
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Health Serv., 25 October 2022
Sec. Mental Health Services
Volume 2 - 2022 | https://doi.org/10.3389/frhs.2022.994474
This article is part of the Research TopicWorld Mental Health Day 2022: Key Drivers of Risk to Mental Health Services and Innovative SolutionsView all 16 articles
 Jacqueline Bannon1*
Jacqueline Bannon1* Charlesnika T. Evans2,3,4
Charlesnika T. Evans2,3,4 Melanie Freedman5
Melanie Freedman5 Cerina Lee6
Cerina Lee6 Thanh Huyen Vu3
Thanh Huyen Vu3 Amisha Wallia2,7
Amisha Wallia2,7 John T. Wilkins2,8
John T. Wilkins2,8 Judith T. Moskowitz5
Judith T. Moskowitz5 Lisa R. Hirschhorn5
Lisa R. Hirschhorn5Burnout, depression, and anxiety are prevalent among healthcare workers (HCWs) during the COVID-19 pandemic and have been previously shown to contribute to poor health outcomes and reduced quality of care. Positive psychological constructs such as positive affect and meaning and purpose are related to resilience in the face of significant stress. No studies have examined these associations among a cohort of HCWs during this pandemic. The purpose of this study was to examine the association of depression, anxiety, positive affect, and meaning and purpose with burnout among HCWs during the COVID-19 pandemic. We utilized data from a cross-sectional survey conducted between September 29-December 8, 2021, among a cohort of 2,411 HCWs from a large, tertiary academic health care system in the Chicago area. We employed the Patient-Reported Outcomes Measurement Information System (PROMIS) measures for depression, anxiety, positive affect, and meaning and purpose and burnout was measured by the Oldenburg Burnout Inventory (OLBI). The majority (80.88%) of HCWs in this study identified as White, Non-Hispanic race/ethnicity, female sex (82.37%), and roughly one third were between ages 30–39 years old (30.98%). Registered nurses (26.96%) accounted for the largest single occupation group. The mean burnout score was 36.87 (SD = 7.65), with 53.38% of participants classified as having burnout, and registered nurses demonstrating the highest proportions of burnout (63.54%). Higher depression (coef = 0.15, SE = 0.03, p < 0.001) and anxiety (coef = 0.25, SE = 0.02, p < 0.001) scores were associated with higher burnout in multivariable linear regression models. Increased positive affect (coef= −0.19, SE= 0.02, p < 0.001) and meaning and purpose (coef= −0.12, SE= 0.01, p < 0.001) scores were significantly associated with reduced burnout. Positive affect and meaning and purpose were inversely associated with burnout among a cohort of HCWs during the COVID-19 pandemic. Previous studies of positive affect and meaning and purpose suggest the potential buffering effect that these indices may have on burnout. Future research is needed to examine the effect of positive affect and meaning and purpose on mitigating the negative impacts of burnout, depression, and anxiety among HCWs as they cope with the stress of the COVID-19 pandemic and beyond.
Burnout is an ongoing, significant threat to healthcare worker (HCW) well-being and to health systems' abilities to deliver quality, people-centered care (1–4). Burnout is characterized by emotional exhaustion (feeling emotionally drained by contact with patients), depersonalization (extreme detachment from patients), and lack of personal accomplishment (feelings of incompetence and lack of job success) (5–7). Burnout has been linked to poor health outcomes for HCWs- including depression, cardiometabolic risk behaviors (e.g. reduced physical activity, cigarette smoking), increased alcohol consumption, and sleep disruptions (8–11)—and the work environment and patients they care for, such as through increased medical errors, absenteeism, and poor quality of care (12–15).
Studies of burnout have highlighted the severe mental health impacts to HCWs amid the COVID-19 pandemic (16–18). Several literature reviews and meta-analyses have noted increased prevalence of depression, anxiety, sleep disturbances, post-traumatic stress, and other psychological disorders among HCWs since the start of the pandemic (19–24). However, studies have less frequently examined domains of positive psychological wellbeing and their associations with HCW burnout. Additionally, there are few evidence-based interventions to reduce burnout, anxiety, and depression among HCWs. Of available evidence-based interventions for HCWs, these interventions largely focus on mindfulness or meditation-based interventions rather than broader psychological domains of wellbeing (25–28).
Growing evidence from groups experiencing a variety of types of significant life stress, suggests that the ability to maintain positive psychological wellbeing in the context of stress may be protective against mental and physical health consequences of stress and burnout (29–32). Psychological wellbeing has traditionally been conceptualized to include both hedonic, or feelings of positive affect, and eudaimonic, or a sense meaning and purpose in life, domains (33–35). Among HCWs, positive affect has been associated with increased creative problem solving and job satisfaction, and these aspects of psychological wellbeing may help to buffer the stress of the COVID-19 pandemic and reduce the likelihood of burnout (36–38). To that end, a focus on wellbeing has recently been prioritized by the U.S. Surgeon General, as health systems must promote meaning and purpose in work to reduce burnout as HCWs provide life-saving care (39).
In the present study, we examine the associations of depression, anxiety, positive affect, and meaning and purpose with burnout among a cohort of HCWs in the US during the COVID-19 pandemic. We hypothesize that burnout will be positively associated with depression and anxiety, and inversely associated with positive affect and meaning and purpose. We will also examine the extent to which demographic factors (e.g. age, biological sex), occupational role, degree of patient contact, and occupational COVID-19 exposure, provide insights into the association between psychological health and burnout.
