
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Rehabil. Sci., 12 February 2025
Sec. Rehabilitation for Musculoskeletal Conditions
Volume 6 - 2025 | https://doi.org/10.3389/fresc.2025.1513442
Dental professionals (DPs) are at significant risk of developing work-related musculoskeletal disorders (WMSDs). This study aimed to determine the prevalence of WMSDs among DPs and identify associated factors based on professional level. A cross-sectional analysis was conducted on 151 dental professionals, including dentists, dental nurses, and dental assistants, from various universities and health institutes in Indonesia. Data were collected using the Nordic Musculoskeletal Questionnaire. Associations between WMSD symptoms and qualitative data (demographics, job characteristics, and other factors) were examined using the Chi-square test, while quantitative data were analyzed using the independent t-test. The results showed that 96% of respondents (145 out of 151) had experienced WMSDs, with the back (68.2%), waist (66.9%), upper neck (60.9%), and lower neck (59.6%) being the most commonly affected regions. Muscle fatigue (53.6%) and pain (49.7%) were the most frequently reported symptoms. Triggering factors included unergonomic body posture (84.1%) and prolonged sitting (53.6%), while protective factors included rest (71.5%) and improved body posture (53%). Physical exercise was significantly associated with WMSDs (p < 0.001). This study highlights the high prevalence of WMSDs among dental professionals and underscores the need for ergonomic training, physical exercise, and equipment modification to mitigate these conditions. Limitations of the study include unequal distribution among professional groups and a gender imbalance, which may affect the generalisability of the findings.
Work-related musculoskeletal disorders (WMSDs) are a common type of work-related illness, accounting for approximately 48% of all cases (1). WMSDs can cause work-related disabilities, reducing productivity and increasing costs (1, 2). WMSDs are a type of multifactorial alteration of muscles and tendons due to repetitive movements and physical tension in the limbs while working caused by the position or movement involved (2). Work-related musculoskeletal disorders (WMSDs) refer to injuries affecting the human support system, such as bones, cartilage, muscles, ligaments, tendons, blood vessels, or nerves. These injuries are primarily caused or worsened by work tasks and the working environment (3–6). Musculoskeletal disorders are classified as work-related when both the working environment and the performance of work significantly contribute to the condition, exacerbate it, or prolong its duration (7).
Health workers, particularly dentists, nurses, doctors, and surgeons, are more susceptible to developing WMSDs. In dentistry, many WMSDs are linked to cumulative trauma, often manifesting as repetitive strain injuries. Studies have shown that dentists are prone to work-related musculoskeletal complaints, with pain being the most common complaint, affecting the neck the most (8–16). Common examples of work conditions that can lead to WMSDs include lifting heavy objects regularly, being exposed to whole-body vibration daily, performing overhead work routinely, working with the neck in a constantly flexed position, or engaging in repetitive forceful tasks (7). Dental practitioners are at risk for repetitive strain injuries due to activities such as gripping and using slender instruments repetitively (e.g., for plaque removal and cavity preparation) and using vibratory instruments like handpieces and ultrasonic scalers (17, 18). The nature of dental work also contributes to WMSD risks, as practitioners frequently sustain awkward postures and non-neutral wrist positions.
A cross-sectional study of 536 dentists in India conducted by Kumar et al. (12) found that all respondents had work-related musculoskeletal complaints, with pain being the most common complaint (99.06%). The neck was the most frequently affected body part. Similarly, Phedy et al. (14) found that 63.5% of 241 Indonesian dentists reported musculoskeletal complaints. Prolonged static postures, repetitive movements, and awkward body positions during patient care are the primary risk factors for developing musculoskeletal disorders (11, 16).
Musculoskeletal disorders can adversely affect patient care quality and work productivity and increase work absence. Therefore, it is crucial to understand musculoskeletal disorders in DPs and develop effective prevention strategies to improve their health and work productivity (11, 12, 19, 20). This research aimed to investigate the prevalence of WMSDs in DPs, comprising dentists, dental nurses, and dental assistants, and to identify the associated factors for WMSD based on professional level.
