
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
PERSPECTIVE article
Front. Rehabil. Sci. , 14 December 2023
Sec. Disability, Rehabilitation, and Inclusion
Volume 4 - 2023 | https://doi.org/10.3389/fresc.2023.1305084
This article is part of the Research Topic International Day of Persons with Disabilities – Children’s Disabilities View all 25 articles
 Linda Nguyen1,2*
Linda Nguyen1,2* Claire Dawe-McCord3,4,5
Claire Dawe-McCord3,4,5 Michael Frost5
Michael Frost5 Musa Arafeh5
Musa Arafeh5 Kyle Chambers5
Kyle Chambers5 Dana Arafeh5
Dana Arafeh5 Kinga Pozniak6
Kinga Pozniak6 Donna Thomson6
Donna Thomson6 JoAnne Mosel6
JoAnne Mosel6 Roberta Cardoso7
Roberta Cardoso7 Barb Galuppi2
Barb Galuppi2 Sonya Strohm2
Sonya Strohm2 Alicia Via-Dufresne Ley7
Alicia Via-Dufresne Ley7 Caitlin Cassidy8
Caitlin Cassidy8 Dayle McCauley2
Dayle McCauley2 Shelley Doucet9
Shelley Doucet9 Hana Alazem10
Hana Alazem10 Anne Fournier11
Anne Fournier11 Ariane Marelli12
Ariane Marelli12 Jan Willem Gorter2,13,14
Jan Willem Gorter2,13,14  on behalf of the CHILD-BRIGHT READYorNot™ Brain-Based Disabilities Trial Study Group
on behalf of the CHILD-BRIGHT READYorNot™ Brain-Based Disabilities Trial Study Group
There is a growing number of youth with healthcare needs such as disabilities or chronic health conditions who require lifelong care. In Canada, transfer to the adult healthcare system typically occurs at age 18 and is set by policy regardless of whether youth and their families are ready. When the transition to adult services is suboptimal, youth may experience detrimental gaps in healthcare resulting in increased visits to the emergency department and poor healthcare outcomes. Despite the critical need to support youth with disabilities and their families to transition to the adult healthcare system, there is limited legislation to ensure a successful transfer or to mandate transition preparation in Canada. This advocacy and policy planning work was conducted in partnership with the Patient and Family Advisory Council (PFAC) within the CHILD-BRIGHT READYorNot™ Brain-Based Disabilities (BBD) Project and the CHILD-BRIGHT Policy Hub. Together, we identified the need to synthesize and better understand existing policies about transition from pediatric to adult healthcare, and to recommend solutions to improve healthcare access and equity as Canadian youth with disabilities become adults. In this perspective paper, we will report on a dialogue with key informants and make recommendations for change in healthcare transition policies at the healthcare/community, provincial and/or territorial, and/or national levels.
A growing number of children and youth with healthcare needs (YHCN) such as disabilities or chronic health conditions require life-long care (1–3). Psychosocial changes during the transition from adolescence to adulthood can be difficult for any individual. YHCN navigate the added challenge of transitioning from pediatric to adult healthcare services. The transition to adult services is defined as the “purposeful, planned movement of adolescents and young adults with chronic health conditions from child-centered to adult-oriented health care systems” (4). The most common age of transfer in Canada is 18, though it ranges from 16 to 25 years old for various services in different settings (5). The timing of transfer is set by policy, rather than by youth readiness. When the transition to adult services is suboptimal, youth may experience detrimental gaps in healthcare, increased visits to the emergency department, undue stress and poor health outcomes (6–9). Families have described the lack of preparation and access to adult healthcare services as “falling off a cliff” (10, 11).
Youth with complex healthcare needs are expected to transfer out of the pediatric system to access adult care services but require continuity of care (12, 13). Despite the rising number of YCHN entering adult services, there is limited legislation to govern the expectations of transition, including successful transfer, or to mandate transition standards in Canada. Current legislations about transition, including the age of transfer, vary greatly between provinces and territories (14, 15). Existing documents about transition are only guidelines or recommendations, which do not formally mandate adherence in practice. With varying implementation of guidelines and recommendations across Canada, transition preparation and follow through for YHCN depends greatly on the unique characteristics of the care environment in which they are receiving care, leading to inequities in access to supports and services.