This was an analysis of data from the Northwestern Medicine Healthcare Worker SARS-CoV-2 Serology Study, a prospective cohort study of healthcare workers from a large, tertiary academic health care system. The study is described in more detail elsewhere but briefly, includes HCWs from 10 hospitals, 18 immediate care centers, and 325 outpatient practices in the Chicago area and surrounding Illinois suburbs (40–42). From May 28 to June 30, 2020, 38,127 Northwestern Medicine HCWs were invited in to participate in an employer-sponsored benefit that provided free SARS-CoV-2 serological testing, for which all HCWs were eligible. A total of 18,985 (49.8%) participated in the employer-sponsored serological benefit. HCWs enrolled in the benefit included 79.6% women and 74.9% non-Hispanic White, 9.7% Asian, 7.3% Hispanic, and 3.1% non-Hispanic Black workers, with a mean age was of 40.6 (SD:12.0) years old, and nurses represented the largest occupational group (n = 1794) (41). Those that attended the serologic testing were recruited to enroll in the Northwestern Medicine Healthcare Worker SARS-CoV-2 Serology Study, a 1-year cohort study, which included monthly, self-administered, online surveys related to COVID-19 exposures, testing, symptoms, and vaccine intentions. In the original 1-year cohort study, 6,510 HCWs enrolled in the study. In June 2021, cohort participants were recruited to continue in an extension cohort study in which 3,538 consented to enroll in the ongoing extension cohort. This present analysis was conducted on psychological health and burnout data collected from the participants who enrolled in the extension and completed a self-administered, online survey between September 29 and December 8, 2021.
Participants were asked to report demographics (e.g. race/ethnicity, age, and sex), household size, and occupation (e.g. registered nurse, physician, phlebotomist, administration, etc.). We also asked about patient contact, exposure to procedures, place of work (including home) and self-reported COVID-19 infection. A total of 19 categorizations of occupational roles were included and can be viewed in Supplemental Table 1. For the main analyses, we collapsed occupations into four categories of registered nurse, physician, administrative roles, or other healthcare workers.
Burnout was measured using the Oldenburg Burnout Inventory (OLBI), a validated 16–item inventory which measures two core dimensions of burnout: exhaustion and disengagement (from work) (43) and has strong validity and reliability among English-speaking workers in the United States (44). Responses to OLBI items range from 1 (totally disagree) to 4 (totally agree), and total scores range from 16 to 64. Consistent with work by Peterson et al. (45) we dichotomized burnout for descriptive analyses such that participants who had an average disengagement score of 2.1 or greater and an average exhaustion score of 2.25 or greater, were classified as having burnout. For our multivariable linear regression analysis, the OLBI score was kept continuous.
We utilized several measures from the Patient-Reported Outcomes Measurement Information System (PROMIS) computer adaptive tests (CAT) for measurement of psychological health, including anxiety, depression, positive affect, and meaning and purpose measures (46–49). All of the selected PROMIS psychological measures are examined as T-scores (M = 50, SD = 10) of the general population (50). We utilized cut points (e.g. high, average, low, etc.) to interpret the clinical significance of T-scores. For the PROMIS depression and anxiety measures, the cut points for normal limits of anxiety or depression are T-score values below 55, mild from 55 to 60, moderate from 60 to 70, and severe above 70. For PROMIS positive affect and meaning and purpose, T-score value cut points for very high scores greater than 70, high from 60 to 70, average from 40 to 60, low from 30 to 50, and very low with values less than 30. See Supplemental Figure 2 for interpretation of these measures. For all PROMIS measures, 3 T-score units can be interpreted as a meaningful difference in T-score values (51, 52).
We completed univariate analyses of all study data, including indices of central tendency (mean, median, 95% CI, etc.). T-tests for comparison of mean values of continuous demographic and health characteristics and chi-squared tests for comparisons of proportions for categorical characteristics were used to assess burnout as a dichotomous variable for descriptive analysis and to guide selection of covariates for our linear regression model. For the main analysis, OLBI scores were analyzed as a continuous outcome measure in a multivariable linear regression model to assess the association between depression, anxiety, positive affect, and meaning and purpose on burnout with selected covariates so that our analysis was sufficiently powered. Variables were included in the model based on the literature or significance at the p < 0.05 level in unadjusted analyses. The most parsimonious model was selected and reported. Moreover, respondents to the psychological health and burnout survey were compared to non-respondents among the 3,538 participants, to determine whether there were any significant differences in demographic characteristics and occupation. All analyses were conducted using Stata/IC (StataCorp) version 15 (53).
This study was approved by the Northwestern University Review board (STU00212515) prior to recruitment of HCWs, and all participants provided written informed consent at study enrollment.
