- 1Cardiac Rehabilitation Unit, Chong Hua Hospital, Cebu City, Philippines
- 2Multidisciplinary Center Diabetes, Thyroid and Endocrine Center (DTEC), Chong Hua Hospital, Cebu City, Philippines
- 3Cardiovascular Prevention and Rehabilitation Program, University Health Network, Toronto, ON, Canada
- 4KITE Research Institute, University Health Network, Toronto, ON, Canada
- 5Department of Physical Therapy, Temerty Faculty of Medicine, University of Toronto, Toronto, ON, Canada
Introduction: Addressing the ongoing needs of individuals with diabetes, particularly in low- and middle-income countries like the Philippines, requires a focus on regular follow-ups with healthcare teams, adherence to healthy behaviors, and effective patient education to prevent long-term complications. The aim of this study was to ascertain the impact of a comprehensive educational program for those living with diabetes in the Philippines.
Methods: In a prospective study, a convenience sample of patients living with diabetes attending a cardiac rehabilitation or an outpatient diabetes clinic in the Philippines received a 12-week education intervention. Participants completed surveys at pre- and post-intervention assessing disease-related knowledge, health literacy, dietary habits, and tobacco use. Physical activity was measured by steps taken per day using wearable devices and by self-report of minutes of moderate or vigorous-intensity exercise per week. Satisfaction with the educational materials was also evaluated by a survey composed of Likert-type scale and open-ended questions. Descriptive statistics, paired t-tests or chi-square were used for data analysis.
Results: Overall, 184 individuals living with diabetes type 2 (mean age = 54.4 ± 12.4, 32% female) completed both assessments. There was significant improvement in disease-related knowledge (p < 0.001), daily steps measured by a wearable device and self-reported minutes of moderate/vigorous-intensity exercise (p < 0.001), and the number of fruit and vegetable servings consumed per day (p = 0.001). No significant changes were observed in health literacy levels. One participant stopped using tobacco at post-education. Educational materials were highly satisfactory to participants. Lack of time, family responsibilities, and poor internet access were the main barriers to learning reported by participants. Suggestions to improve the education provided included assessment of information needs at the start of the education, having short summaries about the topics, follow-ups post-intervention, and inviting family members to sessions.
Discussion: Results of this study demonstrated the positive effects a comprehensive structured patient education intervention on disease-related knowledge and behaviour changes among people living with type 2 diabetes in the Philippines.
1 Introduction
Type 2 diabetes mellitus poses a significant global health threat, with 1 in 11 adults worldwide affected by diabetes, according to the World Heart Federation (1, 2). The prevalence of diabetes is expected to rise substantially, reaching 629 million by 2045 from the current 425 million (2, 3). In the Philippines, the diabetes burden is substantial, with 7.1% of adults diagnosed in 2019, and it stands as the fourth leading cause of mortality in the country (4, 5). Despite the heightened risk of health complications, including cardiovascular disease, for individuals with diabetes, significant gaps persist in the care and prevention of this condition in the Philippines (6, 7).
One of the foremost challenges in contemporary diabetes care involves meeting the ongoing needs of individuals grappling with this chronic condition (8, 9). It is imperative to emphasize the significance of regular follow-ups with healthcare teams and the adherence to healthy behaviors to forestall potential long-term complications associated with diabetes (10). The process of adapting to life with a complex condition like diabetes is intricate and necessitates comprehensive patient education (11). While there is a growing body of evidence supporting the efficacy of patient education in managing chronic conditions, including diabetes (11–13), there is a notable dearth of information regarding effective programs tailored for individuals residing in low- and middle-income countries like the Philippines.
Cardiac rehabilitation (CR) plays a pivotal role in the comprehensive care and education of individuals with diabetes, particularly those at an elevated risk of cardiovascular complications (14). Beyond its traditional focus on heart health, CR programs have evolved to encompass a holistic approach that addresses the intricate interplay between diabetes and cardiovascular well-being (15). These programs provide a structured platform for educating diabetes patients about the synergistic relationship between diabetes management and cardiovascular health (14, 16). Through tailored educational interventions, individuals learn about the intricate nuances of diabetes, its impact on cardiovascular function, and strategies to mitigate associated risks. The emphasis is not only on disease-specific knowledge but also on fostering behavioral changes, such as adopting a heart-healthy lifestyle, adhering to medication and exercise regimens, and understanding the symbiotic connection between blood glucose control and cardiovascular outcomes (14). By integrating diabetes education into CR, healthcare providers can empower patients to take proactive steps in managing their overall health, thereby enhancing their quality of life and reducing the risk of complications (16).
A recent scoping review of diabetes education literature highlighted the scarcity of published research for individuals with diabetes in the Philippines, the available data indicated the effectiveness of patient education in enhancing diabetes knowledge, self-efficacy, anthropometric measures, A1C levels, utilization of healthcare services, and attitudes towards health (7). Regrettably, the review could not pinpoint a specific educational model suitable for this population, including in CR programs. Nonetheless, it underscored the imperative to conduct and disseminate further research on diabetes education in the Philippines.
In this context, we identified an evidence-based and comprehensive educational program—called Diabetes College—for those living with diabetes. Embedded within Health e-University, a virtual institute dedicated to promoting the prevention and management of chronic diseases, Diabetes College has undergone testing in high-income settings, demonstrating its efficacy in enhancing clinical outcomes, promoting heart-healthy behaviors, and augmenting knowledge in those individuals living with diabetes and participating in CR programs (17, 18). Therefore, the aim of this study was to ascertain the impact of this education intervention in those living with diabetes in the Philippines.