There is an increasing need to support and empower youth during healthcare transition. In Canada, the federal government sets general health standards under the Canada Health Act and provides financial support for healthcare services to the provinces and territories. The provinces and territories are then responsible for administering and delivering health services, including the planning and funding of health facilities and implementation of health initiatives (16). The autonomy afforded to individual provinces and territories in determining health programming and funding responsibility has led to differences in healthcare transition planning for youth with disabilities and their families. Despite advocacy efforts from youth, families, and healthcare providers to bring attention to this critical issue, there have been few legislative changes, which may indicate a need for clear evidence to guide policymakers in their decision making (17, 18).
A position statement with calls to action to improve healthcare transition was recently published in Canada (19). It included a call for increased collaboration between pediatric and adult healthcare providers, as well as a streamlined approach for youth with disabilities as they transition to accessing adult health services across levels of care and sectors. The position statement further highlighted the critical importance of policy changes to support positive, successful transitions; for example, the need for flexible age cut-offs to ensure youth with disabilities are developmentally ready for the transition to adult healthcare, and the need for better access to developmentally appropriate transition planning for youth and families. The Children's Healthcare Canada Transition Hub (5) aligns with this call by uniting family and healthcare partners across the entire continuum of care (i.e., pediatric and adult care), ensuring that transition work is conducted collaboratively and in a coordinated manner, with a firm focus on policy change.
Further, a group of American organizations representing a variety of stakeholders recently identified the transition to adulthood as a health system research priority for YHCN (20). They developed The Blueprint for Change as a result of these meetings, and identified four critical areas to address, including health equity, family and child well-being and quality of life, access to services, and financing of services (21). With substantial care gaps worldwide, transitions that are less than optimal, lead to increased stress and vulnerability for YHCN. The inconsistency of planned, purposeful movement from pediatric to adult services amounts to a global health crisis for YHCN (22, 23). These recent examples illustrate the critical importance of addressing transition to adult care in a meaningful, consistent way, across populations and geographic areas.
Since healthcare transition challenges are not condition-specific, in this paper we take a non-categorical approach to the healthcare transition of youth with disabilities and a variety of healthcare needs, allowing national advocacy for change not only within, but also across conditions and families.
The CHILD-BRIGHT READYorNot™ Brain-Based Disabilities (BBD) Project (24) was initiated to develop and evaluate a patient-facing e-health intervention in four Canadian regions (Alberta, Ontario, Quebec, and the Maritimes). The MyREADY Transition™ BBD Application was designed to enhance healthcare transition readiness in youth with BBD. This project used a patient-oriented research approach to partner with a Patient and Family Advisory Council (PFAC) comprised of youth with disabilities and parents throughout all study phases (25, 26). PFAC meetings occurred regularly and included discussions about a range of topics related to healthcare transition, including how to advocate for changes in policy to improve healthcare transition experiences.
Based on these PFAC discussions, an advocacy working group was developed with the specific goal of identifying recommendations for policy changes in healthcare transition. Our working group collaborated with the Policy Hub (a rapid response unit for policy related to childhood disabilities) within the pan-Canadian CHILD-BRIGHT patient-oriented research network (27, 28).
A two-hour dialogue meeting was conducted in February 2022 with nine synchronous and one asynchronous participant from the four Canadian regions described above. The dialogue was co-facilitated and co-hosted by youth partners from the PFAC, with ethics approval from the Hamilton Integrated Research Ethics Board. Participants included three health care providers, one parent partner, four additional youth partners, and two researchers and/or healthcare administrators. To facilitate discussion at the dialogue, participants were presented with two patient vignettes and prompting questions (See Table 1). At the end of the dialogue, stakeholders were asked to identify their top three recommendations for policy changes. The dialogue was audio-recorded, transcribed, and the transcripts were analyzed using conventional content analysis (29). After reviewing the transcripts, themes were inductively identified; these themes are summarized below.
Youth participants highlighted the importance of not having transfer “sprung on [them] at the last minute”, which can lead to additional stress. They advocated for a gradual process to prepare for transition, in which small goals can be reached to develop their confidence and skills to manage their health before transfer occurs. A researcher summarized the discussion shared among youth:
“It’s really about all of those small manageable goals so that if something’s not so hard and you can achieve it, it’s easier to imagine yourself making that next step or doing that next thing than if something is too big of a goal … it is about an ease of adaptability.”
Healthcare providers shared similar sentiments and highlighted the importance of planning early with youth and their families to set and achieve these goals before the transfer to the adult healthcare system occurs.