A total of 2,619 of 3,538 (74%) individuals in the cohort study responded to the online survey, with 19 of respondents missing baseline data (e.g. age, gender, and occupation). Compared to non-respondents, survey respondents were significantly older, and more likely to identify as female sex and White race. Survey respondents also were significantly more likely to work in administrative roles and less likely to work as a physician or registered nurse. After removing participants who had missing data on burnout and key independent variables (e.g. age, gender, and PROMIS measures), a total of 2,411 participants were included in the current analyses (data flow diagram in Supplemental Figure 1). Table 1 contains demographic and work-related characteristics of the sample. The majority (n = 1,950, 80.88%) of HCWs in this study identified as White, Non-Hispanic race, and female sex (n = 1,986, 82.37%), and roughly one third (n = 747, 30.98%) were between ages 30–39 years old. Registered nurses (n = 650, 26.96%) accounted for the largest single occupation of HCWs, followed by physicians (n = 431, 17.88%) and administrators (n = 416, 17.25%). The mean score of burnout as measured by the OLBI was 36.87 (SD = 7.65), with 53.38% participants classified as having burnout based on cutoff scores. The highest proportion of HCWs with burnout were registered nurses (63.54%), followed by physicians (53.60%) and other healthcare occupations (53.28%). The proportion of HCWs experiencing burnout also varied by age, sex, and self-reported COVID-19 infection and exposure (Table 1). For instance, a significantly greater proportion of HCWs reported burnout identified as female sex (n = 1,098, 55.29%, p < 0.001) than those who identified as male sex (n = 189, 44.47%). Further, 71% (n = 251) of HCWs ages 18–29 years old were classified as having burnout, and the proportion of HCWs with burnout were significantly lower among 50–59 years-old (n = 203, 42.74%) and HCWs ages 60 and above (n = 73, 28.63%, p < 0.001). HCWs within single-person households also demonstrated the highest proportion of burnout (60.73%), with fewer individuals reporting burnout among two or more person households. Individuals with self-reported history of COVID-19 infection (n = 207, 58.81%) were significantly more likely to report burnout than those who did not report any history of COVID-19 infection (n = 1,080, 52.45%, p < 0.001).
A total of 359 respondents (14.89%) had a PROMIS-depression score more than one standard deviation above the mean, as well as 346 (14.35%) for the PROMIS-anxiety. Additionally, 14.35% (n = 346) of respondents scored one standard deviation below the mean for the PROMIS-positive affect, and 16.47% (n = 397) scored a standard deviation below the mean for the PROMIS-meaning and purpose score (see Supplemental Figure 2 for PROMIS measure distributions and cut-point descriptions).
In our multivariable linear regression model (Table 2) higher depression (coef = 0.15, SE= 0.03, p < 0.001) anxiety (coef = 0.25, SE = 0.02, p < 0.001) and lower positive affect (coef = −0.19, SE = 0.02, p < 0.001) and meaning and purpose (coef = −0.12, SE= 0.01, p < 0.001) scores were significantly associated with increased burnout scores. In addition, HCWs ages 60 years or older had lower burnout scores (coef = −3.25, SE = 0.46, p < 0.001) compared to individuals who were 18-29 years old; registered nurses (coef = 2.37, SE = 0.38, p < 0.001) and physicians (coef = 1.46, SE = 0.43, p = 0.001) reported greater burnout scores than individuals with administrative roles; and female respondents (coef = 1.07, SE = 0.25, p < 0.001) reported greater burnout scores than males. We also completed a logistic regression analysis which did not find any difference in factors associated with burnout as a dichotomous outcome (see Supplemental Table 1). Each unit increase in positive affect was associated with a 6% decrease in reported burnout (OR: 0.94, SE: 0.01, p < 0.001), and each increase in meaning and purpose was associated with a 5% decrease in burnout (OR: 0.95, SE: 0.01, p < 0.01).
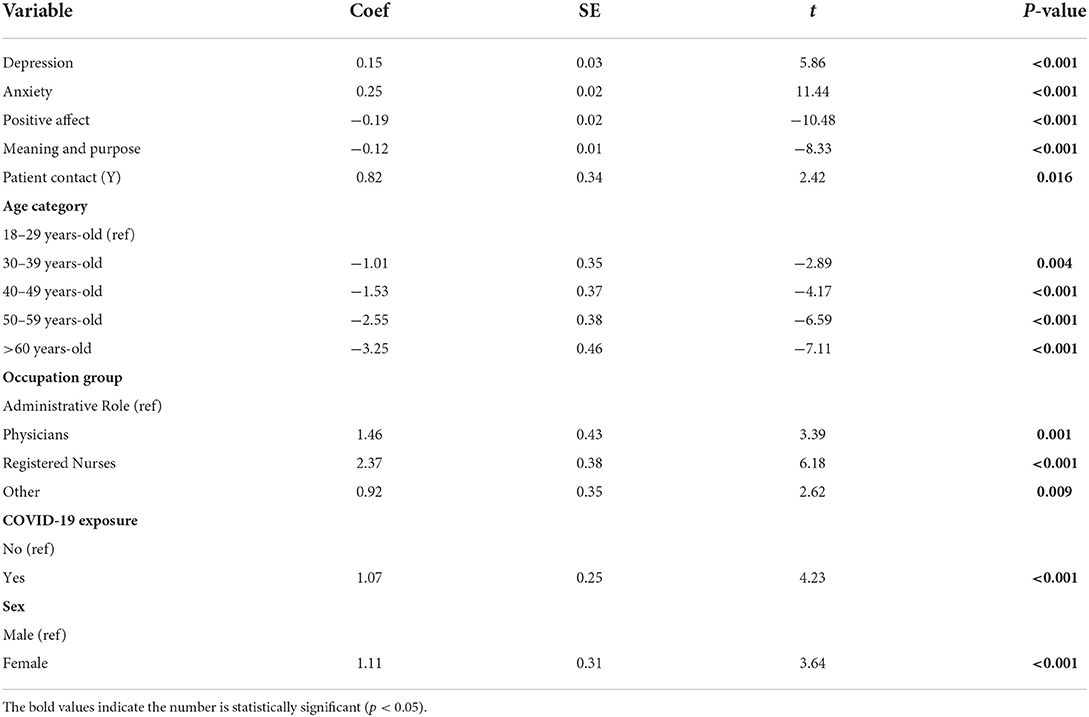
Table 2. Multivariable linear regression analyses of the association between psychological measures and burnout (OLBI) adjusted for demographic characteristics, occupational group, and COVID infection history (n = 2,411).
