Italian physicians. PLoS ONE. (2020) 15(10):1–12. doi: 10.1371/journal.pone.0239024
36. Hakim SA, Abouelezz NF. Use of personal protective devices among health care workers in a teaching hospital in Cairo, Egypt. Egypt J Occup Med. (2016) 40(2):287–300. doi: 10.21608/ejom.2016.846
37. Powell-jackson T, King JJC, Makungu C, Spieker N, Woodd S, Risha P, Goodman C. Infection prevention and control compliance in Tanzanian outpatient facilities : a cross-sectional study with implications for the control of COVID-19. Lancet Glob Health. The Author(s). Published by Elsevier Ltd. This is an Open Access article under the CC BY 4.0 license (2020) 8(6):780–9. doi: 10.1016/S2214-109X(20)30222-9
38. Al-faouri I, Hussein Okour S, Ahmad Alakour N, Alrabadi N. Knowledge and compliance with standard precautions among registered nurses : a cross-sectional study. Ann Med Surg. Elsevier Ltd (2021) 62(December 2020):419–24. doi: 10.1016/j.amsu.2021.01.058
39. Luo Y, He GP, Zhou J-W, Luo Y. Factors impacting compliance with standard precautions in nursing, China. Int J Infect Dis. (2010) 14(12):e1106–14. doi: 10.1016/j.ijid.2009.03.037
40. Sahiledengle B, Gebresilassie A, Getahun T, Hiko D. Infection prevention practices and associated factors among healthcare workers in governmental healthcare facilities in Addis Ababa infection prevention practices and associated factors among healthcare workers in governmental healthcare facilities in add. Ethiop J Health Sci. (2018) 28(2):177–86. doi: 10.4314/ejhs.v28i2.9
Keywords: associated factors, guideline adherence, healthcare, practice, standard precaution
Citation: Keleb A, Lingerew M, Ademas A, Berihun G, Sisay T and Adane M (2023) The magnitude of standard precautions practice and its associated factors among healthcare workers in governmental hospitals of northeastern Ethiopia. Front. Health Serv. 3:1071517. doi: 10.3389/frhs.2023.1071517
Received: 16 October 2022; Accepted: 28 February 2023;
Published: 22 March 2023.
Edited by:
Godfrey Mubyazi, National Institute of Medical Research, TanzaniaReviewed by:
Rebecca A Lorenz, University at Buffalo, United States© 2023 Keleb, Lingerew, Ademas, Berihun, Sisay and Adane. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Awoke Keleb a2FsZWJhd29rZUBnbWFpbC5jb20=
Specialty Section: This article was submitted to Health Policy and Management, a section of the journal Frontiers in Health Services
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.