Multiple youth shared that transition was more than just healthcare, and that transition to adulthood also includes education, social factors, finances, and transportation supports. One youth shared that he was not aware of financial disability support available to him until two years after he transferred to adult services. Youth also identified the importance of peer support and community resources as transition can often be a very lonely experience. One youth shared how a list of resources can be helpful to prepare for transition:
“I feel that if you give patients very early on a list of resources and groups they can join, or tell them that there are others in the community or other things, activities, and support groups in the community that they can join … I think that would have helped the whole process.”
Another youth described the importance of having resources and opportunities to practice skills that they would apply in adult care:
“It’s also important to not just give the resources but also know how to use them. Rather than giving a phone number and just saying, “Call this number.” To actually practice calling that number and what that looks like.”
Healthcare providers recognized the silo approach that often takes place in services when youth are transitioning to adult care where there is a lack of communication and disconnect between services. They expressed that the delivery of services needs to be changed.
Healthcare providers shared that there was not enough time for them to support their patients and families during transition, as transitional care was often a “side of the desk project”. A healthcare provider thought that:
“The people that work in transition do it because they have a passion and it’s not necessarily part of my paid role, but we fit it in because [we] believe that it’s important for our families, our children.”
One healthcare provider shared that she felt underprepared to transition her patients and that she learned everything on the job:
“At first, I was transferring my patients by making a good chart summary and telling them you're going to see this doctor over there, but my patients came back to me and said … “I was not ready”. So, I was really doing things wrong. So, I have to learn, with time, to do things differently.”
Overall, healthcare providers often felt that they had been undereducated on the complexities of preparing youth for transition. Based on their experiences, transition planning was only prioritized when a provider was willing to invest their own time and resources. They also stressed the importance of working as a team during transition planning, including patients and families, as well as multidisciplinary providers.
Participants further reinforced that transition policies and practices vary greatly from region to region, and even from provider to provider within a region. This uneven implementation of transition policies and practices can lead to inequities in access to services by youth and their families. One healthcare provider stressed the importance not just of having a policy but of also implementing and evaluating the policy:
“So, even if you have policies, and this is kind of a policy to say that this hospital has to have a transition program, otherwise, they don't get accredited, but then you have to look at how they do it. … so, it is not only the policy, and then put this policy in place … but then you have to check if it’s done well.”
Another healthcare provider described the importance of conducting research and evaluating transition outcomes related to implementation:
“Has this implementation really increased or improved any form of transitional care? And if it hasn't, that’s where you improve policy on a long term.”
Providers shared some examples of programs, in which they have participated and felt they were successful. However, they cautioned that the programs' success was often due to the involvement of a single “champion” provider, and it was important to consider the sustainability of these programs. One provider shared her dream of a Transition Bureau in each province and territory, which would have oversight of all healthcare transitions. These Transition Bureaus can communicate with each other to ensure that youth and families have access to the resources they require for healthcare transition.
Overall, both youth and healthcare providers felt that organizations should have clear local and regional policies for their practices with checks and balances when the transfer to the adult care system takes place.
The themes discussed during the dialogue are consistent with published literature over recent decades (30–33), and informed the three recommendations proposed by the discussion group to help to prioritize advocacy initiatives and operationalize change. Transition requires collective responsibility from healthcare providers and provincial/territorial/national government systems. Table 2 summarizes recommendations for action, based on published literature (34) and our perspectives.
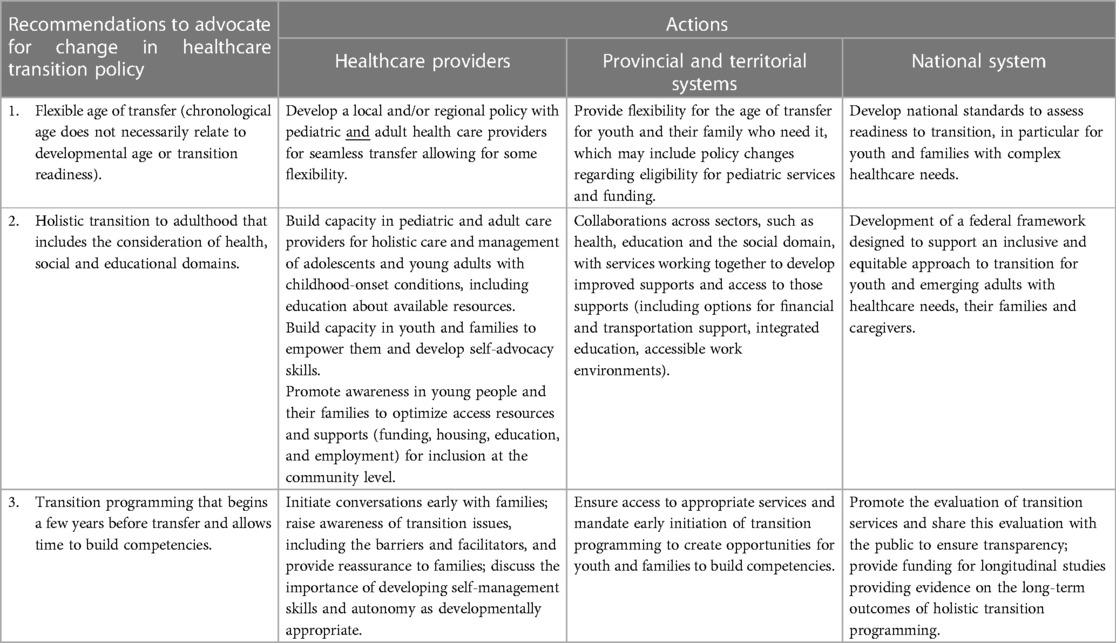
Table 2. Recommendations and collective responsibilities for healthcare providers, and provincial, territorial, and national government systems in Canada to improve healthcare transition.