This research was a cross-sectional study conducted from December 2023 to March 2024. The study collected data on potential risk factors (e.g., demographic information, BMI, exercise frequency) as independent variables, also professional levels and job characteristics (type of profession, duration of working hours and overtime, work position) as possible mediators or moderators. To determine the appropriate sample size for the study, we used a power of 80%, a two-sided significance level of 0.05, and an anticipated difference in incidence rates of 10% (63.5% and 53.5%). The incidence rate of 63.5% was derived from a previous study by Phedy et al. (14). Based on these parameters, the study required a minimum of 25 patients in each group to meet the sample size requirement. The inclusion criteria are dentists, dental nurses, and dental assistants. The exclusion criteria are dentists, dental nurses, and dental assistants with a history of musculoskeletal surgery. The study was without a control arm. The Indonesian version of the Nordic Musculoskeletal Questionnaire was utilized (21, 22). The questionnaire consisted of 27 Likert scale items, to identify areas of the body that have caused musculoskeletal problems in the past 12 months. The musculoskeletal disorders evaluated in this study were pain, stiffness, fatigue, discomfort, “clicking” sounds from joints, and neurological symptoms such as tingling and numbness. We employed an independent t-test to examine the association between WMSD and factors such as gender, age, weekly working hours, overtime hours, and working position. To assess the correlation between musculoskeletal disorders and BMI, exercise frequency, educational level, and type of profession, we conducted a one-way ANOVA test. Statistical analysis was conducted using the SPSS version 29 software, with a p-value of <0.05 considered statistically significant.
The primary objective of this study was to develop a descriptive and inferential statistical framework to assess the relationship between risk factors (e.g., gender, age, weekly working hours, overtime hours, BMI, exercise frequency, educational level, and type of profession) and the prevalence of work-related musculoskeletal disorders (WMSDs) as binary outcomes. To address this objective, we conducted a cross-sectional study design without a control arm to explore associations and develop predictive insights.
In the unadjusted analyses, independent t-tests were used to examine the association between WMSDs and continuous variables such as gender, age, weekly working hours, overtime hours, and working position. Additionally, one-way ANOVA tests were conducted to evaluate the correlation between WMSDs and categorical variables such as BMI, exercise frequency, educational level, and type of profession.
For multivariable analysis, a backward elimination variable selection method was utilized to identify the most significant predictors of WMSDs. Interaction effects between variables, such as type of profession and working hours, were explored to determine potential effect modifications.
All statistical analyses were conducted using SPSS version 29 software, with a p-value of <0.05 considered statistically significant. Results were summarized as mean ± standard deviation (SD) or percentages for descriptive statistics, and p-values for inferential statistics. Additional sensitivity analyses were conducted to validate the findings from the primary analyses using alternative stratifications of professional level and exercise frequency.
This study included 151 dental health practitioners. Table 1 provides an overview of the respondents' characteristics. On average, respondents worked 29.7 h per week, with 56.9% having overtime hours, averaging 7.3 h per week. 73.5% of respondents mostly worked in a sitting position, and the remaining respondents worked in a standing position. Among the 151 respondents, 26.5% did not have an exercise habit, 28.5% exercised less than once a week, 31.8% exercised 1–2 times a week, 9.9% exercised 3–4 times a week, and the remaining respondents exercised more than four times a week. Of the 151 respondents, 145 experienced musculoskeletal disorders as described in Table 2. The Nordic musculoskeletal questionnaire indicates that the back (68.2%) and waist (66.9%) had the highest proportion of musculoskeletal disorders, followed by the upper neck (60.9%) and lower neck (59.6%). Fatigue (53.6%) and pain (49.7%) were the most common symptoms of musculoskeletal disorders (Figure 1). The study also found that unergonomic body posture when working (84.1%) and prolonged sitting (53.6%) were the most aggravating factors (Table 3). On the other hand, taking a short break (71.5%) and improving body posture (53%) were the most influential factors in alleviating musculoskeletal disorders (Table 4). Based on a professional level, dentists had the highest burden of experiencing WMSD, followed by dental nurses and dental assistants (Table 5). According to Table 6, only physical exercise significantly influenced WMSD (sig < 0.001) among dental health practitioners.