We found that among a cohort of HCWs who had been working since prior to the COVID-19 pandemic, higher scores on depression and anxiety were significantly associated with higher burnout. In contrast, positive affect and meaning and purpose were inversely associated with burnout scores. These statistically significant associations were stable even with the adjustment for other independent factors associated with burnout in our cohort (including age, female sex, occupational role, and patient contact, and COVID-19 exposure). We noted that burnout was prevalent (53.38%) in this cohort of HCWs at the time of data collection. Our findings also highlight the intersections of age, occupation, and sex in experienced depression, anxiety, positive affect, and meaning and purpose in association with burnout, with individuals with lower age, female sex, and occupational role as a physician or nurse with greater burnout.
Numerous studies have characterized the extent of burnout amid the COVID-19 pandemic and factors associated with higher rates of burnout. Our findings indicated that half of our participants were classified as having burnout as measured by the OLBI, (45) consistent with other estimates of burnout during the pandemic (54–57). For instance, Denning et al. (56) noted that 67% of HCWs in United Kingdom, Poland, and Singapore reported burnout based on the OLBI. Other studies reported even higher levels of burnout in HCWs, ranging from 75 to 79% (55, 57). These higher rates may be due to slightly different definitions of burnout or measurement at different points in the pandemic. Our findings are also consistent with other studies in that demographic and work characteristics associated with higher burnout scores included female sex (54), being a nurse, physician, or other patient-facing occupational role (56).
Our findings demonstrate that HCWs reported symptoms of depression and anxiety during the COVID-19 pandemic. This is not surprising as other studies have reported high rates of significant psychological distress by HCWs during the COVID-19 pandemic (11, 58–64). A meta-review of 40 systematic reviews of studies of HCWs during the pandemic found that depression and anxiety were the most prevalent mental health conditions (61). In concordance with our findings, another rapid review of the psychological impact to HCWs amid the COVID-19 pandemic noted that nurses who identified as female with contact to COVID-19 patients had the highest prevalence of mental health problems (65). Notably, given that surges in COVID-19 cases are mirrored with increased levels of burnout (66), the data collection period of our study may have led to lower reports of symptoms of depression, anxiety, and burnout in our sample, given the relative lull in COVID-19 cases occurring during that period.
We found a significant inverse association of positive affect and meaning and purpose with burnout in our cohort. Several studies, some completed before the pandemic, had similar findings. For example, one study of social workers in China in May 2021 found that positive affect was inversely associated with psychological distress, while negative affect was associated with higher with psychological distress (38). A study of primary care physicians in Spain conducted in 2013 found that positive affect mediated the relationship between lower resilience, lack of development, and burnout (67). Similarly, Barnett et al. observed that meaning and purpose was significantly inversely associated with burnout prior to the COVID-19 pandemic (37). One study also conducted prior to COVID-19 examining psychological well-being among HCWs noted that nurses, who were overwhelmingly female, reported significantly lower positive affect than other healthcare professionals (68). Similar studies have not been conducted during the COVID-19 pandemic. To our knowledge, our study is the first to report the associations of positive affect and meaning and purpose with burnout scores among a large cohort of multidisciplinary HCWs during the COVID-19 pandemic. While interventions exist to increase positive affect (31, 32, 69–71), researchers have yet to assess the efficacy, feasibility, and acceptability of these targeted interventions among HCWs.
This study has several limitations. First, our study participants largely identified as White race and female sex, and worked as registered nurses, physicians, or administrators, which may limit the generalizability of our findings to HCWs who are non-White, male sex or gender-non-binary, or work in other healthcare roles including staff with patient contact (e.g. custodial staff, nursing assistants, security, etc.). Further, despite high burnout reported among individuals within single person households, we did not include household size in our regression models due to high missingness of data for this variable in our sample. More research is needed to focus on the specific experiences with burnout and psychological wellbeing for these HCWs. The initial recruitment strategies for this cohort study included a focus on COVID-19 testing at the time of data collection, which may have also biased this sample towards HCWs who require in-person work associated with their role. We also utilized online recruitment and survey methods for data collection, which may have limited our ability to reach some HCWs for recruitment and engagement in this study. Of note, our utilization of PROMIS measures has limited our ability to determine clinically significant differences in psychological health and burnout, as PROMIS measures are not diagnostic tools for psychological well-being (52). Further, our analysis was conducted utilizing cross-sectional data, which precludes any ability to determine causality and directionality in the associations between psychological health and burnout. Future studies are needed to examine causal mechanisms of burnout associated with clinically meaningful differences in psychological health, as well as examinations of effective interventions to reduce burnout among HCWs.