2 Methods
2.1 Design
This was a prospective observational study. Patients living with diabetes and attending a CR program or a diabetes outpatient clinic received the 12-week education intervention and completed pre- and post-intervention questionnaires. The study was conducted in the Chong Hua Hospital, Cebu City, Philippines following the standards required by the Declaration of Helsinki and approved by the Hospital's Ethics Committee (approval number: 2021-03). All participants provided written informed consent. Data were collected between November/2021 and August/2023.
2.2 Setting and intervention
Established in 2003, the CR unit at Chong Hua Hospital Heart Institute plays a vital role in the healthcare landscape, attending to an annual average of 250 patients, half of whom are managing diabetes. The phase 2 CR program spans 8 weeks, with patients participating in on-site sessions thrice weekly, each lasting for an hour. The dedicated healthcare team includes three cardiologists, one nurse, one physiotherapist, and one cardiology fellow. While the program primarily centers around exercise, it allocates 15 min per week for essential patient education. This educational component focuses on comprehending heart disease, procedures, medications, weight maintenance, risk factor modification, and dietary instructions. Notably, diabetes education was not integrated into the program before the commencement of this study.
The Diabetes Outpatient Program at the Diabetes, Thyroid, and Endocrine Center (DTEC) within Chong Hua Hospital was established in September 2021, offering care to 550 patients annually. Individuals managing diabetes participate in clinic visits once or twice a month, engaging in exercise and nutrition orientation sessions, as well as counseling. This comprehensive approach is facilitated by consultant endocrinologists on rotation, nurse educators, endocrine fellows, and dietitians, collectively contributing to the holistic management and support of patients with diabetes.
2.3 Educational intervention
The English version of Diabetes College was originally reviewed by 17 diabetes experts in the Philippines encompassing 3 physicians, 2 nurses, 2 pharmacists, 2 physical therapists, and 8 people who identified themselves as “hospital staff”. These experts offered valuable perspectives on how the materials could be structured for enhanced patient support. The consensus among the experts was that the materials were easily comprehensible and featured language and content culturally tailored to individuals residing in the Philippines. Additionally, the materials were reviewed by 4 patient partners, who were satisfied with the information provided and thought the resources were clear and useful.
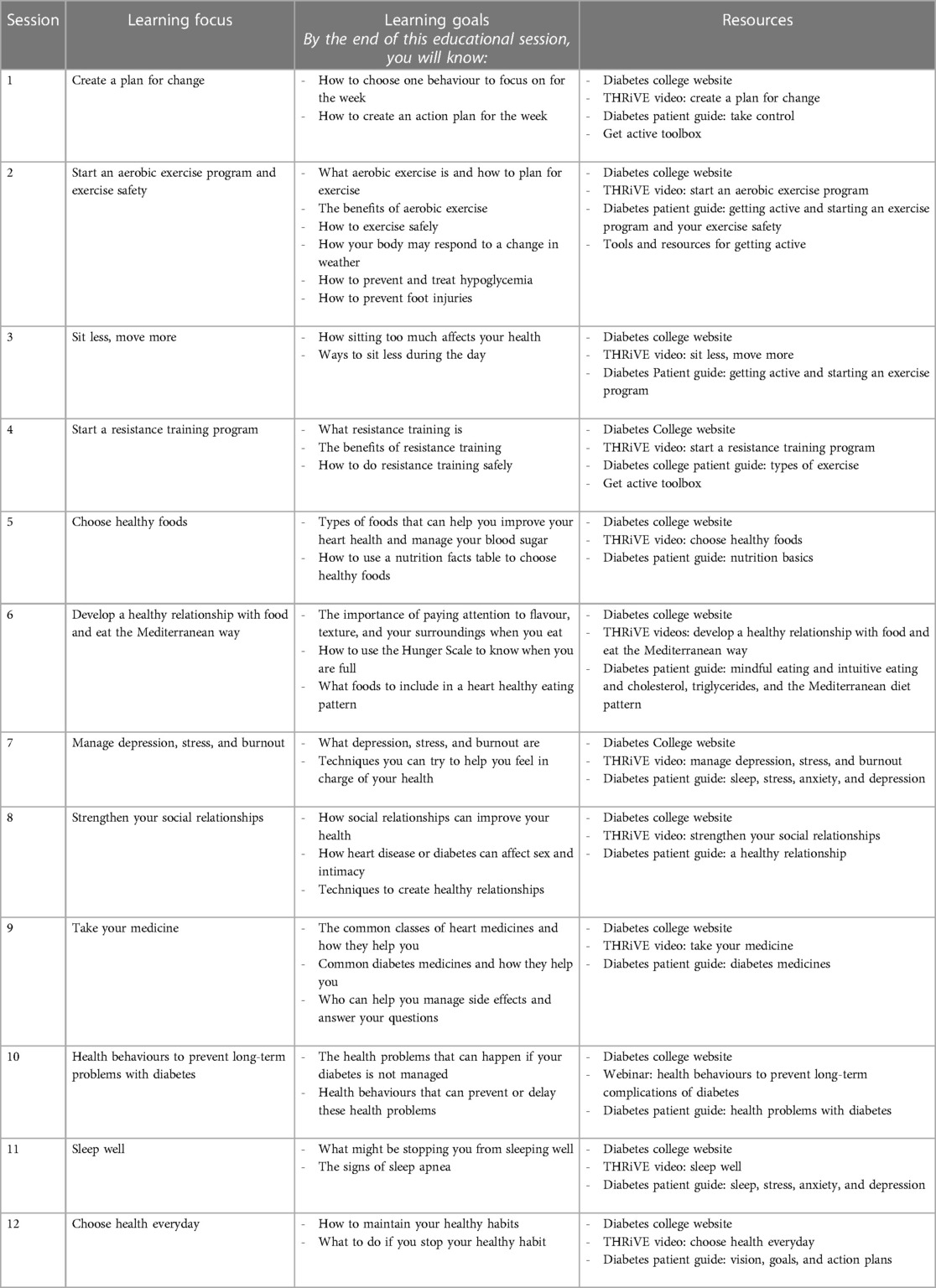
In response to feedback provided by local experts and patients, materials from Diabetes College were structured into a 12-week educational curriculum (refer to Table 1). Study participants were provided with 12 weekly learning schedules containing hyperlinks to online resources, which included a comprehensive patient guide spanning 296 pages and a series of 12 animated videos (THRiVE series), each with an average duration of 5 min. The educational content was categorized into five knowledge pillars: managing diabetes, promoting physical activity, adopting healthy eating habits, enhancing overall well-being, and fostering self-management. The education process was designed to be self-directed, allowing patients the flexibility to engage with the learning materials according to their individual preferences and schedules. Rather than adhering to a rigid structure or timeline, patients had the autonomy to explore the educational content at a pace that suited their needs and learning styles. However, during the CR sessions or clinic visits, patients were encouraged to raise any questions they had regarding the content, and key messages were reiterated to reinforce understanding.