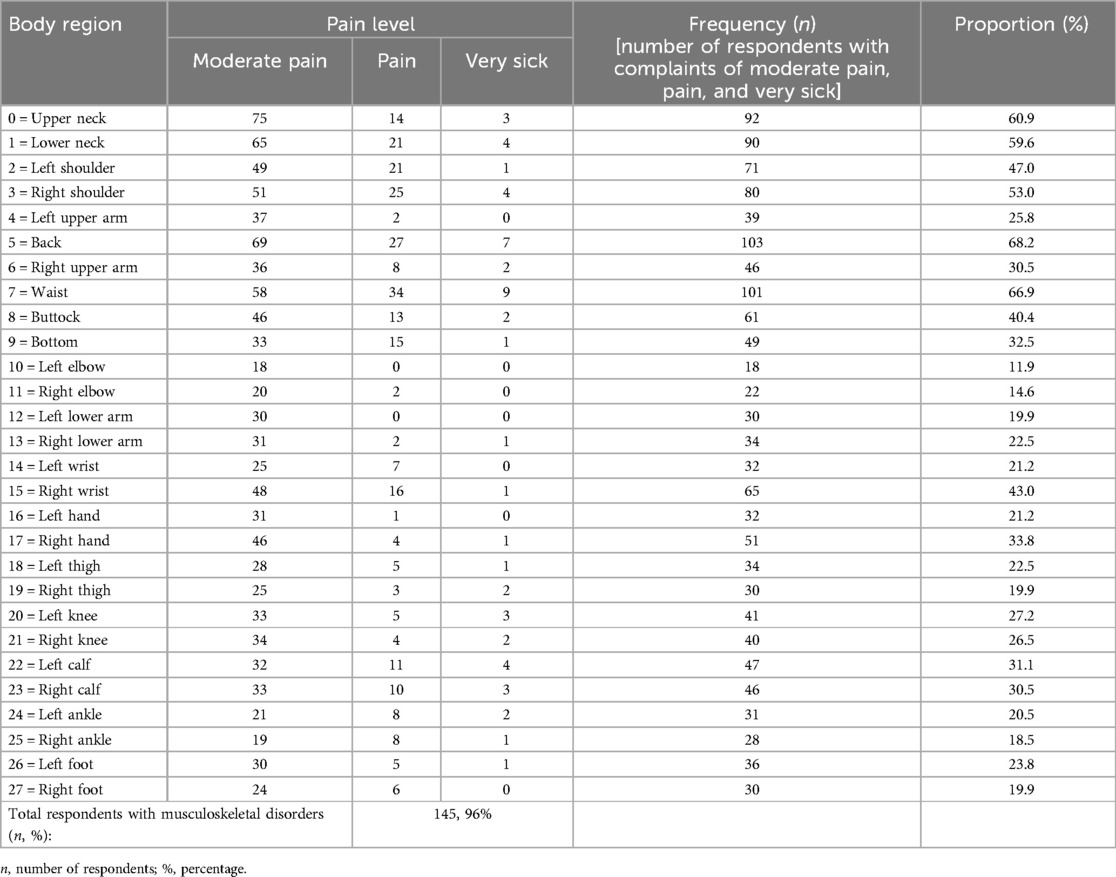
Table 2. Prevalence of musculoskeletal disorders (pain, stiffness, fatigue, discomfort, clicking, and neurological complaints) according to the nordic musculoskeletal questionnaire.
This study investigated the prevalence of work-related musculoskeletal disorders (WMSDs) among dentists, dental nurses, and dental assistants. Data were collected on potential risk factors, including demographic information, body mass index (BMI), and exercise frequency, which were analyzed as independent variables. Additionally, professional levels and job characteristics—such as type of profession, working hours, overtime, and work posture—were examined as potential mediators or moderators. The study revealed that 96% of respondents experienced WMSDs, which indicates that dental practitioners are vulnerable to WMSDs. This result also aligns with previous studies where DPs, which consisted of nurses, doctors, surgeons, and dental health workers, was considered vulnerable to WMSD (8–16).