The first, and perhaps the strongest recommendation from the group, is the need for a more flexible age of transfer (rather than a strict transfer date based on age) since chronological age does not necessarily relate to developmental age or readiness. There are several examples globally of recommendations advocating for a more flexible age of transfer to adult healthcare. For example, the National Health Insurance in Taiwan allows for individuals to access health services from all specialties regardless of age (35). The American Academy of Pediatrics (AAP) policy statement on pediatric age limits argues that 18 or 21 are nothing more than arbitrary numbers to choose to stop pediatric services (36). The AAP policy further suggests that pediatricians may be best suited to provide ongoing care, particularly for youth with complex needs and longstanding relationships with pediatric providers. The policy statement discourages the use of arbitrary age limits on pediatric care, highlighting the uniqueness of each situation, with age being only one of many considerations. Other factors in the timing of transfer can and should include the opinion of the patient/family, the training, abilities, and interests of the providers, with the providers being responsible for balancing their own abilities and limitations with the needs of the patient (36). Tools to benchmark and measure readiness for transition may help understand associated health outcomes (36). The European Alliance of Associations for Rheumatology (EULAR) Pediatric Rheumatology European Society (PReS) developed recommendations for healthcare transition for youth with juvenile-onset rheumatic diseases, and argued that the timing of the transfer could be flexible until the health condition is stable and when the provider considers the youth to be ready for the transfer to adult care services (37). They recommend flexible strategies such as providing opportunities for youth to communicate with adult services prior to the transfer, or having shared clinics between pediatric and adult healthcare providers (37). Such strategies and policies can and should be adopted across Canadian provinces and territories to offer flexibility in the timing of the transfer to adult care. This may include having patients, families and providers working together to agree on the minimum set of requirements to transfer so that healthcare transition can be done equitably and appropriately without a firm age cut-off.
Participants advocated for holistic transition preparation that includes consideration of factors beyond the traditional medical sphere. The transition out of high school to employment, postsecondary education or other post-secondary placements, and the transition to adult disability financial support programs were particularly highlighted. Holistic transition has been a common theme in the published literature as well, with youth and families describing concerns around housing, employment, financial and legal security after transitioning out of pediatric systems (38). Pediatric providers need to consider holistic transition in establishing a plan of care for patients who are transitioning to adulthood. In some cases, these transitional issues only emerge after the transfer to adult care has already taken place, and as such, adult providers need to be prepared to address these areas as well. Unfortunately, many pediatric and adult care providers report a lack of training in this area, and feel unprepared to meet the non-medical needs of patients leaving the pediatric system (39, 40). At a systems level, collaborations can and ideally should occur across sectors, with pediatric and adult services working together to prepare youth and families for the transition to adult services—both medical and social (41).
Thirdly, participants recommended mandated transition programming that begins a few years before transfer and allows time to build competencies. The need to prepare for transition early was frequently highlighted by participants, and also represents one of the core components to support a successful healthcare transition outlined in position statements by both the Canadian Pediatric Society and American Academy of Pediatrics (19, 42). Having these conversations at least one year prior to transition and ideally even earlier, will allow time for youth/families to identify their goals, and develop necessary skills and abilities to take charge of their health (34, 43, 44). Youth with the capacity to do so can work towards gradually becoming more autonomous, with a progressive shifting of responsibility from parents/providers to the patients themselves (34). This may include having youth speak for themselves more in appointments, or taking on more tasks related to their daily care (e.g., refilling their medications) (45). The tasks to work on during this early phase of transition should be uniquely tailored to each individual but can only be a focus of clinical care if efforts are made to uniformly offer transition programming well in advance of transfer to adult services.