2.4 Participants
A convenience sample of individuals diagnosed with type 2 diabetes was recruited for this study. Inclusion criteria comprised a confirmed diagnosis of diabetes type 2. Exclusion criteria encompassed individuals with limited proficiency in English, as well as those experiencing visual or cognitive impairments that might hinder survey completion. All participants were provided with internet cards to facilitate access to online resources.
2.5 Outcome measures
The following outcome measurements were assessed pre- and post-intervention: disease-related knowledge, health literacy, physical activity, dietary habits, and tobacco use. Participants also self-reported their work status, educational level, and marital status at pre-intervention. At post-intervention participants completed a satisfaction and usability survey about the use of educational materials, which included 10 Likert-type, yes/no and open-ended questions. Sociodemographic and clinical characteristics (age, gender, other diagnosis and comorbidities) were extracted from medical records.
Disease-related knowledge was assessed using the DiAbeTes Education Questionnaire (DATE-Q), which includes 20 true/false/I don't know items about self-management, long-term complications, being active, healthy eating, and psychosocial wellbeing (19). Higher scores indicate higher knowledge, with a maximum overall score of 20.
Health literacy was measured using the BRIEF Health Literacy Screening Tool, which asks respondents to complete four questions using a 5-point Likert-type scale (20). Scores range from 4 to 20, with the following health literacy skills categories: 4–12 (inadequate), 13–16 (marginal), and 17–20 (adequate).
Physical activity was assessed by self-report of minutes of moderate or vigorous-intensity exercise per week, and by daily step counts using a wearable device. The number of steps was recorded by asking participants to track steps for 7 consecutive days and record their numbers in a journal. Participants were categorized as active or inactive using a threshold of a mean of 10,000 steps per day over the seven-day period (21).
Dietary habits were assessed by self-reporting fruit and vegetable servings per day. Participants were categorized as following vs. not following the recommendations of consuming at least five servings of fruits and vegetables per day (22). Tobacco use was also self-reported (current, past, never).
2.6 Statistical analysis
SPSS Version 29.0 was used, and the level of significance was set at 0.05 for all tests. First, descriptive statistics were used to describe sociodemographic and clinical characteristics of participants (valid percentages are shown). Secondly, paired t-tests or chi-square tests were used to compare differences in characteristics. Third, changes in outcomes from pre- to post-interventions were assessed using paired t-tests or chi-square test by group (normality was met). Finally, results from the satisfaction/usability survey were reported using descriptive statistics and open-ended response items were coded using content analysis.
3 Results
3.1 Participant characteristics
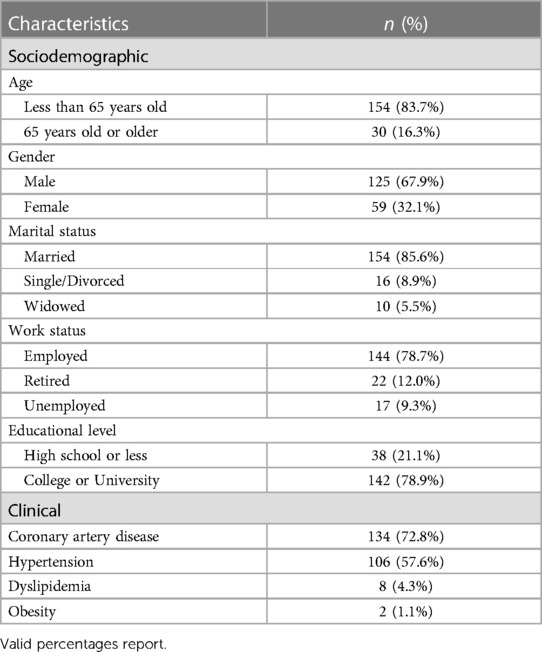
A convenience sample of 184 individuals living with diabetes type 2 (mean age = 54.4 ± 12.4 years old, 32% female) accepted to be part of this study. Sociodemographic and clinical characteristics of the sample are shown in Table 2. Overall, participants were younger (i.e., less than 65 years old), male, married, employed, highly educated (i.e., college or university degree), and also had diagnosis of coronary artery disease. Participants attended a mean of 9.5 ± 1.0 educational sessions.