This study found a higher prevalence rate of WMSDs among DPs than in previous studies. A study by Phedy et al. (14) found a WMSD prevalence rate of 63.5% among young dentists in Indonesia. The main difference between our study and theirs is that we included dentists, dental nurses, and dental assistants. Our study found a prevalence rate higher than that of several other countries, including 95% in Cameroon (23), 94% in a study of 120 dentists in Türkiye (24), 92% among 450 dentists and dental assistants in Germany (25), 87.2% in Australia (26), 86.5% in Lithuania (27), 85.6% in China (28), 81.4% in Brazil (29), 73.3% in India (30), 62% in Greece (31), 59.2% in Saudi Arabia (32), and 42% in the UK (33). The results of our study are consistent with a study in the Czech Republic, which found a WMSD prevalence rate of (34). These findings suggest that musculoskeletal disorders are relatively high and should not be underestimated by DPs.
Several previous studies stated that the body region most susceptible to WMSD was the neck, with pain being the most common symptom (10, 12, 15). A systematic review by AlOtaibi et al. (19) reported that the body regions with the highest prevalence of WMSD were the back (82.3%), neck (82.3%), shoulders (75.4%), and elbows/hands (30.8%). The current study shows that there were four regions with the highest proportion of musculoskeletal disorders, which were the back (68.2%) and waist (66.9%), followed by the upper neck (60.9%) and lower neck (59.6%). These areas are responsible for spinal overcapacity when working. Dental health practitioners often require a 15 to 20-degree forward bending movement, which causes muscular overload in the neck and cervical spine joints and causes contractures and pain in the neck (13). Prolonged static posture resulting from sustained muscle activity in the sternocleidomastoid or trapezius muscles may be a major etiological factor in neck pain among DPs (12, 13, 19). The repetitive stresses over a sustained period of time produce injury with load, causing creep deformation of the paraspinal muscle, possibly to the point of micro-failure (35).
In the lumbar region, musculoskeletal disorders were associated with the sitting working position in the majority of respondents (73.5%), which is in line with a study by Macrì et al. (13) which showed that dentists who mostly work in a sitting position, found the majority of pain in the lumbar and cervical regions. Incorrect sitting posture can cause a progressive reduction of the lordosis curve, which is associated with muscle weakness when maintaining an anteriorization state for a long duration. Dentists' work also often involves equipment requiring the user to maintain an unergonomic body posture, thereby stressing various anatomical locations (36).
Our study results show that the most common symptoms of musculoskeletal disorders were fatigue (53.6%) and pain (49.7%). These results align with a previous study by Phedy et al. (14) who reported that the most common symptoms of musculoskeletal disorders were fatigue (36.5%) and pain (24.9%). This study also shows that the most triggering or aggravating factors were unergonomic body postures when working (84.1%) and prolonged sitting positions (53.6%). Every joint in the body has a neutral movement zone or capacity whose movement does not require high muscle power. If the dentist makes movements outside this zone with an awkward or unergonomic posture, the symptoms of musculoskeletal disorders and the risk of injury will increase. The non-ergonomic positions in question include strained sitting positions, bending forward, tilting the shoulders, head tilts, and others. These are the etiology of WMSD in dental health practitioners (11, 13). Repeated application of low-load tasks or prolonged periods of sitting can result in a reduction of muscle failure tolerance. This can lead to stretching of the posterior spinal ligament, increasing the risk of local instability and injury to uni-segmental structures. Furthermore, this can cause an increase in shearing and bending loads on the neural arch. It is important to be aware of these potential risks and to take measures to minimize them, such as taking frequent breaks and engaging in physical activity to maintain muscle strength and endurance (35).