This project employed patient vignettes to generate discussion and identify recommendations to improve healthcare transition, laying the groundwork for a more comprehensive discussion with policymakers and health economists (46). Future work may benefit from a broader policy development framework such as the Narrative Policy Framework to understand the role of narratives in the policy process at different levels including at the micro (individual), meso (groups/coalitions/organizations), and macro level (institutions/society) (47).
Youth, families, and healthcare professionals are continuously advocating for policy changes to improve the transition from pediatric to adult healthcare. However, advocating for oneself or family member takes immense amounts of time and energy, and adds burden for families (48–50). Healthcare is a human right (51), and from our perspective, the onus should not be on the most vulnerable to engage in advocacy in order to have their human rights met. A future direction is for policymakers to create appropriate supports for individuals throughout the life course and across sectors.
It is critical to mobilize support for the dignity, rights, and well-being of YHCN throughout the transition to adulthood in Canada and internationally. We hope that this paper authored by youth, parents/caregivers, and healthcare providers is a starting point to advocate for change by providing actionable recommendations to improve transition outcomes for youth and families.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
The studies involving humans were approved by Hamilton Integrated Research Ethics Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
LN: Conceptualization, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. CD-M: Conceptualization, Formal analysis, Methodology, Writing – review & editing. MF: Conceptualization, Methodology, Writing – review & editing. MA: Conceptualization, Methodology, Writing – review & editing. KC: Conceptualization, Methodology, Writing – review & editing. DA: Writing – review & editing. KP: Writing – review & editing. DT: Writing – review & editing. JM: Writing – review & editing. RC: Conceptualization, Formal Analysis, Methodology, Writing – review & editing. BG: Conceptualization, Methodology, Writing – review & editing. SS: Conceptualization, Methodology, Writing – review & editing. AV-DL: Conceptualization, Methodology, Writing – review & editing. CC: Writing – review & editing. DM: Writing – review & editing. SD: Writing – review & editing. HA: Writing – review & editing. AF: Writing – review & editing. AM: Writing – review & editing. JWG: Conceptualization, Methodology, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
We gratefully acknowledge funding from the Child Health Initiatives Limiting Disability–Brain Research Improving Growth and Health Trajectories network, funded under the Canadian Institutes of Health Research (CIHR-SCA-145104) Strategy for Patient-Oriented Research initiative, and with funding partner support from Montreal Children’s Hospital Foundation, Faculty of Health Sciences of McMaster University, New Brunswick Health Research Foundation, McMaster Children's Hospital Foundation and Hamilton Health Sciences.
The authors thank the full CHILD-BRIGHT READYorNotTM Brain-Based Disabilities Trial Study Group and collaborators for their expertise throughout all aspects of our project. We wish to further acknowledge the important contributions of all patients and families who partnered as advisors on our Patient and Family Advisory Council (PFAC): DA, young adult/patient partner in Ontario, Canada; MA, young adult/patient partner in Ontario, Canada; KC, young adult/patient partner in Ontario, Canada; CD-M, young adult/patient partner in Ontario, Canada; MF, young adult/patient partner in Alberta, Canada; Julia Hanes, young adult/patient partner in Ontario, Canada; Jessica Havens, young adult/patient partner in Alberta, Canada; JM, parent/family partner in Quebec, Canada; Kinga Pozniak, parent/family partner in Ontario, Canada; Connie Putterman, parent/family partner in Ontario, Canada; Roger Stoddard (in memory), parent/family partner in New Brunswick, Canada; Nathan Tasker, young adult/patient partner in Ontario, Canada; and Donna Thomson, parent/family partner in Ontario, Canada.
JWG and JM received research grants from the Canadian Institutes of Health Research Strategy for Patient-Oriented Research, and JWG held the Scotiabank Chair in Child Health Research during the duration of this study. BG, LN, SS, and AV-DL were paid for their work as project staff members.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Martinez YJ, Ercikan K. Chronic illnesses in Canadian children: what is the effect of illness on academic achievement, and anxiety and emotional disorders? Child Care Health Dev. (2009) 35(3):391–401. doi: 10.1111/j.1365-2214.2008.00916.x
2. Perrin EC, Newacheck P, Pless IB, Drotar D, Gortmaker SL, Leventhal J, et al. Issues involved in the definition and classification of chronic health conditions. Pediatrics. (1993) 91(4):787–93. doi: 10.1542/peds.91.4.787
3. Human Resources and Skills Development Canada. Disability in Canada: A 2006 Profile (2006). Available at: https://publications.gc.ca/collections/collection_2011/rhdcc-hrsdc/HS64-11-2010-eng.pdf (Cited September 25, 2023).