3.2 Effects of education
Mean scores of all outcome measures at each assessment are presented in Table 3. As shown, there was a significant increase from pre- to post-intervention in disease-related knowledge—total scores (p < 0.0001), as well as in all 5 knowledge areas. Being active was the area with the biggest increase in score pre- to post-education. Although significantly increased post-education, knowledge about self-management was the lowest among the 5 areas. No significant changes were observed in health literacy levels.
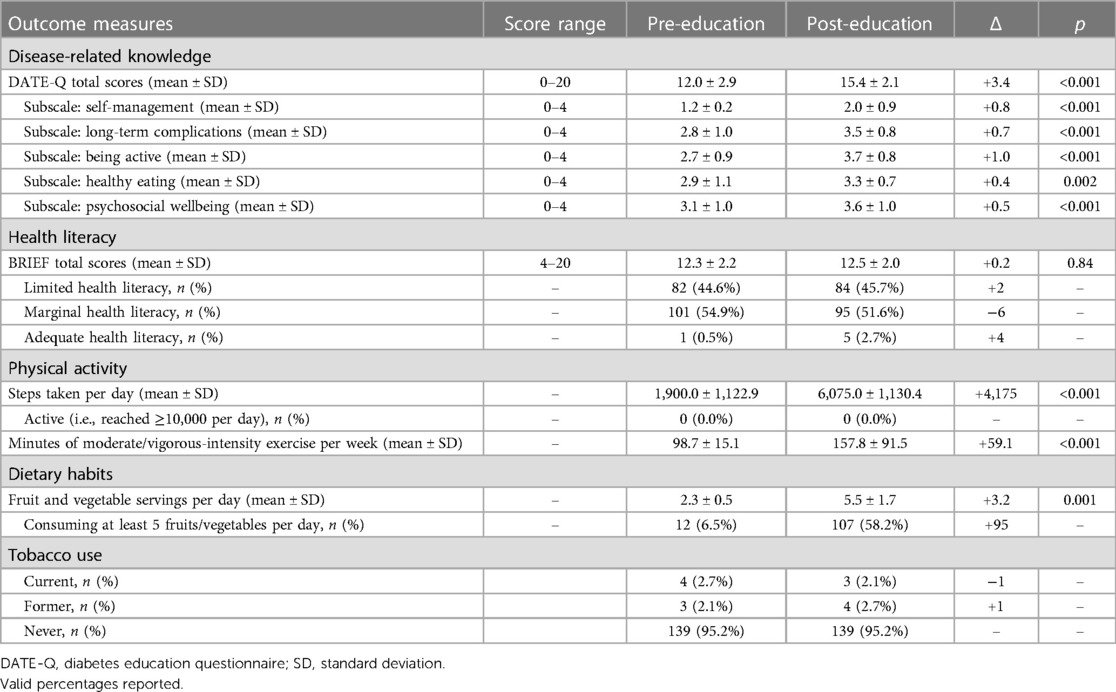
Table 3. Disease-related knowledge, health literacy, physical activity, dietary habits and tobacco use, pre- and post-education (N = 184).
In regard to physical activity, daily steps measured by a device increased significantly at post-education (p < 0.001); however, none of the participants reached the recommended 10,000 steps per day. The self-reported minutes of moderate/vigorous-intensity exercise per week also significantly increased (p < 0.001). In regard to dietary habits, the number of fruit and vegetable servings per day increase significantly post-education (p = 0.001) and the percentage of participants who self-reported consuming at least 5 fruits or vegetables per day increased from 6.5% to 58.2%. Lastly, one participant stopped using tobacco.