The current study also shows that factors that alleviate WMSD were taking a short break (71.5%) and improving body posture (53%). This is in line with previous studies where it was reported that working time, breaks between patients, and improving body posture were protective factors against WMSD among dental health practitioners (9, 11, 13, 19). Our study also shows that exercise was a protective factor against WMSD. The objective of strategies aimed at preventing injury is to ensure that the body's adaptation to stress resulting from exposure to load keeps pace with and ideally surpasses the accumulated tissue damage. To this end, while exposure to load is necessary to accumulate microtrauma, the applied loads must be removed to enable the healing and adaptation process to gradually increase the failure tolerance to the required level (35). The relationship between tissue loading and the risk of injury is optimal, and determining the optimal safety for individual tissue loading entails the application of both the art and science of medicine and biomechanics. A previous study by Letafatkar et al. (37) proved that therapeutic exercise reduces pain and disability and improves posture among dentists who experience chronic neck pain. In the current study, no association was found between the incidence of WMSD and demographic variables and job characteristics. However, previous studies reported that WMSD occurs more often in women; this is because women have low muscle tone, low strength, and hormonal factors that contribute to osteoporosis, making women more susceptible to musculoskeletal injuries (9). In addition, dental health practitioners with minimal work experience (including dental assistants) were also considered vulnerable to WMSD (9, 10, 14, 28).
A systematic review by Roll et al. examined prevention and rehabilitation techniques for musculoskeletal disorders among dental professionals. The study categorized these techniques into three main approaches: physical exercise, ergonomic training, and equipment modification (38). Evidence suggests that ergonomic training, particularly focusing on body posture and optimizing the work environment, can significantly reduce the risk of musculoskeletal disorders. Recommended strategies include maintaining a natural lumbar curve, utilizing magnification systems, adjusting dental chairs, and adopting positional and postural techniques such as avoiding static postures, alternating between standing and sitting, positioning patients at an optimal height, keeping feet parallel to the floor, repositioning feet, rotating shoulders backward, using backrests, and avoiding twisting motions. Furthermore, taking regular breaks combined with targeted stretching exercises—such as chairside directional stretching, microbreak stretches, trigger point release, and hand clasping with outward turning—can further mitigate these risks (39, 40). Additionally, studies have highlighted the benefits of using specific tools, such as magnification loupes, which improve posture and alleviate neck and back pain (41).
This study involved respondents from various dental professions, including dentists, dental nurses, and dental assistants, working in clinics and hospitals across Indonesia. Additionally, the study included dental professionals with diverse professional levels and job characteristics, aiming to provide a representative sample of dental professionals in Indonesia. However, this study has several limitations. First, being retrospective in nature, it is prone to selection bias. Second, there was an unequal distribution of respondents among dentists, dental nurses, and dental assistants. Furthermore, there was a gender imbalance, with a disproportionate female-to-male ratio, and the study did not investigate systemic factors that could contribute to musculoskeletal disorders.
Further research should focus on conducting longitudinal studies to explore the causal relationships between the identified potential risk factors—such as exercise, professional levels, and job characteristics—and the incidence of WMSDs. Additionally, it is crucial to investigate other potential contributing factors, including psychosocial conditions and systemic factors, that may play a role in the development of musculoskeletal disorders.
Work-related musculoskeletal disorders (WMSDs) are highly prevalent among dental professionals (DPs), with prevalence rates reaching as high as 96%. The back and waist are the most commonly affected areas, followed by the upper and lower neck. The primary symptoms of WMSDs include muscle fatigue and pain. Key contributing factors include unergonomic body postures and prolonged sitting during work. Rest, postural correction, and exercise have been shown to be effective in preventing these disorders. WMSDs can lead to work-related disabilities, reduced productivity, compromised patient care, and increased healthcare costs. Therefore, it is crucial to educate dental health practitioners about the importance of preventive measures, including physical exercise, ergonomic training, and equipment modifications. Furthermore, future research should focus on conducting longitudinal studies to better understand the causal relationships between the identified risk factors—such as exercise, professional levels, and job characteristics—and the incidence of WMSDs.
This study has several limitations. First, being retrospective in nature, it is prone to selection bias. Second, there was an unequal distribution of respondents among dentists, dental nurses, and dental assistants. Additionally, there was a gender imbalance, with a disproportionate female-to-male ratio, and the study did not investigate systemic factors that could contribute to musculoskeletal disorders.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by Faculty of Medicine, Universitas Trisakti. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
EK: Conceptualization, Data curation, Investigation, Methodology, Supervision, Writing – original draft, Writing – review & editing. XA: Conceptualization, Data curation, Investigation, Methodology, Writing – original draft, Writing – review & editing. ER: Data curation, Methodology, Writing – review & editing. IA: Methodology, Writing – review & editing. NA: Methodology, Writing – review & editing. M: Methodology, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was funded by a grant from the Faculty of Medicine, Universitas Trisakti [Grant Number: 128/A.1/LPPM-P/USAKTI/XI/2023].