In conclusion, the prevalence of burnout, depression, and anxiety were high among HCWs during the 2nd year of the COVID-19 pandemic. However, positive affect and meaning and purpose were associated with lower levels of burnout. As we have noted in our findings, individuals who are younger, identify as female, and work in patient-facing occupational roles (e.g. RNs, MDs) were associated with higher rates of increased burnout in this study and would benefit from targeted interventions to promote resilience in these populations. Future research is needed to examine the association of specific domains of burnout- including exhaustion and disengagement- with depression, anxiety, meaning and purpose, and positive affect. Individual-level and systems-level interventional studies are needed to develop evidence-based interventions, potentially through increasing positive affect and sense of purpose, to reduce burnout and increase the resiliency and psychological wellbeing of the HCWs who are critical to providing health care before, during, and after current and future pandemics.
Data are available on reasonable request from the principle investigator CE, Y2hhcmxlc25pa2EtZXZhbnNAbm9ydGh3ZXN0ZXJuLmVkdQ== and if in accordance with institutional guidelines.
The studies involving human participants were reviewed and approved by Northwestern University Institutional Review Board (IRB). The patients/participants provided their written informed consent to participate in this study.
JB, LH, CE, and JM contributed to conception and design of the study. JB organized the database and performed the statistical analysis with mentorship from TV. JB wrote the first draft of the manuscript. JB, MF, CL, and JM wrote sections of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
This work was supported by the Northwestern University Clinical and Translational Sciences Institute (UL1TR001422), the Northwestern Memorial Foundation and a grant from the Peter G. Peterson Foundation Grant.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frhs.2022.994474/full#supplementary-material
1. Leo CG, Sabina S, Tumolo MR, Bodini A, Ponzini G, Sabato E, et al. Burnout Among healthcare workers in the COVID 19 era: a review of the existing literature. Front Public Health. (2021) 9:1–6. doi: 10.3389/fpubh.2021.750529
2. Sullivan D, Sullivan V, Weatherspoon D, Frazer C. Comparison of nurse burnout, before and during the COVID-19 pandemic. Nurs Clin North Am. (2022) 57:79–99. doi: 10.1016/j.cnur.2021.11.006
3. McHugh MD, Kutney-Lee A, Cimiotti JP, Sloane DM, Aiken LH. Nurses' widespread job dissatisfaction, burnout, and frustration with health benefits signal problems for patient care. Health Affairs. (2011) 30:202–10. doi: 10.1377/hlthaff.2010.0100
4. Aiken LH, Sermeus W, Van den Heede K, Sloane DM, Busse R, McKee M, et al. Patient safety, satisfaction, and quality of hospital care: cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. BMJ. (2012) 344:e1717. doi: 10.1136/bmj.e1717
5. Maslach C, Jackson SE. The measurement of experienced burnout. J Organ Behav. (1981) 2:99–113. doi: 10.1002/job.4030020205
6. Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory. Lanham, MD: Scarecrow Education (1997).
7. Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. (2001) 52:397–422. doi: 10.1146/annurev.psych.52.1.397
8. Dolan N. The relationship between burnout and job satisfaction in nurses. J Adv Nurs. (1987) 12:3–12. doi: 10.1111/j.1365-2648.1987.tb01297.x
9. Hakanen JJ, Schaufeli WB. Do burnout and work engagement predict depressive symptoms and life satisfaction? A three-wave seven-year prospective study. J Affect Disord. (2012) 141:415–24. doi: 10.1016/j.jad.2012.02.043
10. Shanafelt TD, Balch CM, Dyrbye L, Bechamps G, Russell T, Satele D, et al. Special report: suicidal ideation among American surgeons. Arch Surgery. (2011) 146:54–62. doi: 10.1001/archsurg.2010.292
11. Melnyk BM, Hsieh AP, Tan A, Teall AM, Weberg D, Jun J, et al. Associations among nurses' mental/physical health, lifestyle behaviors, shift length, and workplace wellness support during COVID-19: important implications for health care systems. Nurs Adm Q. (2022) 46:5–18. doi: 10.1097/NAQ.0000000000000499
12. Tawfik DS, Scheid A, Profit J, Shanafelt T, Trockel M, Adair KC, et al. Evidence relating health care provider burnout and quality of care: a systematic review and meta-analysis. Ann Int Med. (2019) 171:555–67. doi: 10.7326/M19-1152
13. Parker PA, Kulik JA. Burnout, self- and supervisor-rated job performance, and absenteeism among nurses. J Behav Med. (1995) 18:581–99. doi: 10.1007/BF01857897
14. Shanafelt TD, Bradley KA, Wipf JE, Back AL. Burnout and self-reported patient care in an internal medicine residency program. Ann Int Med. (2002) 136:358–67. doi: 10.7326/0003-4819-136-5-200203050-00008
15. Peterson U, Bergström G, Demerouti E, Gustavsson P, Asberg M, Nygren A. Burnout levels and self-rated health prospectively predict future long-term sickness absence: a study among female health professionals. J Occup Environ Med. (2011) 53:788–93. doi: 10.1097/JOM.0b013e318222b1dc