3.3 Satisfaction and usability of the education
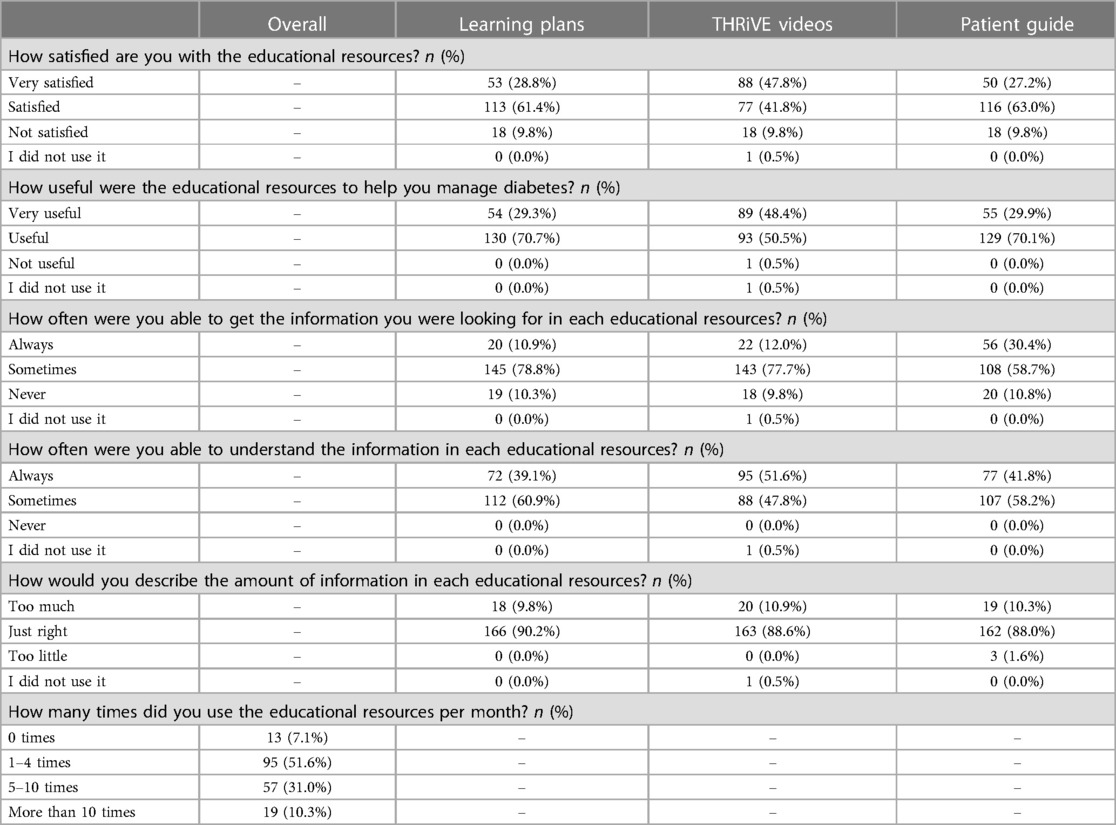
Table 4 presents the satisfaction and usability of educational resources (i.e., learning plans, THRiVE videos, and the patient guide). Overall, the majority of participants were satisfied with the resources provided, thought the resources were useful to help them manage diabetes, were often able to get information they were looking for, and were able to understand the information provided in each educational resource. Most participants also reported the amount of information in each education resource as “just right” and 52% indicated they accessed resources 1–4 times per month while attending the educational intervention.
In regard to content, participants indicated that all 5 knowledge pillars—treat diabetes, get active, eat healthy, feel well, and take control—were explained well, and highlighted the get active sessions as the ones with more impact on their health behaviours. When asked about what they would do if they needed information about a specific topic, 40% of participants reported they would look for answers in the educational materials provided.
Finally, answers from open-ended questions asking about information needs, barriers to learning, and suggestions for improvement were coded. Themes derived from the coded responses revealed persistent information gaps among participants concerning self-management and understanding the impact of diabetes on their quality of life and overall health. Participants identified time constraints, family responsibilities, and limited internet access as the primary barriers to effective learning. Notable suggestions to enhance the educational program included the importance of eliciting patients' specific needs prior to intervention delivery, facilitating the provision of concise summaries and key messages, implementing regular follow-ups with participants post-intervention, and incorporating family members into the educational sessions. These insights from participants offer valuable guidance for refining and optimizing future educational initiatives.
4 Discussion
Despite the increasing prevalence of diabetes in the Philippines, existing evidence highlights the suboptimal state of diabetes care and control, particularly in the realm of patient education. The outcomes of this first-ever study offering a comprehensive diabetes education program to individuals living with diabetes in the Philippines and attending CR, underscore the affirmative impact on disease-related knowledge, physical activity, and dietary habits. These findings are particularly heartening, as they emphasize the potential benefits of a culturally adapted, evidence-based, and patient-centered comprehensive education intervention. The study not only addresses a significant gap in diabetes education but also sheds light on the crucial necessity for Filipinos living with diabetes to acquire the knowledge and skills for effective self-management of their chronic condition. This pioneering effort paves the way for further initiatives aimed at enhancing diabetes care and education in the Philippines. The observed changes in disease-related knowledge and behaviors highlight the clinical significance of the educational intervention. Participants demonstrated significant increases in disease-related knowledge across all five knowledge areas, particularly in understanding the importance of physical activity. Improvements in physical activity levels, dietary habits, and tobacco cessation underscore the positive impact of the intervention on participants' ability to manage diabetes and promote better health outcomes.
It is essential to emphasize that the reasons behind the observed improvements in outcomes are likely influenced by multiple factors. The educational intervention, a key element of either CR or diabetes outpatient programs, involves providing counseling to participants. The CR program, specifically, stands out as a comprehensive secondary prevention initiative where patient education and counseling play integral roles (23). This program is designed to benefit patients dealing with multiple cardiovascular and chronic conditions, creating an avenue for valuable support (24). Within the CR program, individuals living with diabetes not only receive education but also gain access to an interprofessional healthcare team. This team structure allows for comprehensive care, and individuals with diabetes have the valuable opportunity to receive referrals to different specialists, thereby enhancing their self-management support (25). However, it is noteworthy that research has highlighted the importance of more than just the involvement of various healthcare team members in a patient's learning process. To ensure consistent and effective education for those living with type 2 diabetes, it is crucial to have the right resources and adopt a comprehensive approach (26). This approach ensures that individuals with diabetes receive education in a manner that is not only well-coordinated but also tailored to their specific needs and circumstances. The synergy of a well-structured program, an interprofessional team, and appropriate resources contributes to a more impactful and consistent educational experience for individuals managing type 2 diabetes.