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declare that no Generative AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Melhorn JM. Cumulative trauma disorders and repetitive strain injuries. The future – PubMed. (1998). Available online at: https://pubmed.ncbi.nlm.nih.gov/9646754/ (cited January 25, 2024).
2. Yassi A. Work-related musculoskeletal disorders. Curr Opin Rheumatol. (2000) 12(2):124–30. doi: 10.1097/00002281-200003000-00006
3. Anton D, Rosecrance J, Merlino L, Cook T. Prevalence of musculoskeletal symptoms and carpal tunnel syndrome among dental hygienists. Am J Ind Med. (2002) 42(3):248–57. doi: 10.1002/ajim.10110
4. Bernard BP, Putz-Anderson V. Musculoskeletal disorders and workplace factors. A critical review of epidemiologic evidence for work-related musculoskeletal disorders of the neck, upper extremity, and low back (2023). Available online at: https://www.cdc.gov/niosh/docs/97-141/ (cited April 23, 2024).
5. Roth-Isigkeit A, Thyen U, Stöven H, Schwarzenberger J, Schmucker P. Pain among children and adolescents: restrictions in daily living and triggering factors. Pediatrics. (2005) 115(2):e152–62. doi: 10.1542/peds.2004-0682
6. Experience of musculo-skeletal disorders, intensity of pain, and general conditions in work—The case of employees in non-private dental clinics in a county in southern Sweden - PubMed [Internet]. Available online at: https://pubmed.ncbi.nlm.nih.gov/12441624/ (cited April 23, 2024).
7. Bernard BP, Putz-Anderson V, Burt SE, Cole LL, Fairfield-Estill C, Fine LJ, et al. Musculoskeletal disorders and workplace factors: a critical review of epidemiologic evidence for work-related musculoskeletal disorders of the neck, upper extremity, and low back. (19970. Available online at: https://stacks.cdc.gov/view/cdc/21745 (cited April 23, 2024).
8. Ahmad I, Togoo RA, Demah DS, Atheer AA, Deena DA, Mukherjee D, et al. Influence of joint flexibility, hand grip strength and pain on oral hygiene in musculoskeletal disorders-A non-interventional clinical study. J Clin Med. (2023) 12(6):2190. doi: 10.3390/jcm12062190
9. Alzayani MK, Salama KF, Zafar M. Work-related musculoskeletal disorders among dental staff in armed force hospital in Dhahran, Saudi Arabia. Afr Health Sci. (2022) 22(2):602–11. doi: 10.4314/ahs.v22i2.69
10. Felemban RA, Sofi RA, Alhebshi SA, Alharbi SG, Farsi NJ, Abduljabbar FH, et al. Prevalence and predictors of musculoskeletal pain among undergraduate students at a dental school in Saudi Arabia. Clin Cosmet Investig Dent. (2021) 13:39–46. doi: 10.2147/CCIDE.S292970
11. Kawtharani AA, Chemeisani A, Salman F, Haj Younes A, Msheik A. Neck and musculoskeletal pain among dentists: a review of the literature. Cureus. (2023) 15(1):e33609. doi: 10.7759/cureus.33609
12. Kumar VK, Kumar SP, Baliga MR. Prevalence of work-related musculoskeletal complaints among dentists in India: a national cross-sectional survey. Indian J Dent Res. (2013) 24(4):428–38. doi: 10.4103/0970-9290.118387
13. Macrì M, Flores NVG, Stefanelli R, Pegreffi F, Festa F. Interpreting the prevalence of musculoskeletal pain impacting Italian and Peruvian dentists likewise: a cross-sectional study. Front Public Health. (2023) 11:1090683. doi: 10.3389/fpubh.2023.1090683
14. Phedy P, Gatam L. Prevalence and associated factors of musculoskeletal disorders among young dentists in Indonesia. Malays Orthop J. (2016) 10(2):1–5. doi: 10.5704/MOJ.1607.001
15. Prudhvi K, Murthy KR V. Self-reported musculoskeletal pain among dentists in visakhapatnam: a 12-month prevalence study. Indian J Dent Res. (2016) 27(4):348–52. doi: 10.4103/0970-9290.191880
16. Rambabu T, Suneetha K. Prevalence of work related musculoskeletal disorders among physicians, surgeons and dentists: a comparative study. Ann Med Health Sci Res. (2014) 4(4):578. doi: 10.4103/2141-9248.139327
17. Liskiewicz ST, Kerschbaum WE. Cumulative trauma disorders: an ergonomic approach for prevention. J Dent Hyg. (1997) 71(4):162–7.9470570
18. Morse TF, Michalak-Turcotte C, Atwood-Sanders M, Warren N, Peterson DR, Bruneau H, et al. A pilot study of hand and arm musculoskeletal disorders in dental hygiene students. J Dent Hyg. (2003) 77(3):2916–22. Available online at: https://pubmed.ncbi.nlm.nih.gov/14596163/ (cited April 23, 2024).