16. Luceño-Moreno L, Talavera-Velasco B, Vázquez-Estévez D, Martín-García J. Mental health, burnout, and resilience in healthcare professionals after the first wave of COVID-19 pandemic in Spain: a longitudinal study. J Occup Environ Med. (2022) 64:e114–e23. doi: 10.1097/JOM.0000000000002464
17. Dobson H, Malpas CB, Burrell AJ, Gurvich C, Chen L, Kulkarni J, et al. Burnout and psychological distress amongst Australian healthcare workers during the COVID-19 pandemic. Australas Psychiatry. (2021) 29:26–30. doi: 10.1177/1039856220965045
18. Card AJ. Burnout and sources of stress among health care risk managers and patient safety personnel during the COVID-19 pandemic: a pilot study. Disaster Med Public Health Prep. (2021) 1–3. doi: 10.1017/dmp.2021.120
19. Hao Q, Wang D, Xie M, Tang Y, Dou Y, Zhu L, et al. Prevalence and risk factors of mental health problems among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Front Psychiatry. (2021) 12:567381. doi: 10.3389/fpsyt.2021.567381
20. Bahamdan AS. Review of the psychological impact of COVID-19 pandemic on healthcare workers in Saudi Arabia. Risk Manag Healthc Policy. (2021) 14:4105–11. doi: 10.2147/RMHP.S324938
21. Bekele F, Mechessa DF, Sefera B. Prevalence and associated factors of the psychological impact of COVID-19 among communities, health care workers and patients in Ethiopia: a systematic review. Ann Med Surgery. (2021) 66:102403. doi: 10.1016/j.amsu.2021.102403
22. Benfante A, Di Tella M, Romeo A, Castelli L. Traumatic stress in healthcare workers during COVID-19 pandemic: a review of the immediate impact. Front Psychol. (2020) 11:569935. doi: 10.3389/fpsyg.2020.569935
23. Serrano-Ripoll MJ, Zamanillo-Campos R, Castro A. Fiol-de Roque MA, Ricci-Cabello I. Insomnia and sleep quality in healthcare workers fighting against COVID-19: a systematic review of the literature and meta-analysis. Actas Espanolas de Psiquiatria. (2021) 49:155–79.
24. Marvaldi M, Mallet J, Dubertret C, Moro MR, Guessoum SB. Anxiety, depression, trauma-related, and sleep disorders among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Neurosci Biobehav Rev. (2021) 126:252–64. doi: 10.1016/j.neubiorev.2021.03.024
25. Fillion L, Duval S, Dumont S, Gagnon P, Tremblay I, Bairati I, et al. Impact of a meaning-centered intervention on job satisfaction and on quality of life among palliative care nurses. Psycho Oncol J Psychol Soc Behav Dimen Cancer. (2009) 18:1300–10. doi: 10.1002/pon.1513
26. Harding R, Higginson IJ. What is the best way to help caregivers in cancer and palliative care? A systematic literature review of interventions and their effectiveness. Palliative Med. (2003) 17:63–74. doi: 10.1191/0269216303pm667oa
27. Potter P, Deshields T, Rodriguez S. Developing a systemic program for compassion fatigue. Nurs Adm Q. (2013) 37:326–32. doi: 10.1097/NAQ.0b013e3182a2f9dd
28. Holmes EA, O'Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. (2020) 7:547–60. doi: 10.1016/S2215-0366(20)30168-1
29. Folkman S. Positive psychological states and coping with severe stress. Soc Sci Med. (1997) 45:1207–21. doi: 10.1016/S0277-9536(97)00040-3
30. Folkman S, Moskowitz JT. Positive affect and the other side of coping. Am Psychol. (2000) 55:647. doi: 10.1037/0003-066X.55.6.647
31. Moskowitz JT, Carrico AW, Duncan LG, Cohn MA, Cheung EO, Batchelder A, et al. Randomized controlled trial of a positive affect intervention for people newly diagnosed with HIV. J Consult Clin Psychol. (2017) 85:409. doi: 10.1037/ccp0000188
32. Moskowitz JT, Cheung EO, Snowberg KE, Verstaen A, Merrilees J, Salsman JM, et al. Randomized controlled trial of a facilitated online positive emotion regulation intervention for dementia caregivers. Health Psychol. (2019) 38:391–402. doi: 10.1037/hea0000680
33. Waterman AS. Two conceptions of happiness: Contrasts of personal expressiveness (eudaimonia) and hedonic enjoyment. J Pers Soc Psychol. (1993) 64:678. doi: 10.1037/0022-3514.64.4.678
35. Ryan RM, Deci EL. On happiness and human potentials: a review of research on hedonic and eudaimonic wellbeing. Ann Rev Psychol. (2001) 52:141–66. doi: 10.1146/annurev.psych.52.1.141
36. Javadi Sharif T, Hosseinzadeh M, Mahdavi N, Namdar Areshtanab H. G LD. Happiness and its relationship with job burnout in nurses of educational hospitals in Tabriz, Iran. Inl J Commun Based Nurs Midwifery. (2020) 8:295–304. doi: 10.30476/IJCBNM.2020.83298.1138
37. Barnett MD, Moore JM, Garza CJ. Meaning in life and self-esteem help hospice nurses withstand prolonged exposure to death. J Nurs Manag. (2019) 27:775–80. doi: 10.1111/jonm.12737
38. Huang C, Xie X, Cheung SP, Zhou Y. Job demands and resources, positive and negative affect, and psychological distress of social workers in China. Front Psychiatry. (2021) 12:752382. doi: 10.3389/fpsyt.2021.752382
39. Service PH editor. Addressing Health Worker Burnout: The U.S. Surgeon General's Advisory on Building a Thriving Health Workforce. U.S. Department of Health and Human Services PHS, Office of the Surgeon General (2022).