The significance of health literacy in the realm of diabetes care cannot be overstated (27). Recently, the concept of health literacy has undergone a transformation, extending beyond the individual's skills in obtaining, processing, and understanding health information to encompass the demands placed on the health system in delivering information and instructions (28). In this context, this study did not observe an increase in health literacy post-education, which is in contrast to previous studies with people living with diabetes (29). The lack of change in health literacy post-intervention poses significant implications for the overall effectiveness of the educational program, potentially hindering participants' ability to understand and apply health information, sustain behavioral changes, and navigate healthcare systems effectively (29). This disparity might be attributed to inherent limitations in the measurement of health literacy, both within research methodologies and in the clinical setting. It underscores the need for a nuanced approach to comprehensively assess health literacy, considering not only individual capabilities but also the complex dynamics within the health system that influence the effective communication of information and instructions to individuals managing diabetes. Addressing these nuances is crucial for the development of targeted interventions that truly enhance health literacy in diabetes care. It is important to mention that while the incorporation of a health literacy assessment adds value to the study, the selection of the BRIEF Health Literacy Screening Tool warrants discussion regarding its suitability and inherent limitations (20). This tool is often chosen for its brevity and ease of administration, making it practical for use in clinical and research settings. However, it's important to acknowledge that the BRIEF tool provides only a brief assessment of health literacy and may not capture the full spectrum of health literacy skills. Its simplicity might overlook nuanced aspects of health literacy, such as the ability to comprehend complex health information or navigate healthcare systems effectively. Furthermore, the BRIEF Health Literacy Screening Tool may not be sensitive enough to detect variations in health literacy levels among different populations or cultural groups. Its generic nature may limit its applicability in diverse contexts where health literacy challenges may manifest differently.
There is a scarcity of information concerning patients' experiences, perspectives, and preferences in the realm of diabetes education (7, 29). The effectiveness of educational interventions is intricately influenced by the diversity of these experiences, views, and preferences, which can vary significantly both within and across individuals (30). Recognizing this variability is paramount, and cultural adaptation of materials is essential, alongside the provision of a range of resources to cater to these differences (31, 32). This study sought to address this gap by offering a diverse set of educational resources to individuals in the Philippines, meticulously reviewed by both experts and patients. The outcomes of this study not only shed light on patients' preferences regarding diabetes education but also extend an invitation to the broader research community to delve deeper into understanding the educational needs of individuals managing diabetes. The insights gleaned from this study underscore the importance of a patient-centered approach in diabetes education, encouraging ongoing exploration and refinement of educational strategies to better align with the diverse preferences and needs of the individuals involved.
Although our study provides favourable effects of a structured patient education on disease-related knowledge and behaviour changed among people living with type 2 diabetes and attending CR or diabetes programs in the Philippines, results should be interpreted with caution. Firstly, the absence of a comparison group (i.e., a group without education) precludes the drawing of causal conclusions. Moreover, the sustainability of the observed gains in knowledge and the adoption of healthy behaviors over time remains uncertain due to the lack of follow-up assessments. Secondly, the generalizability of results is limited to patients accessing CR and diabetes clinics, representing a minority of patients in the Philippines. Notably, the study sample was predominantly highly educated (79% with a college or university degree). This demographic composition poses a limitation to the generalizability of the study findings to a broader population. High levels of education within the sample suggest a potential bias towards individuals with greater access to resources, higher socioeconomic status, and potentially different health behaviors or attitudes compared to the general population. Consequently, the findings may not accurately reflect the experiences or perspectives of individuals with lower levels of education or socioeconomic status. Thirdly, the absence of structured clinical interviews to assess physical activity and dietary habits, relying solely on self-reported measures, introduces a potential limitation to the study results. Furthermore, it's important to note that this study utilized a convenience sample, and as such, power analysis was not conducted. The decision to employ a convenience sample implies that participants were selected based on availability and accessibility rather than through randomization or rigorous sampling methods. However, it's essential to acknowledge that convenience sampling can introduce selection bias, as individuals who are easily accessible may not be representative of the broader population under study. In addition, the incorporation of both objective measures (such as wearable devices for physical activity) and self-reported measures (via surveys) is advantageous; however, the self-reported data, especially concerning physical activity and dietary habits, has inherent limitations. Finally, critical outcome measures for individuals with diabetes, such as medication adherence and glycemic control, were not evaluated and should be included in future studies. Replication of the study in diverse patient samples across different regions of the Philippines, receiving varied care, is imperative for a more comprehensive understanding of the educational impact in this context.
In summary, the study revealed that implementing a comprehensive diabetes education intervention for individuals with type 2 diabetes in the Philippines led to significant improvements in disease-related knowledge and healthy behaviors, such as physical activity and dietary habits; while acknowledging limitations in generalizability, these promising findings underscore the importance of expanding educational resources and accessibility for Filipinos with diabetes. While acknowledging the study's limitations in terms of generalizability to a broader population, these promising findings underscore the critical importance of expanding educational resources and accessibility tailored to the unique needs of Filipinos living with diabetes. This study serves as a beacon, emphasizing the imperative to cultivate and disseminate effective educational initiatives to empower individuals with diabetes and enhance their overall well-being. Further research and strategic interventions are warranted to ensure the continued success and widespread impact of diabetes education in the Filipino context.