19. AlOtaibi F, Nayfeh FM, Alhussein J, Alturki N, Alfawzan A. Evidence based analysis on neck and low back pain among dental practitioners- A systematic review. J Pharm Bioallied Sci. (2022) 14(Suppl 1):897. doi: 10.4103/jpbs.jpbs_92_22
20. Sartorio F, Ferriero G, Corna S, Dal Negro F, DeAngeli M, Cudazzo A, et al. Relationship between work fatigue and manual dexterity in dental professionals: observational study. Med Lav. (2020) 111(6):493–502. doi: 10.23749/mdl.v111i6.10151
21. Kuorinka I, Jonsson B, Kilbom A, Vinterberg H, Biering-Sørensen F, Andersson G, et al. Standardised nordic questionnaires for the analysis of musculoskeletal symptoms. Appl Ergon. (1987) 18(3):233–7. doi: 10.1016/0003-6870(87)90010-X
22. Ramdan IM, Duma K, Setyowati DL. Reliability and validity test of the Indonesian version of the nordic musculoskeletal questionnaire (NMQ) to measure musculoskeletal disorders (MSD) in traditional women weavers. Glob Med Health Commun. (2019) 7(2):123–30. doi: 10.29313/gmhc.v7i2.4132
23. Agbor AM, Hilbert K. Work-related musculoskeletal disorders amongst oral health workers in Cameroon. OHDM. (2016) 15(6):1–6.
24. Polat Z, Başkan S, Altun S, Tacir I. Musculoskeletal symptoms of dentists from south-east Turkey. Biotechnol Biotechnol Equip. (2007) 21(1):86–90. doi: 10.1080/13102818.2007.10817421
25. Ohlendorf D, Naser A, Haas Y, Haenel J, Fraeulin L, Holzgreve F, et al. Prevalence of musculoskeletal disorders among dentists and dental students in Germany. Int J Environ Res Public Health. (2020) 17(23):1–19. doi: 10.3390/ijerph17238740
26. Leggat PA, Smith DR. Musculoskeletal disorders self-reported by dentists in Queensland. Aust Aust Dent J. (2006) 51(4):324–7. doi: 10.1111/j.1834-7819.2006.tb00451.x
27. Puriene A, Aleksejuniene J, Petrauskiene J, Balciuniene I, Janulyte V. Self-reported occupational health issues among Lithuanian dentists. Ind Health. (2008) 46(4):369–74. doi: 10.2486/indhealth.46.369
28. Yi J, Hu X, Yan B, Zheng W, Li Y, Zhao Z. High and specialty-related musculoskeletal disorders afflict dental professionals even since early training years. J Appl Oral Sci. (2013) 21(4):376–82. doi: 10.1590/1678-775720130165
29. Garbin AJÍ, Soares GB, Arcieri RM, Garbin CAS, Siqueira CE. Musculoskeletal disorders and perception of working conditions: a survey of Brazilian dentists in São Paulo. Int J Occup Med Environ Health. (2017) 30(3):367–77. doi: 10.13075/ijomeh.1896.00724
30. Atri M, Nagraj A. Identifying musculoskeletal disorders amongst dentists—the need for the hour. Int J Med Sci Public Health. (2014) 3(6):730–4. doi: 10.5455/ijmsph.2014.010420144
31. Alexopoulos EC, Stathi IC, Charizani F. Prevalence of musculoskeletal disorders in dentists. BMC Musculoskelet Disord. (2004) 5:16. doi: 10.1186/1471-2474-5-16