40. Evans CT, DeYoung BJ, Gray EL, Wallia A, Ho J, Carnethon M, et al. COVID-19 vaccine intentions and uptake in a tertiary care healthcare system: a longitudinal study. Infect Control Hospital Epidemiol. (2021) 1–19. doi: 10.1017/ice.2021.523
41. Wilkins JT, Gray EL, Wallia A, Hirschhorn LR, Zembower TR, Ho J, et al. editors. “Seroprevalence and correlates of SARS-CoV-2 antibodies in health care workers in Chicago”. In: Open forum Infectious Diseases. Cary, NC: Oxford University Press (2021). doi: 10.1101/2020.09.11.20192385
42. Wilkins JT, Hirschhorn LR, Gray EL, Wallia A, Carnethon M, Zembower TR, et al. Serologic status and SARS-CoV-2 infection over 6 months of follow up in healthcare workers in Chicago: a cohort study. Infect Control Hospital Epidemiol. (2021) 43:1–9. doi: 10.1017/ice.2021.367
43. Demerouti E, Bakker AB, Vardakou I, Kantas A. The convergent validity of two burnout instruments: a multitrait-multimethod analysis. Eur J Psychol Assess. (2003) 19:12. doi: 10.1027//1015-5759.19.1.12
44. Halbesleben JR, Demerouti E. The construct validity of an alternative measure of burnout: investigating the English translation of the Oldenburg Burnout inventory. Work and Stress. (2005) 19:208–20. doi: 10.1080/02678370500340728
45. Peterson U, Demerouti E, Bergström G, Samuelsson M, Åsberg M, Nygren Å. Burnout and physical and mental health among Swedish healthcare workers. J Adv Nurs. (2008) 62:84–95. doi: 10.1111/j.1365-2648.2007.04580.x
46. Hahn EA, DeWalt DA, Bode RK, Garcia SF, DeVellis RF, Correia H, et al. New English and Spanish social health measures will facilitate evaluating health determinants. Health Psychol. (2014) 33:490. doi: 10.1037/hea0000055
47. Salsman JM, Lai JS, Hendrie HC, Butt Z, Zill N, Pilkonis PA, et al. Assessing psychological wellbeing: self-report instruments for the NIH toolbox. Qual Life Res. (2014) 23:205–15. doi: 10.1007/s11136-013-0452-3
48. Pilkonis PA, Choi SW, Reise SP, Stover AM, Riley WT, Cella D, et al. Item banks for measuring emotional distress from the patient-reported outcomes measurement information system (PROMIS®): depression, anxiety, and anger. Assessment. (2011) 18:263–83. doi: 10.1177/1073191111411667
49. Pilkonis PA Yu L, Dodds NE, Johnston KL, Maihoefer CC, Lawrence SM. Validation of the depression item bank from the patient-reported outcomes measurement information system (PROMIS®) in a three-month observational study. J Psychiatr Res. (2014) 56:112–9. doi: 10.1016/j.jpsychires.2014.05.010
50. PROMIS. (n.d.). Available online at: https://www.healthmeasures.net/score-and-interpret/interpret-scores/promis (accessed May 1, 2022).
51. PROMIS Score Cut Points. (n.d.). Available online at: https://www.healthmeasures.net/score-and-interpret/interpret-scores/promis/promis-score-cut-points (accessed May 1, 2022).
52. Meaningful Change for PROMIS (n,.d.). Available online at: https://www.healthmeasures.net/score-and-interpret/interpret-scores/promis/meaningful-change (accessed May 1, 2022).