4. Blum RW, Garell D, Hodgman CH, Jorissen TW, Okinow NA, Orr DP, et al. Transition from child-centered to adult health-care systems for adolescents with chronic conditions. A position paper of the society for adolescent medicine. J Adolesc Health. (1993) 14:570–6. doi: 10.1016/1054-139X(93)90143-D
5. Children’s Healthcare Canada. Health Hub in Transition (2021). Available at: https://www.transitionhub.ca/ (Cited March 31, 2021).
6. Verlenden JV, Zablotsky B, Yeargin-Allsopp M, Peacock G. Healthcare access and utilization for young adults with disability: U.S., 2014–2018. J Adolesc Health. (2022) 70(2):241–8. doi: 10.1016/j.jadohealth.2021.08.023
7. Lugasi T, Achille M, Stevenson M. Patients’ perspective on factors that facilitate transition from child-centered to adult-centered health care: a theory integrated metasummary of quantitative and qualitative studies. J Adolesc Health. (2011) 48(5):429–40. doi: 10.1016/j.jadohealth.2010.10.016
8. Davies H, Rennick J, Majnemer A. Transition from pediatric to adult health care for young adults with neurological disorders: parental perspectives. Can J Neurosci Nurs. (2011) 33(2):32–9.21977770
9. Kennedy A, Sloman F, Douglass JA, Sawyer SM. Young people with chronic illness: the approach to transition. Intern Med J. (2007) 37(8):555–60. doi: 10.1111/j.1445-5994.2007.01440.x
10. Stewart D, Law M, Young NL, Forhan M, Healy H, Burke-Gaffney J, et al. Complexities during transitions to adulthood for youth with disabilities: person-environment interactions. Disabil Rehabil. (2014) 36(23):1998–2004. doi: 10.3109/09638288.2014.885994
11. Last A. Parents of children with complex health needs say they are “slipping through the cracks” (2023). Available at: https://www.chch.com/parents-of-children-with-complex-health-needs-say-they-are-slipping-through-the-cracks/ (Cited August 11, 2023).
12. DeSouza A, Wang D, Wong JJ, Furlan AD, Hogg-Johnson S, Macedo L, et al. Prevalence of unmet rehabilitation needs among Canadians living with long-term conditions or disabilities during the first wave of the COVID-19 pandemic. Arch Phys Med Rehabil. (2023):1–12. doi: 10.1016/j.apmr.2023.07.010 (Epub ahead of print).36170894
13. Sullivan WF, Diepstra H, Heng J, Ally S, Bradley E, Casson I, et al. Primary care of adults with intellectual and developmental disabilities. Can Fam Physician. (2018) 64(4):254–79.29650602
14. SA 2003, c F-5.3. Family support for children with disabilities act. CanLII (2003). Available at: https://www.canlii.org/en/ab/laws/stat/sa-2003-c-f-5.3/latest/sa-2003-c-f-5.3.html#document (Cited August 15, 2023).
15. IWK Health Centre. Transition to adult health care (2023). Available at: https://www.iwk.nshealth.ca/transitions (Cited August 15, 2023).
16. Canada H. Canada’s health care system (2011). Available at: https://www.canada.ca/en/health-canada/services/health-care-system/reports-publications/health-care-system/canada.html (Cited August 11, 2023).
17. Canadian Association of Paediatric Health Centres. A guideline for transition from paediatric to adult health care for youth with special health care needs: A national approach (2016). Available at: https://www.childhealthbc.ca/sites/default/files/caphc_transition_to_adult_health_care_guideline_may_2017.pdf (Cited August 15, 2023).
18. Cleverley K, Gore D, Nasir S, Ashley T, Rich L, Brown C, et al. Facilitating effective transitions from hospital to community for children and adolescent mental health services: overview of the transition support worker role and function. J Can Acad Child Adolesc Psychiatry. (2018) 27(4):228–35.30487938
19. Toulany A, Gorter JW, Harrison ME, Canadian Pediatric Society, Adolescent Health Committee. A call for action: recommendations to improve transition to adult care for youth with complex health care needs (2022). Available at: https://cps.ca/en/documents/position/transition-to-adult-care-for-youth (Cited April 15, 2022).