32. Abduljabbar TA. Musculoskeletal disorders among dentists in Saudi Arabia. Pak Oral Dent J. (2008) 28(1):135–44.
33. Vijay S, Ide M. Musculoskeletal neck and back pain in undergraduate dental students at a UK dental school—a cross-sectional study. Br Dent J. (2016) 221(5):241–5.doi: 10.1038/sj.bdj.2016.642
34. Sustová Z, Hodacová L, Kapitán M. The prevalence of musculoskeletal disorders among dentists in the Czech republic. Acta Medica (Hradec Kralove). (2013) 56(4):150–6. doi: 10.14712/18059694.2014.10
35. McGill SM. The biomechanics of low back injury: implications on current practice in industry and the clinic. J Biomech. (1997) 30(5):465–75. doi: 10.1016/S0021-9290(96)00172-8
36. Risk factors associated with work-related musculoskeletal disorders in dentistry - PubMed [Internet]. Available online at: https://pubmed.ncbi.nlm.nih.gov/27917817/ (cited January 26, 2024).
37. Letafatkar A, Rabiei P, Alamooti G, Bertozzi L, Farivar N, Afshari M. Effect of therapeutic exercise routine on pain, disability, posture, and health status in dentists with chronic neck pain: a randomized controlled trial. Int Arch Occup Environ Health. (2020) 93(3):281–90. Available online at: https://pubmed.ncbi.nlm.nih.gov/31654125/ (cited January 27, 2024). doi: 10.1007/s00420-019-01480-x
38. Roll SC, Tung KD, Chang H, Sehremelis TA, Fukumura YE, Randolph S, et al. Prevention and rehabilitation of musculoskeletal disorders in dental professionals: a systematic review. J Am Dent Assoc. (2019) 150(6):489. doi: 10.1016/j.adaj.2019.01.031
39. Nutalapati R, Gaddipati R, Chitta H, Pinninti M, Boyapati R. Ergonomics in dentistry and the prevention of musculoskeletal disorders in dentists. Int J Occup Health. (2009) 1(1):1–9.
40. Bedi HS, Moon NJ, Bhatia V, Sidhu GK, Khan N. Evaluation of musculoskeletal disorders in dentists and application of DMAIC technique to improve the ergonomics at dental clinics and meta-analysis of literature. J Clin Diagn Res. (2015) 9(6):ZC01–3. doi: 10.7860/JCDR/2015/14041.6126
41. Aghilinejad M, Kabir-Mokamelkhah E, Talebi A, Soleimani R, Dehghan N. The effect of magnification lenses on reducing musculoskeletal discomfort among dentists. Med J Islam Repub Iran. (2016) 30(1):473. Available online at: https://pmc.ncbi.nlm.nih.gov/articles/PMC5419231/ (cited December 27, 2024).28491848
Keywords: musculoskeletal disorders, dentistry, occupational medicine, prevention, work-related musculoskeletal disorders
Citation: Kholinne E, Azalia X, Rahayu EP, Anestessia IJ, Agil N and Muchtar (2025) The prevalence and risk factors of musculoskeletal disorders among Indonesian dental professionals. Front. Rehabil. Sci. 6:1513442. doi: 10.3389/fresc.2025.1513442
Received: 18 October 2024; Accepted: 27 January 2025;
Published: 12 February 2025.
Edited by:
Feng Yang, Georgia State University, United StatesReviewed by:
Dávid Líška, Matej Bel University, SlovakiaCopyright: © 2025 Kholinne, Azalia, Rahayu, Anestessia, Agil and Muchtar. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Erica Kholinne, ZXJpY2FAdHJpc2FrdGkuYWMuaWQ=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.