Data availability statement
The datasets presented in this article are not readily available because of restrictions imposed by the privacy of participants. Requests to access the datasets should be directed to Gabriela Ghisi gabriela.meloghisi@uhn.ca.
Ethics statement
The studies involving humans were approved by Chong Hua Hospital Ethics Committee. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
MT: Formal Analysis, Investigation, Resources, Writing – original draft. IB: Investigation, Writing – review & editing. SB: Investigation, Writing – review & editing. RP: Investigation, Writing – review & editing. BT: Investigation, Writing – review & editing. EG: Investigation, Writing – review & editing. CA: Resources, Writing – review & editing. PO: Conceptualization, Resources, Writing – review & editing. GG: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Resources, Supervision, Writing – original draft.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article.
Funds to conduct this work were received by Sun Life Financial.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Khan MAB, Hashim MJ, King JK, Govender RD, Mustafa H, Al Kaabi J. Epidemiology of type 2 diabetes—global burden of disease and forecasted trends. J Epidemiol Glob Health. (2020) 10(1):107–11. doi: 10.2991/jegh.k.191028.001
2. Mitchell S, Malanda B, Damasceno A, Eckel RH, Gaita D, Kotseva K, et al. A roadmap on the prevention of cardiovascular disease among people living with diabetes. Glob Heart. (2019) 14:215–44. doi: 10.1016/j.gheart.2019.07.009
3. Magliano DJ, Boyko EJ, Committee IDFDAtes. IDF Diabetes Atlas. Brussels: International Diabetes Federation (2021).
4. World Bank World Bank Collection of Development Indicators. (2020). Available online at: https://tradingeconomics.com/philippines/diabetes-prevalence-percent-of-population-ages20-to-79-wb-data.html (accessed November 27, 2023)
5. Philippine Statistics Authority. Causes of deaths in the Philippines (preliminary). (2020). Available online at: https://psa.gov.ph/vital-statistics/id/165640 (accessed November 27, 2023)
6. Arcellana AE, Jimeno C. Challenges and opportunities for diabetes care in the Philippines in the time of the COVID-19 pandemic. J ASEAN Fed Endocr Soc. (2020) 35:55–7. doi: 10.15605/jafes.035.01.04
7. Ghisi GLM, Vanzella LM, Pakosh M, Trani MR, Bilocura I, Bersabal S, et al. Patient education for people living with diabetes in the Philippines: a scoping review of information needs, diabetes knowledge and effectiveness of educational interventions. Diabetes Metab Syndr. (2022) 16(5):102494. doi: 10.1016/j.dsx.2022.102494
8. Adu MD, Malabu UH, Malau-Aduli AEO, Malau-Aduli BS. Enablers and barriers to effective diabetes self-management: a multi-national investigation. PLoS One. (2019) 14(6):e0217771. doi: 10.1371/journal.pone.0217771
9. Whittemore R, Vilar-Compte M, De La Cerda S, Marron D, Conover R, Delvy R, et al. Challenges to diabetes self-management for adults with type 2 diabetes in low-resource settings in Mexico City: a qualitative descriptive study. Int J Equity Health. (2019) 18(1):133. doi: 10.1186/s12939-019-1035-x
10. Coyle ME, Francis K, Chapman Y. Self-management activities in diabetes care: a systematic review. Aust Health Rev. (2013) 37(4):513–22. doi: 10.1071/AH13060
11. Clark M. Diabetes self-management education: a review of published studies. Prim Care Diabetes. (2008) 2(3):113–20. doi: 10.1016/j.pcd.2008.04.004
12. Correia JC, Waqas A, Assal JP, Davies MJ, Somers F, Golay A, et al. Effectiveness of therapeutic patient education interventions for chronic diseases: a systematic review and meta-analyses of randomized controlled trials. Front Med (Lausanne). (2023) 9:996528. doi: 10.3389/fmed.2022.996528
13. Warsi A, Wang PS, LaValley MP, Avorn J, Solomon DH. Self-management education programs in chronic disease: a systematic review and methodological critique of the literature. Arch Intern Med. (2004) 164(15):1641–9. doi: 10.1001/archinte.164.15.1641
14. Campos NA, Palacios GA. Cardiac rehabilitation in patients with diabetes. Panminerva Med. (2021) 63(2):184–92. doi: 10.23736/S0031-0808.21.04308-1
15. Jiménez-Navarro MF, Lopez-Jimenez F, Pérez-Belmonte LM, Lennon RJ, Diaz-Melean C, Rodriguez-Escudero JP, et al. Benefits of cardiac rehabilitation on cardiovascular outcomes in patients with diabetes Mellitus after percutaneous coronary intervention. J Am Heart Assoc. (2017) 6(10):e006404. doi: 10.1161/JAHA.117.006404
16. Hansen D, Kraenkel N, Kemps H, Wilhelm M, Abreu A, Pfeiffer AF, et al. Management of patients with type 2 diabetes in cardiovascular rehabilitation. Eur J Prev Cardiol. (2019) 26(2_suppl):133–44. doi: 10.1177/2047487319882820
17. Health e-University. Available online at: https://www.diabetescollege.ca/ (accessed November 27, 2023)