54. Moll V, Meissen H, Pappas S, Xu K, Rimawi R, Buchman TG, et al. The coronavirus disease 2019 pandemic impacts burnout syndrome differently among multiprofessional critical care clinicians-a longitudinal survey study. Crit Care Med. (2022) 50:440–8. doi: 10.1097/CCM.0000000000005265
55. Sheehan O, Sheehan M, Rau RI, Sullivan IO, McMahon G, Payne A. Burnout on the frontline: the impact of COVID-19 on emergency department staff wellbeing. Irish J Med Sci. (2021) 191:1–9. doi: 10.1007/s11845-021-02795-w
56. Denning M, Goh ET, Tan B, Kanneganti A, Almonte M, Scott A, et al. Determinants of burnout and other aspects of psychological well-being in healthcare workers during the Covid-19 pandemic: a multinational cross-sectional study. PLoS ONE. (2021) 16:e0238666. doi: 10.1371/journal.pone.0238666
57. Tan BYQ, Kanneganti A, Lim LJH, Tan M, Chua YX, Tan L, et al. Burnout and associated factors among health care workers in Singapore during the COVID-19 pandemic. J Am Med Direct Assoc. (2020) 21:1751–8. doi: 10.1016/j.jamda.2020.09.035
58. Rose S, Hartnett J, Pillai S. A comprehensive dataset describing nurse's emotions, perceived stressors and coping mechanisms during the first surge of the COVID-19 pandemic. Data Brief. (2022) 40:107814. doi: 10.1016/j.dib.2022.107814
59. Peccoralo LA, Pietrzak RH, Feingold JH, Syed S, Chan CC, Murrough JW, et al. A prospective cohort study of the psychological consequences of the COVID-19 pandemic on frontline healthcare workers in New York City. Int Arch Occup Environ Health. (2022) 95:1–13. doi: 10.1007/s00420-022-01832-0
60. Yu B, Barnett D, Menon V, Rabiee L, De Castro YS, Kasubhai M, et al. Healthcare worker trauma and related mental health outcomes during the COVID-19 outbreak in New York City. PLoS ONE. (2022) 17:e0267315. doi: 10.1371/journal.pone.0267315
61. Chutiyami M, Cheong AMY, Salihu D, Bello UM, Ndwiga D, Maharaj R, et al. COVID-19 pandemic and overall mental health of healthcare professionals globally: a meta-review of systematic reviews. Front Psychiatry. (2021) 12:804525. doi: 10.3389/fpsyt.2021.804525
62. Xiong N, Fritzsche K, Pan Y, Löhlein J, Leonhart R. The psychological impact of COVID-19 on Chinese healthcare workers: a systematic review and meta-analysis. Soc Psychiatry Psychiatric Epidemiol. (2022) 57:1–15. doi: 10.1007/s00127-022-02264-4
63. Vizheh M, Qorbani M, Arzaghi SM, Muhidin S, Javanmard Z, Esmaeili M. The mental health of healthcare workers in the COVID-19 pandemic: a systematic review. J Diabetes Metab Disord. (2020) 19:1–12. doi: 10.1007/s40200-020-00643-9
64. Maunder RG, Heeney ND, Kiss A, Hunter JJ, Jeffs LP, Ginty L, et al. Psychological impact of the COVID-19 pandemic on hospital workers over time: relationship to occupational role, living with children and elders, and modifiable factors. Gen Hosp Psychiatry. (2021) 71:88–94. doi: 10.1016/j.genhosppsych.2021.04.012
65. Cabarkapa S, Nadjidai SE, Murgier J, Ng CH. The psychological impact of COVID-19 and other viral epidemics on frontline healthcare workers and ways to address it: a rapid systematic review. Brain Behav Immun Health. (2020) 8:100144. doi: 10.1016/j.bbih.2020.100144
66. Melnikow J, Padovani A, Miller M. Frontline physician burnout during the COVID-19 pandemic: national survey findings. BMC Health Serv Res. (2022) 22:365. doi: 10.1186/s12913-022-07728-6
67. Montero-Marin J, Tops M, Manzanera R, Piva Demarzo MM, Álvarez de. Mon M, García-Campayo J. Mindfulness, resilience, and burnout subtypes in primary care physicians: the possible mediating role of positive and negative affect. Front Psychol. (2015) 6:1895. doi: 10.3389/fpsyg.2015.01895
68. Atanes AC, Andreoni S, Hirayama MS, Montero-Marin J, Barros VV, Ronzani TM, et al. Mindfulness, perceived stress, and subjective well-being: a correlational study in primary care health professionals. BMC Compl Altern Med. (2015) 15:303. doi: 10.1186/s12906-015-0823-0
69. Addington EL, Cheung EO, Bassett SM, Kwok I, Schuette SA, Shiu E, et al. The MARIGOLD study: feasibility and enhancement of an online intervention to improve emotion regulation in people with elevated depressive symptoms. J Affect Disord. (2019) 257:352–64. doi: 10.1016/j.jad.2019.07.049
70. Bassett S, Cohn M, Cotten P, Kwok I, Moskowitz J. Feasibility and acceptability of an online positive affect intervention for those living with comorbid HIV depression. AIDS Behav. (2019) 23:753–64. doi: 10.1007/s10461-019-02412-z
Keywords: healthcare worker (HCW), burnout—professional, positive psychology, depression, anxiety, cohort study
Citation: Bannon J, Evans CT, Freedman M, Lee C, Vu TH, Wallia A, Wilkins JT, Moskowitz JT and Hirschhorn LR (2022) Psychological wellbeing and the association with burnout in a cohort of healthcare workers during the COVID-19 pandemic. Front. Health Serv. 2:994474. doi: 10.3389/frhs.2022.994474
Received: 14 July 2022; Accepted: 27 September 2022;
Published: 25 October 2022.
Edited by:
Gerard Leavey, Ulster University, United KingdomReviewed by:
Finola Ferry, Ulster University, United KingdomCopyright © 2022 Bannon, Evans, Freedman, Lee, Vu, Wallia, Wilkins, Moskowitz and Hirschhorn. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jacqueline Bannon, amFjcXVlbGluZS5iYW5ub25Abm0ub3Jn
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.