20. Coller RJ, Berry JG, Kuo DZ, Kuhlthau K, Chung PJ, Perrin JM, et al. Health system research priorities for children and youth with special health care needs. Pediatrics. (2020) 145(3):e20190673. doi: 10.1542/peds.2019-0673
21. McLellan SE, Mann MY, Scott JA, Brown TW. A blueprint for change: guiding principles for a system of services for children and youth with special health care needs and their families. Pediatrics. (2022) 149(Supplement 7):e2021056150C. doi: 10.1542/peds.2021-056150C
22. Narla NP, Ratner L, Bastos FV, Owusu SA, Osei-Bonsu A, Russ CM. Paediatric to adult healthcare transition in resource-limited settings: a narrative review. BMJ Paediatr Open. (2021) 5(1):e001059. doi: 10.1136/bmjpo-2021-001059
23. Kerr H, Widger K, Cullen-Dean G, Price J, O’Halloran P. Transition from children’s to adult services for adolescents/young adults with life-limiting conditions: developing realist programme theory through an international comparison. BMC Palliat Care. (2020) 19(1):115. doi: 10.1186/s12904-020-00620-2
24. Gorter JW, Amaria K, Kovacs A, Rozenblum R, Thabane L, Galuppi B, et al. CHILD-BRIGHT READYorNot brain-based disabilities trial: protocol of a randomised controlled trial (RCT) investigating the effectiveness of a patient-facing e-health intervention designed to enhance healthcare transition readiness in youth. BMJ Open. (2021) 11:48756. doi: 10.1136/bmjopen-2021-048756
25. Baumgardner DJ. Defining patient-oriented research for the average person (and potential research partner). J Patient Cent Res Rev. (2019) 6(1):4–6. doi: 10.17294/2330-0698.1697
26. Government of Canada - Canadian Institutes of Health Research. Strategy for patient-oriented research (2021). Available at: https://cihr-irsc.gc.ca/e/41204.html (Cited November 7, 2021).
27. CHILD-BRIGHT Network. About us: what is CHILD-BRIGHT? (2019). Available at: https://www.child-bright.ca/what-is-child-bright (Cited April 18, 2022).
28. CHILD-BRIGHT Network. Knowledge mobilization. Available at: https://www.child-bright.ca/knowledge-mobilization (Cited August 11, 2023).
29. Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. (2005) 15(9):1277–88. doi: 10.1177/1049732305276687
30. Gorter JW, Stewart D, Woodbury-Smith M. Youth in transition: care, health and development. Child Care Health Dev. (2011) 37(6):757–63. doi: 10.1111/j.1365-2214.2011.01336.x
31. Betz CL, Lobo ML, Nehring WM, Bui K. Voices not heard: a systematic review of adolescents’ and emerging adults’ perspectives of health care transition. Nurs Outlook. (2013) 61(5):311–36. doi: 10.1016/j.outlook.2013.01.008
32. Brown M, Macarthur J, Higgins A, Chouliara Z. Transitions from child to adult health care for young people with intellectual disabilities: a systematic review. J Adv Nurs. (2019) 75(11):2418–34. doi: 10.1111/jan.13985
33. Osako M, Yamaoka Y, Takeuchi C, Mochizuki Y, Fujiwara T. Health care transition for cerebral palsy with intellectual disabilities: a systematic review. Rev Neurol (Paris). (2023) 179(6):585–98. doi: 10.1016/j.neurol.2022.11.013
34. Gorter JW, Gibson BE. Independence in adulthood: ethical challenges in providing transitional care for young people with neurodevelopmental impairments. In: Rosenbaum PL, Ronen GM, Racine E, Johannesen J, Dan B, editors. Ethics in child health: Principles and cases in neurodisability. London: Mac Keith Press (2016):335–48.