18. Ghisi GLM, Aultman C, Konidis R, Foster E, Tahsinul A, Sandison N, et al. Effectiveness of an education intervention associated with an exercise program in improving disease-related knowledge and health behaviours among diabetes patients. Patient Educ Couns. (2020) 103(9):1790–7. doi: 10.1016/j.pec.2020.04.007
19. Ghisi GLM, Aultman C, Konidis R, Foster E, Sandison N, Alavinia M, et al. Development and validation of the DiAbeTes education questionnaire (DATE-Q) to measure knowledge among diabetes and prediabetes patients attending cardiac rehabilitation programs. J Cardiopulm Rehabil Prev. (2021) 41(4):224–9. doi: 10.1097/HCR.0000000000000546
20. Haun J, Luther S, Dodd V, Donaldson P. Measurement variation across health literacy assessments: implications for assessment selection in research and practice. J Health Commun. (2012) 17:141–59. doi: 10.1080/10810730.2012.712615
21. Del Pozo-Cruz J, Alvarez-Barbosa F, Gallardo-Gomez D, Del pozo Cruz B. Optimal number of steps per day to prevent all-cause mortality in people with prediabetes and diabetes. Diabetes Care. (2022) 45(9):2156–8. doi: 10.2337/dc22-0524
22. Food and Agriculture Organization of the United Nations. Nutritional Guidelines for Filipinos. (2012). Available online at: https://www.fao.org/nutrition/education/food-dietary-guidelines/regions/countries/philippines/en/ (accessed November 27, 2023)
23. Grace SL, Turk-Adawi KI, Contractor A, Atrey A, Campbell NR, Derman W, et al. Cardiac rehabilitation delivery model for low-resource settings: an international council of cardiovascular prevention and rehabilitation consensus statement. Prog Cardiovasc Dis. (2016) 59(3):303–22. doi: 10.1016/j.pcad.2016.08.004
24. Bellmann B, Lin T, Greissinger K, Rottner L, Rillig A, Zimmerling S. The beneficial effects of cardiac rehabilitation. Cardiol Ther. (2020) 9(1):35–44. doi: 10.1007/s40119-020-00164-9
25. Lopez-Jimenez F, Kramer VC, Masters B, Stuart PM, Mullooly C, Hinshaw L, et al. Recommendations for managing patients with diabetes mellitus in cardiopulmonary rehabilitation: an American association of cardiovascular and pulmonary rehabilitation statement. J Cardiopulm Rehabil Prev. (2012) 32(2):101–12. doi: 10.1097/HCR.0b013e31823be0bc
26. Powers MA, Bardsley J, Cypress M, Duker P, Funnell MM, Fischl AH, et al. Diabetes self-management education and support in type 2 diabetes: a joint position statement of the American diabetes association, the American association of diabetes educators, and the academy of nutrition and dietetics. Clin Diabetes. (2016) 34(2):70–80. doi: 10.2337/diaclin.34.2.70
27. Cavanaugh KL. Health literacy in diabetes care: explanation, evidence and equipment. Diabetes Manag. (2011) 1(2):191–9. doi: 10.2217/dmt.11.5
28. Berkman ND, Davis TC, Mccormack L. Health literacy: what is it? J Health Commun. (2010) 15(Suppl 2):9–19. doi: 10.1080/10810730.2010.499985
29. Chaves GSS, Britto R, Oh P, Ghisi GLM. Disease-related knowledge, health behaviours and clinical outcomes following an educational intervention in patients with diabetes according to their health literacy level: a systematic review. Cardiorespir Physiother Crit Care Rehabil. (2021) 1:e42809. doi: 10.4322/2675-9977.cpcr.42809
30. Charon R. The patient-physician relationship. Narrative medicine: a model for empathy, reflection, profession, and trust. JAMA. (2001) 286(15):1897–902 doi: 10.1001/jama.286.15.1897
31. Paltzat K, Scott S, Dhaliwal KK, Saunders-Smith T, Manns BJ, Campbell T, et al. Patient perspectives on a tailored self-management education and support intervention for low-income seniors with chronic health conditions. CJC Open. (2023) 5(11):808–15. doi: 10.1016/j.cjco.2023.08.002
Keywords: diabetes mellitus type 2, patient education as topic, health knowledge, attitudes and practice, behavior change, Philippines
Citation: Trani MR, Bilocura I, Bersabal S, Panilagao RK, Toledo BR, Garrido E, Aultman C, Oh P and Ghisi GLM (2024) Effects of a comprehensive structured patient education intervention on disease-related knowledge and behaviour change among people living with type 2 diabetes in the Philippines. Front. Rehabil. Sci. 5:1374850. doi: 10.3389/fresc.2024.1374850
Received: 22 January 2024; Accepted: 14 February 2024;
Published: 28 February 2024.
Edited by:
Buse Ozcan Kahraman, Dokuz Eylul University, TürkiyeReviewed by:
Aylin Tanriverdi, Çankırı Karatekin University, TürkiyeHülya Tuna, Dokuz Eylul University, Türkiye
© 2024 Trani, Bilocura, Bersabal, Panilagao, Toledo, Garrido, Aultman, Oh and Ghisi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gabriela Lima de Melo Ghisi Z2FicmllbGEubWVsb2doaXNpQHVobi5jYQ==
 Maria Rosan Trani1
Maria Rosan Trani1 Paul Oh
Paul Oh Gabriela Lima de Melo Ghisi
Gabriela Lima de Melo Ghisi