35. Jin YT, Chen CM, Chien WC. Factors influencing transitional care from adolescents to young adults with cancer in Taiwan: a population-based study. BMC Pediatr. (2016) 16(1):122. doi: 10.1186/s12887-016-0657-z
36. Hardin AP, Hackell JM, Committee on Practice and Ambulatory Medicine, Simon GR, Boudreau ADA, Baker CN, et al. Age limit of pediatrics. Pediatrics. (2017) 140(3):e20172151. doi: 10.1542/peds.2017-2151
37. Foster HE, Minden K, Clemente D, Leon L, McDonagh JE, Kamphuis S, et al. EULAR/PReS standards and recommendations for the transitional care of young people with juvenile-onset rheumatic diseases. Ann Rheum Dis. (2017) 76(4):639–46. doi: 10.1136/annrheumdis-2016-210112
38. Rehm RS, Fuentes-Afflick E, Fisher LT, Chesla CA. Parent and youth priorities during the transition to adulthood for youth with special health care needs and developmental disability. Adv Nurs Sci. (2012) 35(3):E57–72. doi: 10.1097/ANS.0b013e3182626180
39. Gorter JW, Roebroeck M. Transition to adulthood: enhancing health and quality of life for emerging adults with neurological and developmental conditions. In: Ronen GM, Rosenbaum PL, editors. Life quality outcomes in children and yong people with neurological and developmental conditions: Concepts, evidence and practice. London: Mac Keith Press (2013). p. 302–13.
40. Aisen ML, Kerkovich D, Mast J, Mulroy S, Wren TA, Kay RM, et al. Cerebral palsy: clinical care and neurological rehabilitation. Lancet Neurol. (2011) 10(9):844–52. doi: 10.1016/S1474-4422(11)70176-4
41. Stewart D. Transition to adult services for young people with disabilities: current evidence to guide future research. Dev Med Child Neurol. (2009) 51(Supp. 4):169–73. doi: 10.1111/j.1469-8749.2009.03419.x
42. American Academy of Pediatrics, American Academy of Family Physicians, American College of Physicians. Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics. (2011) 128:182–200. doi: 10.1542/peds.2011-0969
43. King GA, Baldwin PJ, Currie M, Evans J. The effectiveness of transition strategies for youth with disabilities. Children’s Health Care. (2006) 35(2):155–78. doi: 10.1207/s15326888chc3502_4
45. Reiss JG, Gibson RW, Walker LR. Health care transition: youth, family, and provider perspectives. Pediatrics. (2005) 115(1):112–20. doi: 10.1542/peds.2004-1321
46. Niessen LW, Grijseels EWM, Rutten FFH. The evidence-based approach in health policy and health care delivery. Soc Sci Med. (2000) 51(6):859–69. doi: 10.1016/S0277-9536(00)00066-6
47. Shanahan EA, Jones MD, McBeth MK. How to conduct a narrative policy framework study. Soc Sci J. (2018) 55(3):332–45. doi: 10.1016/j.soscij.2017.12.002
48. Robins. The dark side to advocacy. (2021). Available at: https://www.linkedin.com/pulse/dark-side-advocacy-sue-robins (Cited September 25, 2023).
49. Fuld Nasso S, Porter LD, McNiff Landrum KK. The benefits and burdens of patient advocacy. JCO. (2021) 39(28_suppl):204–204. doi: 10.1200/JCO.2020.39.28_suppl.204
50. Woolf E, de Bie A. Politicizing self-advocacy: disabled students navigating ableist expectations in postsecondary education. Disabil Stud Q. (2022) 42(1). doi: 10.18061/dsq.v42i1.8062
51. Health is a fundamental human right. Available at: https://www.who.int/news-room/commentaries/health-is-a-fundamental-human-right (Cited September 25, 2023).
Keywords: healthcare transition, equity, advocacy, human right, policy, disabilities, patient-oriented research, youth and families
Citation: Nguyen L, Dawe-McCord C, Frost M, Arafeh M, Chambers K, Arafeh D, Pozniak K, Thomson D, Mosel J, Cardoso R, Galuppi B, Strohm S, Via-Dufresne Ley A, Cassidy C, McCauley D, Doucet S, Alazem H, Fournier A, Marelli A and Gorter JW (2023) A commentary on the healthcare transition policy landscape for youth with disabilities or chronic health conditions, the need for an inclusive and equitable approach, and recommendations for change in Canada. Front. Rehabil. Sci. 4:1305084. doi: 10.3389/fresc.2023.1305084
Received: 30 September 2023; Accepted: 27 November 2023;
Published: 14 December 2023.
Edited by:
Thorsten Langer, University of Freiburg, GermanyReviewed by:
Silvia Filogna, Stella Maris Foundation (IRCCS), Italy© 2023 Nguyen, Dawe-McCord, Frost, Arafeh, Chambers, Arafeh, Pozniak, Thomson, Mosel, Cardoso, Galuppi, Strohm, Via-Dufresne Ley, Cassidy, McCauley, Doucet, Alazem, Fournier, Marelli and Gorter. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Linda Nguyen bGluZGEubmd1eWVuMkBtY2dpbGwuY2E=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.